Thu, Jan 29, 2026
Volume 15, Issue 4 (Autumn 2025)
PTJ 2025, 15(4): 255-264 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Azizian M, Yalfani A, Gholami-Borujeni B. Comparing the Effect of Combined and Conventional Rehabilitation Protocols on Psychological Indicators in People With Chronic Ankle Instability: A Systematic Review. PTJ 2025; 15 (4) :255-264
URL: http://ptj.uswr.ac.ir/article-1-675-en.html
URL: http://ptj.uswr.ac.ir/article-1-675-en.html
1- Department of Exercise Rehabilitation, Faculty of Sport Sciences, Bu Ali Sina University, Hamedan, Iran.
2- Department of Sport Biomechanics and Motor Behavior, Faculty of Sport Sciences, University of Mazandaran, Babolsar, Iran.
2- Department of Sport Biomechanics and Motor Behavior, Faculty of Sport Sciences, University of Mazandaran, Babolsar, Iran.
Full-Text [PDF 528 kb]
(1087 Downloads)
| Abstract (HTML) (1499 Views)
Full-Text: (468 Views)
Introduction
Lateral ankle sprains (LAS) are among the most common musculoskeletal injuries [1]. In the United States, over one million cases and approximately 23000 individuals are annually admitted to hospital emergency departments due to this condition [2]. LAS is one of the most prevalent injuries to the musculoskeletal system in athletes, non-athletes, and individuals involved in recreational activities [3]. LAS has also been reported as the most widespread recurrent lower extremity injury in most sports [4]. Notably, approximately 40% of individuals affected by LAS are susceptible to reinjuries, which cause chronic ankle instability (CAI) [5]. CAI is characterized by frequent sprains or ankle instability along with symptoms, such as pain, weakness, and a giving-way sensation in the legs, or limited range of motion in the ankle joint [6]. CAI can also damage joints, muscles, and sensory receptors [5], as well as mental and neuromuscular disorders [7]. Such problems can restrict recreational, work-related, and sporting activities in the long term [7]. This reduces health-related quality of life (QoL) and increases kinesiophobia or fear of movement/reinjury in patients with CAI [8].
A recent systematic review was reported. Psychological factors are among the most crucial rehabilitation factors in these people. Kinesiophobia and disabilities result from CAI, leading to an absence of physical activity [9]. CAI exacerbates general health and physical activity [10]. Physical inactivity has been classified as one of the three high-risk behaviors that induce cardiovascular diseases, cancer, diabetes mellitus, and obesity [7]. It was reported that individuals with CAI intensify their kinesiophobia, which diminishes their physical activity [9]. As recommended by the Centers for Disease Control and Prevention, adults should participate in at least 150 minutes of moderate-intensity activities and 75 minutes of high-intensity activities per week [2]. Physical activity is decreased in patients with CAI due to kinesiophobia and fear-avoidance beliefs [11], and this reduction is negatively associated with some chronic diseases. It is considered a risk factor [11]. In this respect, some tools, such as the multidimensional quality of life, Tampa Scale of Kinesiophobia (TSK), and Fear-Avoidance Beliefs Questionnaire (FABQ), have been advocated as useful methods to measure psychological indicators and physical activity in CAI patients [12]. Lower QoL has been related to lower environmental awareness of the body, followed by disturbed proprioception [13]. The central nervous system (CNS) receives information from the surrounding environment through visual and vestibular receptors to perform correct movements, known as body awareness [13]. Kinesiophobia, fear-avoidance beliefs, and quality of life are crucial psychological indicators for people with CAI [8]. Conversely, rehabilitation protocols can strengthen these patients mentally and musculoskeletally under different conditions [8]. Some interruptions in motor control and body awareness are among the most common disorders in CAI patients [14]. Therefore, it would be advantageous to offer an intervention that could lessen participant’s fear of reinjury; therefore, they can resume physical activity [9]. Numerous rehabilitation protocols, such as balance and strength exercises [15], have been shown to improve these symptoms [16]. Neuromuscular training has been introduced as an effective rehabilitation protocol for reducing the prevalence rate of ankle sprains or reinjuries [17]. Such exercises combine balance, proprioception, core stability, and strength [18]. Balance training includes single-leg exercises, performed with eyes open and closed to increasing balance. Also, proprioceptive training includes coordination skills and strengthens the central nervous system [15]. Together, these are useful for improving neuromuscular control in CAI patients [19]. Multimodal protocols for CAI treatment have also been reported to be more effective than simple protocols [15]. In a systematic review, Maricot et al. observed kinesiophobia and reduced QoL problems in CAI sufferers. They advised physiotherapists and sports medicine specialists to improve these factors and consider rehabilitation programs in their protocols [20]. Minoonejad et al. investigated the effects of balance training with an internal focus compared to exercises with an external focus, on kinesiophobia in athletes with CAI. They showed that balance training with an internal focus minimized fear in these individuals [13]. Using a randomized controlled trial, Burcal et al. reported the positive effects of balance exercises on kinesiophobia and fear-avoidance beliefs in patients with CAI [14]. Given the above, psychological indicators and their effects on CAI patients are crucial, and while numerous rehabilitation protocols have been implemented, it is unclear which protocol has better results. To the best of our knowledge, no study has been found to systematically examine the effects of different rehabilitation protocols on psychological indicators in CAI patients. The present study aimed to systematically review the impact of different rehabilitation protocols on psychological indicators in CAI sufferers. We hypothesized that different rehabilitation protocols have different effects on psychological indicators in CAI patients.
Materials and Methods
Searching strategy
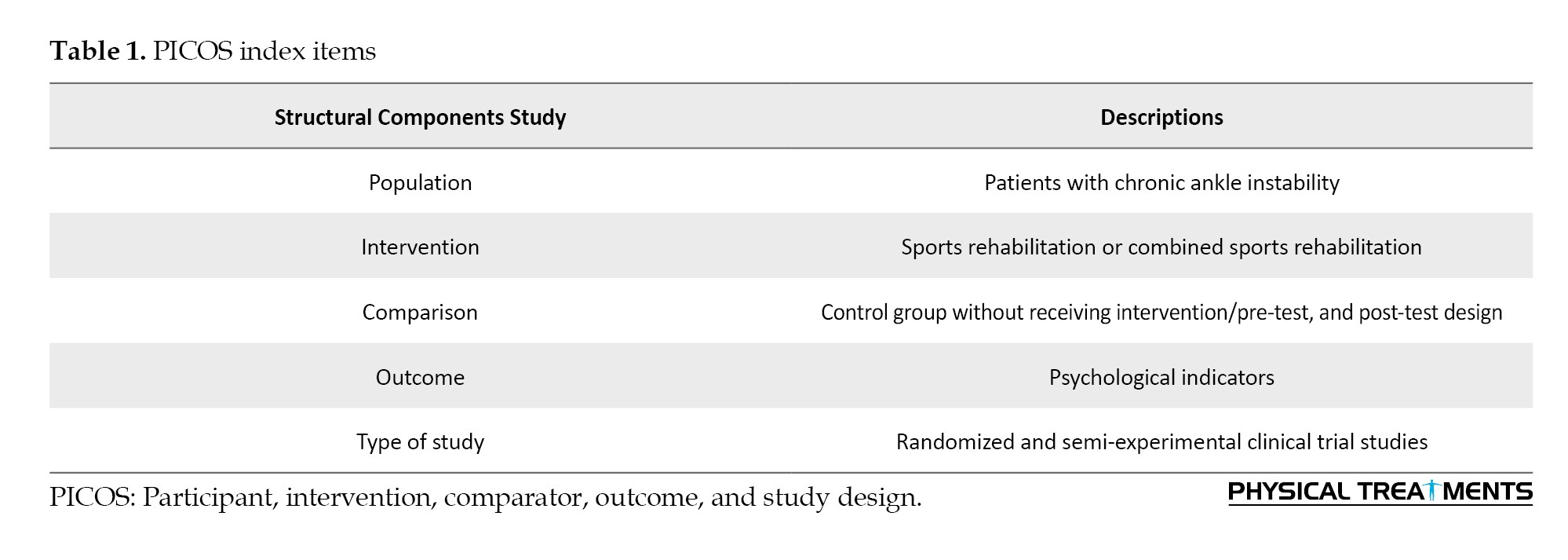
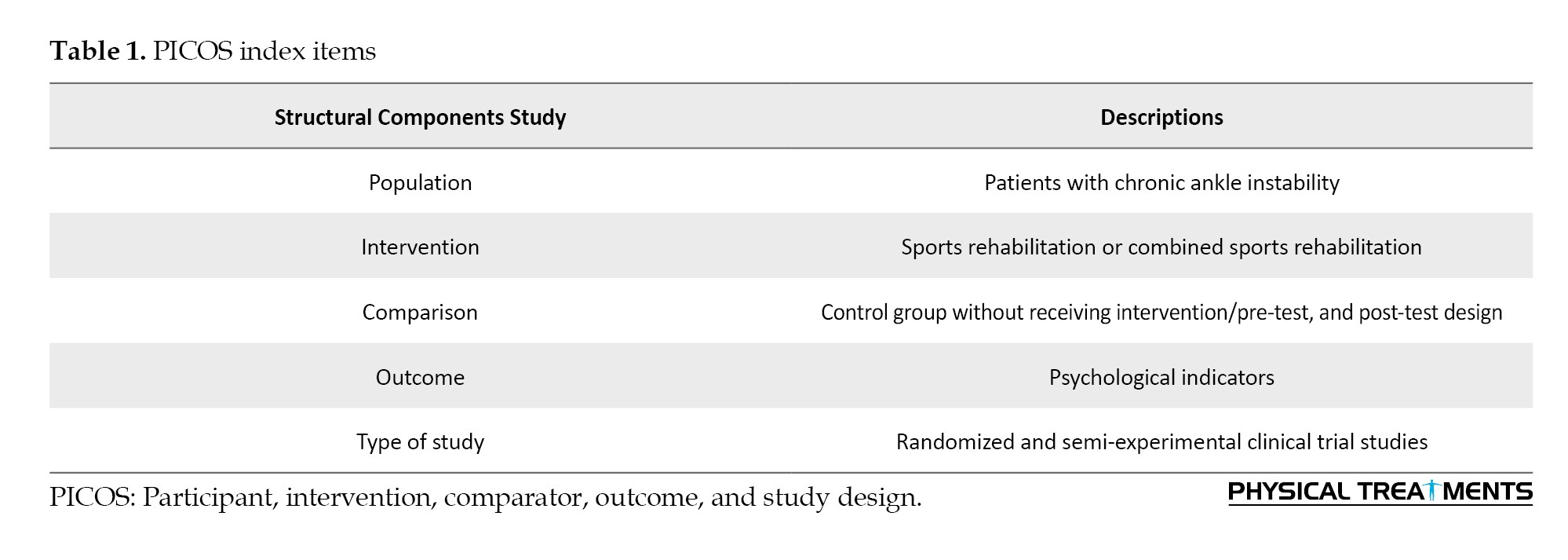
This systematic review was conducted by the guidelines outlined in the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement. The article search started on June 25, 2023, when two researchers (Masoud Azizian and Behnam Gholami-Borujeni) conducted a two-step research for the desired studies using the online databases of PubMed, SPORTDiscus, CINAHL, and Google Scholar. In the first step, the key terms “chronic ankle instability AND balance training OR neuromuscular training OR proprioceptive training OR rehabilitation OR exercise” were used to search the databases. The key terms “chronic ankle instability AND health-related quality of life OR fear of reinjury OR fear-avoidance beliefs questionnaire OR Tampa scale of kinesiophobia” were applied. A search was also conducted in other databases as well as unpublished articles, but no articles were included in the review through this process. The PICOS framework, considering patient (participant, problem, or population), intervention or exposure, control (comparator), outcome, and study design, was applied to include or exclude the studies [21] (Table 1).
Study selection
After removing duplicate studies, two researchers (Masoud Azizian and Behnam Gholami-Borujeni) reviewed the inclusion criteria for the articles based on their titles and abstracts and then excluded irrelevant cases. The full texts of the remaining studies were also reviewed to ensure that they met the inclusion criteria. Any conflicts between the researchers were then resolved by another researcher (Ali Yalfani). The mandatory criteria for selecting the articles were as follows: Language in English, studies published in the last 10 years, patients recruited from the CAI population undergoing rehabilitation interventions, studies that incorporated exercise-based rehabilitation (e.g. strength training, proprioceptive training, balance training), psychological indicators evaluated at the pre-test/post-test phases, experimental and quasi-experimental research designs, and full-text of the studies being available. The exclusion criteria included articles published in non-English languages, case reports, systematic reviews, or meta-analyses, studies that incorporated manual therapy as an intervention, articles using Kinesio-taping, and conference presentations. Both randomized and non-randomized intervention studies were included in the analysis.
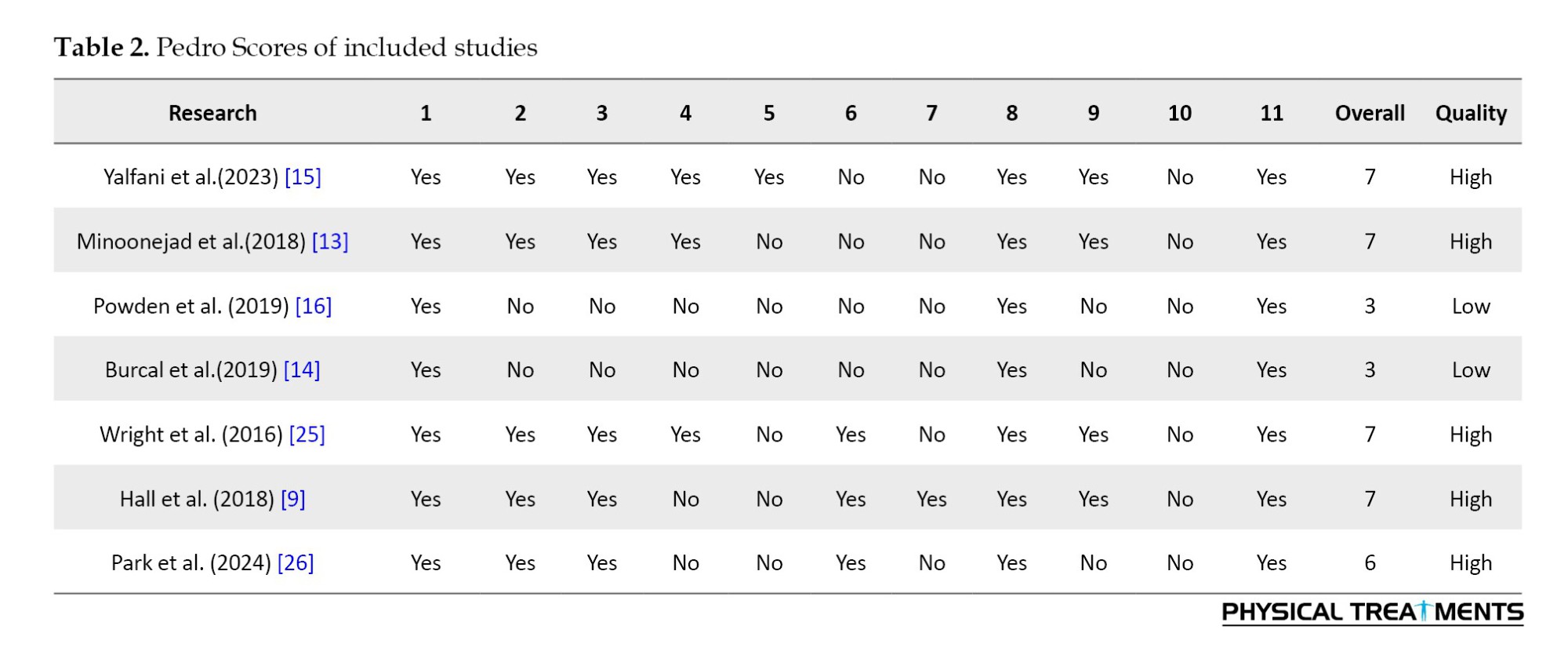
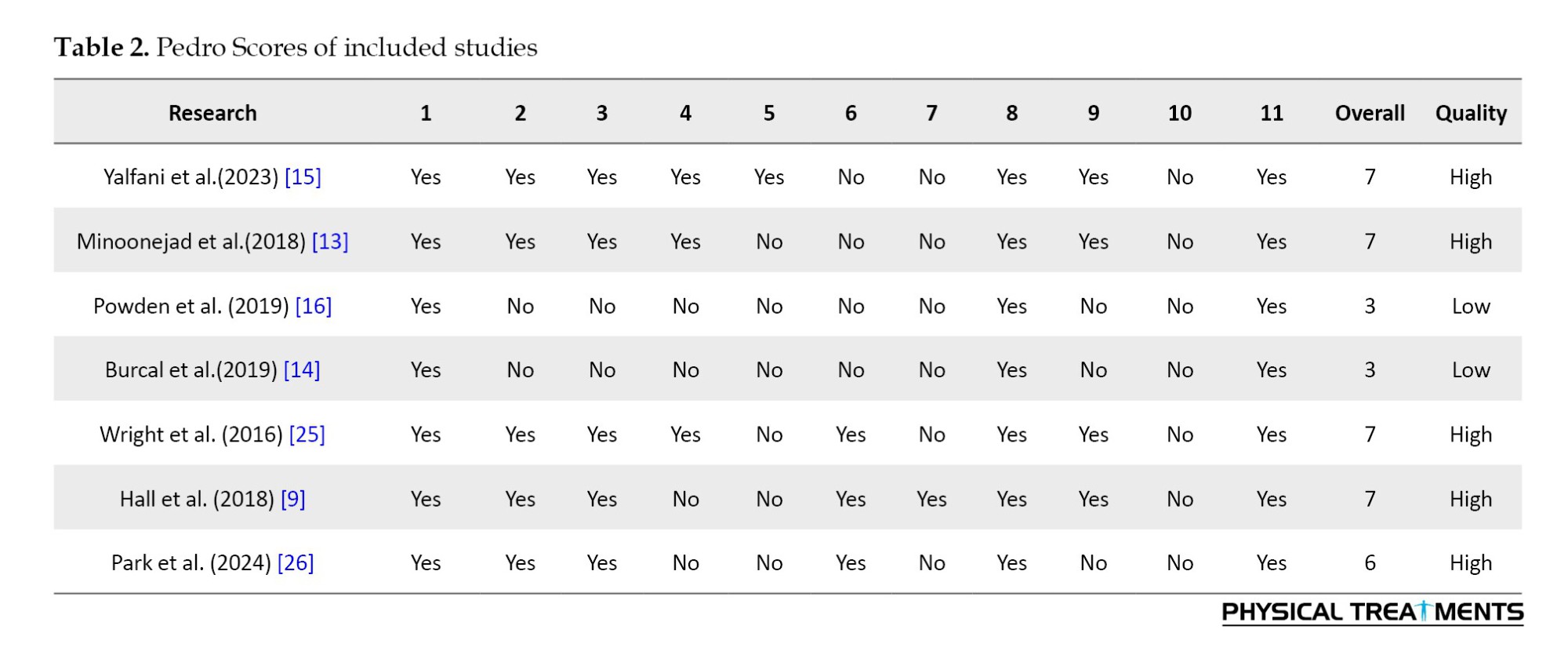
Study quality, certainty of evidence, and bias avoidance
The 11-item PEDro scale was utilized to measure the quality of the selected studies. This scale could reduce the risk of bias as a safe and reliable tool [22, 23]. The following criteria are measured: 1) Participants’ eligibility criteria are determined; 2) Participants are randomly assigned; 3) Participants are concealed; 4) Groups in the pre-test stage are similar; 5) Participants lack comprehension; 6) Participants lack comprehension of the researcher who carried out the exercise program; 7) Participants lack comprehension of the evaluators to measure the dependent variables; 8) The ratio of participants who have at least one key outcome in the measured dependent variable; 9) Participants’ compliance with the intervention; 10) Group comparisons statistically; and 11) Point and variability measures for at least one dependent variable. The answers “yes” and “no” to its items are scored as one and zero, respectively. No score is calculated for the first item, and the total score ranges from 0-10. Studies with scores >6 were considered of high quality, and those with scores below 6 were considered of low quality [18-24]. Two researchers (Masoud Azizian and Behnam Gholami-Borujeni) independently evaluated the articles using the PEDro scale. In the event of any disagreements, another researcher (Ali Yalfani) made the final decision (Table 2).
Results
Study selection
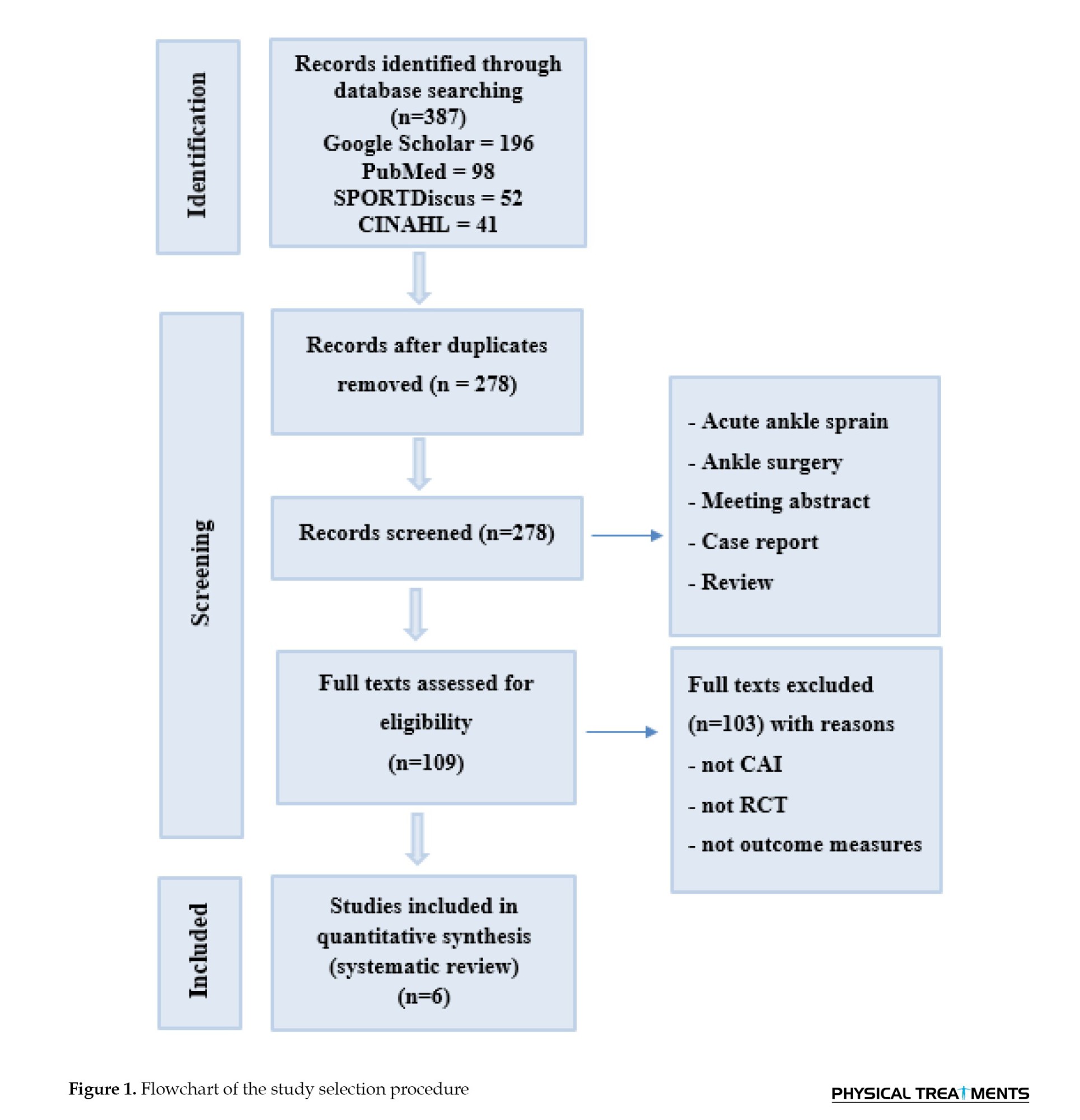
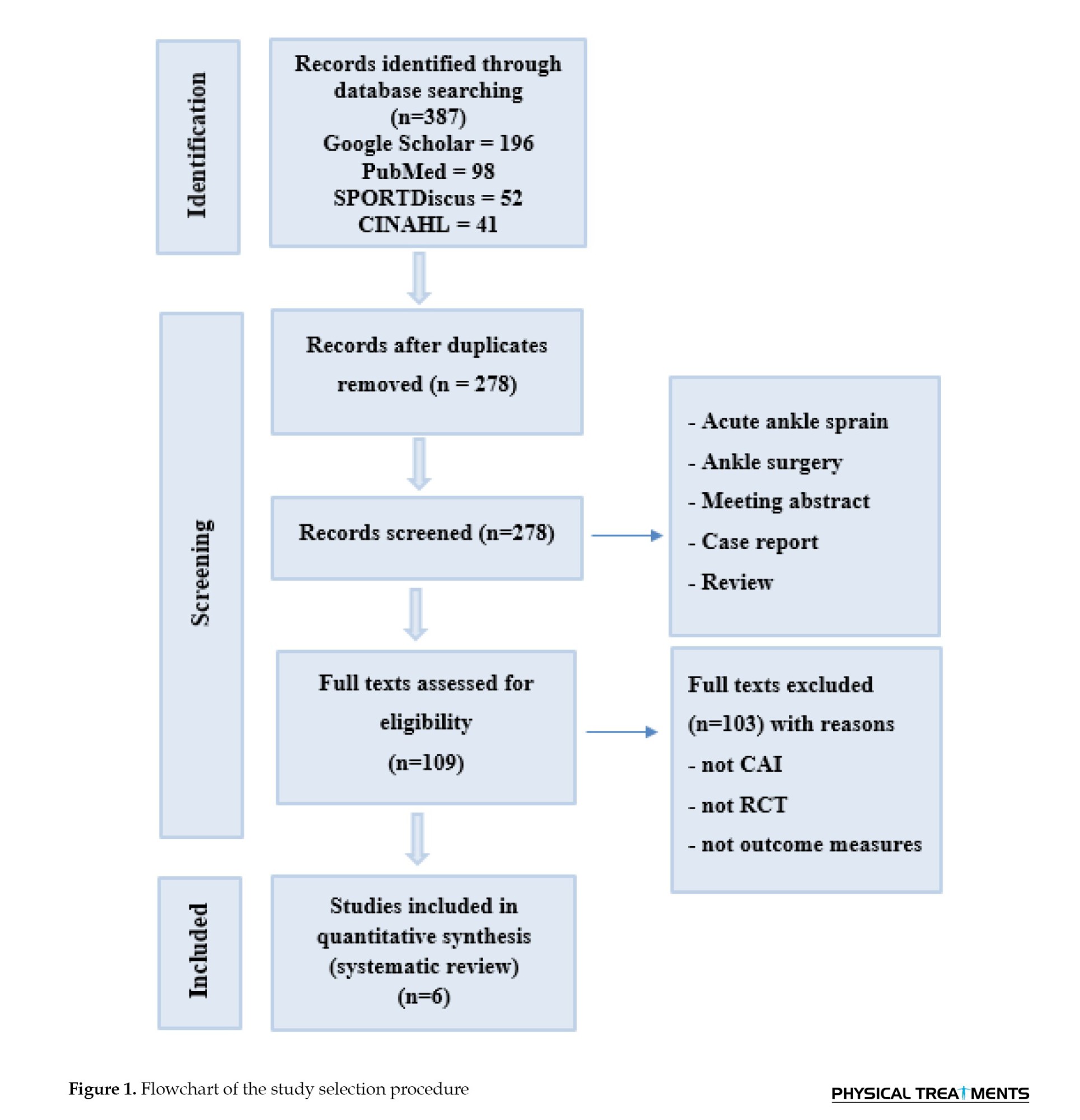
Figure 1 shows the study results. A total of 387 articles were retrieved. Of these, 196, 98, 52, and 41 studies were selected from Google Scholar, PubMed, SPORTDiscus, and CINAHL, respectively. Then, 278 articles were excluded for failing to meet the inclusion criteria. Moreover, 103 studies were removed due to the use of different interventions (Kinesio-taping), populations (acute ankle sprains), case studies, or systematic research designs. Finally, seven studies were selected for review.
Pedro scale
Of these six studies, four and two had high and low quality, respectively, according to the PEDro scale (Table 2).
Study characteristics
From the seven selected studies, four implemented rehabilitation protocols for four weeks [9, 13, 14, 25], while one study lasted six weeks [16] and another eight weeks [15]. Four studies used conventional (physical-only) rehabilitation protocols [9, 13, 14, 25], while two studies used multimodal rehabilitation protocols to evaluate psychological indicators. The systematic review results of seven selected articles, as described in Table 3, showed that multimodal rehabilitation had better outcomes than conventional rehabilitation protocols for improving QoL, kinesiophobia, and fear-avoidance beliefs in patients with CAI. These variables were crucial psychological indicators for the treatment and rehabilitation of individuals with CAI. Hall et al. compared the effects of balance and strength exercises on fear-avoidance beliefs in people with CAI. A total of 39 people with CAI (21 men and 18 women) with a mean age of 20.9±3.8 years. Their results showed a significant difference between balance and strength exercises in reducing fear-avoidance beliefs with a low effect size (P=0.1, η2=0.27) [9].
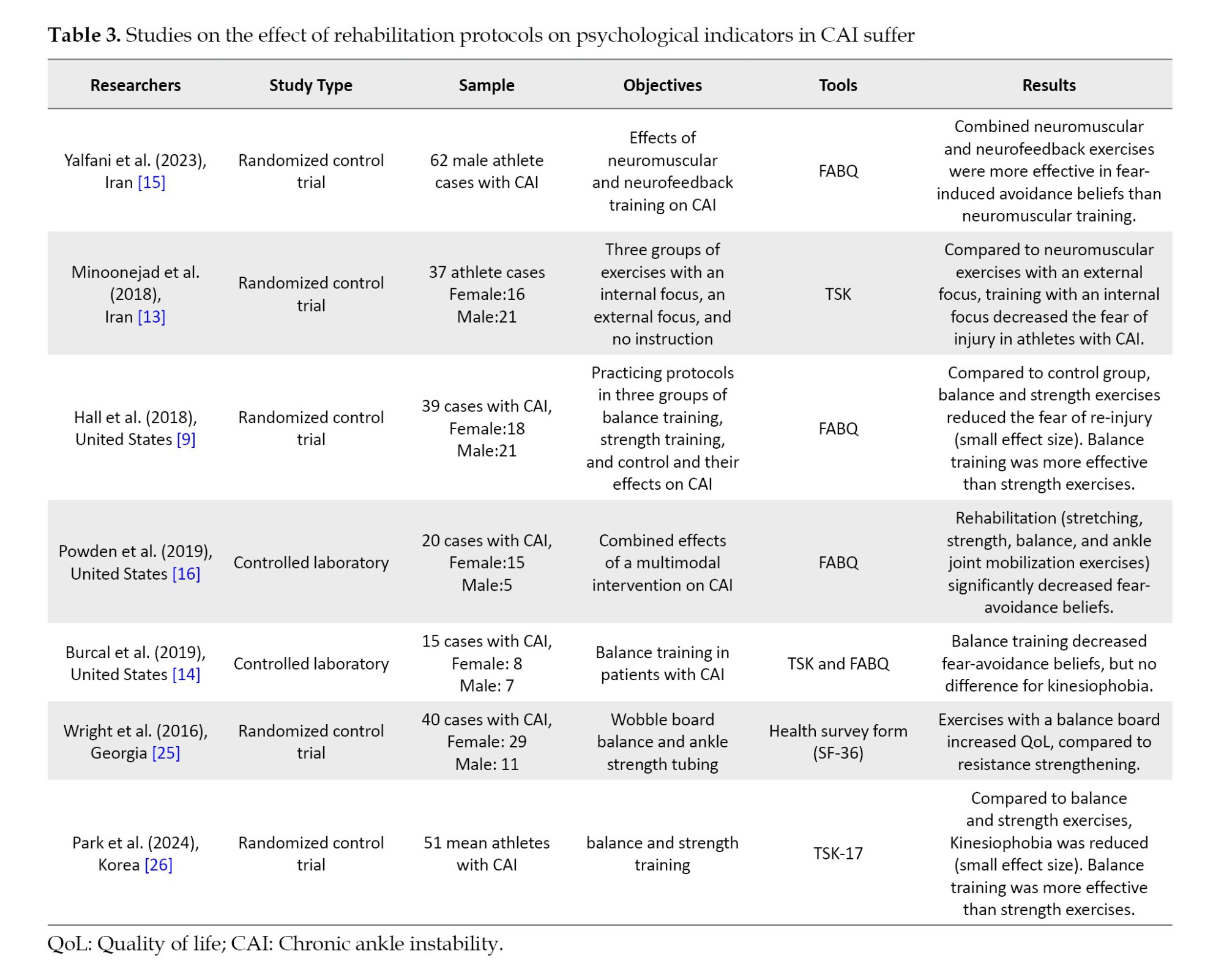
Minoonejad et al. compared the effect of combined neuromuscular exercises with internal and external attention, as well as neuromuscular exercises alone, on Kinesiophobia in athletes with CAI. A statistical sample of 37 athletes (21 boys, and 16 girls) with CAI, with a mean age of 21.61±1.6 years. Their results showed that neuromuscular exercises with internal attention reduced Kinesiophobia compared to neuromuscular exercises with external attention (P=0.001, η2=0.652) [13].
Burcal et al. compared the effect of balance exercises on Kinesiophobia and fear-avoidance beliefs in people with CAI. The statistical sample of 15 people (8 women, and 7 men) with CAI, with a mean age of 20.80±2.37 years. Their results showed that balance exercises reduced the fear-avoidance beliefs (pre=10.00±3.91, post=6.80±4.06). But these exercises did not reduce the Kinesiophobia (pre=19.60±4.34, post=17.73±2.71) [14].
Yelfani et al. compared the effect of combined neuromuscular training with neurofeedback to that of neuromuscular training alone on the fear-avoidance beliefs of athletes with CAI. The statistical sample of 62 male athletes with CAI had a mean age of 21.77±2.78 years. Their results showed that combined exercises reduced the fear-avoidance beliefs compared to neuromuscular exercises (P=0.001, η2=0.266) [15].
Powden et al. compared the effect of multifaceted exercises, including strength, balance, and mobilization, on the fear-avoidance beliefs of people with CAI. The statistical sample of 20 people (15 women, and 5 men) with CAI with a mean of 24.35±6.95 years. They reported that these exercises reduced avoidance beliefs caused by fear (P=0.001, η2=0.72) [16].
Wright et al. investigated the effect of two types of rehabilitation protocols, balance board exercises and resistance exercises, on the quality of life of individuals with CAI. A statistical sample of 40 people (29 women, and 11 men) with CAI with an average age of 22.02±4.56. They reported no difference between the two groups in terms of increasing the quality of life, with the balance board training group (pre=54.77±5.40, post=57.57±3.94) and the resistance training group (pre=52.36±5.94, post=55.56±4.11) [25].
Park et al. compared the effect of two types of balance and strength protocols on the fear of movement in adolescent athletes. They randomly divided 51 soccer players with CAI (14.23±0.73) and CAI into three groups: Strength, balance, and control exercises. They reported that balance and strength training reduced kinesiophobia (P=0.006,η2=1.25) [26].
Discussion
This systematic study aimed to compare the effects of conventional and combined rehabilitation protocols on psychological indicators (QoL,fear-avoidance beliefs, and Kinesiophobia) in patients with CAI. The selected articles showed the impact of conventional (e.g. balance, neuromuscular, strength, and proprioceptive training) and multimodal (both physical and mental) protocols on the psychological indicators of individuals with CAI. The study results demonstrated that multimodal protocols are more effective than conventional protocols on the indicators mentioned above [13, 15, 16, 26]. Studies have reported that balance, strength, proprioceptive, and neuromuscular exercises are effective in improving physical factors, because only exercises attempt to increase balance and strength [9, 14, 25]. Studies on psychological factors have shown inconsistent effects, andthese exercises have short-term effects [14]. On the other hand, combined exercises, including neuromuscular exercises with neurofeedback [15] and balance exercises with internal and external attention, can improve psychological factors in individuals with [13, 15]. The mechanism of combined exercises is that they improve both the musculoskeletal and neuropsychological aspects, which these types of protocols try to improve the CNS [15]. Park et al. noted that while balance exercises help people become more balanced and less kinesiophobic, they do not appear to be effective in eliminating kinesiophobia. They also suggested that incorporating balance training into training regimens can help address psychological and physical aspects of ankle instability [26].
As reported by the International Ankle Consortium in 2016, psychological rehabilitation seemed to be essential for individuals with CAI. Improving psychological indicators would result in a safer and faster return to regular daily and sports activities [26]. Patients with CAI could also experience reduced QoL and daily activities as well as kinesiophobia, which could decrease physical activities and psychological indicators [15]. It was also reported that lower QoL would decrease the ability of the feet and ankles during daily activities among CAI patients [12]. In this regard, physiotherapists and sports medicine therapists suggested that these mental indicators need to be considered in rehabilitation objectives [9]. A higher ability of the feet and ankles, as well as more physical activities, could also improve psychological indicators [15-26].
Compared to healthy individuals, patients with CAI were likely to experience changes in the CNS and motor control [27], which could result in the occurrence of CAI [28]. One of the major factors in the variations of CNS and the progression of CAI is the disturbance in the proprioceptive system of the ankle joint, which makes it unable to correctly recognize the precise movements of the joint [7]. Balance, proprioceptive, and strength exercises can thus strengthen the CNS and motor control [4-27]. Balance and proprioceptive exercises are common exercises for CAI rehabilitation [2]. These types of exercises can affect the disturbed proprioception of the joint and gradually improve it, as well as the CNS [17]. Compared to strength exercises, balance training may also have a more beneficial effect on the psychological indicators of patients with CAI [9] because it can correct the damaged proprioception of the joint and improve motor control [4]. Burcal et al. reported conflicting results on the effect of balance exercises as they decreased fear-induced avoidance beliefs, but kinesiophobia was not affected in CAI sufferers [14]. Besides, Minoonejad et al. observed that combined balance exercises using internal and external focus, compared to no focus, decreased kinesiophobia in athletes with CAI [13], indicating that balance training may not be solely effective for the rehabilitation of psychological indicators [14]. Because CAI is an injury that causes changes in the brain and mind of individuals, athletes often reduce their activity after this injury due to the fear of movement and re-injury [4, 15]. To improve movement planning and modify the CNS to improve psychological factors and rehabilitation of people with CAI, auxiliary protocols should be performed to influence the minds of patients [20]. Neuroplastic cortical alterations are also induced by injury-related fear and a history of ligamentous damage [28]. Injury-related fear and neuroplastic alterations linked to ligamentous damage may compete in the neural circuitry [3]. A person with a history of LAS may find that this competition interferes with their situational awareness by distracting them from the work at hand and filling their attention with fear or anxiety [15]. The cognitive-motor planning required to control a desired neuromuscular response may be affected by this disturbance, which can have a detrimental effect, such as re-injury of the ankle joint [29].
This study is consistent with the findings of Kasimis et al. who suggest that a four- to six-week of combined resistance and proprioceptive exercise program may improve the quality of life in athletes with CAI [30]. Needle et al. also showed that compared to conventional sports exercises, multimodal rehabilitation protocols are necessary for CAI patients [31]. As evidenced, much attention needs to be dedicated to the CNS and musculoskeletal system in rehabilitation protocols, and both psychosocial and physical indicators need to be considered [15]. Multimodal rehabilitation in patients with CAI could also affect both psychological and physical indicators [10-32]. Powden et al. reported the impact of multimodal rehabilitation protocols (including balance, strength, and mobilization exercises) on psychological indicators in CAI patients, concluding that multimodal rehabilitation was more effective than conventional protocols [16]. Some researchers believe that CAI is also a mental state [27-33]; therefore, mental disorders and changes in the CNS could make individuals prone to reinjures [4-35]. A recent study reported that adding mental neurofeedback exercises to conventional sports increases the effectiveness of the rehabilitation protocol for improving psychological indicators in athletes with CAI [15]. Therefore, multimodal rehabilitation protocols can more effectively improve CNS functioning as well as cognitive and musculoskeletal systems in patients with CAI [4, 36].
Conclusion
The results of the present study showed that multimodal rehabilitation is more effective than conventional rehabilitation protocols for improving the physical and psychological indicators of CAI patients. Such conventional programs (e.g. balance, strength, and proprioceptive training) cannot solely improve both physical and psychological indicators. Rehabilitation specialists are advised to add psychological exercises (neurofeedback and attention training) to the conventional protocol to simultaneously involve the CNS and musculoskeletal system in the rehabilitation program for CAI patients.
Limitations
One limitation of the present study was that the populations of the selected articles consisted of either athletes (two studies) or non-athletes (four studies) with CAI. As the type of rehabilitation exercises could vary for athletes and non-athletes, this limitation might have affected the study results. Another limitation was that the selected studies examined only three psychological indicators (QoL, kinesiophobia, and fear-induced avoidance beliefs), while other indicators (e.g. anxiety and depression) also seem crucial in CAI sufferers. The present study only investigated conventional and multimodal rehabilitation protocols in CAI patients. However, other rehabilitation protocols (e.g. cognitive protocols, brain electrical stimulation, and Kinesio-taping) have been applied in the literature and warrant investigation in future studies. Another limitation of the present study is that the nature of the interventions used and combined in the studies varied, which may have affected the effectiveness of the protocols.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grants from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Masoud Azizian and Behnam Gholami-Borujeni; Drafting the article: Masoud Azizian and Behnam Gholami-Borujeni; Review and editing: Ali Yalfani and Behnam Gholami-Borujeni; monitoring progress: Ali Yalfani; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors appreciate all individuals who contributed to the completion of this manuscript.
References
Lateral ankle sprains (LAS) are among the most common musculoskeletal injuries [1]. In the United States, over one million cases and approximately 23000 individuals are annually admitted to hospital emergency departments due to this condition [2]. LAS is one of the most prevalent injuries to the musculoskeletal system in athletes, non-athletes, and individuals involved in recreational activities [3]. LAS has also been reported as the most widespread recurrent lower extremity injury in most sports [4]. Notably, approximately 40% of individuals affected by LAS are susceptible to reinjuries, which cause chronic ankle instability (CAI) [5]. CAI is characterized by frequent sprains or ankle instability along with symptoms, such as pain, weakness, and a giving-way sensation in the legs, or limited range of motion in the ankle joint [6]. CAI can also damage joints, muscles, and sensory receptors [5], as well as mental and neuromuscular disorders [7]. Such problems can restrict recreational, work-related, and sporting activities in the long term [7]. This reduces health-related quality of life (QoL) and increases kinesiophobia or fear of movement/reinjury in patients with CAI [8].
A recent systematic review was reported. Psychological factors are among the most crucial rehabilitation factors in these people. Kinesiophobia and disabilities result from CAI, leading to an absence of physical activity [9]. CAI exacerbates general health and physical activity [10]. Physical inactivity has been classified as one of the three high-risk behaviors that induce cardiovascular diseases, cancer, diabetes mellitus, and obesity [7]. It was reported that individuals with CAI intensify their kinesiophobia, which diminishes their physical activity [9]. As recommended by the Centers for Disease Control and Prevention, adults should participate in at least 150 minutes of moderate-intensity activities and 75 minutes of high-intensity activities per week [2]. Physical activity is decreased in patients with CAI due to kinesiophobia and fear-avoidance beliefs [11], and this reduction is negatively associated with some chronic diseases. It is considered a risk factor [11]. In this respect, some tools, such as the multidimensional quality of life, Tampa Scale of Kinesiophobia (TSK), and Fear-Avoidance Beliefs Questionnaire (FABQ), have been advocated as useful methods to measure psychological indicators and physical activity in CAI patients [12]. Lower QoL has been related to lower environmental awareness of the body, followed by disturbed proprioception [13]. The central nervous system (CNS) receives information from the surrounding environment through visual and vestibular receptors to perform correct movements, known as body awareness [13]. Kinesiophobia, fear-avoidance beliefs, and quality of life are crucial psychological indicators for people with CAI [8]. Conversely, rehabilitation protocols can strengthen these patients mentally and musculoskeletally under different conditions [8]. Some interruptions in motor control and body awareness are among the most common disorders in CAI patients [14]. Therefore, it would be advantageous to offer an intervention that could lessen participant’s fear of reinjury; therefore, they can resume physical activity [9]. Numerous rehabilitation protocols, such as balance and strength exercises [15], have been shown to improve these symptoms [16]. Neuromuscular training has been introduced as an effective rehabilitation protocol for reducing the prevalence rate of ankle sprains or reinjuries [17]. Such exercises combine balance, proprioception, core stability, and strength [18]. Balance training includes single-leg exercises, performed with eyes open and closed to increasing balance. Also, proprioceptive training includes coordination skills and strengthens the central nervous system [15]. Together, these are useful for improving neuromuscular control in CAI patients [19]. Multimodal protocols for CAI treatment have also been reported to be more effective than simple protocols [15]. In a systematic review, Maricot et al. observed kinesiophobia and reduced QoL problems in CAI sufferers. They advised physiotherapists and sports medicine specialists to improve these factors and consider rehabilitation programs in their protocols [20]. Minoonejad et al. investigated the effects of balance training with an internal focus compared to exercises with an external focus, on kinesiophobia in athletes with CAI. They showed that balance training with an internal focus minimized fear in these individuals [13]. Using a randomized controlled trial, Burcal et al. reported the positive effects of balance exercises on kinesiophobia and fear-avoidance beliefs in patients with CAI [14]. Given the above, psychological indicators and their effects on CAI patients are crucial, and while numerous rehabilitation protocols have been implemented, it is unclear which protocol has better results. To the best of our knowledge, no study has been found to systematically examine the effects of different rehabilitation protocols on psychological indicators in CAI patients. The present study aimed to systematically review the impact of different rehabilitation protocols on psychological indicators in CAI sufferers. We hypothesized that different rehabilitation protocols have different effects on psychological indicators in CAI patients.
Materials and Methods
Searching strategy
This systematic review was conducted by the guidelines outlined in the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement. The article search started on June 25, 2023, when two researchers (Masoud Azizian and Behnam Gholami-Borujeni) conducted a two-step research for the desired studies using the online databases of PubMed, SPORTDiscus, CINAHL, and Google Scholar. In the first step, the key terms “chronic ankle instability AND balance training OR neuromuscular training OR proprioceptive training OR rehabilitation OR exercise” were used to search the databases. The key terms “chronic ankle instability AND health-related quality of life OR fear of reinjury OR fear-avoidance beliefs questionnaire OR Tampa scale of kinesiophobia” were applied. A search was also conducted in other databases as well as unpublished articles, but no articles were included in the review through this process. The PICOS framework, considering patient (participant, problem, or population), intervention or exposure, control (comparator), outcome, and study design, was applied to include or exclude the studies [21] (Table 1).
Study selection
After removing duplicate studies, two researchers (Masoud Azizian and Behnam Gholami-Borujeni) reviewed the inclusion criteria for the articles based on their titles and abstracts and then excluded irrelevant cases. The full texts of the remaining studies were also reviewed to ensure that they met the inclusion criteria. Any conflicts between the researchers were then resolved by another researcher (Ali Yalfani). The mandatory criteria for selecting the articles were as follows: Language in English, studies published in the last 10 years, patients recruited from the CAI population undergoing rehabilitation interventions, studies that incorporated exercise-based rehabilitation (e.g. strength training, proprioceptive training, balance training), psychological indicators evaluated at the pre-test/post-test phases, experimental and quasi-experimental research designs, and full-text of the studies being available. The exclusion criteria included articles published in non-English languages, case reports, systematic reviews, or meta-analyses, studies that incorporated manual therapy as an intervention, articles using Kinesio-taping, and conference presentations. Both randomized and non-randomized intervention studies were included in the analysis.
Study quality, certainty of evidence, and bias avoidance
The 11-item PEDro scale was utilized to measure the quality of the selected studies. This scale could reduce the risk of bias as a safe and reliable tool [22, 23]. The following criteria are measured: 1) Participants’ eligibility criteria are determined; 2) Participants are randomly assigned; 3) Participants are concealed; 4) Groups in the pre-test stage are similar; 5) Participants lack comprehension; 6) Participants lack comprehension of the researcher who carried out the exercise program; 7) Participants lack comprehension of the evaluators to measure the dependent variables; 8) The ratio of participants who have at least one key outcome in the measured dependent variable; 9) Participants’ compliance with the intervention; 10) Group comparisons statistically; and 11) Point and variability measures for at least one dependent variable. The answers “yes” and “no” to its items are scored as one and zero, respectively. No score is calculated for the first item, and the total score ranges from 0-10. Studies with scores >6 were considered of high quality, and those with scores below 6 were considered of low quality [18-24]. Two researchers (Masoud Azizian and Behnam Gholami-Borujeni) independently evaluated the articles using the PEDro scale. In the event of any disagreements, another researcher (Ali Yalfani) made the final decision (Table 2).
Results
Study selection
Figure 1 shows the study results. A total of 387 articles were retrieved. Of these, 196, 98, 52, and 41 studies were selected from Google Scholar, PubMed, SPORTDiscus, and CINAHL, respectively. Then, 278 articles were excluded for failing to meet the inclusion criteria. Moreover, 103 studies were removed due to the use of different interventions (Kinesio-taping), populations (acute ankle sprains), case studies, or systematic research designs. Finally, seven studies were selected for review.
Pedro scale
Of these six studies, four and two had high and low quality, respectively, according to the PEDro scale (Table 2).
Study characteristics
From the seven selected studies, four implemented rehabilitation protocols for four weeks [9, 13, 14, 25], while one study lasted six weeks [16] and another eight weeks [15]. Four studies used conventional (physical-only) rehabilitation protocols [9, 13, 14, 25], while two studies used multimodal rehabilitation protocols to evaluate psychological indicators. The systematic review results of seven selected articles, as described in Table 3, showed that multimodal rehabilitation had better outcomes than conventional rehabilitation protocols for improving QoL, kinesiophobia, and fear-avoidance beliefs in patients with CAI. These variables were crucial psychological indicators for the treatment and rehabilitation of individuals with CAI. Hall et al. compared the effects of balance and strength exercises on fear-avoidance beliefs in people with CAI. A total of 39 people with CAI (21 men and 18 women) with a mean age of 20.9±3.8 years. Their results showed a significant difference between balance and strength exercises in reducing fear-avoidance beliefs with a low effect size (P=0.1, η2=0.27) [9].
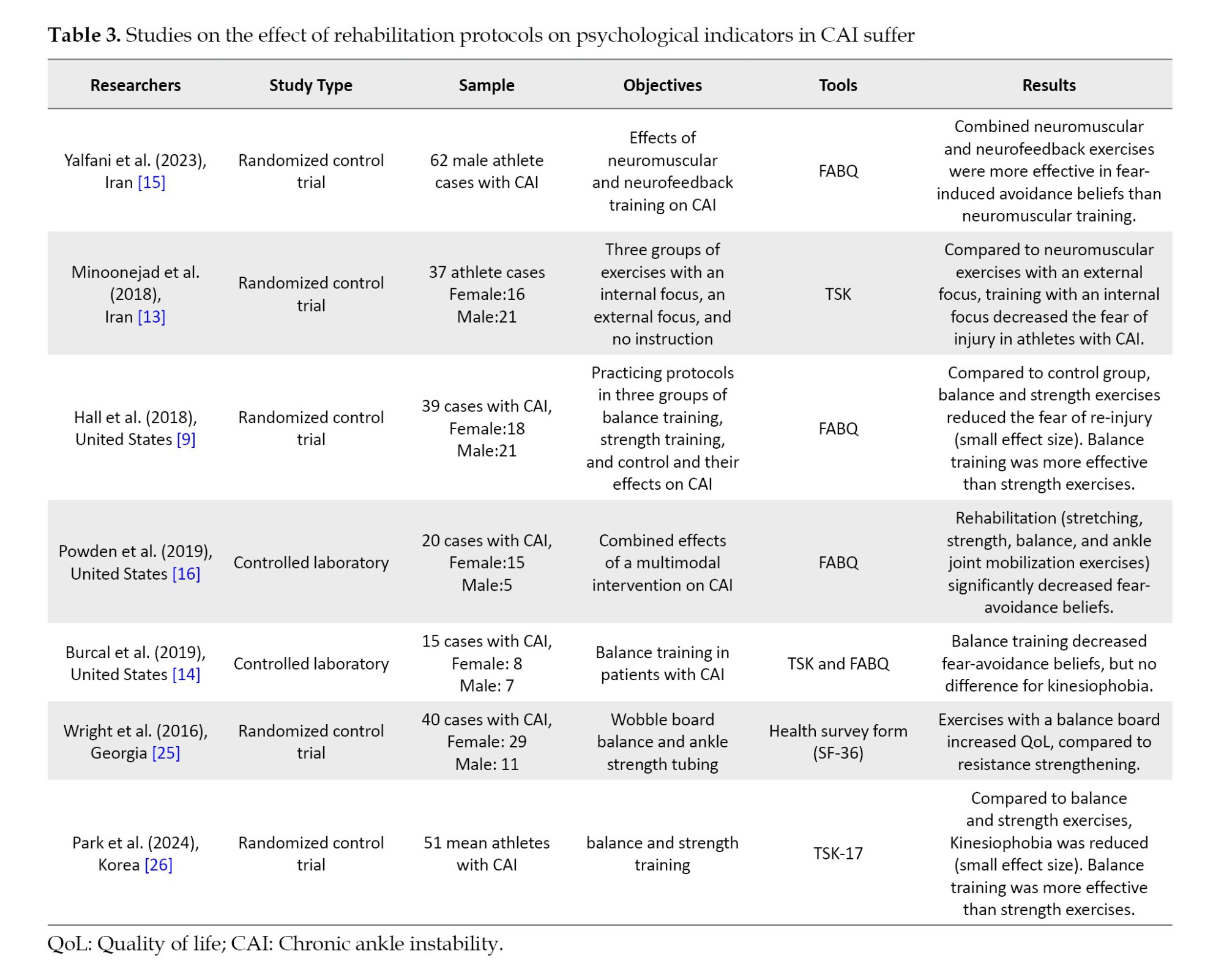
Minoonejad et al. compared the effect of combined neuromuscular exercises with internal and external attention, as well as neuromuscular exercises alone, on Kinesiophobia in athletes with CAI. A statistical sample of 37 athletes (21 boys, and 16 girls) with CAI, with a mean age of 21.61±1.6 years. Their results showed that neuromuscular exercises with internal attention reduced Kinesiophobia compared to neuromuscular exercises with external attention (P=0.001, η2=0.652) [13].
Burcal et al. compared the effect of balance exercises on Kinesiophobia and fear-avoidance beliefs in people with CAI. The statistical sample of 15 people (8 women, and 7 men) with CAI, with a mean age of 20.80±2.37 years. Their results showed that balance exercises reduced the fear-avoidance beliefs (pre=10.00±3.91, post=6.80±4.06). But these exercises did not reduce the Kinesiophobia (pre=19.60±4.34, post=17.73±2.71) [14].
Yelfani et al. compared the effect of combined neuromuscular training with neurofeedback to that of neuromuscular training alone on the fear-avoidance beliefs of athletes with CAI. The statistical sample of 62 male athletes with CAI had a mean age of 21.77±2.78 years. Their results showed that combined exercises reduced the fear-avoidance beliefs compared to neuromuscular exercises (P=0.001, η2=0.266) [15].
Powden et al. compared the effect of multifaceted exercises, including strength, balance, and mobilization, on the fear-avoidance beliefs of people with CAI. The statistical sample of 20 people (15 women, and 5 men) with CAI with a mean of 24.35±6.95 years. They reported that these exercises reduced avoidance beliefs caused by fear (P=0.001, η2=0.72) [16].
Wright et al. investigated the effect of two types of rehabilitation protocols, balance board exercises and resistance exercises, on the quality of life of individuals with CAI. A statistical sample of 40 people (29 women, and 11 men) with CAI with an average age of 22.02±4.56. They reported no difference between the two groups in terms of increasing the quality of life, with the balance board training group (pre=54.77±5.40, post=57.57±3.94) and the resistance training group (pre=52.36±5.94, post=55.56±4.11) [25].
Park et al. compared the effect of two types of balance and strength protocols on the fear of movement in adolescent athletes. They randomly divided 51 soccer players with CAI (14.23±0.73) and CAI into three groups: Strength, balance, and control exercises. They reported that balance and strength training reduced kinesiophobia (P=0.006,η2=1.25) [26].
Discussion
This systematic study aimed to compare the effects of conventional and combined rehabilitation protocols on psychological indicators (QoL,fear-avoidance beliefs, and Kinesiophobia) in patients with CAI. The selected articles showed the impact of conventional (e.g. balance, neuromuscular, strength, and proprioceptive training) and multimodal (both physical and mental) protocols on the psychological indicators of individuals with CAI. The study results demonstrated that multimodal protocols are more effective than conventional protocols on the indicators mentioned above [13, 15, 16, 26]. Studies have reported that balance, strength, proprioceptive, and neuromuscular exercises are effective in improving physical factors, because only exercises attempt to increase balance and strength [9, 14, 25]. Studies on psychological factors have shown inconsistent effects, andthese exercises have short-term effects [14]. On the other hand, combined exercises, including neuromuscular exercises with neurofeedback [15] and balance exercises with internal and external attention, can improve psychological factors in individuals with [13, 15]. The mechanism of combined exercises is that they improve both the musculoskeletal and neuropsychological aspects, which these types of protocols try to improve the CNS [15]. Park et al. noted that while balance exercises help people become more balanced and less kinesiophobic, they do not appear to be effective in eliminating kinesiophobia. They also suggested that incorporating balance training into training regimens can help address psychological and physical aspects of ankle instability [26].
As reported by the International Ankle Consortium in 2016, psychological rehabilitation seemed to be essential for individuals with CAI. Improving psychological indicators would result in a safer and faster return to regular daily and sports activities [26]. Patients with CAI could also experience reduced QoL and daily activities as well as kinesiophobia, which could decrease physical activities and psychological indicators [15]. It was also reported that lower QoL would decrease the ability of the feet and ankles during daily activities among CAI patients [12]. In this regard, physiotherapists and sports medicine therapists suggested that these mental indicators need to be considered in rehabilitation objectives [9]. A higher ability of the feet and ankles, as well as more physical activities, could also improve psychological indicators [15-26].
Compared to healthy individuals, patients with CAI were likely to experience changes in the CNS and motor control [27], which could result in the occurrence of CAI [28]. One of the major factors in the variations of CNS and the progression of CAI is the disturbance in the proprioceptive system of the ankle joint, which makes it unable to correctly recognize the precise movements of the joint [7]. Balance, proprioceptive, and strength exercises can thus strengthen the CNS and motor control [4-27]. Balance and proprioceptive exercises are common exercises for CAI rehabilitation [2]. These types of exercises can affect the disturbed proprioception of the joint and gradually improve it, as well as the CNS [17]. Compared to strength exercises, balance training may also have a more beneficial effect on the psychological indicators of patients with CAI [9] because it can correct the damaged proprioception of the joint and improve motor control [4]. Burcal et al. reported conflicting results on the effect of balance exercises as they decreased fear-induced avoidance beliefs, but kinesiophobia was not affected in CAI sufferers [14]. Besides, Minoonejad et al. observed that combined balance exercises using internal and external focus, compared to no focus, decreased kinesiophobia in athletes with CAI [13], indicating that balance training may not be solely effective for the rehabilitation of psychological indicators [14]. Because CAI is an injury that causes changes in the brain and mind of individuals, athletes often reduce their activity after this injury due to the fear of movement and re-injury [4, 15]. To improve movement planning and modify the CNS to improve psychological factors and rehabilitation of people with CAI, auxiliary protocols should be performed to influence the minds of patients [20]. Neuroplastic cortical alterations are also induced by injury-related fear and a history of ligamentous damage [28]. Injury-related fear and neuroplastic alterations linked to ligamentous damage may compete in the neural circuitry [3]. A person with a history of LAS may find that this competition interferes with their situational awareness by distracting them from the work at hand and filling their attention with fear or anxiety [15]. The cognitive-motor planning required to control a desired neuromuscular response may be affected by this disturbance, which can have a detrimental effect, such as re-injury of the ankle joint [29].
This study is consistent with the findings of Kasimis et al. who suggest that a four- to six-week of combined resistance and proprioceptive exercise program may improve the quality of life in athletes with CAI [30]. Needle et al. also showed that compared to conventional sports exercises, multimodal rehabilitation protocols are necessary for CAI patients [31]. As evidenced, much attention needs to be dedicated to the CNS and musculoskeletal system in rehabilitation protocols, and both psychosocial and physical indicators need to be considered [15]. Multimodal rehabilitation in patients with CAI could also affect both psychological and physical indicators [10-32]. Powden et al. reported the impact of multimodal rehabilitation protocols (including balance, strength, and mobilization exercises) on psychological indicators in CAI patients, concluding that multimodal rehabilitation was more effective than conventional protocols [16]. Some researchers believe that CAI is also a mental state [27-33]; therefore, mental disorders and changes in the CNS could make individuals prone to reinjures [4-35]. A recent study reported that adding mental neurofeedback exercises to conventional sports increases the effectiveness of the rehabilitation protocol for improving psychological indicators in athletes with CAI [15]. Therefore, multimodal rehabilitation protocols can more effectively improve CNS functioning as well as cognitive and musculoskeletal systems in patients with CAI [4, 36].
Conclusion
The results of the present study showed that multimodal rehabilitation is more effective than conventional rehabilitation protocols for improving the physical and psychological indicators of CAI patients. Such conventional programs (e.g. balance, strength, and proprioceptive training) cannot solely improve both physical and psychological indicators. Rehabilitation specialists are advised to add psychological exercises (neurofeedback and attention training) to the conventional protocol to simultaneously involve the CNS and musculoskeletal system in the rehabilitation program for CAI patients.
Limitations
One limitation of the present study was that the populations of the selected articles consisted of either athletes (two studies) or non-athletes (four studies) with CAI. As the type of rehabilitation exercises could vary for athletes and non-athletes, this limitation might have affected the study results. Another limitation was that the selected studies examined only three psychological indicators (QoL, kinesiophobia, and fear-induced avoidance beliefs), while other indicators (e.g. anxiety and depression) also seem crucial in CAI sufferers. The present study only investigated conventional and multimodal rehabilitation protocols in CAI patients. However, other rehabilitation protocols (e.g. cognitive protocols, brain electrical stimulation, and Kinesio-taping) have been applied in the literature and warrant investigation in future studies. Another limitation of the present study is that the nature of the interventions used and combined in the studies varied, which may have affected the effectiveness of the protocols.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grants from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Masoud Azizian and Behnam Gholami-Borujeni; Drafting the article: Masoud Azizian and Behnam Gholami-Borujeni; Review and editing: Ali Yalfani and Behnam Gholami-Borujeni; monitoring progress: Ali Yalfani; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors appreciate all individuals who contributed to the completion of this manuscript.
References
- Hall EA, Chomistek AK, Kingma JJ, Docherty CL. Balance-and strength-training protocols to improve chronic ankle instability deficits, part I: Assessing clinical outcome measures. Journal of Athletic Training. 2018; 53(6):568-77. [DOI:10.4085/1062-6050-385-16] [PMID]
- Simon JE, Docherty CL. Health-related quality of life is decreased in middle-aged adults with chronic ankle instability. Journal of Science and Medicine in Sport. 2018; 21(12):1206-9. [DOI:10.1016/j.jsams.2018.05.008] [PMID]
- Fraser JJ, Koldenhoven RM, Jaffri AH, Park JS, Saliba SF, Hart JM, et al. Foot impairments contribute to functional limitation in individuals with ankle sprain and chronic ankle instability. Knee Surgery, Sports Traumatology, Arthroscopy. 2020; 28(5):1600-10. [DOI:10.1007/s00167-018-5028-x] [PMID]
- Rosen AB, McGrath ML, Maerlender AL. Males with chronic ankle instability demonstrate deficits in neurocognitive function compared to control and copers. Research in Sports Medicine. 2021; 29(2):116-28. [DOI:10.1080/15438627.2020.1723099] [PMID]
- Fakontis C, Iakovidis P, Kasimis K, Lytras D, Koutras G, Fetlis A, et al. Efficacy of resistance training with elastic bands compared to proprioceptive training on balance and self-report measures in patients with chronic ankle instability: A systematic review and meta-analysis. Physical Therapy in Sport. 2023; 64:74-84. [DOI:10.1016/j.ptsp.2023.09.009] [PMID]
- Hertel J, Corbett RO. An updated model of chronic ankle instability. Journal of Athletic Training. 2019; 54(6):572-88. [DOI:10.4085/1062-6050-344-18] [PMID]
- Holland B, Needle AR, Battista RA, West ST, Christiana RW. Physical activity levels among rural adolescents with a history of ankle sprain and chronic ankle instability. Plos One. 2019; 14(4):e0216243. [DOI:10.1371/journal.pone.0216243] [PMID]
- Kosik KB, Johnson NF, Terada M, Thomas-Fenwick AC, Mattacola CG, Gribble PA. Health-related quality of life among middle-aged adults with chronic ankle instability, copers, and uninjured controls. Journal of Athletic Training. 2020; 55(7):733-8. [DOI:10.4085/1062-6050-190-19] [PMID]
- Hall EA, Docherty CL, Simon J, Kingma JJ, Klossner JC. Strength-training protocols to improve deficits in participants with chronic ankle instability: A randomized controlled trial. Journal of Athletic Training. 2015; 50(1):36-44. [DOI:10.4085/1062-6050-49.3.71] [PMID]
- Feyzioğlu Ö, Öztürk Ö, Gadis S. Effect of chronic ankle instability on functionality, mental and physical health among elite athletes: A case-control study. Turkiye Klinikleri Journal of Sports Sciences. 2023; 15(1):123-30. [DOI:10.5336/sportsci.2022-92483]
- Hubbard-Turner T, Turner MJ. Physical activity levels in college students with chronic ankle instability. Journal of Athletic Training. 2015; 50(7):742-7. [DOI:10.4085/1062-6050-50.3.05] [PMID]
- Houston MN, Van Lunen BL, Hoch MC. Health-related quality of life in individuals with chronic ankle instability. Journal of Athletic Training. 2014; 49(6):758-63. [DOI:10.4085/1062-6050-49.3.54] [PMID]
- Minoonejad H, Bazrafshan H, Akoochakian M, Aslani M. Effect of attention instructions of balance training in athletes with ankle instability. Physical Treatments-Specific Physical Therapy Journal. 2018; 8(1):45-54. [DOI:10.32598/ptj.8.1.45]
- Burcal CJ, Jeon H, Gonzales JM, Faust ME, Thomas AC, Hubbard-Turner TJ, et al. Cortical measures of motor planning and balance training in patients with chronic ankle instability. Journal of Athletic Training. 2019; 54(6):727-36. [DOI:10.4085/1062-6050-450-17] [PMID]
- Yalfani A, Azizian M, Gholami-Borujeni B. Adding neurofeedback training to neuromuscular training for rehabilitation of chronic ankle instability: A 3-arm randomized controlled trial. Sports Health. 2023; 16(5):797-807.[DOI:10.1177/19417381231219198] [PMID]
- Powden CJ, Hoch JM, Jamali BE, Hoch MC. A 4-week multimodal intervention for individuals with chronic ankle instability: Examination of disease-oriented and patient-oriented outcomes. Journal of Athletic Training. 2019; 54(4):384-396. [DOI:10.4085/1062-6050-344-17] [PMID]
- Kim KJ, Kim YE, Jun HJ, Lee JS, Ji SH, Ji SG, et al. Which treatment is more effective for functional ankle instability: Strengthening or combined muscle strengthening and proprioceptive exercises? Journal of Physical Therapy Science. 2014; 26(3):385-8. [DOI:10.1589/jpts.26.385] [PMID]
- Caldemeyer LE, Brown SM, Mulcahey MK. Neuromuscular training for the prevention of ankle sprains in female athletes: A systematic review. The Physician and Sportsmedicine. 2020; 48(4):363-9. [DOI:10.1080/00913847.2020.1732246] [PMID]
- Baral N, Pearlson K. Effect of proprioceptive training on fear of re-injury and functional performance in athletes with Lateral Ankle Sprain (LAS). RGUHS Journal of Physiotherapy. 2021; 1(1):1-6. [DOI:10.26463/rjpt.1_1_3]
- Maricot A, Dick E, Walravens A, Pluym B, Lathouwers E, De Pauw K, et al. Brain Neuroplasticity Related to Lateral Ankle Ligamentous Injuries: A systematic review. Sports Medicine. 2023; 53(7):1423-43. [DOI:10.1007/s40279-023-01834-z] [PMID]
- Lawry-Popelka B, Chung S, McCann RS. Cross-education balance effects after unilateral rehabilitation in individuals with chronic ankle instability: A systematic review. Journal of Athletic Training. 2022; 57(11-12):1055-61. [DOI:10.4085/1062-6050-625-21] [PMID]
- Sedaghati P, Baharmast Hossein Abadi A, Zolghadr H. Effect of core stability exercises on volleyball players: A systematic review. Physical Treatments-Specific Physical Therapy Journal. 2023; 13(3):147-58. [DOI:10.32598/ptj.13.3.405.3]
- Herbert R, Moseley A, Sherrington C. PEDro: A database of randomised controlled trials in physiotherapy. Health Information Management. 1998; 28(4):186-8. [DOI:10.1177/183335839902800410] [PMID]
- Luan L, Zhu M, Adams R, Witchalls J, Pranata A, Han J. Effects of acupuncture or similar needling therapy on pain, proprioception, balance, and self-reported function in individuals with chronic ankle instability: A systematic review and meta-analysis. Complementary Therapies in Medicine. 2023; 77:102983. [DOI:10.1016/j.ctim.2023.102983] [PMID]
- Wright CJ, Linens SW, Cain MS. A randomized controlled trial comparing rehabilitation efficacy in chronic ankle instability. Journal of Sport Rehabilitation. 2017; 26(4):238-49. [DOI:10.1123/jsr.2015-0189] [PMID]
- Park HS, Oh JK, Kim JY, Yoon JH. The effect of strength and balance training on kinesiophobia, ankle instability, function, and performance in elite adolescent soccer players with functional ankle instability: A prospective cluster randomized controlled trial. Journal of Sports Science & Medicine. 2024; 23(1):323-332. [DOI:10.52082/jssm.2024.593] [PMID]
- Gribble PA, Bleakley CM, Caulfield BM, Docherty CL, Fourchet F, Fong DT, et al. Evidence review for the 2016 International Ankle Consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. British Journal of Sports Medicine. 2016; 50(24):1496-505. [DOI:10.1136/bjsports-2016-096189] [PMID]
- Maricot AR, Dick EA, Walravens AA, Pluym B, Verschueren J, Tassignon B, et al. Brain plasticity in patients with lateral ankle sprain and chronic ankle instability: A systematic review. Paper presente at: 26e Symposium Vereniging voor Bewegings-en Sportwetenschappen. 2021 December 10; Brussels, Belgium.
- Bain KA, Hoch MC, Kosik KB, Gribble PA, Hoch JM. Psychological impairments in individuals with history of ankle sprain: A systematic review. Physiotherapy Theory and Practice. 2022; 38(12):1889-907. [DOI:10.1080/09593985.2021.1920079] [PMID]
- Kasimis K, Iakovidis P, Lytras D, Koutras G, Fetlis A, Myrogiannis IS. Effects of resistance and proprioceptive training on an athletic population with chronic ankle instability: A scoping review. Critical Reviews™ in Physical and Rehabilitation Medicine. 2024; 36(1). [Link]
- Needle AR, Lepley AS, Grooms DR. Central nervous system adaptation after ligamentous injury: A summary of theories, evidence, and clinical interpretation. Sports Medicine. 2017; 47(7):1271-88. [DOI:10.1007/s40279-016-0666-y] [PMID]
- Arnold BL, Wright CJ, Ross SE. Functional ankle instability and health-related quality of life. Journal of Athletic Training. 2011; 46(6):634-41. [DOI:10.4085/1062-6050-46.6.634] [PMID]
- Terada M, Kosik KB, Gribble PA. Association of diaphragm contractility and postural control in a chronic ankle instability population: A preliminary study. Sports Health. 2024; 16(1):19-25. [DOI:10.1177/19417381221147304] [PMID]
- Al Mahrouqi MM, MacDonald DA, Vicenzino B, Smith MD. Quality of life, function and disability in individuals with chronic ankle symptoms: A cross-sectional online survey. Journal of Foot and Ankle Research. 2020; 13(1):67. [DOI:10.1186/s13047-020-00432-w] [PMID]
- Houston MN, Hoch JM, Hoch MC. Patient-reported outcome measures in individuals with chronic ankle instability: A systematic review. Journal of Athletic Training. 2015; 50(10):1019-33. [DOI:10.4085/1062-6050-50.9.01] [PMID]
- Liu N, Yang C, Song Q, Yang F, Chen Y. Patients with chronic ankle instability exhibit increased sensorimotor cortex activation and correlation with poorer lateral balance control ability during single-leg stance: A FNIRS study. Frontiers in Human Neuroscience. 2024; 18:1366443. [DOI:10.3389/fnhum.2024.1366443] [PMID] [PMCID]
Type of Study: Research |
Subject:
Sport injury and corrective exercises
Received: 2024/09/3 | Accepted: 2025/01/7 | Published: 2025/10/18
Received: 2024/09/3 | Accepted: 2025/01/7 | Published: 2025/10/18
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |