Tue, Nov 18, 2025
Volume 15, Issue 2 (Spring 2025)
PTJ 2025, 15(2): 111-118 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Jafarnezhadgero A, Hamlabadi M P, Fakhri Mirzanag E, Orouji A, Letafatkar A. Impact of Movement Pattern Training on Muscular Co-contraction in Patients With Low Back Pain During Walking. PTJ 2025; 15 (2) :111-118
URL: http://ptj.uswr.ac.ir/article-1-636-en.html
URL: http://ptj.uswr.ac.ir/article-1-636-en.html
AmirAli Jafarnezhadgero *1 

 , Milad Piran Hamlabadi2
, Milad Piran Hamlabadi2 

 , Ehsan Fakhri Mirzanag2
, Ehsan Fakhri Mirzanag2 

 , Afshin Orouji3
, Afshin Orouji3 
 , Amir Letafatkar3
, Amir Letafatkar3 




 , Milad Piran Hamlabadi2
, Milad Piran Hamlabadi2 

 , Ehsan Fakhri Mirzanag2
, Ehsan Fakhri Mirzanag2 

 , Afshin Orouji3
, Afshin Orouji3 
 , Amir Letafatkar3
, Amir Letafatkar3 


1- Department of Sport Management and Biomechanics, Faculty of Education Sciences and Psychology, University of Mohaghegh Ardabili, Ardabil, Iran.
2- Department of Physical Education and Sport Sciences, Faculty of Education Sciences and Psychology, University of Mohaghegh Ardabili, Ardabil, Iran.
3- Department of Corrective Exercise and Sports Injuries, School of Physical Education and Sport Sciences, University of Kharazmi, Tehran, Iran.
2- Department of Physical Education and Sport Sciences, Faculty of Education Sciences and Psychology, University of Mohaghegh Ardabili, Ardabil, Iran.
3- Department of Corrective Exercise and Sports Injuries, School of Physical Education and Sport Sciences, University of Kharazmi, Tehran, Iran.
Full-Text [PDF 478 kb]
(471 Downloads)
| Abstract (HTML) (2313 Views)
Full-Text: (307 Views)
Introduction
Low back pain (LBP) occurs in about 80% of people in their lifetime [1]. In 2015, approximately 7.3% of the population worldwide experienced activity limitations due to LBP [2]. LBP begins at 20 and 40 [2], with a high prevalence observed between 30 and 60 [3]. As a result, LBP is a common health problem that primary care settings frequently encounter [4]. LBP is associated with alterations in walking mechanics [3]. Excess foot pronation during the loading phase of walking can cause disrupted lower limb alignments and, ultimately LBP [5]. The trunk has been conceptualized as a pendulum [6]. As a result, the trunk-lower limb system is essential for the spine as a kinematic chain. This system consists of several parts and joints affecting the lumbar area and lower limb interaction while moving. Any dysfunction impacting this complex can disturb this connection, resulting in atypical motion. Different walking problems, like shorter steps and stiff coordination between body sections, are observed in people suffering from LBP [7].
The co-contraction of knee muscles is a mechanism for modifying joint stability and loading [8]. Individuals with LBP may show changed simultaneous contraction of lower limb muscles when walking. Generalized co-contraction is the simultaneous activation of all knee muscle groups [9]. Wang et al. reported that patients with lumbar disk herniation show enhanced biceps femoris root mean square at the stance phase. Positive relationships have been reported between tibialis anterior and gastrocnemius co-contraction and the disability index [10].
One common complication of this condition can be altered movement patterns during walking, leading to increased co-contraction of knee and ankle muscles [11]. Despite existing interventions, such as movement pattern training, the impact of these interventions on reducing knee and ankle muscular co-contraction in patients with non-specific chronic LBP (NSCLBP) during walking remains poorly understood. Movement pattern training is a therapeutic exercise that improves movement quality, coordination, and efficiency [12]. The training involves specific exercises and techniques designed to retrain and optimize movement patterns to enhance functional performance and reduce the risk of injury [13]. Movement pattern training addresses faulty movement patterns, postural imbalances, muscle imbalances, and improper biomechanics to help individuals move more effectively and efficiently [14]. This type of training can be beneficial for improving sports performance, rehabilitation from injuries, and enhancing overall movement quality in daily activities [14]. However, there is a need to assess the effect of movement pattern exercises in addressing this specific issue to improve the management and outcomes of NSCLBP. Therefore, this study aims to investigate the impact of movement pattern training on general lower limb muscular co-contraction at walking in patients with NSCLBP.
Materials and Methods
Study design and participants
This research was conducted with the ethical code of IR.SBU.REC.1399.060), and registration number of IRCT20181024041444N1. Informed consent was received from all samples. The study recruited 40 male patients with LBP from local clinics. The G*power software, version 3.1.9.7, was used to estimate the required sample size [15]. The software determined that at least 40 participants would be needed. The subjects were divided into intervention (EG, n=20) and control (CG, n=20) groups. The inclusion criteria were as follows: Pain persisting >3 months, visual analog scale >3 cm, and disability index of >10 [16]. The exclusion criteria were as follows: LBP of traumatic origin, history of surgery, and musculoskeletal misalignments [17].
The eligible participants were allocated into both groups using the block randomization method [18].
Training protocol
The exercise protocol used in this study was based on that introduced by Harris-Hayes et al. [19]. All the participants belonging to the EG underwent a total of 18 training sessions for 6 weeks. The movement pattern training program incorporated two primary components: Task-specific exercise (e.g. based on walking) for specific tasks and hip musculature strengthening.
Participants were instructed to start with a minimum number of exercise repetitions, gradually increasing as tolerated, ensuring correct execution and the absence of hip pain. At each visit, a therapist evaluated the performance of specific functional tasks and strength exercises, focusing on mastery for autonomous practice. Functional independence required patients to replicate modified lower limb movements accurately. Once achieved, no further guidance was issued, but patients were advised to maintain these patterns in daily activities. Symptom-inducing tasks were addressed in the first session, with subsequent instruction in later sessions. Strength exercise independence demanded precise execution and muscle engagement, progressing to higher resistance via altered body positioning or elastic bands upon achieving two sets of 20 repetitions [19]. The CG group received no treatment. The movement pattern training was divided into levels 1-3 without resistance to the band and 4-5 with band resistance. The training in the first week includes familiarization with the training protocols. From weeks 2 to 5, including week 2, the strength training for the hip external rotator at extension is implemented. In week 3, the strength training for the hip external rotator with the hip in flexion started. In week 4, hip flexor strengthening exercises are practiced. Week 5 includes hip abductor strengthening, and in week 6, the participants practiced strength training for the hip external rotator and abductor. The intervention group performed 18 exercise sessions over 6 weeks.
Co-contraction
All subjects walked along an 18-m path before and after training. Ag/AgCl electrodes were used to record the activities of tibialis anterior (TA), gastrocnemius medialis (Gas-M), biceps femoris (BF), semitendinosus (ST), vastus lateralis (VL), vastus medialis (VM), rectus femoris (RF) of the dominant limb [8]. The sample rate was 1000 Hz using an EMG system (Biometrics Ltd, UK) [5]. The root mean square (RMS) data were calculated at loading, mid-stance, and push-off sub-phases [20-22]. Maximum voluntary isometric contraction was applied to normalize EMG amplitude [23].
The general co-contraction was calculated using the Equation 1 [24]:
1. General ankle co-contraction=Tibialis anterior+Gastrocnemius medialis
General knee co-contraction=Sum of all agonist and antagonist mean EMG activities [25].
The stance phase was determined using a Bertec force plate (USA) with a 10 N vertical force threshold.
Statistical analysis
We utilized the G*Power freeware tool to estimate the sample size [26]. The data normality was confirmed by the Shapiro-Wilk test. A two-way ANOVA with repeated measures was applied in the statistical section. Eta-squared (η2) was used to calculate effect size [27]. The α level was set at 0.05.
Results
Results of baseline data
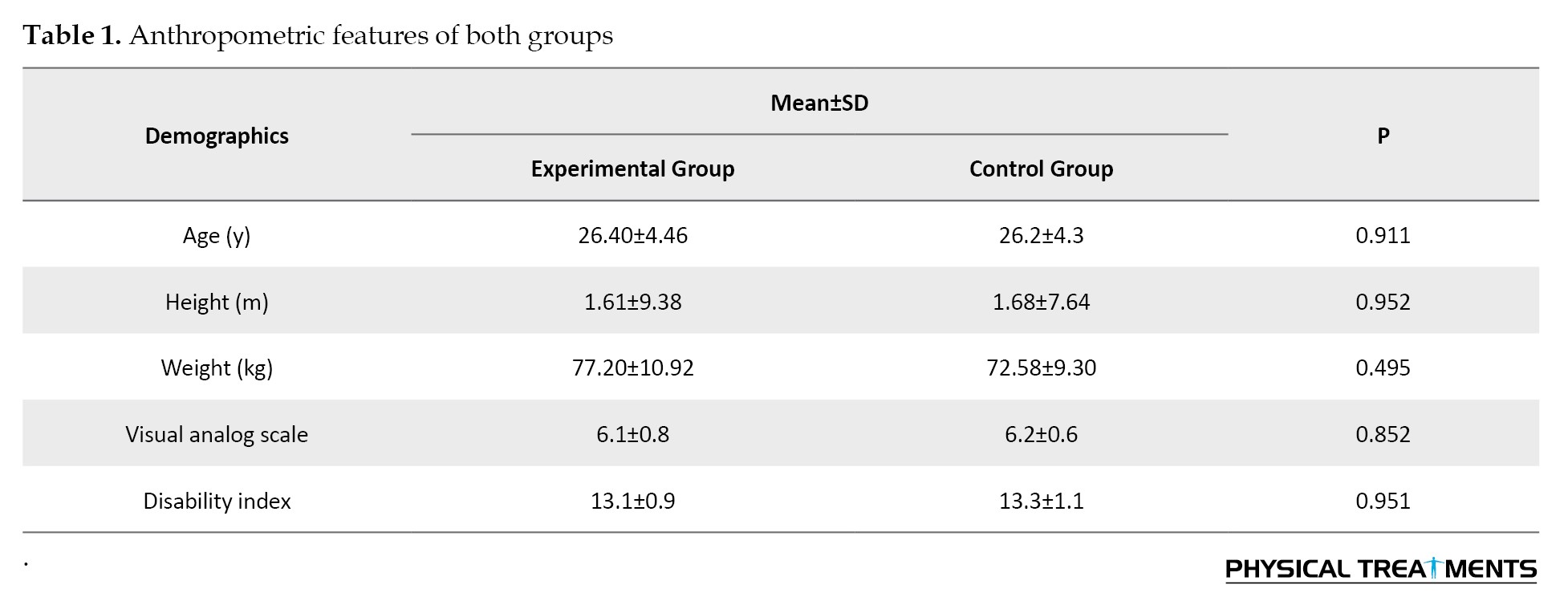
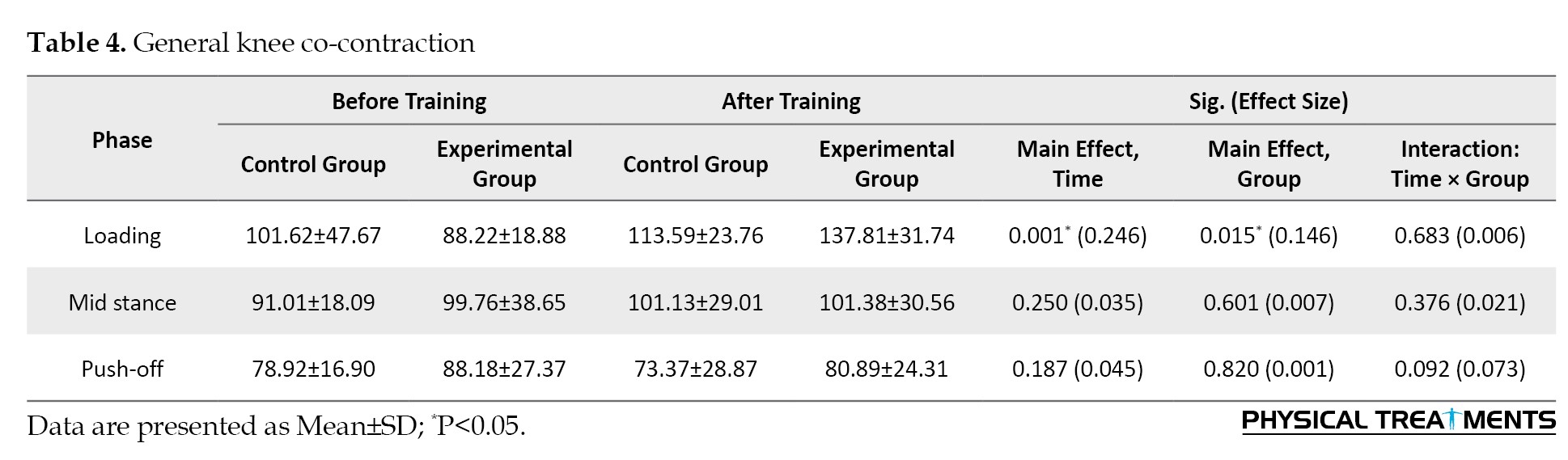
All subjects received their assigned treatment as planned, and the adherence rate for both groups was 100% (Table 1).
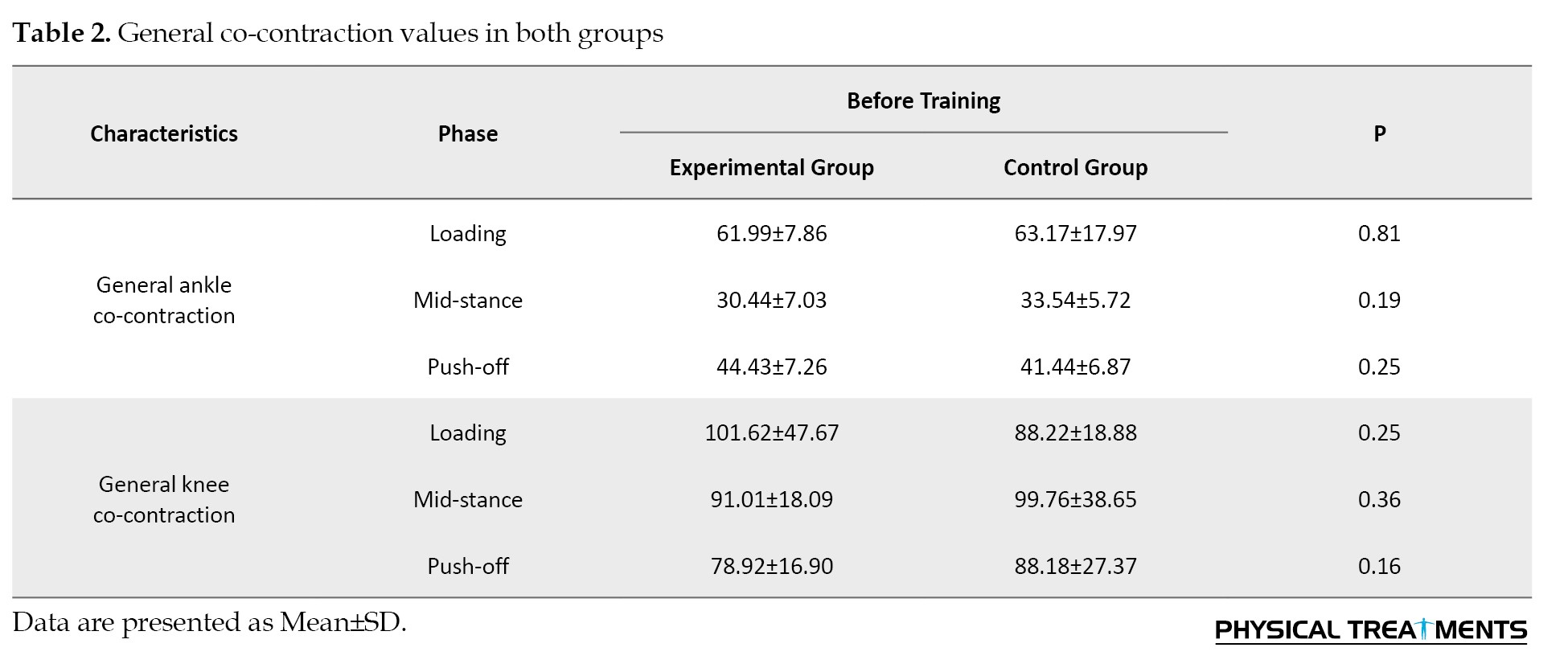
No differences were found for baseline knee and ankle general co-contraction values (P>0.05) (Table 2).
Results of co-contraction data
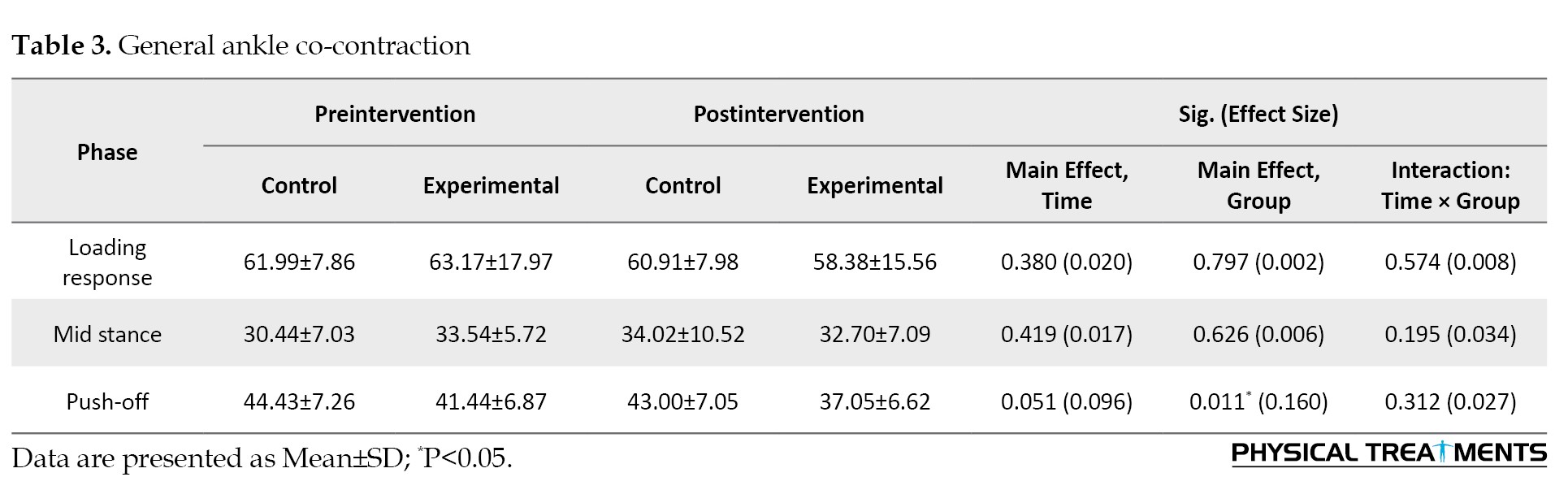
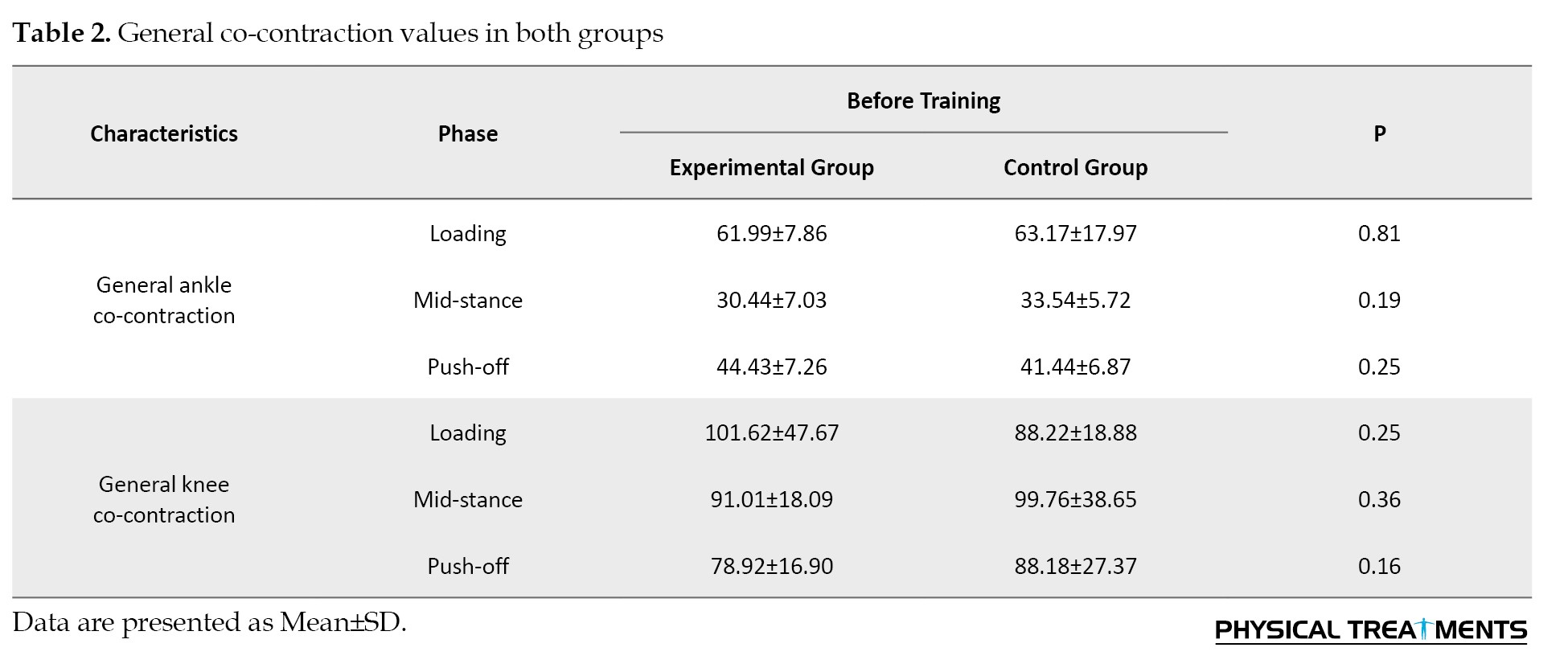
The main effect of “Group” for general co-contraction of the ankle was significant during push off phase (P=0.011, ƞ2=0.160). Results revealed greater general co-contraction of the ankle at propulsion in the control group than in the experimental group (Table 3).
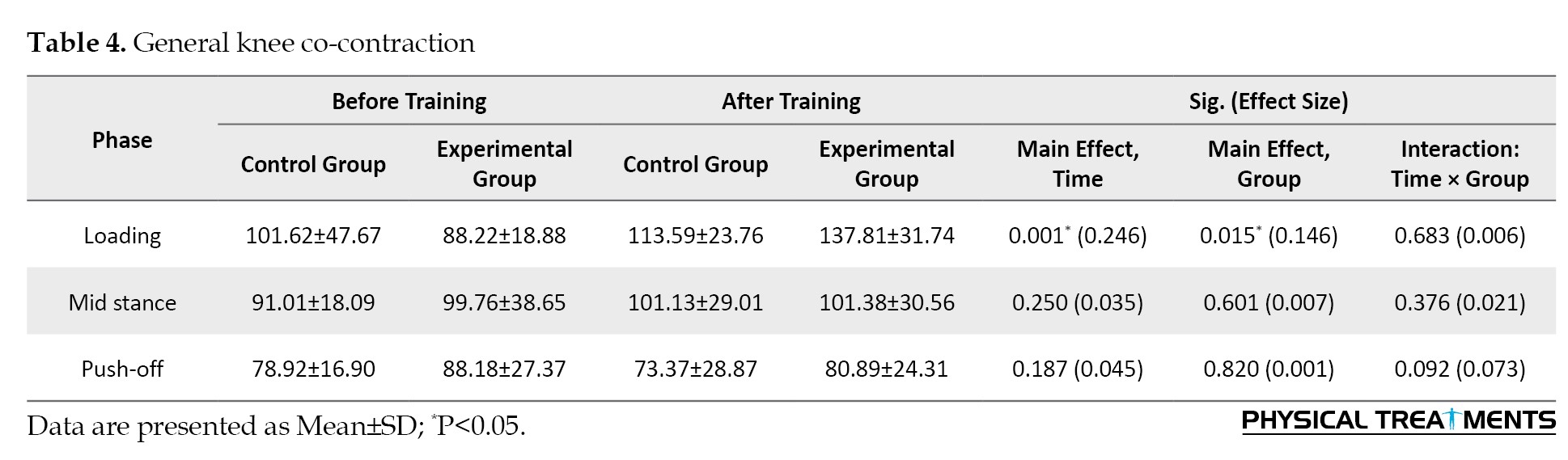
Effects of “Time” for general co-contraction of the knee was significant during loading phase (P=0.001, ƞ2=0.246). Greater general co-contraction of the knee at loading after training was observed compared to before training. Findings showed greater general co-contraction of the knee at the loading phase in the experimental group than in the control group (P>0.05) (Table 4).
Discussion
This research assesses the impact of movement pattern training on general knee and ankle muscular co-contraction during walking in NSCLBP patients. The findings indicate a significant decrease in general co-contraction of the ankle at propulsion. Instead, they work in synergy to position the foot correctly in preparation for the next heel strike [28]. The occurrence of TA/GL co-contraction throughout the posture has been reported in numerous studies [29, 30]. Also, our study did not show a significant effect for general ankle co-contraction at the mid-stance phase during walking. The recruitment of the TA during this phase is not associated with ankle dorsiflexion but rather with its activation as a foot-invertor muscle. Consequently, the TA and GL muscles do not function antagonistically but rather engage in co-contraction to maintain balance [31], as supported by Di Nardo’s study, which reported smaller-level co-contractions [32]. Therefore, the decrease in general ankle co-contraction at the propulsion could suggest that movement pattern training may positively impact the efficiency and coordination of walking in patients with non-specific chronic LBP [33].
Additionally, the study revealed significant changes in general co-contraction of the knee at the loading. The increase in knee co-contraction at the loading in the intervention group suggests that the movement pattern training intervention had a specific effect on knee muscle activation patterns during the initial phase of walking. This condition could indicate improved neuromuscular control, joint stability, or functional coordination at the knee joint following the intervention [34]. Furthermore, the differences between the experimental and control groups highlight the potential benefits of targeted movement pattern training in addressing gait abnormalities and muscle co-contraction patterns in individuals with LBP. The results suggest that focusing on specific movement patterns can alter muscle activation strategies during gait, potentially improving movement efficiency and reducing compensatory mechanisms that may contribute to pain and dysfunction [35]. Also, previous research has identified knee joint instability as contributing to falls in individuals. The heightened general contractility in the knee joint may be linked to joint stability. Consequently, increasing general knee co-contraction may serve as a core strategy for enhancing joint stability during walking [36].
Conclusion
Our training protocol affects the general co-contraction of the lower limb muscles in patients with LBP. The increased co-contraction of the knee during the loading in the intervention group could indicate improved neuromuscular control, joint stability, or functional coordination at the knee joint following the intervention. Also, focusing on specific movement patterns can lead to alterations in muscle activation strategies during gait, potentially improving movement efficiency and reducing compensatory mechanisms that may contribute to pain and dysfunction.
Limitations
We evaluated only male participants, highlighting a gap that future research should aim to fill by exploring the effects of similar training protocols on female populations, who may exhibit different biomechanical and physiological responses to movement pattern training.
Ethical Considerations
Compliance with ethical guidelines
This research was conducted with the ethical code of IR.SBU.REC.1399.060 and registration number of IRCT20181024041444N1. Informed consent was received from all samples.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, Supervision, and Writing the original draft: AmirAli Jafarnezhadgero and Ehsan Fakhri Mirzanag; Methodology and Statistics analysis: Ehsan Fakhri Mirzanag and Milad Piran Hamlabadi; Investigation and Data collection: Afshiin Orouji, Amir Letafatkar, and Milad Piran Hamlabadi; Review and editing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the participants in this study for their voluntary participation.
References
Low back pain (LBP) occurs in about 80% of people in their lifetime [1]. In 2015, approximately 7.3% of the population worldwide experienced activity limitations due to LBP [2]. LBP begins at 20 and 40 [2], with a high prevalence observed between 30 and 60 [3]. As a result, LBP is a common health problem that primary care settings frequently encounter [4]. LBP is associated with alterations in walking mechanics [3]. Excess foot pronation during the loading phase of walking can cause disrupted lower limb alignments and, ultimately LBP [5]. The trunk has been conceptualized as a pendulum [6]. As a result, the trunk-lower limb system is essential for the spine as a kinematic chain. This system consists of several parts and joints affecting the lumbar area and lower limb interaction while moving. Any dysfunction impacting this complex can disturb this connection, resulting in atypical motion. Different walking problems, like shorter steps and stiff coordination between body sections, are observed in people suffering from LBP [7].
The co-contraction of knee muscles is a mechanism for modifying joint stability and loading [8]. Individuals with LBP may show changed simultaneous contraction of lower limb muscles when walking. Generalized co-contraction is the simultaneous activation of all knee muscle groups [9]. Wang et al. reported that patients with lumbar disk herniation show enhanced biceps femoris root mean square at the stance phase. Positive relationships have been reported between tibialis anterior and gastrocnemius co-contraction and the disability index [10].
One common complication of this condition can be altered movement patterns during walking, leading to increased co-contraction of knee and ankle muscles [11]. Despite existing interventions, such as movement pattern training, the impact of these interventions on reducing knee and ankle muscular co-contraction in patients with non-specific chronic LBP (NSCLBP) during walking remains poorly understood. Movement pattern training is a therapeutic exercise that improves movement quality, coordination, and efficiency [12]. The training involves specific exercises and techniques designed to retrain and optimize movement patterns to enhance functional performance and reduce the risk of injury [13]. Movement pattern training addresses faulty movement patterns, postural imbalances, muscle imbalances, and improper biomechanics to help individuals move more effectively and efficiently [14]. This type of training can be beneficial for improving sports performance, rehabilitation from injuries, and enhancing overall movement quality in daily activities [14]. However, there is a need to assess the effect of movement pattern exercises in addressing this specific issue to improve the management and outcomes of NSCLBP. Therefore, this study aims to investigate the impact of movement pattern training on general lower limb muscular co-contraction at walking in patients with NSCLBP.
Materials and Methods
Study design and participants
This research was conducted with the ethical code of IR.SBU.REC.1399.060), and registration number of IRCT20181024041444N1. Informed consent was received from all samples. The study recruited 40 male patients with LBP from local clinics. The G*power software, version 3.1.9.7, was used to estimate the required sample size [15]. The software determined that at least 40 participants would be needed. The subjects were divided into intervention (EG, n=20) and control (CG, n=20) groups. The inclusion criteria were as follows: Pain persisting >3 months, visual analog scale >3 cm, and disability index of >10 [16]. The exclusion criteria were as follows: LBP of traumatic origin, history of surgery, and musculoskeletal misalignments [17].
The eligible participants were allocated into both groups using the block randomization method [18].
Training protocol
The exercise protocol used in this study was based on that introduced by Harris-Hayes et al. [19]. All the participants belonging to the EG underwent a total of 18 training sessions for 6 weeks. The movement pattern training program incorporated two primary components: Task-specific exercise (e.g. based on walking) for specific tasks and hip musculature strengthening.
Participants were instructed to start with a minimum number of exercise repetitions, gradually increasing as tolerated, ensuring correct execution and the absence of hip pain. At each visit, a therapist evaluated the performance of specific functional tasks and strength exercises, focusing on mastery for autonomous practice. Functional independence required patients to replicate modified lower limb movements accurately. Once achieved, no further guidance was issued, but patients were advised to maintain these patterns in daily activities. Symptom-inducing tasks were addressed in the first session, with subsequent instruction in later sessions. Strength exercise independence demanded precise execution and muscle engagement, progressing to higher resistance via altered body positioning or elastic bands upon achieving two sets of 20 repetitions [19]. The CG group received no treatment. The movement pattern training was divided into levels 1-3 without resistance to the band and 4-5 with band resistance. The training in the first week includes familiarization with the training protocols. From weeks 2 to 5, including week 2, the strength training for the hip external rotator at extension is implemented. In week 3, the strength training for the hip external rotator with the hip in flexion started. In week 4, hip flexor strengthening exercises are practiced. Week 5 includes hip abductor strengthening, and in week 6, the participants practiced strength training for the hip external rotator and abductor. The intervention group performed 18 exercise sessions over 6 weeks.
Co-contraction
All subjects walked along an 18-m path before and after training. Ag/AgCl electrodes were used to record the activities of tibialis anterior (TA), gastrocnemius medialis (Gas-M), biceps femoris (BF), semitendinosus (ST), vastus lateralis (VL), vastus medialis (VM), rectus femoris (RF) of the dominant limb [8]. The sample rate was 1000 Hz using an EMG system (Biometrics Ltd, UK) [5]. The root mean square (RMS) data were calculated at loading, mid-stance, and push-off sub-phases [20-22]. Maximum voluntary isometric contraction was applied to normalize EMG amplitude [23].
The general co-contraction was calculated using the Equation 1 [24]:
1. General ankle co-contraction=Tibialis anterior+Gastrocnemius medialis
General knee co-contraction=Sum of all agonist and antagonist mean EMG activities [25].
The stance phase was determined using a Bertec force plate (USA) with a 10 N vertical force threshold.
Statistical analysis
We utilized the G*Power freeware tool to estimate the sample size [26]. The data normality was confirmed by the Shapiro-Wilk test. A two-way ANOVA with repeated measures was applied in the statistical section. Eta-squared (η2) was used to calculate effect size [27]. The α level was set at 0.05.
Results
Results of baseline data
All subjects received their assigned treatment as planned, and the adherence rate for both groups was 100% (Table 1).
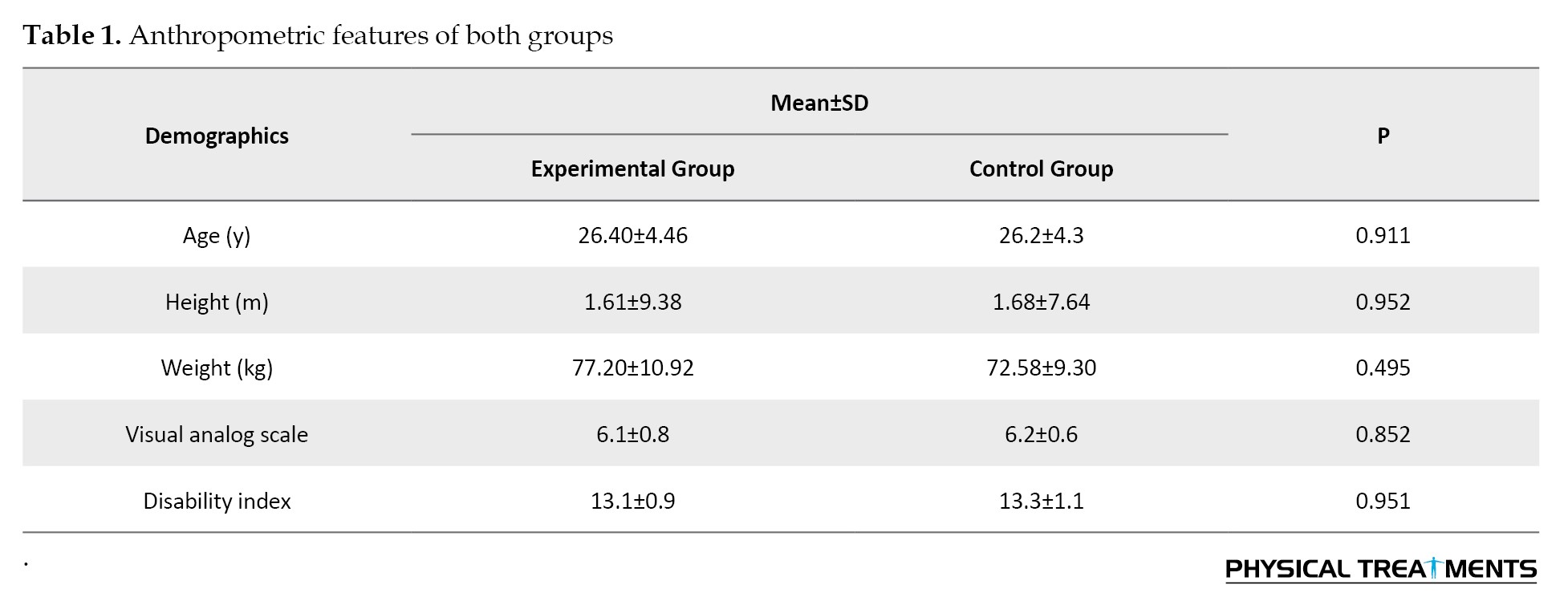
No differences were found for baseline knee and ankle general co-contraction values (P>0.05) (Table 2).
Results of co-contraction data
The main effect of “Group” for general co-contraction of the ankle was significant during push off phase (P=0.011, ƞ2=0.160). Results revealed greater general co-contraction of the ankle at propulsion in the control group than in the experimental group (Table 3).
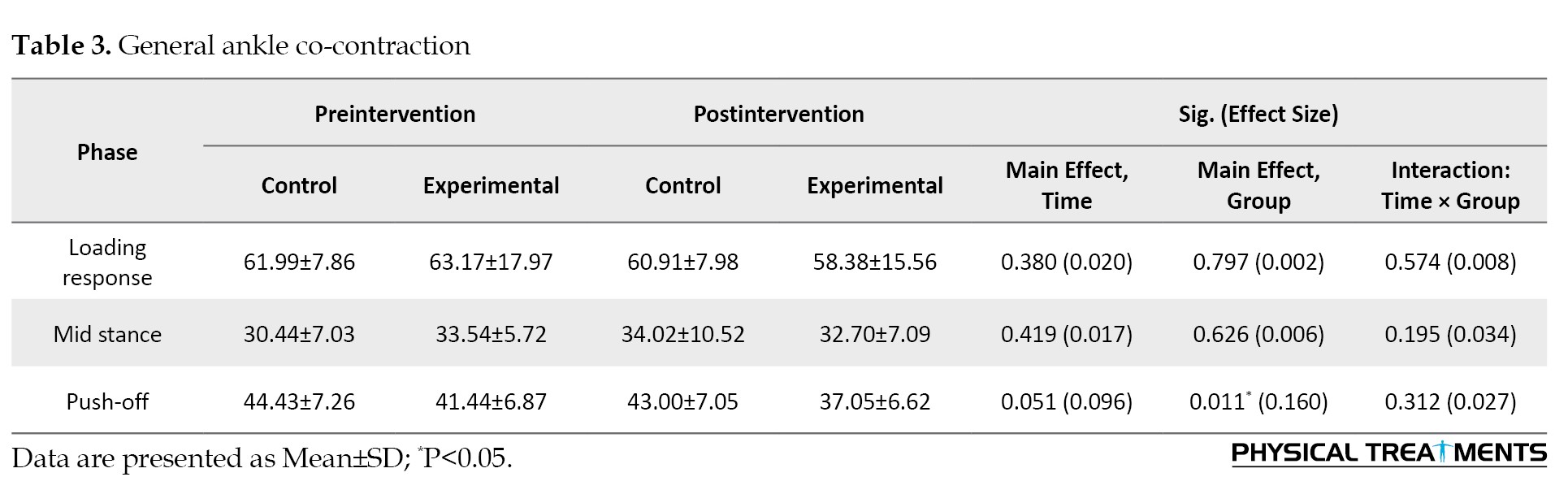
Effects of “Time” for general co-contraction of the knee was significant during loading phase (P=0.001, ƞ2=0.246). Greater general co-contraction of the knee at loading after training was observed compared to before training. Findings showed greater general co-contraction of the knee at the loading phase in the experimental group than in the control group (P>0.05) (Table 4).
Discussion
This research assesses the impact of movement pattern training on general knee and ankle muscular co-contraction during walking in NSCLBP patients. The findings indicate a significant decrease in general co-contraction of the ankle at propulsion. Instead, they work in synergy to position the foot correctly in preparation for the next heel strike [28]. The occurrence of TA/GL co-contraction throughout the posture has been reported in numerous studies [29, 30]. Also, our study did not show a significant effect for general ankle co-contraction at the mid-stance phase during walking. The recruitment of the TA during this phase is not associated with ankle dorsiflexion but rather with its activation as a foot-invertor muscle. Consequently, the TA and GL muscles do not function antagonistically but rather engage in co-contraction to maintain balance [31], as supported by Di Nardo’s study, which reported smaller-level co-contractions [32]. Therefore, the decrease in general ankle co-contraction at the propulsion could suggest that movement pattern training may positively impact the efficiency and coordination of walking in patients with non-specific chronic LBP [33].
Additionally, the study revealed significant changes in general co-contraction of the knee at the loading. The increase in knee co-contraction at the loading in the intervention group suggests that the movement pattern training intervention had a specific effect on knee muscle activation patterns during the initial phase of walking. This condition could indicate improved neuromuscular control, joint stability, or functional coordination at the knee joint following the intervention [34]. Furthermore, the differences between the experimental and control groups highlight the potential benefits of targeted movement pattern training in addressing gait abnormalities and muscle co-contraction patterns in individuals with LBP. The results suggest that focusing on specific movement patterns can alter muscle activation strategies during gait, potentially improving movement efficiency and reducing compensatory mechanisms that may contribute to pain and dysfunction [35]. Also, previous research has identified knee joint instability as contributing to falls in individuals. The heightened general contractility in the knee joint may be linked to joint stability. Consequently, increasing general knee co-contraction may serve as a core strategy for enhancing joint stability during walking [36].
Conclusion
Our training protocol affects the general co-contraction of the lower limb muscles in patients with LBP. The increased co-contraction of the knee during the loading in the intervention group could indicate improved neuromuscular control, joint stability, or functional coordination at the knee joint following the intervention. Also, focusing on specific movement patterns can lead to alterations in muscle activation strategies during gait, potentially improving movement efficiency and reducing compensatory mechanisms that may contribute to pain and dysfunction.
Limitations
We evaluated only male participants, highlighting a gap that future research should aim to fill by exploring the effects of similar training protocols on female populations, who may exhibit different biomechanical and physiological responses to movement pattern training.
Ethical Considerations
Compliance with ethical guidelines
This research was conducted with the ethical code of IR.SBU.REC.1399.060 and registration number of IRCT20181024041444N1. Informed consent was received from all samples.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, Supervision, and Writing the original draft: AmirAli Jafarnezhadgero and Ehsan Fakhri Mirzanag; Methodology and Statistics analysis: Ehsan Fakhri Mirzanag and Milad Piran Hamlabadi; Investigation and Data collection: Afshiin Orouji, Amir Letafatkar, and Milad Piran Hamlabadi; Review and editing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the participants in this study for their voluntary participation.
References
- Maetzel A, Li L. The economic burden of low back pain: A review of studies published between 1996 and 2001. Best Practice & Research. Clinical Rheumatology. 2002; 16(1):23-30. [DOI:10.1053/berh.2001.0204] [PMID]
- GBD 2015 Healthcare Access and Quality Collaborators. Electronic address: Cjlm@uw.edu; GBD 2015 Healthcare Access and Quality Collaborators. Healthcare Access and Quality Index based on mortality from causes amenable to personal health care in 195 countries and territories, 1990-2015: A novel analysis from the Global Burden of Disease Study 2015. The Lancet. 2017; 390(10091):231-66. [PMID]
- Bird AR, Payne CB. Foot function and low back pain. The Foot. 1999; 9(4):175-80. [DOI:10.1054/foot.1999.0563]
- Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, et al. A systematic review of the global prevalence of low back pain. Arthritis and Rheumatism. 2012; 64(6):2028-37. [DOI:10.1002/art.34347] [PMID]
- Farahpour N, Jafarnezhadgero A, Allard P, Majlesi M. Muscle activity and kinetics of lower limbs during walking in pronated feet individuals with and without low back pain. Journal of Electromyography and Kinesiology. 2018; 39:35-41. [DOI:10.1016/j.jelekin.2018.01.006] [PMID]
- Zeinali-Davarani Sh, Hemami H, Barin K, Shirazi-Adl A, Parnianpour M. Dynamic stability of spine using stability-based optimization and muscle spindle reflex. IEEE Transactions on Neural Systems and Rehabilitation Engineering. 2008; 16(1):106-18. [DOI:10.1109/TNSRE.2007.906963]
- Sadeghisani M, Manshadi FD, Kalantari KK, Rahimi A, Namnik N, Karimi MT, et al. Correlation between Hip Rotation Range-of-Motion Impairment and Low Back Pain. A literature review. Ortopedia, Traumatologia, Rehabilitacja. 2015; 17(5):455-62. [DOI:10.5604/15093492.1186813] [PMID]
- Hubley-Kozey C, Deluzio K, Dunbar M. Muscle co-activation patterns during walking in those with severe knee osteoarthritis. Clinical Biomechanics (Bristol). 2008; 23(1):71-80. [DOI:10.1016/j.clinbiomech.2007.08.019] [PMID]
- Lloyd DG, Buchanan TS. Strategies of muscular support of varus and valgus isometric loads at the human knee. Journal of Biomechanics. 2001; 34(10):1257-67. [DOI:10.1016/S0021-9290(01)00095-1] [PMID]
- Wang W, Wei H, Shi R, Lin L, Zhang L, Yue S, et al. Dysfunctional muscle activities and co-contraction in the lower-limb of lumbar disc herniation patients during walking. Scientific Reports. 2020; 10(1):20432. [DOI:10.1038/s41598-020-77150-7]
- Laird RA, Kent P, Keating JL. Modifying patterns of movement in people with low back pain -does it help? A systematic review. BMC Musculoskeletal Disorders. 2012; 13:169. [DOI:10.1186/1471-2474-13-169] [PMID]
- Letafatkar A, Nazarzadeh M, Hadadnezhad M, Farivar N. The efficacy of a HUBER exercise system mediated sensorimotor training protocol on proprioceptive system, lumbar movement control and quality of life in patients with chronic non-specific low back pain. Journal of Back and Musculoskeletal Rehabilitation. 2017; 30(4):767-78. [DOI:10.3233/BMR-150404] [PMID]
- Blazevich AJ, Wilson CJ, Alcaraz PE, Rubio-Arias JA. Effects of resistance training movement pattern and velocity on isometric muscular rate of force development: A systematic review with Meta-analysis and Meta-regression. Sports Medicine. 2020; 50(5):943-63. [DOI:10.1007/s40279-019-01239-x] [PMID]
- Garbenytė-Apolinskienė T, Šiupšinskas L, Salatkaitė S, Gudas R, Radvila R. The effect of integrated training program on functional movements patterns, dynamic stability, biomechanics, and muscle strength of lower limbs in elite young basketball players. Sport Sciences for Health. 2018; 14:245-50. [DOI:10.1007/s11332-017-0409-y]
- Jafarnezhadgero A, Fatollahi A, Amirzadeh N, Siahkouhian M, Granacher U. Ground reaction forces and muscle activity while walking on sand versus stable ground in individuals with pronated feet compared with healthy controls. PLoS One. 2019; 14(9):e0223219. [DOI:10.1371/journal.pone.0223219] [PMID]
- Piran Hamlabadi M, Jafarnezhadgero AA. [Effect of simple and sensori thoracolumbosacral braces on gait kinetics in low back pain patients (Persian)]. Journal of Gorgan University of Medical Sciences. 2022; 24(1):53-9. [Link]
- Lamoth CJ, Meijer OG, Daffertshofer A, Wuisman PI, Beek PJ. Effects of chronic low back pain on trunk coordination and back muscle activity during walking: Changes in motor control. European Spine Journal. 2006; 15(1):23-40. [DOI:10.1007/s00586-004-0825-y] [PMID]
- Piran HM, Jafarnezhadgero A, Hoseinpour K. [Comparison of the effect of polyurethan thermoplastics military boots mileage on lower limb muscle activities during running in people with and without back pain (Persian)]. Journal of Anesthesiology and Pain. 2023; 14(2):116-25. [Link]
- Harris-Hayes M, Czuppon S, Van Dillen LR, Steger-May K, Sahrmann S, Schootman M, et al., Movement-pattern training to improve function in people with chronic hip joint pain: A feasibility randomized clinical trial. Journal of Orthopaedic & Sports Physical Therapy. 2016; 46(6):452-61. [DOI:10.2519/jospt.2016.6279] [PMID]
- Whittle MW. Gait analysis: An introduction. Amsterdam: Elsevier Ltd; 2007. [Link]
- Dugan SA, Bhat KP. Biomechanics and analysis of running gait. Physical Medicine and Rehabilitation Clinics. 2005; 16(3):603-21. [Link]
- Shorter AL, Rouse EJ. Ankle mechanical impedance during the stance phase of running. IEEE Transactions on Bio-Medical Engineering. 2020; 67(6):1595-603. [DOI:10.1109/TBME.2019.2940927] [PMID]
- Piran Hamlabadi M, Jafarnezhadgero A, Hoseinpour K. [Evaluation of running mechanics in new and old polyurethanes military boots in males with and without pronated feet (Persian)]. Studies in Sport Medicine. 2024; 16(39):47-66. [DOI:10.22089/smj.2023.14610.1673]
- Emami S, Jafarnezhadgero A, Hamlabadi P. [The effect of knee orthosis on co-contraction values of knee and ankle muscles during running in people with knee deformity in the frontal plane (Persian)]. Iranian Journal of Rehabilitation Research in Nursing. 2022; 8(4): 76-87. [Link]
- Hamlabadi MP, Jafarnezhadgero AA. [Effect of 2 types of thoracholumbosacral braces on ankle and knee joint co-contraction in individuals with kyphosis during running (Persian)]. Journal of Gorgan University of Medical Sciences. 2023; 25(3):27-35. [Link]
- Fueki K, Yoshida-Kohno E, Wakabayashi N. Oral health-related quality of life in patients with non-metal clasp dentures: a randomised cross-over trial. Journal of Oral Rehabilitation. 2017; 44(5):405-413. [DOI:10.1111/joor.12494] [PMID]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences.New York: Routledge; 2013. [DOI:10.4324/9780203774441]
- Winter DA. Biomechanics and motor control of human movement. New Jersey: John Wiley & Sons; 2009. [Link]
- Falconer K. Quantitative assessment of cocontraction at the ankle joint in walking. Electromyogr Clin Neurophysiol. 1985; 25:135-48. [Link]
- Olney SJ. Quantitative evaluation of cocontraction of knee and ankle muscles in normal walking. Biomechanics IX-A Champain IL: Human Kinetics; 1985. [Link]
- Nardo FD, Mengarelli A, Ghetti G, Fioretti S. Statistical analysis of EMG signal acquired from tibialis anterior during gait. In: Roa Romero L, editor. XIII Mediterranean Conference on Medical and Biological Engineering and Computing 2013. Cham: Springer; 2014. [DOI:10.1007/978-3-319-00846-2_153]
- Di Nardo F, Mengarelli A, Maranesi E, Burattini L, Fioretti S. Assessment of the ankle muscle co-contraction during normal gait: A surface electromyography study. Journal of Electromyography and Kinesiology. 2015;2 5(2):347-54.[DOI:10.1016/j.jelekin.2014.10.016]
- Du W, Li H, Omisore OM, Wang L, Chen W, Sun X. Co-contraction characteristics of lumbar muscles in patients with lumbar disc herniation during different types of movement. Biomedical Engineering Online. 2018; 17(1):8. [PMID]
- Mohammadi V, Letafatkar A, Jafarnezhadgero A A. Effects of core stability training on kinematic and kinetic variables in patients with chronic low back pain. Physical Treatments - Specific Physical Therapy Journal. 2023; 13 (1) :55-66 [DOI:10.32598/ptj.13.1.551.1]
- Schmitz A, Silder A, Heiderscheit B, Mahoney J, Thelen DG. Differences in lower-extremity muscular activation during walking between healthy older and young adults.Journal of Electromyography and Kinesiology. 2009; 19(6):1085-91. [DOI:10.1016/j.jelekin.2008.10.008]
- Rubenstein LZ. Falls in older people: Epidemiology, risk factors and strategies for prevention. Age and Ageing. 2006; 35(suppl_2):ii37-41. [DOI:10.1093/ageing/afl084]
Type of Study: Research |
Subject:
General
Received: 2024/04/8 | Accepted: 2024/10/20 | Published: 2025/04/1
Received: 2024/04/8 | Accepted: 2024/10/20 | Published: 2025/04/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |