Thu, Jan 8, 2026
Volume 15, Issue 1 (Winter 2025)
PTJ 2025, 15(1): 51-58 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Yousefian molla R, Hajiahmad T, Kazemi R. Investigating Upper Extremity Function and Quality of Life Following Long-term Hand Biofeedback Electromyography Exercise in Elderly Stroke Patients. PTJ 2025; 15 (1) :51-58
URL: http://ptj.uswr.ac.ir/article-1-657-en.html
URL: http://ptj.uswr.ac.ir/article-1-657-en.html
1- Department of Sports Biomechanics, Faculty of of Physical Education and Sports Sciences, Central Tehran Branch, Islamic Azad University, Tehran, Iran.
2- Tabassom Stroke Rehabilitation Clinic, Tehran, Iran.
2- Tabassom Stroke Rehabilitation Clinic, Tehran, Iran.
Keywords: Cerebrovascular accident, Psychophysiological feedback, Function, Upper limb, Life quality
Full-Text [PDF 1062 kb]
(582 Downloads)
| Abstract (HTML) (2869 Views)
Full-Text: (545 Views)
Introduction
Stroke is the most common neurological disease that leads to death and disability [1]. The most common and broadest cause of disability in stroke is motor disability, which usually affects one side of the body and causes mutual functional disability of the brain [2]. After a stroke, a person usually becomes disabled in movement control and lag in movement and neurological skills; meanwhile, their adaptation and learning, and the implementation of new tasks of their movement program are disturbed [1]. Accordingly, disability after a stroke usually deprives patients of proper participation in daily life activities. It prevents them from social interactions [3] and as a result, it causes a decrease in the quality of life of these people [4]. In other words, following a stroke, patients’ work performance decreases, and they become incapable of meeting their expected needs and functional demands in their daily activities, such as self-care tasks, bathing, climbing the stairs, and achieving independence in life [5, 6].
Previous research indicates that functional disability following a stroke is more common in the upper limb than in the lower limb [7]. Damage to the middle cerebral artery, which supplies the majority of blood to the brain for upper limb and hand function affects stroke patients [1], leading to motor disability in the hands and upper limbs [3]. This disability significantly impacts daily life activities. Studies show that most stroke patients experience dysfunction in their hands or upper limbs, becoming dependent on daily activities [3, 8]. Furthermore, only some stroke patients with upper limb issues return to normal function, while others regain some abilities, and do not recover any normal upper limb function [9].
Rehabilitation is used to help stroke patients regain their previous social roles, improve their performance, reduce hospitalization time, decrease economic and social costs and achieve relative independence [10, 11, 12].
Recent advancements in science have led to the development of new rehabilitation techniques for stroke patients [8, 13, 14]. Biofeedback therapy is widely used as a treatment method for rehabilitating stroke patients [5, 6, 8]. Some authors have noted that biofeedback electromyography rehabilitation has positive effects on improving motor control and functional capacities in stroke patients [1]. This approach provides valuable physiological and physical performance information in areas that may be challenging to assess using other methods [2, 15]. Past research directly demonstrates the positive effects of this treatment method on post-stroke rehabilitation, including improvements in hand function, muscle strength, active range of motion, and motor skills [16, 17]. Some studies even suggest that biofeedback electromyography produces better results in upper limb function recovery, especially in hand-functional training for stroke patients, compared to physiotherapy and occupational therapy alone [4, 8, 18]. On the other hand, some studies maintain that using this method alone has no benefits [19], while others suggest that it does not affect overall health, range of motion, functional ability, or activity [8, 20].
This study examines the effects of long-term hand biofeedback therapy on the upper limb function and quality of life of elderly people who have had a stroke. There is a lack of comprehensive research in this area, hence, this study fills the and addresses any conflicting findings from previous studies.
Materials and Methods
This study was designed as a randomized controlled trial (RCT) with a causal-comparative approach, using a pre-test and post-test design. The subjects of the study were stroke patients who were referred to the rehabilitation clinic by a neurologist. The diagnosis of stroke was confirmed through clinical evaluations and brain imaging conducted by a neurologist. To be included in the study, the patients had to be over 60 years old, able to walk independently (showing proper movement return in the lower limb), be at the fourth stage of Branstrom for upper limb function [1] and have experienced the stroke more than a year before. Meanwhile, the exclusion criteria were cognitive disorders affecting communication, sensory disorders in the upper limb, history of upper limb surgery or fractures, and participation in a previous rehabilitation program for at least the last three months [3]. Patients voluntarily consented to participate by signing a written consent form and the entire treatment process was explained to them.
A total of 40 stroke patients were selected for this study based on the inclusion and exclusion criteria. They were divided into two groups using a double-blind process, namely a control group (10 men and 10 women) and an electromyography biofeedback training group (EMG-BF) (9 men, 11 women). All patients were initially evaluated for upper limb function and quality of life, and their scores were recorded. Rehabilitation sessions, with and without biofeedback exercises, were conducted by a specialist. After two years of treatment, post-test evaluations were performed to assess the impact of electromyography biofeedback training on upper limb function and quality of life for both groups.
The patients’ upper limb function and quality of life were assessed using the disabilities of the arm, shoulder, and hand (DASH) questionnaire [21] and the short form 36 health survey questionnaire (SF-36) before any intervention [22]. The DASH test is a reliable, valid, and responsive assessment tool designed to evaluate upper limb function. It consists of 30 self-report items and is used to measure the rate of upper limb disability and the impact of activity in individuals with upper limb musculoskeletal conditions. The final score ranges from 0 to 100, with a higher score indicating greater disability [21]. The SF-36 test is also a valid and reliable questionnaire used to assess the quality of life in different groups. It evaluates eight important concepts: Physical performance, role limitations due to physical health, bodily pain, general health, vitality, social functioning, role limitations due to emotional health and mental health. The score for this test ranges from 0 to 100, with a higher score indicating better overall health. This test is also recognized as valid for stroke patients and the elderly [22].
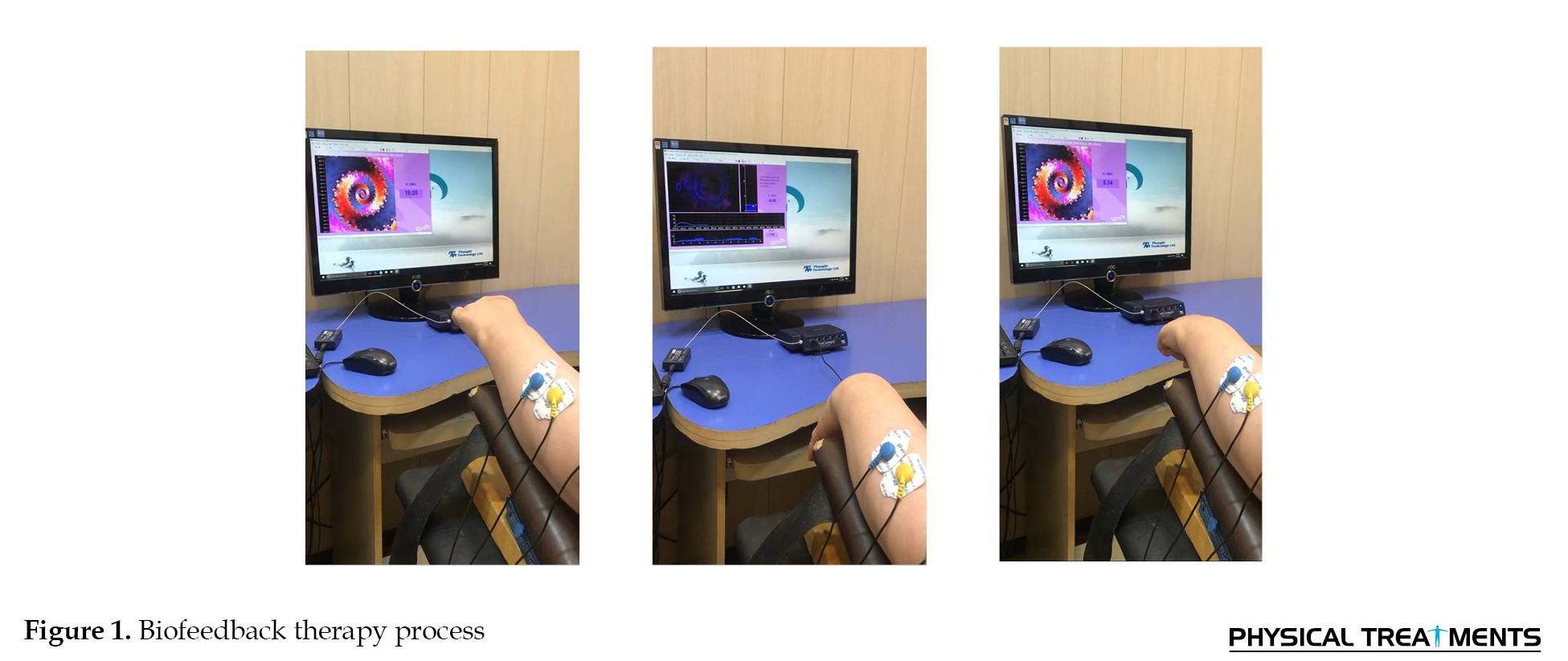
After the initial assessment, the control group’s patients underwent traditional rehabilitation for two years, with 5 weekly sessions, each lasting about 60 min. The rehabilitation program included manual therapy techniques, such as passive and active motion, mobilization, stretching, proprioceptive neuromuscular facilitation, and the rood approach [23]. The intervention group received a similar rehabilitation program, but with the addition of EMG-BF exercises for 15 min at the end of each session. Before starting the exercise protocol, the rehabilitation specialist evaluated the voluntary muscle contraction of all patients. Each patient had a training session to become familiar with the biofeedback device and treatment. During the treatment session, the patient sat 1 m away from the computer monitor and had surface EMG-BF sensors attached to the skin on the extensor muscles of the wrist and fingers. The patient was then asked to contract these muscles for 5 s, followed by 10 s of rest, and this cycle was repeated for 15 min during each session [24] (Figure 1). The SPSS software, version 22, was used for statistical analysis. Descriptive statistics, such as Mean±SD for two groups were analyzed. The Shapiro-Wilk test was used to check if the data had a normal distribution. To examine the impact of long-term biofeedback exercises on the quality of life and DASH in cerebrovascular accident people before and after the exercises, an inferential paired t-test with a significance level of P≤0.05 was used.
Results
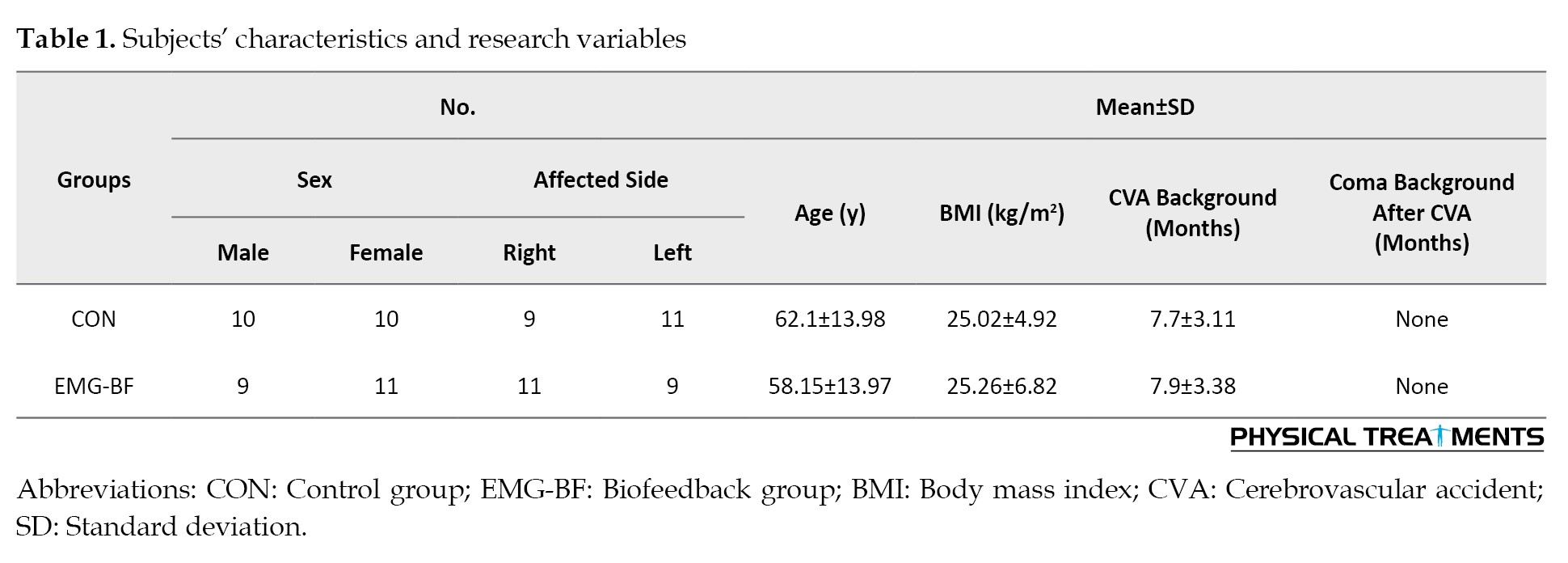
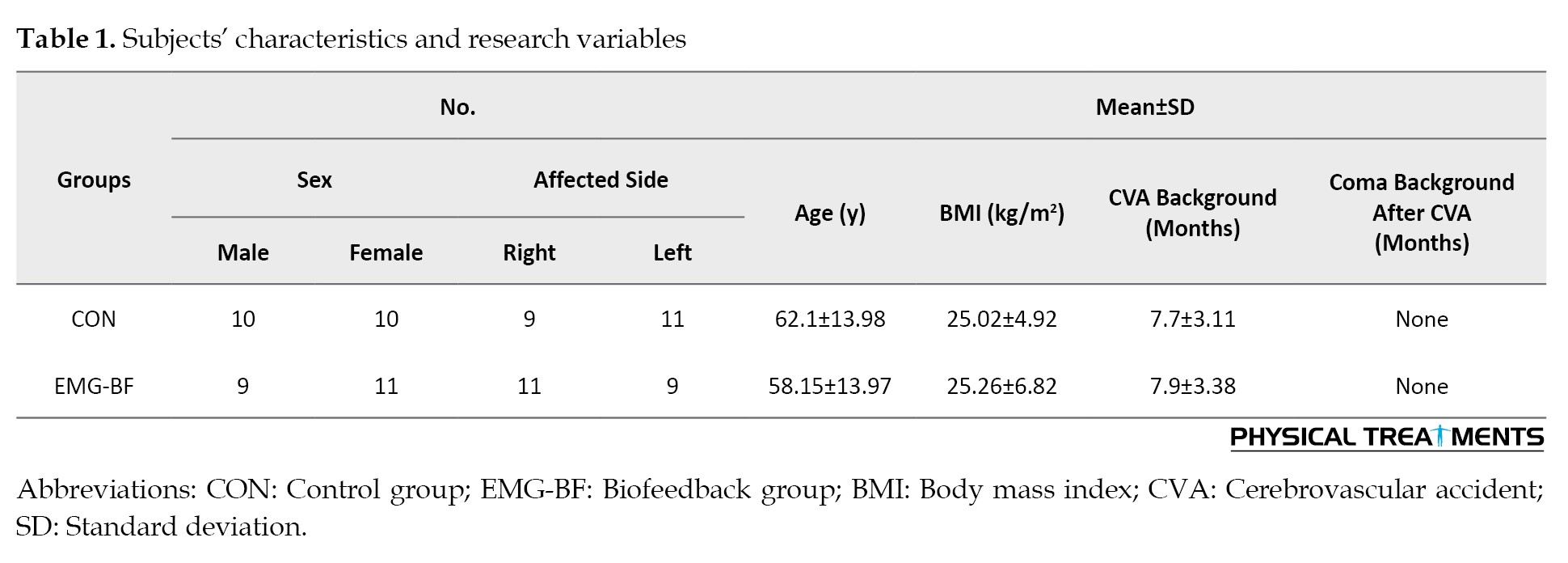
The results of descriptive statistics for the subjects’ characteristics and research variables can be found in Table 1.
The test for data normality indicated that the data had a normal distribution.
Table 2 displays the results of the paired t-test and the impact of long-term EMG-BF innervations on upper extremity function and quality of life in stroke patients.
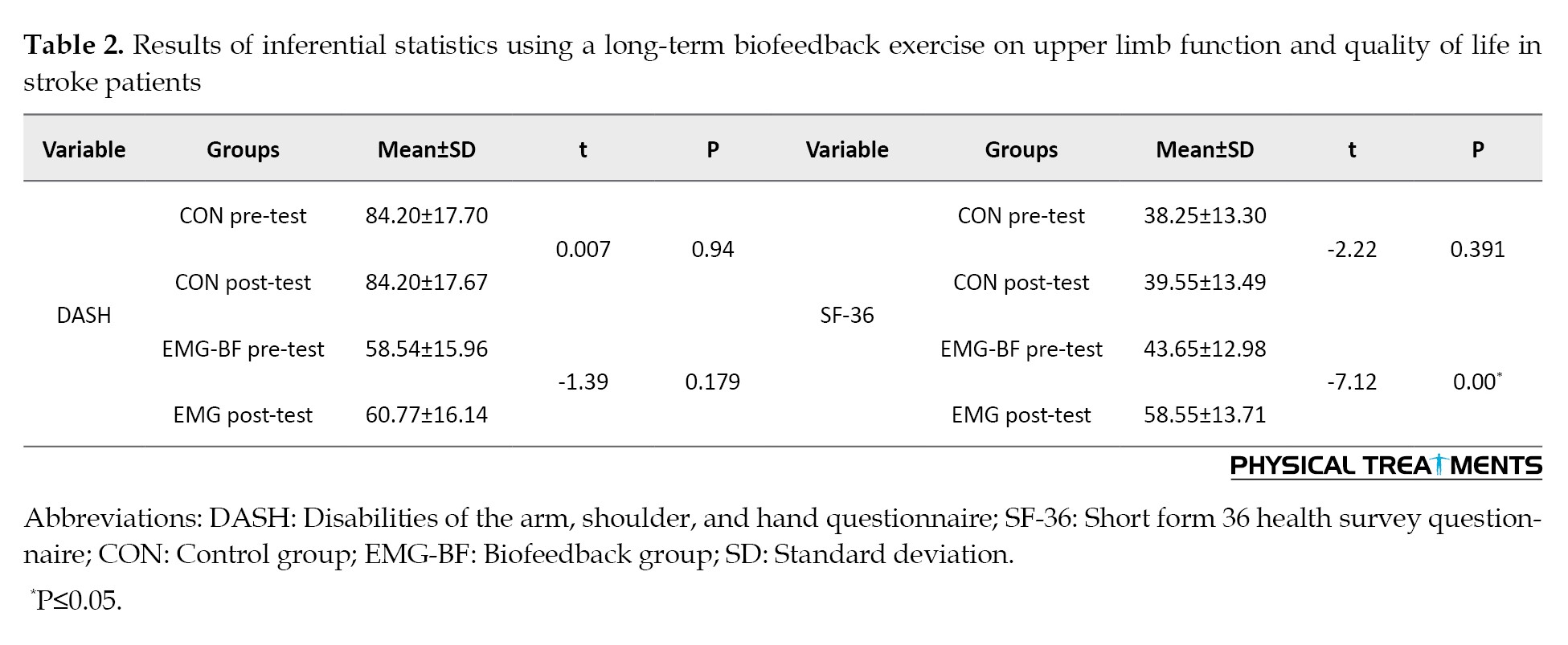
Accordingly, there was no significant difference in upper extremity function in both the control (P=0.94) and EMG-BF groups (P=0.179) after two years. However, there was no noticeable difference in the quality of life of the control group (P=0.391). There was a significant difference after long-term use of EMG-BF (P=0.00) in the intervention group (P≤0.05).
Discussion
This study investigated the impact of long-term biofeedback training on the upper limb function and quality of life of stroke patients. The results indicated that after two years of hand biofeedback, only the quality of life improved, while the function of the upper limb did not show significant changes.
Long-term stroke rehabilitation is a significant research topic [25]. Different methods have varying effects on patients’ performance and quality of life [25]. Previous research has looked at the impact of biofeedback exercises on stroke patients [26, 27], with some focusing on long-term use [28, 29]. However, there has been no direct study specifically investigating the long-term effects of hand biofeedback on upper limb function and quality of life, as discussed in this article. Some previous studies have compared the effects of using biofeedback on upper limb function in stroke patients, showing varying results consistent and inconsistent with the present study [20, 28, 30]. A systematic review study found that biofeedback was effective only in shoulder abduction and did not directly impact other upper limb movements [30]. In our study, we did not specifically look into shoulder abduction. The findings indicated that biofeedback did not have a direct impact on upper limb function, particularly the shoulder. Meanwhile, in a study similar to this study, a combined biofeedback and rehabilitation program was effective for stroke patients. However, the evaluation method used in most of the reviewed studies differs from the functional test of the DASH [31]. Furthermore, a meta-analysis study showed that biofeedback has a positive effect on the evaluation of some upper limb tests, but in evaluations, such as functional independence measure, consistent with the present study, it has no effect [26]. Several studies have highlighted the positive impact of utilizing biofeedback on hand function [17, 27], However, as the present research focuses on the entire function of the upper limb, it is not possible to directly align with these two studies. On the other hand, a study closely related to the current research compared the short-term and long-term effects of using biofeedback on stroke. It acknowledged that biofeedback has a positive short-term effect on stroke factors but has no long-term impact [28].
The positive effects of biofeedback on the quality of life of people with various complications have been confirmed [32, 33]. There have been several studies examining the impact of biofeedback on the quality of life of individuals who have had a stroke [27, 30], However, none of these studies have considered the long-term effects of this intervention. One study [30] looked at the effect of biofeedback on hemiplegic stroke patients and found that the quality of life for stroke survivors did not improve significantly after just five weeks of biofeedback. These results were inconsistent with the findings of our research, which is likely one of the reasons for the lack of agreement, and our research also looked at the long-term use of the biofeedback method. However, day 14 and day 16 showed a positive effect that was consistent with our study regarding the impact of biofeedback on the quality of life of the elderly, even when used for a short time.
The results of this research can be justified as not all factors affecting quality of life are linked to shoulder function. Quality of life encompasses a wide range of variables for improvement. This study only examined the impact of biofeedback and does not necessarily mean that all rehabilitation methods would have the same results. Additionally, the biofeedback method used in the study focused solely on the hands. Improving hand and finger function can directly impact quality of life, which may not be directly tied to shoulder function. For example, some stroke patients may have shoulder function issues but still have adequate mobility in the lower part of the upper limb, allowing them to perform daily activities reasonably.
Conclusion
Long-term use of the biofewedback exercise method in stroke patients primarily impacts their quality of life rather than significantly affecting the function of their upper limbs. Therefore, it is advisable to incorporate biofeedback as a complementary treatment in long-term rehabilitation, focusing on improving these patients’ overall quality of life.
One of the main limitations of our research is the limited number of samples for examination and the use of the biofeedback training method for less than 2 years. This is something we hope will be considered in future research.
Ethical Considerations
Compliance with ethical guidelines
The study protocol was approved by the Ethics Committee of the Kinesiology Research Center of Kharazmi University, Tehran, Iran (Code: IR-KHU.KRC.1000.232).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interpretation of the results and drafting of the manuscript. Each author approved the final version of the manuscript for submission.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The author would like to thank Tabassom Rehabilitation Stroke Clinic for its support and also patients participating in this study.
Stroke is the most common neurological disease that leads to death and disability [1]. The most common and broadest cause of disability in stroke is motor disability, which usually affects one side of the body and causes mutual functional disability of the brain [2]. After a stroke, a person usually becomes disabled in movement control and lag in movement and neurological skills; meanwhile, their adaptation and learning, and the implementation of new tasks of their movement program are disturbed [1]. Accordingly, disability after a stroke usually deprives patients of proper participation in daily life activities. It prevents them from social interactions [3] and as a result, it causes a decrease in the quality of life of these people [4]. In other words, following a stroke, patients’ work performance decreases, and they become incapable of meeting their expected needs and functional demands in their daily activities, such as self-care tasks, bathing, climbing the stairs, and achieving independence in life [5, 6].
Previous research indicates that functional disability following a stroke is more common in the upper limb than in the lower limb [7]. Damage to the middle cerebral artery, which supplies the majority of blood to the brain for upper limb and hand function affects stroke patients [1], leading to motor disability in the hands and upper limbs [3]. This disability significantly impacts daily life activities. Studies show that most stroke patients experience dysfunction in their hands or upper limbs, becoming dependent on daily activities [3, 8]. Furthermore, only some stroke patients with upper limb issues return to normal function, while others regain some abilities, and do not recover any normal upper limb function [9].
Rehabilitation is used to help stroke patients regain their previous social roles, improve their performance, reduce hospitalization time, decrease economic and social costs and achieve relative independence [10, 11, 12].
Recent advancements in science have led to the development of new rehabilitation techniques for stroke patients [8, 13, 14]. Biofeedback therapy is widely used as a treatment method for rehabilitating stroke patients [5, 6, 8]. Some authors have noted that biofeedback electromyography rehabilitation has positive effects on improving motor control and functional capacities in stroke patients [1]. This approach provides valuable physiological and physical performance information in areas that may be challenging to assess using other methods [2, 15]. Past research directly demonstrates the positive effects of this treatment method on post-stroke rehabilitation, including improvements in hand function, muscle strength, active range of motion, and motor skills [16, 17]. Some studies even suggest that biofeedback electromyography produces better results in upper limb function recovery, especially in hand-functional training for stroke patients, compared to physiotherapy and occupational therapy alone [4, 8, 18]. On the other hand, some studies maintain that using this method alone has no benefits [19], while others suggest that it does not affect overall health, range of motion, functional ability, or activity [8, 20].
This study examines the effects of long-term hand biofeedback therapy on the upper limb function and quality of life of elderly people who have had a stroke. There is a lack of comprehensive research in this area, hence, this study fills the and addresses any conflicting findings from previous studies.
Materials and Methods
This study was designed as a randomized controlled trial (RCT) with a causal-comparative approach, using a pre-test and post-test design. The subjects of the study were stroke patients who were referred to the rehabilitation clinic by a neurologist. The diagnosis of stroke was confirmed through clinical evaluations and brain imaging conducted by a neurologist. To be included in the study, the patients had to be over 60 years old, able to walk independently (showing proper movement return in the lower limb), be at the fourth stage of Branstrom for upper limb function [1] and have experienced the stroke more than a year before. Meanwhile, the exclusion criteria were cognitive disorders affecting communication, sensory disorders in the upper limb, history of upper limb surgery or fractures, and participation in a previous rehabilitation program for at least the last three months [3]. Patients voluntarily consented to participate by signing a written consent form and the entire treatment process was explained to them.
A total of 40 stroke patients were selected for this study based on the inclusion and exclusion criteria. They were divided into two groups using a double-blind process, namely a control group (10 men and 10 women) and an electromyography biofeedback training group (EMG-BF) (9 men, 11 women). All patients were initially evaluated for upper limb function and quality of life, and their scores were recorded. Rehabilitation sessions, with and without biofeedback exercises, were conducted by a specialist. After two years of treatment, post-test evaluations were performed to assess the impact of electromyography biofeedback training on upper limb function and quality of life for both groups.
The patients’ upper limb function and quality of life were assessed using the disabilities of the arm, shoulder, and hand (DASH) questionnaire [21] and the short form 36 health survey questionnaire (SF-36) before any intervention [22]. The DASH test is a reliable, valid, and responsive assessment tool designed to evaluate upper limb function. It consists of 30 self-report items and is used to measure the rate of upper limb disability and the impact of activity in individuals with upper limb musculoskeletal conditions. The final score ranges from 0 to 100, with a higher score indicating greater disability [21]. The SF-36 test is also a valid and reliable questionnaire used to assess the quality of life in different groups. It evaluates eight important concepts: Physical performance, role limitations due to physical health, bodily pain, general health, vitality, social functioning, role limitations due to emotional health and mental health. The score for this test ranges from 0 to 100, with a higher score indicating better overall health. This test is also recognized as valid for stroke patients and the elderly [22].
After the initial assessment, the control group’s patients underwent traditional rehabilitation for two years, with 5 weekly sessions, each lasting about 60 min. The rehabilitation program included manual therapy techniques, such as passive and active motion, mobilization, stretching, proprioceptive neuromuscular facilitation, and the rood approach [23]. The intervention group received a similar rehabilitation program, but with the addition of EMG-BF exercises for 15 min at the end of each session. Before starting the exercise protocol, the rehabilitation specialist evaluated the voluntary muscle contraction of all patients. Each patient had a training session to become familiar with the biofeedback device and treatment. During the treatment session, the patient sat 1 m away from the computer monitor and had surface EMG-BF sensors attached to the skin on the extensor muscles of the wrist and fingers. The patient was then asked to contract these muscles for 5 s, followed by 10 s of rest, and this cycle was repeated for 15 min during each session [24] (Figure 1). The SPSS software, version 22, was used for statistical analysis. Descriptive statistics, such as Mean±SD for two groups were analyzed. The Shapiro-Wilk test was used to check if the data had a normal distribution. To examine the impact of long-term biofeedback exercises on the quality of life and DASH in cerebrovascular accident people before and after the exercises, an inferential paired t-test with a significance level of P≤0.05 was used.
Results
The results of descriptive statistics for the subjects’ characteristics and research variables can be found in Table 1.
The test for data normality indicated that the data had a normal distribution.
Table 2 displays the results of the paired t-test and the impact of long-term EMG-BF innervations on upper extremity function and quality of life in stroke patients.
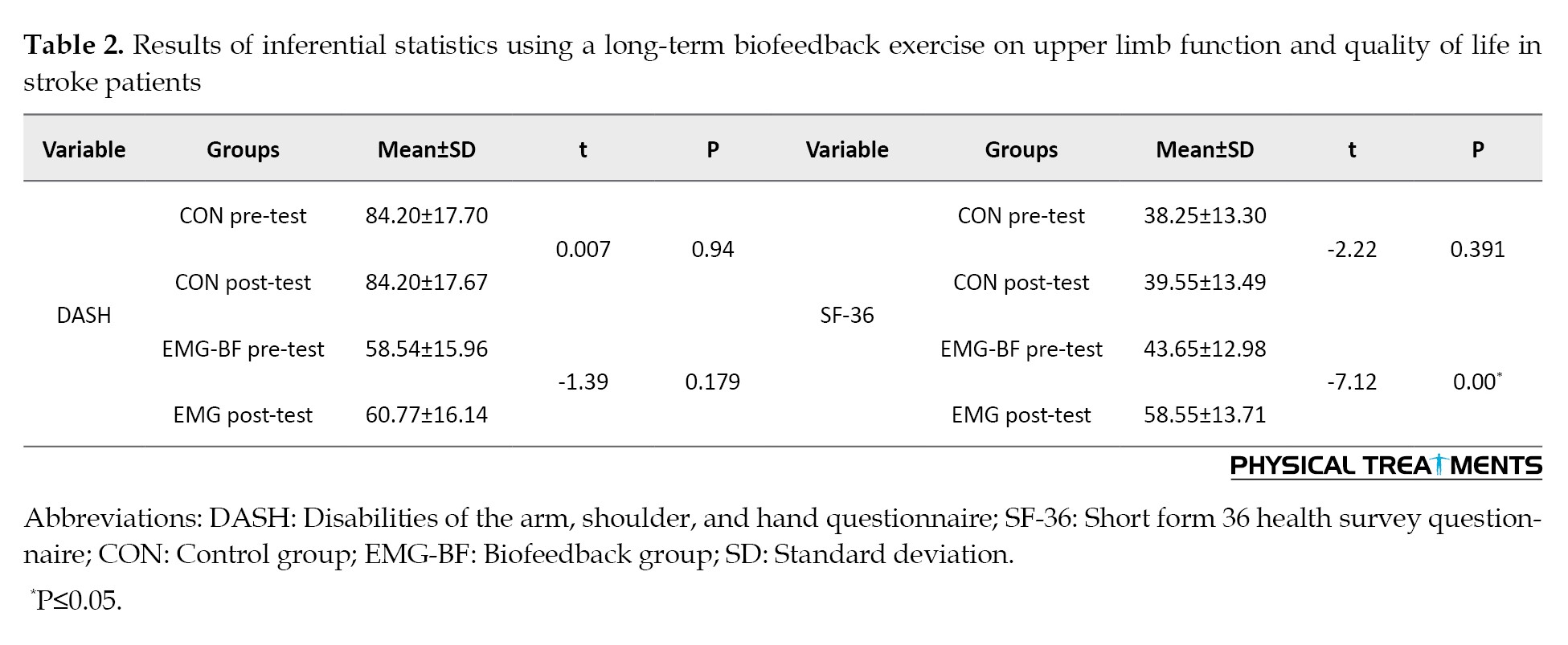
Accordingly, there was no significant difference in upper extremity function in both the control (P=0.94) and EMG-BF groups (P=0.179) after two years. However, there was no noticeable difference in the quality of life of the control group (P=0.391). There was a significant difference after long-term use of EMG-BF (P=0.00) in the intervention group (P≤0.05).
Discussion
This study investigated the impact of long-term biofeedback training on the upper limb function and quality of life of stroke patients. The results indicated that after two years of hand biofeedback, only the quality of life improved, while the function of the upper limb did not show significant changes.
Long-term stroke rehabilitation is a significant research topic [25]. Different methods have varying effects on patients’ performance and quality of life [25]. Previous research has looked at the impact of biofeedback exercises on stroke patients [26, 27], with some focusing on long-term use [28, 29]. However, there has been no direct study specifically investigating the long-term effects of hand biofeedback on upper limb function and quality of life, as discussed in this article. Some previous studies have compared the effects of using biofeedback on upper limb function in stroke patients, showing varying results consistent and inconsistent with the present study [20, 28, 30]. A systematic review study found that biofeedback was effective only in shoulder abduction and did not directly impact other upper limb movements [30]. In our study, we did not specifically look into shoulder abduction. The findings indicated that biofeedback did not have a direct impact on upper limb function, particularly the shoulder. Meanwhile, in a study similar to this study, a combined biofeedback and rehabilitation program was effective for stroke patients. However, the evaluation method used in most of the reviewed studies differs from the functional test of the DASH [31]. Furthermore, a meta-analysis study showed that biofeedback has a positive effect on the evaluation of some upper limb tests, but in evaluations, such as functional independence measure, consistent with the present study, it has no effect [26]. Several studies have highlighted the positive impact of utilizing biofeedback on hand function [17, 27], However, as the present research focuses on the entire function of the upper limb, it is not possible to directly align with these two studies. On the other hand, a study closely related to the current research compared the short-term and long-term effects of using biofeedback on stroke. It acknowledged that biofeedback has a positive short-term effect on stroke factors but has no long-term impact [28].
The positive effects of biofeedback on the quality of life of people with various complications have been confirmed [32, 33]. There have been several studies examining the impact of biofeedback on the quality of life of individuals who have had a stroke [27, 30], However, none of these studies have considered the long-term effects of this intervention. One study [30] looked at the effect of biofeedback on hemiplegic stroke patients and found that the quality of life for stroke survivors did not improve significantly after just five weeks of biofeedback. These results were inconsistent with the findings of our research, which is likely one of the reasons for the lack of agreement, and our research also looked at the long-term use of the biofeedback method. However, day 14 and day 16 showed a positive effect that was consistent with our study regarding the impact of biofeedback on the quality of life of the elderly, even when used for a short time.
The results of this research can be justified as not all factors affecting quality of life are linked to shoulder function. Quality of life encompasses a wide range of variables for improvement. This study only examined the impact of biofeedback and does not necessarily mean that all rehabilitation methods would have the same results. Additionally, the biofeedback method used in the study focused solely on the hands. Improving hand and finger function can directly impact quality of life, which may not be directly tied to shoulder function. For example, some stroke patients may have shoulder function issues but still have adequate mobility in the lower part of the upper limb, allowing them to perform daily activities reasonably.
Conclusion
Long-term use of the biofewedback exercise method in stroke patients primarily impacts their quality of life rather than significantly affecting the function of their upper limbs. Therefore, it is advisable to incorporate biofeedback as a complementary treatment in long-term rehabilitation, focusing on improving these patients’ overall quality of life.
One of the main limitations of our research is the limited number of samples for examination and the use of the biofeedback training method for less than 2 years. This is something we hope will be considered in future research.
Ethical Considerations
Compliance with ethical guidelines
The study protocol was approved by the Ethics Committee of the Kinesiology Research Center of Kharazmi University, Tehran, Iran (Code: IR-KHU.KRC.1000.232).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interpretation of the results and drafting of the manuscript. Each author approved the final version of the manuscript for submission.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The author would like to thank Tabassom Rehabilitation Stroke Clinic for its support and also patients participating in this study.
References
- Lirio-Romero C, Torres-Lacomba M, Gómez-Blanco A, Acero-Cortés A, Retana-Garrido A, de la Villa-Polo P, et al. Electromyographic biofeedback improves upper extremity function: A randomized, single-blinded, controlled trial. Physiotherapy. 2021; 110:54-62. [DOI:10.1016/j.physio.2020.02.002] [PMID]
- Zadnia A, Kobravi HR, Sheikh M, Asghar Hosseini H. Generating the visual biofeedback signals applicable to reduction of wrist spasticity: A pilot study on stroke patients. Basic and Clinical Neuroscience. 2018; 9(1):15-26. [DOI:10.29252/nirp.bcn.9.1.15] [PMID] [PMCID]
- Doğan-Aslan M, Nakipoğlu-Yüzer GF, Doğan A, Karabay I, Özgirgin N. The effect of electromyographic biofeedback treatment in improving upper extremity functioning of patients with hemiplegic stroke. Journal of Stroke and Cerebrovascular Diseases. 2012; 21(3):187-92. [DOI:10.1016/j.jstrokecerebrovasdis.2010.06.006] [PMID]
- Moreland J, Thomson MA. Efficacy of electromyographic biofeedback compared with conventional physical therapy for upper-extremity function in patients following stroke: A research overview and meta-analysis. Physical Therapy. 1994;74(6):534-43. [DOI:10.1093/ptj/74.6.534] [PMID]
- Park BR, Lee MY, Jeong HC, Lee SS, Kim YK. FES-assisted biofeedback system for upper extremity in chronic hemiplegia. Paper presented at: 11th Annual Conference of the International FES Society. 1 September 2006; Zao, Japan. [Link]
- Sturma A, Hruby LA, Prahm C, Mayer JA, Aszmann OC. Rehabilitation of upper extremity nerve injuries using surface EMG biofeedback: Protocols for clinical application. Frontiers in Neuroscience. 2018; 12:906. [DOI:10.3389/fnins.2018.00906] [PMID] [PMCID]
- De Baets L, Van Deun S, Monari D, Jaspers E. Three-dimensional kinematics of the scapula and trunk, and associated scapular muscle timing in individuals with stroke. Human Movement Science. 2016; 48:82-90. [DOI:10.1016/j.humov.2016.04.009] [PMID]
- Kim JH. The effects of training using EMG biofeedback on stroke patients upper extremity functions. Journal of Physical Therapy Science. 2017; 29(6):1085-8. [DOI:10.1589/jpts.29.1085] [PMID] [PMCID]
- Kamonseki DH, Calixtre LB, Barreto RPG, Camargo PR. Effects of electromyographic biofeedback interventions for shoulder pain and function: Systematic review and meta-analysis. Clinical Rehabilitation. 2021; 35(7):952-63. [DOI:10.1177/0269215521990950] [PMID]
- Witney AG, Wing A, Thonnard JL, Smith AM. The cutaneous contribution to adaptive precision grip. Trends in Neurosciences. 2004; 27(10):637-43. [DOI:10.1016/j.tins.2004.08.006] [PMID]
- Uswatte G, Taub E, Morris D, Light K, Thompson P. The Motor Activity Log-28: Assessing daily use of the hemiparetic arm after stroke. Neurology. 2006; 67(7):1189-94. [DOI:10.1212/01.wnl.0000238164.90657.c2] [PMID]
- Harishchandre MS, Singaravelan R. Effectiveness of emg biofeedback on improving hand function in hemiplegic stroke patients. Romanian Journal of Physical Therapy/Revista Romana de Kinetoterapie. 2012; 18(30):57-64. [Link]
- Rattanatharn R. Effect of EMG biofeedback to improve upper extremity in children with cerebral palsy: A randomized controlled trail. Chulalongkorn Medical Journal. 2017; 61(4):451-63. [DOI:10.58837/CHULA.CMJ.61.4.4]
- Wolf SL, Binder-Macleod SA. Electromyographic biofeedback applications to the hemiplegic patient: Changes in lower extremity neuromuscular and functional status. Physical Therapy. 1983; 63(9):1404-13. [DOI:10.1093/ptj/63.9.1404]
- Zhang T, Lu J, Hu F, Wu L, Guo M. A sensor-based virtual piano biofeedback system for stroke rehabilitation. Paper presented at: IEEE Global Humanitarian Technology Conference (GHTC 2014); 13 October 2014; San Jose, USA. [Link]
- Stanton R, Ada L, Dean CM, Preston E. Biofeedback improves activities of the lower limb after stroke: A systematic review.Journal of Physiotherapy. 2011; 57(3):145-55. [DOI:10.1016/S1836-9553(11)70035-2] [PMID]
- Pollock A, Farmer SE, Brady MC, Langhorne P, Mead GE, Mehrholz J, et al. Interventions for improving upper limb function after stroke. Cochrane Database of Systematic Reviews. 2014; 11. [DOI:10.1002/14651858.CD010820.pub2]
- Greenberg S, Fowler RS Jr. Kinesthetic biofeedback: A treatment modality for elbow range of motion in hemiplegia. The American Journal of Occupational Therapy. 1980; 34(11):738-43. [DOI:10.5014/ajot.34.11.738] [PMID]
- Kim YK, Song JC, Choi JW, Kim JH, Hwang YT. Functional electric stimulation-assisted biofeedback therapy system for chronic hemiplegic upper extremity function. Journal of Korean Physical Therapy. 2012; 24(6):409-13. [Link]
- Cordo P, Wolf S, Lou JS, Bogey R, Stevenson M, Hayes J, Roth E. Treatment of severe hand impairment following stroke by combining assisted movement, muscle vibration, and biofeedback. Journal of Neurologic Physical Therapy. 2013; 37(4):194-203. [DOI:10.1097/NPT.0000000000000023] [PMID]
- Dalton E, Lannin NA, Laver K, Ross L, Ashford S, McCluskey A, et al. Validity, reliability and ease of use of the disabilities of arm, shoulder and hand questionnaire in adults following stroke. Disability and Rehabilitation. 2017; 39(24):2504-11. [DOI:10.1080/09638288.2016.1229364] [PMID]
- Hobart JC, Williams LS, Moran K, Thompson AJ. Quality of life measurement after stroke: Uses and abuses of the SF-36. Stroke. 2002; 33(5):1348-56. [DOI:10.1161/01.STR.0000015030.59594.B3] [PMID]
- Harvey RL, Macko RF, Stein J, Winstein CJ, Phd P, Zorowitz RD. Stroke recovery and rehabilitation. New York: Demos Medical Publishing; 2008. [Link]
- Andrasik F, Schwartz MS. Biofeedback: A practitioner’s guide: Guilford Publications; 2017. [Link]
- Teasell R, Mehta S, Pereira S, McIntyre A, Janzen S, Allen L, et al. Time to rethink long-term rehabilitation management of stroke patients. Topics in Stroke Rehabilitation. 2012; 19(6):457-62. [DOI:10.1310/tsr1906-457] [PMID]
- Bonini-Rocha AC, de Andrade ALS, Santos Pereira RD, de Moraes AM, Matheus LBG, da Fonseca ST, et al. Biofeedback interventions for short term upper limb function following stroke: A systematic review with meta-analysis. Journal of Hand Therapy. 2023; 36(3):693-705. [DOI:10.1016/j.jht.2022.05.001] [PMID]
- Kotov SV, Isakova EV, Egorova YV. [The impact of a comprehensive support response biofeedback program on patient recovery and quality of life after stroke (Persian)]. Zhurnal nevrologii i psikhiatrii imeni S.S. Korsakova. 2022; 122(10):88-95. [DOI:10.17116/jnevro202212210188] [PMID]
- Teran-Yengle P, Cole KJ, Yack HJ. Short and long-term effects of gait retraining using real-time biofeedback to reduce knee hyperextension pattern in young women. Gait & Posture. 2016; 50:185-9. [DOI:10.1016/j.gaitpost.2016.08.019] [PMID]
- Flor H, Haag G, Turk DC. Long-term efficacy of EMG biofeedback for chronic rheumatic back pain. Pain. 1986; 27(2):195-202. [DOI:10.1016/0304-3959(86)90210-1] [PMID]
- Glanz M, Klawansky S, Stason W, Berkey C, Shah N, Phan H, et al. Biofeedback therapy in poststroke rehabilitation: A meta-analysis of the randomized controlled trials. Archives of Physical Medicine and Rehabilitation. 1995; 76(6):508-15. [DOI:10.1016/S0003-9993(95)80503-6] [PMID]
- Feng S, Tang M, Huang G, Wang J, He S, Liu D, et al. EMG biofeedback combined with rehabilitation training may be the best physical therapy for improving upper limb motor function and relieving pain in patients with the post-stroke shoulder-hand syndrome: A Bayesian network meta-analysis. Frontiers in Neurology. 2023; 13:1056156. [DOI:10.3389/fneur.2022.1056156] [PMID] [PMCID]
- Wagner B, Steiner M, Huber DFX, Crevenna R. The effect of biofeedback interventions on pain, overall symptoms, quality of life and physiological parameters in patients with pelvic pain: A systematic review. Wiener Klinische Wochenschrift. 2022; 134(Suppl 1):11-48. [DOI:10.1007/s00508-021-01827-w] [PMID] [PMCID]
- Marin-Pardo O, Donnelly MR, Phanord CS, Wong K, Liew SL. Improvements in motor control are associated with improved quality of life following an at-home muscle biofeedback program for chronic stroke. Frontiers in Human Neuroscience. 2024; 18:1356052. [DOI:10.3389/fnhum.2024.1356052] [PMID] [PMCID]
Type of Study: Research |
Subject:
General
Received: 2024/07/11 | Accepted: 2024/09/15 | Published: 2024/01/13
Received: 2024/07/11 | Accepted: 2024/09/15 | Published: 2024/01/13
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |