Mon, Feb 2, 2026
Volume 15, Issue 2 (Spring 2025)
PTJ 2025, 15(2): 131-140 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mahmoudi Z, Mohammadi R, Paknazar F. The Impact of Quadratus Plantae Muscle Dry Needling on Pain and Thickness of the Plantar Fascia in Individuals With Plantar Fasciitis. PTJ 2025; 15 (2) :131-140
URL: http://ptj.uswr.ac.ir/article-1-669-en.html
URL: http://ptj.uswr.ac.ir/article-1-669-en.html
1- Student Research Committee, Semnan University of Medical Sciences, Semnan, Iran.
2- Neuromusculoskeletal Rehabilitation Research Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
3- Social Determinants of Health Research Center, Semnan University of Medical Sciences, Semnan, Iran.
2- Neuromusculoskeletal Rehabilitation Research Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
3- Social Determinants of Health Research Center, Semnan University of Medical Sciences, Semnan, Iran.
Full-Text [PDF 1365 kb]
(1031 Downloads)
| Abstract (HTML) (2837 Views)
Full-Text: (371 Views)
Introduction
Plantar fasciitis is the most common cause of non-traumatic adult heel pain [1] and one of the common causes of pain and disability, which occurs in approximately 10% of the general population throughout their lifetime [2]. Diagnosis is usually based on history, physical evaluation, and the presence of pain on the inner side of the heel [3]. Plantar fasciitis has a gradual onset and often worsens after a few weeks or months [4]. It is associated with persistent, knifelike pain [5] in the bottom of the foot near the heel. The pain usually occurs in the early morning on the first step after immobility [5], and heel tenderness was also reported [6]. Plantar fasciitis is associated with obesity (body mass index [BMI] over 30), variations in physical activity level, prolonged periods of standing, alteration in foot arch [7], sedentary lifestyle [8], and calf muscle shortness [9]. Even though heel pain is quite common and significantly impacts quality of life (QoL), there is no optimal treatment [10]. Several treatments are recommended for plantar fasciitis [11]. In the initial stage, conservative treatments, including rest, custom-made insoles (orthotic insoles), night splints, and stretching exercises, are widely used to relieve symptoms [12]. Manual treatments, including joint and soft tissue mobilization, manual stretching of calf muscles, the release of trigger points [13], and nerve mobilization techniques [14], can be effective on plantar fasciitis. Drug therapy, platelet-enriched plasma treatment [15], shockwave therapy [16], botulism toxin, ultrasound, tapping techniques [11, 17] and low level laser therapy [18] are suggested for plantar fasciitis. Travell and Simons proposed that trigger points (TrPs) in the intrinsic muscles of the foot and surrounding muscles can significantly contribute to heel pain [19]. Some studies reported trigger points of soleus [20], gastrocnemius [13, 20-22], posterior tibialis [23], popliteal [23], abductor halluces [20, 21, 24], flexor halluces [21], peroneus longus [23], flexor digitorum brevis [20, 24], and quadratus plantaris muscles [20, 21] in patients with heel pain. Quadratus plantae has proximal anatomic attachment sites and mechanical function with the plantar fascia [24]. Several studies mentioned the role of the quadratus plantae muscle in the pathogenesis of heel pain [25]. The lateral plantar nerve contains sensory fibers that serve the calcaneal periosteum, the plantar ligament, the medial head of the quadratus plantae, and motor fibers that innervate the quadratus plantae muscle. Consequently, if the lateral plantar nerve gets trapped between the two heads of the quadratus plantae muscle, it can lead to heel pain [26]. The quadratus plantae and flexor hallucis brevis contain several active trigger points in individuals experiencing plantar heel pain. Since both muscles are anatomically and intrinsically linked to the plantar fascia, the taut bands associated with their trigger points can create tension at the calcaneal insertion and the plantar fascia, which may exacerbate plantar heel pain [21]. Dry needling of muscles is associated with the foot and leg, which is suggested to improve the symptoms of plantar fasciitis [10]. Therefore, TrPs dry needling, an aggressive method, has recently been widely used as a superseded procedure for plantar fasciitis [27]. In this method, a filiform metal needle is inserted into the trigger point without the introduction of any substance. Dry needling may be combined with electrical current [28]. Dry needling produces pain-relieving effects near the trigger point by activating the descending inhibitory pathway of the central nervous system [29]. Several studies evaluated the impact of TrPs dry needling in the treatment of heel pain [13, 22, 29-31]. One of the visible diagnostic criteria in chronic plantar fasciitis is the increased thickness and hypoechogenicity using ultrasonography [31]. Plantar fascia thickness is measured as a differential sign, before and after treatment, and suggested as a suitable indicator for an acceptable response to non-surgical treatment of plantar fasciitis [32]. No study was found that checked the effect of intrinsic plantar muscles dry needling on plantar fascia thickness change by ultrasound evaluation to prove the usefulness of dry needling method. Therefore, we decided to peruse the effect of dry needling on pain and thickness change of the plantar fascia in subjects with plantar fasciitis using ultrasound imaging.
Materials and Methods
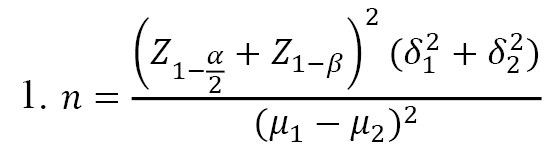
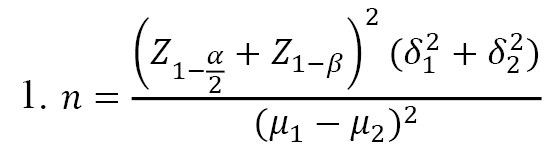
Forty volunteers with plantar fasciitis participated in this study using non-probability convenient sampling. The inclusion criteria of the study included the following: Age over 18 [22, 31], pain on the first step in the morning, pain lasted more than one month [22], and pain level on the visual analog scale (VAS) scale was at least 4 [22]. The exclusion criteria of the study included diabetes and rheumatology diseases [22], fear of needles [22], pregnancy [10, 22], presence of trigger points and muscle shortening in gastrocnemius and hamstring muscles, infection, neuropathy, and coagulation disorders [20], history of injection in the last 6 months [10, 22], and history of cardiovascular diseases [13]. The research was a clinical trial with single-blind randomization and received approval from the University’s Ethics Committee. As for the dependent variable of plantar fascia thickness changes, based on the article by Mahowald and Grady [7], a Mean±SD thickness reduction of 0.82±1.04 mm was reported. Based on this effect size and the application of the sample size formula to compare the means in two balanced groups, taking into account the α was 0.05 and the statistical power of 80%, the final sample size was calculated by the following formula (Equation 1).
The sampling method in this study was convenient sampling. The allocation of samples (into two groups) was done randomly using the stratified permuted block randomization method with 5 blocks of 8 assigned to two groups. The order of interventions A and B in blocks numbered 1 to 5 was determined by the design methodological advisor and provided to the project executive supervisor. The researcher asked the executive supervisor to attribute each eligible person and to avoid possible bias. He was getting an assignment. The executive supervisor first selected the block using a random number generator, and then eligible individuals were assigned to one of two groups, A or B, in a predetermined order. Note that if a block was selected based on random numbers already filling all 8 sequences, another random number was selected for that individual.
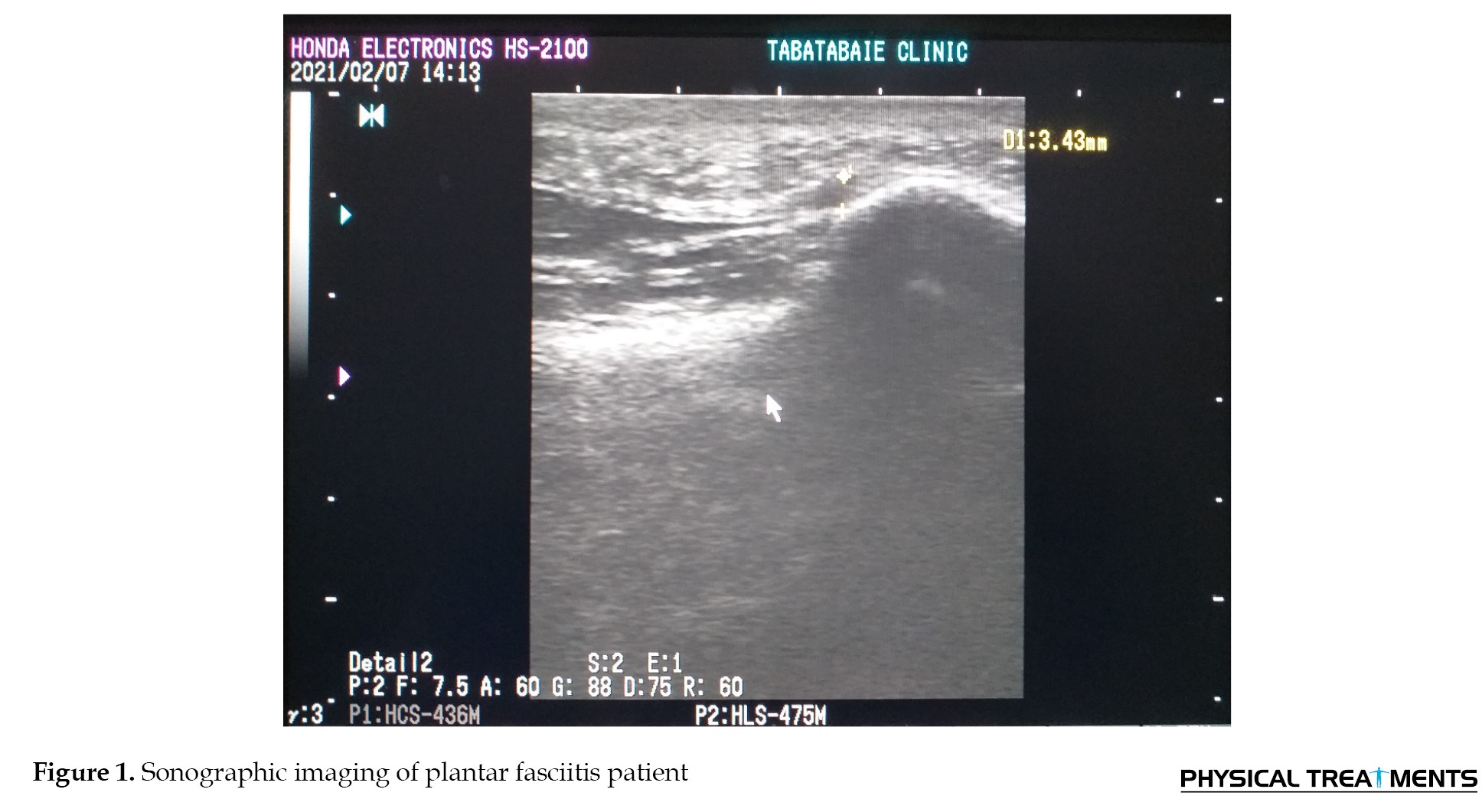
At the beginning of the study, the subjects read and signed the consent form. Based on the list prepared before the study, a physiotherapist evaluated and treated the individuals who met the criteria. First, the plantar fascia thickness was measured with ultrasound, and the pain level was calculated based on the VAS before intervention in both intervention and control groups. Participants in both groups performed plantar fascia massage and stretch for 2 weeks. To stretch the plantar fascia, the patient was instructed to first sit on a chair, place the affected foot on the contralateral knee, and then apply force distal to the metatarsophalangeal joints with his/her hand and pull them upwards until stretch was felt in the soles of the feet. The participants held the stretch for 10 seconds and repeated it 10 times. Participants were instructed to repeat plantar fascia stretch exercises thrice daily [33]. To massage the plantar fascia, the patient should sit in a chair and place one foot on a small tennis ball or water bottle with a sturdy surface, then gently move the ball or bottle back and forth under their foot for 1-3 minutes, thrice daily [34]. In addition to exercise therapy, quadratus plantae trigger points dry needling was performed twice a week in the intervention group for 2 weeks. After 2 weeks, plantar fascia thickness and VAS were assessed in both groups again. An ultrasound (model HS2100 made in Japan with a frequency of 7.5 MHz and a linear probe of 4.5 cm) was used to measure plantar fascia thickness (Figure 1). The patient was lying on a bed in a prone position, knees completely straight and ankles in 90 degrees of flexion. The ultrasound transducer was positioned in the sagittal plane over the medial band of the plantar fascia, 5 mm beneath where the plantar fascia attaches to the medial tuberosity of the calcaneus. Then, the plantar fascia thickness was assessed [35]. A needle with a length of 50 mm and a diameter of 0.3 mm was used to apply quadratus plantae dry needling. The patient was placed in the prone position, and ankles were free from the end of the bed. The physiotherapist sat on the chair facing the patient’s leg. The patient’s leg was held firmly to prevent sudden movements. First, the muscle trigger point was palpated, and then the needle was inserted directly, from the inside or outside, just under the calcaneus bone [35]. The VAS is a straight line measuring 100 mm, marked with “no pain” at one end and “worst pain imaginable” at the opposite end [36]. This ruler has two scales, qualitative and quantitative. The patient marks his or her pain intensity with a vertical line on the qualitative side, then the examiner turns the ruler and reports the marked location numerically [37].
Statistical analyses were conducted using SPSS software version 22. The Shapiro-Wilk test was used to check the normality. The independent t-test was used to evaluate the difference between independent groups, and paired t-test to assess the difference between dependent groups. The significance level was considered 0.05 in all tests.
Results
Demographic characteristics of the patients in both groups are listed in Table 1.
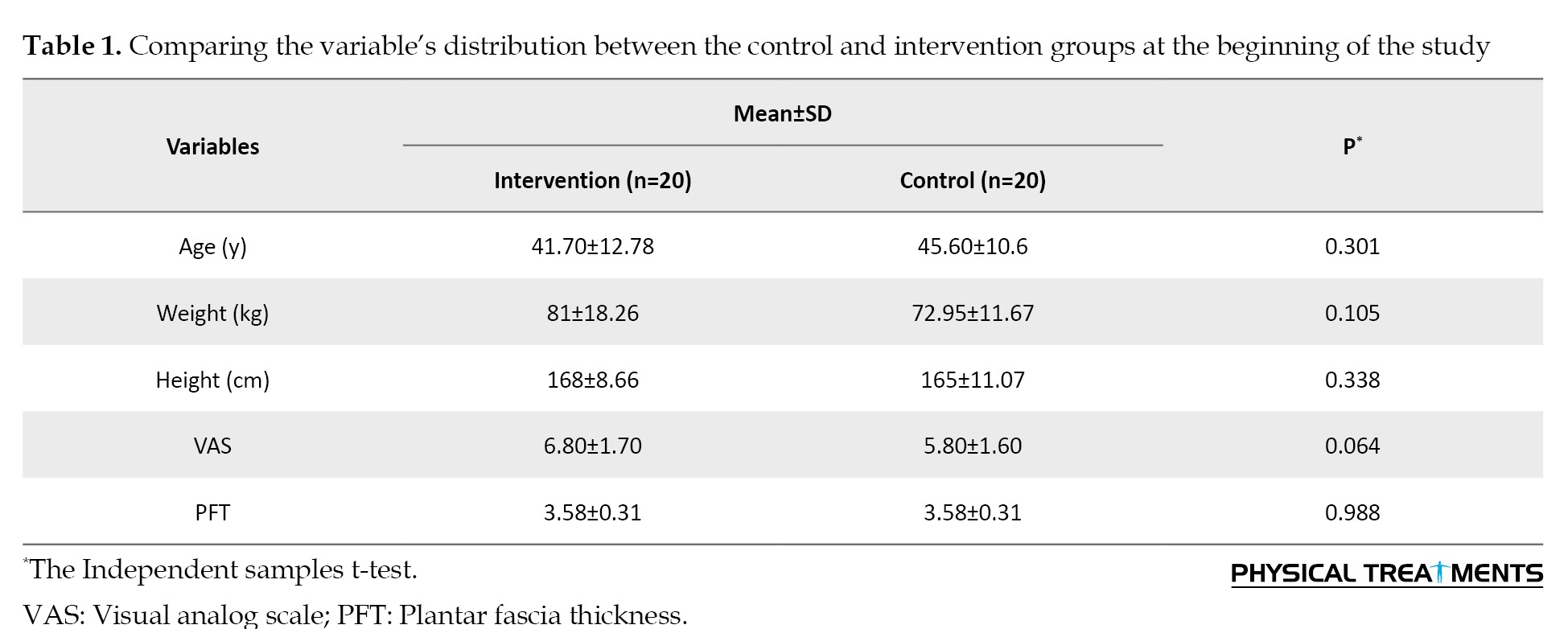
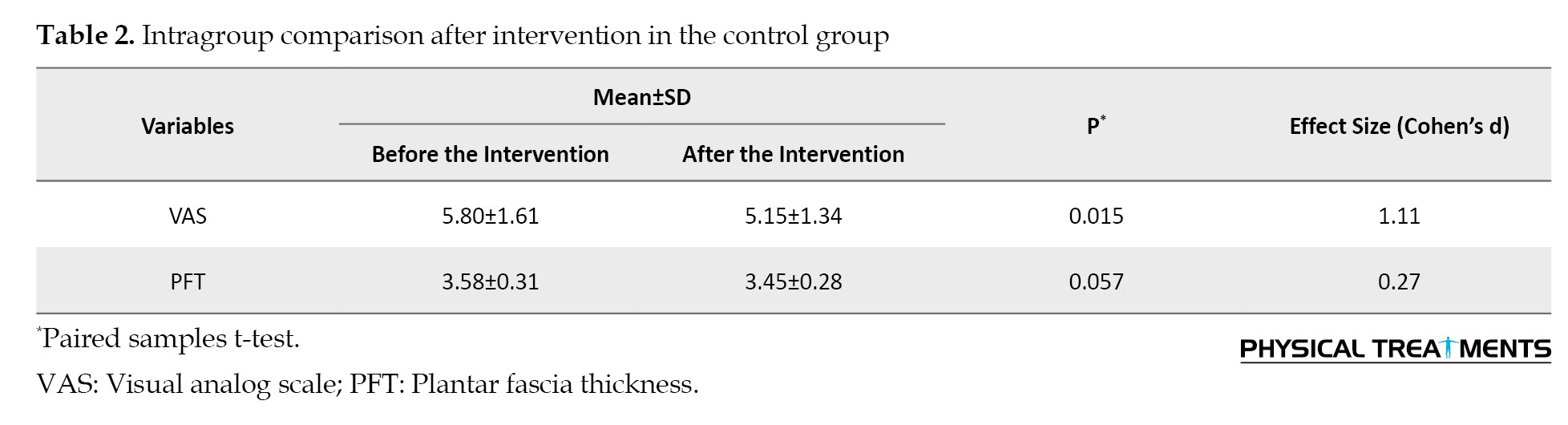
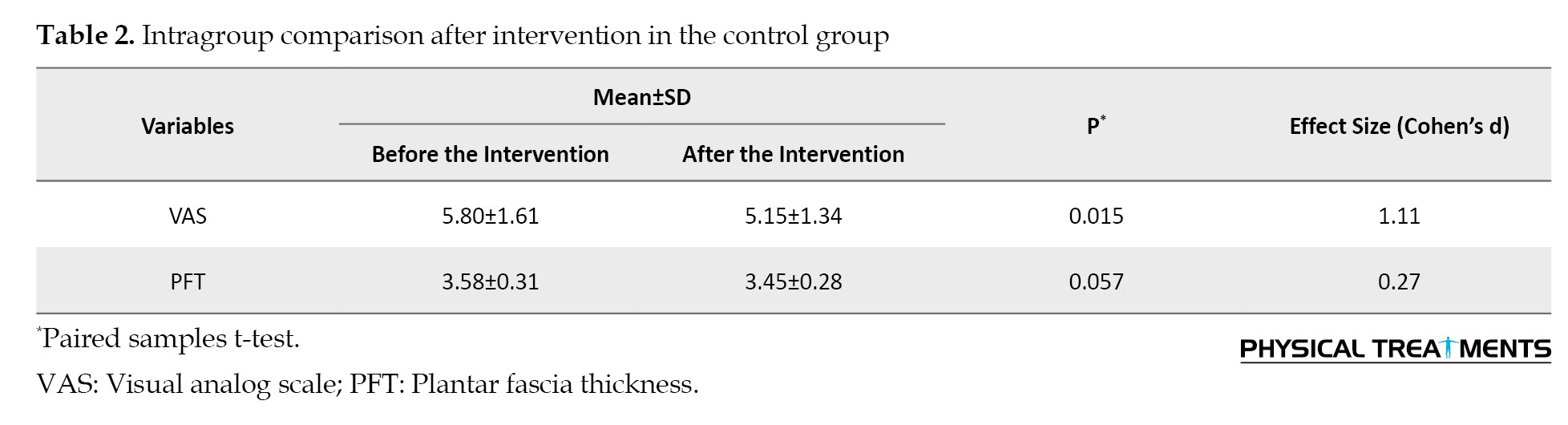
The intervention and control groups did not show any significant difference at baseline. The results indicated that both groups exhibited a normal distribution of variables. In the control group, the results showed that a decrease in the VAS scale after therapeutic exercise was statistically significant (P=0.015). Still, there was no notable reduction in the thickness of the plantar fascia (Table 2).
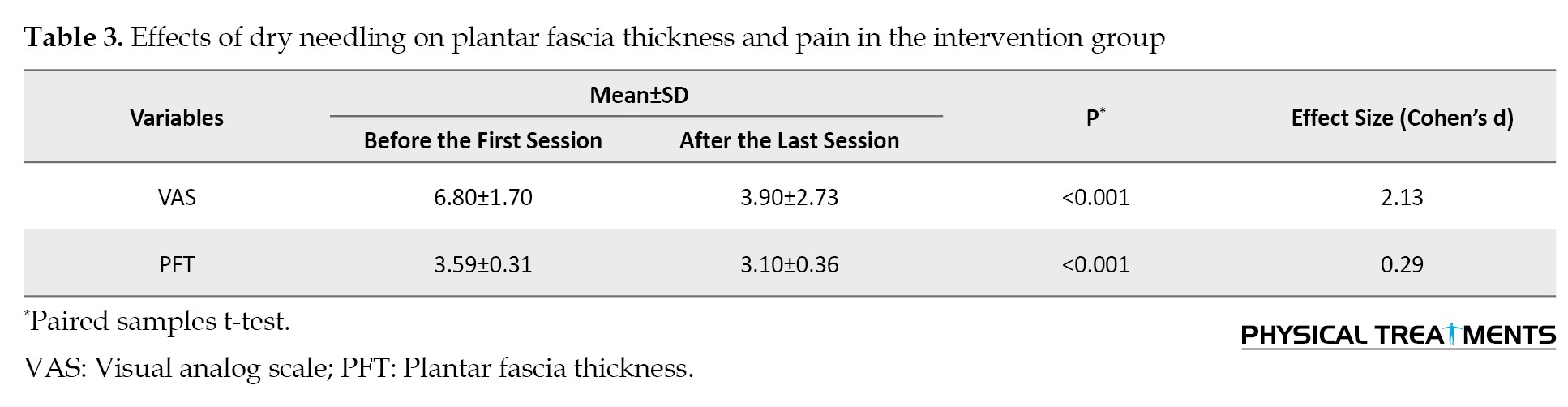
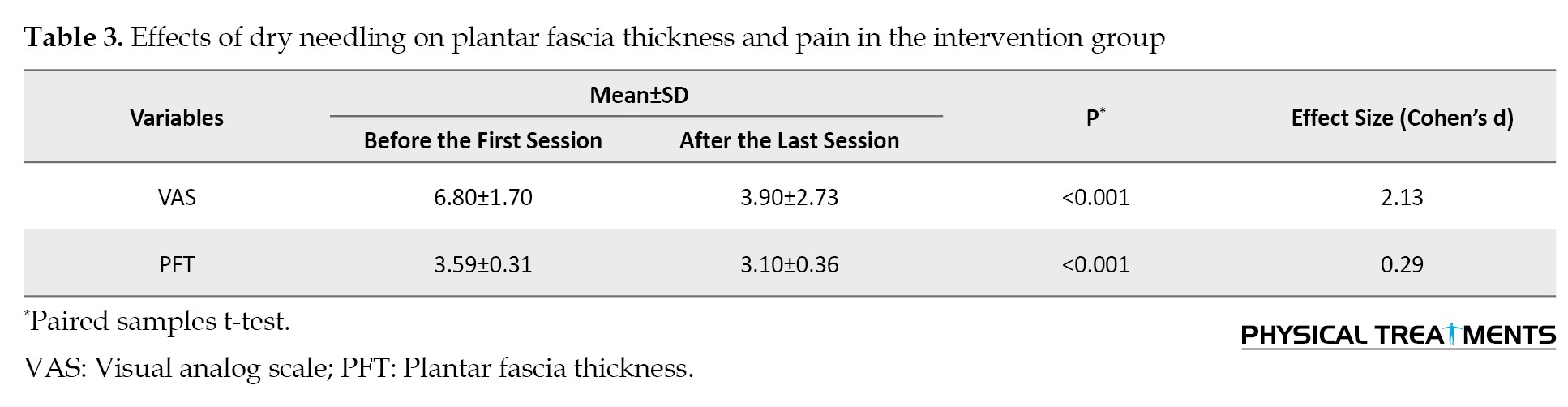
According to Table 3, plantar fascia thickness and VAS scale following dry needling significantly decreased statistically after 2 weeks.
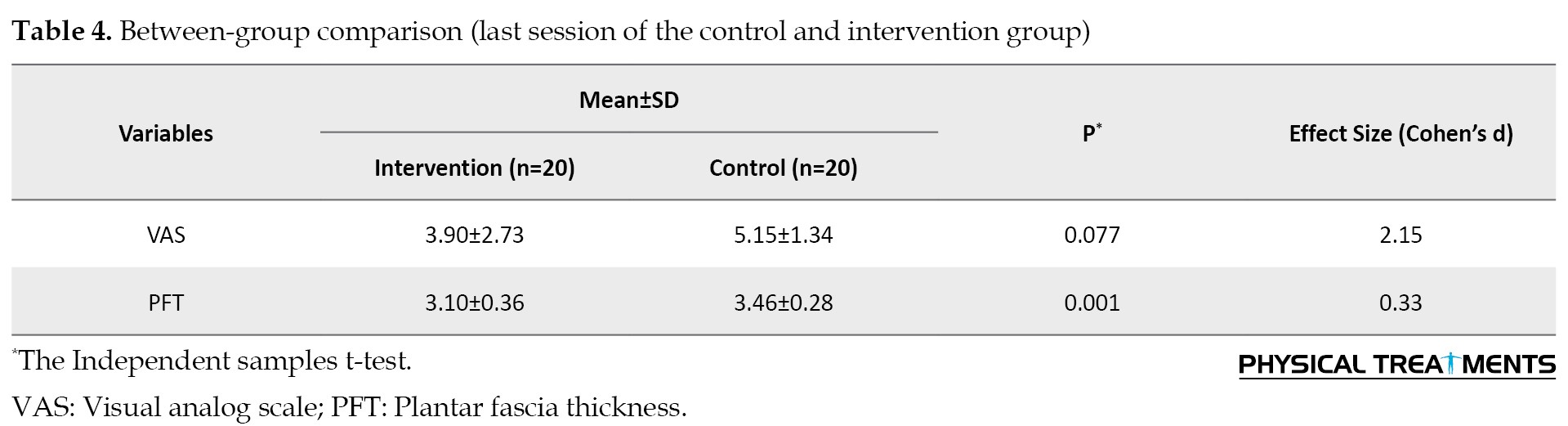
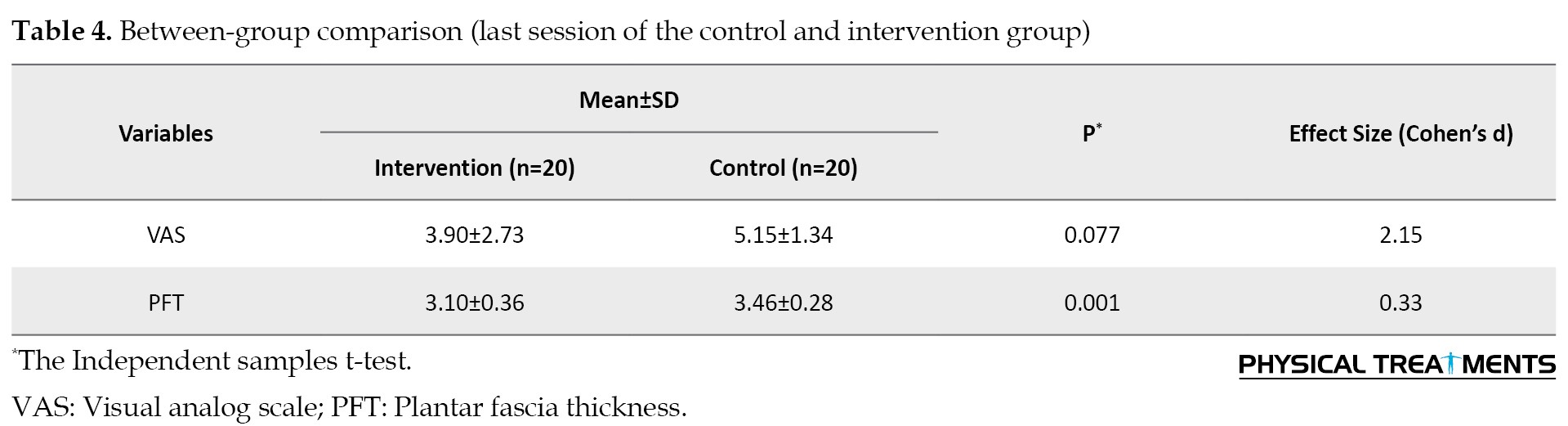
There was no significant difference between the two groups in plantar fascia thickness (P=0.988) and VAS scale (P=0.064) at the beginning of the study (Table 2). The results showed that at the end of the study, there was no significant difference (P=0.077) in the VAS scale between the two groups. Still, the two groups had a significant difference (P=0.001) in plantar fascia thickness (Table 4).
Discussion
This research aimed to examine how dry needling of the quadratus plantae muscle impacts the thickness of the plantar fascia and the level of pain experienced by individuals with plantar fasciitis. Data statistical analysis showed no statistical difference between the two groups regarding primary and background variables. Intra-group comparison in intervention and control groups showed that VAS significantly decreased after dry needling and therapeutic exercise. Additionally, the comparison within the intervention group indicated a marked reduction in plantar fascia thickness following the two weeks. However, there was no notable variation in the thickness of the plantar fascia when compared with the control group after 2 weeks of treatment. In between groups, no significant difference was seen in VAS after 2 weeks of treatment. Still, a significant decrease in plantar fascia thickness following dry needling was obtained compared to the control group.
Visual analog scale (VAS)
Intra-group comparison in both groups showed a significant decrease in VAS, so results showed that therapeutic exercise and dry needling effectively improved pain caused by plantar fasciitis. No significant difference was seen in the VAS between-group comparisons after 2 weeks of treatment. This result can be due to the positive effect of massaging and stretching plantar fascia in flexibility improvement, increasing circulation, and reducing the subsequent pain [33]. On the other hand, it shows that massage and stretch of plantar fascia are as effective as dry needling in improving pain. Although today, dry needling of trigger points is widely used to manage all types of myofascial pain syndromes caused by overstimulated points in skeletal muscle [38], the results of the studies are contradictory. A systematic review found that dry needling was not significantly superior to placebo in musculoskeletal pain control. This review only included four clinical studies. The studies had a small sample size and low quality, and their data sets showed significant statistical heterogeneity, making it difficult to draw definitive conclusions [39]. Conversely, Tough and White investigated the impact of dry needling of trigger points in a review study including 6 clinical trial studies. The patient population was diverse and included trapezius muscle pain, gluteal muscle trigger points, chronic neck pain, and chronic back pain. Analysis of the results of this review study showed that dry needling of trigger points is effective in pain reduction [40]. Only a few studies have been conducted on the effectiveness of dry needling in treating heel pain [10, 13, 22]. Cotchett et al. investigated the effect of a 6-week dry needling treatment on pain based on the VAS scale and the foot health status questionnaire. A statistically significant enhancement in plantar heel discomfort was observed, although caution was advised regarding potential unwanted side effects [20]. In a case report study, Akhbari et al. investigated the effect of a 2-week dry needling treatment on plantar fasciitis, which reported a 60%-70% reduction in pain [13]. In the study of Eftekharsadat following dry needling treatment of trigger points in the gastrocnemius and soleus muscles, pain reduction was obtained based on the VAS scale [22]. These studies are limited due to some implementation limitations that reduced the quality. One of these studies was a case report where only one patient was treated with dry needling [13]. Two studies lacked a control group to compare the effect of the intervention (dry needling). It is challenging to accurately analyze the absolute impact of dry needling due to the absence of a control group [10, 22]. In Eftekharsadat’s study, pain improvement after dry needling was assessed in the intervention group and compared to the control group, which is inconsistent with the present study. The control group in both studies performed plantar fascia massage and stretch. The different results of these two studies could be due to the different target muscles. On the other hand, the duration of treatment in Eftekharsadat’s study was 4 weeks, and in the present study, it was 2 weeks [22]. The purpose of the studies was different when studying the impact of dry needling on alleviating symptoms of plantar fasciitis. In two studies, the myofascial pathway of the lower limb, such as the gluteal, hamstring, gastrocnemius, and soleus muscles, was treated [20]. In another study, TrP dry needling was performed on gastrocnemius and soleus muscles [22]. Meanwhile, according to the Delphi study, quadratus plantae is the main muscle for dry needling technique in patients with plantar fasciitis treated in the present study [41]. The main belief about trigger points is that they are caused by excessive release of acetylcholine from motor end plates. Long-term release of acetylcholine leads to chronic shortening and contraction of sarcomeres, and reduced blood circulation leads to hypoxia and local ischemia [42]. The secretion of prostaglandins, bradykinins, cytokines, and histamine occurs as a consequence, sensitizing muscle afferent sensory nerve fibers, which may be associated with trigger point sensitivity. These chemicals lead to central sensitization of posterior horn neurons [43]. The exact mechanism of the effect of dry needling is not completely clear. Still, some studies showed that dry needling modulates the biochemical environment around trigger points and mediators that cause pain [27]. On the other hand, dry needling reduces local sensory signals [44]. Another hypothesis suggests that dry needling activates inhibitory interneurons and disrupts the transmission of the normal pain message to the sensory cortex [45]. Also, reduction of tissue blood supply and hypoxia is one of the causes of trigger points, so any treatment that increases blood circulation reduces the effects of metabolites and pain [46]. Cagnie and Shah reported that following TrPs dry needling blood circulation and oxygen increased [47, 48]. According to the mentioned reasons, the reduction of pain following dry needling in the intervention group can be justified.
Plantar fascia thickness
In the intra-group comparison, plantar fascia thickness decreased significantly in the intervention group after 2 weeks of treatment, and the difference obtained was more than the minimal detectable change (MDC), which is clinically significant. On the other hand, there was no significant difference in plantar fascia thickness in the control group after 2 weeks of treatment. The between-group comparison showed that the decrease in the plantar fascia thickness after dry needling is statistically significant compared to the control group, and the difference obtained is outside the MDC range and is clinically significant. Findings related to plantar fascia thickness show that dry needling of the quadratus plantae muscle effectively reduces the plantar fascia thickness as one of the diagnostic criteria for plantar fasciitis. Several studies investigated plantar fascia thickness in people with plantar fasciitis; these studies show that plantar fascia thickness increases significantly in these people [11, 14, 29, 31, 44, 49]. Therefore, increasing the plantar fascia thickness is a reliable diagnostic criterion in plantar fasciitis patients. In a study similar to the present research, Mahowald et al. examined the relationship between plantar fascia thickness changes and pain reduction in patients with plantar fasciitis. This study reveals a significant relationship between pain reduction based on the VAS scale and the reduction of plantar fascia thickness, so in 74.4% of the involved feet, the reduction of the plantar fascia thickness was associated with the reduction in pain [7]. In the present study, pain reduction following dry needling was associated with a significant reduction in plantar fascia thickness, which aligns with Mahowald’s study. However, in the control group, after 2 weeks of treatment, the significant reduction in the VAS scale was not accompanied by a significant decrease in the plantar fascia thickness. This contradiction can be due to the difference in the type of treatment used. In Mahowald’s study, patients with plantar fasciitis underwent various treatments, including cold therapy, corticosteroid injection under ultrasound guidance, custom-made shoes (modifying shoes), and muscle stretching. The results of the study by Lao also showed that the pressure pain threshold is significantly lower and plantar fascia thickness is greater than that in people with plantar fasciitis compared to the control group [50].
Puentedura investigated the effect of dry needling of the multifidus muscles in the chronic back. He showed that dry needling decreased the thickness of the muscle at resting position and increased the thickness of the muscle during maximum concentric contraction. The mechanism of this effect is not completely clear, but mechanical and neural theories are proposed [51]. The mechanical effects include the breaking of the contraction in the trigger point, the local stretching of the contractile structures of the cell, and the reduction of the actin and myosin filament overlap. The potential neural effects include the reduction of metabolic mediators, the reduction of the peripheral pain threshold, and the activation of the central inhibitory mechanisms of the descending pathways. The increase in muscle thickness during maximum concentric contraction is due to the increase in neuromuscular control following dry needling, and the decrease in resting thickness can be considered a result of inhibiting muscle over-activity. It seems that dry needling causes more muscle relaxation during resting position and decreases thickness by activating the descending inhibitory pathway. Relaxation increases the thickness and strength of the muscle during contraction [52]. The plantar fascia stretches from the medial tubercle of the calcaneus to the proximal interphalangeal joints. As a connective tissue layer, it significantly contributes to the transfer of forces from muscles and the Achilles tendon [53]. Quadratus plantaris originates from the medial and lateral aspect of the calcaneus bone and extends to the front of the sole to the flexor digitorum longus muscle [54]. Also, based on Simmons’ suggestion, the existence of trigger points in the muscles of the plantar region and near the foot can significantly contribute to heel pain [30].
Conclusion
Dry needling of the quadratus plantaris muscle trigger points can effectively affect the plantar fasciitis. Patients should be followed up after the treatment to check the long-term effects of dry needling in future studies. Also, studies involving larger groups of participants could be conducted to validate these results.
Ethical Considerations
Compliance with ethical guidelines
This research was a clinical trial (IRCT20160424027562N10) that has been approved by the Ethics Committee of the Semnan University of Medical Sciences (Code: IR.SEMUMS.REC.1399.244).
Funding
The present article was extracted from the master’s thesis of Zeinab Mahmoodi, approved by Semnan University of Medical Sciences, Semnan Iran.
Authors' contributions
Data collection and Writing–original draft: Zeinab Mahmoodi; Development the initial idea and protocol: Roghayeh Mohammadi; Data analysis: Fatemeh Paknazar; Review of the manuscript: Roghayeh Mohammadi and Fatemeh Paknazar.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank the Neuromuscular Rehabilitation Research Center of Semnan University of Medical Sciences.
References
Plantar fasciitis is the most common cause of non-traumatic adult heel pain [1] and one of the common causes of pain and disability, which occurs in approximately 10% of the general population throughout their lifetime [2]. Diagnosis is usually based on history, physical evaluation, and the presence of pain on the inner side of the heel [3]. Plantar fasciitis has a gradual onset and often worsens after a few weeks or months [4]. It is associated with persistent, knifelike pain [5] in the bottom of the foot near the heel. The pain usually occurs in the early morning on the first step after immobility [5], and heel tenderness was also reported [6]. Plantar fasciitis is associated with obesity (body mass index [BMI] over 30), variations in physical activity level, prolonged periods of standing, alteration in foot arch [7], sedentary lifestyle [8], and calf muscle shortness [9]. Even though heel pain is quite common and significantly impacts quality of life (QoL), there is no optimal treatment [10]. Several treatments are recommended for plantar fasciitis [11]. In the initial stage, conservative treatments, including rest, custom-made insoles (orthotic insoles), night splints, and stretching exercises, are widely used to relieve symptoms [12]. Manual treatments, including joint and soft tissue mobilization, manual stretching of calf muscles, the release of trigger points [13], and nerve mobilization techniques [14], can be effective on plantar fasciitis. Drug therapy, platelet-enriched plasma treatment [15], shockwave therapy [16], botulism toxin, ultrasound, tapping techniques [11, 17] and low level laser therapy [18] are suggested for plantar fasciitis. Travell and Simons proposed that trigger points (TrPs) in the intrinsic muscles of the foot and surrounding muscles can significantly contribute to heel pain [19]. Some studies reported trigger points of soleus [20], gastrocnemius [13, 20-22], posterior tibialis [23], popliteal [23], abductor halluces [20, 21, 24], flexor halluces [21], peroneus longus [23], flexor digitorum brevis [20, 24], and quadratus plantaris muscles [20, 21] in patients with heel pain. Quadratus plantae has proximal anatomic attachment sites and mechanical function with the plantar fascia [24]. Several studies mentioned the role of the quadratus plantae muscle in the pathogenesis of heel pain [25]. The lateral plantar nerve contains sensory fibers that serve the calcaneal periosteum, the plantar ligament, the medial head of the quadratus plantae, and motor fibers that innervate the quadratus plantae muscle. Consequently, if the lateral plantar nerve gets trapped between the two heads of the quadratus plantae muscle, it can lead to heel pain [26]. The quadratus plantae and flexor hallucis brevis contain several active trigger points in individuals experiencing plantar heel pain. Since both muscles are anatomically and intrinsically linked to the plantar fascia, the taut bands associated with their trigger points can create tension at the calcaneal insertion and the plantar fascia, which may exacerbate plantar heel pain [21]. Dry needling of muscles is associated with the foot and leg, which is suggested to improve the symptoms of plantar fasciitis [10]. Therefore, TrPs dry needling, an aggressive method, has recently been widely used as a superseded procedure for plantar fasciitis [27]. In this method, a filiform metal needle is inserted into the trigger point without the introduction of any substance. Dry needling may be combined with electrical current [28]. Dry needling produces pain-relieving effects near the trigger point by activating the descending inhibitory pathway of the central nervous system [29]. Several studies evaluated the impact of TrPs dry needling in the treatment of heel pain [13, 22, 29-31]. One of the visible diagnostic criteria in chronic plantar fasciitis is the increased thickness and hypoechogenicity using ultrasonography [31]. Plantar fascia thickness is measured as a differential sign, before and after treatment, and suggested as a suitable indicator for an acceptable response to non-surgical treatment of plantar fasciitis [32]. No study was found that checked the effect of intrinsic plantar muscles dry needling on plantar fascia thickness change by ultrasound evaluation to prove the usefulness of dry needling method. Therefore, we decided to peruse the effect of dry needling on pain and thickness change of the plantar fascia in subjects with plantar fasciitis using ultrasound imaging.
Materials and Methods
Forty volunteers with plantar fasciitis participated in this study using non-probability convenient sampling. The inclusion criteria of the study included the following: Age over 18 [22, 31], pain on the first step in the morning, pain lasted more than one month [22], and pain level on the visual analog scale (VAS) scale was at least 4 [22]. The exclusion criteria of the study included diabetes and rheumatology diseases [22], fear of needles [22], pregnancy [10, 22], presence of trigger points and muscle shortening in gastrocnemius and hamstring muscles, infection, neuropathy, and coagulation disorders [20], history of injection in the last 6 months [10, 22], and history of cardiovascular diseases [13]. The research was a clinical trial with single-blind randomization and received approval from the University’s Ethics Committee. As for the dependent variable of plantar fascia thickness changes, based on the article by Mahowald and Grady [7], a Mean±SD thickness reduction of 0.82±1.04 mm was reported. Based on this effect size and the application of the sample size formula to compare the means in two balanced groups, taking into account the α was 0.05 and the statistical power of 80%, the final sample size was calculated by the following formula (Equation 1).
The sampling method in this study was convenient sampling. The allocation of samples (into two groups) was done randomly using the stratified permuted block randomization method with 5 blocks of 8 assigned to two groups. The order of interventions A and B in blocks numbered 1 to 5 was determined by the design methodological advisor and provided to the project executive supervisor. The researcher asked the executive supervisor to attribute each eligible person and to avoid possible bias. He was getting an assignment. The executive supervisor first selected the block using a random number generator, and then eligible individuals were assigned to one of two groups, A or B, in a predetermined order. Note that if a block was selected based on random numbers already filling all 8 sequences, another random number was selected for that individual.
At the beginning of the study, the subjects read and signed the consent form. Based on the list prepared before the study, a physiotherapist evaluated and treated the individuals who met the criteria. First, the plantar fascia thickness was measured with ultrasound, and the pain level was calculated based on the VAS before intervention in both intervention and control groups. Participants in both groups performed plantar fascia massage and stretch for 2 weeks. To stretch the plantar fascia, the patient was instructed to first sit on a chair, place the affected foot on the contralateral knee, and then apply force distal to the metatarsophalangeal joints with his/her hand and pull them upwards until stretch was felt in the soles of the feet. The participants held the stretch for 10 seconds and repeated it 10 times. Participants were instructed to repeat plantar fascia stretch exercises thrice daily [33]. To massage the plantar fascia, the patient should sit in a chair and place one foot on a small tennis ball or water bottle with a sturdy surface, then gently move the ball or bottle back and forth under their foot for 1-3 minutes, thrice daily [34]. In addition to exercise therapy, quadratus plantae trigger points dry needling was performed twice a week in the intervention group for 2 weeks. After 2 weeks, plantar fascia thickness and VAS were assessed in both groups again. An ultrasound (model HS2100 made in Japan with a frequency of 7.5 MHz and a linear probe of 4.5 cm) was used to measure plantar fascia thickness (Figure 1). The patient was lying on a bed in a prone position, knees completely straight and ankles in 90 degrees of flexion. The ultrasound transducer was positioned in the sagittal plane over the medial band of the plantar fascia, 5 mm beneath where the plantar fascia attaches to the medial tuberosity of the calcaneus. Then, the plantar fascia thickness was assessed [35]. A needle with a length of 50 mm and a diameter of 0.3 mm was used to apply quadratus plantae dry needling. The patient was placed in the prone position, and ankles were free from the end of the bed. The physiotherapist sat on the chair facing the patient’s leg. The patient’s leg was held firmly to prevent sudden movements. First, the muscle trigger point was palpated, and then the needle was inserted directly, from the inside or outside, just under the calcaneus bone [35]. The VAS is a straight line measuring 100 mm, marked with “no pain” at one end and “worst pain imaginable” at the opposite end [36]. This ruler has two scales, qualitative and quantitative. The patient marks his or her pain intensity with a vertical line on the qualitative side, then the examiner turns the ruler and reports the marked location numerically [37].
Statistical analyses were conducted using SPSS software version 22. The Shapiro-Wilk test was used to check the normality. The independent t-test was used to evaluate the difference between independent groups, and paired t-test to assess the difference between dependent groups. The significance level was considered 0.05 in all tests.
Results
Demographic characteristics of the patients in both groups are listed in Table 1.
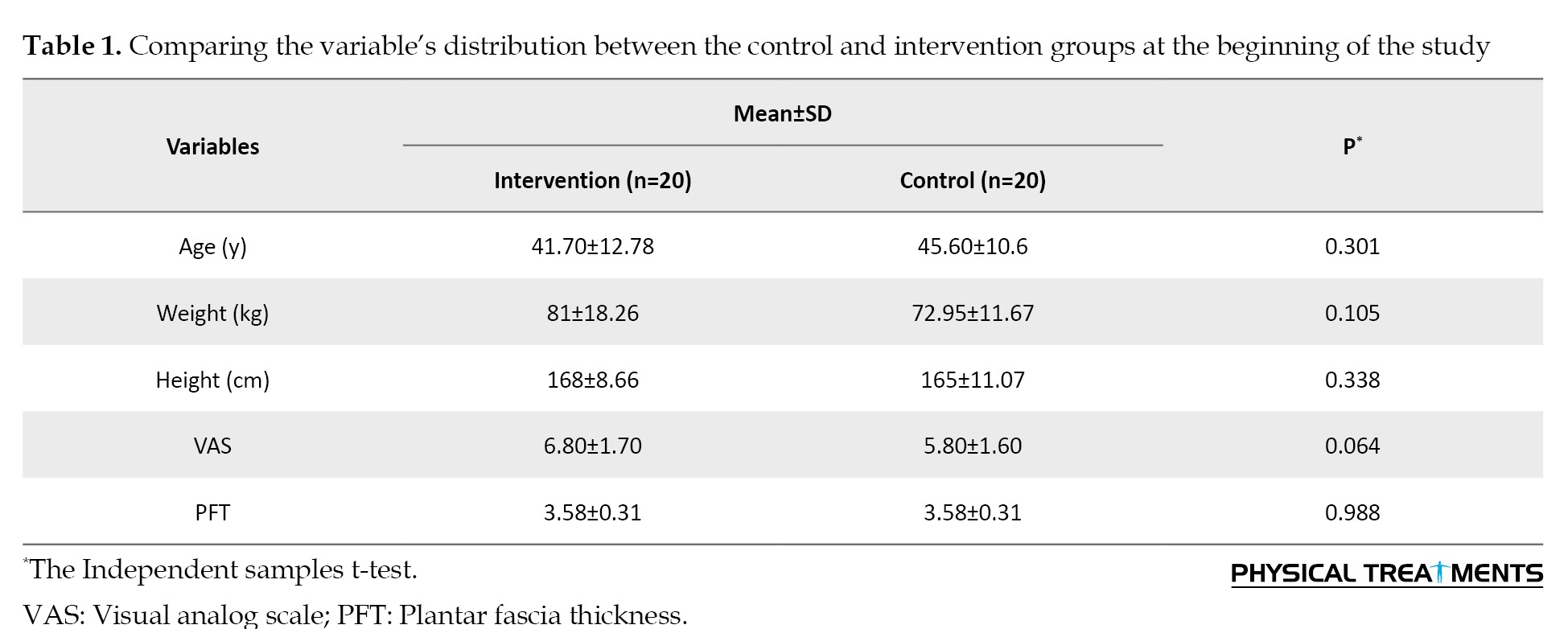
The intervention and control groups did not show any significant difference at baseline. The results indicated that both groups exhibited a normal distribution of variables. In the control group, the results showed that a decrease in the VAS scale after therapeutic exercise was statistically significant (P=0.015). Still, there was no notable reduction in the thickness of the plantar fascia (Table 2).
According to Table 3, plantar fascia thickness and VAS scale following dry needling significantly decreased statistically after 2 weeks.
There was no significant difference between the two groups in plantar fascia thickness (P=0.988) and VAS scale (P=0.064) at the beginning of the study (Table 2). The results showed that at the end of the study, there was no significant difference (P=0.077) in the VAS scale between the two groups. Still, the two groups had a significant difference (P=0.001) in plantar fascia thickness (Table 4).
Discussion
This research aimed to examine how dry needling of the quadratus plantae muscle impacts the thickness of the plantar fascia and the level of pain experienced by individuals with plantar fasciitis. Data statistical analysis showed no statistical difference between the two groups regarding primary and background variables. Intra-group comparison in intervention and control groups showed that VAS significantly decreased after dry needling and therapeutic exercise. Additionally, the comparison within the intervention group indicated a marked reduction in plantar fascia thickness following the two weeks. However, there was no notable variation in the thickness of the plantar fascia when compared with the control group after 2 weeks of treatment. In between groups, no significant difference was seen in VAS after 2 weeks of treatment. Still, a significant decrease in plantar fascia thickness following dry needling was obtained compared to the control group.
Visual analog scale (VAS)
Intra-group comparison in both groups showed a significant decrease in VAS, so results showed that therapeutic exercise and dry needling effectively improved pain caused by plantar fasciitis. No significant difference was seen in the VAS between-group comparisons after 2 weeks of treatment. This result can be due to the positive effect of massaging and stretching plantar fascia in flexibility improvement, increasing circulation, and reducing the subsequent pain [33]. On the other hand, it shows that massage and stretch of plantar fascia are as effective as dry needling in improving pain. Although today, dry needling of trigger points is widely used to manage all types of myofascial pain syndromes caused by overstimulated points in skeletal muscle [38], the results of the studies are contradictory. A systematic review found that dry needling was not significantly superior to placebo in musculoskeletal pain control. This review only included four clinical studies. The studies had a small sample size and low quality, and their data sets showed significant statistical heterogeneity, making it difficult to draw definitive conclusions [39]. Conversely, Tough and White investigated the impact of dry needling of trigger points in a review study including 6 clinical trial studies. The patient population was diverse and included trapezius muscle pain, gluteal muscle trigger points, chronic neck pain, and chronic back pain. Analysis of the results of this review study showed that dry needling of trigger points is effective in pain reduction [40]. Only a few studies have been conducted on the effectiveness of dry needling in treating heel pain [10, 13, 22]. Cotchett et al. investigated the effect of a 6-week dry needling treatment on pain based on the VAS scale and the foot health status questionnaire. A statistically significant enhancement in plantar heel discomfort was observed, although caution was advised regarding potential unwanted side effects [20]. In a case report study, Akhbari et al. investigated the effect of a 2-week dry needling treatment on plantar fasciitis, which reported a 60%-70% reduction in pain [13]. In the study of Eftekharsadat following dry needling treatment of trigger points in the gastrocnemius and soleus muscles, pain reduction was obtained based on the VAS scale [22]. These studies are limited due to some implementation limitations that reduced the quality. One of these studies was a case report where only one patient was treated with dry needling [13]. Two studies lacked a control group to compare the effect of the intervention (dry needling). It is challenging to accurately analyze the absolute impact of dry needling due to the absence of a control group [10, 22]. In Eftekharsadat’s study, pain improvement after dry needling was assessed in the intervention group and compared to the control group, which is inconsistent with the present study. The control group in both studies performed plantar fascia massage and stretch. The different results of these two studies could be due to the different target muscles. On the other hand, the duration of treatment in Eftekharsadat’s study was 4 weeks, and in the present study, it was 2 weeks [22]. The purpose of the studies was different when studying the impact of dry needling on alleviating symptoms of plantar fasciitis. In two studies, the myofascial pathway of the lower limb, such as the gluteal, hamstring, gastrocnemius, and soleus muscles, was treated [20]. In another study, TrP dry needling was performed on gastrocnemius and soleus muscles [22]. Meanwhile, according to the Delphi study, quadratus plantae is the main muscle for dry needling technique in patients with plantar fasciitis treated in the present study [41]. The main belief about trigger points is that they are caused by excessive release of acetylcholine from motor end plates. Long-term release of acetylcholine leads to chronic shortening and contraction of sarcomeres, and reduced blood circulation leads to hypoxia and local ischemia [42]. The secretion of prostaglandins, bradykinins, cytokines, and histamine occurs as a consequence, sensitizing muscle afferent sensory nerve fibers, which may be associated with trigger point sensitivity. These chemicals lead to central sensitization of posterior horn neurons [43]. The exact mechanism of the effect of dry needling is not completely clear. Still, some studies showed that dry needling modulates the biochemical environment around trigger points and mediators that cause pain [27]. On the other hand, dry needling reduces local sensory signals [44]. Another hypothesis suggests that dry needling activates inhibitory interneurons and disrupts the transmission of the normal pain message to the sensory cortex [45]. Also, reduction of tissue blood supply and hypoxia is one of the causes of trigger points, so any treatment that increases blood circulation reduces the effects of metabolites and pain [46]. Cagnie and Shah reported that following TrPs dry needling blood circulation and oxygen increased [47, 48]. According to the mentioned reasons, the reduction of pain following dry needling in the intervention group can be justified.
Plantar fascia thickness
In the intra-group comparison, plantar fascia thickness decreased significantly in the intervention group after 2 weeks of treatment, and the difference obtained was more than the minimal detectable change (MDC), which is clinically significant. On the other hand, there was no significant difference in plantar fascia thickness in the control group after 2 weeks of treatment. The between-group comparison showed that the decrease in the plantar fascia thickness after dry needling is statistically significant compared to the control group, and the difference obtained is outside the MDC range and is clinically significant. Findings related to plantar fascia thickness show that dry needling of the quadratus plantae muscle effectively reduces the plantar fascia thickness as one of the diagnostic criteria for plantar fasciitis. Several studies investigated plantar fascia thickness in people with plantar fasciitis; these studies show that plantar fascia thickness increases significantly in these people [11, 14, 29, 31, 44, 49]. Therefore, increasing the plantar fascia thickness is a reliable diagnostic criterion in plantar fasciitis patients. In a study similar to the present research, Mahowald et al. examined the relationship between plantar fascia thickness changes and pain reduction in patients with plantar fasciitis. This study reveals a significant relationship between pain reduction based on the VAS scale and the reduction of plantar fascia thickness, so in 74.4% of the involved feet, the reduction of the plantar fascia thickness was associated with the reduction in pain [7]. In the present study, pain reduction following dry needling was associated with a significant reduction in plantar fascia thickness, which aligns with Mahowald’s study. However, in the control group, after 2 weeks of treatment, the significant reduction in the VAS scale was not accompanied by a significant decrease in the plantar fascia thickness. This contradiction can be due to the difference in the type of treatment used. In Mahowald’s study, patients with plantar fasciitis underwent various treatments, including cold therapy, corticosteroid injection under ultrasound guidance, custom-made shoes (modifying shoes), and muscle stretching. The results of the study by Lao also showed that the pressure pain threshold is significantly lower and plantar fascia thickness is greater than that in people with plantar fasciitis compared to the control group [50].
Puentedura investigated the effect of dry needling of the multifidus muscles in the chronic back. He showed that dry needling decreased the thickness of the muscle at resting position and increased the thickness of the muscle during maximum concentric contraction. The mechanism of this effect is not completely clear, but mechanical and neural theories are proposed [51]. The mechanical effects include the breaking of the contraction in the trigger point, the local stretching of the contractile structures of the cell, and the reduction of the actin and myosin filament overlap. The potential neural effects include the reduction of metabolic mediators, the reduction of the peripheral pain threshold, and the activation of the central inhibitory mechanisms of the descending pathways. The increase in muscle thickness during maximum concentric contraction is due to the increase in neuromuscular control following dry needling, and the decrease in resting thickness can be considered a result of inhibiting muscle over-activity. It seems that dry needling causes more muscle relaxation during resting position and decreases thickness by activating the descending inhibitory pathway. Relaxation increases the thickness and strength of the muscle during contraction [52]. The plantar fascia stretches from the medial tubercle of the calcaneus to the proximal interphalangeal joints. As a connective tissue layer, it significantly contributes to the transfer of forces from muscles and the Achilles tendon [53]. Quadratus plantaris originates from the medial and lateral aspect of the calcaneus bone and extends to the front of the sole to the flexor digitorum longus muscle [54]. Also, based on Simmons’ suggestion, the existence of trigger points in the muscles of the plantar region and near the foot can significantly contribute to heel pain [30].
Conclusion
Dry needling of the quadratus plantaris muscle trigger points can effectively affect the plantar fasciitis. Patients should be followed up after the treatment to check the long-term effects of dry needling in future studies. Also, studies involving larger groups of participants could be conducted to validate these results.
Ethical Considerations
Compliance with ethical guidelines
This research was a clinical trial (IRCT20160424027562N10) that has been approved by the Ethics Committee of the Semnan University of Medical Sciences (Code: IR.SEMUMS.REC.1399.244).
Funding
The present article was extracted from the master’s thesis of Zeinab Mahmoodi, approved by Semnan University of Medical Sciences, Semnan Iran.
Authors' contributions
Data collection and Writing–original draft: Zeinab Mahmoodi; Development the initial idea and protocol: Roghayeh Mohammadi; Data analysis: Fatemeh Paknazar; Review of the manuscript: Roghayeh Mohammadi and Fatemeh Paknazar.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank the Neuromuscular Rehabilitation Research Center of Semnan University of Medical Sciences.
References
- Wu CH, Chiu YH, Chang KV, Wu WT, Özçakar L. Ultrasound elastography for the evaluation of plantar fasciitis: A systematic review and meta-analysis. European Journal of Radiology. 2022; 155:110495. [DOI:10.1016/j.ejrad.2022.110495] [PMID]
- Al-Siyabi Z, Karam M, Al-Hajri E, Alsaif A, Alazemi M, Aldubaikhi AA. Extracorporeal Shockwave Therapy Versus Ultrasound Therapy for Plantar Fasciitis: A systematic review and Meta-Analysis. Cureus. 2022; 14(1):e20871.[DOI:10.7759/cureus.20871] [PMID]
- Karabay N, Toros T, Hurel C. Ultrasonographic evaluation in plantar fasciitis. The Journal of Foot and Ankle Surgery : Official Publication of the American College of Foot and Ankle Surgeons. 2007; 46(6):442-6. [DOI:10.1053/j.jfas.2007.08.006] [PMID]
- Bartold SJ. The plantar fascia as a source of pain—biomechanics, presentation and treatment. Journal of Bodywork and Movement Therapies. 2004; 8(3):214-26. [DOI:10.1016/S1360-8592(03)00087-1]
- Latt LD, Jaffe DE, Tang Y, Taljanovic MS. Evaluation and Treatment of Chronic Plantar Fasciitis. Foot & Ankle Orthopaedics. 2020; 5(1):2473011419896763.[DOI:10.1177/2473011419896763] [PMID] [PMCID]
- Hoefnagels EM, Weerheijm L, Witteveen AG, Louwerens J-WK, Keijsers N. The effect of lengthening the gastrocnemius muscle in chronic therapy resistant plantar fasciitis. Foot and Ankle Surgery. 2021; 27(5):543-9. [DOI:10.1016/j.fas.2020.07.003] [PMID]
- Mahowald S, Legge BS, Grady JF. The correlation between plantar fascia thickness and symptoms of plantar fasciitis. Journal of the American Podiatric Medical Association. 2011; 101(5):385-9. [DOI:10.7547/1010385] [PMID]
- Alanazi M, Khan R, Muqri A, Alnosaier Z, Dalak M, Alajlani S, et al. Plantar fasciitis in primary care: A review. International Journal of Medicine in Developing Countries. 2022; 6(7):1002-5. [DOI:10.24911/IJMDC.51-1654542136]
- Thummar RC, Rajaseker S, Anumasa R. Association between trigger points in hamstring, posterior leg, foot muscles and plantar fasciopathy: A cross-sectional study. Journal of Bodywork and Movement Therapies. 2020; 24(4):373-8. [DOI:10.1016/j.jbmt.2020.07.018]
- Cotchett MP, Landorf KB, Munteanu SE, Raspovic AM. Consensus for dry needling for plantar heel pain (plantar fasciitis): A modified Delphi study. Acupuncture in Medicine : Journal of the British Medical Acupuncture Society. 2011; 29(3):193-202. [DOI:10.1136/aim.2010.003145] [PMID]
- Uygur E, Aktaş B, Eceviz E, Yilmazoğlu EG, Poyanli O. Preliminary report on the role of dry needling versus corticosteroid injection, an effective treatment method for plantar fasciitis: A randomized controlled trial. The Journal of Foot and Ankle Surgery : Official Publication of the American College of Foot and Ankle Surgeons. 2019; 58(2):301-5. [DOI:10.1053/j.jfas.2018.08.058] [PMID]
- Li H, Lv H, Lin T. Comparison of efficacy of eight treatments for plantar fasciitis: A network meta-analysis. Journal of Cellular Physiology. 2018; 234(1):860-70. [DOI:10.1002/jcp.26907]
- Akhbari B, Salavati M, Ezzati K, Mohammadi Rad S. The use of dry needling and myofascial meridians in a case of plantar fasciitis. Journal of Chiropractic Medicine. 2014; 13(1):43-8. [DOI:10.1016/j.jcm.2014.01.006] [PMID] [PMCID]
- Cotchett MP, Landorf KB, Munteanu SE. Effectiveness of dry needling and injections of myofascial trigger points associated with plantar heel pain: A systematic review. Journal of Foot and Ankle Research. 2010; 3:18. [DOI:10.1186/1757-1146-3-18] [PMID] [PMCID]
- Dunning J, Butts R, Henry N, Mourad F, Brannon A, Rodriguez H, et al. Electrical dry needling as an adjunct to exercise, manual therapy and ultrasound for plantar fasciitis: A multi-center randomized clinical trial. Plos One. 2018; 13(10):e0205405. [DOI:10.1371/journal.pone.0205405] [PMID]
- Charles R, Fang L, Zhu R, Wang J. The effectiveness of shockwave therapy on patellar tendinopathy, Achilles tendinopathy, and plantar fasciitis: A systematic review and meta-analysis. Frontiers in Immunology. 2023; 14:1193835. [DOI:10.3389/fimmu.2023.1193835] [PMID] [PMCID]
- Bohart Z, Sussman WI, Sellon J, Sajkowicz N. Toxins for orthopedics. In: Williams Ch, Sussman WL, Pitts J, editors. Atlas of Interventional Orthopedics Procedures: Essential Guide for Fluoroscopy and Ultrasound Guided Procedures. Amsterdam: Elsevier; 2022. [DOI:10.1016/B978-0-323-75514-6.00011-X]
- Chauhan M. Efficacy of two different doses of low level laser therapy on pain and function in plantar fasciitis: A comparative study. Indian Journal of Natural Sciences. 2023; 14(79):59553-60. [Link]
- Simons D, Travell J, Simons LS. Travell & Simons' Myofascial Pain and Dysfunction: Upper half of body. Pennsylvania: Williams and Wilkins; 1999. [Link]
- Cotchett MP, Munteanu SE, Landorf KB. Effectiveness of trigger point dry needling for plantar heel pain: A randomized controlled trial. Physical Therapy. 2014; 94(8):1083-94. [DOI:10.2522/ptj.20130255] [PMID]
- Ortega-Santiago R, Ríos-León M, Martín-Casas P, Fernández-de-Las-Peñas C, Plaza-Manzano G. Active muscle trigger points are associated with pain and related disability in patients with plantar heel pain: A case-control study. Pain Medicine. 2020; 21(5):1032-8. [DOI:10.1093/pm/pnz086]
- Eftekharsadat B, Babaei-Ghazani A, Zeinolabedinzadeh V. Dry needling in patients with chronic heel pain due to plantar fasciitis: A single-blinded randomized clinical trial. Medical Journal of the Islamic Republic of Iran. 2016; 30:401. [PMID]
- Ríos-Díaz J, Martínez-Payá JJ, del Baño-Aledo ME, de Groot-Ferrando A, Botía-Castillo P, Fernández-Rodríguez D. Sonoelastography of Plantar Fascia: Reproducibility and pattern description in healthy subjects and symptomatic subjects. Ultrasound in Medicine & Biology. 2015; 41(10):2605-13. [DOI:10.1016/j.ultrasmedbio.2015.05.024] [PMID]
- Christie S, Styn G Jr, Ford G, Terryberry K. Proximal Plantar Intrinsic Tendinopathy: Anatomical and biomechanical considerations in plantar heel pain. Journal of the American Podiatric Medical Association. 2019; 109(5):412-5. [PMID]
- Rondhuis JJ, Huson A. The first branch of the lateral plantar nerve and heel pain. Acta Morphologica Neerlando-Scandinavica. 1986; 24(4):269-79. [PMID]
- Sooriakumaran P, Sivananthan S. Why does man have a quadratus plantae? A review of its comparative anatomy. Croatian Medical Journal. 2005; 46(1):30-5. [PMID]
- Salehi S, Shadmehr A, Olyaee G, Bashardoust Tajali S, Mir SM. Effectiveness of dry needling for the management of plantar fasciitis: A review study. Journal of Modern Rehabilitation. 2019; 13:1-10. [DOI:10.32598/JMR.13.1.1]
- Fernández-de-Las-Peñas C, Nijs J. Trigger point dry needling for the treatment of myofascial pain syndrome: Current perspectives within a pain neuroscience paradigm.Journal of Pain Research. 2019; 12:1899-1911. [DOI:10.2147/JPR.S154728] [PMID] [PMCID]
- Charles D, Hudgins T, MacNaughton J, Newman E, Tan J, Wigger M. A systematic review of manual therapy techniques, dry cupping and dry needling in the reduction of myofascial pain and myofascial trigger points. Journal of Bodywork and Movement Therapies. 2019; 23(3):539-46. [DOI:10.1016/j.jbmt.2019.04.001] [PMID]
- He C, Ma H. Effectiveness of trigger point dry needling for plantar heel pain: a meta-analysis of seven randomized controlled trials. Journal of Pain Research. 2017; 10:1933-42. [DOI:10.2147/JPR.S141607] [PMID] [PMCID]
- El Mallah RM, Elattar EA, Zidan HF. Platelet-rich plasma versus dry needling of myofascial meridian trigger points in the treatment of plantar fasciitis. Egyptian Rheumatology and Rehabilitation. 2017; 44:58-68. [DOI:10.4103/1110-161X.205661]
- Gamba C, Sala-Pujals A, Perez-Prieto D, Ares-Vidal J, Solano-Lopez A, Gonzalez-Lucena G, et al. Relationship of plantar fascia thickness and preoperative pain, function, and quality of life in recalcitrant plantar fasciitis. Foot & Ankle International. 2018; 39(8):930-4. [DOI:10.1177/1071100718772041]
- Digiovanni BF, Nawoczenski DA, Malay DP, Graci PA, Williams TT, Wilding GE, et al. Plantar fascia-specific stretching exercise improves outcomes in patients with chronic plantar fasciitis. A prospective clinical trial with two-year follow-up. The Journal of Bone and Joint Surgery. 2006; 88(8):1775-81. [DOI:10.2106/00004623-200608000-00013]
- Lee TL, Marx BL. Noninvasive, Multimodality Approach to Treating Plantar Fasciitis: A case study. Journal of Acupuncture and Meridian Studies. 2018; 11(4):162-4. [DOI:10.1016/j.jams.2018.04.002] [PMID]
- Ozdemir H, Yilmaz E, Murat A, Karakurt L, Poyraz AK, Ogur E. Sonographic evaluation of plantar fasciitis and relation to body mass index. European Journal of Radiology. 2005; 54(3):443-7. [DOI:10.1016/j.ejrad.2004.09.004] [PMID]
- Bodian CA, Freedman G, Hossain S, Eisenkraft JB, Beilin Y. The visual analog scale for pain: Clinical significance in postoperative patients. Anesthesiology. 2001; 95(6):1356-61. [DOI:10.1097/00000542-200112000-00013] [PMID]
- Boonstra AM, Schiphorst Preuper HR, Reneman MF, Posthumus JB, Stewart RE. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. International Journal of Rehabilitation Research. 2008; 31(2):165-9. [DOI:10.1097/MRR.0b013e3282fc0f93] [PMID]
- Neufeld SK, Cerrato R. Plantar fasciitis: evaluation and treatment. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2008; 16(6):338-46. [DOI:10.5435/00124635-200806000-00006] [PMID]
- Tough EA, White AR, Cummings TM, Richards SH, Campbell JL. Acupuncture and dry needling in the management of myofascial trigger point pain: A systematic review and meta-analysis of randomised controlled trials. European Journal of Pain. 2009; 13(1):3-10. [DOI:10.1016/j.ejpain.2008.02.006] [PMID]
- Tough EA, White AR. Effectiveness of acupuncture/dry needling for myofascial trigger point pain. Physical Therapy Reviews. 2011; 16(2):147-54. [DOI:10.1179/1743288X11Y.0000000007]
- Cotchett MP, Landorf KB, Munteanu SE, Raspovic A. Effectiveness of trigger point dry needling for plantar heel pain: study protocol for a randomised controlled trial. Journal of Foot and Ankle Research. 2011; 4:5. [DOI:10.1186/1757-1146-4-5] [PMID]
- Teasdale T. Safety, effectiveness and impact of dry needling trigger points in athletes: Asystematic review. SIRC. 2018. [Link]
- Mense S. The pathogenesis of muscle pain. Current Pain and Headache Reports. 2003; 7(6):419-25. [DOI:10.1007/s11916-003-0057-6] [PMID]
- Melzack R. Myofascial trigger points: relation to acupuncture and mechanisms of pain. Archives of Physical Medicine and Rehabilitation. 1981; 62(3):114-7. [PMID]
- Furlan AD, van Tulder M, Cherkin D, Tsukayama H, Lao L, Koes B, et al. Acupuncture and dry-needling for low back pain: An updated systematic review within the framework of the cochrane collaboration. Spine. 2005; 30(8):944-63. [DOI:10.1097/01.brs.0000158941.21571.01] [PMID]
- Al-Boloushi Z, Gómez-Trullén EM, Bellosta-López P, López-Royo MP, Fernández D, Herrero P. Comparing two dry needling interventions for plantar heel pain: A protocol for a randomized controlled trial. Journal of Orthopaedic Surgery and Research. 2019; 14(1):31. [DOI:10.1186/s13018-019-1066-4] [PMID]
- Cagnie B, Barbe T, De Ridder E, Van Oosterwijck J, Cools A, Danneels L. The influence of dry needling of the trapezius muscle on muscle blood flow and oxygenation. Journal of Manipulative and Physiological Therapeutics. 2012; 35(9):685-91. [DOI:10.1016/j.jmpt.2012.10.005] [PMID]
- Shah JP, Danoff JV, Desai MJ, Parikh S, Nakamura LY, Phillips TM, et al. Biochemicals associated with pain and inflammation are elevated in sites near to and remote from active myofascial trigger points. Archives of Physical Medicine and Rehabilitation. 2008; 89(1):16-23. [DOI:10.1016/j.apmr.2007.10.018] [PMID]
- Chou LW, Kao MJ, Lin JG. Probable mechanisms of needling therapies for myofascial pain control. Evidence-based Complementary and Alternative Medicine: eCAM. 2012; 2012:705327. [DOI:10.1155/2012/705327] [PMID]
- Fernández-Lao C, Galiano-Castillo N, Cantarero-Villanueva I, Martín-Martín L, Prados-Olleta N, Arroyo-Morales M. Analysis of pressure pain hypersensitivity, ultrasound image, and quality of life in patients with chronic plantar pain: A preliminary study. Pain Medicine. 2016; 17(8):1530-41. [DOI:10.1093/pm/pnv022] [PMID]
- Cagnie B, Dewitte V, Barbe T, Timmermans F, Delrue N, Meeus M. Physiologic effects of dry needling. Current Pain and Headache Reports. 2013; 17(8):348. [DOI:10.1007/s11916-013-0348-5] [PMID]
- Puentedura EJ, Buckingham SJ, Morton D, Montoya C, Fernandez de Las Penas C. Immediate changes in resting and contracted thickness of transversus abdominis after dry needling of lumbar multifidus in healthy participants: A randomized controlled crossover trial. Journal of Manipulative and Physiological Therapeutics. 2017; 40(8):615-23. [DOI:10.1016/j.jmpt.2017.06.013] [PMID]
- Cocco G, Ricci V, Boccatonda A, Abate M, Guagnano MT, Schiavone C. Ultrasound follow-up of spontaneous tears of the plantar fascia treated with conservative therapies: Two case reports. Medicine. 2019; 98(52):e18428. [DOI:10.1097/MD.0000000000018428] [PMID] [PMCID]
- Shiotani H, Yamashita R, Mizokuchi T, Naito M, Kawakami Y. Site-and sex-differences in morphological and mechanical properties of the plantar fascia: A supersonic shear imaging study. Journal of Biomechanics. 2019; 85:198-203. [DOI:10.1016/j.jbiomech.2019.01.014] [PMID]
Type of Study: Research |
Subject:
Sport injury and corrective exercises
Received: 2024/08/17 | Accepted: 2024/11/19 | Published: 2025/04/1
Received: 2024/08/17 | Accepted: 2024/11/19 | Published: 2025/04/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |