Sun, Feb 8, 2026
Volume 15, Issue 1 (Winter 2025)
PTJ 2025, 15(1): 1-14 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Fasihi L, Shahrbanian S, Jahangiri M. Effects of Combined Training on Fatigue in Multiple Sclerosis: A Systematic Review and Meta-analysis of Randomized Controlled Trials. PTJ 2025; 15 (1) :1-14
URL: http://ptj.uswr.ac.ir/article-1-665-en.html
URL: http://ptj.uswr.ac.ir/article-1-665-en.html
1- Department of Sport Sciences, Faculty of Humanities, Tarbiat Modares University, Tehran, Iran.
Full-Text [PDF 1828 kb]
(808 Downloads)
| Abstract (HTML) (3563 Views)
Full-Text: (1070 Views)
Introduction
Multiple sclerosis (MS) is a chronic and progressive autoimmune disease that affects the central nervous system, which includes the spinal cord and brain [1]. It is estimated that 2.8 million people worldwide suffer from MS [2]. The exact cause of MS is still unknown; however, it is considered to be caused by a complex interaction between genetic and environmental factors [3]. Fatigue, reduced mobility, emotional and cognitive issues, difficulty sleeping, and a reduction in one’s sense of autonomy and quality of life (QoL) are among the most typical symptoms [4].
At least 75% of patients with MS report experiencing fatigue at some time in their disease course, making it one of the most prevalent symptoms [1]. According to reports, one of the biggest factors that disturbs the life of people with MS is fatigue [2, 3]. People with MS frequently experience significant social, familial, and occupational disruptions [4]. They characterize weariness as an unusual feeling of exhaustion or as an increased weakness during physical activity. According to clinical reports, fatigue in patients with MS is defined as weakness that is exacerbated by exercise and heat, lack of energy, increased sleepiness, or increasing symptoms [5]. The following conditions are thought to be secondary causes of exhaustion in these patients: Spasticity, motor weakness, enuresis, neurological problems, pain, depression, sensitivity to heat, and sleep disturbances [6]. To control MS symptoms, rehabilitation therapies such as exercise, cognitive behavioral therapy, energy-saving education, vocational rehabilitation, and telerehabilitation are frequently used [7]. It is extremely challenging to manage fatigue in individuals with MS, to the point where most therapies are ineffective in reducing fatigue symptoms in these patients [8].
Physical activity is a non-pharmacological therapeutic strategy for MS that has demonstrated substantial evidence. According to Rietberg et al.’s study, there is a considerable body of evidence that supports the use of exercise to improve physical performance, muscle strength, exercise tolerance, and mobility-related skills [9]. In a review article by Finlayson and Asano, the cumulative impact of exercise treatments was assessed for both exercise and non-exercise conditions relative to control groups. Numerous exercise regimens were found to have a randomized effect on fatigue, including progressive resistance training, yoga, mountain climbing, and vestibular, abaxial, and tail muscle rehabilitation programs. With a pooled estimate of -0.57 (95% confidence interval [CI], -0.1%, -1.14%) and significant heterogeneity (Q=26.30, I2=64%, P=0.013), there was a significant decrease in fatigue [10]. Heine et al. (2015) reported that sensitivity analysis of the different types of exercise training (muscle power, endurance, task-oriented, and other training groups) revealed that the effects of exercise on fatigue were greater for the following training groups: Endurance exercise (effect size=-0.43 [95% CI, -0.69%, -0.17%], P=0.005), muscle power training (effect size=0.03 [95% CI, -1.02%, -0.32%], P=0.93), or task-oriented training (effect size=-0.34 [95% CI, -1.02 %, -0.23%], P≤0.05) [11]. People with MS can benefit from physical activity in several ways, including improved QoL, fatigue reduction, function restoration, disease management, and QoL enhancement [12]. Despite these advantages, sedentary lifestyles and insufficient physical exercise cause individuals with MS to be less physically active than the general population. This is a sedentary behavior linked to an increased risk of MS [12].
Combined resistance and endurance training into a training session is a desirable strategy that may cut down on the time needed to complete each exercise separately [13] and maximize the unique advantages of each exercise type [14]. Based on the current understanding, it is advised that people with MS combine aerobic and resistance training to reap the physiological benefits of both [15].
Compound exercise has been linked to decreased fatigue and possible benefits for patients with MS, according to several research [16, 17]. For instance, combined exercise enhances fatigue, muscle strength, and QoL [17]. In people with MS, combined exercise therapy affects walking distance, fatigue, and balance [18]. However, combined exercise has not always been successful in lowering fatigue in individuals with MS. The impact of these workouts on fatigue in individuals with MS can be better understood according to this systematic study and meta-analysis. Accordingly, this review summarizes the results of combined exercise in reducing perceived fatigue in individuals with MS.
Materials and Methods
The meta-analysis and systematic review were registered in Open Science Framework (OSF) and followed the preferred reporting items for systematic reviews and meta-analysis reporting standards (Table 1).
Study definitions
The following definitions were used as a guide for the systematic review and meta-analysis. By working a muscle or muscle group against external resistance, resistance training is a type of physical activity intended to increase muscle strength and fitness [16].
Activities involving continuous or intermittent locomotor or ergometer tasks carried out at submaximal amounts of effort are referred to as aerobic exercise. Usually, maximum oxygen uptake, relative maximal heart rate, or rating of perceived exertion are used to decide how long such exercises should last. Combining weight training and aerobic exercise into a single workout is known as combined exercise [19].
Eligibility criteria
This evaluation included studies that looked at the effects of combined exercise training in reducing subjective fatigue in patients with MS. The inclusion criteria were as follows: 1) Adult participants aged 18 years or older who had been diagnosed with MS, there were no minimum participant requirements for inclusion; 2) Regarding the intervention, concentrating on a certain exercise technique (combined exercise) at any frequency, duration, or intensity; 3) Regarding the comparator, it involved comparison across groups, with a control group not exercising (e.g. receiving standard practice, maintaining ordinary lifestyle, engaging in regular physical activity, or being on a waiting); 4) Regarding the study type, it was randomized controlled trials; and 5) The outcome was fatigue.
Meanwhile, the exclusion criteria were: 1) Studies combining exercise with other interventions (such as educational, nutritional and pharmaceutical); 2) Studies with a short intervention period ≤4 weeks which included exercise programs that could not be estimated and/or quantified, provided only an overall score, or used other study designs (e.g. quasi-RCT, sectional, cross), 3) Studies that presented only general findings, 4) Studies using other research designs (e.g. cross-sectional, quasi-RCT, and crossover) and 5) Reports not written in English.
Search strategy
A comprehensive search was conducted across five electronic databases (PEDro, PubMed/Medline, ScienceDirect, Frontiers, Wiley online library) to ensure the inclusion of a wide range of relevant articles from the existing literature. A comprehensive search was conducted from the inception of the available literature until May 2024. The search strings were manually created, without the use of automatic search tools, utilizing the main keywords “multiple sclerosis” and “exercise”. The search terms used were “combined training” OR “concurrent training” OR “aerobic and resistance training” OR “strength and endurance training” AND “multiple sclerosis”. Each keyword was searched individually in conjunction with the term “multiple sclerosis” within the database.
The initial screening process entailed assessing the article titles and abstracts to ensure they met the eligibility criteria. The writers then obtained and meticulously studied the entire text of all eligible papers. Articles that satisfied all of the inclusion criteria were included in the systematic review and duplicate articles were deleted at this stage. Furthermore, the reference lists of the retrieved articles were inspected to discover any further related publications.
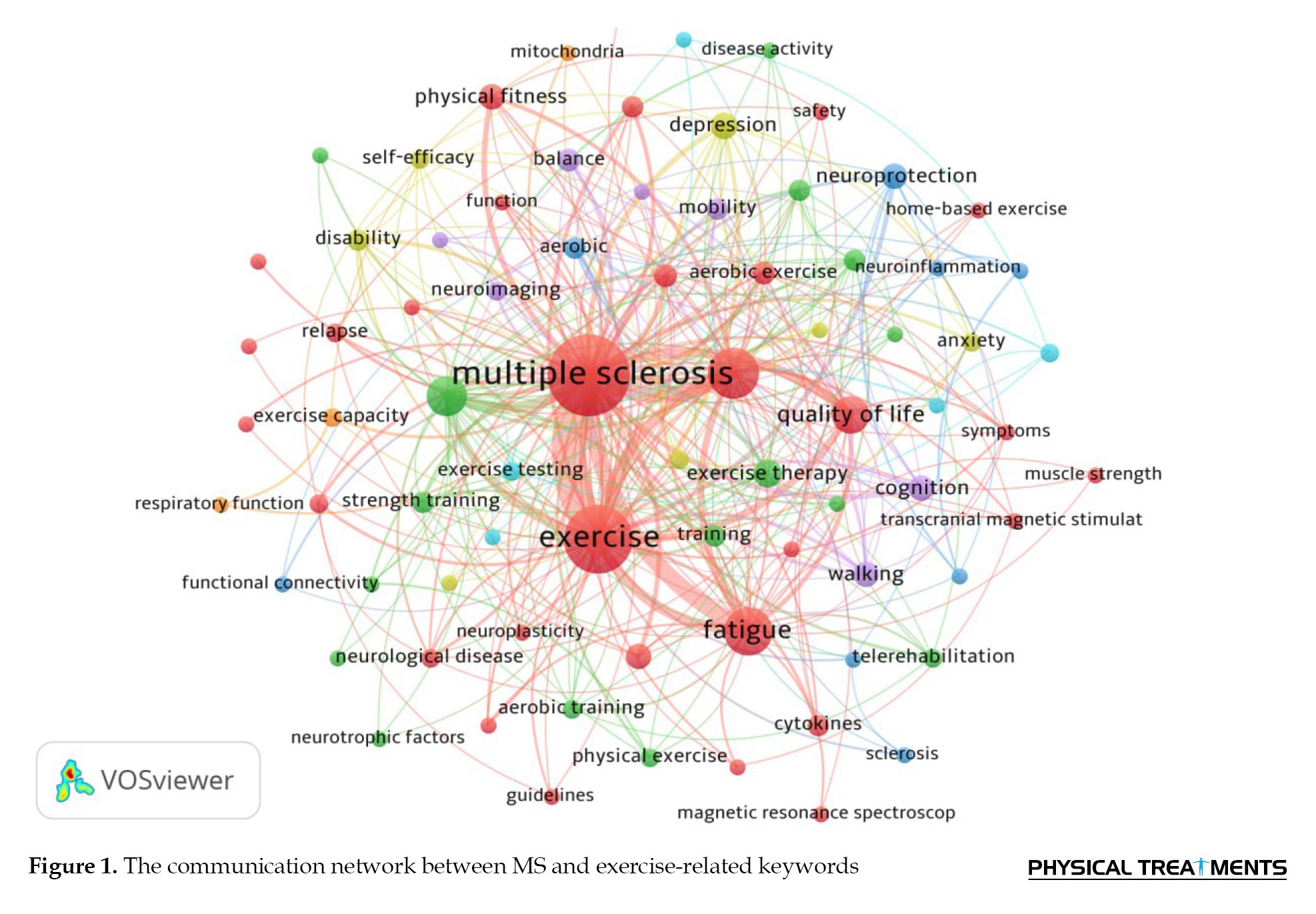
A review of the research literature on MS disease indicates that the keywords primarily employed include fatigue, QoL, muscle strength, balance, walking capacity, etc. (Figure 1).
Data extraction
The following data was taken out of each study to allow for a comparative comparison of the research findings: Authors’ names, publication year, study design, and quality assessment. Other participant characteristics included age, sample size, gender, MS type and expanded disability status scale (EDSS) scores. Intervention characteristics include frequency, duration, intensity, type, and training regimen. Fatigue was the study’s [4] outcome measurement. Additionally, outcomes, such as Mean±SD and CIs were recorded if data were supplied.
Quality assessment
Every study underwent a quality assessment utilizing the physiotherapy evidence database (PEDro) criteria. Using the PEDro scale, readers can quickly ascertain whether a clinical study offers substantial and reliable results for implementation in clinical practice [20]. The database categorizes only clinical studies, and the total number of satisfied items (0–10) is added to establish the trial’s score. Reviews and guidelines are not assigned grades. As part of this process, separate analyses are carried out by two certified assessors. If there is a disagreement, a third assessor reviews the study until classification is determined [21]. Two authors independently evaluated the articles. In case of disagreement between raters, a third reviewer was consulted and conflicts were resolved through consensus-based discussions [22].
Level of evidence and grading
The ranking approach developed by Haynes et al. [23] was followed to determine the levels of evidence that were utilized to condense the review’s findings. This scale, which is based on a study score on the PEDro scale, has been used in multiple systematic reviews and meta-analyses looking at exercise training in people with MS [24–27]. A certification of Level 1a or strong evidence was given if two or more RCTs of “high” quality (PEDro≥6) demonstrated a beneficial effect of the combined training on the study result. A level 1b designation or a moderate trial was assigned in cases where an RCT was deemed to be of “high quality” (PEDro≥6) [23].
Quantitative synthesis of studies
By merging the findings of related studies that showed clinical and methodological uniformity, we conducted a meta-analysis to get a quantitative statistical picture of the effect of the combined training on the study’s outcomes. A forest plot with 95% CI was used to compare data from homogenous studies comparing patients with MS who had combined resistance and resistance training and those who did not. Because a random-effects model could account for any variation in the effect of combined resistance and resistance training across studies, it was chosen for the meta-analysis. A fixed-effects model, on the other hand, assumes that every study estimates the same effect. To assess statistical heterogeneity, the Q test (χ2) was used and the degree of heterogeneity was reported using the I2 statistic, where higher values indicate greater heterogeneity [28]. Publication bias was assessed by examining funnel plots and performing the Egger intercept test [29]. Statistical analysis was performed using the comprehensive meta-analysis software, version 4.
Statistical analysis
All pertinent outcome data were collected following the techniques described in the studies, and all correlation data were input into the comprehensive meta-analysis software, version 4, to aid in the assessment of overall mean correlations for criterion validity. Weighted mean effect sizes and 95% CIs across trials for efficacy were computed after correlations were transformed to Fisher Z scores. The random-effects meta-analyses were based on these results. Relative odds ratios with 95% CIs were used to display the data.
This study could analyze individual trials since the random effects model meta-analyses provided an estimate of the mean distribution of effects. Rather than using a fixed effects model, this was accomplished by assigning more weight to studies with lower sample sizes and less weight to studies with larger sample sizes in the analysis [30]. The resulting estimates were re-transformed into correlation coefficients for convenience of comprehension [31]. When an effect size’s corresponding CI did not include zero, it was considered statistically significant (P<0.05) [32]. To assess the significance of differences in effect sizes, 95% CIs were used as a comparison measure. The standard Q2 test was used to measure heterogeneity. The weighted sum of squared differences between the effects of individual studies and the pooled effect of all studies indicates the presence of heterogeneity [33]. Furthermore, the I2 coefficient was employed, indicating the proportion of overall variation among studies that may be attributed to genuine heterogeneity rather than random fluctuation. I2 gives a calculation of how much of the variation in a meta-analysis is due to discrepancies between the trials included, as opposed to random sampling error. Higher values of I2 indicate more heterogeneity and the range is from 0% to 100% [34]. Funnel plots and quantitative methods, such as the Egger intercept test, filling method, and trim-and-rank correlation test were used to examine publication bias [35]. Indicators suggesting the absence of publication bias include symmetric inverted funnel plots, non-significant values of the Egger regression test for intercepts, non-significant negative rank correlations, and unchanged effect sizes using the trim-and-fill approach. The statistical analysis was carried out with version 4.0 of the Comprehensive meta-analysis software, version 4.
Results
Study selection
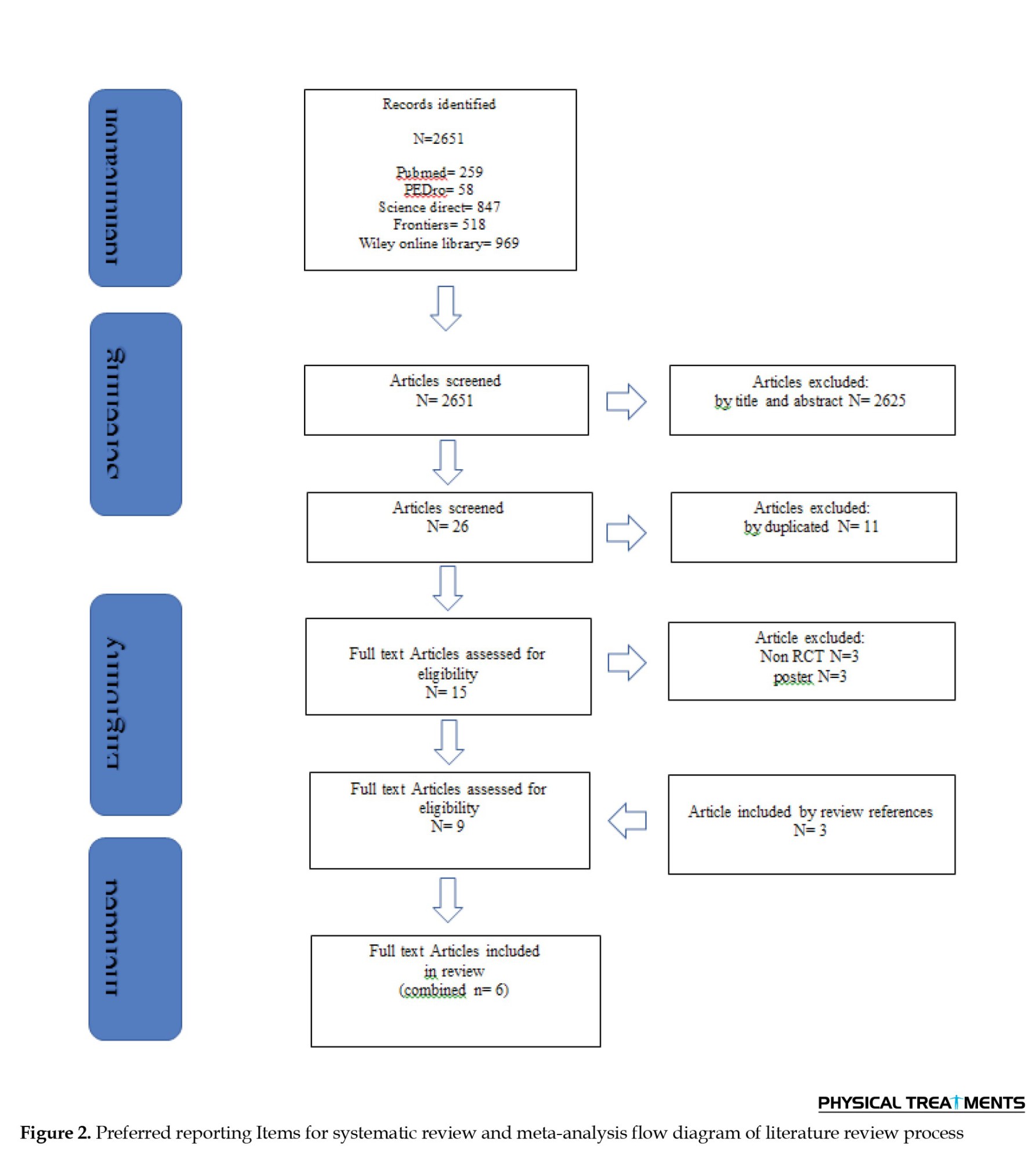
The search strategy in five electronic databases yielded 2651 full-text articles. Considering the inclusion and exclusion criteria, studies with non-randomized controlled trial designs (e.g. pilot, cross-sectional, survey, crossover and feasibility studies [n=26]), studies with non-training-based intervention designs (e.g. medical components, educational or training-nutrition combinations [n=27]), studies using comparison parameters other than training (e.g. aerobic training vs strength training, repeated measures [n=23]), studies using overlapping studies in multiple databases [n=23]), and studies with different measurement scales of fatigue (n=3) were excluded from the analysis. Overall, 6 RCT studies that satisfied the inclusion criteria were included in the qualitative analysis [17, 36–40]. Figure 2 displays a flow chart of the components mentioned in the systematic review and the ensuing meta-analysis.
Characteristics of the included studies
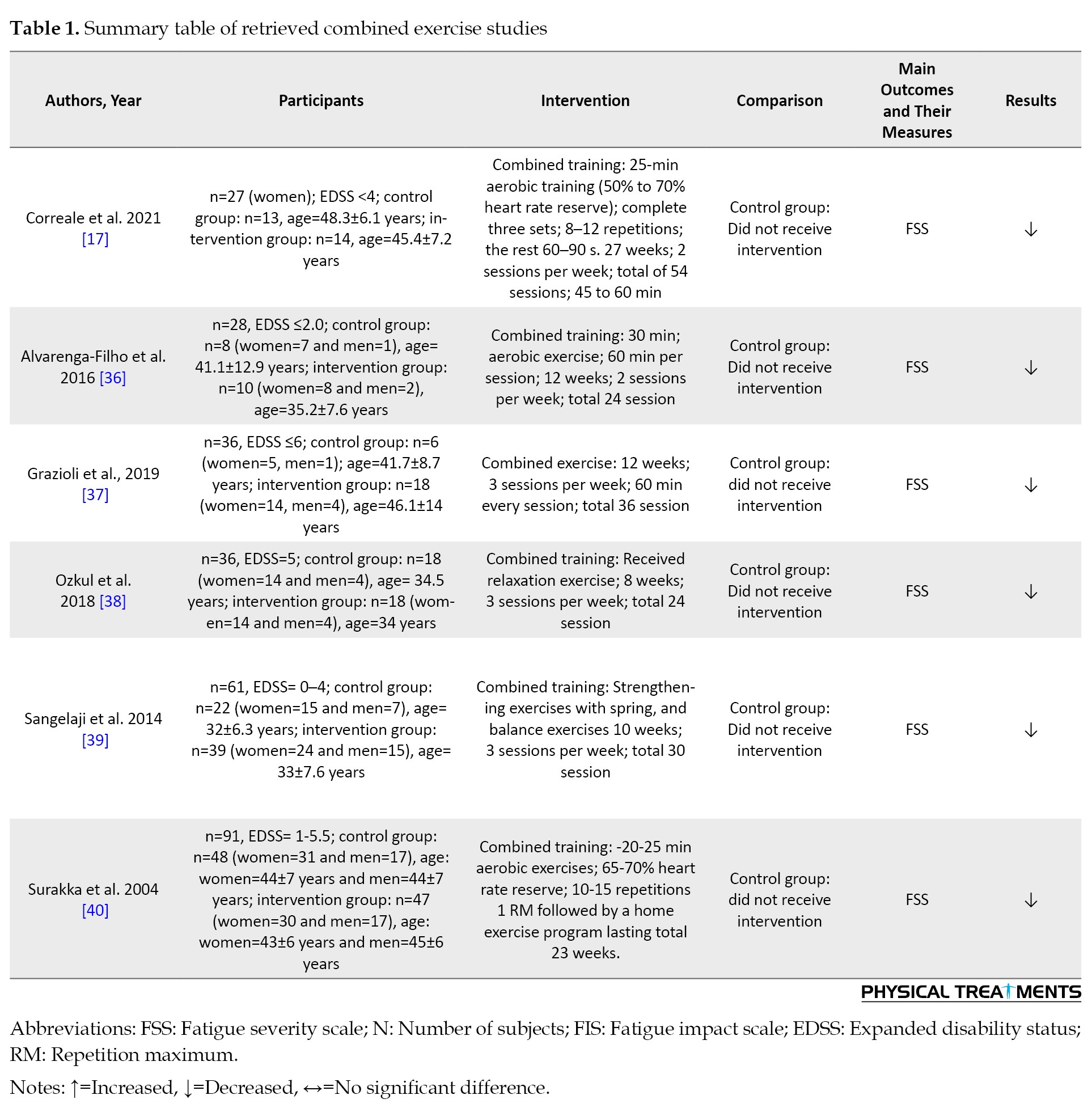
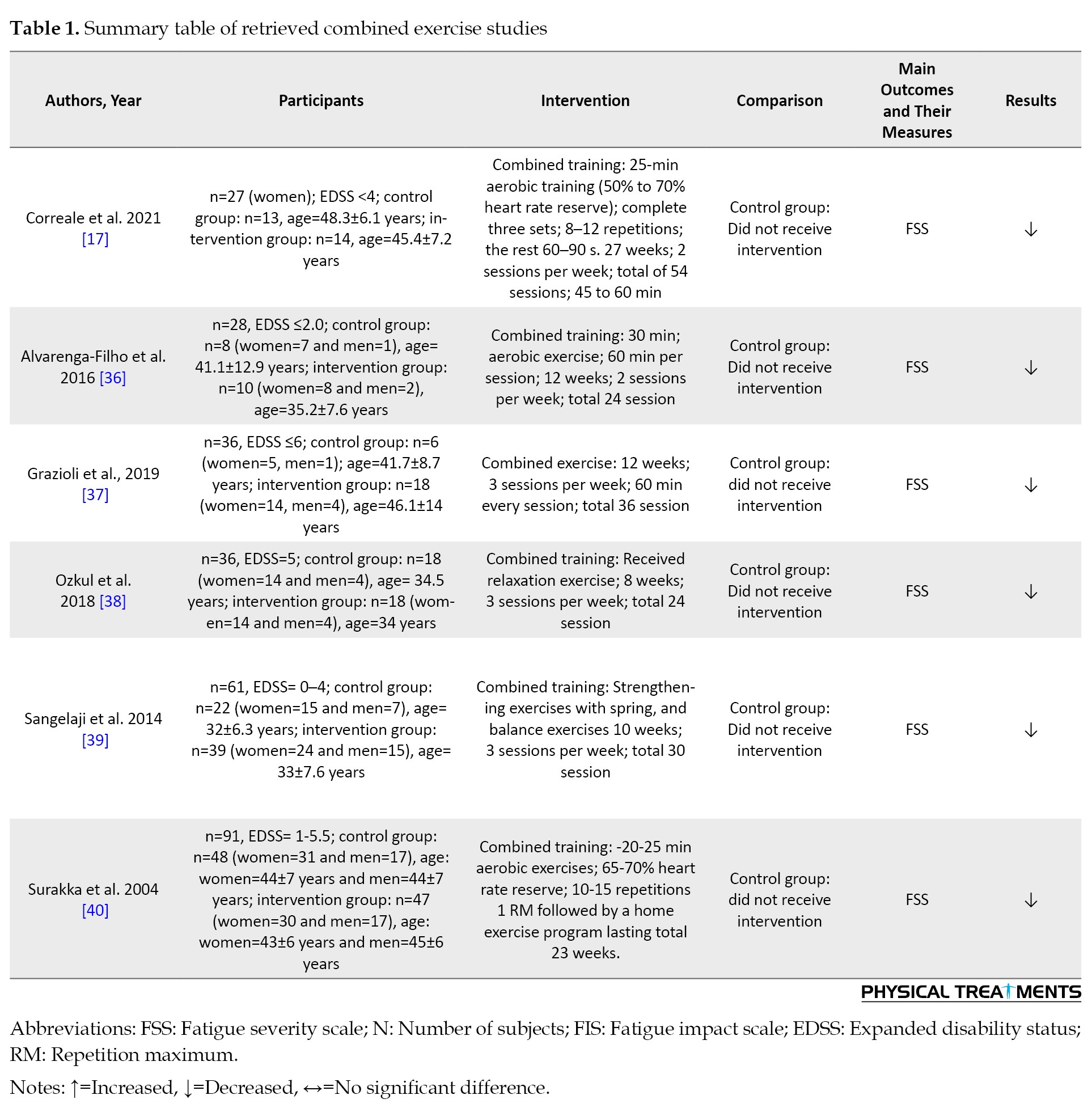
Characteristics of the six studies are provided in Table 1.
Participants’ characteristics
The selected 6 RCTs included a total of 279 participants with a Mean±SD age of 42.58±6.72 years, of which 115 were healthy controls and 164 were people with MS. The age range of participants ranged from 32 [39] to 48 [17] years. Of the participants, 189(74.89%) were female, while the remaining participants were male (n=90 [25.11%]). One study included only females with a total of 27 participants [17] (7.53%), while five studies (n=252 [92.47%]) included participants of both genders [36–40]. Five of the studies focused specifically on relapsing-remitting people with MS (83.33%) [17, 36-38, 40]. One study did not report a specific MS type (16.67%) [39].
In three studies [17, 37, 38], the diagnosis of MS was based on the McDonald criteria. In the remaining studies, the diagnostic criteria for MS were not specified. All studies included a control group. EDSS scores ranged from 0 to 6. Table 1 summarizes the main findings of the included studies.
Study interventions
Physical activity interventions were present across studies. Specific interventions are listed in Table 1.
The duration of the training protocols varied between 8 [38] and 27 [17] weeks. Except for one studies [38], the majority of studies followed a sequence of endurance training followed by resistance training. Sub-maximal exercise intensity was utilized in all studies. Three studies [17, 38, 39] incorporated aerobic exercise using an ergometer bicycle and treadmill. In three study [17, 37, 39], resistance training primarily targeted the lower limbs, while in two studies [17, 37], resistance training encompassed the entire body. The retrieved articles primarily focused on assessing perceived fatigue as an outcome variable.
Methodological quality and study classification
The methodological quality of the included studies ranged from poor to excellent, as indicated in Table 2.
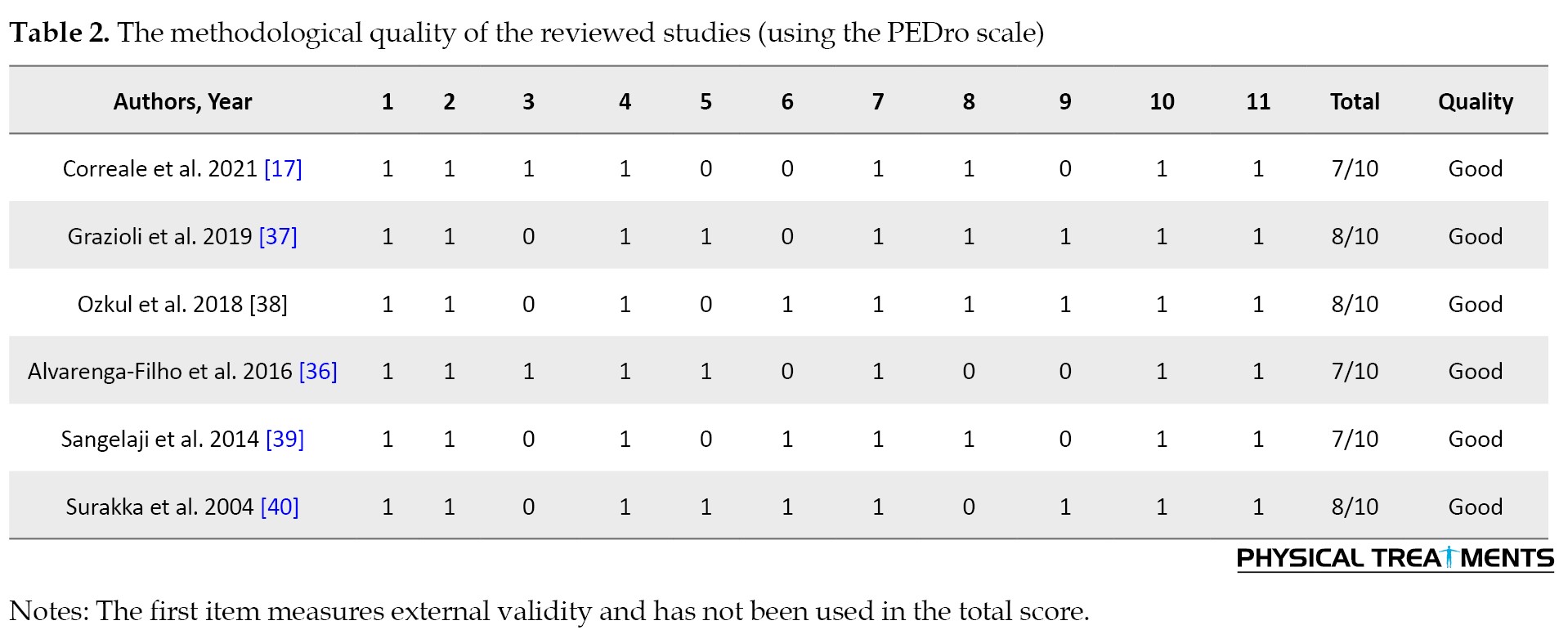
All RCTs were classified as good quality [17, 36–40]. The most common methodological issue observed was the lack of blinding of subjects and therapists, followed by the absence of intention-to-treat analysis. Additionally, many studies had small sample sizes of participants with MS and most studies did not conduct an a priori power analysis for sample size estimation. The detailed results of the quality assessment are in Table 2.
Data synthesis
The standardized effects model of meta-analyses calculated the standardized mean differences between combined training groups compared to control groups for perceived fatigue in individuals with MS.
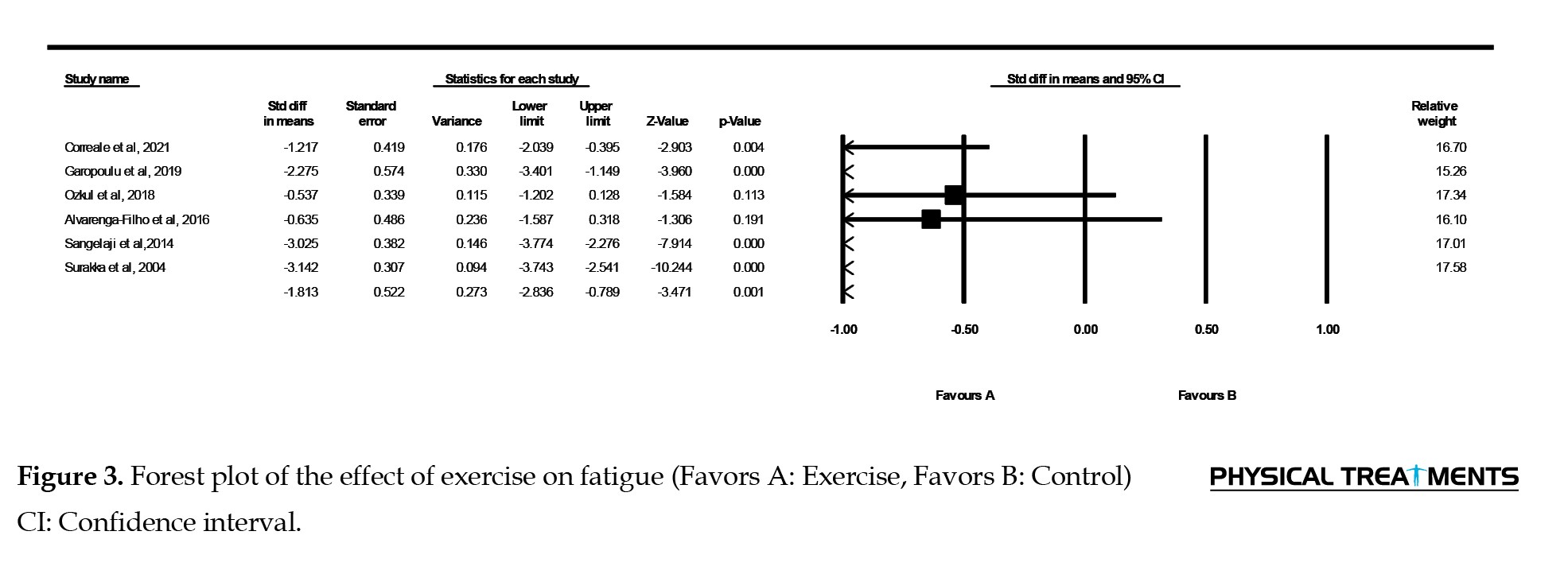
Figure 3 shows that participants who participated in a multimodal exercise program reported significantly less fatigue (Z=3.47, P=0.001) than those who did not. The pooled random mean difference in fatigue between the groups was 1.81 (95% CI, 2.83%, 0.79%). Accordingly, based on the results of the studies included in this review, people who underwent multimodal training reported 1.8 units less fatigue on the FSS than people in the control group. In addition, a 95% CI of 2.83% to 0.79% indicates that the fatigue parameter in the MS population who were involved in combined training is between 2.83 and 0.79 units less than those who did not participate.
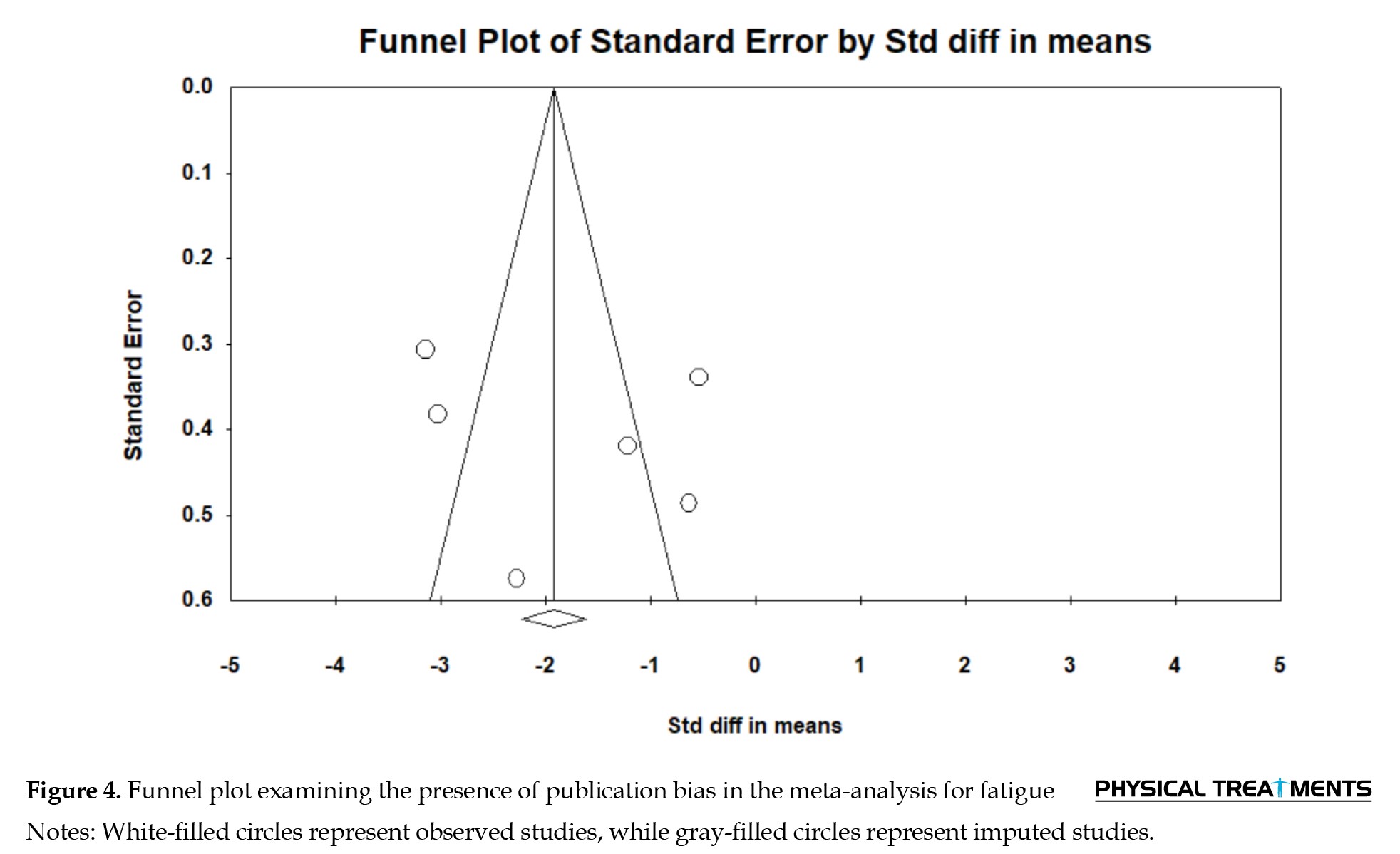
Due to the possibility of publication bias, the symmetric inverted funnel plot as shown in Figure 3 does not show clear signs of publication bias. Moreover, the non-significant negative rank correlation test (τ=0.13, P=0.35) and the non-significant Egger regression test intercept (intercept=4.01, P=0.29) do not show clear evidence of publication bias. In Figure 4, the funnel plot examines the presence of publication bias in meta-analyses for fatigue. However, the significant Q test (Q=51, P=0.001) indicated heterogeneity in the data, and the I2 index (90%) quantified a high level of heterogeneity. As all reviewed RCTs showed significant differences between the control and combined exercise groups, exercise training is effective in reducing fatigue in patients with MS.
Discussion
To the best of our knowledge, this is the first study to examine and evaluate the literature on how combined training affects individuals with MS weariness. The results of this review including 6 RCTs involving 2651 participants suggest there is evidence supporting that a combined training program is an effective therapeutic strategy for reducing fatigue among individuals with MS.
The majority of individuals with MS complain of fatigue, which is typically connected to a physical impairment. There is no established explanation for this multifaceted and intricate MS symptom, although fatigue is thought to be caused by several different variables [41]. Rehabilitative-based interventions have demonstrated a greater impact than medication-based tiredness therapies [42]. Studies on the connection between fatigue and activity in people with MS have been undertaken recently, which has raised concerns regarding this condition. Our results are consistent with other research demonstrating that people with MS might anticipate less fatigue with combined exercise program therapies [15, 36-40, 43, 44].
The results show that combined training intervention is effective in reducing fatigue. Due to its impact on fatigue, interventions utilizing this training style can result in notable improvements in muscular strength and endurance, which is pertinent for individuals with MS. These outcomes perfectly align with those of a previous investigation on how combined exercise affects tiredness in MS patients. Research examining the association between combined strength and endurance training for 12 weeks and tiredness in people with MS indicated a significant correlation [17]. In a study on tiredness and QoL in individuals with MS, multiple combined exercise treatment regimens were used. The results showed a comparable connection between exercise combinations and sleep quality, with combined therapeutic training being related to lower fatigue perception [45].
Pathophysiological processes, such as altered skeletal muscle function, including a reduction in type I muscle fibers, reduced oxidative capacity, and a predominantly anaerobic activity of extrafusal skeletal muscle fibers, may contribute to increased fatigue [41]. Also, skeletal muscle weakness and fatigue contribute to decreased activity and movement in individuals with MS, potentially leading to muscle atrophy [42]. Combined training, (resistance, and endurance training), offers dual benefits in patients with MS. Resistance training aids in reducing muscle atrophy and increasing muscle strength, while endurance training enhances mitochondrial quantity and oxidative capacity, ultimately reducing fatigue in patients with MS.
Morphological adaptations, such as increased cross-sectional area of the muscle (hypertrophy), along with other factors like hyperplasia, changes in fiber type, muscle structure, myofilament density, connective tissue structure, tendons, and nerve adaptations, play vital roles in strengthening muscle following resistance training [44]. Furthermore, as the findings of the current study indicate, combined training can increase the walking capacity of people with MS in their daily activities, potentially by enhancing muscle strength, neuromuscular coordination, and reduction of perceived fatigue. Studies employing low frequency/intensity have often extended the length of the intervention; however, other factors, such as exercise duration or intensity, may also affect dose-response relationships. Lastly, when participants were preselected based on their level of weariness, or when fatigue was viewed as the key outcome, this category performed best. The link between these results and the findings from recent research examining the impact of behavioral treatments and exercise on overall weariness has been demonstrated by several different studies. There might be several issues with this study.
Conclusion
In people with MS, exercise is a useful intervention to reduce fatigue. According to the available RCTs, combined training seems to be the most effective type of training in reducing fatigue. Given that combined exercises (resistance and endurance) have more benefits for people with MS compared to endurance or resistance exercises alone. Our results indicate that combined exercise is positive and effective for the recovery of people with MS, which should be taken into consideration when designing exercise and treatment programs for patients with MS aimed at reducing fatigue. The conflicting and limited nature of the results summarized in this study suggests that more comprehensive studies are needed to better understand and quantify the effect of regular physical activity on reducing fatigue in patients with MS. However, to find out which kind of combined exercise training is best for people with MS, additional research is necessary. Furthermore, future research should examine the effects of nutritional restriction in conjunction with a longer and more diverse exercise training time in individuals with MS.
Study limitations
This study faced several limitations that may affect the generalizability of our findings. First, we only included reviewed RCTs that were English, which could potentially introduce bias and overestimate the effect size. Although we attempted to address observed biases using the trim and fill method, the exclusion of non-English studies and unpublished results may have affected the calculated effect sizes. These factors may reduce the likelihood of discovering additional articles relevant to the review topic. Second, the high variability in methodology, outcome measures, and protocols used in different studies hinders the possibility of conducting a meta-analysis for specific variables such as muscle strength and balance and thus limits the reporting of only qualitative results. Thirdly, the limited number of studies in the combined training group (resistance and aerobic) did not allow accurate results to be presented and should be considered in future studies. Fourth, there was high heterogeneity between studies, which may be due to differences in exercise protocols, differences in severity of MS disease in different studies, and possible drug use in patients. Fifth, the small number of subjects in the included studies as well as the lack of a control group in some studies are important methodological limitations that should be considered. Despite extensive studies on the effects of sports training on MS, it is still recommended to investigate the importance of combined training in individuals with MS in future studies. In addition, it is better to investigate the relationship between the changes caused by combined exercise and the complications of MS disease to clarify the possible mechanism of the effects of exercise on improving the complications of MS disease. However, this review possesses several strengths. For instance, it did not impose restrictions on the search based on a specific date or outcome variable. Additionally, the study adhered to the Cochrane guidelines for meta-analysis and systematic review. Moreover, the quality of all included studies was assessed to mitigate the potential for biased findings.
Given the absence of definitive treatment for individuals with MS, along with the high cost and potential side effects associated with drug therapies, patients may turn to modified and cost-effective approaches like exercise to alleviate symptoms and halt disease progression. Among different training modalities, combined, resistance, and endurance training offer distinct advantages and benefits to people with MS compared to solely engaging in endurance or resistance training. Consequently, individuals experiencing symptoms such as fatigue, impaired balance, reduced physical strength, and difficulties performing daily tasks can derive significant advantages from adopting combined, resistance, and endurance training. Sports physiologists, physiotherapists, clinicians, and other healthcare providers can employ this training methodology in patients with mild to moderate disability caused by MS, aiming to prevent further disability and alleviate symptoms.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Writing the original draft and investigation: Leila Fasihi and Mohammad Jahangiri; Data collection: Leila Fasihi; Supervision, data analysis, review and editing: Shahnaz Shahrbanian;
Conflict of interest
The authors declared no conflict of interest.
References
Multiple sclerosis (MS) is a chronic and progressive autoimmune disease that affects the central nervous system, which includes the spinal cord and brain [1]. It is estimated that 2.8 million people worldwide suffer from MS [2]. The exact cause of MS is still unknown; however, it is considered to be caused by a complex interaction between genetic and environmental factors [3]. Fatigue, reduced mobility, emotional and cognitive issues, difficulty sleeping, and a reduction in one’s sense of autonomy and quality of life (QoL) are among the most typical symptoms [4].
At least 75% of patients with MS report experiencing fatigue at some time in their disease course, making it one of the most prevalent symptoms [1]. According to reports, one of the biggest factors that disturbs the life of people with MS is fatigue [2, 3]. People with MS frequently experience significant social, familial, and occupational disruptions [4]. They characterize weariness as an unusual feeling of exhaustion or as an increased weakness during physical activity. According to clinical reports, fatigue in patients with MS is defined as weakness that is exacerbated by exercise and heat, lack of energy, increased sleepiness, or increasing symptoms [5]. The following conditions are thought to be secondary causes of exhaustion in these patients: Spasticity, motor weakness, enuresis, neurological problems, pain, depression, sensitivity to heat, and sleep disturbances [6]. To control MS symptoms, rehabilitation therapies such as exercise, cognitive behavioral therapy, energy-saving education, vocational rehabilitation, and telerehabilitation are frequently used [7]. It is extremely challenging to manage fatigue in individuals with MS, to the point where most therapies are ineffective in reducing fatigue symptoms in these patients [8].
Physical activity is a non-pharmacological therapeutic strategy for MS that has demonstrated substantial evidence. According to Rietberg et al.’s study, there is a considerable body of evidence that supports the use of exercise to improve physical performance, muscle strength, exercise tolerance, and mobility-related skills [9]. In a review article by Finlayson and Asano, the cumulative impact of exercise treatments was assessed for both exercise and non-exercise conditions relative to control groups. Numerous exercise regimens were found to have a randomized effect on fatigue, including progressive resistance training, yoga, mountain climbing, and vestibular, abaxial, and tail muscle rehabilitation programs. With a pooled estimate of -0.57 (95% confidence interval [CI], -0.1%, -1.14%) and significant heterogeneity (Q=26.30, I2=64%, P=0.013), there was a significant decrease in fatigue [10]. Heine et al. (2015) reported that sensitivity analysis of the different types of exercise training (muscle power, endurance, task-oriented, and other training groups) revealed that the effects of exercise on fatigue were greater for the following training groups: Endurance exercise (effect size=-0.43 [95% CI, -0.69%, -0.17%], P=0.005), muscle power training (effect size=0.03 [95% CI, -1.02%, -0.32%], P=0.93), or task-oriented training (effect size=-0.34 [95% CI, -1.02 %, -0.23%], P≤0.05) [11]. People with MS can benefit from physical activity in several ways, including improved QoL, fatigue reduction, function restoration, disease management, and QoL enhancement [12]. Despite these advantages, sedentary lifestyles and insufficient physical exercise cause individuals with MS to be less physically active than the general population. This is a sedentary behavior linked to an increased risk of MS [12].
Combined resistance and endurance training into a training session is a desirable strategy that may cut down on the time needed to complete each exercise separately [13] and maximize the unique advantages of each exercise type [14]. Based on the current understanding, it is advised that people with MS combine aerobic and resistance training to reap the physiological benefits of both [15].
Compound exercise has been linked to decreased fatigue and possible benefits for patients with MS, according to several research [16, 17]. For instance, combined exercise enhances fatigue, muscle strength, and QoL [17]. In people with MS, combined exercise therapy affects walking distance, fatigue, and balance [18]. However, combined exercise has not always been successful in lowering fatigue in individuals with MS. The impact of these workouts on fatigue in individuals with MS can be better understood according to this systematic study and meta-analysis. Accordingly, this review summarizes the results of combined exercise in reducing perceived fatigue in individuals with MS.
Materials and Methods
The meta-analysis and systematic review were registered in Open Science Framework (OSF) and followed the preferred reporting items for systematic reviews and meta-analysis reporting standards (Table 1).
Study definitions
The following definitions were used as a guide for the systematic review and meta-analysis. By working a muscle or muscle group against external resistance, resistance training is a type of physical activity intended to increase muscle strength and fitness [16].
Activities involving continuous or intermittent locomotor or ergometer tasks carried out at submaximal amounts of effort are referred to as aerobic exercise. Usually, maximum oxygen uptake, relative maximal heart rate, or rating of perceived exertion are used to decide how long such exercises should last. Combining weight training and aerobic exercise into a single workout is known as combined exercise [19].
Eligibility criteria
This evaluation included studies that looked at the effects of combined exercise training in reducing subjective fatigue in patients with MS. The inclusion criteria were as follows: 1) Adult participants aged 18 years or older who had been diagnosed with MS, there were no minimum participant requirements for inclusion; 2) Regarding the intervention, concentrating on a certain exercise technique (combined exercise) at any frequency, duration, or intensity; 3) Regarding the comparator, it involved comparison across groups, with a control group not exercising (e.g. receiving standard practice, maintaining ordinary lifestyle, engaging in regular physical activity, or being on a waiting); 4) Regarding the study type, it was randomized controlled trials; and 5) The outcome was fatigue.
Meanwhile, the exclusion criteria were: 1) Studies combining exercise with other interventions (such as educational, nutritional and pharmaceutical); 2) Studies with a short intervention period ≤4 weeks which included exercise programs that could not be estimated and/or quantified, provided only an overall score, or used other study designs (e.g. quasi-RCT, sectional, cross), 3) Studies that presented only general findings, 4) Studies using other research designs (e.g. cross-sectional, quasi-RCT, and crossover) and 5) Reports not written in English.
Search strategy
A comprehensive search was conducted across five electronic databases (PEDro, PubMed/Medline, ScienceDirect, Frontiers, Wiley online library) to ensure the inclusion of a wide range of relevant articles from the existing literature. A comprehensive search was conducted from the inception of the available literature until May 2024. The search strings were manually created, without the use of automatic search tools, utilizing the main keywords “multiple sclerosis” and “exercise”. The search terms used were “combined training” OR “concurrent training” OR “aerobic and resistance training” OR “strength and endurance training” AND “multiple sclerosis”. Each keyword was searched individually in conjunction with the term “multiple sclerosis” within the database.
The initial screening process entailed assessing the article titles and abstracts to ensure they met the eligibility criteria. The writers then obtained and meticulously studied the entire text of all eligible papers. Articles that satisfied all of the inclusion criteria were included in the systematic review and duplicate articles were deleted at this stage. Furthermore, the reference lists of the retrieved articles were inspected to discover any further related publications.
A review of the research literature on MS disease indicates that the keywords primarily employed include fatigue, QoL, muscle strength, balance, walking capacity, etc. (Figure 1).
Data extraction
The following data was taken out of each study to allow for a comparative comparison of the research findings: Authors’ names, publication year, study design, and quality assessment. Other participant characteristics included age, sample size, gender, MS type and expanded disability status scale (EDSS) scores. Intervention characteristics include frequency, duration, intensity, type, and training regimen. Fatigue was the study’s [4] outcome measurement. Additionally, outcomes, such as Mean±SD and CIs were recorded if data were supplied.
Quality assessment
Every study underwent a quality assessment utilizing the physiotherapy evidence database (PEDro) criteria. Using the PEDro scale, readers can quickly ascertain whether a clinical study offers substantial and reliable results for implementation in clinical practice [20]. The database categorizes only clinical studies, and the total number of satisfied items (0–10) is added to establish the trial’s score. Reviews and guidelines are not assigned grades. As part of this process, separate analyses are carried out by two certified assessors. If there is a disagreement, a third assessor reviews the study until classification is determined [21]. Two authors independently evaluated the articles. In case of disagreement between raters, a third reviewer was consulted and conflicts were resolved through consensus-based discussions [22].
Level of evidence and grading
The ranking approach developed by Haynes et al. [23] was followed to determine the levels of evidence that were utilized to condense the review’s findings. This scale, which is based on a study score on the PEDro scale, has been used in multiple systematic reviews and meta-analyses looking at exercise training in people with MS [24–27]. A certification of Level 1a or strong evidence was given if two or more RCTs of “high” quality (PEDro≥6) demonstrated a beneficial effect of the combined training on the study result. A level 1b designation or a moderate trial was assigned in cases where an RCT was deemed to be of “high quality” (PEDro≥6) [23].
Quantitative synthesis of studies
By merging the findings of related studies that showed clinical and methodological uniformity, we conducted a meta-analysis to get a quantitative statistical picture of the effect of the combined training on the study’s outcomes. A forest plot with 95% CI was used to compare data from homogenous studies comparing patients with MS who had combined resistance and resistance training and those who did not. Because a random-effects model could account for any variation in the effect of combined resistance and resistance training across studies, it was chosen for the meta-analysis. A fixed-effects model, on the other hand, assumes that every study estimates the same effect. To assess statistical heterogeneity, the Q test (χ2) was used and the degree of heterogeneity was reported using the I2 statistic, where higher values indicate greater heterogeneity [28]. Publication bias was assessed by examining funnel plots and performing the Egger intercept test [29]. Statistical analysis was performed using the comprehensive meta-analysis software, version 4.
Statistical analysis
All pertinent outcome data were collected following the techniques described in the studies, and all correlation data were input into the comprehensive meta-analysis software, version 4, to aid in the assessment of overall mean correlations for criterion validity. Weighted mean effect sizes and 95% CIs across trials for efficacy were computed after correlations were transformed to Fisher Z scores. The random-effects meta-analyses were based on these results. Relative odds ratios with 95% CIs were used to display the data.
This study could analyze individual trials since the random effects model meta-analyses provided an estimate of the mean distribution of effects. Rather than using a fixed effects model, this was accomplished by assigning more weight to studies with lower sample sizes and less weight to studies with larger sample sizes in the analysis [30]. The resulting estimates were re-transformed into correlation coefficients for convenience of comprehension [31]. When an effect size’s corresponding CI did not include zero, it was considered statistically significant (P<0.05) [32]. To assess the significance of differences in effect sizes, 95% CIs were used as a comparison measure. The standard Q2 test was used to measure heterogeneity. The weighted sum of squared differences between the effects of individual studies and the pooled effect of all studies indicates the presence of heterogeneity [33]. Furthermore, the I2 coefficient was employed, indicating the proportion of overall variation among studies that may be attributed to genuine heterogeneity rather than random fluctuation. I2 gives a calculation of how much of the variation in a meta-analysis is due to discrepancies between the trials included, as opposed to random sampling error. Higher values of I2 indicate more heterogeneity and the range is from 0% to 100% [34]. Funnel plots and quantitative methods, such as the Egger intercept test, filling method, and trim-and-rank correlation test were used to examine publication bias [35]. Indicators suggesting the absence of publication bias include symmetric inverted funnel plots, non-significant values of the Egger regression test for intercepts, non-significant negative rank correlations, and unchanged effect sizes using the trim-and-fill approach. The statistical analysis was carried out with version 4.0 of the Comprehensive meta-analysis software, version 4.
Results
Study selection
The search strategy in five electronic databases yielded 2651 full-text articles. Considering the inclusion and exclusion criteria, studies with non-randomized controlled trial designs (e.g. pilot, cross-sectional, survey, crossover and feasibility studies [n=26]), studies with non-training-based intervention designs (e.g. medical components, educational or training-nutrition combinations [n=27]), studies using comparison parameters other than training (e.g. aerobic training vs strength training, repeated measures [n=23]), studies using overlapping studies in multiple databases [n=23]), and studies with different measurement scales of fatigue (n=3) were excluded from the analysis. Overall, 6 RCT studies that satisfied the inclusion criteria were included in the qualitative analysis [17, 36–40]. Figure 2 displays a flow chart of the components mentioned in the systematic review and the ensuing meta-analysis.
Characteristics of the included studies
Characteristics of the six studies are provided in Table 1.
Participants’ characteristics
The selected 6 RCTs included a total of 279 participants with a Mean±SD age of 42.58±6.72 years, of which 115 were healthy controls and 164 were people with MS. The age range of participants ranged from 32 [39] to 48 [17] years. Of the participants, 189(74.89%) were female, while the remaining participants were male (n=90 [25.11%]). One study included only females with a total of 27 participants [17] (7.53%), while five studies (n=252 [92.47%]) included participants of both genders [36–40]. Five of the studies focused specifically on relapsing-remitting people with MS (83.33%) [17, 36-38, 40]. One study did not report a specific MS type (16.67%) [39].
In three studies [17, 37, 38], the diagnosis of MS was based on the McDonald criteria. In the remaining studies, the diagnostic criteria for MS were not specified. All studies included a control group. EDSS scores ranged from 0 to 6. Table 1 summarizes the main findings of the included studies.
Study interventions
Physical activity interventions were present across studies. Specific interventions are listed in Table 1.
The duration of the training protocols varied between 8 [38] and 27 [17] weeks. Except for one studies [38], the majority of studies followed a sequence of endurance training followed by resistance training. Sub-maximal exercise intensity was utilized in all studies. Three studies [17, 38, 39] incorporated aerobic exercise using an ergometer bicycle and treadmill. In three study [17, 37, 39], resistance training primarily targeted the lower limbs, while in two studies [17, 37], resistance training encompassed the entire body. The retrieved articles primarily focused on assessing perceived fatigue as an outcome variable.
Methodological quality and study classification
The methodological quality of the included studies ranged from poor to excellent, as indicated in Table 2.
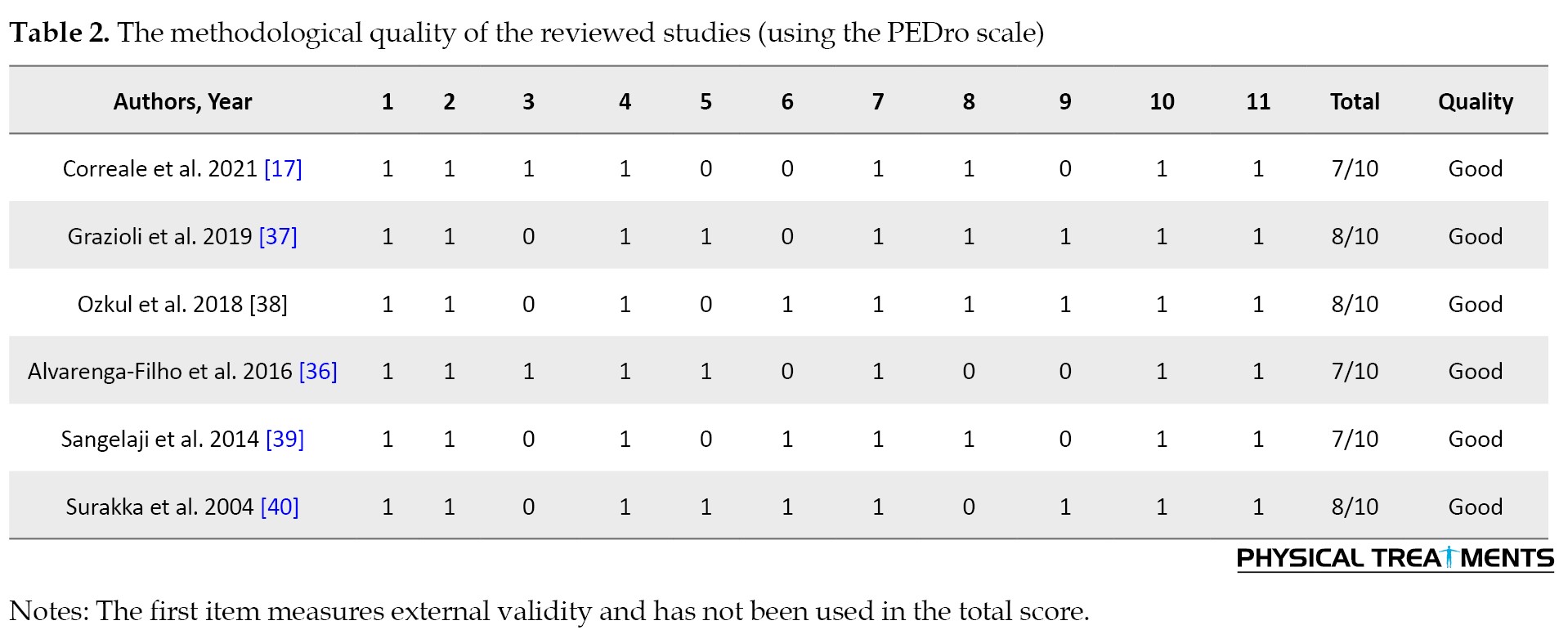
All RCTs were classified as good quality [17, 36–40]. The most common methodological issue observed was the lack of blinding of subjects and therapists, followed by the absence of intention-to-treat analysis. Additionally, many studies had small sample sizes of participants with MS and most studies did not conduct an a priori power analysis for sample size estimation. The detailed results of the quality assessment are in Table 2.
Data synthesis
The standardized effects model of meta-analyses calculated the standardized mean differences between combined training groups compared to control groups for perceived fatigue in individuals with MS.
Figure 3 shows that participants who participated in a multimodal exercise program reported significantly less fatigue (Z=3.47, P=0.001) than those who did not. The pooled random mean difference in fatigue between the groups was 1.81 (95% CI, 2.83%, 0.79%). Accordingly, based on the results of the studies included in this review, people who underwent multimodal training reported 1.8 units less fatigue on the FSS than people in the control group. In addition, a 95% CI of 2.83% to 0.79% indicates that the fatigue parameter in the MS population who were involved in combined training is between 2.83 and 0.79 units less than those who did not participate.
Due to the possibility of publication bias, the symmetric inverted funnel plot as shown in Figure 3 does not show clear signs of publication bias. Moreover, the non-significant negative rank correlation test (τ=0.13, P=0.35) and the non-significant Egger regression test intercept (intercept=4.01, P=0.29) do not show clear evidence of publication bias. In Figure 4, the funnel plot examines the presence of publication bias in meta-analyses for fatigue. However, the significant Q test (Q=51, P=0.001) indicated heterogeneity in the data, and the I2 index (90%) quantified a high level of heterogeneity. As all reviewed RCTs showed significant differences between the control and combined exercise groups, exercise training is effective in reducing fatigue in patients with MS.
Discussion
To the best of our knowledge, this is the first study to examine and evaluate the literature on how combined training affects individuals with MS weariness. The results of this review including 6 RCTs involving 2651 participants suggest there is evidence supporting that a combined training program is an effective therapeutic strategy for reducing fatigue among individuals with MS.
The majority of individuals with MS complain of fatigue, which is typically connected to a physical impairment. There is no established explanation for this multifaceted and intricate MS symptom, although fatigue is thought to be caused by several different variables [41]. Rehabilitative-based interventions have demonstrated a greater impact than medication-based tiredness therapies [42]. Studies on the connection between fatigue and activity in people with MS have been undertaken recently, which has raised concerns regarding this condition. Our results are consistent with other research demonstrating that people with MS might anticipate less fatigue with combined exercise program therapies [15, 36-40, 43, 44].
The results show that combined training intervention is effective in reducing fatigue. Due to its impact on fatigue, interventions utilizing this training style can result in notable improvements in muscular strength and endurance, which is pertinent for individuals with MS. These outcomes perfectly align with those of a previous investigation on how combined exercise affects tiredness in MS patients. Research examining the association between combined strength and endurance training for 12 weeks and tiredness in people with MS indicated a significant correlation [17]. In a study on tiredness and QoL in individuals with MS, multiple combined exercise treatment regimens were used. The results showed a comparable connection between exercise combinations and sleep quality, with combined therapeutic training being related to lower fatigue perception [45].
Pathophysiological processes, such as altered skeletal muscle function, including a reduction in type I muscle fibers, reduced oxidative capacity, and a predominantly anaerobic activity of extrafusal skeletal muscle fibers, may contribute to increased fatigue [41]. Also, skeletal muscle weakness and fatigue contribute to decreased activity and movement in individuals with MS, potentially leading to muscle atrophy [42]. Combined training, (resistance, and endurance training), offers dual benefits in patients with MS. Resistance training aids in reducing muscle atrophy and increasing muscle strength, while endurance training enhances mitochondrial quantity and oxidative capacity, ultimately reducing fatigue in patients with MS.
Morphological adaptations, such as increased cross-sectional area of the muscle (hypertrophy), along with other factors like hyperplasia, changes in fiber type, muscle structure, myofilament density, connective tissue structure, tendons, and nerve adaptations, play vital roles in strengthening muscle following resistance training [44]. Furthermore, as the findings of the current study indicate, combined training can increase the walking capacity of people with MS in their daily activities, potentially by enhancing muscle strength, neuromuscular coordination, and reduction of perceived fatigue. Studies employing low frequency/intensity have often extended the length of the intervention; however, other factors, such as exercise duration or intensity, may also affect dose-response relationships. Lastly, when participants were preselected based on their level of weariness, or when fatigue was viewed as the key outcome, this category performed best. The link between these results and the findings from recent research examining the impact of behavioral treatments and exercise on overall weariness has been demonstrated by several different studies. There might be several issues with this study.
Conclusion
In people with MS, exercise is a useful intervention to reduce fatigue. According to the available RCTs, combined training seems to be the most effective type of training in reducing fatigue. Given that combined exercises (resistance and endurance) have more benefits for people with MS compared to endurance or resistance exercises alone. Our results indicate that combined exercise is positive and effective for the recovery of people with MS, which should be taken into consideration when designing exercise and treatment programs for patients with MS aimed at reducing fatigue. The conflicting and limited nature of the results summarized in this study suggests that more comprehensive studies are needed to better understand and quantify the effect of regular physical activity on reducing fatigue in patients with MS. However, to find out which kind of combined exercise training is best for people with MS, additional research is necessary. Furthermore, future research should examine the effects of nutritional restriction in conjunction with a longer and more diverse exercise training time in individuals with MS.
Study limitations
This study faced several limitations that may affect the generalizability of our findings. First, we only included reviewed RCTs that were English, which could potentially introduce bias and overestimate the effect size. Although we attempted to address observed biases using the trim and fill method, the exclusion of non-English studies and unpublished results may have affected the calculated effect sizes. These factors may reduce the likelihood of discovering additional articles relevant to the review topic. Second, the high variability in methodology, outcome measures, and protocols used in different studies hinders the possibility of conducting a meta-analysis for specific variables such as muscle strength and balance and thus limits the reporting of only qualitative results. Thirdly, the limited number of studies in the combined training group (resistance and aerobic) did not allow accurate results to be presented and should be considered in future studies. Fourth, there was high heterogeneity between studies, which may be due to differences in exercise protocols, differences in severity of MS disease in different studies, and possible drug use in patients. Fifth, the small number of subjects in the included studies as well as the lack of a control group in some studies are important methodological limitations that should be considered. Despite extensive studies on the effects of sports training on MS, it is still recommended to investigate the importance of combined training in individuals with MS in future studies. In addition, it is better to investigate the relationship between the changes caused by combined exercise and the complications of MS disease to clarify the possible mechanism of the effects of exercise on improving the complications of MS disease. However, this review possesses several strengths. For instance, it did not impose restrictions on the search based on a specific date or outcome variable. Additionally, the study adhered to the Cochrane guidelines for meta-analysis and systematic review. Moreover, the quality of all included studies was assessed to mitigate the potential for biased findings.
Given the absence of definitive treatment for individuals with MS, along with the high cost and potential side effects associated with drug therapies, patients may turn to modified and cost-effective approaches like exercise to alleviate symptoms and halt disease progression. Among different training modalities, combined, resistance, and endurance training offer distinct advantages and benefits to people with MS compared to solely engaging in endurance or resistance training. Consequently, individuals experiencing symptoms such as fatigue, impaired balance, reduced physical strength, and difficulties performing daily tasks can derive significant advantages from adopting combined, resistance, and endurance training. Sports physiologists, physiotherapists, clinicians, and other healthcare providers can employ this training methodology in patients with mild to moderate disability caused by MS, aiming to prevent further disability and alleviate symptoms.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Writing the original draft and investigation: Leila Fasihi and Mohammad Jahangiri; Data collection: Leila Fasihi; Supervision, data analysis, review and editing: Shahnaz Shahrbanian;
Conflict of interest
The authors declared no conflict of interest.
References
- Herndon RM. Multiple sclerosis: Immunology, pathology and pathophysiology. New York: Demos Medical Publishing; 2002. [Link]
- Abbaspoor E, Zolfaghari M, Ahmadi B, Khodaei K. The effect of combined functional training on BDNF, IGF-1, and their association with health-related fitness in the multiple sclerosis women. Growth Hormone & IGF Research. 2020; 52:101320. [DOI:10.1016/j.ghir.2020.101320] [PMID]
- Shahrbanian S, Duquette P, E Mayo N. Impairment, disability and fatigue in multiple sclerosis. Caspian Journal of Internal Medicine. 2018; 9(3):244-51. [DOI: 10.22088/cjim.9.3.244] [PMID]
- Motl RW, Sandroff BM, Pilutti LA, Cutter GR, Aldunate R, Kidwell-Chandler A, et al. Randomized controlled trial of the behavioral intervention for increasing physical activity in multiple sclerosis project: Secondary, patient-reported outcomes. Contemporary Clinical Trials. 2023; 125:107056. [DOI:10.1016/j.cct.2022.107056] [PMID]
- Cederberg KL. Restless legs syndrome and multiple sclerosis: The possible role of physical activity for managing symptoms [doctoral dissertation]. Birmingham: The University of Alabama at Birmingham; 2020. [Link]
- Hensman MY. A qualitative and quantitative exploration of sedentary behaviour, physical activity and exercise in people with multiple sclerosis [doctoral dissertation]. Birmingham: University of Birmingham; 2022. [Link]
- Amatya B, Khan F, Galea M. Rehabilitation for people with multiple sclerosis: An overview of Cochrane Reviews. The Cochrane Database of Systematic Reviews. 2019; 1(1):CD012732. [DOI:10.1002/14651858.CD012732.pub2] [PMID] [PMCID]
- Lee D, Newell R, Ziegler L, Topping A. Treatment of fatigue in multiple sclerosis: A systematic review of the literature. International Journal of Nursing Practice. 2008; 14(2):81-93. [DOI:10.1111/j.1440-172X.2008.00670.x] [PMID]
- Rietberg MB, Brooks D, Uitdehaag BM, Kwakkel G. Exercise therapy for multiple sclerosis. The Cochrane Database of Systematic Reviews. 2005; 2005(1):CD003980. [DOI:10.1002/14651858.CD003980.pub2] [PMID] [PMCID]
- Asano M, Finlayson ML. Meta-analysis of three different types of fatigue management interventions for people with multiple sclerosis: Exercise, education, and medication. Multiple Sclerosis International. 2014; 2014:798285. [DOI:10.1155/2014/798285] [PMID] [PMCID]
- Heine M, van de Port I, Rietberg MB, van Wegen EE, Kwakkel G. Exercise therapy for fatigue in multiple sclerosis. The Cochrane Database of Systematic Reviews. 2015; 2015(9):CD009956. [DOI:10.1002/14651858.CD009956.pub2] [PMID] [PMCID]
- Reina-Gutiérrez S, Meseguer-Henarejos AB, Torres-Costoso A, Álvarez-Bueno C, Cavero-Redondo I, Núñez de Arenas-Arroyo S, et al. Effect of different types of exercise on fitness in people with multiple sclerosis: A network meta-analysis. Scandinavian Journal of Medicine & Science in Sports. 2023; 33(10):1916-28. [DOI:10.1111/sms.14407] [PMID]
- Gäbler M, Prieske O, Hortobágyi T, Granacher U. The effects of concurrent strength and endurance training on physical fitness and athletic performance in youth: A systematic review and meta-analysis. Frontiers in Physiology. 2018; 9:1057. [DOI:10.3389/fphys.2018.01057] [PMID] [PMCID]
- Wens I, Hansen D, Verboven K, Deckx N, Kosten L, Stevens AL, et al. Impact of 24 weeks of resistance and endurance exercise on glucose tolerance in persons with multiple sclerosis. American Journal of Physical Medicine & Rehabilitation. 2015; 94(10 Suppl 1):838-47. [DOI:10.1097/PHM.0000000000000257] [PMID]
- Ozkul C, Guclu-Gunduz A, Eldemir K, Apaydin Y, Yazici G, Irkec C. Combined exercise training improves cognitive functions in multiple sclerosis patients with cognitive impairment: A single-blinded randomized controlled trial. Multiple Sclerosis and Related Disorders. 2020; 45:102419. [DOI:10.1016/j.msard.2020.102419] [PMID]
- Taul-Madsen L, Connolly L, Dennett R, Freeman J, Dalgas U, Hvid LG. Is aerobic or resistance training the most effective exercise modality for improving lower extremity physical function and perceived fatigue in people with multiple sclerosis? A systematic review and meta-analysis. Archives of Physical Medicine and Rehabilitation. 2021; 102(10):2032-48. [DOI:10.1016/j.apmr.2021.03.026] [PMID]
- Correale L, Buzzachera CF, Liberali G, Codrons E, Mallucci G, Vandoni M, et al. Effects of combined endurance and resistance training in women with multiple sclerosis: A randomized controlled study. Frontiers in Neurology. 2021; 12:698460. [DOI:10.3389/fneur.2021.698460] [PMID] [PMCID]
- Andreu-Caravaca L, Ramos-Campo DJ, Chung LH, Rubio-Arias JÁ. Dosage and effectiveness of aerobic training on cardiorespiratory fitness, functional capacity, balance, and fatigue in people with multiple sclerosis: A systematic review and meta-analysis. Archives of Physical Medicine and Rehabilitation. 2021; 102(9):1826-39. [DOI:10.1016/j.apmr.2021.01.078] [PMID]
- Izquierdo M, Merchant RA, Morley JE, Anker SD, Aprahamian I, Arai H, et al. International exercise recommendations in older adults (ICFSR): Expert consensus guidelines. The Journal of Nutrition, Health & Aging. 2021; 25(7):824-53. [DOI:10.1007/s12603-021-1665-8] [PMID]
- Kamper SJ, Moseley AM, Herbert RD, Maher CG, Elkins MR, Sherrington C. 15 years of tracking physiotherapy evidence on PEDro, where are we now? British Journal of Sports Medicine. 2015; 49(14):907-9. [DOI:10.1136/bjsports-2014-094468] [PMID]
- Blyth FM, Briggs AM, Schneider CH, Hoy DG, March LM. The global burden of musculoskeletal pain-where to from here? American Journal of Public Health. 2019; 109(1):35-40. [DOI:10.2105/AJPH.2018.304747] [PMID] [PMCID]
- Furlan JC, Singh J, Hsieh J, Fehlings MG. Methodology of systematic reviews and recommendations. Journal of Neurotrauma. 2011; 28(8):1335-9. [DOI:10.1089/neu.2009.1146] [PMID] [PMCID]
- Haynes B, Glasziou P, Straus S. Advances in evidence-based information resources for clinical practice. ACP Journal Club. 2000; 132(1):A11-4. [DOI:10.1136/ebm.5.1.4] [PMID]
- Latimer-Cheung AE, Pilutti LA, Hicks AL, Martin Ginis KA, Fenuta AM, MacKibbon KA, et al. Effects of exercise training on fitness, mobility, fatigue, and health-related quality of life among adults with multiple sclerosis: A systematic review to inform guideline development. Archives of Physical Medicine and Rehabilitation. 2013; 94(9):1800-28. [DOI:10.1016/j.apmr.2013.04.020] [PMID]
- Ensari I, Motl RW, Pilutti LA. Exercise training improves depressive symptoms in people with multiple sclerosis: Results of a meta-analysis. Journal of Psychosomatic Research. 2014; 76(6):465-71. [DOI:10.1016/j.jpsychores.2014.03.014] [PMID]
- Platta ME, Ensari I, Motl RW, Pilutti LA. Effect of exercise training on fitness in multiple sclerosis: A meta-analysis. Archives of Physical Medicine and Rehabilitation. 2016; 97(9):1564-72. [DOI:10.1016/j.apmr.2016.01.023] [PMID]
- Pilutti LA, Greenlee TA, Motl RW, Nickrent MS, Petruzzello SJ. Effects of exercise training on fatigue in multiple sclerosis: A meta-analysis. Psychosomatic Medicine. 2013; 75(6):575-80. [DOI:10.1097/PSY.0b013e31829b4525] [PMID]
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327(7414):557-60. [DOI:10.1136/bmj.327.7414.557] [PMID] [PMCID]
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997; 315(7109):629-34. [DOI:10.1136/bmj.315.7109.629] [PMID] [PMCID]
- Jennions MD, Lortie CJ, Rosenberg MS, Rothstein HR. Publication and related biases. In: Koricheva J, Gurevitch J, Mengersen K, editors. Handbook of meta-analysis in ecology and evolution. Princeton: Princeton University Press; 2013 [DOI:10.1515/9781400846184-016]
- Cooper SR, Jackson JJ, Barch DM, Braver TS. Neuroimaging of individual differences: A latent variable modeling perspective. Neuroscience and Biobehavioral Reviews. 2019; 98:29-46. [DOI:10.1016/j.neubiorev.2018.12.022] [PMID] [PMCID]
- Yanes JA, McKinnell ZE, Reid MA, Busler JN, Michel JS, Pangelinan MM, et al. Effects of cannabinoid administration for pain: A meta-analysis and meta-regression. Experimental and Clinical Psychopharmacology. 2019; 27(4):370-82. [DOI:10.1037/pha0000281] [PMID] [PMCID]
- Cumming G, Fidler F, Kalinowski P, Lai J. The statistical recommendations of the American Psychological Association Publication Manual: Effect sizes, confidence intervals, and meta-analysis. Australian Journal of Psychology. 2012; 64(3):138-46. [DOI:10.1037/pha0000281] [PMID] [PMCID]
- Bowden J, Tierney JF, Copas AJ, Burdett S. Quantifying, displaying and accounting for heterogeneity in the meta-analysis of RCTs using standard and generalised Q statistics. BMC Medical Research Methodology. 2011; 11:41. [DOI:10.1186/1471-2288-11-41] [PMID] [PMCID]
- Nakagawa S, Lagisz M, Jennions MD, Koricheva J, Noble DWA, Parker TH, et al. Methods for testing publication bias in ecological and evolutionary meta-analyses. Methods in Ecology and Evolution. 202; 13(1):4-21. [DOI:10.1111/2041-210X.13724]
- Alvarenga-Filho H, Sacramento PM, Ferreira TB, Hygino J, Abreu JEC, Carvalho SR, et al. Combined exercise training reduces fatigue and modulates the cytokine profile of T-cells from multiple sclerosis patients in response to neuromediators. Journal of Neuroimmunology. 2016; 293:91-99. [DOI:10.1016/j.jneuroim.2016.02.014] [PMID]
- Grazioli E, Tranchita E, Borriello G, Cerulli C, Minganti C, Parisi A. The effects of concurrent resistance and aerobic exercise training on functional status in patients with multiple sclerosis. Current Sports Medicine Reports. 2019; 18(12):452-7. [DOI:10.1249/JSR.0000000000000661] [PMID]
- Ozkul C, Guclu-Gunduz A, Irkec C, Fidan I, Aydin Y, Ozkan T, et al. Effect of combined exercise training on serum brain-derived neurotrophic factor, suppressors of cytokine signaling 1 and 3 in patients with multiple sclerosis. Journal of Neuroimmunology. 2018; 316:121-9. [DOI:10.1016/j.jneuroim.2018.01.002] [PMID]
- Sangelaji B, Nabavi SM, Estebsari F, Banshi MR, Rashidian H, Jamshidi E, et al. Effect of combination exercise therapy on walking distance, postural balance, fatigue and quality of life in multiple sclerosis patients: A clinical trial study. Iranian Red Crescent Medical Journal. 2014; 16(6):e17173. [DOI:10.5812/ircmj.17173] [PMID] [PMCID]
- Surakka J, Romberg A, Ruutiainen J, Aunola S, Virtanen A, Karppi SL, etv al. Effects of aerobic and strength exercise on motor fatigue in men and women with multiple sclerosis: A randomized controlled trial. Clinical Rehabilitation. 2004; 18(7):737-46. [DOI:10.1191/0269215504cr780oa] [PMID]
- Brañas P, Jordan R, Fry-Smith A, Burls A, Hyde C. Treatments for fatigue in multiple sclerosis: A rapid and systematic review. Health Technology Assessment. 2000; 4(27):1-61. [DOI:10.3310/hta4270] [PMID]
- Chiapeta AV, Oliveira CEP, Moraes AA, Moreira OC, Natali AJ, Carneiro-Júnior MA. Effects of resistance training on pain, functionality and quality of life in women with fibromyalgia: A systematic review. Journal of Bodywork and Movement Therapies. 2024; 40:761-8. [DOI:10.1016/j.jbmt.2024.05.014] [PMID]
- Garopoulou V, Meke M, Latsiou E, Papakonstantinou G, Mouzakidis C, Notas K, et al. The efficacy of different Aerobic, Pilates and combined therapeutic exercise protocols to functional capacity, fatigue and quality of life in adults with Multiple Sclerosis: Controlled experimental intervention Journal of Physical Activity, Nutrition and Rehabilitation. 2019; 554-72. [Link]
- Sangelaji B, Kordi M, Banihashemi F, Nabavi SM, Khodadadeh S, Dastoorpoor M. A combined exercise model for improving muscle strength, balance, walking distance, and motor agility in multiple sclerosis patients: A randomized clinical trial. Iranian Journal of Neurology. 2016; 15(3):111. [PMID]
- Torres-Costoso A, Martínez-Vizcaíno V, Reina-Gutiérrez S, Álvarez-Bueno C, Guzmán-Pavón MJ, Pozuelo-Carrascosa DP, et al. Effect of exercise on fatigue in multiple sclerosis: A network meta-analysis comparing different types of exercise. Archives of Physical Medicine and Rehabilitation. 2022; 103(5):970-87. [DOI:10.1016/j.apmr.2021.08.008] [PMID]
Type of Study: Research |
Subject:
General
Received: 2024/08/5 | Accepted: 2024/09/10 | Published: 2024/01/13
Received: 2024/08/5 | Accepted: 2024/09/10 | Published: 2024/01/13
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |