Tue, Nov 11, 2025
Volume 14, Issue 4 (Autumn 2024)
PTJ 2024, 14(4): 303-310 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sedaghati P, Alghosi M, Hosseini F, Ghafouri M, Fallahi Farrash F, Parvaneh Sarand A. Correlation Between Sagittal Plane Curvature of the Upright Human Spine and Postural Stability in Adults. PTJ 2024; 14 (4) :303-310
URL: http://ptj.uswr.ac.ir/article-1-629-en.html
URL: http://ptj.uswr.ac.ir/article-1-629-en.html
Parisa Sedaghati1 

 , Mohammad Alghosi1
, Mohammad Alghosi1 

 , Fereshteh Hosseini1
, Fereshteh Hosseini1 
 , Mohammad Ghafouri1
, Mohammad Ghafouri1 
 , Fatemeh Fallahi Farrash1
, Fatemeh Fallahi Farrash1 
 , Ali Parvaneh Sarand *1
, Ali Parvaneh Sarand *1 




 , Mohammad Alghosi1
, Mohammad Alghosi1 

 , Fereshteh Hosseini1
, Fereshteh Hosseini1 
 , Mohammad Ghafouri1
, Mohammad Ghafouri1 
 , Fatemeh Fallahi Farrash1
, Fatemeh Fallahi Farrash1 
 , Ali Parvaneh Sarand *1
, Ali Parvaneh Sarand *1 


1- Department of Sports Injury and Corrective Exercise, Faculty of Physical Education and Sports Sciences, University of Guilan, Rasht, Iran.
Full-Text [PDF 591 kb]
(662 Downloads)
| Abstract (HTML) (2907 Views)
Full-Text: (475 Views)
Introduction
The human spine is a complex structure that continuously adapts, especially during the critical developmental phases of adolescence and early adulthood. Sagittal plane curvature, including cervical and lumbar lordosis and thoracic kyphosis, is essential for spinal alignment, mobility, and postural stability [1]. Understanding the relationship between sagittal plane curvature and postural stability, especially in the context of gender differences, is essential for optimizing musculoskeletal health and preventing postural-related disorders in young adults [2]. Research on the disparities in spinal curvatures between genders has attracted considerable interest in recent years. Studies have highlighted differences in sagittal plane curvature between men and women that are attributed to biomechanical and anthropometric factors [3]. For example, women frequently display greater lumbar lordosis and thoracic kyphosis than men, while men exhibit more pronounced cervical lordosis [4, 5]. Gender disparities in spinal curvatures may contribute to variations in postural stability and susceptibility to musculoskeletal conditions [3]. While the relationship between gender and spinal curvatures has been studied, there remains limited consensus on its implications for postural stability, particularly in young adults. Recent advancements in biomechanical assessments and postural analysis techniques provide opportunities to clarify these relationships with greater precision and objectivity. To address this gap, we propose a cross-sectional study examining the correlation between sagittal plane curvature and postural stability in young adults of both genders. Our study will utilize cutting-edge methodologies, including three-dimensional spinal imaging, surface electromyography, and force platform analysis, to evaluate spinal curvature parameters and postural stability metrics in a cohort of young adults. By exploring gender-specific patterns of sagittal plane curvature and their relationship with postural stability parameters, we aim to offer novel insights into musculoskeletal health disparities and guide targeted interventions to enhance postural control and mitigate the risk of spinal disorders in young men and women.
Through comprehensive analysis and interpretation of our results, we aspire to advance the understanding of gender differences in spinal curvatures and their influence on postural stability. Ultimately, our research aims to contribute to evidence-based strategies to promote musculoskeletal health and well-being among young adults.
Materials and Methods
Design
We conducted a cross-sectional study to examine the correlation between sagittal plane curvature and postural stability in young adults. We adhered to the guidelines set forth by strengthening the reporting of observational studies in epidemiology [6] when compiling our report. The research was conducted in the laboratory of the Faculty of Physical Education and Sport Sciences at the University of Guilan from May 2023 to July 2023. All participants voluntarily agreed to participate in the study and were given a thorough explanation of the research objectives. They provided their consent by signing a written document, by the principles outlined in the Declaration of Helsinki.
Participants
The statistical population of this study comprised all recreationally active university students who volunteered to participate. Before conducting the study, a power analysis was performed using G*Power software, version 3.1. This analysis determined that a sample size of 108 participants was necessary to achieve 80% statistical power, with an α level of 0.05 and an effect size of 0.56 for a standard two-tailed hypothesis [7]. To account for potential dropouts (10% dropout rate), the target recruitment sample size was increased to 120 participants. The study’s participants were categorized by gender, with 60 male and 60 female individuals in each group. The study included participants who were between the ages of 18 and 35 years, regularly engaged in physical activity for a minimum of 30 minutes per session, at least four times per week (definition of a recreationally active adult) [8], not exhibiting any noticeable musculoskeletal abnormalities, having no history of surgery in the trunk or lower extremity and having no visual, vestibular or neuromuscular impairments.
Research instruments and procedures
In our study, we utilized the approach proposed by Salisbury and Porter [9] to measure spinal curvature angles. Specifically, we measured the kyphosis angle by assessing the T2 and T12 vertebrae, while the lordosis angle was determined by referencing the T12 and S2 points. The palpation method, used to identify vertebral levels, demonstrated a high accuracy rate of 97%. The participants were positioned in a natural standing posture with their legs shoulder-width apart and their backs facing the examiner. They were instructed to maintain a forward gaze to facilitate the identification of the spinous processes. To locate the C7 spinous process, the participant was asked to bend their head down while the examiner placed their index and middle fingers over the two vertebrae protruding from the neck. The participant was then asked to perform neck extension; during this movement, the C7 spinous process remained under the examiner’s fingers. From this point, the T2 vertebra was located by counting down. To identify the T12 vertebra, the participant was asked to place their hands on the edge of the table and shift their body weight onto their hands, which allowed for proper identification of the T12 vertebra [10]. Then, Youdas’s instruction was followed [11]. The location of the T12 spinous process was estimated by palpating the bottom edge of the 12th rib with the thumb and moving upward and inward until it disappeared into soft tissue. A straight line was then drawn from the tip of the finger at the last palpable point to the midline of the spine [12]. The posterior superior iliac spine, located in the posterior hip region, was identified by two dimples. These dimples were located through tactile examination using the index and middle fingers to determine the S2 point [13]. Connecting these points with a line would lead to the S2 spinous process. After the desired vertebrae were identified and marked, a flexible ruler (calibrated in 1/16-inch measurements on one side and 1 mm increments on the other side. Made of plastic) was placed on them with some pressure, and then T2, T12, and S2 points were identified on the ruler. Without altering the ruler’s position, it was transferred to a screen board with the side in contact with the skin facing up. A schematic representation of the ruler was drawn on paper, and subsequently, the T2 and T12 points were connected before linking the T12 and S2 points. The resulting measurements for thoracic length, lumbar length, and deepest arcs were then substituted for L and H in Equation 1 to calculate the angles [10].
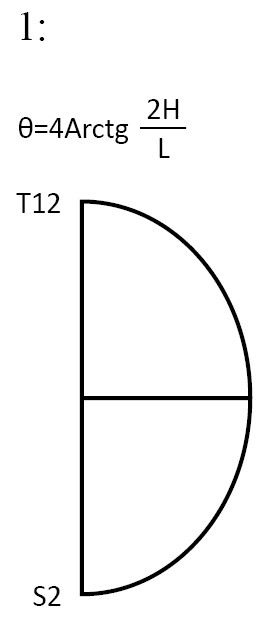
θ: Thoracic or lumbar angle, L: Arc length, H: The longest point curve drawn from a straight line (arc width).
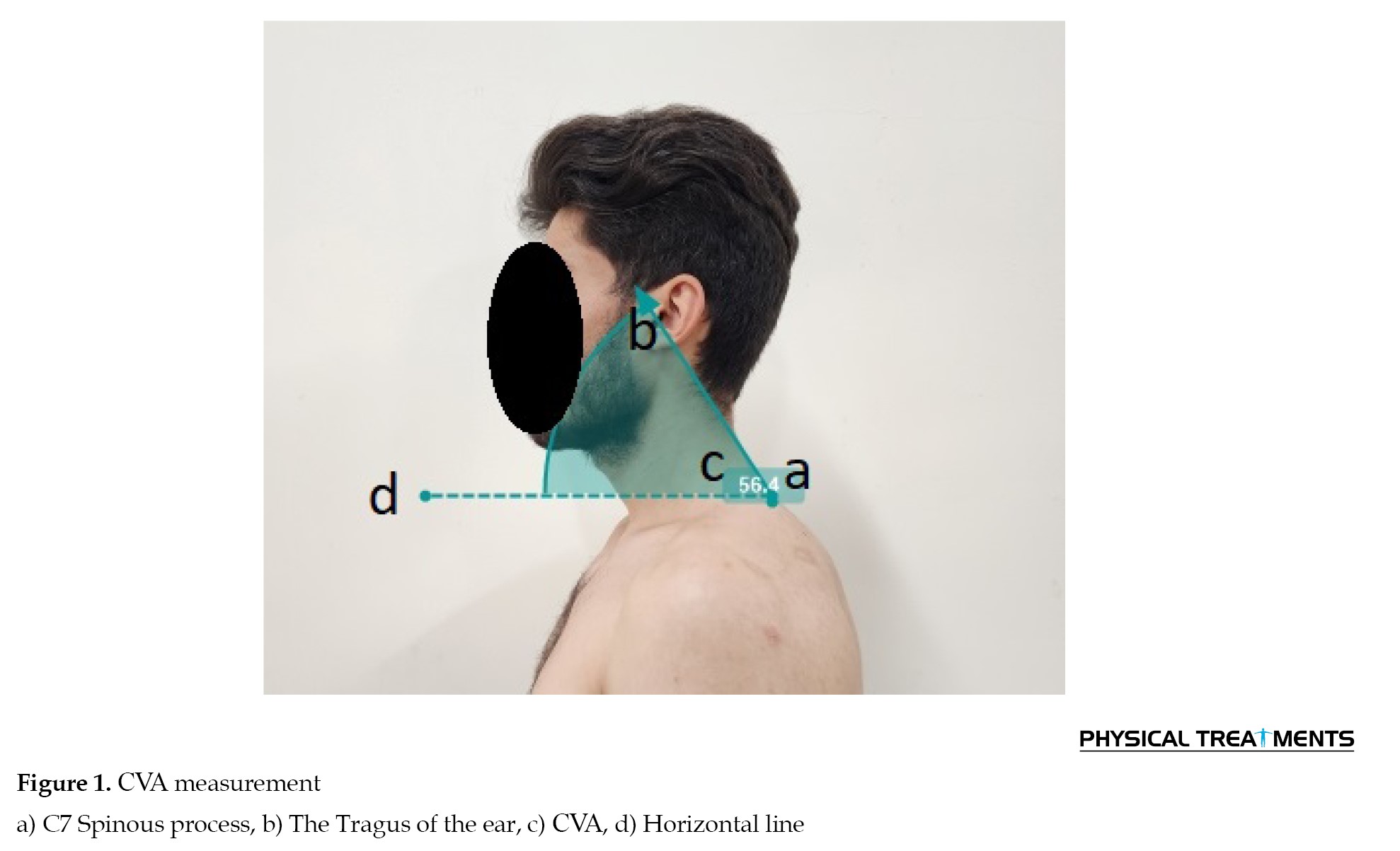
The craniovertebral angle (CVA) was measured using a valid and reliable photographic method, following the measurement protocol established by Falla et al. [14]. A lateral view image was captured with the participants sitting on a chair, allowing for the establishment of the CVA. A digital camera (Xiaomi Note 10 Pro mobile) mounted on a tripod was placed 0.8 meters away from the individual. The camera lens axis was perpendicular to the individual’s sagittal plane at a height corresponding to the seventh cervical vertebrae. Markers were attached to the tragus of the ear and the spinous processes of the seventh cervical vertebrae and securely fixed. The CVA was measured as the angle between a line drawn from the tragus of the ear to the seventh cervical vertebrae and a horizontal line, using the Kinovea software, (Figure 1). To measure postural stability, the balance error scoring system (BESS) was utilized [15]. This tool has been utilized in previous research conducted among recreationally active individuals, defined as those engaging in physical activity for at least 30 minutes, a minimum of four times per week, as reported in previous studies [8, 16]. The BESS comprised three stances, double-leg stance, single-leg stance, and tandem stance. These stances were performed on both a firm surface and a medium-density foam block (Danesh Salar Iranian Co., Tehran, Iran), with eyes closed, resulting in six conditions. Each trial lasted for 20 s, measured using a stopwatch. Errors were counted based on predefined criteria, including actions, such as opening eyes, lifting hands off hips, stepping, stumbling or falling out of position, lifting forefoot or heel, abducting the hip by more than 30°, or failing to return to the test position within a timeframe of 5 seconds [15]. The error scores from each of the six conditions were aggregated to derive the total BESS score. Participants were instructed to assume a tandem stance, with their nondominant foot positioned behind the dominant foot while maintaining contact between their great toe and heel. They were directed to remain motionless with their eyes closed and hands on hips throughout all conditions. Before data collection, each participant completed two familiarization trials for each condition. To maintain scoring consistency, a single examiner positioned 2.5-3 m from the participant observed the eyes, hips, and feet simultaneously, and scored all participants and trials [8, 16]. Intra-tester reliability was established by videotaping and subsequently scoring both live and recorded conditions. The resulting intra-class correlation coefficient for total BESS scores was 0.92, indicating strong consistency in scoring.
Before participating in the study, all participants provided written consent, signifying their voluntary agreement to take part. Additionally, participants were informed of their right to withdraw from the study at any point without facing negative consequences. Ethical considerations guided the study to ensure participant confidentiality and privacy. Data collected from participants were handled with utmost care, and securely stored, and any identifying information was strictly kept confidential.
Data analysis
Data were analyzed using IBM SPSS (IBM Corp. Released 2021. IBM SPSS Statistics for Windows, Version 28.0. Armonk, NY: IBM Corp). The Shapiro-Wilk test was employed to assess the normality of the data distribution. Descriptive statistics, including Mean±SD, were calculated for the study variables. Correlation analyses were conducted using Pearson’s and Spearman’s tests at a significance level of P≤0.05 to examine relationships between variables.
Results
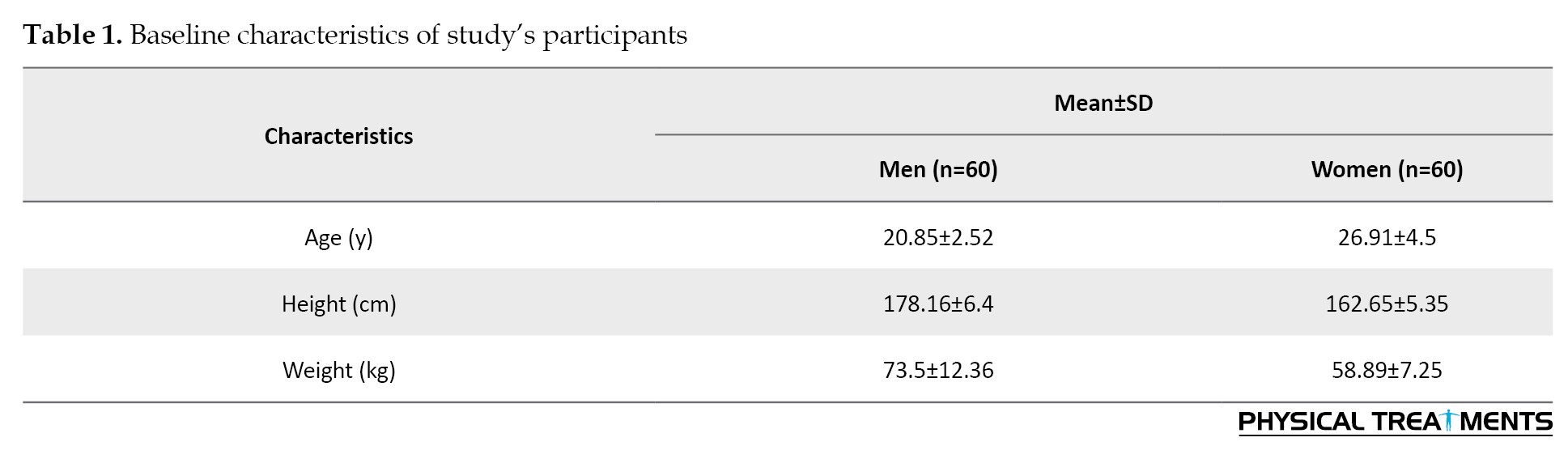
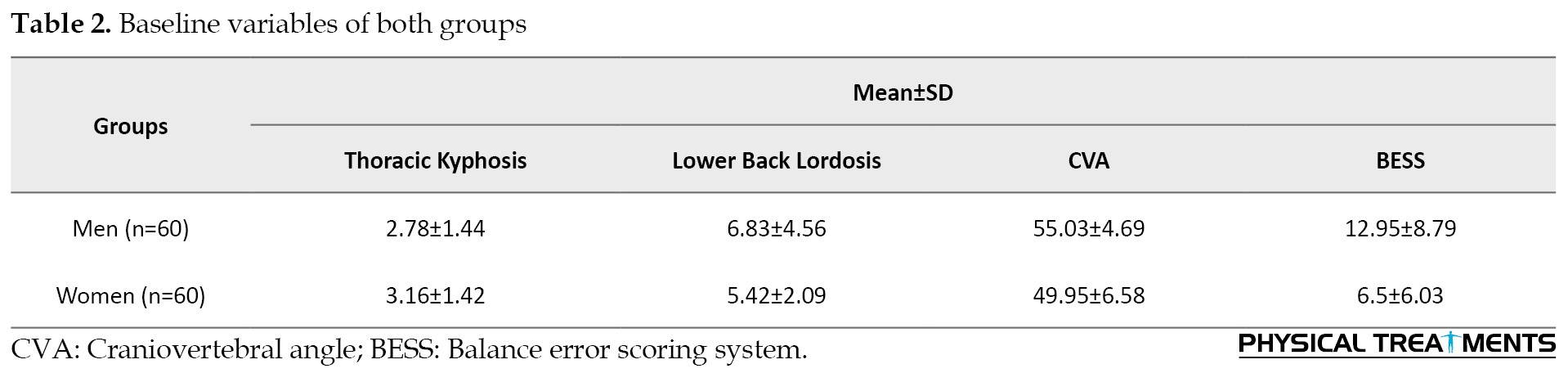
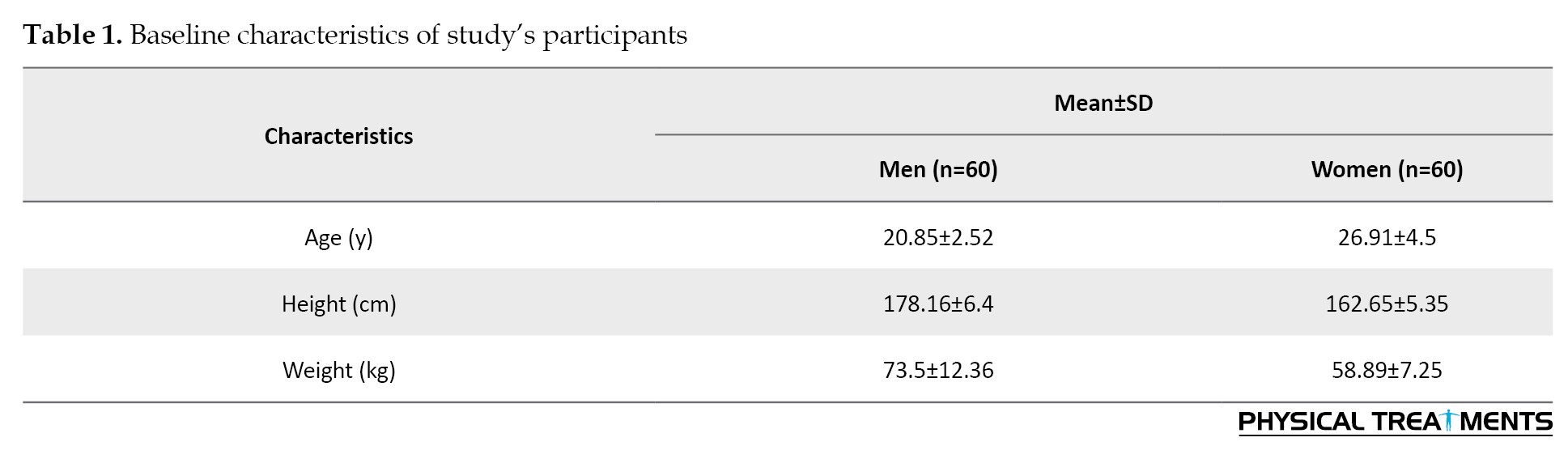
Table 1 presents the baseline study participant’s characteristics, and Table 2 presents the baseline variables that were examined in both groups.
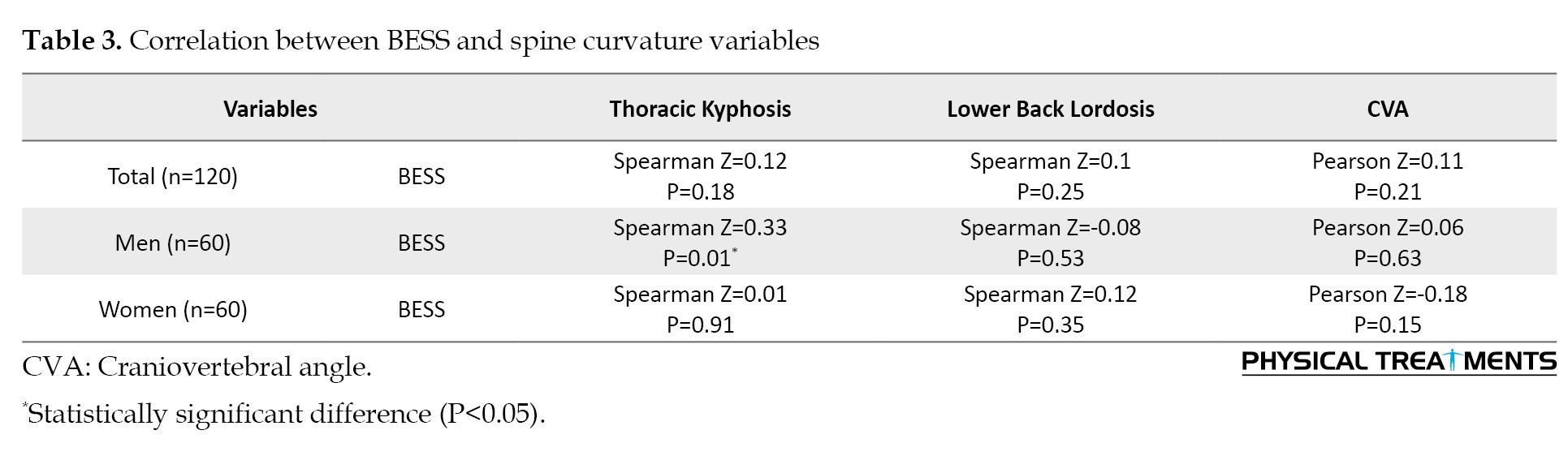
Based on the results of the normality test, it was determined that all variables, except for CVA, had a non-normal distribution. Consequently, Pearson’s correlation coefficient was utilized to examine the relationship between CVA and BESS, while Spearman’s rank correlation coefficient was employed for the remaining variables.
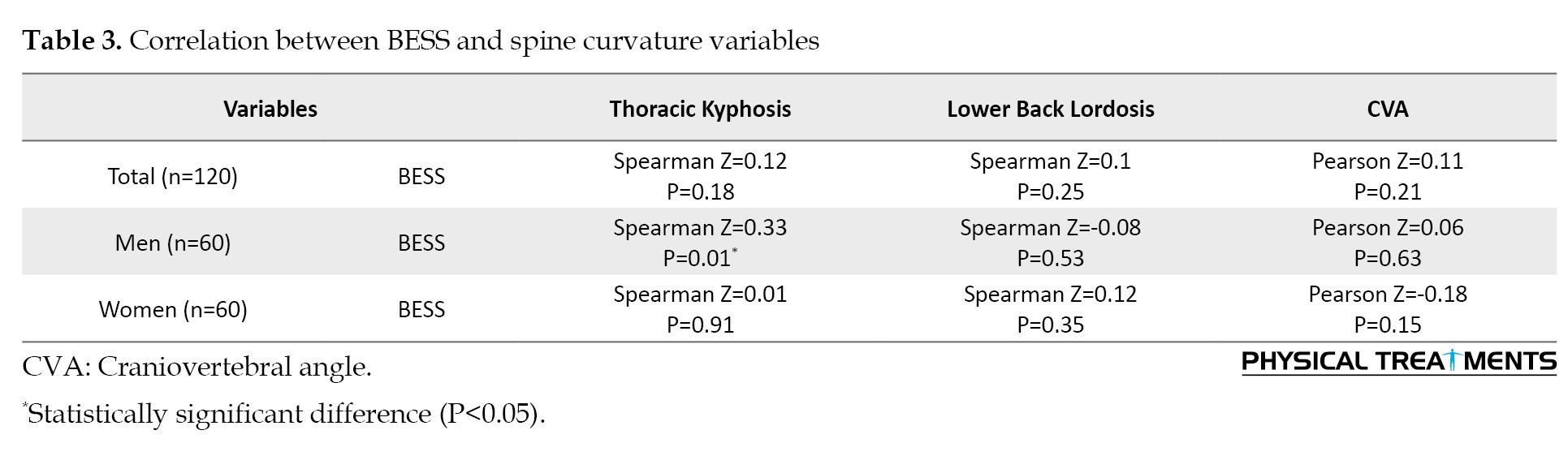
We examined the relationship between BESS and kyphosis, lower back lordosis, and CVA. The results revealed no significant relationships between these variables, except for the male group, where a significant relationship was observed between BESS and kyphosis (Table 3).
Discussion
This study was conducted to investigate the relationship between spinal curvature and postural stability for optimal spinal health. The results showed no significant relationships between thoracic kyphosis, lower back lordosis, and CVA with BESS scores, except for the male group, where a significant relationship was observed between BESS and kyphosis (P=0.01). Nault et al. [17] demonstrated that increasing thoracic kyphosis is associated with greater displacement of the center of gravity, while Norasteh et al. [18] found that higher degrees of kyphosis lead to reduced static and dynamic balance. Indeed, hyperkyphosis is associated with lower balance compared to hypokyphosis [18]. One potential reason for this decline in balance with increased kyphosis can be the forward and downward shift of the body’s center of gravity. This shift alters the body’s biomechanics, making it more challenging to maintain stability and balance [5, 19]. Additionally, the risk of falls due to poor balance increases with kyphosis in older adults [20]. Eshraghi et al. [21] analyzed the balance in adolescent girls with hyperkyphosis and observed differences compared to those without posture issues. They found that gender and age influence balance parameters, with girls typically performing better in static balance tests, while boys excelled in dynamic balance tests. Indeed, these results underscore the nuanced relationship between gender, age, and balance performance, highlighting the necessity of considering these factors when evaluating postural stability. By recognizing the influence of gender and age on balance parameters, healthcare professionals can tailor interventions and strategies to address individual needs effectively, ultimately promoting better postural health outcomes [22]. However, Sedaghati et al. [23] found no correlation between kyphosis and postural control.
In our study, we observed no relationship between lordosis and BESS scores among young athletes. This lack of correlation can potentially be attributed to their extensive sports participation, which may have contributed to their adept postural control and stability. Previous research has suggested that lumbar kyphosis, rather than thoracic kyphosis, is associated with postural instability, especially in elderly osteoporotic patients. These results highlighted the multifactorial nature of postural stability and suggested that different factors may influence balance outcomes across various populations and age groups [24]. Lumbar kyphosis indeed has a more significant impact on spine posture compared to thoracic kyphosis. Changes in the lumbar lordosis angle have been found to correlate with various balance parameters. This suggests that alterations in lumbar curvature may play a crucial role in determining postural stability and balance outcomes. Understanding these relationships can help inform interventions aimed at optimizing spinal alignment and improving overall postural control [24].
In the present study, no significant relationship was found between CVA and BESS scores among young athletes. However, CVA and spine curvature are interconnected parameters that play significant roles in spinal alignment, biomechanics, and clinical outcomes. Research suggests that alterations in CVA and spine curvature may be associated with various musculoskeletal conditions, including scoliosis, low back pain, and cervico-craniofacial pain. Understanding the relationship between these parameters and their implications for musculoskeletal health is crucial for informing clinical assessment, treatment planning, and rehabilitation strategies [25]. Research has delved into the relationship between CVA and BESS scores, a widely used tool to assess postural stability. Brascher et al. explored the relationship between CVA posture and clinical features in patients with cervico-craniofacial pain. They discovered the relationships between abnormal CVA and symptoms, such as headaches and temporomandibular joint disorders, underscoring the significance of evaluating CVA alignment in patients with neck and craniofacial pain. This emphasizes the intricate connection between CVA posture and musculoskeletal symptoms, shedding light on the importance of comprehensive assessment and management strategies for individuals with such conditions [26]. While the direct relationship between CVA and BESS scores has not been extensively studied, understanding the role of CVA posture in musculoskeletal function and symptomatology can offer valuable insights into postural stability and balance. Further research is warranted to elucidate the specific relationship between CVA and BESS scores in various populations and clinical contexts.
The study’s main limitations include the small sample size, which may hinder the ability to fully assess the correlation between sagittal plane curvature of the upright human spine and postural stability. Additionally, the study assessed CVA instead of the forward head angle, which can provide valuable insights into the relationship between head and neck positioning and overall spinal alignment. The wide age range of the participants may have introduced additional variability in the results, as spinal curvatures and postural stability can vary significantly with age. Furthermore, the reliance on self-reported data about participants’ medical history, including any history of surgery in the trunk or lower extremity and the absence of visual, vestibular or neuromuscular impairments, may not capture all relevant medical conditions that could potentially influence the study outcomes. To address these limitations, future studies can benefit from evaluating these spinal angles in both young and older non-athlete populations to enhance our understanding of their role in postural stability and balance across different age groups, while also considering a larger sample size and more comprehensive medical assessments to ensure a more robust and reliable analysis of the relationship between sagittal plane spinal curvature and postural stability.
Conclusion
According to our study’s results, we discovered no significant correlations between BESS and lower back lordosis or CVA. However, a notable relationship was observed between BESS and kyphosis among male recreational active adults. These results imply that thoracic kyphosis can be a crucial element in evaluating postural stability in recreational adult populations, given the relationship between spinal curvature, particularly kyphosis angle, and balance. Additional research is warranted to validate these results and investigate possible interventions targeting balance improvement in recreational adults with kyphosis.
Ethical Considerations
Compliance with ethical guidelines
The study received approval from the Research Ethics Committee of the Sport Science Research Institute of Iran (Code: IR.SSRC.REC.1402.096, Date: 2023/08/22). Participants were briefed on the research’s objectives and the stages of its execution. They were assured of the confidentiality of their information and had the freedom to withdraw from the study at any point. Additionally, participants were informed that they could access the research results upon request.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
The human spine is a complex structure that continuously adapts, especially during the critical developmental phases of adolescence and early adulthood. Sagittal plane curvature, including cervical and lumbar lordosis and thoracic kyphosis, is essential for spinal alignment, mobility, and postural stability [1]. Understanding the relationship between sagittal plane curvature and postural stability, especially in the context of gender differences, is essential for optimizing musculoskeletal health and preventing postural-related disorders in young adults [2]. Research on the disparities in spinal curvatures between genders has attracted considerable interest in recent years. Studies have highlighted differences in sagittal plane curvature between men and women that are attributed to biomechanical and anthropometric factors [3]. For example, women frequently display greater lumbar lordosis and thoracic kyphosis than men, while men exhibit more pronounced cervical lordosis [4, 5]. Gender disparities in spinal curvatures may contribute to variations in postural stability and susceptibility to musculoskeletal conditions [3]. While the relationship between gender and spinal curvatures has been studied, there remains limited consensus on its implications for postural stability, particularly in young adults. Recent advancements in biomechanical assessments and postural analysis techniques provide opportunities to clarify these relationships with greater precision and objectivity. To address this gap, we propose a cross-sectional study examining the correlation between sagittal plane curvature and postural stability in young adults of both genders. Our study will utilize cutting-edge methodologies, including three-dimensional spinal imaging, surface electromyography, and force platform analysis, to evaluate spinal curvature parameters and postural stability metrics in a cohort of young adults. By exploring gender-specific patterns of sagittal plane curvature and their relationship with postural stability parameters, we aim to offer novel insights into musculoskeletal health disparities and guide targeted interventions to enhance postural control and mitigate the risk of spinal disorders in young men and women.
Through comprehensive analysis and interpretation of our results, we aspire to advance the understanding of gender differences in spinal curvatures and their influence on postural stability. Ultimately, our research aims to contribute to evidence-based strategies to promote musculoskeletal health and well-being among young adults.
Materials and Methods
Design
We conducted a cross-sectional study to examine the correlation between sagittal plane curvature and postural stability in young adults. We adhered to the guidelines set forth by strengthening the reporting of observational studies in epidemiology [6] when compiling our report. The research was conducted in the laboratory of the Faculty of Physical Education and Sport Sciences at the University of Guilan from May 2023 to July 2023. All participants voluntarily agreed to participate in the study and were given a thorough explanation of the research objectives. They provided their consent by signing a written document, by the principles outlined in the Declaration of Helsinki.
Participants
The statistical population of this study comprised all recreationally active university students who volunteered to participate. Before conducting the study, a power analysis was performed using G*Power software, version 3.1. This analysis determined that a sample size of 108 participants was necessary to achieve 80% statistical power, with an α level of 0.05 and an effect size of 0.56 for a standard two-tailed hypothesis [7]. To account for potential dropouts (10% dropout rate), the target recruitment sample size was increased to 120 participants. The study’s participants were categorized by gender, with 60 male and 60 female individuals in each group. The study included participants who were between the ages of 18 and 35 years, regularly engaged in physical activity for a minimum of 30 minutes per session, at least four times per week (definition of a recreationally active adult) [8], not exhibiting any noticeable musculoskeletal abnormalities, having no history of surgery in the trunk or lower extremity and having no visual, vestibular or neuromuscular impairments.
Research instruments and procedures
In our study, we utilized the approach proposed by Salisbury and Porter [9] to measure spinal curvature angles. Specifically, we measured the kyphosis angle by assessing the T2 and T12 vertebrae, while the lordosis angle was determined by referencing the T12 and S2 points. The palpation method, used to identify vertebral levels, demonstrated a high accuracy rate of 97%. The participants were positioned in a natural standing posture with their legs shoulder-width apart and their backs facing the examiner. They were instructed to maintain a forward gaze to facilitate the identification of the spinous processes. To locate the C7 spinous process, the participant was asked to bend their head down while the examiner placed their index and middle fingers over the two vertebrae protruding from the neck. The participant was then asked to perform neck extension; during this movement, the C7 spinous process remained under the examiner’s fingers. From this point, the T2 vertebra was located by counting down. To identify the T12 vertebra, the participant was asked to place their hands on the edge of the table and shift their body weight onto their hands, which allowed for proper identification of the T12 vertebra [10]. Then, Youdas’s instruction was followed [11]. The location of the T12 spinous process was estimated by palpating the bottom edge of the 12th rib with the thumb and moving upward and inward until it disappeared into soft tissue. A straight line was then drawn from the tip of the finger at the last palpable point to the midline of the spine [12]. The posterior superior iliac spine, located in the posterior hip region, was identified by two dimples. These dimples were located through tactile examination using the index and middle fingers to determine the S2 point [13]. Connecting these points with a line would lead to the S2 spinous process. After the desired vertebrae were identified and marked, a flexible ruler (calibrated in 1/16-inch measurements on one side and 1 mm increments on the other side. Made of plastic) was placed on them with some pressure, and then T2, T12, and S2 points were identified on the ruler. Without altering the ruler’s position, it was transferred to a screen board with the side in contact with the skin facing up. A schematic representation of the ruler was drawn on paper, and subsequently, the T2 and T12 points were connected before linking the T12 and S2 points. The resulting measurements for thoracic length, lumbar length, and deepest arcs were then substituted for L and H in Equation 1 to calculate the angles [10].
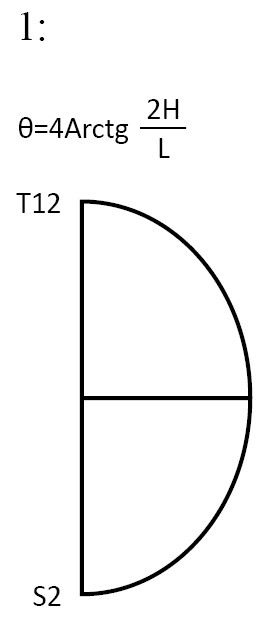
θ: Thoracic or lumbar angle, L: Arc length, H: The longest point curve drawn from a straight line (arc width).
The craniovertebral angle (CVA) was measured using a valid and reliable photographic method, following the measurement protocol established by Falla et al. [14]. A lateral view image was captured with the participants sitting on a chair, allowing for the establishment of the CVA. A digital camera (Xiaomi Note 10 Pro mobile) mounted on a tripod was placed 0.8 meters away from the individual. The camera lens axis was perpendicular to the individual’s sagittal plane at a height corresponding to the seventh cervical vertebrae. Markers were attached to the tragus of the ear and the spinous processes of the seventh cervical vertebrae and securely fixed. The CVA was measured as the angle between a line drawn from the tragus of the ear to the seventh cervical vertebrae and a horizontal line, using the Kinovea software, (Figure 1). To measure postural stability, the balance error scoring system (BESS) was utilized [15]. This tool has been utilized in previous research conducted among recreationally active individuals, defined as those engaging in physical activity for at least 30 minutes, a minimum of four times per week, as reported in previous studies [8, 16]. The BESS comprised three stances, double-leg stance, single-leg stance, and tandem stance. These stances were performed on both a firm surface and a medium-density foam block (Danesh Salar Iranian Co., Tehran, Iran), with eyes closed, resulting in six conditions. Each trial lasted for 20 s, measured using a stopwatch. Errors were counted based on predefined criteria, including actions, such as opening eyes, lifting hands off hips, stepping, stumbling or falling out of position, lifting forefoot or heel, abducting the hip by more than 30°, or failing to return to the test position within a timeframe of 5 seconds [15]. The error scores from each of the six conditions were aggregated to derive the total BESS score. Participants were instructed to assume a tandem stance, with their nondominant foot positioned behind the dominant foot while maintaining contact between their great toe and heel. They were directed to remain motionless with their eyes closed and hands on hips throughout all conditions. Before data collection, each participant completed two familiarization trials for each condition. To maintain scoring consistency, a single examiner positioned 2.5-3 m from the participant observed the eyes, hips, and feet simultaneously, and scored all participants and trials [8, 16]. Intra-tester reliability was established by videotaping and subsequently scoring both live and recorded conditions. The resulting intra-class correlation coefficient for total BESS scores was 0.92, indicating strong consistency in scoring.
Before participating in the study, all participants provided written consent, signifying their voluntary agreement to take part. Additionally, participants were informed of their right to withdraw from the study at any point without facing negative consequences. Ethical considerations guided the study to ensure participant confidentiality and privacy. Data collected from participants were handled with utmost care, and securely stored, and any identifying information was strictly kept confidential.
Data analysis
Data were analyzed using IBM SPSS (IBM Corp. Released 2021. IBM SPSS Statistics for Windows, Version 28.0. Armonk, NY: IBM Corp). The Shapiro-Wilk test was employed to assess the normality of the data distribution. Descriptive statistics, including Mean±SD, were calculated for the study variables. Correlation analyses were conducted using Pearson’s and Spearman’s tests at a significance level of P≤0.05 to examine relationships between variables.
Results
Table 1 presents the baseline study participant’s characteristics, and Table 2 presents the baseline variables that were examined in both groups.
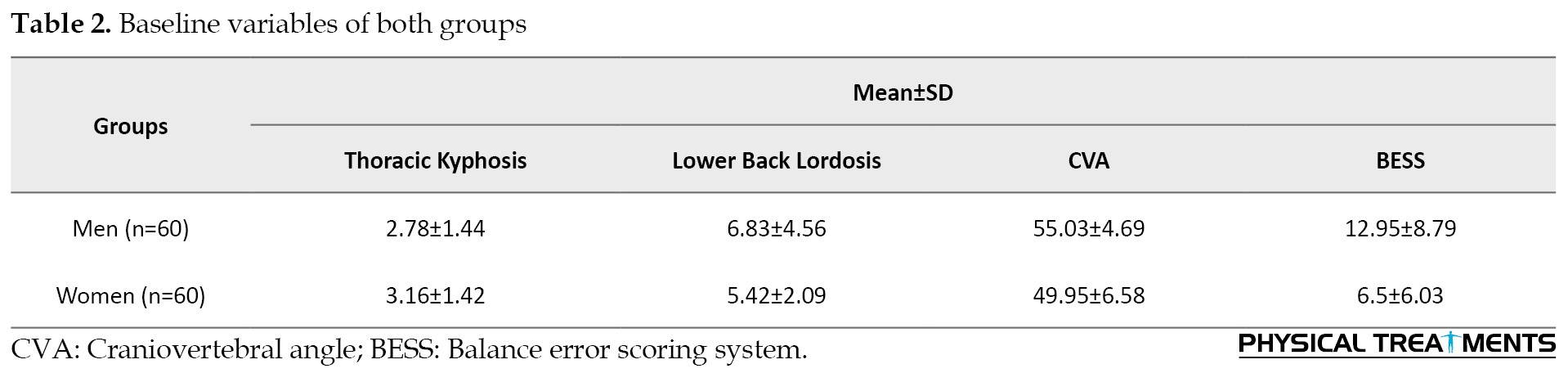
Based on the results of the normality test, it was determined that all variables, except for CVA, had a non-normal distribution. Consequently, Pearson’s correlation coefficient was utilized to examine the relationship between CVA and BESS, while Spearman’s rank correlation coefficient was employed for the remaining variables.
We examined the relationship between BESS and kyphosis, lower back lordosis, and CVA. The results revealed no significant relationships between these variables, except for the male group, where a significant relationship was observed between BESS and kyphosis (Table 3).
Discussion
This study was conducted to investigate the relationship between spinal curvature and postural stability for optimal spinal health. The results showed no significant relationships between thoracic kyphosis, lower back lordosis, and CVA with BESS scores, except for the male group, where a significant relationship was observed between BESS and kyphosis (P=0.01). Nault et al. [17] demonstrated that increasing thoracic kyphosis is associated with greater displacement of the center of gravity, while Norasteh et al. [18] found that higher degrees of kyphosis lead to reduced static and dynamic balance. Indeed, hyperkyphosis is associated with lower balance compared to hypokyphosis [18]. One potential reason for this decline in balance with increased kyphosis can be the forward and downward shift of the body’s center of gravity. This shift alters the body’s biomechanics, making it more challenging to maintain stability and balance [5, 19]. Additionally, the risk of falls due to poor balance increases with kyphosis in older adults [20]. Eshraghi et al. [21] analyzed the balance in adolescent girls with hyperkyphosis and observed differences compared to those without posture issues. They found that gender and age influence balance parameters, with girls typically performing better in static balance tests, while boys excelled in dynamic balance tests. Indeed, these results underscore the nuanced relationship between gender, age, and balance performance, highlighting the necessity of considering these factors when evaluating postural stability. By recognizing the influence of gender and age on balance parameters, healthcare professionals can tailor interventions and strategies to address individual needs effectively, ultimately promoting better postural health outcomes [22]. However, Sedaghati et al. [23] found no correlation between kyphosis and postural control.
In our study, we observed no relationship between lordosis and BESS scores among young athletes. This lack of correlation can potentially be attributed to their extensive sports participation, which may have contributed to their adept postural control and stability. Previous research has suggested that lumbar kyphosis, rather than thoracic kyphosis, is associated with postural instability, especially in elderly osteoporotic patients. These results highlighted the multifactorial nature of postural stability and suggested that different factors may influence balance outcomes across various populations and age groups [24]. Lumbar kyphosis indeed has a more significant impact on spine posture compared to thoracic kyphosis. Changes in the lumbar lordosis angle have been found to correlate with various balance parameters. This suggests that alterations in lumbar curvature may play a crucial role in determining postural stability and balance outcomes. Understanding these relationships can help inform interventions aimed at optimizing spinal alignment and improving overall postural control [24].
In the present study, no significant relationship was found between CVA and BESS scores among young athletes. However, CVA and spine curvature are interconnected parameters that play significant roles in spinal alignment, biomechanics, and clinical outcomes. Research suggests that alterations in CVA and spine curvature may be associated with various musculoskeletal conditions, including scoliosis, low back pain, and cervico-craniofacial pain. Understanding the relationship between these parameters and their implications for musculoskeletal health is crucial for informing clinical assessment, treatment planning, and rehabilitation strategies [25]. Research has delved into the relationship between CVA and BESS scores, a widely used tool to assess postural stability. Brascher et al. explored the relationship between CVA posture and clinical features in patients with cervico-craniofacial pain. They discovered the relationships between abnormal CVA and symptoms, such as headaches and temporomandibular joint disorders, underscoring the significance of evaluating CVA alignment in patients with neck and craniofacial pain. This emphasizes the intricate connection between CVA posture and musculoskeletal symptoms, shedding light on the importance of comprehensive assessment and management strategies for individuals with such conditions [26]. While the direct relationship between CVA and BESS scores has not been extensively studied, understanding the role of CVA posture in musculoskeletal function and symptomatology can offer valuable insights into postural stability and balance. Further research is warranted to elucidate the specific relationship between CVA and BESS scores in various populations and clinical contexts.
The study’s main limitations include the small sample size, which may hinder the ability to fully assess the correlation between sagittal plane curvature of the upright human spine and postural stability. Additionally, the study assessed CVA instead of the forward head angle, which can provide valuable insights into the relationship between head and neck positioning and overall spinal alignment. The wide age range of the participants may have introduced additional variability in the results, as spinal curvatures and postural stability can vary significantly with age. Furthermore, the reliance on self-reported data about participants’ medical history, including any history of surgery in the trunk or lower extremity and the absence of visual, vestibular or neuromuscular impairments, may not capture all relevant medical conditions that could potentially influence the study outcomes. To address these limitations, future studies can benefit from evaluating these spinal angles in both young and older non-athlete populations to enhance our understanding of their role in postural stability and balance across different age groups, while also considering a larger sample size and more comprehensive medical assessments to ensure a more robust and reliable analysis of the relationship between sagittal plane spinal curvature and postural stability.
Conclusion
According to our study’s results, we discovered no significant correlations between BESS and lower back lordosis or CVA. However, a notable relationship was observed between BESS and kyphosis among male recreational active adults. These results imply that thoracic kyphosis can be a crucial element in evaluating postural stability in recreational adult populations, given the relationship between spinal curvature, particularly kyphosis angle, and balance. Additional research is warranted to validate these results and investigate possible interventions targeting balance improvement in recreational adults with kyphosis.
Ethical Considerations
Compliance with ethical guidelines
The study received approval from the Research Ethics Committee of the Sport Science Research Institute of Iran (Code: IR.SSRC.REC.1402.096, Date: 2023/08/22). Participants were briefed on the research’s objectives and the stages of its execution. They were assured of the confidentiality of their information and had the freedom to withdraw from the study at any point. Additionally, participants were informed that they could access the research results upon request.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
- Chau LTC, Hu Z, Ko KSY, Man GCW, Yeung KH, Law YY, et al. Global sagittal alignment of the spine, pelvis, lower limb after vertebral compression fracture and its effect on quality of life. BMC Musculoskeletal Disorders. 2021; 22(1):476. [DOI:10.1186/s12891-021-04311-8] [PMID]
- Gong H, Sun L, Yang R, Pang J, Chen B, Qi R, et al. Changes of upright body posture in the sagittal plane of men and women occurring with aging-a cross sectional study. BMC Geriatrics. 2019; 19(1):71. [DOI:10.1186/s12877-019-1096-0] [PMID]
- Puszczałowska-Lizis E, Mól M, Omorczyk J. Inter-gender differences in the formation of anteroposterior spinal curvatures in people practicing ballroom dancing. Acta of Bioengineering and Biomechanics. 2020; 22(4):123-31. [PMID]
- Kedar E, Ezra D, Pelleg-Kallevag R, Stein D, Peled N, May H, et al. Capturing the cervical spine shape: Angular measurements versus geometric morphometric methods. Clinical Anatomy (New York, N.Y.). 2024. [DOI:10.1002/ca.24166] [PMID]
- Youssef H. [The effect of thoracic kyphosis posture on static balance (MSc thesis) (Turkish)]. İstanbul: Marmara Universitesi; 2021. [Link]
- von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. International Journal of Surgery. 2014; 12(12):1495-9.[DOI:10.1016/j.ijsu.2014.07.013] [PMID]
- Ledolter J, Kardon RH. Focus on data: Statistical design of experiments and sample size selection using power analysis. Investigative Ophthalmology & Visual Science. 2020; 61(8):11. [DOI:10.1167/iovs.61.8.11] [PMID]
- Susco TM, Valovich McLeod TC, Gansneder BM, Shultz SJ. Balance recovers within 20 minutes after exertion as measured by the balance error scoring system. Journal of Athletic Training. 2004; 39(3):241-6. [PMID]
- Salisbury PJ, Porter RW. Measurement of lumbar sagittal mobility a comparison of methods. Spine (Phila Pa 1976). 1987; 12(2):190-3. [DOI:10.1097/00007632-198703000-00017] [PMID]
- Reshma, Sirajudeen M, Chinnakalai T, Suhail M, al-Hussinan N, Pillai P. Reliability of the flexible ruler in measuring lumbar lordosis among children. Journal of Clinical and Diagnostic Research. 2020; 14(11):1-4. [DOI:10.7860/JCDR/2020/45472.14239]
- Youdas JW, Suman VJ, Garrett TR. Reliability of measurements of lumbar spine sagittal mobility obtained with the flexible curve. The Journal of Orthopaedic and Sports Physical Therapy. 1995; 21(1):13-20. [DOI:10.2519/jospt.1995.21.1.13] [PMID]
- Seidi F, Rajabi R, Ebrahimi T, Tavanai A, Moussavi S. The Iranian flexible ruler reliability and validity in lumbar lordosis measurements. World Journal of Sport Sciences. 2009; 2(2):95-9. [Link]
- Chakraverty R, Pynsent P, Isaacs K. Which spinal levels are identified by palpation of the iliac crests and the posterior superior iliac spines? Journal of Anatomy. 2007; 210(2):232-6. [DOI:10.1111/j.1469-7580.2006.00686.x] [PMID]
- Falla D, Jull G, Russell T, Vicenzino B, Hodges P. Effect of neck exercise on sitting posture in patients with chronic neck pain. Physical Therapy. 2007; 87(4):408-17. [DOI:10.2522/ptj.20060009] [PMID]
- Bell DR, Guskiewicz KM, Clark MA, Padua DA. Systematic review of the balance error scoring system. Sports Health. 2011; 3(3):287-95. [DOI:10.1177/1941738111403122] [PMID]
- Erkmen N, Taşkın H, Kaplan T, Sanioǧlu A. The effect of fatiguing exercise on balance performance as measured by the balance error scoring system. Isokinetics and Exercise Science. 2009; 17(2):121-7. [DOI:10.3233/IES-2009-0343]
- Nault ML, Allard P, Hinse S, Le Blanc R, Caron O, Labelle H, et al. Relations between standing stability and body posture parameters in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2002; 27(17):1911-7. [DOI:10.1097/00007632-200209010-00018] [PMID]
- Norasteh AA, Hosseini R, Daneshmandi H, Shah Heidari S. [Balance assessment in students with hyperkyphosis and hyperlordosis (Persian)]. Sport Sciences and Health Research. 2014; 6(1):57-71. [DOI:10.22059/jsmed.2014.50131]
- Hey HWD, Lin S, Tay HW, Tay YJ, Liu GK, Wong HK. Understanding “Kyphosis” and “Lordosis” for Sagittal Balancing in Two Common Standing Postures. Spine (Phila Pa 1976). 2021; 46(23):1603-11. [DOI:10.1097/BRS.0000000000004106] [PMID]
- McDaniels-Davidson C, Davis A, Wing D, Macera C, Lindsay SP, Schousboe JT, et al. Kyphosis and incident falls among community-dwelling older adults. Osteoporosis International. 2018; 29(1):163-9. [DOI:10.1007/s00198-017-4253-3] [PMID]
- Eshraghi A, Maroufi N, Sanjari M, Keyhani M, Saeedi H. Static & dynamic balance of schoolgirls with hyperkyphosis. Scoliosis. 2009; 4 (Suppl 2):5. [DOI:10.1186/1748-7161-4-S2-O5]
- Odunaiya N, Oladeji O, Oguntibeju O. Assessment of antigravity and postural control in health children in Ibadan, Nigeria. Pakistan Journal of Medical Sciences. 2009; 25(4):583-90. [Link]
- Sedaghati P, Zolghadr H, Daneshmandi H. [Postural control status in relation to anthropometric and postural indices of active people (Persian)]. Journal of Sport Biomechanics. 2019; 5(1):50-61. [DOI:10.32598/biomechanics.5.1.5]
- Ishikawa Y, Miyakoshi N, Kasukawa Y, Hongo M, Shimada Y. Spinal curvature and postural balance in patients with osteoporosis. Osteoporosis International. 2009; 20(12):2049-53. [DOI:10.1007/s00198-009-0919-9] [PMID]
- Hiyama A, Sakai D, Watanabe M, Katoh H, Sato M, Mochida J. Sagittal alignment of the cervical spine in adolescent idiopathic scoliosis: A comparative study of 42 adolescents with idiopathic scoliosis and 24 normal adolescents. European Spine Journal. 2016; 25(10):3226-33. [DOI:10.1007/s00586-016-4701-3] [PMID]
- Brascher AK, Blunk JA, Bauer K, Feldmann R Jr, Benrath J. Comprehensive curriculum for phantom-based training of ultrasound-guided intercostal nerve and stellate ganglion blocks. Pain Medicine. 2014; 15(10):1647-56. [DOI:10.1111/pme.12365] [PMID]
Type of Study: Research |
Subject:
Sport injury and corrective exercises
Received: 2024/02/17 | Accepted: 2024/07/27 | Published: 2024/10/1
Received: 2024/02/17 | Accepted: 2024/07/27 | Published: 2024/10/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |