Sat, Oct 11, 2025
Volume 14, Issue 4 (Autumn 2024)
PTJ 2024, 14(4): 331-338 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Khorramroo F, Mousavi S H, Minoonejad H. Lower Limb Coordination After Post-op Complications in a Case With Ankle Stiffness. PTJ 2024; 14 (4) :331-338
URL: http://ptj.uswr.ac.ir/article-1-632-en.html
URL: http://ptj.uswr.ac.ir/article-1-632-en.html
1- Department of Sport Injuries and Biomechanics, Faculty of Sport Sciences and Health, University of Tehran, Tehran, Iran.
Full-Text [PDF 677 kb]
(531 Downloads)
| Abstract (HTML) (2683 Views)
Full-Text: (432 Views)
Introduction
Ankle stiffness is a crucial factor in human movement and musculoskeletal health. Understanding ankle stiffness is vital for comprehending joint mechanics, neuromuscular control, and lower extremities coordination [1]. Low joint stiffness can lead to injury, while joint excessive stiffness may not absorb enough strain energy, increasing the risk of overuse injuries. Excessive stiffness can result from injury, age-related changes, or pathological conditions, leading to compensatory movement patterns and gait abnormalities [1]. Gait analysis provides valuable insights into functional mobility and overall musculoskeletal and neurological health and coordination between the ankle, knee, and hip joints during walking [2].
Throughout the gait cycle, the lower extremity joints collaborate to provide stability, absorb shock, and generate propulsion [3]. In the initial contact and loading response (LR) phases, the ankle joint undergoes dorsiflexion for shock absorption, the knee joint undergoes flexion to absorb the impact of a foot strike, and the hip joint undergoes extension for propulsion. In midstance (MS) and terminal stance, the ankle transitions into plantarflexion, while the knee and hip extend to provide push-off (PO) force. During the swing phase, the ankle undergoes dorsiflexion, and the knee flexes for limb clearance and forward progression [4].
Disruptions in lower limb joint coordination can significantly impact an individual’s gait and mobility, particularly in cases of increased ankle stiffness. This can lead to altered movement patterns and compensatory mechanisms, increasing energy expenditure, and the risk of secondary musculoskeletal issues [5]. Decreased ankle range of motion can limit dorsiflexion and plantarflexion, leading to compensatory knee flexion and extension, respectively [6]. It can also affect lower extremity alignment, potentially influencing hip abduction and adduction during weight-bearing activities and requiring increased hip flexion during the swing phase [7]. It may result in reduced forward progression of the tibia over the foot during the stance phase, leading to increased hip flexion to clear the foot during the swing phase [8].
Comprehending lower limb coordination is crucial to identify deviations in movement patterns and devising targeted interventions to enhance gait efficiency and alleviate the risk of musculoskeletal complications [2]. Addressing ankle stiffness and its impact on lower limb joint coordination is paramount to optimize gait patterns and mitigating potential complications [9]. Various interventions, including minimal shoes [10], myofascial release [11], biofeedback [12, 13], instrument-assisted soft tissue mobilization (IASTM) [11], and Faradic electrotherapy (FES) [14], have demonstrated potential for improving lower limb biomechanics. Nonetheless, the specific effects of these interventions on lower limb joint coordination during gait warrant further exploration. Hence, this case study was conducted to examine the effect of a 12-week intervention, including IASTM and FES on ankle-knee-hip coordination in a patient exhibiting uncommon excessive ankle stiffness. By focusing on the coordination of the ankle, knee, and hip joints, this study was conducted to provide valuable information on how these interventions can improve walking patterns and eliminate musculoskeletal disorders in individuals experiencing post-operative issues related to stiffness.
Case Description
A 41-year-old female athlete who had been exercising regularly since the age of 10 experienced a fracture of the tibia, fibula, calcaneus, and Achilles tendon rupture in her right leg during a high jump at the age of 34. This led to infection and compartment syndrome necessitating several surgeries to prevent the patient from amputation. The patient regained the ability to walk after 3.5 years, at the age of 37.5 years. At the time of the study, which was 3.5 years after recovering from the fracture, the patient was 41 years old, with a height of 1.68 m, a mass of 59 kg, a body mass index of 20.9, and leg lengths of 84.5 cm (right) and 86.5 cm (left). Ankle stiffness was measured using the Isokinetic Biodex system as reported in our previously published study [15]. The excessive ankle stiffness was confirmed by a certified physician. Throughout our interventions, the participant continued her daily workout routine, which included swimming and fitness training. Interventions were evaluated from December 2022 to March 2023. The experiments were performed by the ethical standards of the Helsinki Declaration. This study was approved by the Research Ethics Committees of the Faculty of Physical Education and Sport Sciences, Tehran University. The participants provided written consent.
All datasets analyzed in the current study are included in this published article and any more data is available from the corresponding author on reasonable request.
Data collection
A motion capture system comprising 12 cameras (6 Infra-red Cameras: MX T40-S, 4 IR Cameras), (Vero [v2.2]; (vicon motion capture system, two Video Cameras: Bonita 720c) (Vicon Motion Systems Ltd., Oxford, UK) at a sampling rate of 120 Hz, it was utilized to track the position of the 50 passive reflective markers (14 mm) positioned based on Oxford foot model. The individual walked barefoot at a comfortable pace along a 5 m walkway.
Intervention
The treatments were administered by a licensed physiotherapist (Hooman Minoonejad) and an instructor (Fateme Khorramroo). The program involved three sessions a week at home, for 12 weeks, with the participants beginning each session with a five-minute warm-up that involved moving the ankle in three different planes of movement. Two interventions were utilized, including IASTM techniques based on the instructions for the Graston technique [16] and FES [14]. These interventions were applied on different days, alternating between electrotherapy on the tibialis anterior, gastrocnemius muscles, and foot soles, and myofascial release [14], friction massage [17], and Graston technique [16] (using GT5, GT6, and GT2) on calf muscles, Achilles tendon, sole and on the spots with adhesions on the other day. Participants received electrotherapy on the same day as their exercise sessions. We utilized a device called the Beurer EM 49 Digital TENS/EMS for the electrotherapy [18], with an impulse duration of 250 µs and a frequency ranging from 25 to 50 Hz [18]. We gradually extended the intervention timing by 2-3 minutes every two weeks, if the participant was not distressed after the first progressed session and reported readiness for longer durations.
Data analysis
The initiation of the stance phase was determined from the heel marker in the kinematic data. The frame in which the heel marker had the least measure was determined as heel contact with the ground. The results were averaged across 5 trials. Nexus software was used to filter the data of the Vicon system and gap filling of the missing markers was done by the Rigid body and pattern fill method in Nexus software, version 2.16. Woltring filter with MSE mode 10 was implemented by Nexus [19].
Calculations for inter-joint coordination
We used the vector coding method used by Jafarnezhadgero et al. [2].
Statistical analysis
This descriptive study used Excel software to calculate the mean for pre and post-tests.
Results
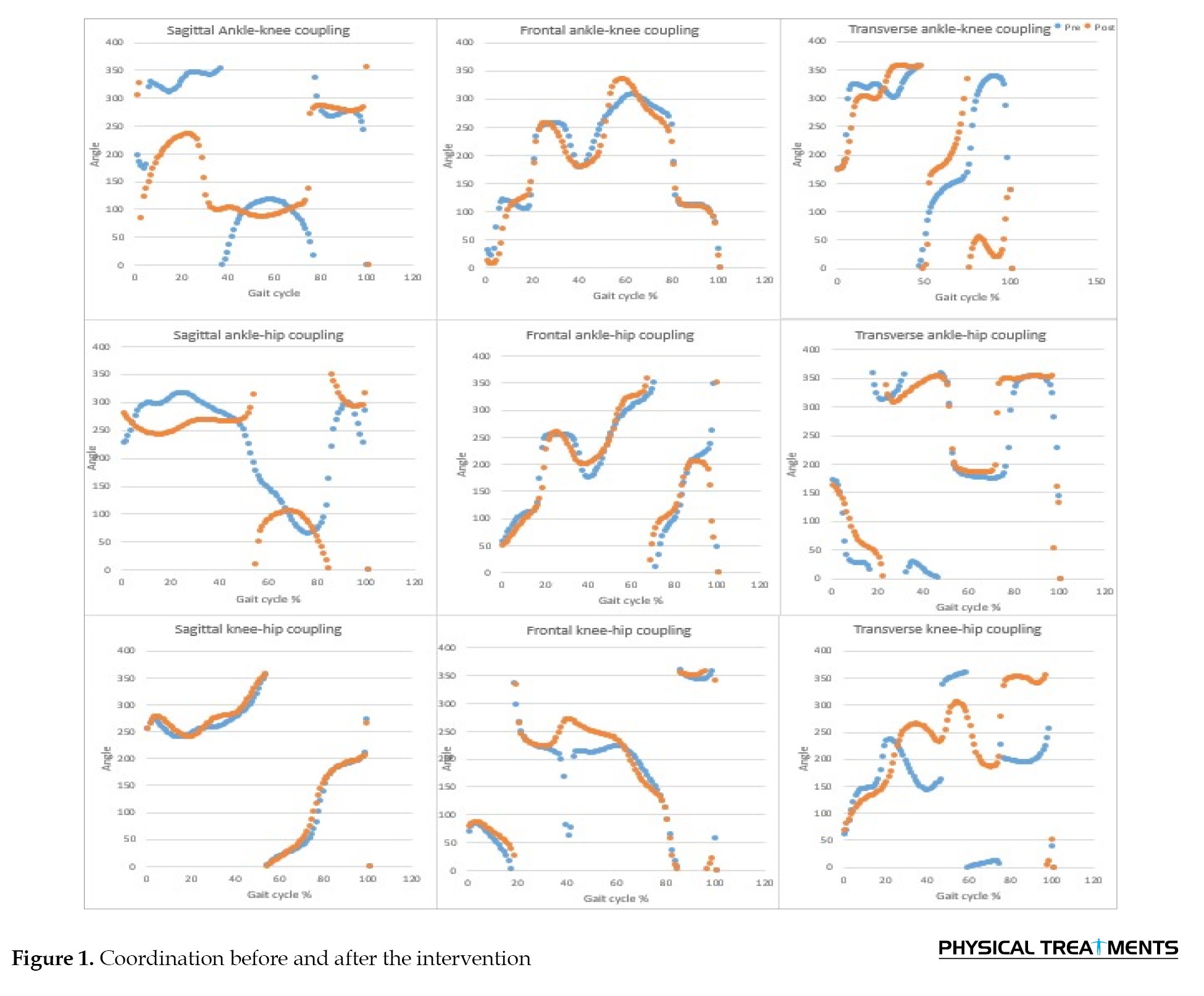
Table 1 and Figure 1 show Coordination in each subphase of stance phase before and after intervention.
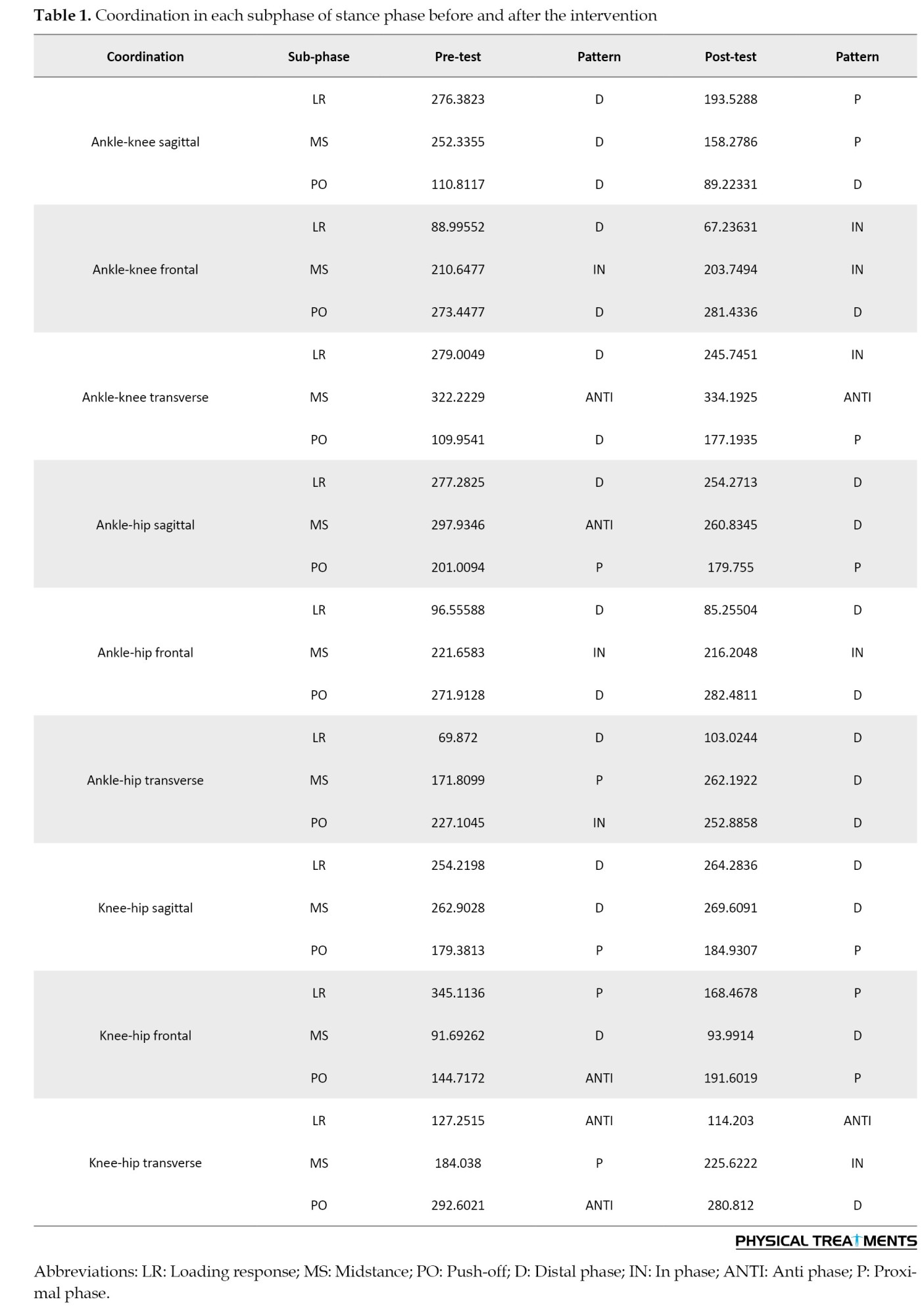
Ankle-knee coordination
The interventions altered the ankle-knee coordination occurring in LR and MS in the sagittal, LR in the frontal and LR, and PO in the transverse plane.
Ankle-hip coordination
The interventions altered the ankle-hip coordination occurring in MS and PO in the sagittal plane and transverse, and MS in the transverse plane.
Knee-hip coordination
The interventions altered the knee-hip coordination occurring in PO in the frontal plane, MS, and PO in the transverse plane.
Discussion
The present study was conducted to investigate the effect of a 12-week intervention, including IASTM and FES on ankle, knee, and hip 3-dimensional coordination during walking in a patient with excessive ankle stiffness. The results of the study revealed alterations in the post-test. Specifically, the patient demonstrated increased ankle ROM leading to a more fluid and efficient gait pattern. These improvements were also accompanied by a reduction in pain and discomfort during walking, indicating a positive impact of the intervention on the patient's overall functional mobility.
The observed improvements in gait coordination are consistent with the proposed mechanisms of action of IASTM and FES. IASTM can impact lower limb inter-joint coordination during gait by improving soft tissue mobility and flexibility, enhancing ankle joint range of motion, and addressing soft tissue restrictions and adhesions. Similarly, FES can improve muscle activation and control around the ankle and knee, contributing to more efficient joint mechanics and aiding in motor learning and the development of new movement patterns. Additionally, IASTM and FES can help to improve proprioception, which can help the muscles around the ankle and hip which are most needed in the stance phase [20], and the muscles surrounding the ankle in stabilizing the foot during weight transfers to the toes [21] leading to more optimal coordination.
Ankle-knee coordination
Our results for ankle-knee sagittal plane coordination demonstrated that during LR and MS subjects showed a proximal pattern in the post-test, indicating that the knee flexes before the ankle after the 12-week interventions. This is consistent with the results of Yaserifar et al. [22] which showed that the knee-ankle coordination in soccer players showed a distal phase coordination pattern of the ankle less often during the gait cycle. The observed coordination pattern in the subjects under investigation approached a level of similarity to that of healthy individuals in LR and MS for the ankle-knee in the sagittal plane, which was the main objective of this study for the patient.
Our results for ankle-knee frontal plane coordination demonstrated an in-phase pattern in LR indicating a simultaneous movement.
Ankle-knee transverse plane coordination in LR showed an in-phase pattern and in PO showed a proximal pattern. This indicates that in LR ankle and the knee move in the same direction and PO, the knee moves before the ankle. Our results are in contrast with the known normal transverse plane ankle knee coordination during LR, which occurs when the ankle and knee move in an anti-phase pattern relative to each other [23].
However, A study conducted by Aquino et al. [7] showed that ankle dorsiflexion restriction caused a decreased pelvic rotation angle and lower hip and knee maximum flexion in the stance phase. In the post-test, a sooner knee movement in LR, MS, and PO happened which shows improvements in sagittal plane coordination.
Ankle-hip coordination
Ankle-hip flexion/extension showed that the ankle moves before the hip in MS versus an anti-phase pattern in the pre-test. This indicates that the compensatory movement of the hip may have been diminished in the post-test due to increased ankle ROM in the transverse plane. Our pre-test results are consistent with Yen et al.'s [24] study which changed to distal pattern in the post-test. This may be due to the increased ankle ROM in the post-test. Ankle-hip in the transverse plane showed a sooner ankle rotation (distal pattern) in the post-test, which contrasts the findings of Yen et al. [24] that reported an anti-phase pattern in PO. This also may be due to increased ankle ROM and changes in muscle activity of the dorsi and plantar flexors.
A study conducted by Guan et al. [6] showed that knee and hip angles compensated for the decreased ankle ROM and less work generation was observed at the knee and more work absorption at the ankle.
Knee-hip coordination
The study found a sooner hip motion in the knee-hip abduction/adduction in the PO in the post-test compared to an anti-phase pattern in the pre-test. Furthermore, an in-phase coordination pattern was observed in the post-test for knee-hip internal/external rotation indicating that both segments move simultaneously in MS and the ankle moves before the hip in the PO in the post-test. This may be due to increased plantarflexion ROM and strength after the intervention. Furthermore, results of transverse plane knee-hip coordination showed a less scattered pattern in the post-test. Yaserifar et al. [22] reported that hip-knee had an anti-phase pattern (knee flexion and hip extension during LR which is in contrast with our results, and hip phase (proximal) in MS and PO which is consistent with our results, and soccer players showed an in-phase pattern in mentioned phases.
These results suggest the importance of muscle strength and coordination in influencing joint motion patterns during gait, highlighting the need for further research to explore potential interventions.
The results of this study have crucial implications for clinical practice. The use of IASTM and FES as part of a comprehensive rehabilitation program may be beneficial for individuals with excessive ankle stiffness, as it can help to address underlying soft tissue restrictions and improve neuromuscular control. This, in turn, may lead to enhanced functional mobility and reduced risk of secondary musculoskeletal complications.
Conclusion
In conclusion, the results of this study suggest that a 12-week intervention, including IASTM and FES, can change lower limb coordination in ankle-knee, ankle-hip sagittal and transverse, and knee-hip frontal and transverse planes during different subphases of gait after intervention in a patient with excessive ankle stiffness. The observed coordination pattern in the subjects under investigation approached a level of similarity to that of healthy individuals in LR and MS for the ankle-knee sagittal plane. These results have crucial implications for the rehabilitation of individuals with ankle stiffness and highlight the potential benefits of incorporating these interventions into clinical practice. Further research is required to validate these results and to clarify the underlying mechanisms involved.
Limitations and recommendation
This case study has a few limitations. Firstly, it focuses on just one patient, which limits the external validity (the ability to apply the results to a broader population). It is also challenging to determine the specific contribution of either IASTM, electrotherapy, or the combined treatment to the patient's progress. Additionally, it is essential to consider the impact of a unilateral ankle injury on the uninjured ankle and to assess any asymmetries between both sides. Lastly, recommending interventions for upper joints may be beneficial due to compensatory movements in the hip joint and trunk, as well as reduced postural control [6].
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committees of the Faculty of Physical Education and Sport Sciences, University of Tehran (Code: IR.UT.SPORT.REC.1401.045).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Methodology and supervision: Seyed Hamed Mousavi and Hooman Minoonejad; Visualization: Fateme Khorramroo; Conceptualization, writing-review and editing, investigation and project administration: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors express their sincere gratitude to the participant for the generous and dedicated collaboration throughout this study.
References
Ankle stiffness is a crucial factor in human movement and musculoskeletal health. Understanding ankle stiffness is vital for comprehending joint mechanics, neuromuscular control, and lower extremities coordination [1]. Low joint stiffness can lead to injury, while joint excessive stiffness may not absorb enough strain energy, increasing the risk of overuse injuries. Excessive stiffness can result from injury, age-related changes, or pathological conditions, leading to compensatory movement patterns and gait abnormalities [1]. Gait analysis provides valuable insights into functional mobility and overall musculoskeletal and neurological health and coordination between the ankle, knee, and hip joints during walking [2].
Throughout the gait cycle, the lower extremity joints collaborate to provide stability, absorb shock, and generate propulsion [3]. In the initial contact and loading response (LR) phases, the ankle joint undergoes dorsiflexion for shock absorption, the knee joint undergoes flexion to absorb the impact of a foot strike, and the hip joint undergoes extension for propulsion. In midstance (MS) and terminal stance, the ankle transitions into plantarflexion, while the knee and hip extend to provide push-off (PO) force. During the swing phase, the ankle undergoes dorsiflexion, and the knee flexes for limb clearance and forward progression [4].
Disruptions in lower limb joint coordination can significantly impact an individual’s gait and mobility, particularly in cases of increased ankle stiffness. This can lead to altered movement patterns and compensatory mechanisms, increasing energy expenditure, and the risk of secondary musculoskeletal issues [5]. Decreased ankle range of motion can limit dorsiflexion and plantarflexion, leading to compensatory knee flexion and extension, respectively [6]. It can also affect lower extremity alignment, potentially influencing hip abduction and adduction during weight-bearing activities and requiring increased hip flexion during the swing phase [7]. It may result in reduced forward progression of the tibia over the foot during the stance phase, leading to increased hip flexion to clear the foot during the swing phase [8].
Comprehending lower limb coordination is crucial to identify deviations in movement patterns and devising targeted interventions to enhance gait efficiency and alleviate the risk of musculoskeletal complications [2]. Addressing ankle stiffness and its impact on lower limb joint coordination is paramount to optimize gait patterns and mitigating potential complications [9]. Various interventions, including minimal shoes [10], myofascial release [11], biofeedback [12, 13], instrument-assisted soft tissue mobilization (IASTM) [11], and Faradic electrotherapy (FES) [14], have demonstrated potential for improving lower limb biomechanics. Nonetheless, the specific effects of these interventions on lower limb joint coordination during gait warrant further exploration. Hence, this case study was conducted to examine the effect of a 12-week intervention, including IASTM and FES on ankle-knee-hip coordination in a patient exhibiting uncommon excessive ankle stiffness. By focusing on the coordination of the ankle, knee, and hip joints, this study was conducted to provide valuable information on how these interventions can improve walking patterns and eliminate musculoskeletal disorders in individuals experiencing post-operative issues related to stiffness.
Case Description
A 41-year-old female athlete who had been exercising regularly since the age of 10 experienced a fracture of the tibia, fibula, calcaneus, and Achilles tendon rupture in her right leg during a high jump at the age of 34. This led to infection and compartment syndrome necessitating several surgeries to prevent the patient from amputation. The patient regained the ability to walk after 3.5 years, at the age of 37.5 years. At the time of the study, which was 3.5 years after recovering from the fracture, the patient was 41 years old, with a height of 1.68 m, a mass of 59 kg, a body mass index of 20.9, and leg lengths of 84.5 cm (right) and 86.5 cm (left). Ankle stiffness was measured using the Isokinetic Biodex system as reported in our previously published study [15]. The excessive ankle stiffness was confirmed by a certified physician. Throughout our interventions, the participant continued her daily workout routine, which included swimming and fitness training. Interventions were evaluated from December 2022 to March 2023. The experiments were performed by the ethical standards of the Helsinki Declaration. This study was approved by the Research Ethics Committees of the Faculty of Physical Education and Sport Sciences, Tehran University. The participants provided written consent.
All datasets analyzed in the current study are included in this published article and any more data is available from the corresponding author on reasonable request.
Data collection
A motion capture system comprising 12 cameras (6 Infra-red Cameras: MX T40-S, 4 IR Cameras), (Vero [v2.2]; (vicon motion capture system, two Video Cameras: Bonita 720c) (Vicon Motion Systems Ltd., Oxford, UK) at a sampling rate of 120 Hz, it was utilized to track the position of the 50 passive reflective markers (14 mm) positioned based on Oxford foot model. The individual walked barefoot at a comfortable pace along a 5 m walkway.
Intervention
The treatments were administered by a licensed physiotherapist (Hooman Minoonejad) and an instructor (Fateme Khorramroo). The program involved three sessions a week at home, for 12 weeks, with the participants beginning each session with a five-minute warm-up that involved moving the ankle in three different planes of movement. Two interventions were utilized, including IASTM techniques based on the instructions for the Graston technique [16] and FES [14]. These interventions were applied on different days, alternating between electrotherapy on the tibialis anterior, gastrocnemius muscles, and foot soles, and myofascial release [14], friction massage [17], and Graston technique [16] (using GT5, GT6, and GT2) on calf muscles, Achilles tendon, sole and on the spots with adhesions on the other day. Participants received electrotherapy on the same day as their exercise sessions. We utilized a device called the Beurer EM 49 Digital TENS/EMS for the electrotherapy [18], with an impulse duration of 250 µs and a frequency ranging from 25 to 50 Hz [18]. We gradually extended the intervention timing by 2-3 minutes every two weeks, if the participant was not distressed after the first progressed session and reported readiness for longer durations.
Data analysis
The initiation of the stance phase was determined from the heel marker in the kinematic data. The frame in which the heel marker had the least measure was determined as heel contact with the ground. The results were averaged across 5 trials. Nexus software was used to filter the data of the Vicon system and gap filling of the missing markers was done by the Rigid body and pattern fill method in Nexus software, version 2.16. Woltring filter with MSE mode 10 was implemented by Nexus [19].
Calculations for inter-joint coordination
We used the vector coding method used by Jafarnezhadgero et al. [2].
Statistical analysis
This descriptive study used Excel software to calculate the mean for pre and post-tests.
Results
Table 1 and Figure 1 show Coordination in each subphase of stance phase before and after intervention.
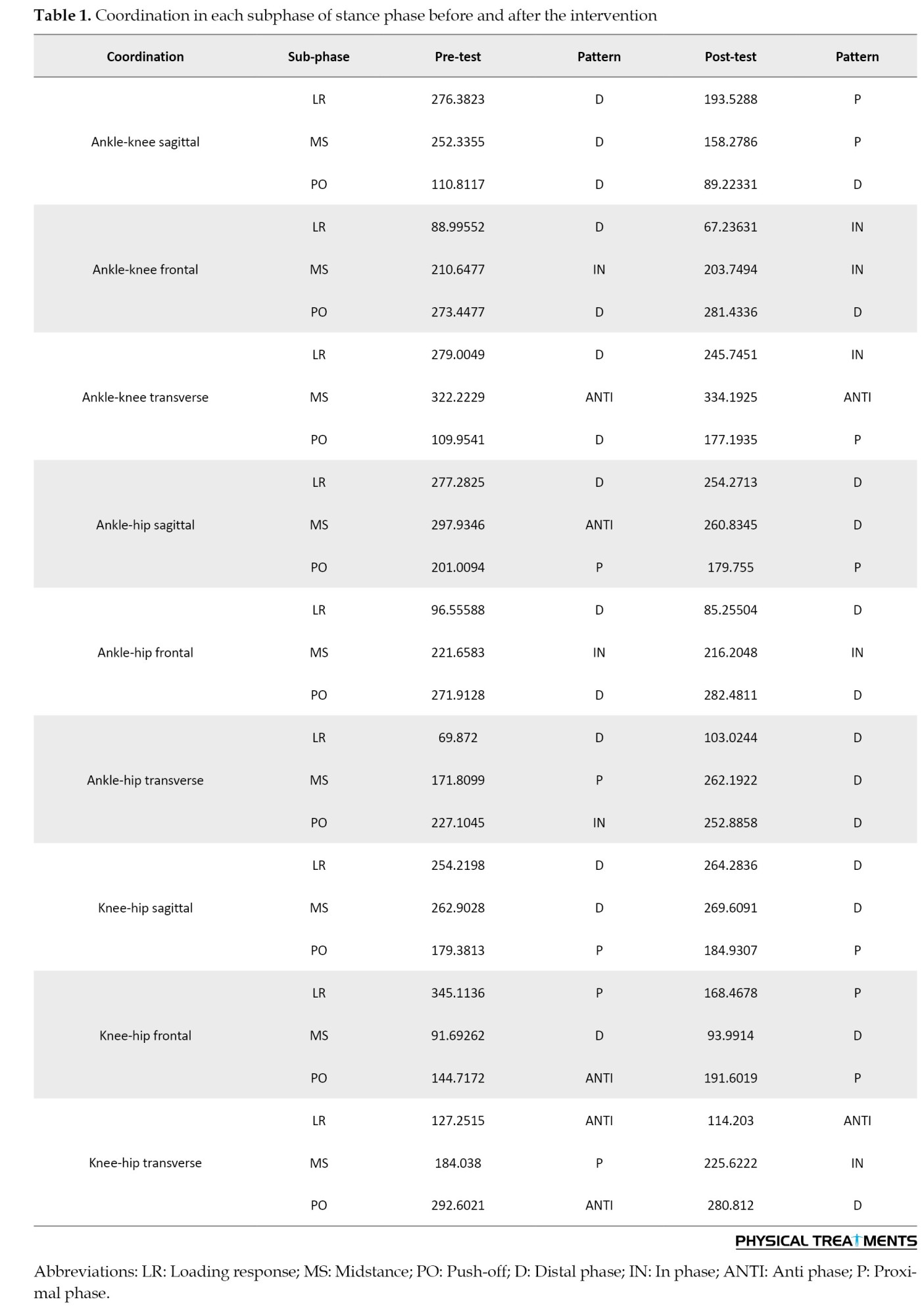
Ankle-knee coordination
The interventions altered the ankle-knee coordination occurring in LR and MS in the sagittal, LR in the frontal and LR, and PO in the transverse plane.
Ankle-hip coordination
The interventions altered the ankle-hip coordination occurring in MS and PO in the sagittal plane and transverse, and MS in the transverse plane.
Knee-hip coordination
The interventions altered the knee-hip coordination occurring in PO in the frontal plane, MS, and PO in the transverse plane.
Discussion
The present study was conducted to investigate the effect of a 12-week intervention, including IASTM and FES on ankle, knee, and hip 3-dimensional coordination during walking in a patient with excessive ankle stiffness. The results of the study revealed alterations in the post-test. Specifically, the patient demonstrated increased ankle ROM leading to a more fluid and efficient gait pattern. These improvements were also accompanied by a reduction in pain and discomfort during walking, indicating a positive impact of the intervention on the patient's overall functional mobility.
The observed improvements in gait coordination are consistent with the proposed mechanisms of action of IASTM and FES. IASTM can impact lower limb inter-joint coordination during gait by improving soft tissue mobility and flexibility, enhancing ankle joint range of motion, and addressing soft tissue restrictions and adhesions. Similarly, FES can improve muscle activation and control around the ankle and knee, contributing to more efficient joint mechanics and aiding in motor learning and the development of new movement patterns. Additionally, IASTM and FES can help to improve proprioception, which can help the muscles around the ankle and hip which are most needed in the stance phase [20], and the muscles surrounding the ankle in stabilizing the foot during weight transfers to the toes [21] leading to more optimal coordination.
Ankle-knee coordination
Our results for ankle-knee sagittal plane coordination demonstrated that during LR and MS subjects showed a proximal pattern in the post-test, indicating that the knee flexes before the ankle after the 12-week interventions. This is consistent with the results of Yaserifar et al. [22] which showed that the knee-ankle coordination in soccer players showed a distal phase coordination pattern of the ankle less often during the gait cycle. The observed coordination pattern in the subjects under investigation approached a level of similarity to that of healthy individuals in LR and MS for the ankle-knee in the sagittal plane, which was the main objective of this study for the patient.
Our results for ankle-knee frontal plane coordination demonstrated an in-phase pattern in LR indicating a simultaneous movement.
Ankle-knee transverse plane coordination in LR showed an in-phase pattern and in PO showed a proximal pattern. This indicates that in LR ankle and the knee move in the same direction and PO, the knee moves before the ankle. Our results are in contrast with the known normal transverse plane ankle knee coordination during LR, which occurs when the ankle and knee move in an anti-phase pattern relative to each other [23].
However, A study conducted by Aquino et al. [7] showed that ankle dorsiflexion restriction caused a decreased pelvic rotation angle and lower hip and knee maximum flexion in the stance phase. In the post-test, a sooner knee movement in LR, MS, and PO happened which shows improvements in sagittal plane coordination.
Ankle-hip coordination
Ankle-hip flexion/extension showed that the ankle moves before the hip in MS versus an anti-phase pattern in the pre-test. This indicates that the compensatory movement of the hip may have been diminished in the post-test due to increased ankle ROM in the transverse plane. Our pre-test results are consistent with Yen et al.'s [24] study which changed to distal pattern in the post-test. This may be due to the increased ankle ROM in the post-test. Ankle-hip in the transverse plane showed a sooner ankle rotation (distal pattern) in the post-test, which contrasts the findings of Yen et al. [24] that reported an anti-phase pattern in PO. This also may be due to increased ankle ROM and changes in muscle activity of the dorsi and plantar flexors.
A study conducted by Guan et al. [6] showed that knee and hip angles compensated for the decreased ankle ROM and less work generation was observed at the knee and more work absorption at the ankle.
Knee-hip coordination
The study found a sooner hip motion in the knee-hip abduction/adduction in the PO in the post-test compared to an anti-phase pattern in the pre-test. Furthermore, an in-phase coordination pattern was observed in the post-test for knee-hip internal/external rotation indicating that both segments move simultaneously in MS and the ankle moves before the hip in the PO in the post-test. This may be due to increased plantarflexion ROM and strength after the intervention. Furthermore, results of transverse plane knee-hip coordination showed a less scattered pattern in the post-test. Yaserifar et al. [22] reported that hip-knee had an anti-phase pattern (knee flexion and hip extension during LR which is in contrast with our results, and hip phase (proximal) in MS and PO which is consistent with our results, and soccer players showed an in-phase pattern in mentioned phases.
These results suggest the importance of muscle strength and coordination in influencing joint motion patterns during gait, highlighting the need for further research to explore potential interventions.
The results of this study have crucial implications for clinical practice. The use of IASTM and FES as part of a comprehensive rehabilitation program may be beneficial for individuals with excessive ankle stiffness, as it can help to address underlying soft tissue restrictions and improve neuromuscular control. This, in turn, may lead to enhanced functional mobility and reduced risk of secondary musculoskeletal complications.
Conclusion
In conclusion, the results of this study suggest that a 12-week intervention, including IASTM and FES, can change lower limb coordination in ankle-knee, ankle-hip sagittal and transverse, and knee-hip frontal and transverse planes during different subphases of gait after intervention in a patient with excessive ankle stiffness. The observed coordination pattern in the subjects under investigation approached a level of similarity to that of healthy individuals in LR and MS for the ankle-knee sagittal plane. These results have crucial implications for the rehabilitation of individuals with ankle stiffness and highlight the potential benefits of incorporating these interventions into clinical practice. Further research is required to validate these results and to clarify the underlying mechanisms involved.
Limitations and recommendation
This case study has a few limitations. Firstly, it focuses on just one patient, which limits the external validity (the ability to apply the results to a broader population). It is also challenging to determine the specific contribution of either IASTM, electrotherapy, or the combined treatment to the patient's progress. Additionally, it is essential to consider the impact of a unilateral ankle injury on the uninjured ankle and to assess any asymmetries between both sides. Lastly, recommending interventions for upper joints may be beneficial due to compensatory movements in the hip joint and trunk, as well as reduced postural control [6].
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committees of the Faculty of Physical Education and Sport Sciences, University of Tehran (Code: IR.UT.SPORT.REC.1401.045).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Methodology and supervision: Seyed Hamed Mousavi and Hooman Minoonejad; Visualization: Fateme Khorramroo; Conceptualization, writing-review and editing, investigation and project administration: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors express their sincere gratitude to the participant for the generous and dedicated collaboration throughout this study.
References
- Hedrick EA, Malcolm P, Wilken JM, Takahashi KZ. The effects of ankle stiffness on mechanics and energetics of walking with added loads: a prosthetic emulator study. Journal of NeuroEngineering and Rehabilitation. 2019; 16(1):148. [PMID]
- Jafarnezhadgero A, Mousavi SH, Madadi-Shad M, Hijmans JM. Quantifying lower limb inter-joint coordination and coordination variability after four-month wearing arch support foot orthoses in children with flexible flat feet. Human Movement Science. 2020; 70:102593. [DOI:10.1016/j.humov.2020.102593] [PMID]
- DeJong P, Hatamiya NS, Barkley LC. Running gait analysis and biomechanics. Current Sports Medicine Reports. 2022; 21(4):107-8. [DOI:10.1249/JSR.0000000000000944] [PMID]
- Neumann DA. Kinesiology of the musculoskeletal system-e-book: Foundations for rehabilitation. Amsterdam: Elsevier Health Sciences; 2016. [Link]
- Mousavi SH, Hijmans JM, Rajabi R, Diercks R, Zwerver J, van der Worp H. Kinematic risk factors for lower limb tendinopathy in distance runners: A systematic review and meta-analysis. Gait & Posture. 2019; 69:13-24. [DOI:10.1016/j.gaitpost.2019.01.011] [PMID]
- Guan X, Kuai S, Song L, Liu W, Liu Y, Ji L, Wang R. Effects of ankle joint motion on pelvis-hip biomechanics and muscle activity patterns of healthy individuals in knee immobilization gait. Journal of Healthcare Engineering. 2019; 2019:3812407. [DOI:10.1155/2019/3812407] [PMID]
- Aquino MRC, Resende RA, Kirkwood RN, Souza TR, Fonseca ST, Ocarino JM. Spatial-temporal parameters, pelvic and lower limb movements during gait in individuals with reduced passive ankle dorsiflexion. Gait and Posture. 2022; 93:32-38. [DOI:10.1016/j.gaitpost.2022.01.010] [PMID]
- Rao Y, Yang N, Gao T, Zhang S, Shi H, Lu Y, et al. Effects of peak ankle dorsiflexion angle on lower extremity biomechanics and pelvic motion during walking and jogging. Frontiers in Neurology. 2024; 14:1269061. [DOI:10.3389/fneur.2023.1269061] [PMID]
- Khorramroo F, Mousavi SH, Minoonejad H, Sorkhabi M. Managing post-operative complications in a patient with excessive ankle stiffness: A case study addressing gait biomechanics and EMG. Sport Sciences and Health Research. 2023; 15(2):145-58. [DOI:10.22059/sshr.2023.368736.1111]
- Khorramroo F, Mousavi SH. The effects of minimal shoes on ankle kinematics during running: A systematic review. Journal of Advanced Sport Technology. 2022; 6(2):20-38. [DOI:10.22098/jast.2022.1918]
- Cheatham SW, Baker R, Kreiswirth E. Instrument Assisted Soft-tissue Mobilization: A commentary on clinical practice guidelines for rehabilitation professionals. International Journal of Sports Physical Therapy. 2019; 14(4):670-82. [PMID]
- Mousavi SH, Khorramroo F, Minoonejad H, Zwerver J. Effects of biofeedback on biomechanical factors associated with chronic ankle instability: A systematic review with meta-analysis. BMC Sports Science, Medicine and Rehabilitation. 2023; 15(1):168. [DOI:10.1186/s13102-023-00780-7] [PMID]
- Mousavi SH, Khorramroo F, Jafarnezhadgero A. Gait retraining targeting foot pronation: A systematic review and meta-analysis. Plos One. 2024; 19(3):e0298646. [DOI:10.1371/journal.pone.0298646] [PMID]
- Ganesh GS, Kumari R, Pattnaik M, Mohanty P, Mishra C, Kaur P, et al. Effectiveness of Faradic and Russian currents on plantar flexor muscle spasticity, ankle motor recovery, and functional gait in stroke patients. Physiotherapy Research International : The Journal for Researchers and Clinicians in Physical Therapy. 2018; 23(2):e1705. [DOI:10.1002/pri.1705] [PMID]
- Khorramroo F, Mousavi SH, Minoonejad H, Sorkhabi M. Managing post-operative complications in a patient with excessive ankle stiffness: A case study addressing balance, muscle strength and quality of life. International Journal of of Motor Control and Learning. 2024; 5(4):e146340. [DOI:10.5812/jmcl-146340]
- Stanek J, Sullivan T, Davis S. Comparison of compressive myofascial release and the graston technique for improving ankle-dorsiflexion range of motion. Journal of Athletic Training. 2018; 53(2):160-7. [DOI:10.4085/1062-6050-386-16] [PMID]
- Joseph MF, Taft K, Moskwa M, Denegar CR. Deep friction massage to treat tendinopathy: a systematic review of a classic treatment in the face of a new paradigm of understanding. Journal of Sport Rehabilitation. 2012; 21(4):343-53. [DOI:10.1123/jsr.21.4.343] [PMID]
- Beurer. EM49 Digital TENS EMS Device. UK: Beurer; 2024. [Link]
- Baniasad M, Farahmand F, Arazpour M, Zohoor H. Coordinated activities of trunk and upper extremity muscles during walker-assisted paraplegic gait: A synergy study. Human Movement Science. 2018; 62:184-93. [DOI:10.1016/j.humov.2018.10.002] [PMID]
- Lee HS, Lee JH, Kim HS. Activities of ankle muscles during gait analyzed by simulation using the human musculoskeletal model. Journal of Exercise Rehabilitation. 2019; 15(2):229-34. [DOI:10.12965/jer.1938054.027] [PMID]
- Hunt AE, Smith RM. Mechanics and control of the flat versus normal foot during the stance phase of walking. Clinical Biomechanics. 2004; 19(4):391-7. [DOI:10.1016/j.clinbiomech.2003.12.010] [PMID]
- Yaserifar M, Fallah Mohammadi Z, Hosseininejad SE, Paeen Afrakoti IE, Meijer K, Boonstra TW. Coordination variability reduced for soccer players compared to non-athletes during the stance phase of gait. The Journal of Sports Medicine and Physical Fitness. 2023; 63(5):630-8. [PMID]
- Ferber R, Davis IM, Williams DS. Effect of foot orthotics on rearfoot and tibia joint coupling patterns and variability. Journal of Biomechanics. 2005; 38(3):477-83. [DOI:10.1016/j.jbiomech.2004.04.019] [PMID]
- Yen SC, Chui KK, Corkery MB, Allen EA, Cloonan CM. Hip-ankle coordination during gait in individual’s with chronic ankle instability. Gait and Posture. 2017; 53:193-200. [DOI:10.1016/j.gaitpost.2017.02.001] [PMID]
Type of Study: case report |
Subject:
Sport injury and corrective exercises
Received: 2024/02/27 | Accepted: 2024/07/14 | Published: 2024/10/1
Received: 2024/02/27 | Accepted: 2024/07/14 | Published: 2024/10/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |