Thu, Jan 29, 2026
Volume 15, Issue 4 (Autumn 2025)
PTJ 2025, 15(4): 333-344 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Aslani F, Ranjbaripour T, Meschi F, Shokrgozar A, Sodagar S. The Effectiveness of Aerobic Exercise With or Without Mindfulness on Fasting Blood Sugar, Hemoglobin A1C, and Depression Levels in Women With Type 2 Diabetes. PTJ 2025; 15 (4) :333-344
URL: http://ptj.uswr.ac.ir/article-1-688-en.html
URL: http://ptj.uswr.ac.ir/article-1-688-en.html
Fatemeh Aslani1 

 , Tahereh Ranjbaripour *1
, Tahereh Ranjbaripour *1 
 , Farahnaz Meschi1
, Farahnaz Meschi1 

 , Alireza Shokrgozar1
, Alireza Shokrgozar1 
 , Sheida Sodagar1
, Sheida Sodagar1 



 , Tahereh Ranjbaripour *1
, Tahereh Ranjbaripour *1 
 , Farahnaz Meschi1
, Farahnaz Meschi1 

 , Alireza Shokrgozar1
, Alireza Shokrgozar1 
 , Sheida Sodagar1
, Sheida Sodagar1 

1- Department of Health Psychology, Ka.C., Islamic Azad University, Karaj, Iran.
Full-Text [PDF 781 kb]
(409 Downloads)
| Abstract (HTML) (1150 Views)
Full-Text: (423 Views)
Introduction
Diabetes is the most common cause of death worldwide. The prevalence and incidence of type 2 diabetes (T2D) increased by 24.3% worldwide between 1990 and 2021. By 2050, it is projected that 1.31 billion people will have T2D [1]. In Iran, the prevalence of diabetes is relatively high, with 15% of the adult population affected and over 25% in the pre-diabetes stage [2]. To avoid acute complications and lower the risk of long-term diabetes-related complications, multifaceted treatments are required [3]. Regardless of the patient’s age, suitable and applicable management methods that engage patients in managing their disease can help improve their health and quality of life by controlling glycated hemoglobin A1C (HbA1C) levels [4]. Information and health education alone may be insufficient for many individuals to achieve permanent changes. While the benefits of proven pharmacological treatments are established, there is an increasing interest in complementary and alternative medicine, especially in mind-body interventions [5]. Due to its psychological benefits, mindfulness, which originated in ancient Buddhist traditions, has become increasingly integrated into contemporary medical practices [3]. Meditation-based interventions have shown positive effects in managing stress and diabetes by modulating neuro-humoral mechanisms [6]. Researchers have demonstrated increased interest in how mindfulness interventions can be effective in managing blood sugar levels and improving the mental wellbeing of people with diabetes [7]. The simultaneous presence of psychological and physical diseases presents a major challenge to global healthcare. Depression is twice as prevalent in individuals with diabetes as in those without diabetes. The presence of depression in individuals with diabetic also leads to poor diabetes management [8]. Mental health issues, such as depression can exacerbate diabetes by affecting how individuals think, their adherence to treatment, and their practice of self-care. Conversely, diabetes can worsen mental health problems. Fortunately, if one improves, the other tends to improve as well [9]. Recent neuroimaging studies have demonstrated that a range of contemplative practices, including mindfulness meditation, are related to changes in the patterns of communication between the main brain networks traditionally associated with various cognitive functions, including attention, self-processing, rumination, and insight, thereby improving depression [10]. Mindfulness can foster long-term adherence to exercise and motivation for diabetes management by focusing on the mind-body relationship and observing current experiences in a non-judgmental and non-evaluative manner, which in turn can help reduce depression and blood sugar levels [11]. Care guidelines presented by both mindfulness experts and healthcare professionals can effectively alleviate the distress and depression of patients, leading to an increase in their self-care abilities. Mindfulness is proposed as a low-cost psychological therapeutic intervention with lasting benefits, reinforcing therapeutic effects, and reducing medical costs [12]. One of the most crucial recommendations for treating diabetes is regular exercise and an active lifestyle. Despite the awareness of the beneficial role of exercise in diabetes, adherence to exercise regimens among patients is often low [13]. People who master mindfulness learn how to deal with intrusive negative thoughts and cultivate a present-moment awareness. With the help of mindfulness, people can keep the motivational engine running for exercising and managing diabetes, and become aware of the feelings that cause frustration in continuing their treatment. Incorporating mindfulness exercises into physical activity increases patients’ willingness to engage in physical activity and enhances their awareness of bodily sensations during exercise [14]. Glucose and cortisol levels in women with T2D can be better managed by mindfulness, combined with aerobic exercise [15]. Mindfulness through focused attention and mind-body awareness can promote the sustainable exercise regimens [16]. In terms of sex, the risk of both cardiovascular diseases and mortality in females with diabetes is higher than that in males. Therefore, understanding the types of interventions that may increase diabetes diagnosis, especially in T2D women, can help reduce gender inequalities in diabetes [17].
While the effects of each of the interventions, exercise and mindfulness, on diabetes have been widely studied, fewer studies have investigated the effect of combining aerobic exercise with mindfulness therapy. Therefore, new interventions are needed that not only facilitate successful behavior change in physical activity but also address barriers that typically affect the performance and adherence to exercise. Accordingly, the present study aimed to examine the effectiveness of aerobic exercise, with and without mindfulness, on fasting blood sugar, HbA1C, and depression levels in women with T2D.
Materials and Methods
A pre- and post-test quasi-experimental research design with a three-month follow-up, involving three experimental groups and one control group was used in this study. The study population consisted of all women with T2D who visited Sasan Sharghi’s diabetes center in Karaj City in 2023. Since it is recommended that experimental studies have at least 15 participants per group [18], the sample size was determined to be 60 (15 participants in each group) [15]. We had to use the sampling method available at one of the diabetes centers, which is one of the study’s limitations. The participants were randomly allocated to four groups using a random number generator: Three experimental groups (n=15 participants per group) and one control group (n=15). The aerobic exercise group included 15 individuals who received aerobic exercise training in addition to their medical treatment. The second group, consisting of 15 participants, underwent mindfulness treatment, while the third group (n=15) engaged in aerobic exercise three times a week and mindfulness training once a week. The control group received only medical treatments. The inclusion criteria included women with T2D aged 45-60 years who could perform moderate-intensity aerobic exercise, without other chronic diseases, and no involvement in any auxiliary or comprehensive therapeutic approaches before or during the study. Additionally, participants were required to have no psychiatric disorders or psychological or psychiatric interventions in the past year. Additionally, participants should not have severe osteoporosis or other exercise restrictions and should not have participated in systematic aerobic exercises or mindfulness practices prior to joining the group. The exclusion criteria were missing two or more regularly scheduled therapy sessions, failure to complete assigned tasks, and lack of willingness to continue treatment. Many other factors, such as nutrition, economic and cultural issues, and the type of drugs used, affect blood sugar, but we could not control them in this study. Ethical considerations for the current study included obtaining written informed and voluntary consent, the right to withdraw from the study, maintaining confidentiality, avoiding harm, non-discrimination, and non-exploitation. All participants provided an informed consent to participate in the study. Repeated measures analysis of variance (ANOVA) and Bonferroni post hoc tests were used to analyze the data. All statistical analyses were performed using SPSS software, version 26.
Intervention
Beck depression inventory (BDI-II)
The BDI was first developed by Beck et al. [19]. In 1996, Beck and his associates made significant revisions. This questionnaire consists of 21 items designed to assess both the feedback and symptoms or signs of depression in patients. Respondents were required to use a four-point Likert scale, ranging from zero to three. The items cover areas, such as sadness, pessimism, sense of failure, guilt, insomnia, loss of appetite, and self-dislike. Thus, this scale measures the severity of depression in individuals, encompassing a range of symptoms from mild to very severe, with a scoring range from a minimum of zero to a maximum of 63 [19]. By summing the scores for each item, an individual’s total score is obtained directly. The internal consistency of BDI-2 has been reported to be between 0.73 and 0.92, with an average of 0.86; the α coefficient is 0.86 for patients and 0.8 for controls [20]. In a study conducted by Hamidi et al., the intra-class correlation coefficient was calculated to be 0.81. The internal consistency of the test was 0.93 and 0.64 using Cronbach’s α and split-half methods, respectively. In a convergent validity assessment, the Beck questionnaire demonstrated a correlation of 0.80 with the total score on the GHQ-28. The internal consistency of this questionnaire in the present study was calculated at 0.86 [20].
Mindfulness intervention
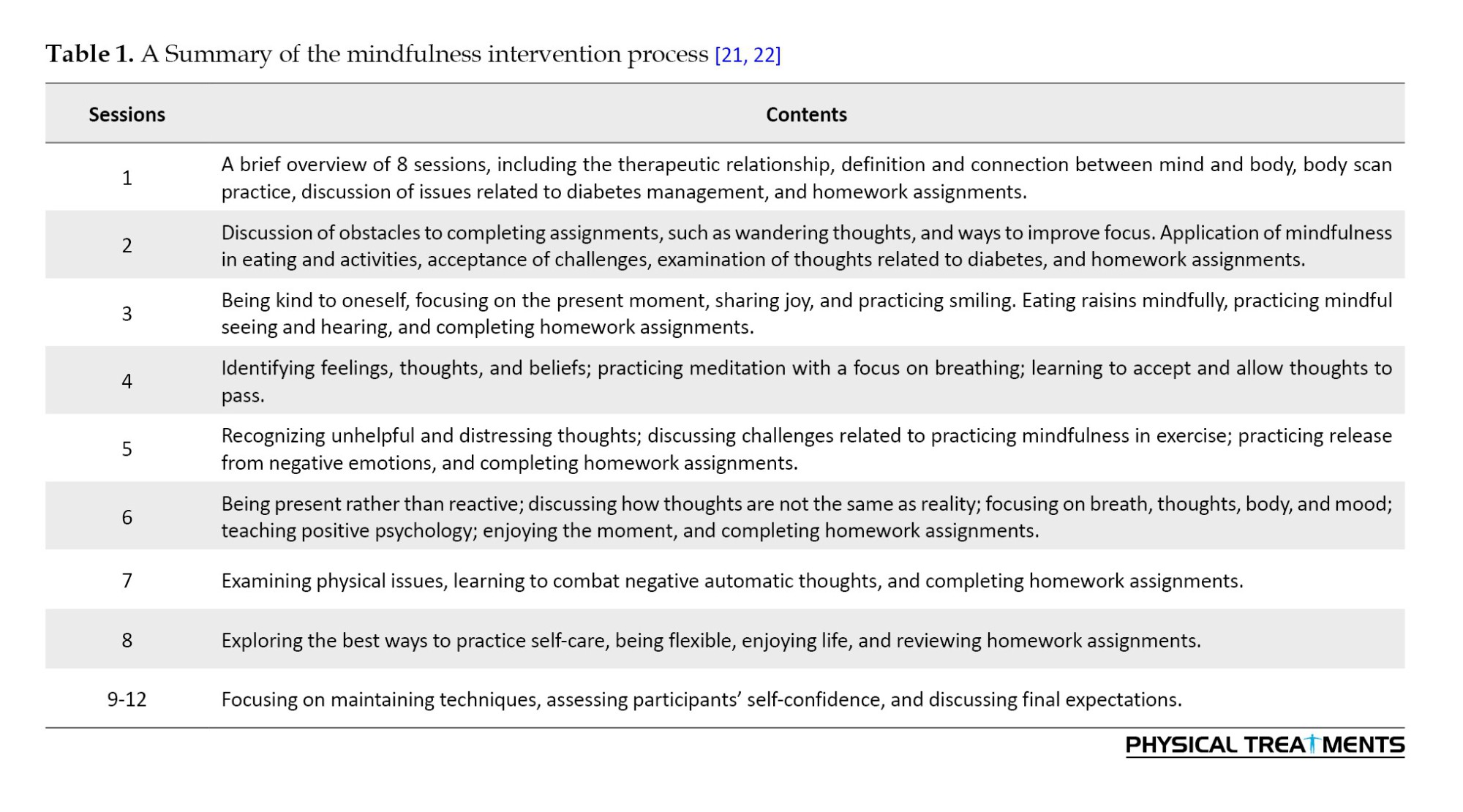
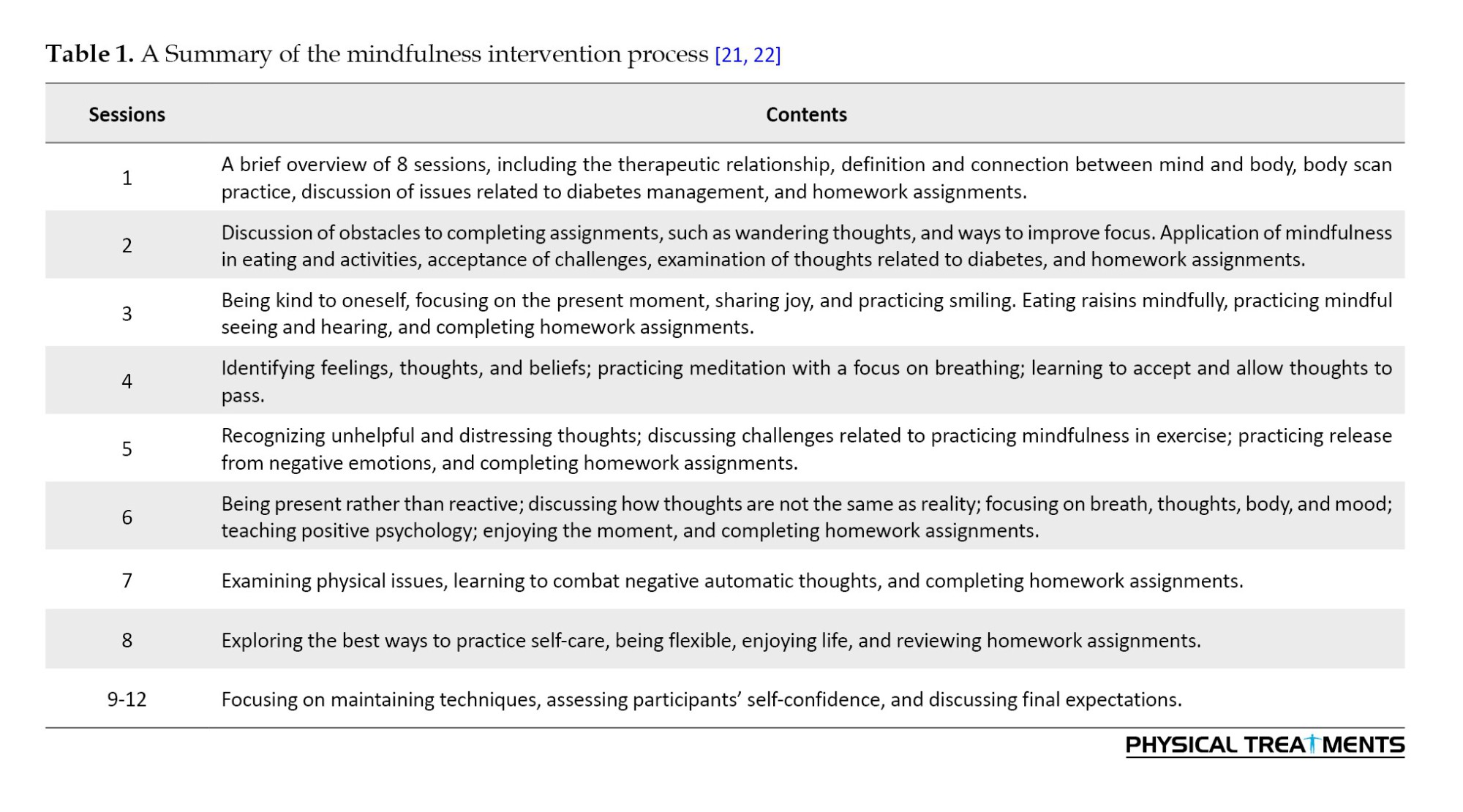
Two authors were present in each intervention session. After practicing the techniques and assigning tasks for the next session, they monitored the completion of tasks from the previous session. Obstacles to completing the tasks were identified and a solution was taught, ensuring task completion (Table 1).
Aerobic exercise
Summary of aerobic exercise intervention based on the Cooper protocol [23]:
Each aerobic exercise session lasted 30 minutes (three times a week for 12 weeks). The participants performed a 10-minute warm-up (such as light jogging, combined hand and foot movements, and stretching), followed by 15 minutes of the main exercise. The main exercise involved walking, which gradually increased in intensity and ended with running. Each session ended with a 5-minute cool-down to return to a resting state. During aerobic exercises, participants were encouraged to walk and incorporate hand and foot movements as needed throughout the session when they became fatigued. Given the participants’ lack of regular exercise and poor fitness, the first two weeks focused on brisk walking (with a heart rate intensity of approximately 60% of maximum heart rate for 20-25 minutes). The exercise intensity and duration were gradually increased each week. A doctoral student in physical education used a heart rate monitor to display heart rate and measure the target intensity of 60%. In this study, we calculated the intensity of approximately 60% of the maximum heart rate using a heart rate display watch with the help of two physical education students.
Procedure
Necessary permissions were obtained to conduct this study on women with T2D. First, the participants were contacted and invited to participate. Next, they were informed about the research, its objectives, and the publication of results. Eligible participants then completed the self-reporting tools. Finally, data were collected once the self-reporting tools were completed. Upon their visit, patients were provided with additional explanations regarding the research, its objectives, and how the results would be published. The BDI-II, fasting blood sugar, and HbA1C levels were measured in both the control and intervention groups, before, immediately after, and three months after the intervention.
Results
Table 2 presents the ages and education levels of the participants.
Table 2 presents both the Mean±SD of the participants’ age. The one-way ANOVA test results indicated that no statistically significant difference was found among the four groups in terms of age mean. The frequency of participants’ education levels is observed in the Table 2, and the Fisher’s exact test results showed no statistically significant difference among the groups in terms of education levels.
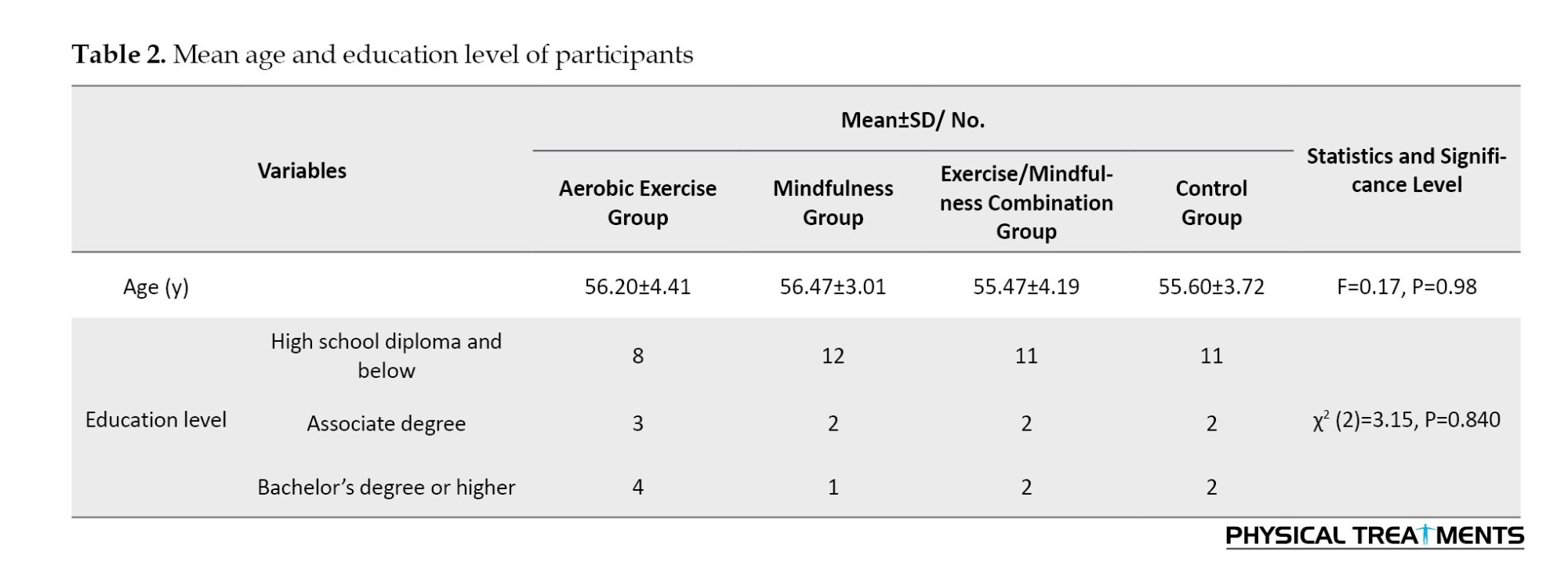
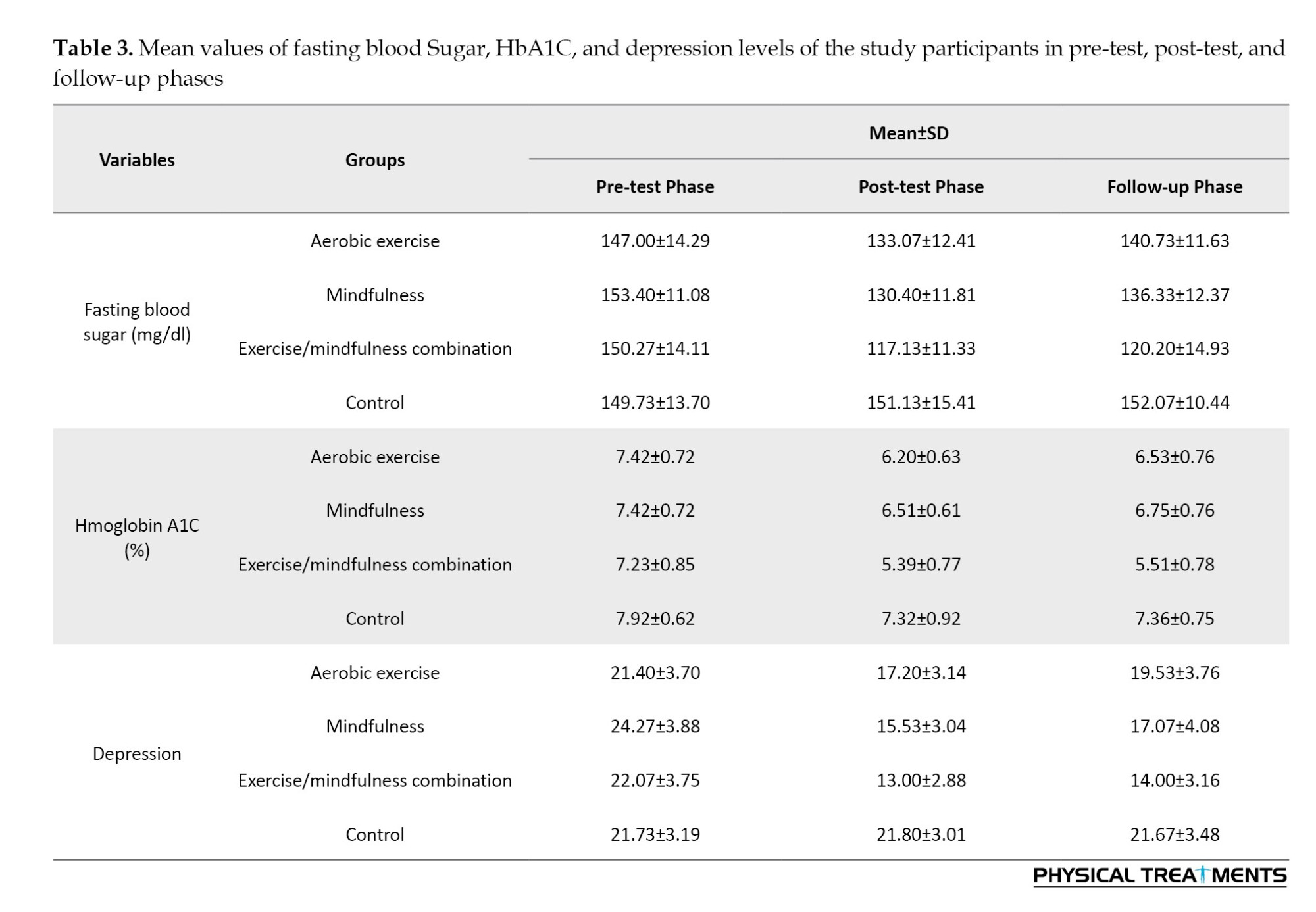
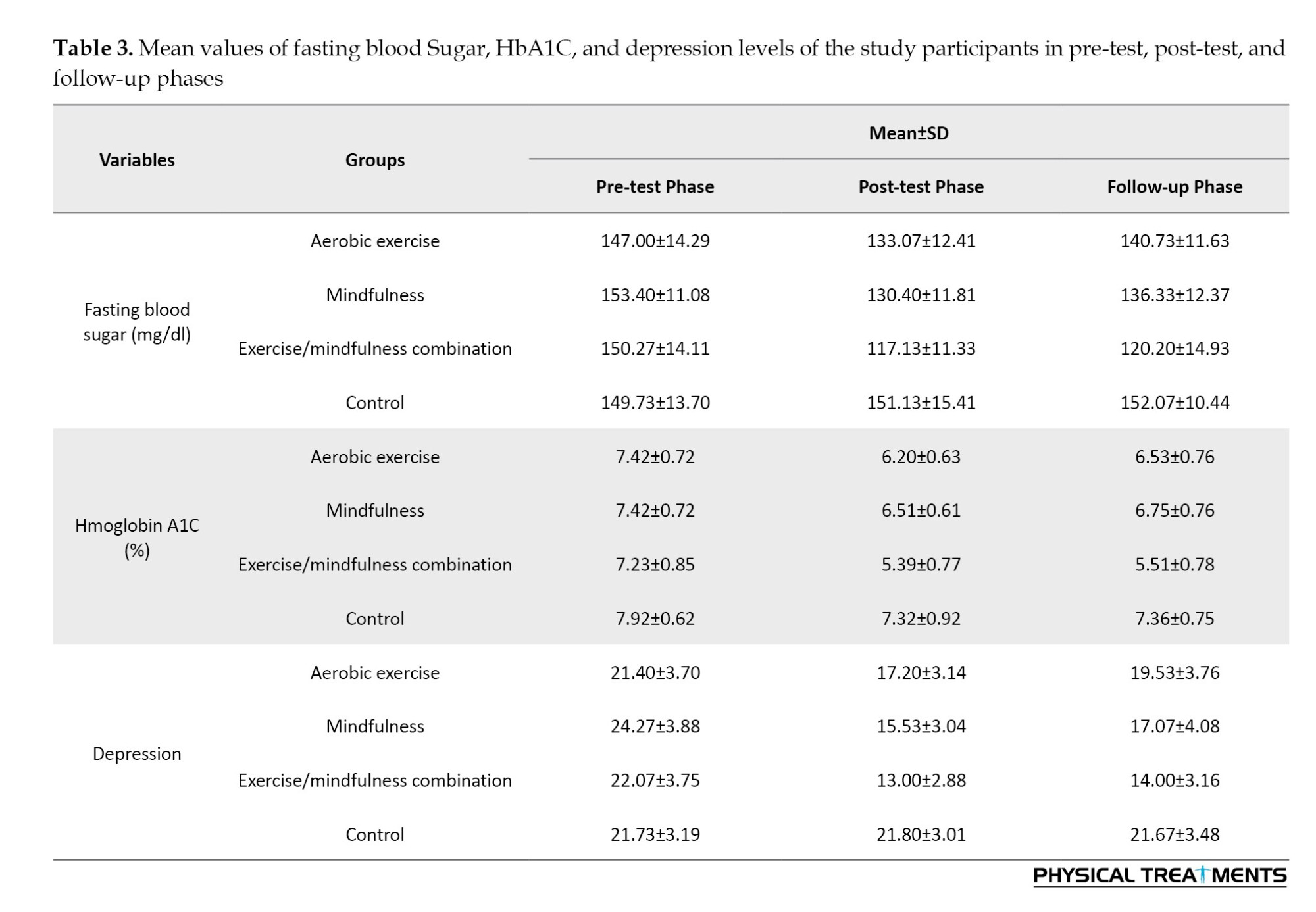
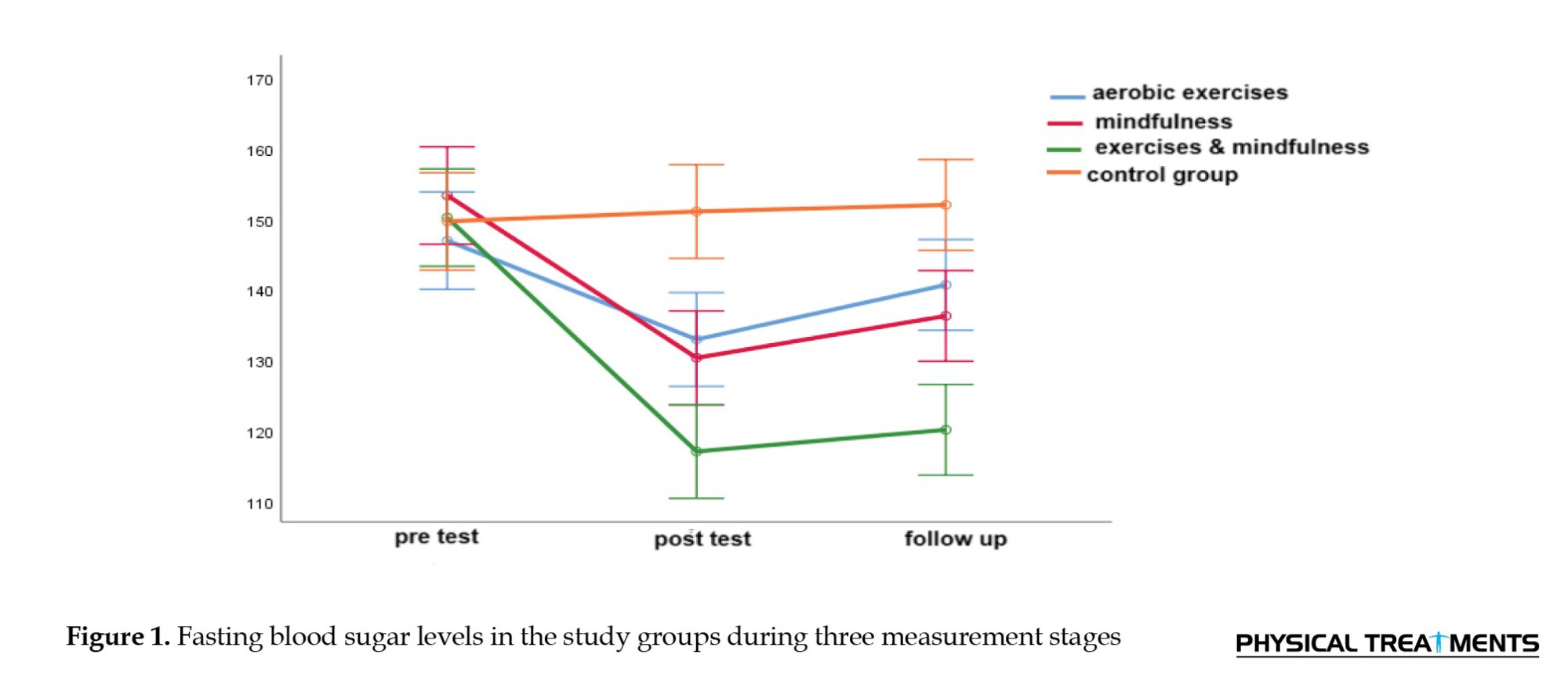
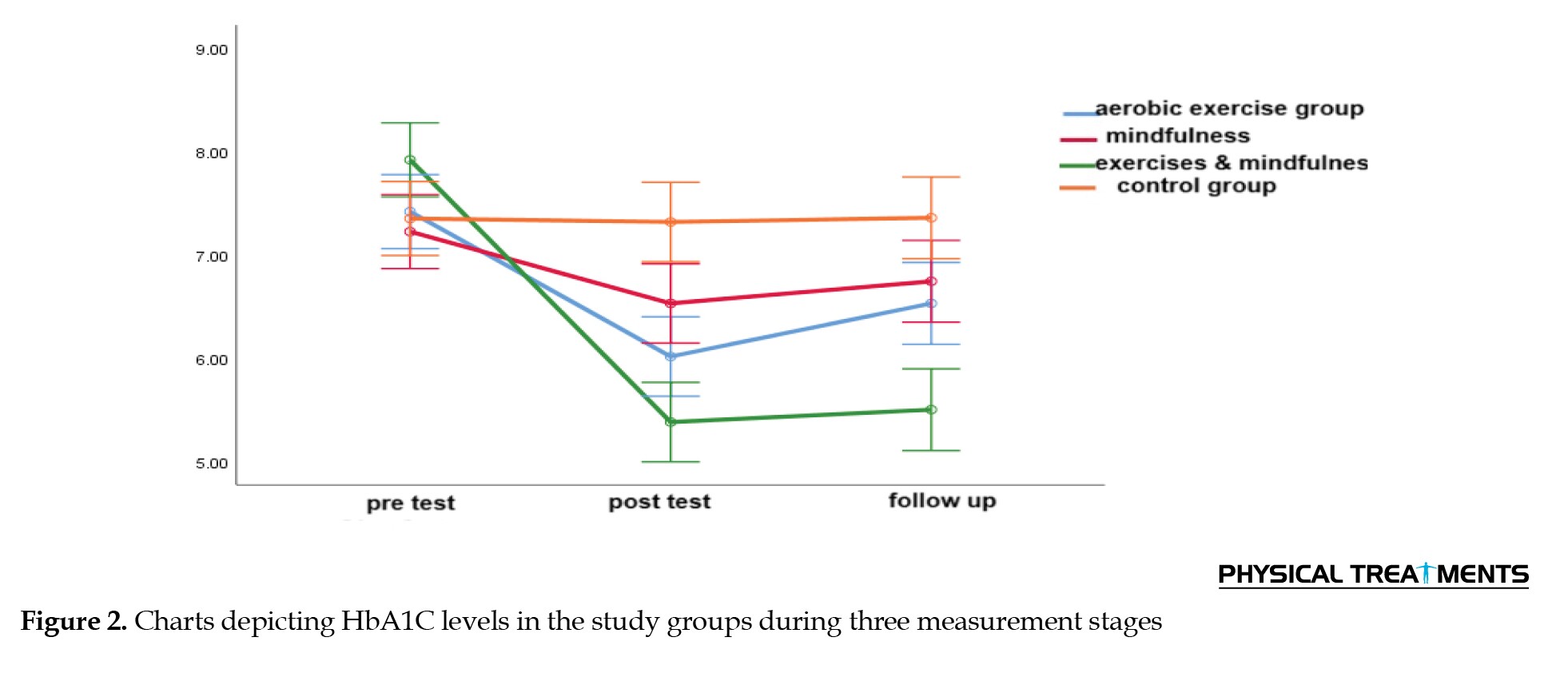
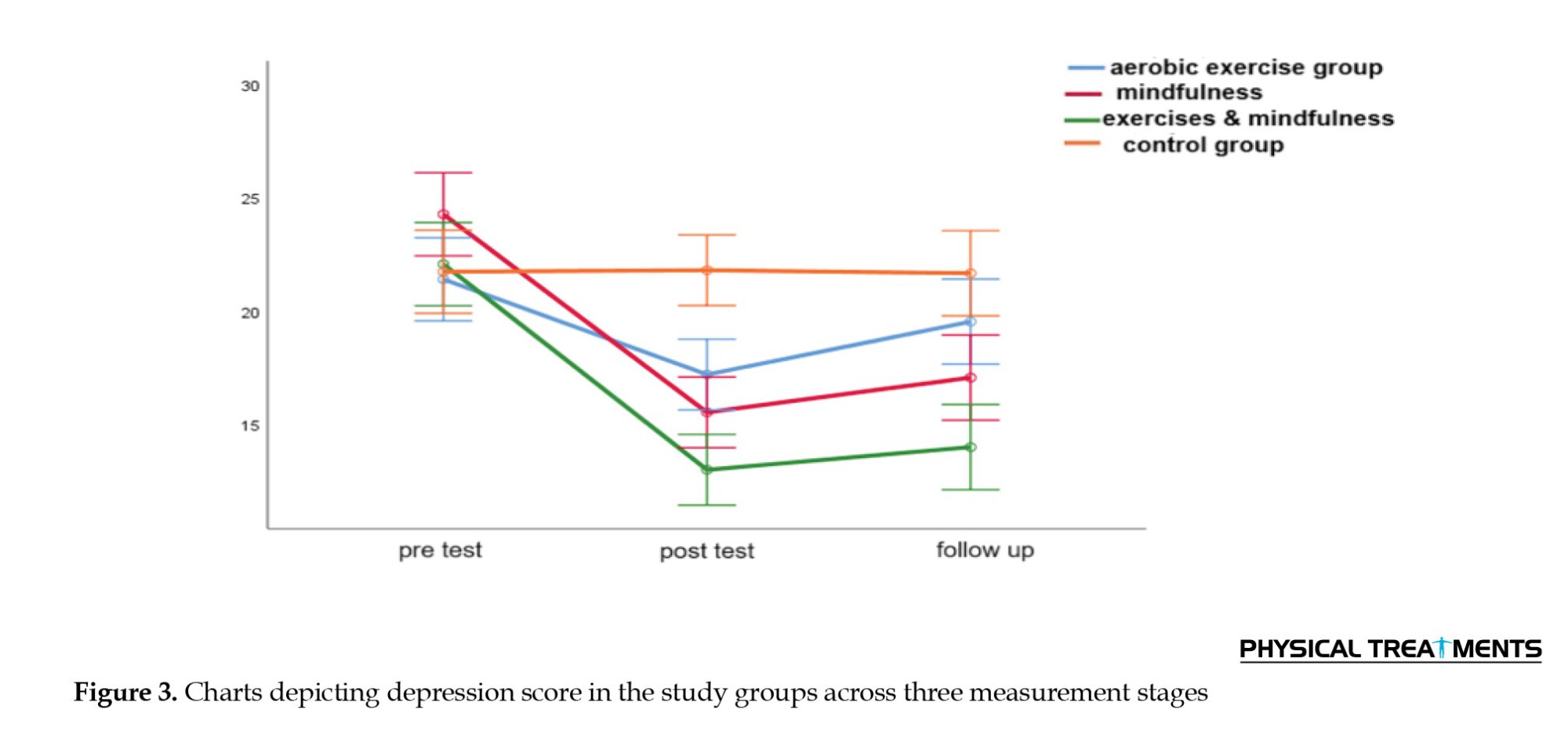
Table 3 presents the Mean±SD of fasting blood sugar and depression levels among the four groups in the pre-test, post-test, and follow-up phases.
As shown in Table 3, the mean values of the research variables (including fasting blood sugar, HbA1C, and depression levels) were lower in the intervention groups compared to the controls in both the post-test and follow-up phases. In contrast, no similar changes were observed in the controls during these phases.
The assumptions of repeated measures ANOVA were assessed before testing the research hypotheses. The assumption of normal distribution of the data was assessed using the Shapiro-Wilk test, suggesting that the data were normally distributed. Mauchly’s test was employed to assess the assumption of equality of the covariance matrices of the dependent variables. The results confirmed that this assumption was also met (P>0.05). The sphericity or equality of the error covariance matrix was evaluated using Mauchly’s test. The chi-square value obtained from Mauchly’s test for fasting blood sugar levels was P=0.005, for HbA1C levels was P=0.001, and for depression was P=0.672. Since the sphericity assumption was not met for fasting blood sugar levels, the degrees of freedom for the variables were adjusted using the Greenhouse-Geisser method.
Table 4 presents the results obtained from the multivariate analysis of the effectiveness of aerobic exercise with and without mindfulness on fasting blood sugar, HbA1C, and depression levels.
As shown in Table 4, aerobic exercise with and without mindfulness had a significant effect on fasting blood sugar (Wilks’ Lambda=0.440, η²=0.336, P=0.001, F=9.30), HbA1C (Wilks’ Lambda=0.419, η²=0.353, P=0.001, F=10.03), and depression levels (Wilks’ Lambda=0.482, η²=0.305, P=0.001, F=8.06).
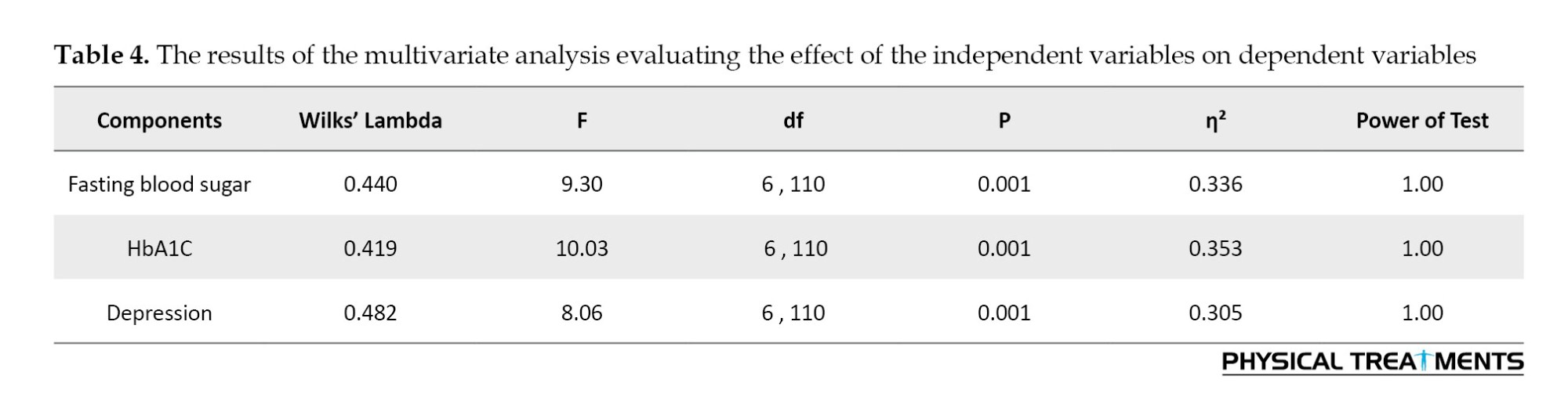
Table 5 presents the results of the repeated-measures ANOVA assessing the effect of aerobic exercise with and without mindfulness on fasting blood sugar, HbA1C, and depression levels.
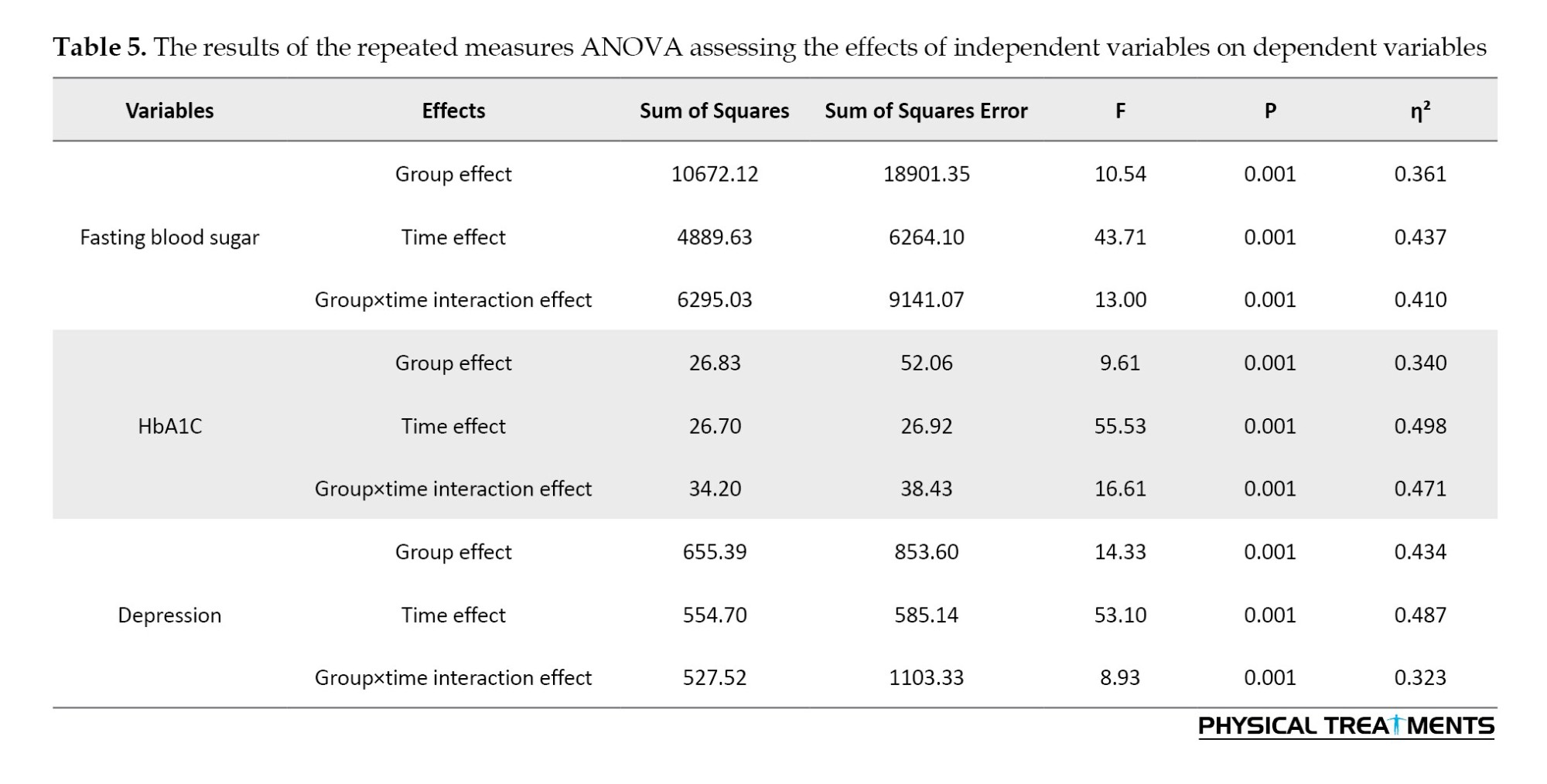
Table 5 shows that the interaction effect of group×time on fasting blood sugar (η²=0.410, P=0.001, F=13.00), and HbA1C levels (η²=0.471, P=0.001, F=16.61), and depression (η²=0.323, P=0.001, F=8.93) was significant. These findings revealed that the independent variables had a significant effect on fasting blood sugar, HbA1C, and depression levels. Table 6 presents the results obtained from the Bonferroni post hoc test, comparing the mean scores of fasting blood sugar, HbA1C, and depression levels among the four groups across three phases.
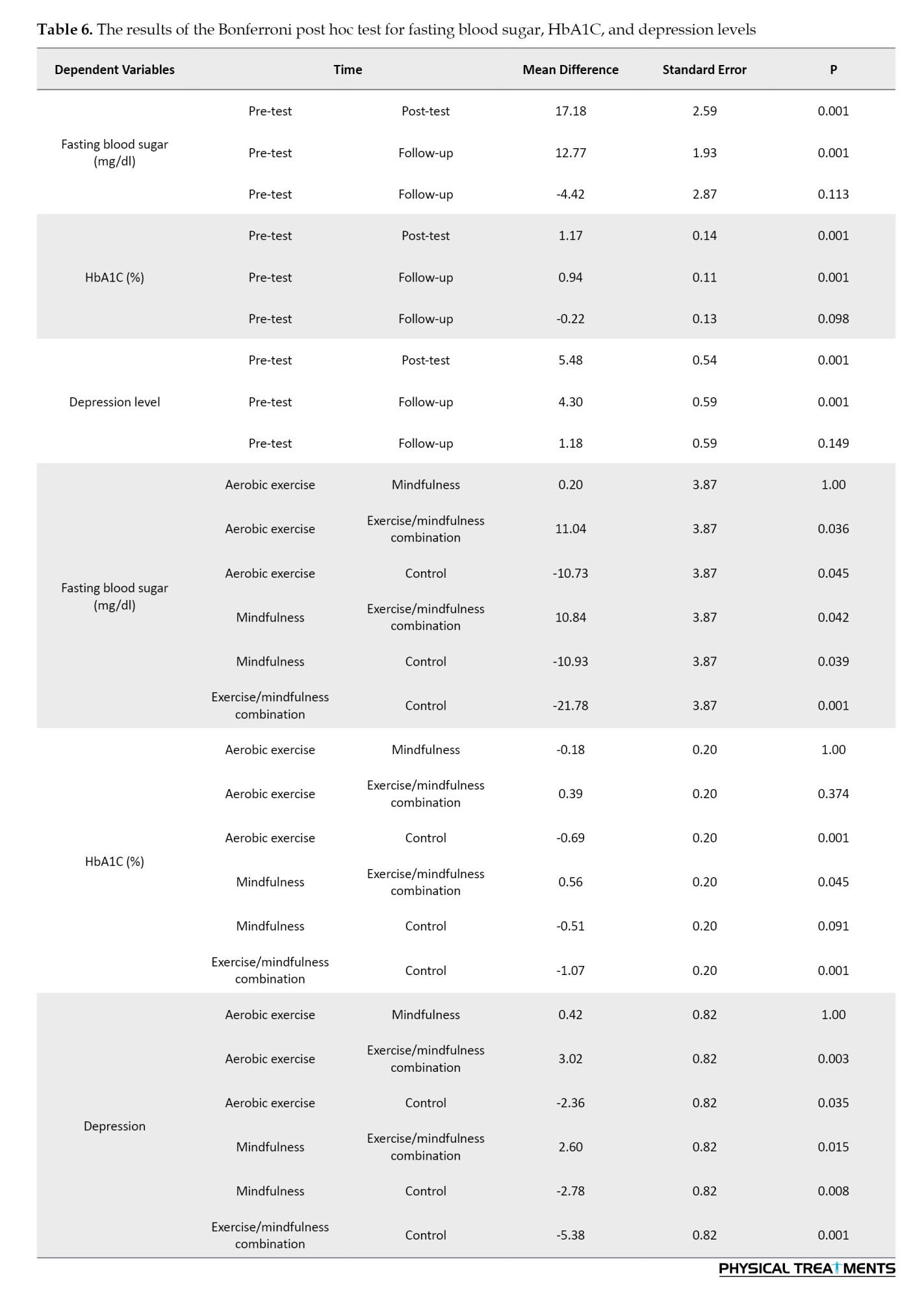
As shown in Table 6, the Bonferroni test results demonstrated statistically significant difference between the effects of aerobic exercise and aerobic exercise combined with mindfulness therapy (P=0.036), as well as between mindfulness and aerobic exercise combined with mindfulness (P=0.042) on fasting blood sugar levels. Specifically, the combination of aerobic exercise and mindfulness significantly reduced fasting blood sugar levels in participants compared to either aerobic exercise alone or mindfulness alone. No statistically significant differences were observed between the effects of aerobic exercise and mindfulness alone on fasting blood sugar levels. Therefore, it can be concluded that aerobic exercise combined with mindfulness is more effective in reducing fasting blood sugar levels in women with T2D compared to either aerobic exercise or mindfulness alone.
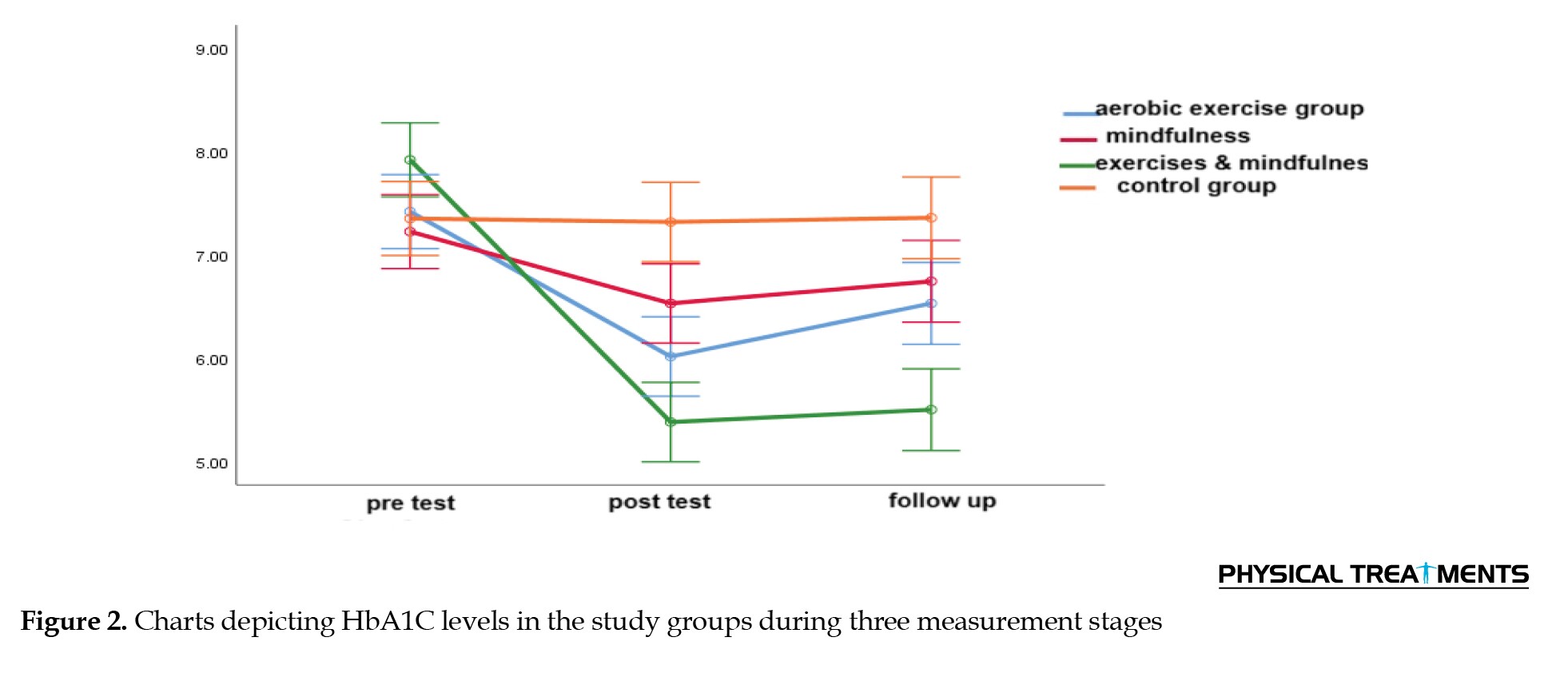
As shown in Table 6, no statistically significant difference was observed in the effects of aerobic exercise and the combination of aerobic exercise and mindfulness on HbA1c levels, as well as between the effects of aerobic exercise and mindfulness treatment alone on HbA1c levels. However, a significant difference was observed between mindfulness and the combination of aerobic exercise and mindfulness (P=0.045), showing a greater reduction in HbA1c levels compared to mindfulness alone. Thus, it can be concluded that the combination of aerobic exercise and mindfulness was more effective in reducing HbA1c levels in women with T2D than mindfulness intervention alone.
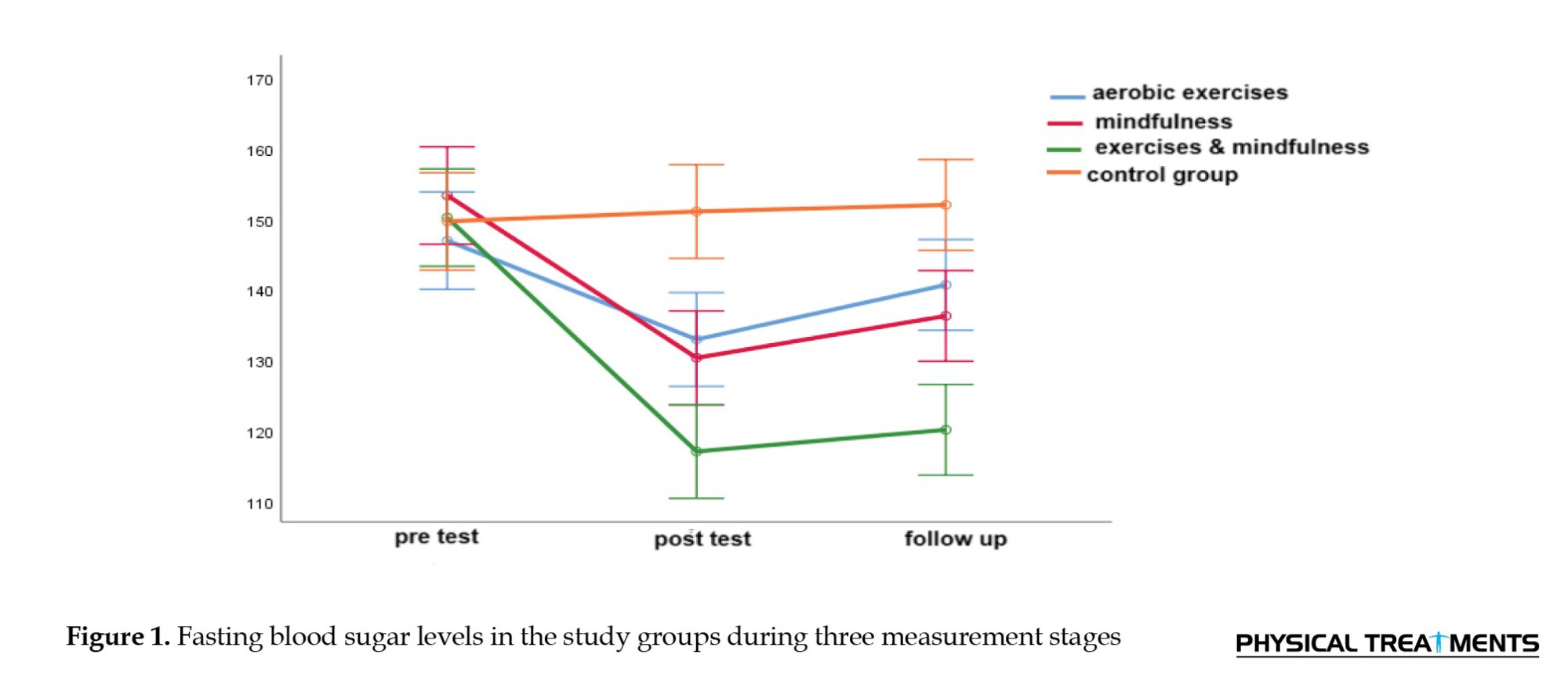
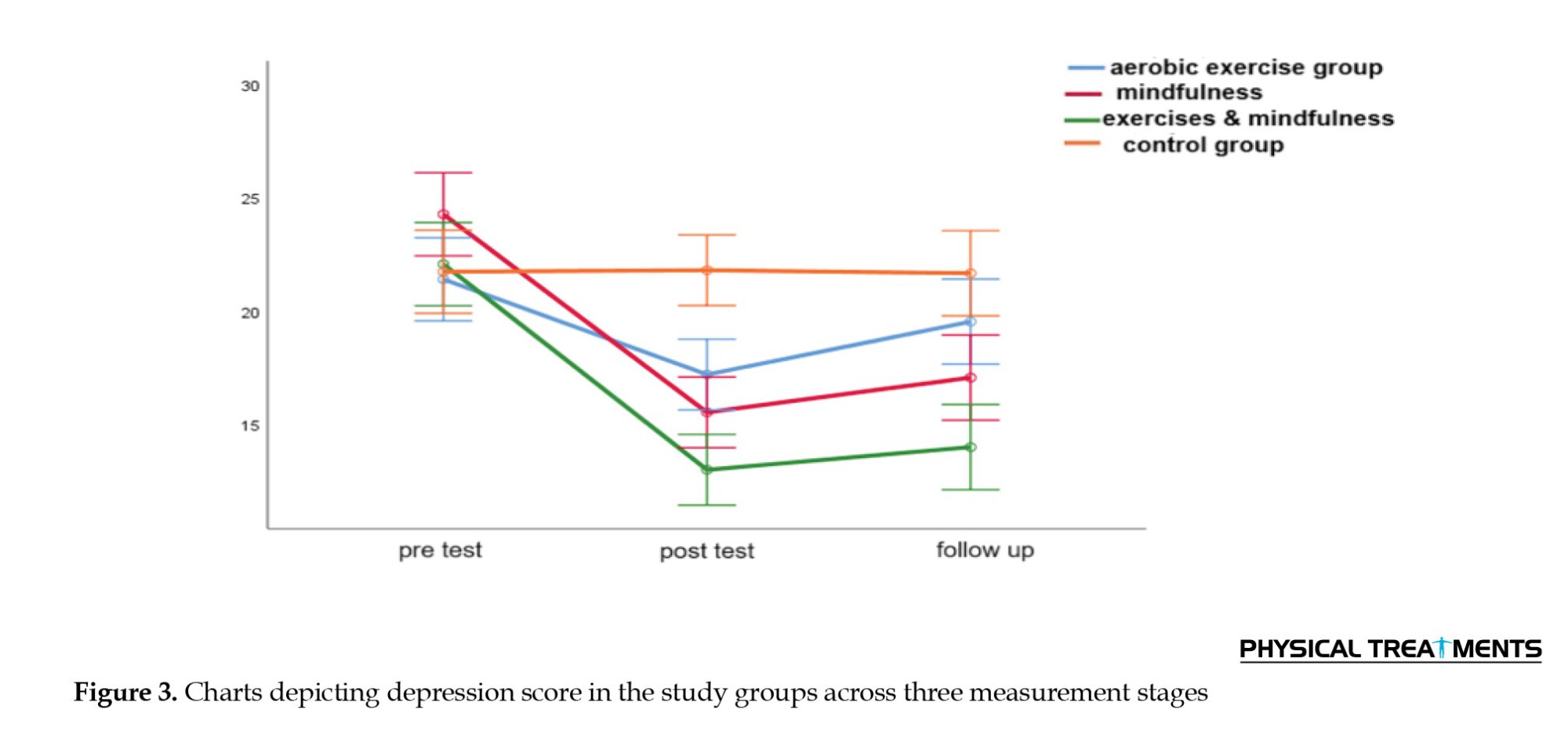
As shown in Table 6, significant differences were observed in the effects of aerobic exercise and the combination of aerobic exercise and mindfulness (P=0.003) and between mindfulness and the combination of aerobic exercise and mindfulness (P=0.015) on depression. Aerobic exercise combined with mindfulness led to a greater reduction in depression in participants compared to either aerobic exercise or mindfulness alone. No statistically significant differences were observed between the effects of aerobic exercise alone and mindfulness alone on depression. Therefore, it can be concluded that the combination of aerobic exercise and mindfulness was more effective in reducing depression in women with T2D than either aerobic exercise or mindfulness alone (Figure 1, 2 and 3).
Discussion
The results demonstrated that the combination of aerobic exercise and mindfulness therapy was more effective in reducing fasting blood sugar, HbA1C, and depression levels in patients with diabetes.
These findings align with those reported by Obaya et al. [15] and Vencatachellum et al. [16]. Following stress and depression, the sympathetic nervous system becomes overactive, resulting in increased levels of hormones from the hypothalamic-pituitary-adrenal (HPA) axis, subsequently raising the cortisol levels. This hormonal surge disrupts insulin regulation and stimulates gluconeogenesis, resulting in decreased insulin levels. Disrupting insulin signaling affects the neurotransmission of serotonin, dopamine, and norepinephrine, leading to elevated blood sugar levels [24]. The relationship between diabetes and depression is bidirectional, with diabetes increasing the risk of depression and vice versa. Psychological stress is considered a significant factor contributing to the pathogenesis, leading to disruption of the HPA axis, elevated cortisol levels, and impaired neurotransmission of serotonin and dopamine. Such dysregulations interfere with physiological processes, such as sleep, the gut-brain axis, metabolism, and mood stability. Coping mechanisms related to behavior, such as an unhealthy diet, can also increase blood sugar levels and exacerbate diabetes. Furthermore, the presence of diabetes, along with care challenges and disease complications, intensifies stress and depression [25]. Exercise alleviates depressive symptoms by regulating the activity of the HPA axis, increasing neurogenesis, reducing pro-inflammatory cytokines, and improving cardiovascular fitness. Additionally, aerobic exercise enhances insulin sensitivity and mitochondrial function [26]. High-intensity aerobic exercise for seven days may improve blood sugar levels without body weight loss by increasing insulin-stimulated glucose disposal and suppressing hepatic glucose production [27]. Increased self-efficacy is one of the most recognized psychological mechanisms used to assess the relationship between exercise and depression. Utilizing exercise to regulate emotions may contribute to a decrease in depressive symptoms. Exercise can decrease negative mood states and enhance positive moods. Behavioral activation is a therapeutic process that involves structured efforts to promote health-oriented behaviors, positive thoughts, and moods, thereby improving quality of life [28]. The results demonstrated that aerobic exercise combined with mindfulness therapy was more effective in reducing fasting blood sugar and HbA1c levels. These findings are consistent with those of Singh et al. [29], Hamasaki [30], and Donyaei et al. [26]. There is growing evidence showing that mindfulness can play a crucial role in physical health, including blood sugar control, by regulating the autonomic nervous system and the HPA axis, and decreasing pro-inflammatory cytokines [30]. Furthermore, mindfulness practice may promote heart and blood vessel health via producing adiponectin and endothelial nitric oxide, and exerting anti-inflammatory effects on interleukin-6 and tumor necrosis factor. Epigenetic changes associated with both glucose metabolism and inflammation, such as DNA methylation, are induced by mindfulness-based interventions [31]. Different brain areas (including large-scale neural networks in the cortex, subcortical gray and white matter, cerebellum, and brainstem) are influenced by mindfulness. Several cross-sectional and short-term longitudinal studies using MRI have reported functional and structural changes in the brain. Neuroplasticity changes have been reported in the polar frontal cortex, sensory cortex, anterior cingulate cortex, middle cingulate cortex, orbitofrontal cortex, insula, superior longitudinal fasciculus, corpus callosum, hippocampus, and temporal-parietal connectivity when using both meditation and mindfulness practices. Reported neuroplasticity changes include higher activation of specific areas and lower activation of others, as well as increased cortical thickness, density, and gray matter volume. Some neuroplasticity changes induced by mindfulness are related to increased attention regulation, emotional regulation, and self-awareness [32]. Overall, the integration of mindfulness and physical activity in diabetes management has shown promise, leading to improved psychological well-being, increased engagement in physical activity, greater attention to disease management, as well as enhanced blood glucose control [33]. Based on the discussed points, it can be concluded that the combination of aerobic exercise and mindfulness may be more effective in reducing fasting blood sugar, HbA1c, and depression levels in patients with T2D than either intervention alone, and this effectiveness may also be more sustained. Despite these limitations, our findings demonstrate the clinical importance of mindfulness in diabetes management. To confirm the findings of this study, similar studies with longer follow-up are suggested.
Conclusion
This study aimed to investigate the effects of aerobic exercise with and without mindfulness on fasting blood sugar, HbA1c, and depression levels in women with T2D. The results demonstrated that aerobic exercise combined with mindfulness therapy was more effective in reducing fasting blood sugar, HbA1c, and depression levels among T2D patients.
Limitation
This study had some limitations. This study was conducted only on women and cannot be generalized to men. Due to the focus on integrating mindfulness with physical activity, other factors contributing to diabetes prevention, such as nutrition, economic-cultural issues, and the type of drugs used, may not have been fully addressed. We did not measure inflammatory factors, such as cortisol and interleukin-6, which can improve after mindfulness. This study has limitations due to its small sample size and short duration, which may affect the accuracy of the results. We had to use convenience sampling in one of the diabetes centers. We will conduct multi-center and large-sample studies for mindfulness-based interventions.
Recommendations
A long-term study and follow-up with a larger sample size, including both genders in different diabetic populations, is suggested. In this case, it would be wiser to generalize the results to a larger population. Therefore, we suggest examining inflammatory factors, such as cortisol and interleukin-6, before and after treatment. We suggest that physicians explain to patients the importance of managing intrusive thoughts in the hopelessness and depression caused by diabetes and recommend that they use mindfulness techniques during medical treatment.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Islamic Azad University, Karaj Branch, Karaj, (Code: IR.IAU.K.REC.1402.125). The ethical considerations for the current study included obtaining informed and voluntary consent, the right to withdraw from the study at any time, maintaining confidentiality, avoiding harm, ensuring non-discrimination, and preventing non-exploitation.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Supervision and data analysis: Fatemeh Aslani and Tahereh Ranjbaripour; Writing-original draft, review, and editing: Fatemeh Aslani; Data collection: Farahnaz Meschi and Fatemeh Aslani; Conceptualization and Methodology: All authors.
Conflict of interest
The authors declared no conflict of interests.
Acknowledgments
The authors express their gratitude to the Faculty of Physical Education and the Faculty of Medical Sciences at Islamic Azad University, Karaj Branch, for providing the sports hall, to the doctoral students of physical education for their collaboration in this research, and to Sasan Abbasi Sharghi, a specialist in endocrinology and nephrology, along with all colleagues who contributed to the execution of this study.
References
Diabetes is the most common cause of death worldwide. The prevalence and incidence of type 2 diabetes (T2D) increased by 24.3% worldwide between 1990 and 2021. By 2050, it is projected that 1.31 billion people will have T2D [1]. In Iran, the prevalence of diabetes is relatively high, with 15% of the adult population affected and over 25% in the pre-diabetes stage [2]. To avoid acute complications and lower the risk of long-term diabetes-related complications, multifaceted treatments are required [3]. Regardless of the patient’s age, suitable and applicable management methods that engage patients in managing their disease can help improve their health and quality of life by controlling glycated hemoglobin A1C (HbA1C) levels [4]. Information and health education alone may be insufficient for many individuals to achieve permanent changes. While the benefits of proven pharmacological treatments are established, there is an increasing interest in complementary and alternative medicine, especially in mind-body interventions [5]. Due to its psychological benefits, mindfulness, which originated in ancient Buddhist traditions, has become increasingly integrated into contemporary medical practices [3]. Meditation-based interventions have shown positive effects in managing stress and diabetes by modulating neuro-humoral mechanisms [6]. Researchers have demonstrated increased interest in how mindfulness interventions can be effective in managing blood sugar levels and improving the mental wellbeing of people with diabetes [7]. The simultaneous presence of psychological and physical diseases presents a major challenge to global healthcare. Depression is twice as prevalent in individuals with diabetes as in those without diabetes. The presence of depression in individuals with diabetic also leads to poor diabetes management [8]. Mental health issues, such as depression can exacerbate diabetes by affecting how individuals think, their adherence to treatment, and their practice of self-care. Conversely, diabetes can worsen mental health problems. Fortunately, if one improves, the other tends to improve as well [9]. Recent neuroimaging studies have demonstrated that a range of contemplative practices, including mindfulness meditation, are related to changes in the patterns of communication between the main brain networks traditionally associated with various cognitive functions, including attention, self-processing, rumination, and insight, thereby improving depression [10]. Mindfulness can foster long-term adherence to exercise and motivation for diabetes management by focusing on the mind-body relationship and observing current experiences in a non-judgmental and non-evaluative manner, which in turn can help reduce depression and blood sugar levels [11]. Care guidelines presented by both mindfulness experts and healthcare professionals can effectively alleviate the distress and depression of patients, leading to an increase in their self-care abilities. Mindfulness is proposed as a low-cost psychological therapeutic intervention with lasting benefits, reinforcing therapeutic effects, and reducing medical costs [12]. One of the most crucial recommendations for treating diabetes is regular exercise and an active lifestyle. Despite the awareness of the beneficial role of exercise in diabetes, adherence to exercise regimens among patients is often low [13]. People who master mindfulness learn how to deal with intrusive negative thoughts and cultivate a present-moment awareness. With the help of mindfulness, people can keep the motivational engine running for exercising and managing diabetes, and become aware of the feelings that cause frustration in continuing their treatment. Incorporating mindfulness exercises into physical activity increases patients’ willingness to engage in physical activity and enhances their awareness of bodily sensations during exercise [14]. Glucose and cortisol levels in women with T2D can be better managed by mindfulness, combined with aerobic exercise [15]. Mindfulness through focused attention and mind-body awareness can promote the sustainable exercise regimens [16]. In terms of sex, the risk of both cardiovascular diseases and mortality in females with diabetes is higher than that in males. Therefore, understanding the types of interventions that may increase diabetes diagnosis, especially in T2D women, can help reduce gender inequalities in diabetes [17].
While the effects of each of the interventions, exercise and mindfulness, on diabetes have been widely studied, fewer studies have investigated the effect of combining aerobic exercise with mindfulness therapy. Therefore, new interventions are needed that not only facilitate successful behavior change in physical activity but also address barriers that typically affect the performance and adherence to exercise. Accordingly, the present study aimed to examine the effectiveness of aerobic exercise, with and without mindfulness, on fasting blood sugar, HbA1C, and depression levels in women with T2D.
Materials and Methods
A pre- and post-test quasi-experimental research design with a three-month follow-up, involving three experimental groups and one control group was used in this study. The study population consisted of all women with T2D who visited Sasan Sharghi’s diabetes center in Karaj City in 2023. Since it is recommended that experimental studies have at least 15 participants per group [18], the sample size was determined to be 60 (15 participants in each group) [15]. We had to use the sampling method available at one of the diabetes centers, which is one of the study’s limitations. The participants were randomly allocated to four groups using a random number generator: Three experimental groups (n=15 participants per group) and one control group (n=15). The aerobic exercise group included 15 individuals who received aerobic exercise training in addition to their medical treatment. The second group, consisting of 15 participants, underwent mindfulness treatment, while the third group (n=15) engaged in aerobic exercise three times a week and mindfulness training once a week. The control group received only medical treatments. The inclusion criteria included women with T2D aged 45-60 years who could perform moderate-intensity aerobic exercise, without other chronic diseases, and no involvement in any auxiliary or comprehensive therapeutic approaches before or during the study. Additionally, participants were required to have no psychiatric disorders or psychological or psychiatric interventions in the past year. Additionally, participants should not have severe osteoporosis or other exercise restrictions and should not have participated in systematic aerobic exercises or mindfulness practices prior to joining the group. The exclusion criteria were missing two or more regularly scheduled therapy sessions, failure to complete assigned tasks, and lack of willingness to continue treatment. Many other factors, such as nutrition, economic and cultural issues, and the type of drugs used, affect blood sugar, but we could not control them in this study. Ethical considerations for the current study included obtaining written informed and voluntary consent, the right to withdraw from the study, maintaining confidentiality, avoiding harm, non-discrimination, and non-exploitation. All participants provided an informed consent to participate in the study. Repeated measures analysis of variance (ANOVA) and Bonferroni post hoc tests were used to analyze the data. All statistical analyses were performed using SPSS software, version 26.
Intervention
Beck depression inventory (BDI-II)
The BDI was first developed by Beck et al. [19]. In 1996, Beck and his associates made significant revisions. This questionnaire consists of 21 items designed to assess both the feedback and symptoms or signs of depression in patients. Respondents were required to use a four-point Likert scale, ranging from zero to three. The items cover areas, such as sadness, pessimism, sense of failure, guilt, insomnia, loss of appetite, and self-dislike. Thus, this scale measures the severity of depression in individuals, encompassing a range of symptoms from mild to very severe, with a scoring range from a minimum of zero to a maximum of 63 [19]. By summing the scores for each item, an individual’s total score is obtained directly. The internal consistency of BDI-2 has been reported to be between 0.73 and 0.92, with an average of 0.86; the α coefficient is 0.86 for patients and 0.8 for controls [20]. In a study conducted by Hamidi et al., the intra-class correlation coefficient was calculated to be 0.81. The internal consistency of the test was 0.93 and 0.64 using Cronbach’s α and split-half methods, respectively. In a convergent validity assessment, the Beck questionnaire demonstrated a correlation of 0.80 with the total score on the GHQ-28. The internal consistency of this questionnaire in the present study was calculated at 0.86 [20].
Mindfulness intervention
Two authors were present in each intervention session. After practicing the techniques and assigning tasks for the next session, they monitored the completion of tasks from the previous session. Obstacles to completing the tasks were identified and a solution was taught, ensuring task completion (Table 1).
Aerobic exercise
Summary of aerobic exercise intervention based on the Cooper protocol [23]:
Each aerobic exercise session lasted 30 minutes (three times a week for 12 weeks). The participants performed a 10-minute warm-up (such as light jogging, combined hand and foot movements, and stretching), followed by 15 minutes of the main exercise. The main exercise involved walking, which gradually increased in intensity and ended with running. Each session ended with a 5-minute cool-down to return to a resting state. During aerobic exercises, participants were encouraged to walk and incorporate hand and foot movements as needed throughout the session when they became fatigued. Given the participants’ lack of regular exercise and poor fitness, the first two weeks focused on brisk walking (with a heart rate intensity of approximately 60% of maximum heart rate for 20-25 minutes). The exercise intensity and duration were gradually increased each week. A doctoral student in physical education used a heart rate monitor to display heart rate and measure the target intensity of 60%. In this study, we calculated the intensity of approximately 60% of the maximum heart rate using a heart rate display watch with the help of two physical education students.
Procedure
Necessary permissions were obtained to conduct this study on women with T2D. First, the participants were contacted and invited to participate. Next, they were informed about the research, its objectives, and the publication of results. Eligible participants then completed the self-reporting tools. Finally, data were collected once the self-reporting tools were completed. Upon their visit, patients were provided with additional explanations regarding the research, its objectives, and how the results would be published. The BDI-II, fasting blood sugar, and HbA1C levels were measured in both the control and intervention groups, before, immediately after, and three months after the intervention.
Results
Table 2 presents the ages and education levels of the participants.
Table 2 presents both the Mean±SD of the participants’ age. The one-way ANOVA test results indicated that no statistically significant difference was found among the four groups in terms of age mean. The frequency of participants’ education levels is observed in the Table 2, and the Fisher’s exact test results showed no statistically significant difference among the groups in terms of education levels.
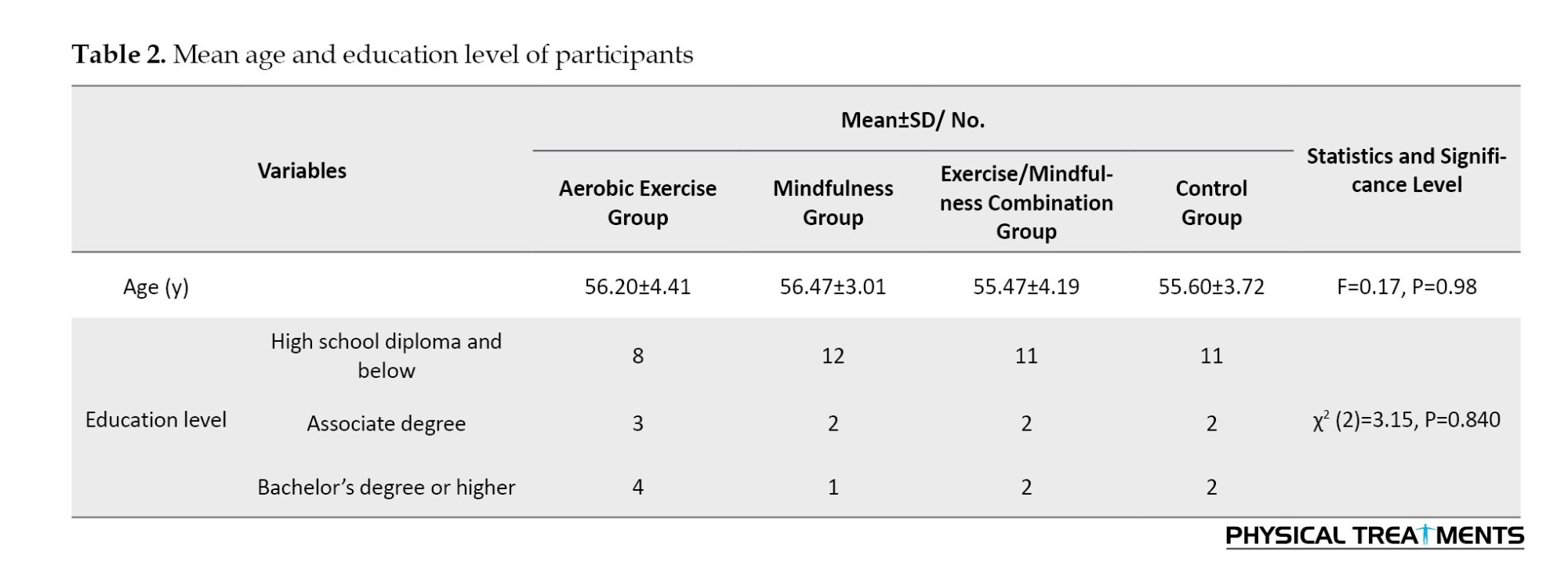
Table 3 presents the Mean±SD of fasting blood sugar and depression levels among the four groups in the pre-test, post-test, and follow-up phases.
As shown in Table 3, the mean values of the research variables (including fasting blood sugar, HbA1C, and depression levels) were lower in the intervention groups compared to the controls in both the post-test and follow-up phases. In contrast, no similar changes were observed in the controls during these phases.
The assumptions of repeated measures ANOVA were assessed before testing the research hypotheses. The assumption of normal distribution of the data was assessed using the Shapiro-Wilk test, suggesting that the data were normally distributed. Mauchly’s test was employed to assess the assumption of equality of the covariance matrices of the dependent variables. The results confirmed that this assumption was also met (P>0.05). The sphericity or equality of the error covariance matrix was evaluated using Mauchly’s test. The chi-square value obtained from Mauchly’s test for fasting blood sugar levels was P=0.005, for HbA1C levels was P=0.001, and for depression was P=0.672. Since the sphericity assumption was not met for fasting blood sugar levels, the degrees of freedom for the variables were adjusted using the Greenhouse-Geisser method.
Table 4 presents the results obtained from the multivariate analysis of the effectiveness of aerobic exercise with and without mindfulness on fasting blood sugar, HbA1C, and depression levels.
As shown in Table 4, aerobic exercise with and without mindfulness had a significant effect on fasting blood sugar (Wilks’ Lambda=0.440, η²=0.336, P=0.001, F=9.30), HbA1C (Wilks’ Lambda=0.419, η²=0.353, P=0.001, F=10.03), and depression levels (Wilks’ Lambda=0.482, η²=0.305, P=0.001, F=8.06).
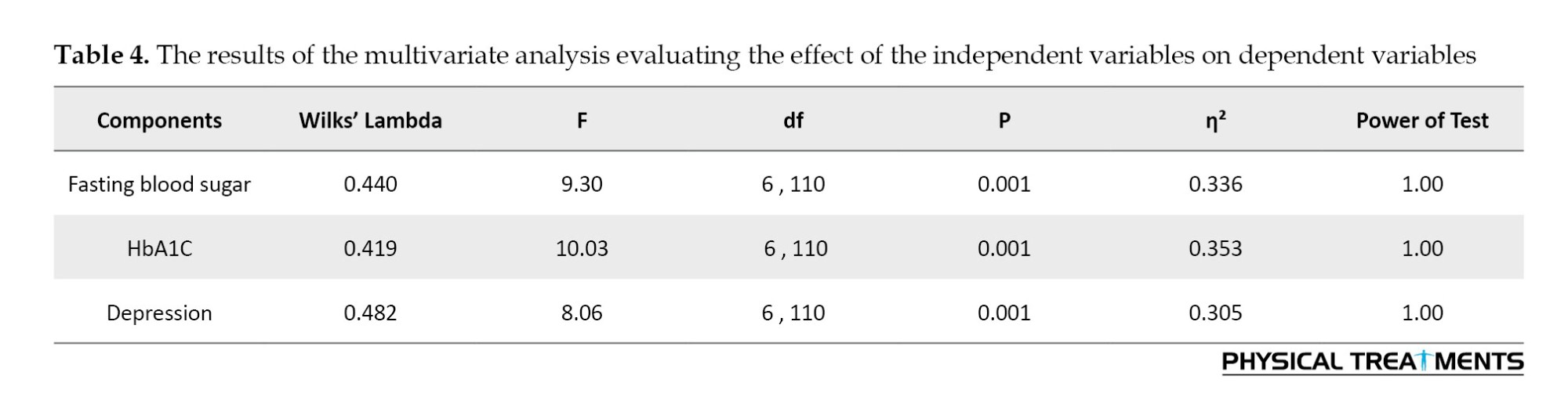
Table 5 presents the results of the repeated-measures ANOVA assessing the effect of aerobic exercise with and without mindfulness on fasting blood sugar, HbA1C, and depression levels.
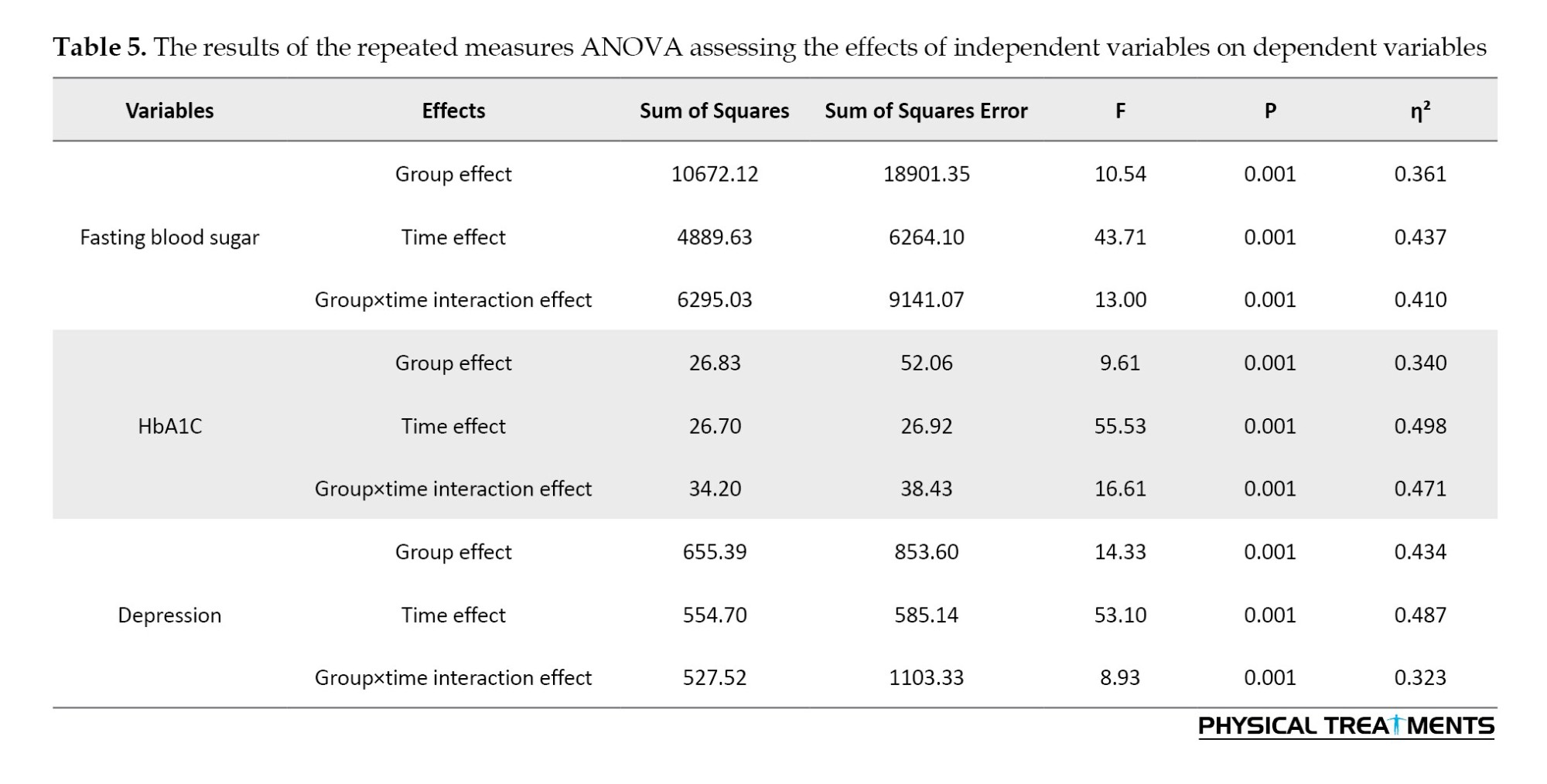
Table 5 shows that the interaction effect of group×time on fasting blood sugar (η²=0.410, P=0.001, F=13.00), and HbA1C levels (η²=0.471, P=0.001, F=16.61), and depression (η²=0.323, P=0.001, F=8.93) was significant. These findings revealed that the independent variables had a significant effect on fasting blood sugar, HbA1C, and depression levels. Table 6 presents the results obtained from the Bonferroni post hoc test, comparing the mean scores of fasting blood sugar, HbA1C, and depression levels among the four groups across three phases.
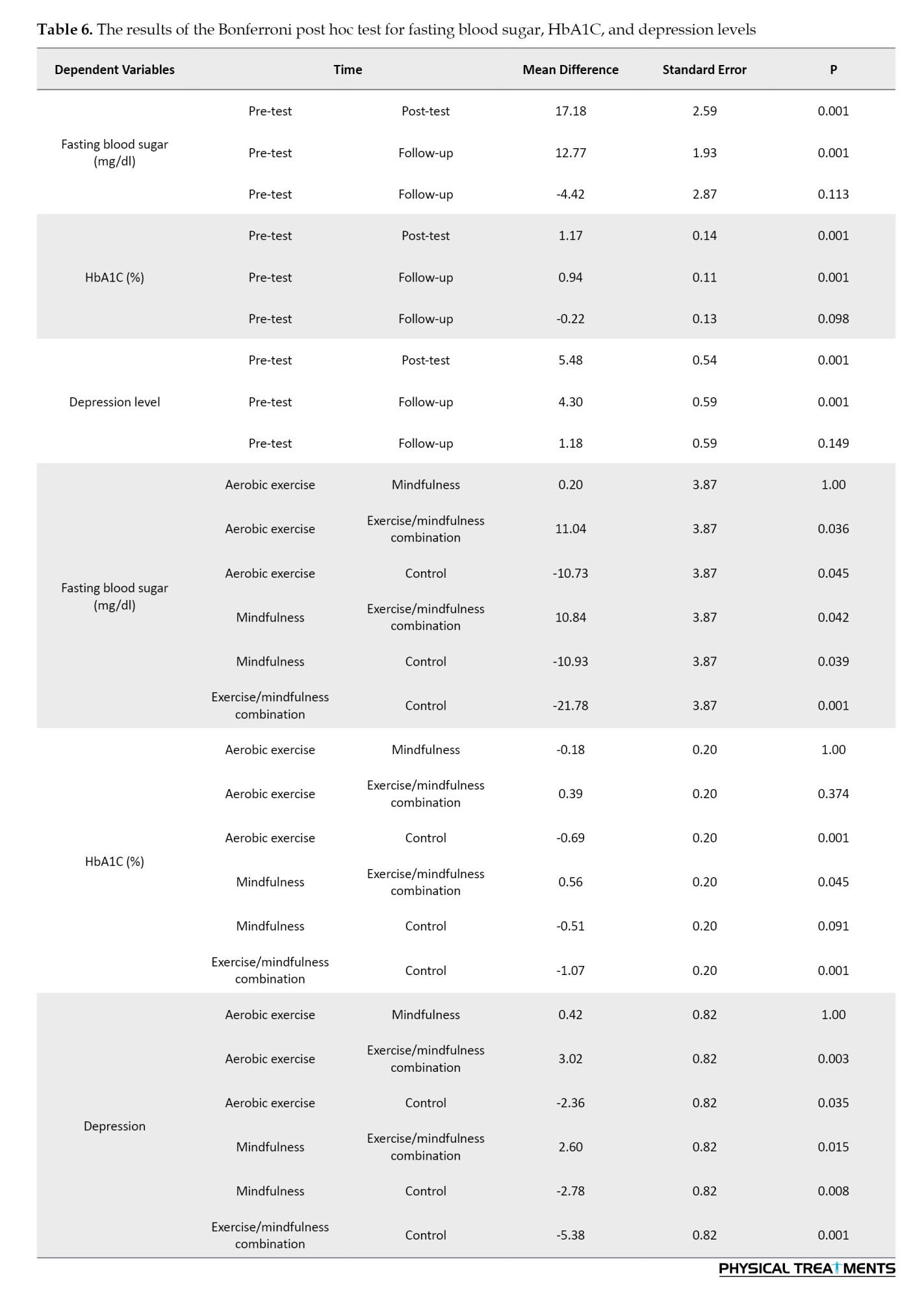
As shown in Table 6, the Bonferroni test results demonstrated statistically significant difference between the effects of aerobic exercise and aerobic exercise combined with mindfulness therapy (P=0.036), as well as between mindfulness and aerobic exercise combined with mindfulness (P=0.042) on fasting blood sugar levels. Specifically, the combination of aerobic exercise and mindfulness significantly reduced fasting blood sugar levels in participants compared to either aerobic exercise alone or mindfulness alone. No statistically significant differences were observed between the effects of aerobic exercise and mindfulness alone on fasting blood sugar levels. Therefore, it can be concluded that aerobic exercise combined with mindfulness is more effective in reducing fasting blood sugar levels in women with T2D compared to either aerobic exercise or mindfulness alone.
As shown in Table 6, no statistically significant difference was observed in the effects of aerobic exercise and the combination of aerobic exercise and mindfulness on HbA1c levels, as well as between the effects of aerobic exercise and mindfulness treatment alone on HbA1c levels. However, a significant difference was observed between mindfulness and the combination of aerobic exercise and mindfulness (P=0.045), showing a greater reduction in HbA1c levels compared to mindfulness alone. Thus, it can be concluded that the combination of aerobic exercise and mindfulness was more effective in reducing HbA1c levels in women with T2D than mindfulness intervention alone.
As shown in Table 6, significant differences were observed in the effects of aerobic exercise and the combination of aerobic exercise and mindfulness (P=0.003) and between mindfulness and the combination of aerobic exercise and mindfulness (P=0.015) on depression. Aerobic exercise combined with mindfulness led to a greater reduction in depression in participants compared to either aerobic exercise or mindfulness alone. No statistically significant differences were observed between the effects of aerobic exercise alone and mindfulness alone on depression. Therefore, it can be concluded that the combination of aerobic exercise and mindfulness was more effective in reducing depression in women with T2D than either aerobic exercise or mindfulness alone (Figure 1, 2 and 3).
Discussion
The results demonstrated that the combination of aerobic exercise and mindfulness therapy was more effective in reducing fasting blood sugar, HbA1C, and depression levels in patients with diabetes.
These findings align with those reported by Obaya et al. [15] and Vencatachellum et al. [16]. Following stress and depression, the sympathetic nervous system becomes overactive, resulting in increased levels of hormones from the hypothalamic-pituitary-adrenal (HPA) axis, subsequently raising the cortisol levels. This hormonal surge disrupts insulin regulation and stimulates gluconeogenesis, resulting in decreased insulin levels. Disrupting insulin signaling affects the neurotransmission of serotonin, dopamine, and norepinephrine, leading to elevated blood sugar levels [24]. The relationship between diabetes and depression is bidirectional, with diabetes increasing the risk of depression and vice versa. Psychological stress is considered a significant factor contributing to the pathogenesis, leading to disruption of the HPA axis, elevated cortisol levels, and impaired neurotransmission of serotonin and dopamine. Such dysregulations interfere with physiological processes, such as sleep, the gut-brain axis, metabolism, and mood stability. Coping mechanisms related to behavior, such as an unhealthy diet, can also increase blood sugar levels and exacerbate diabetes. Furthermore, the presence of diabetes, along with care challenges and disease complications, intensifies stress and depression [25]. Exercise alleviates depressive symptoms by regulating the activity of the HPA axis, increasing neurogenesis, reducing pro-inflammatory cytokines, and improving cardiovascular fitness. Additionally, aerobic exercise enhances insulin sensitivity and mitochondrial function [26]. High-intensity aerobic exercise for seven days may improve blood sugar levels without body weight loss by increasing insulin-stimulated glucose disposal and suppressing hepatic glucose production [27]. Increased self-efficacy is one of the most recognized psychological mechanisms used to assess the relationship between exercise and depression. Utilizing exercise to regulate emotions may contribute to a decrease in depressive symptoms. Exercise can decrease negative mood states and enhance positive moods. Behavioral activation is a therapeutic process that involves structured efforts to promote health-oriented behaviors, positive thoughts, and moods, thereby improving quality of life [28]. The results demonstrated that aerobic exercise combined with mindfulness therapy was more effective in reducing fasting blood sugar and HbA1c levels. These findings are consistent with those of Singh et al. [29], Hamasaki [30], and Donyaei et al. [26]. There is growing evidence showing that mindfulness can play a crucial role in physical health, including blood sugar control, by regulating the autonomic nervous system and the HPA axis, and decreasing pro-inflammatory cytokines [30]. Furthermore, mindfulness practice may promote heart and blood vessel health via producing adiponectin and endothelial nitric oxide, and exerting anti-inflammatory effects on interleukin-6 and tumor necrosis factor. Epigenetic changes associated with both glucose metabolism and inflammation, such as DNA methylation, are induced by mindfulness-based interventions [31]. Different brain areas (including large-scale neural networks in the cortex, subcortical gray and white matter, cerebellum, and brainstem) are influenced by mindfulness. Several cross-sectional and short-term longitudinal studies using MRI have reported functional and structural changes in the brain. Neuroplasticity changes have been reported in the polar frontal cortex, sensory cortex, anterior cingulate cortex, middle cingulate cortex, orbitofrontal cortex, insula, superior longitudinal fasciculus, corpus callosum, hippocampus, and temporal-parietal connectivity when using both meditation and mindfulness practices. Reported neuroplasticity changes include higher activation of specific areas and lower activation of others, as well as increased cortical thickness, density, and gray matter volume. Some neuroplasticity changes induced by mindfulness are related to increased attention regulation, emotional regulation, and self-awareness [32]. Overall, the integration of mindfulness and physical activity in diabetes management has shown promise, leading to improved psychological well-being, increased engagement in physical activity, greater attention to disease management, as well as enhanced blood glucose control [33]. Based on the discussed points, it can be concluded that the combination of aerobic exercise and mindfulness may be more effective in reducing fasting blood sugar, HbA1c, and depression levels in patients with T2D than either intervention alone, and this effectiveness may also be more sustained. Despite these limitations, our findings demonstrate the clinical importance of mindfulness in diabetes management. To confirm the findings of this study, similar studies with longer follow-up are suggested.
Conclusion
This study aimed to investigate the effects of aerobic exercise with and without mindfulness on fasting blood sugar, HbA1c, and depression levels in women with T2D. The results demonstrated that aerobic exercise combined with mindfulness therapy was more effective in reducing fasting blood sugar, HbA1c, and depression levels among T2D patients.
Limitation
This study had some limitations. This study was conducted only on women and cannot be generalized to men. Due to the focus on integrating mindfulness with physical activity, other factors contributing to diabetes prevention, such as nutrition, economic-cultural issues, and the type of drugs used, may not have been fully addressed. We did not measure inflammatory factors, such as cortisol and interleukin-6, which can improve after mindfulness. This study has limitations due to its small sample size and short duration, which may affect the accuracy of the results. We had to use convenience sampling in one of the diabetes centers. We will conduct multi-center and large-sample studies for mindfulness-based interventions.
Recommendations
A long-term study and follow-up with a larger sample size, including both genders in different diabetic populations, is suggested. In this case, it would be wiser to generalize the results to a larger population. Therefore, we suggest examining inflammatory factors, such as cortisol and interleukin-6, before and after treatment. We suggest that physicians explain to patients the importance of managing intrusive thoughts in the hopelessness and depression caused by diabetes and recommend that they use mindfulness techniques during medical treatment.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Islamic Azad University, Karaj Branch, Karaj, (Code: IR.IAU.K.REC.1402.125). The ethical considerations for the current study included obtaining informed and voluntary consent, the right to withdraw from the study at any time, maintaining confidentiality, avoiding harm, ensuring non-discrimination, and preventing non-exploitation.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Supervision and data analysis: Fatemeh Aslani and Tahereh Ranjbaripour; Writing-original draft, review, and editing: Fatemeh Aslani; Data collection: Farahnaz Meschi and Fatemeh Aslani; Conceptualization and Methodology: All authors.
Conflict of interest
The authors declared no conflict of interests.
Acknowledgments
The authors express their gratitude to the Faculty of Physical Education and the Faculty of Medical Sciences at Islamic Azad University, Karaj Branch, for providing the sports hall, to the doctoral students of physical education for their collaboration in this research, and to Sasan Abbasi Sharghi, a specialist in endocrinology and nephrology, along with all colleagues who contributed to the execution of this study.
References
- GBD 2021 Diabetes Collaborators. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: A systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2023; 402(10397):203-34. [DOI:10.1016/S0140-6736(23)01301-6] [PMID]
- Khamseh ME, Sepanlou SG, Hashemi-Madani N, Joukar F, Mehrparvar AH, Faramarzi E, et al. Nationwide prevalence of diabetes and prediabetes and associated risk factors among Iranian Adults: Analysis of data from PERSIAN Cohort Study. Diabetes Therapy: Research, Treatment and Education of Diabetes and Related Disorders. 2021; 12(11):2921-38. [DOI:10.1007/s13300-021-01152-5] [PMID]
- Gandhi A, Rajkumar R, Dakka SN, Sania J, Khurram F, Cabrera J. Mindfulness training for cardiovascular health in type 2 diabetes: A critical review. Current Problems in Cardiology. 2024; 49(12):102833. [DOI:10.1016/j.cpcardiol.2024.102833] [PMID]
- Sukartini T, Nursalam N, Pradipta RO, Ubudiyah M. Potential methods to improve self-management in those with type 2 diabetes: A narrative review. International Journal of Endocrinology and Metabolism. 2023; 21(1):e119698. [DOI:10.5812/ijem-119698] [PMID]
- Brenner J, LeBlang S, Lizotte-Waniewski M, Schmidt B, Espinosa PS, DeMets DL, et al. Mindfulness with paced breathing reduces blood pressure. Medical Hypotheses. 2020; 142:109780. [DOI:10.1016/j.mehy.2020.109780] [PMID]
- Dalpatadu KPC, Galappatthy P, Katulanda P, Jayasinghe S. Effects of meditation on physiological and metabolic parameters in patients with type 2 diabetes mellitus "MindDM": Study protocol for a randomized controlled trial. Trials. 2022; 23(1):821. [DOI:10.1186/s13063-022-06771-2] [PMID]
- Jiang S, Pan X, Li H, Su Y. Global trends and developments in mindfulness interventions for diabetes: A bibliometric study. Diabetology & Metabolic Syndrome. 2024; 16(1):43. [DOI:10.1186/s13098-024-01288-x] [PMID]
- Sartorius N. Depression and diabetes. Dialogues in Clinical Neuroscience. 2018; 20(1):47-52. [DOI:10.31887/DCNS.2018.20.1/nsartorius] [PMID]
- Speight J, Hermanns N, Ehrmann D; PsychoSocial Aspects of Diabetes Study Group of the European Association for the Study of Diabetes. Data on diabetes-specific distress are needed to improve the quality of diabetes care. Lancet. 2021; 397(10290):2149. [DOI:10.1016/S0140-6736(21)00633-4] [PMID]
- Catoira B, Van Overwalle F, Van Schuerbeek P, Raeymaekers H, Heleven E, Baetens K, et al. The effects of stimulating the cerebellum on social sequences: A tDCS-fMRI pilot study: Los efectos de estimular el cerebelo en secuencias sociales: Un estudio piloto con tDCS y fMRI. International Journal of Clinical and Health Psychology. 2023; 23(3):100373. [DOI:10.1016/j.ijchp.2023.100373] [PMID]
- Wielgosz J, Goldberg SB, Kral TR, Dunne JD, Davidson RJ. Mindfulness meditation and psychopathology. Annual Review of Clinical Psychology. 2019; 15:285-316. [DOI:10.1146/annurev-clinpsy-021815-093423] [PMID]
- Bao H. Intervention effect of mindfulness-based cognitive therapy on diabetes-related distress and self-care. Iranian Journal of Public Health. 2022; 51(3):606-14. [DOI:10.18502/ijph.v51i3.8937] [PMID]
- Zahalka SJ, Abushamat LA, Scalzo RL, Reusch JEB. The Role of exercise in diabetes.In: Feingold KR, Ahmed SF, Anawalt B, Blackman MR, Boyce A, Chrousos G, et al, editors. Endotext. South Dartmouth: MDText.com, Inc.; 2000. [PMID]
- Gál É, Stefan S, Cristea IA. The efficacy of mindfulness meditation apps in enhancing users’ well-being and mental health related outcomes: A meta-analysis of randomized controlled trials. Journal of Affective Disorders. 2021; 279:131-42. [DOI:10.1016/j.jad.2020.09.134] [PMID]
- Obaya HE, Abdeen HA, Salem AA, Shehata MA, Aldhahi MI, Muka T, et al. Effect of aerobic exercise, slow deep breathing and mindfulness meditation on cortisol and glucose levels in women with type 2 diabetes mellitus: A randomized controlled trial. Frontiers in Physiology. 2023; 14:1186546. [DOI:10.3389/fphys.2023.1186546] [PMID]
- Vencatachellum S, van der Meulen M, Van Ryckeghem DM, Van Damme S, Vögele C. Brief mindfulness training can mitigate the influence of prior expectations on pain perception. European Journal of Pain. 2021; 25(9):2007-19. [DOI:10.1002/ejp.1817] [PMID]
- Glovaci D, Fan W, Wong ND. Epidemiology of diabetes mellitus and cardiovascular disease. Current Cardiology Reports. 2019; 21(4):21. [DOI:10.1007/s11886-019-1107-y] [PMID]
- Delavar A. The effect of moocs instructional design model-based on student’s learning and motivation. Man In India. 2017; 97(11):115-26. [Link]
- Beck AT, Steer RA, Brown G. Beck depression inventory-II. Psychological assessment. 1996. [DOI:10.1037/t00742-000]
- Hamidi R, Fekrizadeh Z, Azadbakht M, Garmaroudi G, Taheri Tanjani P, Fathizadeh S, et al. [Validity and reliability Beck Depression Inventory-II among the Iranian elderly population (Persian)]. Journal of Sabzevar University of Medical Sciences. 2015; 22(1):189-98. [Link]
- Yazdani P, Sarafraz MR. The effect of MBCT mindfulness-based cognitive therapy techniques on increasing hope in cancer patients undergoing radiotherapy. International Journal of New Findings in Health and Educational Sciences (IJHES). 2024; 2(3):101-15. [DOI:10.63053/ijhes.92]
- Weng X, Liao S, Wang F, Wang H, Yang L. Evaluation of mindfulness training combined with aerobic exercise on neurological function and quality of life in patients with peripheral neuropathy type 2 diabetes mellitus. Contrast Media & Molecular Imaging. 2022; 2022:7665483. [DOI:10.1155/2022/7665483] [PMID]
- Cooper KH. The history of aerobics (50 years and still counting). Research Quarterly for Exercise and Sport. 2018; 89(2):129-34. [DOI:10.1080/02701367.2018.1452469] [PMID]
- Joseph JJ, Golden SH. Cortisol dysregulation: the bidirectional link between stress, depression, and type 2 diabetes mellitus. Annals of the New York Academy of Sciences. 2017; 1391(1):20-34. [DOI:10.1111/nyas.13217] [PMID]
- Subba R, Sandhir R, Singh SP, Mallick BN, Mondal AC. Pathophysiology linking depression and type 2 diabetes: psychotherapy, physical exercise, and fecal microbiome transplantation as damage control. European Journal of Neuroscience. 2021; 53(8):2870-900. [DOI:10.1111/ejn.15136] [PMID]
- Donyaei A, Kiani E, Bahrololoum H, Moser O. Effect of combined aerobic-resistance training and subsequent detraining on brain-derived neurotrophic factor (BDNF) and depression in women with type 2 diabetes mellitus: A randomized controlled trial. Diabetic Medicine. 2024; 41(3):e15188. [DOI:10.1111/dme.15188] [PMID]
- Phielix E, Meex R, Moonen-Kornips E, Hesselink M, Schrauwen P. Exercise training increases mitochondrial content and ex vivo mitochondrial function similarly in patients with type 2 diabetes and in control individuals. Diabetologia. 2010; 53(8):1714-21. [DOI:10.1007/s00125-010-1764-2] [PMID]
- Craft LL. Potential psychological mechanisms underlying the exercise and depression relationship. In: Ekkekakis P, editor. Routledge handbook of physical activity and mental health. London: Routledge; 2023.[DOI:10.4324/9781003423430-13]
- Singh B, Koneru YC, Zimmerman H, Kanagala SG, Milne I, Sethi A, et al. A step in the right direction: Exploring the effects of aerobic exercise on HbA1c reduction. The Egyptian Journal of Internal Medicine. 2023; 35(1):58. [DOI:10.1186/s43162-023-00247-8]
- Hamasaki H. The effects of mindfulness on Glycemic Control in people with diabetes: An overview of systematic reviews and meta-analyses. Medicines. 2023; 10(9):53. [DOI:10.3390/medicines10090053] [PMID]
- García-Campayo J, Puebla-Guedea M, Labarga A, Urdánoz A, Roldán M, Pulido L, et al. Epigenetic response to mindfulness in peripheral blood leukocytes involves genes linked to common human diseases. Mindfulness. 2018; 9(4):1146-59. [DOI:10.1007/s12671-017-0851-6]
- Priya G, Kalra S. Mind-body interactions and mindfulness meditation in diabetes. European Endocrinology. 2018; 14(1):35-41. [DOI:10.17925/EE.2018.14.1.35] [PMID]
- Sun W, Lu EY, Wang C, Tsang HWH. Neurobiological mechanisms for the antidepressant effects of mind-body and physical exercises: A systematic review. Mental Health and Physical Activity. 2023; 100538. [DOI:10.1016/j.mhpa.2023.100538]
Type of Study: Research |
Subject:
Sport injury and corrective exercises
Received: 2024/11/6 | Accepted: 2025/01/13 | Published: 2025/10/18
Received: 2024/11/6 | Accepted: 2025/01/13 | Published: 2025/10/18
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |