Fri, Feb 6, 2026
Volume 15, Issue 3 (Summer 2025)
PTJ 2025, 15(3): 183-194 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ashoury H, Yalfani A, Arjipour M. Water Kinetic Exercises’ Effects on Pain, Plantar Pressure, Disability, and Kinesiophobia in Chronic Low Back Pain: An Randomized Clinical Trail. PTJ 2025; 15 (3) :183-194
URL: http://ptj.uswr.ac.ir/article-1-627-en.html
URL: http://ptj.uswr.ac.ir/article-1-627-en.html
1- Department of Sport Pathology and Corrective Movements, Faculty of Sport Sciences, Bu Ali Sina University, Hamedan, Iran. & Department of Physical Education and Sport Sciences, Payame Noor University, Tehran, Iran.
2- Department of Sport Injuries and Corrective Exercises, Faculty of Sport Sciences, Bu-Ali Sina University, Hamedan, Iran.
3- Departments of Neurosurgery, Faculty of Medicine, Hamadan University of Medical Sciences, Hamadan, Iran.
2- Department of Sport Injuries and Corrective Exercises, Faculty of Sport Sciences, Bu-Ali Sina University, Hamedan, Iran.
3- Departments of Neurosurgery, Faculty of Medicine, Hamadan University of Medical Sciences, Hamadan, Iran.
Full-Text [PDF 956 kb]
(534 Downloads)
| Abstract (HTML) (2284 Views)
Full-Text: (391 Views)
Introduction
The prevalence of low back pain (LBP) has been highlighted by the World Health Organization (WHO) as a significant health concern, affecting individuals regularly and leading to a decline in their overall well-being and quality of life (QoL). Moreover, it can hinder their functional abilities, contributing to absenteeism in the workplace, early retirement, and in more severe instances, disabilities [1]. The prevalence of LBP in Iran ranges from 14.4% to 84.1% in various subsets of the population, such as working populations, pregnant women, and students, following world trends [2]. Regardless of the etiology, LBP ranks as the third most frequent contributor to morbidity and disability within the Iranian population aged 15–69 [2]. The reported annual incidence rate of LBP in Iran stands at 65%, affecting both males and females equally [3]. Studies have shown that the prevalence of LBP in Iranian men is approximately 27–28%, and varies depending on the type of population studied. Proper control and management of these forces are crucial for injury prevention and optimal performance [4]. Plantar variables, including foot pressure distribution and arch height, significantly affect individuals with LBP. Altered pressure patterns often arise as compensatory mechanisms to relieve discomfort but can lead to abnormal gait and increased strain on the lumbar spine [4]. Addressing these factors is essential for effective management of LBP [5, 6]. LBP is one of the disorders that disrupts the mechanical function of walking and alters ground reaction forces [5].
Studies have shown that the foot pressure pattern in individuals with LBP differs during standing and walking compared to healthy individuals, suggesting the presence of compensatory mechanisms to prevent pain [5]. The continuous activation of pain receptors in chronic LBP leads to changes in the cortical and subcortical regions of the brain [7]. This condition leads to disturbances in sensory and motor nerves, as well as changes in the neurochemical processes involved in the central nervous system’s response to pain [7]. Moreover, the presence of chronic LBP in affected individuals causes changes in the deep sensory receptors of the spinal column, which can send inadequate and inaccurate messages about body position [8]. Consequently, this results in impaired muscle activation and reduced neuromuscular control, ultimately leading to altered movement patterns and disruption in the absorption of ground reaction forces, causing a general imbalance in both static and dynamic stability in these patients [9]. As a result, the foot pressure pattern in individuals suffering from LBP becomes disrupted [10]. During hydrotherapy (HT) sessions, changes in weight and load on the spine can be facilitated by changing the immersion level in water, allowing for an earlier start compared to dry land exercises [10]. HT for LBP initiates treatment interventions sooner than pain-free and dry land methods [11]. People with initiates exhibit changes in their motor control, characterized by a reduced range of motion of the pelvis, increased ground reaction force, and differences in walking speed and step length; thus, LBP significantly impacts walking ability [12]. Abnormal muscle recruitment and reduced neuromuscular control lead to spinal proprioception deficits [13]. Finally, this mechanism increases the loading speed and reaction force of the earth and decreases the absorption capacity [14]. Water offers more resistance compared to air because of its higher viscosity. This increased resistance can enhance sensory feedback and awareness, leading to improved stability for individuals [10]. Thus, HT is an active therapeutic method for improving balance because the unique properties of water reduce pressure on the spine, increase spinal stability, and aid in performing physical activities without pain [15]. Incorporating motion-based therapy into open/closed kinetic chain (O/CKC) exercises can improve spinal management for optimal trunk function [16].
HT, a therapeutic approach that involves exercises performed in water, has a significant impact on the kinetics of gait [17]. The characteristics of water, including buoyancy and resistance, create a distinctive environment conducive to enhancing gait mechanics and efficiency [17]. By reducing the impact on joints and providing support, HT allows individuals to practice walking patterns with less pain and stress on the body [18]. The resistance of water also helps strengthen the muscles involved in gait, leading to better control and coordination during walking [16]. In addition, multidirectional resistance in water can challenge balance and stability, further enhancing the overall quality of gait [19]. Incorporating HT into gait training can help individuals improve their walking abilities, increase muscle strength, and enhance overall mobility [18].
HT significantly influences kinetics in rehabilitation and movement therapy [20]. The unique properties of water, such as buoyancy and resistance, create an environment that can enhance the effectiveness of kinetic exercises [20]. By using water resistance, individuals can engage in controlled and stable movements, which can lead to improved muscle activation and coordination throughout the kinetic chain [21]. Additionally, the reduced impact on joints in water allows for smoother and more fluid movements, promoting proper alignment and biomechanics [21]. Incorporating HT into kinetic training can optimize muscle recruitment, movement efficiency, and overall functional performance, making it a valuable tool for improving movement patterns and enhancing physical rehabilitation outcomes [22]. Most studies that have been conducted on the use of kinetic chain exercises have focused on their effects on knee and hip joints on land or in water [22]. However, there has been limited research on the impact of these exercises on people with chronic LBP in water. The effects of these workouts on individuals with persistent back pain in the water have not been studied. Thus, the purpose of this research was to assess the effect of O/CKC exercises in water on plantar pressure variables, pain, and disability in males suffering from non-specific chronic LBP (NSCLBP).
Materials and methods
Study design
This double-blind, randomized controlled trial with a pre-post-test design assessed males with NSCLBP. In blocks 4 and 6, the randomized codes were produced using Random Allocation software, version 1.0. Allocation concealment was ensured through the use of sealed envelopes that were sequentially numbered. An unbiased researcher, not involved in data collection, opened and sequentially distributed these envelopes to patients. The patients were randomly assigned to three groups: Control (20 patients), closed kinetic chain exercises (CKCE) (20 patients), and open kinetic chain exercises (OKCE) (20patients). Patients were kept blind to their group assignment during the study, and they were instructed to keep their group assignment concealed from the assessors. Participants received detailed instructions about the research goals and methods before the study. Consent was given voluntarily by all participants and/or their legal guardians in compliance with the Helsinki Declaration [23].
Sample size
The sample size was determined using G*Power software, version 3.1 considering a power of 0.8, a significance level of 0.5, and an effect size of 0.8 [17].
Recruitment and participants
Sixty male patients aged 40 to 60 years (mean age, 48.1±5.97), all approved by a neurosurgeon, participated in this randomized controlled trial. For eight weeks, the experimental groups underwent kinetic chain exercises three times weekly. The control group received no intervention (Figure 1).
.PNG)
The inclusion criteria were a history of discomfort lasting more than 12 weeks, an age range of 40 to 60 years, and the absence of any prior hip or spine surgery. Exclusion criteria included pain in other areas, participation in therapeutic exercises, sciatic pain, lower and upper limb deformities, the use of physiotherapy within the last year, spondylolysis, neuromuscular disorders, and respiratory problems [24].
Intervention
HT intervention
Following the evaluation of the previously mentioned parameters, an eight-week HT program was initiated. This program included three sessions per week, each lasting 60 minutes, and was conducted by a skilled aquatic sports therapist. Each session began with a 5-minute warm-up, followed by 50 minutes of motor chain exercises, and concluded with a 5-minute cool-down. At Bu-Ali Sina University in Hamadan, a specialist guided the OKCE group through noodle-assisted aquatic therapy in the deep end of the swimming pool, supervised by four lifeguards. Earlier research suggested that the exercise programs for these groups included increases in volume, intensity, duration, and repetition rates (Table 1).
.PNG)
Prior to the assessments, participants engaged in a 6-minute warm-up, consisting of 3 minutes of general warm-up activities and 3 minutes of stretching exercises. The foot pressing model, FDMeS, from Zebris Co., Germany, was used to measure gait variables, and the Win FDM-S stance software, version 01.02.09 was utilized for data analysis. The subjects were instructed to stand and then walk normally over a pressure distribution device [25]. They were asked to take one step in the middle of the device, and the data were recorded. The subjects were required to follow the path while walking in a regular pattern. The criteria examined included the total stance time (contact time), the maximum number of vertical forces of the first, depth, and second components, and the time required to reach these components (Figure 2) [26, 27].
.PNG)
After collecting data from the plantar pressure device, the components of the ground reaction force were normalized by dividing the body weight of the individuals. The results were then expressed as a multiplier of the body weight. These variables were calculated using the average data obtained from three successful walking iterations. The normalized ground reaction force components provided valuable insights into the distribution of pressure and weight during walking, allowing for a more in-depth analysis of gait patterns and potential areas of improvement [28] (Table 2).
.PNG)
Outcome measures
Plantar pressure variables
For the evaluation of plantar pressure, we utilized a Zebris plantar pressure device (intraclass correlation coefficient [ICC]=0.91). The patient stood barefoot with their eyes open on the designated area of the platform, ensuring that both feet were positioned correctly. The feet and ankles were maintained in a neutral position, with the patient’s hands positioned alongside the trunk. To reduce disturbances to the vestibular system and avoid head movements, the patient was instructed to concentrate on a 10 cm diameter marker located on the wall, 2 meters away. Each test was performed three times within a 30-second duration, allowing for a 2-minute rest interval between each trial. The plantar pressure data were evaluated using Win FDM-S software, version 01-02-09 (Figure 2), [29-31].
Pain
Pain evaluation was carried out using a 10-centimeter visual analog scale (VAS). This scale is utilized to gauge how individuals perceive pain, with participants indicating their pain intensity by marking a point within the scale’s prescribed range. In the current study, individuals with pain scores above four were included [32, 33].
Disability
The oswestry disability index (DOI), consisting of ten items with six subcategories each, was used to assess disability. The disability levels were categorized as lower (scores of 25), moderate (scores of 25-50), severe (scores of 50-75), and acute (scores of 75-100) [34].
Tampa scale for kinesiophobia (TSK)
The TSK was employed to evaluate the fear of movement during both the pre-test and post-test assessments. This questionnaire includes 11 items, with participants directed to answer each item based on their genuine feelings. Responses are rated using a four-point Likert scale, where a score of one is assigned to “I strongly disagree,” and a score of four is given to “I strongly agree” [28].
Statistical analysis
We evaluated the homogeneity of variance using the Levene test and assessed the normal distribution of the data with the Shapiro-Wilk test. Before performing a two-way repeated measures ANOVA to examine the effect of the intervention on plantar pressure variables, pain, and disability, these exploratory tests were carried out. In the one-way ANOVA, the effect size of the group×time interaction was assessed using the partial eta squared (η²p) measure. Our analysis was carried out with a significance threshold of P<0.05, and group differences were assessed using the analysis of covariance (ANCOVA) [34]. Data analysis was performed using SPSS software, version 26.
Results
Demographic details, including age, height, weight, and BMI (P>0.05) are included in Table 3. Age, weight, height, and BMI did not differ statistically significantly across the groups (P>0.05).
.PNG)
Pain and disability
There was a significant difference (P<0.05) in the participants’ levels of pain, disability, and Kinesiophobia between the CKCE and OKCE groups, according to the statistical analysis utilizing paired t-tests. The scores of the control group were not substantially different before and after the intervention (P>0.05) (Table 4).
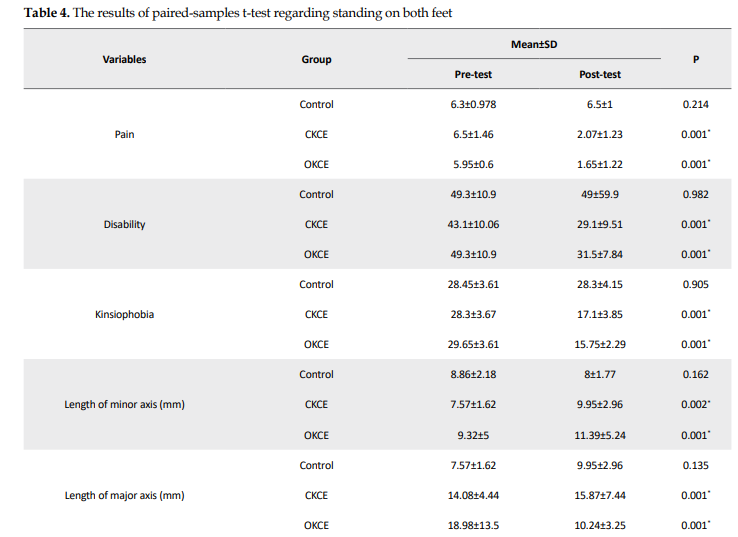
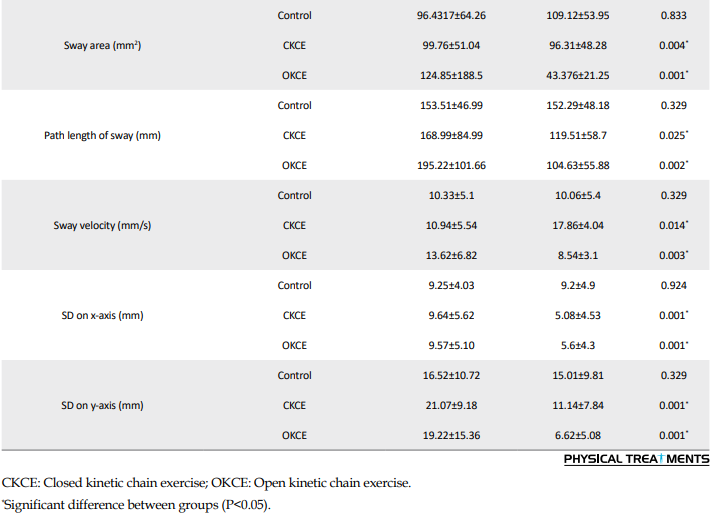
Additionally, the ANOVA results revealed significant reductions in disability (F2=9.138, P=0.001, η2=0.253), pain (F2=112.386, P=0.001, η2=0.801), and kinesiophobia (F2=110.700, P=0.001, η2=0.798) scores among the experimental groups, indicating a large effect size (Table 5).
.PNG)
Plantar pressure variables
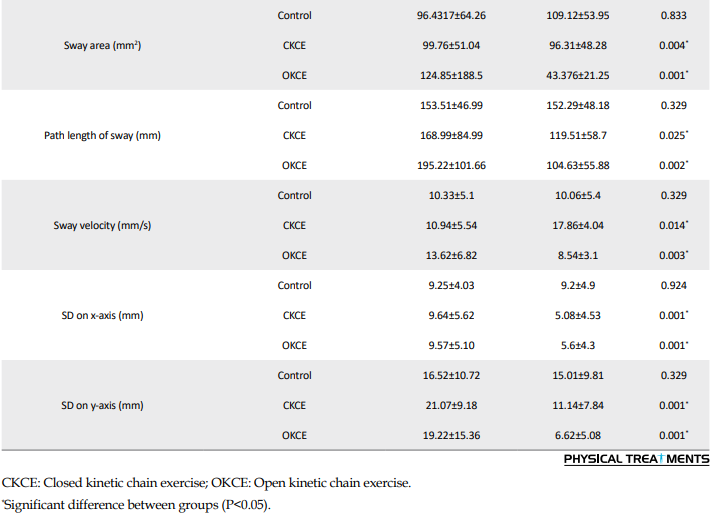
The results of ANCOVA showed that the experimental groups had a significant difference in the plantar pressure variables, including the length of the minor axis (mm) (F2=6.015, P=0.004, η2=0.207), length of the major axis (mm) (F2=12.178, P=0.001, η2=0.303), sway area (mm²) (F2=6.52, P=0.001, η2=0.340), the path length of sway (mm) (F2=6.52, P=0.048, η2=0.129), sway velocity (mm/s) (F2=9.893, P=0.001, η2=0.261), standard deviation on the x-axis (mm) (F2=9.21, P=0.001, η2=0.248), and standard deviation on the y-axis (mm) (F2=18.599, P=0.001, η2=0.399) (Table 5).
Discussion
This double-blind randomized controlled trial assessed the effect of O/CKC exercises in water on plantar pressure variables, pain, and disability in men with chronic LBP. Our findings revealed a significant improvement in plantar pressure variables within the experimental groups compared to the control group. As a result, our initial hypothesis was confirmed. Previous research has indicated that people who suffer from LBP may experience motor disorders in other parts of their body while performing motor tasks [35]. For example, LBP can reduce the intensity of muscle activity in the lower extremities during walking and standing and can also decrease the ground reaction force rate of loading [36, 37]. The observed effects highlight potential differences in movement patterns among individuals with LBP during standing, particularly concerning their lower extremities, compared to those without such pain. This may increase the risk of lower extremity injuries [38, 39]. Several studies have shown that the lack of coordination in the lumbar region, especially during sudden movements, can result in musculoskeletal injury. To better understand spinal movement patterns and the relationship between kinetic and kinematic changes in individuals with chronic LBP, postural compensatory strategies can be used [17, 39]. As a result, it is conceivable that people with LBP improve their control of movements by walking more slowly and carefully, allowing for greater safety when facing deviations [18].
Studies investigating the standing pattern of patients with NSCLBP have shown an increase in the activity of the vertebral column straightener muscle and a decrease in the reverse rotation between the pelvis, back, and thoracic spine [28]. Furthermore, in contrast to those without pain, those with LBP often increase their stride rate rather than their stride length when instructed to walk faster [40]. The findings of this study support previous research by Delitto et al. [37], Alaca et al. [38], Pires et al. [39], Yalfani et al. [17], and Khojastehpour et al. [40], which suggests that a stable spine can lead to better body mechanics while standing, particularly for individuals who experience back pain. When the hip, knee, and ankle joints deviate from their normal positions, it can cause an uneven distribution of force and impair everyday functioning in the body [37-40, 17]. Weakness or improper muscle function can cause instability, leading to excessive pressure on the joint and further irritation [35]. On the other hand, in patients with NSCLBP, plantar pressure distribution is higher in the forefoot than in the hindfoot [39]. In general, patients with NSCLBP often use ankle strategies for postural control. Consequently, the ankle strategy increased the center of pressure deflection forward, thereby increasing the load on the forefoot [18].
In the domains of pain and disability index, the experimental group showed a notable improvement compared to the control group. According to Monticone et al. [41], Tavakoli et al. [42], and Yalfani et al. [17], significant improvements were observed in pain levels and disability index in patients with chronic LBP who underwent exercise. The aforementioned studies showed that exercise improves disability, and reduces pain in patients with chronic LBP, which is consistent with our findings [41, 42, 17]. Research has indicated that NSCLBP is linked to dysfunction and weakness in the abdominal muscles, along with alterations in walking variables [40]. For example, Carayannopoulos et al. stated that therapeutic exercises in water led to a significant reduction in pain and disability and a significant improvement in walking parameters in the experimental group. HT is a helpful form of treatment for patients with chronic LBP and can help alleviate muscle tension, reduce pain, and relieve stiffness in the back [14]. Additionally, the buoyancy of the water can help reduce pressure on the joints and spine, allowing patients to perform exercises that may be difficult or painful on land [24]. Many patients find relief and improved mobility through regular HT sessions [43]. In this regard, Baena et al. concluded that the aquatic environment itself helps relieve pain, increase blood flow, and block pain receptors, in addition to removing stimulants and creating the possibility for the stimulation and secretion of endorphins, all of which are mechanisms of pain reduction in people with back pain [29]. It is clear that the severity of pain determines disability in these patients; therefore, it can be concluded that along with the reduction of pain, disability is also reduced [15]. In addition, Khojastehpour et al. and Cuesta-Vargas et al. showed that practicing in a water environment led to a significant reduction in pain in people with CLBP, which reduced the severity of their disability [40, 43].
Maintaining pelvic and lumbar stability is essential for balancing forces in the vertebrae, pelvis, and motor chains, ultimately enabling proper limb movement [40]. Weakness or improper muscle function can cause instability, leading to excessive pressure on the joints and further irritation [40]. Proper control and absorption of these forces during physical activities are particularly crucial for injury prevention [44]. The formula for the rate of load indicates that an increase in Earth’s reaction force peak also results in a corresponding increase in the rate of load [29]. The groups that participated in both O/CKC exercises in water showed an improvement in neuromuscular control in the lumbar and pelvic areas. This improvement helps distribute forces to the lower limbs, thus reducing the pressure on the lumbar and lower limbs, and ultimately reducing the ground reaction force and load levels in these individuals. Consequently, as HT exercises serve to improve limb movement control and lessen the strain on the lower limbs and vertical reaction force, they can be a useful therapeutic choice for people with chronic LBP. These exercises can aid in the recovery process for individuals with chronic LBP by potentially decreasing the reaction force and load during walking. However, the study had some limitations that future researchers should consider. The initial statistical sample solely comprised male individuals experiencing nonspecific chronic LBP. Second, the study solely focused on the effects of kinetic chain exercise programs on vertical component of ground reaction force (VGRF) and rate of loading in NSCLBP, neglecting other variables related to walking in this condition. Finally, there was a lack of long-term follow-up in the study.
Conclusion
The results highlight the significant effects of HT for men with chronic LBP. The plantar pressure variables can be efficiently changed by both O/CKC exercises in water. Moreover, HT can manage pain and disability in this specific group of individuals. Given these outcomes, it is recommended that healthcare professionals, including physicians, physiotherapists, and occupational therapists, incorporate both closed and open kinetic chain exercises into HT for chronic LBP patients.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Bu-Ali Sina University, Hamadan, Iran (Code: IR.BASU.REC.1402.011), which complies with the 2008 Helsinki Declaration’s tenets. The informed consent of the patients was obtained prior to any data collection. Moreover, this study was registered by the Iranian Registry of Clinical Trials (IRCT), Tehran, Iran (Code: IRCT20190129042534N1).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Each author contributed equally to the preparation of this paper.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank all of the patients who took part in this clinical trial.
References
The prevalence of low back pain (LBP) has been highlighted by the World Health Organization (WHO) as a significant health concern, affecting individuals regularly and leading to a decline in their overall well-being and quality of life (QoL). Moreover, it can hinder their functional abilities, contributing to absenteeism in the workplace, early retirement, and in more severe instances, disabilities [1]. The prevalence of LBP in Iran ranges from 14.4% to 84.1% in various subsets of the population, such as working populations, pregnant women, and students, following world trends [2]. Regardless of the etiology, LBP ranks as the third most frequent contributor to morbidity and disability within the Iranian population aged 15–69 [2]. The reported annual incidence rate of LBP in Iran stands at 65%, affecting both males and females equally [3]. Studies have shown that the prevalence of LBP in Iranian men is approximately 27–28%, and varies depending on the type of population studied. Proper control and management of these forces are crucial for injury prevention and optimal performance [4]. Plantar variables, including foot pressure distribution and arch height, significantly affect individuals with LBP. Altered pressure patterns often arise as compensatory mechanisms to relieve discomfort but can lead to abnormal gait and increased strain on the lumbar spine [4]. Addressing these factors is essential for effective management of LBP [5, 6]. LBP is one of the disorders that disrupts the mechanical function of walking and alters ground reaction forces [5].
Studies have shown that the foot pressure pattern in individuals with LBP differs during standing and walking compared to healthy individuals, suggesting the presence of compensatory mechanisms to prevent pain [5]. The continuous activation of pain receptors in chronic LBP leads to changes in the cortical and subcortical regions of the brain [7]. This condition leads to disturbances in sensory and motor nerves, as well as changes in the neurochemical processes involved in the central nervous system’s response to pain [7]. Moreover, the presence of chronic LBP in affected individuals causes changes in the deep sensory receptors of the spinal column, which can send inadequate and inaccurate messages about body position [8]. Consequently, this results in impaired muscle activation and reduced neuromuscular control, ultimately leading to altered movement patterns and disruption in the absorption of ground reaction forces, causing a general imbalance in both static and dynamic stability in these patients [9]. As a result, the foot pressure pattern in individuals suffering from LBP becomes disrupted [10]. During hydrotherapy (HT) sessions, changes in weight and load on the spine can be facilitated by changing the immersion level in water, allowing for an earlier start compared to dry land exercises [10]. HT for LBP initiates treatment interventions sooner than pain-free and dry land methods [11]. People with initiates exhibit changes in their motor control, characterized by a reduced range of motion of the pelvis, increased ground reaction force, and differences in walking speed and step length; thus, LBP significantly impacts walking ability [12]. Abnormal muscle recruitment and reduced neuromuscular control lead to spinal proprioception deficits [13]. Finally, this mechanism increases the loading speed and reaction force of the earth and decreases the absorption capacity [14]. Water offers more resistance compared to air because of its higher viscosity. This increased resistance can enhance sensory feedback and awareness, leading to improved stability for individuals [10]. Thus, HT is an active therapeutic method for improving balance because the unique properties of water reduce pressure on the spine, increase spinal stability, and aid in performing physical activities without pain [15]. Incorporating motion-based therapy into open/closed kinetic chain (O/CKC) exercises can improve spinal management for optimal trunk function [16].
HT, a therapeutic approach that involves exercises performed in water, has a significant impact on the kinetics of gait [17]. The characteristics of water, including buoyancy and resistance, create a distinctive environment conducive to enhancing gait mechanics and efficiency [17]. By reducing the impact on joints and providing support, HT allows individuals to practice walking patterns with less pain and stress on the body [18]. The resistance of water also helps strengthen the muscles involved in gait, leading to better control and coordination during walking [16]. In addition, multidirectional resistance in water can challenge balance and stability, further enhancing the overall quality of gait [19]. Incorporating HT into gait training can help individuals improve their walking abilities, increase muscle strength, and enhance overall mobility [18].
HT significantly influences kinetics in rehabilitation and movement therapy [20]. The unique properties of water, such as buoyancy and resistance, create an environment that can enhance the effectiveness of kinetic exercises [20]. By using water resistance, individuals can engage in controlled and stable movements, which can lead to improved muscle activation and coordination throughout the kinetic chain [21]. Additionally, the reduced impact on joints in water allows for smoother and more fluid movements, promoting proper alignment and biomechanics [21]. Incorporating HT into kinetic training can optimize muscle recruitment, movement efficiency, and overall functional performance, making it a valuable tool for improving movement patterns and enhancing physical rehabilitation outcomes [22]. Most studies that have been conducted on the use of kinetic chain exercises have focused on their effects on knee and hip joints on land or in water [22]. However, there has been limited research on the impact of these exercises on people with chronic LBP in water. The effects of these workouts on individuals with persistent back pain in the water have not been studied. Thus, the purpose of this research was to assess the effect of O/CKC exercises in water on plantar pressure variables, pain, and disability in males suffering from non-specific chronic LBP (NSCLBP).
Materials and methods
Study design
This double-blind, randomized controlled trial with a pre-post-test design assessed males with NSCLBP. In blocks 4 and 6, the randomized codes were produced using Random Allocation software, version 1.0. Allocation concealment was ensured through the use of sealed envelopes that were sequentially numbered. An unbiased researcher, not involved in data collection, opened and sequentially distributed these envelopes to patients. The patients were randomly assigned to three groups: Control (20 patients), closed kinetic chain exercises (CKCE) (20 patients), and open kinetic chain exercises (OKCE) (20patients). Patients were kept blind to their group assignment during the study, and they were instructed to keep their group assignment concealed from the assessors. Participants received detailed instructions about the research goals and methods before the study. Consent was given voluntarily by all participants and/or their legal guardians in compliance with the Helsinki Declaration [23].
Sample size
The sample size was determined using G*Power software, version 3.1 considering a power of 0.8, a significance level of 0.5, and an effect size of 0.8 [17].
Recruitment and participants
Sixty male patients aged 40 to 60 years (mean age, 48.1±5.97), all approved by a neurosurgeon, participated in this randomized controlled trial. For eight weeks, the experimental groups underwent kinetic chain exercises three times weekly. The control group received no intervention (Figure 1).
.PNG)
The inclusion criteria were a history of discomfort lasting more than 12 weeks, an age range of 40 to 60 years, and the absence of any prior hip or spine surgery. Exclusion criteria included pain in other areas, participation in therapeutic exercises, sciatic pain, lower and upper limb deformities, the use of physiotherapy within the last year, spondylolysis, neuromuscular disorders, and respiratory problems [24].
Intervention
HT intervention
Following the evaluation of the previously mentioned parameters, an eight-week HT program was initiated. This program included three sessions per week, each lasting 60 minutes, and was conducted by a skilled aquatic sports therapist. Each session began with a 5-minute warm-up, followed by 50 minutes of motor chain exercises, and concluded with a 5-minute cool-down. At Bu-Ali Sina University in Hamadan, a specialist guided the OKCE group through noodle-assisted aquatic therapy in the deep end of the swimming pool, supervised by four lifeguards. Earlier research suggested that the exercise programs for these groups included increases in volume, intensity, duration, and repetition rates (Table 1).
.PNG)
Prior to the assessments, participants engaged in a 6-minute warm-up, consisting of 3 minutes of general warm-up activities and 3 minutes of stretching exercises. The foot pressing model, FDMeS, from Zebris Co., Germany, was used to measure gait variables, and the Win FDM-S stance software, version 01.02.09 was utilized for data analysis. The subjects were instructed to stand and then walk normally over a pressure distribution device [25]. They were asked to take one step in the middle of the device, and the data were recorded. The subjects were required to follow the path while walking in a regular pattern. The criteria examined included the total stance time (contact time), the maximum number of vertical forces of the first, depth, and second components, and the time required to reach these components (Figure 2) [26, 27].
.PNG)
After collecting data from the plantar pressure device, the components of the ground reaction force were normalized by dividing the body weight of the individuals. The results were then expressed as a multiplier of the body weight. These variables were calculated using the average data obtained from three successful walking iterations. The normalized ground reaction force components provided valuable insights into the distribution of pressure and weight during walking, allowing for a more in-depth analysis of gait patterns and potential areas of improvement [28] (Table 2).
.PNG)
Outcome measures
Plantar pressure variables
For the evaluation of plantar pressure, we utilized a Zebris plantar pressure device (intraclass correlation coefficient [ICC]=0.91). The patient stood barefoot with their eyes open on the designated area of the platform, ensuring that both feet were positioned correctly. The feet and ankles were maintained in a neutral position, with the patient’s hands positioned alongside the trunk. To reduce disturbances to the vestibular system and avoid head movements, the patient was instructed to concentrate on a 10 cm diameter marker located on the wall, 2 meters away. Each test was performed three times within a 30-second duration, allowing for a 2-minute rest interval between each trial. The plantar pressure data were evaluated using Win FDM-S software, version 01-02-09 (Figure 2), [29-31].
Pain
Pain evaluation was carried out using a 10-centimeter visual analog scale (VAS). This scale is utilized to gauge how individuals perceive pain, with participants indicating their pain intensity by marking a point within the scale’s prescribed range. In the current study, individuals with pain scores above four were included [32, 33].
Disability
The oswestry disability index (DOI), consisting of ten items with six subcategories each, was used to assess disability. The disability levels were categorized as lower (scores of 25), moderate (scores of 25-50), severe (scores of 50-75), and acute (scores of 75-100) [34].
Tampa scale for kinesiophobia (TSK)
The TSK was employed to evaluate the fear of movement during both the pre-test and post-test assessments. This questionnaire includes 11 items, with participants directed to answer each item based on their genuine feelings. Responses are rated using a four-point Likert scale, where a score of one is assigned to “I strongly disagree,” and a score of four is given to “I strongly agree” [28].
Statistical analysis
We evaluated the homogeneity of variance using the Levene test and assessed the normal distribution of the data with the Shapiro-Wilk test. Before performing a two-way repeated measures ANOVA to examine the effect of the intervention on plantar pressure variables, pain, and disability, these exploratory tests were carried out. In the one-way ANOVA, the effect size of the group×time interaction was assessed using the partial eta squared (η²p) measure. Our analysis was carried out with a significance threshold of P<0.05, and group differences were assessed using the analysis of covariance (ANCOVA) [34]. Data analysis was performed using SPSS software, version 26.
Results
Demographic details, including age, height, weight, and BMI (P>0.05) are included in Table 3. Age, weight, height, and BMI did not differ statistically significantly across the groups (P>0.05).
.PNG)
Pain and disability
There was a significant difference (P<0.05) in the participants’ levels of pain, disability, and Kinesiophobia between the CKCE and OKCE groups, according to the statistical analysis utilizing paired t-tests. The scores of the control group were not substantially different before and after the intervention (P>0.05) (Table 4).
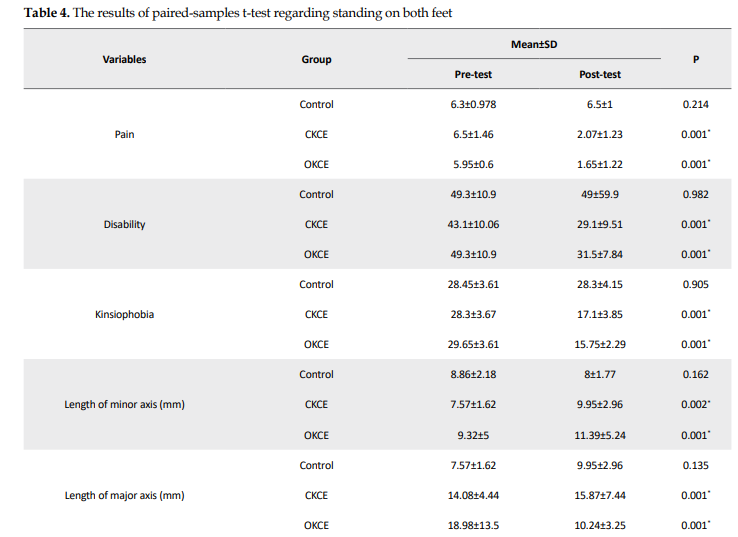
Additionally, the ANOVA results revealed significant reductions in disability (F2=9.138, P=0.001, η2=0.253), pain (F2=112.386, P=0.001, η2=0.801), and kinesiophobia (F2=110.700, P=0.001, η2=0.798) scores among the experimental groups, indicating a large effect size (Table 5).
.PNG)
Plantar pressure variables
The results of ANCOVA showed that the experimental groups had a significant difference in the plantar pressure variables, including the length of the minor axis (mm) (F2=6.015, P=0.004, η2=0.207), length of the major axis (mm) (F2=12.178, P=0.001, η2=0.303), sway area (mm²) (F2=6.52, P=0.001, η2=0.340), the path length of sway (mm) (F2=6.52, P=0.048, η2=0.129), sway velocity (mm/s) (F2=9.893, P=0.001, η2=0.261), standard deviation on the x-axis (mm) (F2=9.21, P=0.001, η2=0.248), and standard deviation on the y-axis (mm) (F2=18.599, P=0.001, η2=0.399) (Table 5).
Discussion
This double-blind randomized controlled trial assessed the effect of O/CKC exercises in water on plantar pressure variables, pain, and disability in men with chronic LBP. Our findings revealed a significant improvement in plantar pressure variables within the experimental groups compared to the control group. As a result, our initial hypothesis was confirmed. Previous research has indicated that people who suffer from LBP may experience motor disorders in other parts of their body while performing motor tasks [35]. For example, LBP can reduce the intensity of muscle activity in the lower extremities during walking and standing and can also decrease the ground reaction force rate of loading [36, 37]. The observed effects highlight potential differences in movement patterns among individuals with LBP during standing, particularly concerning their lower extremities, compared to those without such pain. This may increase the risk of lower extremity injuries [38, 39]. Several studies have shown that the lack of coordination in the lumbar region, especially during sudden movements, can result in musculoskeletal injury. To better understand spinal movement patterns and the relationship between kinetic and kinematic changes in individuals with chronic LBP, postural compensatory strategies can be used [17, 39]. As a result, it is conceivable that people with LBP improve their control of movements by walking more slowly and carefully, allowing for greater safety when facing deviations [18].
Studies investigating the standing pattern of patients with NSCLBP have shown an increase in the activity of the vertebral column straightener muscle and a decrease in the reverse rotation between the pelvis, back, and thoracic spine [28]. Furthermore, in contrast to those without pain, those with LBP often increase their stride rate rather than their stride length when instructed to walk faster [40]. The findings of this study support previous research by Delitto et al. [37], Alaca et al. [38], Pires et al. [39], Yalfani et al. [17], and Khojastehpour et al. [40], which suggests that a stable spine can lead to better body mechanics while standing, particularly for individuals who experience back pain. When the hip, knee, and ankle joints deviate from their normal positions, it can cause an uneven distribution of force and impair everyday functioning in the body [37-40, 17]. Weakness or improper muscle function can cause instability, leading to excessive pressure on the joint and further irritation [35]. On the other hand, in patients with NSCLBP, plantar pressure distribution is higher in the forefoot than in the hindfoot [39]. In general, patients with NSCLBP often use ankle strategies for postural control. Consequently, the ankle strategy increased the center of pressure deflection forward, thereby increasing the load on the forefoot [18].
In the domains of pain and disability index, the experimental group showed a notable improvement compared to the control group. According to Monticone et al. [41], Tavakoli et al. [42], and Yalfani et al. [17], significant improvements were observed in pain levels and disability index in patients with chronic LBP who underwent exercise. The aforementioned studies showed that exercise improves disability, and reduces pain in patients with chronic LBP, which is consistent with our findings [41, 42, 17]. Research has indicated that NSCLBP is linked to dysfunction and weakness in the abdominal muscles, along with alterations in walking variables [40]. For example, Carayannopoulos et al. stated that therapeutic exercises in water led to a significant reduction in pain and disability and a significant improvement in walking parameters in the experimental group. HT is a helpful form of treatment for patients with chronic LBP and can help alleviate muscle tension, reduce pain, and relieve stiffness in the back [14]. Additionally, the buoyancy of the water can help reduce pressure on the joints and spine, allowing patients to perform exercises that may be difficult or painful on land [24]. Many patients find relief and improved mobility through regular HT sessions [43]. In this regard, Baena et al. concluded that the aquatic environment itself helps relieve pain, increase blood flow, and block pain receptors, in addition to removing stimulants and creating the possibility for the stimulation and secretion of endorphins, all of which are mechanisms of pain reduction in people with back pain [29]. It is clear that the severity of pain determines disability in these patients; therefore, it can be concluded that along with the reduction of pain, disability is also reduced [15]. In addition, Khojastehpour et al. and Cuesta-Vargas et al. showed that practicing in a water environment led to a significant reduction in pain in people with CLBP, which reduced the severity of their disability [40, 43].
Maintaining pelvic and lumbar stability is essential for balancing forces in the vertebrae, pelvis, and motor chains, ultimately enabling proper limb movement [40]. Weakness or improper muscle function can cause instability, leading to excessive pressure on the joints and further irritation [40]. Proper control and absorption of these forces during physical activities are particularly crucial for injury prevention [44]. The formula for the rate of load indicates that an increase in Earth’s reaction force peak also results in a corresponding increase in the rate of load [29]. The groups that participated in both O/CKC exercises in water showed an improvement in neuromuscular control in the lumbar and pelvic areas. This improvement helps distribute forces to the lower limbs, thus reducing the pressure on the lumbar and lower limbs, and ultimately reducing the ground reaction force and load levels in these individuals. Consequently, as HT exercises serve to improve limb movement control and lessen the strain on the lower limbs and vertical reaction force, they can be a useful therapeutic choice for people with chronic LBP. These exercises can aid in the recovery process for individuals with chronic LBP by potentially decreasing the reaction force and load during walking. However, the study had some limitations that future researchers should consider. The initial statistical sample solely comprised male individuals experiencing nonspecific chronic LBP. Second, the study solely focused on the effects of kinetic chain exercise programs on vertical component of ground reaction force (VGRF) and rate of loading in NSCLBP, neglecting other variables related to walking in this condition. Finally, there was a lack of long-term follow-up in the study.
Conclusion
The results highlight the significant effects of HT for men with chronic LBP. The plantar pressure variables can be efficiently changed by both O/CKC exercises in water. Moreover, HT can manage pain and disability in this specific group of individuals. Given these outcomes, it is recommended that healthcare professionals, including physicians, physiotherapists, and occupational therapists, incorporate both closed and open kinetic chain exercises into HT for chronic LBP patients.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Bu-Ali Sina University, Hamadan, Iran (Code: IR.BASU.REC.1402.011), which complies with the 2008 Helsinki Declaration’s tenets. The informed consent of the patients was obtained prior to any data collection. Moreover, this study was registered by the Iranian Registry of Clinical Trials (IRCT), Tehran, Iran (Code: IRCT20190129042534N1).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Each author contributed equally to the preparation of this paper.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank all of the patients who took part in this clinical trial.
References
- Phattharasupharerk S, Purepong N, Eksakulkla S, Siriphorn A. Effects of qigong practice in office workers with chronic non-specific low back pain: A randomized control trial. Journal of Bodywork and Movement Therapies. 2019; 23(2):375-81. [DOI:10.1016/j.jbmt.2018.02.004] [PMID]
- Mousavi SJ, Akbari ME, Mehdian H, Mobini B, Montazeri A, Akbarnia B, et al. Low back pain in Iran: A growing need to adapt and implement evidence-based practice in developing countries. Spine. 2011; 36(10):E638-46. [DOI:10.1097/BRS.0b013e3181fa1da2] [PMID]
- Yalfani A, Ahmadnezhad L, Gholami Borujeni B, Khoshnamvand Z. The effect of six weeks core stability exercise training on balance, pain and function in women with chronic low back pain. Journal of Health and Care. 2017; 18(4):336-46. [Link]
- Alexander IJ, Chao EY, Johnson KA. The assessment of dynamic foot-to-ground contact forces and plantar pressure distribution: a review of the evolution of current techniques and clinical applications. Foot & Ankle. 1990; 11(3):152-67. [DOI:10.1177/107110079001100306] [PMID]
- Ghafouri M, Teymourzadeh A, Nakhostin-Ansari A, Sepanlou SG, Dalvand S, et al. Prevalence and predictors of low back pain among the Iranian population: Results from the Persian cohort study. Annals of Medicine and Surgery. 2022; 74:103243. [DOI:10.1016/j.amsu.2022.103243] [PMID]
- Dufek JS, Bates BT. Biomechanical factors associated with injury during landing in jump sports. Sports Medicine. 1991; 12:326-37. [DOI:10.2165/00007256-199112050-00005]
- Fatollahi A, Barghamadi M, Darvishani MA. Effect of hydrotherapy on muscle activities and running kinetics in adult males with pronated foot: A randomized clinical trial. Pamukkale Journal of Sport Sciences. 2023; 14(3):297-313. [DOI:10.54141/psbd.1350754]
- Christakou A, Boulnta F. The effectiveness of hydrotherapy in patients with chronic low back pain. Physiotherapy Quarterly. 2020; 28(3):32-8. [DOI:10.5114/pq.2020.95772]
- Bento P CB, Pereira G, Ugrinowitsch C, Rodacki A LF. The effects of a water-based exercise program on strength and functionality of older adults. Journal of Aging and Physical Activity. 2012; 20(4):469-83. [DOI:10.1123/japa.20.4.469] [PMID]
- Hewett TE, Myer GD, Ford KR, Heidt RS Jr, Colosimo AJ, McLean SG, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study. The American Journal of Sports Medicine. 2005; 33(4):492-501. [DOI:10.1177/0363546504269591] [PMID]
- Lee H, Hübscher M, Moseley GL, Kamper SJ, Traeger AC, Mansell G, et al. How does pain lead to disability? A systematic review and meta-analysis of mediation studies in people with back and neck pain. Pain. 2015; 156(6):988-97. [DOI:10.1097/j.pain.0000000000000146] [PMID]
- Rum L, Brasiliano P, Vannozzi G, Laudani L, Macaluso A. Non-specific chronic low back pain elicits kinematic and neuromuscular changes in walking and gait termination. Gait & Posture. 2021; 84:238-44. [DOI:10.1016/j.gaitpost.2020.12.005] [PMID]
- Russo M, Deckers K, Eldabe S, Kiesel K, Gilligan C, Vieceli J, et al. Muscle control and non-specific chronic low back pain. Neuromodulation. 2018; 21(1):1-9. [DOI:10.1111/ner.12738] [PMID]
- Carayannopoulos AG, Han A, Burdenko IN. The benefits of combining water and land-based therapy. Journal of Exercise Rehabilitation. 2020; 16(1):20-6. [DOI:10.12965/jer.1938742.371] [PMID]
- Kwon YJ, Park SJ, Jefferson J, Kim K. The effect of open and closed kinetic chain exercises on dynamic balance ability of normal healthy adults. Journal of Physical Therapy Science. 2013; 25(6):671-4. [DOI:10.1589/jpts.25.671] [PMID]
- Ariyoshi M, Sonoda K, Nagata K, Mashima T, Zenmyo M, Paku C, et al. Efficacy of aquatic exercises for patients with low-back pain. The Kurume Medical Journal. 1999; 46(2):91-6. [DOI:10.2739/kurumemedj.46.91] [PMID]
- Yalfani A, Raeisi Z, Koumasian Z. Effects of eight-week water versus mat pilates on female patients with chronic nonspecific low back pain: Double-blind randomized clinical trial. Journal of Bodywork and Movement Therapies. 2020; 24(4):70-5. [DOI:10.1016/j.jbmt.2020.06.002] [PMID]
- Brody LT, Geigle PR. Aquatic exercise for rehabilitation and training. Champaign: Human Kinetics; 2009. [DOI:10.5040/9781718210691]
- Heywood S, McClelland J, Geigle P, Rahmann A, Villalta E, Mentiplay B, et al. Force during functional exercises on land and in water in older adults with and without knee osteoarthritis: Implications for rehabilitation. Knee. 2019; 26(1):61-72. [DOI:10.1016/j.knee.2018.11.003] [PMID]
- Tagesson S, Oberg B, Good L, Kvist J. A comprehensive rehabilitation program with quadriceps strengthening in closed versus open kinetic chain exercise in patients with anterior cruciate ligament deficiency: A randomized clinical trial evaluating dynamic tibial translation and muscle function. The American Journal of Sports Medicine. 2008; 36(2):298-307. [DOI:10.1177/0363546507307867] [PMID]
- Gomes Neto M, Pontes SS, Almeida LO, da Silva CM, da Conceição Sena C, Saquetto MB. Effects of water-based exercise on functioning and quality of life in people with Parkinson's disease: A systematic review and meta-analysis. Clinical Rehabilitation. 2020; 34(12):1425-35. [DOI:10.1177/0269215520943660] [PMID]
- Boutron I, Moher D, Altman DG, Schulz KF, Ravaud P, CONSORT Group*. Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: Explanation and elaboration. Annals of internal medicine. 2008; 148(4):295-309. [DOI:10.7326/0003-4819-148-4-200802190-00008]
- Kim Y, Vakula MN, Waller B, Bressel E. A systematic review and meta-analysis comparing the effect of aquatic and land exercise on dynamic balance in older adults. BMC Geriatrics. 2020; 20(1):302. [DOI:10.1186/s12877-020-01702-9] [PMID]
- Boonstra AM, Schiphorst Preuper HR, Reneman MF, Posthumus JB, Stewart RE. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. International Journal of Rehabilitation Research. 2008; 31(2):165-9. [DOI:10.1097/MRR.0b013e3282fc0f93] [PMID]
- Bisson EJ, Katz L, Vader K, Bossio JA, Wilson R, Duggan S. Pain-related fear in adults living with chronic pain: development and psychometric validation of a brief form of the tampa scale of kinesiophobia. Archives of Physical Medicine and Rehabilitation. 2022; 103(5):875-81.e1. [DOI:10.1016/j.apmr.2021.09.001] [PMID]
- Braun BJ, Veith NT, Hell R, Döbele S, Roland M, Rollmann M, et al. Validation and reliability testing of a new, fully integrated gait analysis insole. Journal of Foot and Ankle Research. 2015; 8:54. [DOI:10.1186/s13047-015-0111-8] [PMID]
- Gholami Borujeni B, Yalfani A. Reduction of postural sway in athletes with chronic low back pain through eight weeks of inspiratory muscle training: A randomized controlled trial. Clinical Biomechanics. 2019; 69:215-20. [DOI:10.1016/j.clinbiomech.2019.09.006] [PMID]
- Baena-Beato PÁ, Artero EG, Arroyo-Morales M, Robles-Fuentes A, Gatto-Cardia MC, Delgado-Fernández M. Aquatic therapy improves pain, disability, quality of life, body composition and fitness in sedentary adults with chronic low back pain. A controlled clinical trial. Clinical Rehabilitation. 2014; 28(4):350-60. [DOI:10.1177/0269215513504943] [PMID]
- Rostami A, Letafatkar A, Khaleghi Tazji M. The effects of feedback exercises on peak vertical ground reaction force and rate of loading associated with lower extremity injury in landing after volleyball blocks. Sport Sciences and Health Research. 2019; 10(2):197-211. [DOI:0.22059/jsmed.2019.258996.901]
- Wearing SC, Urry SR, Smeathers JE. Ground reaction forces at discrete sites of the foot derived from pressure plate measurements. Foot & Ankle International. 2001; 22(8):653-61. [DOI:10.1177/107110070102200807] [PMID]
- Zulkifli SS, Loh WP. A state-of-the-art review of foot pressure. Foot and Ankle Surgery. 2020; 26(1):25-32. [DOI:10.1016/j.fas.2018.12.005] [PMID]
- Kovács I, Tihanyi J, Devita P, Rácz L, Barrier J, Hortobágyi T. Foot placement modifies kinematics and kinetics during drop jumping. Medicine and Science in Sports and Exercise. 1999; 31(5):708-16. [DOI:10.1097/00005768-199905000-00014] [PMID]
- Irandoust K, Taheri M. The effect of aquatic training on kinematic walking patterns of elderly women. International Archives of Health Sciences. 2019; 6(1):1-5. [DOI:10.4103/iahs.iahs_1_19]
- Richardson JT. Eta squared and partial eta squared as measures of effect size in educational research. Educational Research Review. 2011; 6(2):135-47. [DOI:10.1016/j.edurev.2010.12.001]
- Lamoth CJ, Meijer OG, Daffertshofer A, Wuisman PI, Beek PJ. Effects of chronic low back pain on trunk coordination and back muscle activity during walking: Changes in motor control. European Spine Journal. 2006; 15(1):23-40. [DOI:10.1007/s00586-004-0825-y] [PMID]
- Heywood S, McClelland J, Mentiplay B, Geigle P, Rahmann A, Clark R. Effectiveness of aquatic exercise in improving lower limb strength in musculoskeletal conditions: A systematic review and meta-analysis. Archives of Physical Medicine and Rehabilitation. 2017; 98(1):173-86. [DOI:10.1016/j.apmr.2016.08.472] [PMID]
- Delitto A, George SZ, Van Dillen L, Whitman JM, Sowa G, Shekelle P, et al. Low back pain. J Orthop Sports Phys Ther. 2012; 42(4):A1-57. [DOI:10.2519/jospt.2012.42.4.A1] [PMID]
- Alaca N, Kaba H, Atalay A. Associations between the severity of disability level and fear of movement and pain beliefs in patients with chronic low back pain. Journal of Back and Musculoskeletal Rehabilitation. 2020; 33(5):785-91. [DOI:10.3233/BMR-171039] [PMID]
- Pires D, Cruz EB, Caeiro C. Aquatic exercise and pain neurophysiology education versus aquatic exercise alone for patients with chronic low back pain: A randomized controlled trial. Clinical Rehabilitation. 2015; 29(6):538-47. [DOI:10.1177/0269215514549033] [PMID]
- Khojastehpour B, Atri AE, Javaheri SA. Comparison the effect of core stabilization training in water and on land on pain and dynamic postural stability in women with chronic non-specific low back pain. Journal of Anesthesiology and Pain. 2019; 10(2):75-90. [Link]
- Monticone M, Ferrante S, Rocca B, Baiardi P, Dal Farra F, Foti C. Effect of a long-lasting multidisciplinary program on disability and fear-avoidance behaviors in patients with chronic low back pain: Results of a randomized controlled trial. The Clinical Journal of Pain. 2013; 29(11):929-38. [DOI:10.1097/AJP.0b013e31827fef7e] [PMID]
- Tavakoli MN, Mirghaemi TS. The effectiveness of cognitive-behavioral group therapy anger and assertiveness of adolescents. International Journal of Education and Applied Sciences. 2023; 3(4):20-8. [DOI:10.22034/injoeas.2023.365081.1038]
- Cuesta-Vargas AI, Adams N, Salazar JA, Belles A, Hazañas S, Arroyo-Morales M. Deep water running and general practice in primary care for non-specific low back pain versus general practice alone: Randomized controlled trial. Clinical Rheumatology. 2012; 31(7):1073-8. [DOI:10.1007/s10067-012-1977-5] [PMID]
- Haddas R, James CR, Hooper TL. Lower extremity fatigue, sex, and landing performance in a population with recurrent low back pain. Journal of Athletic Training. 2015; 50(4):378-84. [DOI:10.4085/1062-6050-49.3.61] [PMID]
Type of Study: Research |
Subject:
General
Received: 2024/01/31 | Accepted: 2024/07/21 | Published: 2024/10/1
Received: 2024/01/31 | Accepted: 2024/07/21 | Published: 2024/10/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |