Wed, Jul 9, 2025
Volume 14, Issue 2 (Spring 2024)
PTJ 2024, 14(2): 147-158 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ebrahimipour E, Anbarian M, Sabet F, Tafti N. Quantifying Spatial-temporal Parameters During Stair Ascent and Descent Among Knee Osteoarthritis Populations. PTJ 2024; 14 (2) :147-158
URL: http://ptj.uswr.ac.ir/article-1-610-en.html
URL: http://ptj.uswr.ac.ir/article-1-610-en.html
1- Department of Sports Biomechanics, Faculty of Sports Sciences, Bu-Ali Sina University, Hamedan, Iran.
2- Department of Orthotics and Prosthetics, Faculty of Rehabilitation Sciences, Hamedan University of Medical Sciences, Hamadan, Iran.
2- Department of Orthotics and Prosthetics, Faculty of Rehabilitation Sciences, Hamedan University of Medical Sciences, Hamadan, Iran.
Full-Text [PDF 1237 kb]
(736 Downloads)
| Abstract (HTML) (2943 Views)
Full-Text: (465 Views)
Introduction
Knee osteoarthritis (KOA) is a prevalent orthopedic illness that has a significant impact on the overall well-being of patients. Its primary manifestation involves the degeneration of the articular cartilage, and it is more commonly found among middle-aged and elderly individuals [1]. KOA results in a range of difficulties, including discomfort, limited joint mobility, significant medical costs, and a heightened likelihood of disability [2]. These issues are often linked to various factors, such as age, obesity, inflammation, previous injuries, and genetic predisposition [2]. According to previous studies, at least 10% of individuals aged 55 years and above suffer from KOA, among whom, approximately one-fourth experience disability [3].
The primary symptoms associated with KOA are pain, decreased functionality, and occasional stiffness in the joints [4], which restricts individuals’ ability to perform tasks, such as standing up from a chair, walking comfortably, or climbing stairs [5]. Moreover, individuals with KOA exhibit different movement patterns and muscle activation strategies compared to healthy individuals when walking or climbing stairs [5, 6]. The alterations can impact the knee’s capacity to distribute loads effectively, potentially playing a role in the advancement of the condition [6]. Furthermore, patients with knee KOA have been found to exhibit specific gait parameters during level walking, including slower walking speed, lower stepping frequency, shorter stride length, longer stride duration, and increased time with both feet on the ground [7].
Various factors, such as reduced joint mobility, weakened muscle strength, and impaired proprioception play a role in altering walking patterns among patients with KOA [8]. Among different types of movements, navigating stairs poses a significant challenge and risk, with approximately 10% of falls resulting in older adults occurring on stairs [9]. Descending stairs can be especially dangerous due to the greater stress placed on the joints compared to ascending stairs [10]. Falls on stairs are more likely to happen during the slow-down phase of descending compared to ascending, with the risk being as high as 3 to 1 [11]. Stair climbing demands strength and puts greater stress on weight-bearing joints compared to regular walking for healthy people [10]. Additionally, it involves placing the entire body weight on one leg at a time, exerting forces to move the body upward and forward to the next step [12].
A recent study reported that patients with KOA develop compensatory strategies in the joints near and far from the affected knee, which helps them adjust to their impaired walking and reduces their ability to climb stairs [13]. Although we have noticed variations in joint movements in the lower limbs when comparing individuals with KOA and those without, particularly during stair climbing, our understanding of how these alterations in joint mechanics impact the overall adjustments in gait during stair climbing is limited [14]. To gain a comprehensive grasp of how KOA impacts an individual’s overall functionality during the important daily activity of stair climbing, it is crucial to thoroughly examine the timing and spatial aspects of gait [14]. This examination can provide valuable insights for improving treatment and rehabilitation programs and, subsequently, enhancing the quality of life for these patients [14]. With this in mind, this study compares specific spatial variables (step length, step width, stride length, and velocity) and temporal variables (time spent in single and double-support, and total support) between individuals in the early stages of KOA and healthy individuals during both stair ascent and descent.
Our hypotheses are twofold. Firstly, we expect that individuals in the early stages of KOA will display notable variances in spatial gait characteristics (step length, step width, stride length, and speed) when compared to healthy individuals during both stair ascent and descent. Secondly, we anticipate that patients with early-stage KOA will exhibit distinct differences in temporal gait characteristics (time spent in single and double-support, and total support) compared to healthy individuals while climbing up and down stairs.
Materials and Methods
Study participants
This nested case-control study involved the participation of 12 individuals diagnosed with KOA, of whom six were male and six were female. In addition, 12 healthy controls (six males and six females), were also recruited for the study (Table 1).

The recruitment of KOA subjects was carried out within a large local orthopedic practice, while control subjects were enlisted through targeted advertisements in public places.
The sample size determination in our study was conducted through a comprehensive power analysis, incorporating spatial-temporal data from prior scholarly works by Hicks-Little et al. [14] and Asay et al. [15], utilizing a standardized mean difference of 1.0 to represent a clinically significant distinction between our KOA and healthy control groups in terms of spatial-temporal stair gait variables. A desired statistical power of 0.80 was set, with a significance level (α) of 0.05.
Inclusion and exclusion criteria
The study outlined clear inclusion criteria for the participants as follows. Firstly, individuals aged 45 years or older were considered eligible. Secondly, the diagnosis of KOA was established based on the clinical criteria provided by the American College of Rheumatology [16]. Moreover, the severity of the disease was evaluated using the Kellgren-Lawrence grading scale, a widely accepted tool for assessing and classifying radiographic features of KOA [16]. Specifically, a Kellgren-Lawrence grade greater than one indicated the presence of KOA. The patient group consisted of six individuals diagnosed with grade two KOA and an additional six individuals with grade one KOA. It is crucial to emphasize that a qualified physician conducted the clinical evaluation of participants with bilateral medial KOA, assessing disease severity through physical examination and knee radiography. The diagnostic criteria for osteoarthritis were based on established guidelines and protocols. The control group, composed of healthy subjects, was carefully selected to ensure the absence of knee joint pain and minimal to no radiographic evidence of joint surface degradation. These individuals were matched with the KOA group in terms of age and demographic characteristics.
Furthermore, a rigorous exclusion protocol was implemented to ensure the inclusion of only participants who met meticulous inclusion criteria in the study. The participants excluded from participation if they were older than 80 years old, with a history of strokes, uncontrolled hypertension, and neuromuscular diseases, such as multiple sclerosis or Parkinson disease were excluded, as well as those with neurological disorders including cerebral palsy, dementia, and vertigo. Additionally, participants requiring mobility assistive devices, recent treatments, or having a body mass index over 40 kg/m2 indicating obesity, lower extremity fractures, concurrent hip osteoarthritis, awaiting arthroplasty, or having cardiovascular diseases were also excluded. Furthermore, the participants needing assistance to perform standing or walking tasks, who had undergone any form of treatment within the previous two months, or who had received rehabilitation or medication treatment during the study period were not included. Moreover, participants who had received injections or undergone surgical procedures within six months before the study were excluded [16, 17].
Study measurements
Before the commencement of testing, all participants were required to complete the modified version of the Western Ontario McMaster (WOMAC) osteoarthritis index. This well-established assessment tool is widely utilized to evaluate pain, joint stiffness, and functional limitations in individuals with KOA [18]. The modified WOMAC index encompasses a comprehensive evaluation of these three constructs, consisting of 5 pain-related items, 2 stiffness items, and 7 functional items.
The study employed a Qualisys 3D motion capture system (Qualisys AB, Göteborg, Sweden) comprising eight infrared optoelectronic cameras (Miqus M1) to accurately capture and analyze spatial-temporal variables associated with stair negotiation. The participants were instructed to ascend and descend a customized three-step staircase with specific dimensions (step height=18 cm, tread length=28.5 cm). For a comprehensive stair gait analysis, a bilateral 50-reflective-spherical marker configuration, following the OpenSim marker set by Moissenet et al. (2019) was employed to cover the lower limbs [19] (Figure 1). Before the test trials, a single static calibration trial was performed. The participants were asked to climb the stairs barefoot and place one foot on each step while maintaining their self-selected pace. The timing of each stride event during ascent and descent was expressed as a percentage of the stair gait cycle according to Protopapadaki et al. (2007) [20]. In the context of stair locomotion, the definition of a complete gait cycle during ascent involved the initial contact of the affected extremity on the first step, followed by the culmination of the cycle with the contact of the same foot on the third step. In contrast, a complete gait cycle during descent commenced with the affected extremity making contact on the second step and concluded with contact on the floor [14].
To fully assess and describe the stair gait of the participants, various spatial-temporal variables were measured. These variables included step length, step width, stride length, velocity, single-support time, double-support time, and total support time. Measurements were in cm for step length, step width, and stride length, and cm/s for velocity. The data collected from each marker was sampled at a rate of 120 Hz and filtered using a second-order zero-lag Butterworth digital filter with a cutoff frequency of 6 Hz. The averages from three ascending and descending trials were used for data analysis. The processed coordinate data was analyzed using the Qualisys Track Manager (QTM) software, version 2022.2 and Excel to obtain specific spatial and temporal stair gait variables of interest.
Statistical analyses
In the initial stage of the study, we computed the Mean±SD of demographic variables and spatial-temporal variables for each participant, distinguishing them based on their group (KOA vs healthy controls) and stair direction (ascent vs descent). Our objective was to assess the effects of group and stair direction on spatial variables, including step length, step width, stride length, and velocity, as well as on temporal variables such as single- and double-support time, total support, and swing time. To achieve this, we conducted a 2×2 repeated-measures multivariate analysis of covariance for the spatial variables, and another 2×2 repeated-measures multivariate analysis of covariance for the temporal variables. Subsequently, we employed follow-up univariate F tests to individually evaluate the effects of group, direction, and the interaction between the independent variables on the stair gait outcome variables in both spatial and temporal domains. All statistical analyses were performed using the SPSS software, version 24 (SPSS Inc, Chicago, Ill).
Results
Table 1 presents the Mean±SD for the characteristics of the subjects, anthropometric variables, and the modified WOMAC questionnaire scores. According to the results of the independent sample t-test, the two groups under investigation, namely the KOA and control groups, were similar in terms of age (P=0.92), height (P=0.41), mass (P=0.87), and body mass index (P=0.87). In contrast, following the WOMAC osteoarthritis index, the KOA group exhibited higher global scores (P<0.001), greater overall pain (P<0.001), increased joint stiffness (P<0.001), and reduced function (P<0.001) than the healthy matched controls, as anticipated.
The analysis of the spatial gait variables yielded significant findings. Firstly, there was no significant interaction between the group (KOA and healthy groups) and direction (ascending and descending stairs), indicating that the combined spatial gait variables were not influenced by the relationship between these factors (Wilks Λ=0.856, F(7, 27)=0.588, P=0.801). However, significant main effects were observed for both the groups (Wilks Λ=0.540, F(7, 27)=3.086, P=0.023) and direction (Wilks Λ=0.199, F(7, 27)=10.783, P<0.001). Similarly, the analysis of the temporal gait variables revealed no significant interaction between the group and direction for the linear combination (Wilks Λ=0.672, F(7, 27)=0.613, P=0.911). However, notable main effects were found for both the group and direction (Wilks Λ=0.455, F(7, 27)=4.010, P=0.018), as well as for the direction alone (Wilks Λ=0.255, F(7, 27)=8.934, P=0.001).
Further investigation of the individual effects of group and direction on each spatial and temporal stair gait variable revealed significant differences, as presented in Table 2 and Table 3.

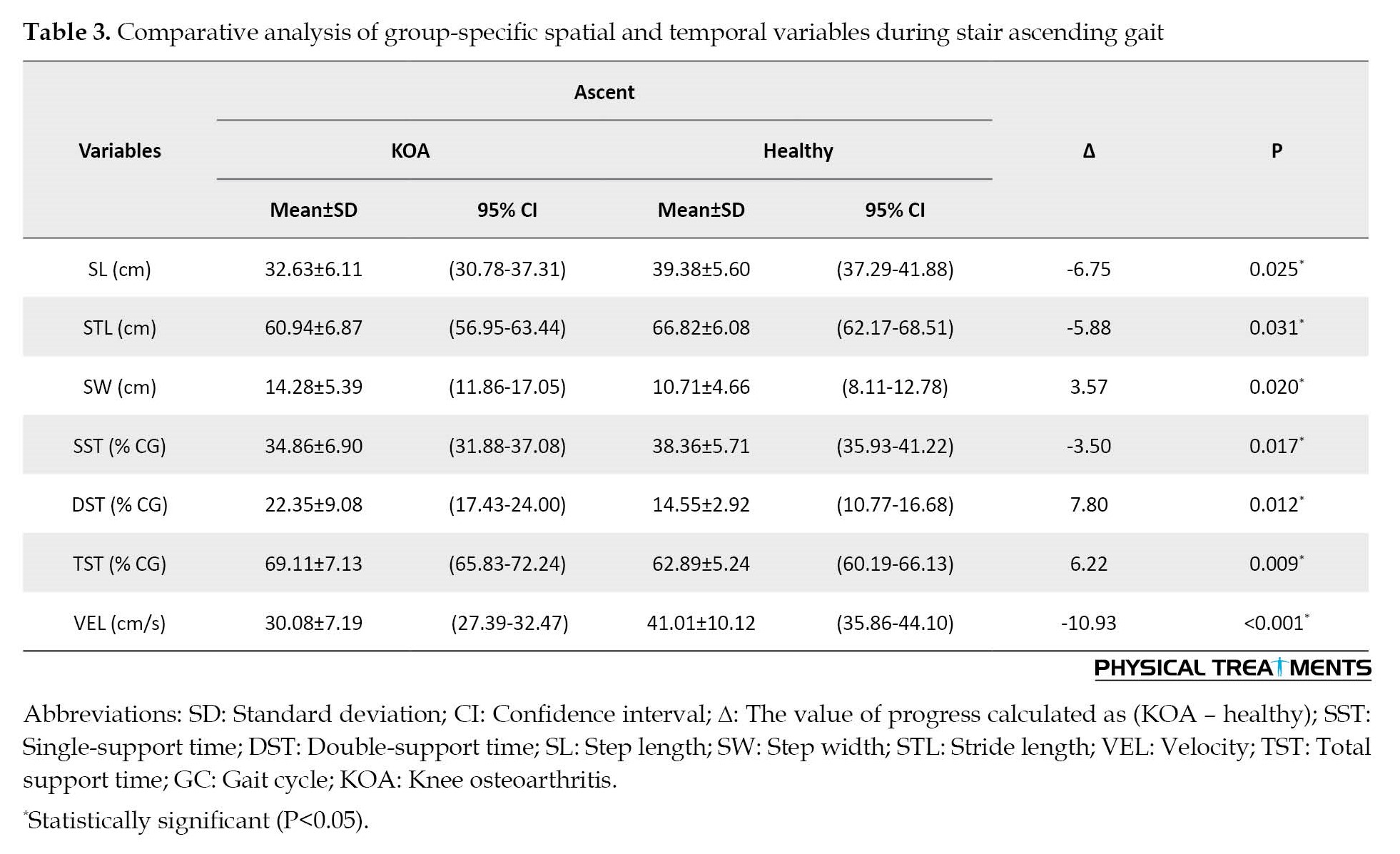
In terms of stair descending, the KOA group displayed distinct stair gait characteristics compared to the control group. They exhibited shorter step length (F(1, 24)=6.002, P=0.019), wider step width (F(1, 24)=4.623, P=0.029), shorter stride length (F(1, 24)=6.098, P=0.022), reduced time in single-support time (F(1, 24)=5.551, P=0.011), increased time in double-support time (F(1, 24)=7.875, P=0.009), prolonged total support time (F(1, 24)=9.862, P=0.003), and lower velocity (F(1, 24)=18.509, P<0.001). Similarly, during stair ascending, the KOA group also demonstrated significant differences compared to the control group. They exhibited shorter step length (F(1, 24)=5.977, P=0.025), wider step width (F(1, 24)=5.333, P=0.029), shorter stride length (F(1, 24)=4.796, P=0.031), reduced time in single-support time (F(1, 24)=6.798, P=0.017), increased time in double-support time (F(1, 24)=10.021, P=0.004), prolonged total support time (F(1, 24)=13.262, P=0.009), and lower velocity (F(1, 24)=16.863, P<0.001). These findings highlight the significant differences in spatial and temporal gait variables observed in individuals with KOA during both stair descending and ascending when compared to the control group.
Notably, during stair ascent, there was a decrease in overall stair gait velocity compared to stair descent (F(1, 24)=30.411, P<0.001). Additionally, step width was greater during stair descent compared to ascent (F(1, 24)=4.013, P=0.039), while no significant differences were observed for step length (F(1, 24)=0.792, P=0.318) and stride length (F(1, 24)=0.344, P=0.571) between the two directions. Moreover, during stair ascent, it was found that more time was allocated to single-support time (F(1, 24)=7.996, P=0.009), double-support time (F(1, 24)=4.112, P=0.038), and total support time (F(1, 24)=11.100, P<0.001) compared to stair descent.
Discussion
In this study, the researchers compared how patients with KOA negotiate stairs in terms of their spatial and temporal stair gait, to those of healthy individuals of the same age. Our study revealed that patients with KOA exhibit certain changes in their walking patterns when climbing stairs compared to healthy individuals. These changes include narrower step widths, shorter stride lengths, slower walking speed, increased time in the double-support stance, reduced time in the single-support stance, and overall, more time spent in the total support phase compared to the swing phase. These findings suggest that individuals with moderate KOA adapt their gait during stair climbing due to the presence of joint pathology. Our results align with previous research that has examined gait characteristics in KOA patients during both level walking [5, 7] and stair climbing [10, 14].
Individuals with KOA face significant challenges when it comes to climbing stairs. Previous studies have shown that there are notable differences in how patients with moderate to severe KOA climb stairs compared to healthy individuals [10, 21]. These variations encompass movements of the trunk, knee extensor moments [10], and the hip and ankle joints [21]. Nonetheless, the implications of these alterations in movements of lower-extremity joints on overall gait adjustments, particularly during stair ascent and descent, remain poorly comprehended. Consequently, our study ascertained whether distinct spatial (step length, step width, stride length, and velocity) and temporal (single- and double-support time, total support, and swing time) gait characteristics differ between individuals in the early stages of KOA and healthy individuals during the act of climbing up and down stairs.
When examining the step and stride characteristics of both groups, several significant dissimilarities were noted. Individuals with KOA demonstrated a broader step width but a shorter step and stride lengths in comparison to the control group. Furthermore, the participants with KOA exhibited a decreased total velocity, indicating a slower ascent and descent on stairs. Moreover, individuals with KOA spent more time in the double support phase and less time in the single support phase when compared to the control group. Additionally, the KOA group displayed an extended overall support duration and a reduced swing duration as opposed to the control group.
The findings about differences in step width and stride length were expected since patients with KOA typically widen their stance to better manage the position of their center of mass over their base of support [22]. Previous studies investigating gait in KOA patients during level walking have also shown that they tend to have shorter strides and step lengths compared to healthy individuals [7, 8]. This adjustment in gait is a natural response to the pain, stiffness, muscle weakness, and instability experienced by those with KOA, as it allows them to better control the position of their center of mass [14]. Additionally, research indicates that these alterations in gait may also be adaptations to the abnormal loading on the knee joint caused by the degenerative disease [23].
Numerous studies investigating walking patterns in young and older adults have similarly discovered that older individuals typically exhibit wider step widths. This observation implies that these modifications serve as adaptive mechanisms aimed at preserving balance during walking [21, 24, 25]. Additional research suggests that individuals with KOA encounter a reduction in stride length and gait velocity. This decline is attributed to the impairment of mechanoreceptors in their proprioceptive system, which is a consequence of degenerative joint disease [26]. Due to the aforementioned damage, people with KOA undergo adaptations in their walking techniques to offset the proprioceptive deficiencies in their joints. Moreover, modifying step length serves as a compensatory kinematic process enabling individuals who are overweight to walk with lower knee torque compared to their body mass index [27]. However, there were no differences in body mass index values between the KOA group and the healthy comparison group, although when examining the body mass index values of the subjects with KOA in this particular study, the majority were classified as obese.
Both groups also exhibited a wider step width while going down the stairs compared to going up. This widening of step width during descent is attributed to the heightened requirement for balance and control compared to ascent [14]. As outlined in the research conducted by Hicks-Little et al. (2012), individuals have to counterbalance the effects of gravity and acceleration while descending stairs. One effective method to achieve this is by widening the step width, which enhances the control of the center of mass over the supporting surface [14]. There were no significant disparities observed in step length or stride length between going up and going down. This could be attributed to the fact that these aspects are to some degree influenced by the characteristics of the staircase itself.
The observed difference in the overall stair climbing velocity of both groups is not surprising considering the observed deficiencies in step and stride length between groups. These combined deficiencies in the timing and spacing of their walking steps are a result of the subjects attempting to maintain control of their body’s center of mass while climbing stairs. To achieve this, they increase the time spent in both the double and total support phase, inevitably leading to a decrease in their overall gait velocity. This adjustment allows them to sustain their upright balance throughout the entire walking cycle. Additionally, it is suspected that the slower velocity at which the subjects with KOA climb stairs is influenced by the pain, stiffness, and muscle weakness they experience. The average reported pain level among these individuals was 7 out of 20, with stiffness ratings of 3.5 out of 8, and functional disability indicating difficulty with activities that require muscular strength according to the WOMAC osteoarthritis index. Numerous studies investigating gait in individuals with KOA have consistently reported slower walking velocities, shorter stride lengths, longer periods of double support, and increased total support time during walking [7, 28-30]. While our focus was specifically on stair climbing gait, our findings align with research that has investigated various aspects of timing and spacing in the gait of patients with KOA during level walking.
When examining the overall walking speed of all participants, regardless of the staircase level, it was discovered that they moved at a slower pace while going up the stairs compared to going down. This result was expected since individuals have to overcome gravity while ascending, which decreases their linear momentum. In contrast, when descending, the force of gravity accelerates the body downward, resulting in an increased linear momentum. The body’s downward acceleration demands a more robust dynamic balance from the leg supporting the body weight to manage the swinging motion during the descent [14].
The differences observed in the timing of the walking phases of the two groups align with previous findings indicating that KOA patients have reduced stability in a single support phase and therefore rely more on double support to maintain stability [7, 8, 14]. Nadeau et al. (2003) have also researched healthy older adults and showed similar results to the control group in this study [31]. This can be attributed to KOA patients relying more on the stance phase during walking to enhance stability while minimizing the time spent in the swing phase to avoid potential balance issues and reduce joint pain during the single support phase. Additionally, Lee and Chou’s (2007) research has suggested that KOA affects the temporal control of the quadriceps, leading to alterations in gait cycle phases [21]; therefore, the presence of quadriceps muscle inhibition may further contribute to the observed changes in temporal and spatial variables compared to the control group.
When comparing the act of going up and down stairs among all participants, they had longer durations in the single support, double support, and total support phases during going up than going down. This resulted in a shorter duration of the swing phase during ascent compared to descent. These observations correspond to the unique physical demands imposed on the body during stair ascent and descent. During ascent, muscle energy is transformed into potential energy for the body, requiring concentric muscle contractions to generate the necessary force for lifting each step. Conversely, during descent, the muscles must absorb potential energy, necessitating eccentric muscle contractions to create controlling forces and decelerate the body. These disparities support our findings that individuals spend more time in the total support phase when ascending stairs [14].
Conclusion
The findings of our study indicate that patients with KOA demonstrate distinct alterations in their gait patterns while negotiating stairs when compared to healthy individuals of the same age. Specifically, individuals with KOA exhibited narrower step widths, shorter stride lengths, slower walking speed, increased time in the double-support stance, reduced time in the single-support stance, and a greater duration in the total support phase relative to the swing phase. These results suggest that individuals with early-stage KOA adapt their gait during stair climbing in response to joint pathology.
These findings have significant implications for various areas. Firstly, they provide valuable insights for healthcare professionals, enabling them to understand the unique gait alterations in KOA patients during stair negotiation. This knowledge can facilitate more accurate diagnosis, improved treatment strategies, and customized rehabilitation programs. Additionally, these findings can contribute to the development of assistive devices or adaptations in environments such as stairwells to better accommodate the specific needs of individuals with KOA. Furthermore, the identified gait alterations can serve as objective measures for assessing disease progression and treatment efficacy over time. By monitoring and analyzing these gait parameters, clinicians can track the impact of interventions, observe improvements or deterioration, and make informed decisions regarding therapeutic approaches. Overall, the findings pave the way for enhanced patient care and intervention strategies tailored towards improving the stair negotiation abilities and overall mobility of individuals with KOA.
Study limitations
We should recognize the constraints of our research. Firstly, our study included a relatively small number of participants, consisting of both males and females. While we attempted to mitigate the impact of gender by analyzing covariances, future studies need to incorporate a larger sample size to attain more robust and conclusive outcomes. Additionally, further investigations should focus on exploring lower limb joint position sense deficits and muscle strength weaknesses in both patient and healthy cohorts. By studying the influence of these variables on stair gait characteristics, we can gain a deeper comprehension of the underlying mechanisms contributing to the disparities between the two groups.
Ethical Considerations
Compliance with ethical guidelines
The study adhered to ethical protocols outlined by the Research Ethics Committee of the Bu-Ali Sina University of Hamedan and was duly registered with the committee (Code: IR.BASU.REC.1402.017), ensuring compliance with established guidelines.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors made an equal contribution to the research process and writing the article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors are thankful to all the participants in this study.
References
Knee osteoarthritis (KOA) is a prevalent orthopedic illness that has a significant impact on the overall well-being of patients. Its primary manifestation involves the degeneration of the articular cartilage, and it is more commonly found among middle-aged and elderly individuals [1]. KOA results in a range of difficulties, including discomfort, limited joint mobility, significant medical costs, and a heightened likelihood of disability [2]. These issues are often linked to various factors, such as age, obesity, inflammation, previous injuries, and genetic predisposition [2]. According to previous studies, at least 10% of individuals aged 55 years and above suffer from KOA, among whom, approximately one-fourth experience disability [3].
The primary symptoms associated with KOA are pain, decreased functionality, and occasional stiffness in the joints [4], which restricts individuals’ ability to perform tasks, such as standing up from a chair, walking comfortably, or climbing stairs [5]. Moreover, individuals with KOA exhibit different movement patterns and muscle activation strategies compared to healthy individuals when walking or climbing stairs [5, 6]. The alterations can impact the knee’s capacity to distribute loads effectively, potentially playing a role in the advancement of the condition [6]. Furthermore, patients with knee KOA have been found to exhibit specific gait parameters during level walking, including slower walking speed, lower stepping frequency, shorter stride length, longer stride duration, and increased time with both feet on the ground [7].
Various factors, such as reduced joint mobility, weakened muscle strength, and impaired proprioception play a role in altering walking patterns among patients with KOA [8]. Among different types of movements, navigating stairs poses a significant challenge and risk, with approximately 10% of falls resulting in older adults occurring on stairs [9]. Descending stairs can be especially dangerous due to the greater stress placed on the joints compared to ascending stairs [10]. Falls on stairs are more likely to happen during the slow-down phase of descending compared to ascending, with the risk being as high as 3 to 1 [11]. Stair climbing demands strength and puts greater stress on weight-bearing joints compared to regular walking for healthy people [10]. Additionally, it involves placing the entire body weight on one leg at a time, exerting forces to move the body upward and forward to the next step [12].
A recent study reported that patients with KOA develop compensatory strategies in the joints near and far from the affected knee, which helps them adjust to their impaired walking and reduces their ability to climb stairs [13]. Although we have noticed variations in joint movements in the lower limbs when comparing individuals with KOA and those without, particularly during stair climbing, our understanding of how these alterations in joint mechanics impact the overall adjustments in gait during stair climbing is limited [14]. To gain a comprehensive grasp of how KOA impacts an individual’s overall functionality during the important daily activity of stair climbing, it is crucial to thoroughly examine the timing and spatial aspects of gait [14]. This examination can provide valuable insights for improving treatment and rehabilitation programs and, subsequently, enhancing the quality of life for these patients [14]. With this in mind, this study compares specific spatial variables (step length, step width, stride length, and velocity) and temporal variables (time spent in single and double-support, and total support) between individuals in the early stages of KOA and healthy individuals during both stair ascent and descent.
Our hypotheses are twofold. Firstly, we expect that individuals in the early stages of KOA will display notable variances in spatial gait characteristics (step length, step width, stride length, and speed) when compared to healthy individuals during both stair ascent and descent. Secondly, we anticipate that patients with early-stage KOA will exhibit distinct differences in temporal gait characteristics (time spent in single and double-support, and total support) compared to healthy individuals while climbing up and down stairs.
Materials and Methods
Study participants
This nested case-control study involved the participation of 12 individuals diagnosed with KOA, of whom six were male and six were female. In addition, 12 healthy controls (six males and six females), were also recruited for the study (Table 1).

The recruitment of KOA subjects was carried out within a large local orthopedic practice, while control subjects were enlisted through targeted advertisements in public places.
The sample size determination in our study was conducted through a comprehensive power analysis, incorporating spatial-temporal data from prior scholarly works by Hicks-Little et al. [14] and Asay et al. [15], utilizing a standardized mean difference of 1.0 to represent a clinically significant distinction between our KOA and healthy control groups in terms of spatial-temporal stair gait variables. A desired statistical power of 0.80 was set, with a significance level (α) of 0.05.
Inclusion and exclusion criteria
The study outlined clear inclusion criteria for the participants as follows. Firstly, individuals aged 45 years or older were considered eligible. Secondly, the diagnosis of KOA was established based on the clinical criteria provided by the American College of Rheumatology [16]. Moreover, the severity of the disease was evaluated using the Kellgren-Lawrence grading scale, a widely accepted tool for assessing and classifying radiographic features of KOA [16]. Specifically, a Kellgren-Lawrence grade greater than one indicated the presence of KOA. The patient group consisted of six individuals diagnosed with grade two KOA and an additional six individuals with grade one KOA. It is crucial to emphasize that a qualified physician conducted the clinical evaluation of participants with bilateral medial KOA, assessing disease severity through physical examination and knee radiography. The diagnostic criteria for osteoarthritis were based on established guidelines and protocols. The control group, composed of healthy subjects, was carefully selected to ensure the absence of knee joint pain and minimal to no radiographic evidence of joint surface degradation. These individuals were matched with the KOA group in terms of age and demographic characteristics.
Furthermore, a rigorous exclusion protocol was implemented to ensure the inclusion of only participants who met meticulous inclusion criteria in the study. The participants excluded from participation if they were older than 80 years old, with a history of strokes, uncontrolled hypertension, and neuromuscular diseases, such as multiple sclerosis or Parkinson disease were excluded, as well as those with neurological disorders including cerebral palsy, dementia, and vertigo. Additionally, participants requiring mobility assistive devices, recent treatments, or having a body mass index over 40 kg/m2 indicating obesity, lower extremity fractures, concurrent hip osteoarthritis, awaiting arthroplasty, or having cardiovascular diseases were also excluded. Furthermore, the participants needing assistance to perform standing or walking tasks, who had undergone any form of treatment within the previous two months, or who had received rehabilitation or medication treatment during the study period were not included. Moreover, participants who had received injections or undergone surgical procedures within six months before the study were excluded [16, 17].
Study measurements
Before the commencement of testing, all participants were required to complete the modified version of the Western Ontario McMaster (WOMAC) osteoarthritis index. This well-established assessment tool is widely utilized to evaluate pain, joint stiffness, and functional limitations in individuals with KOA [18]. The modified WOMAC index encompasses a comprehensive evaluation of these three constructs, consisting of 5 pain-related items, 2 stiffness items, and 7 functional items.
The study employed a Qualisys 3D motion capture system (Qualisys AB, Göteborg, Sweden) comprising eight infrared optoelectronic cameras (Miqus M1) to accurately capture and analyze spatial-temporal variables associated with stair negotiation. The participants were instructed to ascend and descend a customized three-step staircase with specific dimensions (step height=18 cm, tread length=28.5 cm). For a comprehensive stair gait analysis, a bilateral 50-reflective-spherical marker configuration, following the OpenSim marker set by Moissenet et al. (2019) was employed to cover the lower limbs [19] (Figure 1). Before the test trials, a single static calibration trial was performed. The participants were asked to climb the stairs barefoot and place one foot on each step while maintaining their self-selected pace. The timing of each stride event during ascent and descent was expressed as a percentage of the stair gait cycle according to Protopapadaki et al. (2007) [20]. In the context of stair locomotion, the definition of a complete gait cycle during ascent involved the initial contact of the affected extremity on the first step, followed by the culmination of the cycle with the contact of the same foot on the third step. In contrast, a complete gait cycle during descent commenced with the affected extremity making contact on the second step and concluded with contact on the floor [14].
To fully assess and describe the stair gait of the participants, various spatial-temporal variables were measured. These variables included step length, step width, stride length, velocity, single-support time, double-support time, and total support time. Measurements were in cm for step length, step width, and stride length, and cm/s for velocity. The data collected from each marker was sampled at a rate of 120 Hz and filtered using a second-order zero-lag Butterworth digital filter with a cutoff frequency of 6 Hz. The averages from three ascending and descending trials were used for data analysis. The processed coordinate data was analyzed using the Qualisys Track Manager (QTM) software, version 2022.2 and Excel to obtain specific spatial and temporal stair gait variables of interest.
Statistical analyses
In the initial stage of the study, we computed the Mean±SD of demographic variables and spatial-temporal variables for each participant, distinguishing them based on their group (KOA vs healthy controls) and stair direction (ascent vs descent). Our objective was to assess the effects of group and stair direction on spatial variables, including step length, step width, stride length, and velocity, as well as on temporal variables such as single- and double-support time, total support, and swing time. To achieve this, we conducted a 2×2 repeated-measures multivariate analysis of covariance for the spatial variables, and another 2×2 repeated-measures multivariate analysis of covariance for the temporal variables. Subsequently, we employed follow-up univariate F tests to individually evaluate the effects of group, direction, and the interaction between the independent variables on the stair gait outcome variables in both spatial and temporal domains. All statistical analyses were performed using the SPSS software, version 24 (SPSS Inc, Chicago, Ill).
Results
Table 1 presents the Mean±SD for the characteristics of the subjects, anthropometric variables, and the modified WOMAC questionnaire scores. According to the results of the independent sample t-test, the two groups under investigation, namely the KOA and control groups, were similar in terms of age (P=0.92), height (P=0.41), mass (P=0.87), and body mass index (P=0.87). In contrast, following the WOMAC osteoarthritis index, the KOA group exhibited higher global scores (P<0.001), greater overall pain (P<0.001), increased joint stiffness (P<0.001), and reduced function (P<0.001) than the healthy matched controls, as anticipated.
The analysis of the spatial gait variables yielded significant findings. Firstly, there was no significant interaction between the group (KOA and healthy groups) and direction (ascending and descending stairs), indicating that the combined spatial gait variables were not influenced by the relationship between these factors (Wilks Λ=0.856, F(7, 27)=0.588, P=0.801). However, significant main effects were observed for both the groups (Wilks Λ=0.540, F(7, 27)=3.086, P=0.023) and direction (Wilks Λ=0.199, F(7, 27)=10.783, P<0.001). Similarly, the analysis of the temporal gait variables revealed no significant interaction between the group and direction for the linear combination (Wilks Λ=0.672, F(7, 27)=0.613, P=0.911). However, notable main effects were found for both the group and direction (Wilks Λ=0.455, F(7, 27)=4.010, P=0.018), as well as for the direction alone (Wilks Λ=0.255, F(7, 27)=8.934, P=0.001).
Further investigation of the individual effects of group and direction on each spatial and temporal stair gait variable revealed significant differences, as presented in Table 2 and Table 3.

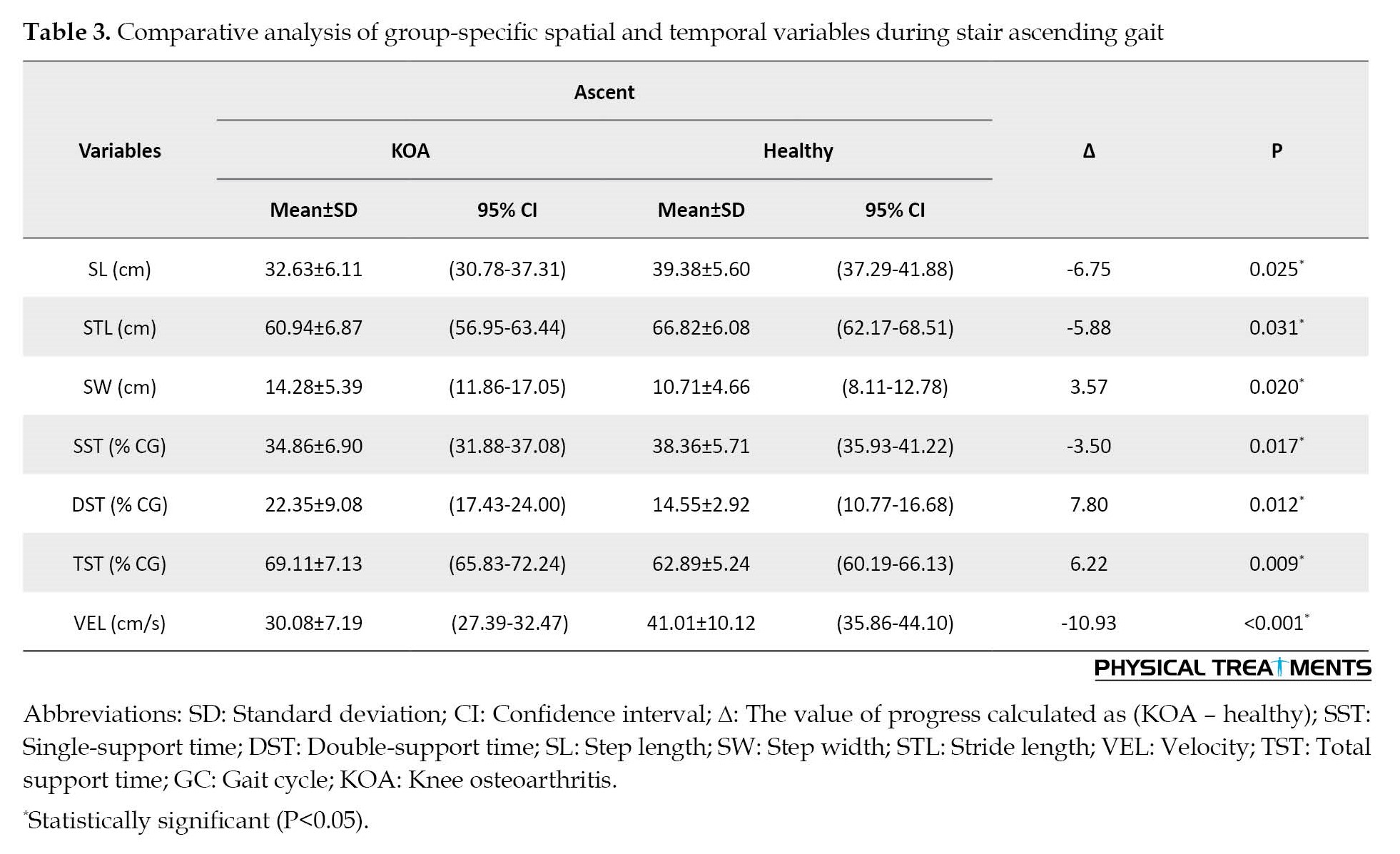
In terms of stair descending, the KOA group displayed distinct stair gait characteristics compared to the control group. They exhibited shorter step length (F(1, 24)=6.002, P=0.019), wider step width (F(1, 24)=4.623, P=0.029), shorter stride length (F(1, 24)=6.098, P=0.022), reduced time in single-support time (F(1, 24)=5.551, P=0.011), increased time in double-support time (F(1, 24)=7.875, P=0.009), prolonged total support time (F(1, 24)=9.862, P=0.003), and lower velocity (F(1, 24)=18.509, P<0.001). Similarly, during stair ascending, the KOA group also demonstrated significant differences compared to the control group. They exhibited shorter step length (F(1, 24)=5.977, P=0.025), wider step width (F(1, 24)=5.333, P=0.029), shorter stride length (F(1, 24)=4.796, P=0.031), reduced time in single-support time (F(1, 24)=6.798, P=0.017), increased time in double-support time (F(1, 24)=10.021, P=0.004), prolonged total support time (F(1, 24)=13.262, P=0.009), and lower velocity (F(1, 24)=16.863, P<0.001). These findings highlight the significant differences in spatial and temporal gait variables observed in individuals with KOA during both stair descending and ascending when compared to the control group.
Notably, during stair ascent, there was a decrease in overall stair gait velocity compared to stair descent (F(1, 24)=30.411, P<0.001). Additionally, step width was greater during stair descent compared to ascent (F(1, 24)=4.013, P=0.039), while no significant differences were observed for step length (F(1, 24)=0.792, P=0.318) and stride length (F(1, 24)=0.344, P=0.571) between the two directions. Moreover, during stair ascent, it was found that more time was allocated to single-support time (F(1, 24)=7.996, P=0.009), double-support time (F(1, 24)=4.112, P=0.038), and total support time (F(1, 24)=11.100, P<0.001) compared to stair descent.
Discussion
In this study, the researchers compared how patients with KOA negotiate stairs in terms of their spatial and temporal stair gait, to those of healthy individuals of the same age. Our study revealed that patients with KOA exhibit certain changes in their walking patterns when climbing stairs compared to healthy individuals. These changes include narrower step widths, shorter stride lengths, slower walking speed, increased time in the double-support stance, reduced time in the single-support stance, and overall, more time spent in the total support phase compared to the swing phase. These findings suggest that individuals with moderate KOA adapt their gait during stair climbing due to the presence of joint pathology. Our results align with previous research that has examined gait characteristics in KOA patients during both level walking [5, 7] and stair climbing [10, 14].
Individuals with KOA face significant challenges when it comes to climbing stairs. Previous studies have shown that there are notable differences in how patients with moderate to severe KOA climb stairs compared to healthy individuals [10, 21]. These variations encompass movements of the trunk, knee extensor moments [10], and the hip and ankle joints [21]. Nonetheless, the implications of these alterations in movements of lower-extremity joints on overall gait adjustments, particularly during stair ascent and descent, remain poorly comprehended. Consequently, our study ascertained whether distinct spatial (step length, step width, stride length, and velocity) and temporal (single- and double-support time, total support, and swing time) gait characteristics differ between individuals in the early stages of KOA and healthy individuals during the act of climbing up and down stairs.
When examining the step and stride characteristics of both groups, several significant dissimilarities were noted. Individuals with KOA demonstrated a broader step width but a shorter step and stride lengths in comparison to the control group. Furthermore, the participants with KOA exhibited a decreased total velocity, indicating a slower ascent and descent on stairs. Moreover, individuals with KOA spent more time in the double support phase and less time in the single support phase when compared to the control group. Additionally, the KOA group displayed an extended overall support duration and a reduced swing duration as opposed to the control group.
The findings about differences in step width and stride length were expected since patients with KOA typically widen their stance to better manage the position of their center of mass over their base of support [22]. Previous studies investigating gait in KOA patients during level walking have also shown that they tend to have shorter strides and step lengths compared to healthy individuals [7, 8]. This adjustment in gait is a natural response to the pain, stiffness, muscle weakness, and instability experienced by those with KOA, as it allows them to better control the position of their center of mass [14]. Additionally, research indicates that these alterations in gait may also be adaptations to the abnormal loading on the knee joint caused by the degenerative disease [23].
Numerous studies investigating walking patterns in young and older adults have similarly discovered that older individuals typically exhibit wider step widths. This observation implies that these modifications serve as adaptive mechanisms aimed at preserving balance during walking [21, 24, 25]. Additional research suggests that individuals with KOA encounter a reduction in stride length and gait velocity. This decline is attributed to the impairment of mechanoreceptors in their proprioceptive system, which is a consequence of degenerative joint disease [26]. Due to the aforementioned damage, people with KOA undergo adaptations in their walking techniques to offset the proprioceptive deficiencies in their joints. Moreover, modifying step length serves as a compensatory kinematic process enabling individuals who are overweight to walk with lower knee torque compared to their body mass index [27]. However, there were no differences in body mass index values between the KOA group and the healthy comparison group, although when examining the body mass index values of the subjects with KOA in this particular study, the majority were classified as obese.
Both groups also exhibited a wider step width while going down the stairs compared to going up. This widening of step width during descent is attributed to the heightened requirement for balance and control compared to ascent [14]. As outlined in the research conducted by Hicks-Little et al. (2012), individuals have to counterbalance the effects of gravity and acceleration while descending stairs. One effective method to achieve this is by widening the step width, which enhances the control of the center of mass over the supporting surface [14]. There were no significant disparities observed in step length or stride length between going up and going down. This could be attributed to the fact that these aspects are to some degree influenced by the characteristics of the staircase itself.
The observed difference in the overall stair climbing velocity of both groups is not surprising considering the observed deficiencies in step and stride length between groups. These combined deficiencies in the timing and spacing of their walking steps are a result of the subjects attempting to maintain control of their body’s center of mass while climbing stairs. To achieve this, they increase the time spent in both the double and total support phase, inevitably leading to a decrease in their overall gait velocity. This adjustment allows them to sustain their upright balance throughout the entire walking cycle. Additionally, it is suspected that the slower velocity at which the subjects with KOA climb stairs is influenced by the pain, stiffness, and muscle weakness they experience. The average reported pain level among these individuals was 7 out of 20, with stiffness ratings of 3.5 out of 8, and functional disability indicating difficulty with activities that require muscular strength according to the WOMAC osteoarthritis index. Numerous studies investigating gait in individuals with KOA have consistently reported slower walking velocities, shorter stride lengths, longer periods of double support, and increased total support time during walking [7, 28-30]. While our focus was specifically on stair climbing gait, our findings align with research that has investigated various aspects of timing and spacing in the gait of patients with KOA during level walking.
When examining the overall walking speed of all participants, regardless of the staircase level, it was discovered that they moved at a slower pace while going up the stairs compared to going down. This result was expected since individuals have to overcome gravity while ascending, which decreases their linear momentum. In contrast, when descending, the force of gravity accelerates the body downward, resulting in an increased linear momentum. The body’s downward acceleration demands a more robust dynamic balance from the leg supporting the body weight to manage the swinging motion during the descent [14].
The differences observed in the timing of the walking phases of the two groups align with previous findings indicating that KOA patients have reduced stability in a single support phase and therefore rely more on double support to maintain stability [7, 8, 14]. Nadeau et al. (2003) have also researched healthy older adults and showed similar results to the control group in this study [31]. This can be attributed to KOA patients relying more on the stance phase during walking to enhance stability while minimizing the time spent in the swing phase to avoid potential balance issues and reduce joint pain during the single support phase. Additionally, Lee and Chou’s (2007) research has suggested that KOA affects the temporal control of the quadriceps, leading to alterations in gait cycle phases [21]; therefore, the presence of quadriceps muscle inhibition may further contribute to the observed changes in temporal and spatial variables compared to the control group.
When comparing the act of going up and down stairs among all participants, they had longer durations in the single support, double support, and total support phases during going up than going down. This resulted in a shorter duration of the swing phase during ascent compared to descent. These observations correspond to the unique physical demands imposed on the body during stair ascent and descent. During ascent, muscle energy is transformed into potential energy for the body, requiring concentric muscle contractions to generate the necessary force for lifting each step. Conversely, during descent, the muscles must absorb potential energy, necessitating eccentric muscle contractions to create controlling forces and decelerate the body. These disparities support our findings that individuals spend more time in the total support phase when ascending stairs [14].
Conclusion
The findings of our study indicate that patients with KOA demonstrate distinct alterations in their gait patterns while negotiating stairs when compared to healthy individuals of the same age. Specifically, individuals with KOA exhibited narrower step widths, shorter stride lengths, slower walking speed, increased time in the double-support stance, reduced time in the single-support stance, and a greater duration in the total support phase relative to the swing phase. These results suggest that individuals with early-stage KOA adapt their gait during stair climbing in response to joint pathology.
These findings have significant implications for various areas. Firstly, they provide valuable insights for healthcare professionals, enabling them to understand the unique gait alterations in KOA patients during stair negotiation. This knowledge can facilitate more accurate diagnosis, improved treatment strategies, and customized rehabilitation programs. Additionally, these findings can contribute to the development of assistive devices or adaptations in environments such as stairwells to better accommodate the specific needs of individuals with KOA. Furthermore, the identified gait alterations can serve as objective measures for assessing disease progression and treatment efficacy over time. By monitoring and analyzing these gait parameters, clinicians can track the impact of interventions, observe improvements or deterioration, and make informed decisions regarding therapeutic approaches. Overall, the findings pave the way for enhanced patient care and intervention strategies tailored towards improving the stair negotiation abilities and overall mobility of individuals with KOA.
Study limitations
We should recognize the constraints of our research. Firstly, our study included a relatively small number of participants, consisting of both males and females. While we attempted to mitigate the impact of gender by analyzing covariances, future studies need to incorporate a larger sample size to attain more robust and conclusive outcomes. Additionally, further investigations should focus on exploring lower limb joint position sense deficits and muscle strength weaknesses in both patient and healthy cohorts. By studying the influence of these variables on stair gait characteristics, we can gain a deeper comprehension of the underlying mechanisms contributing to the disparities between the two groups.
Ethical Considerations
Compliance with ethical guidelines
The study adhered to ethical protocols outlined by the Research Ethics Committee of the Bu-Ali Sina University of Hamedan and was duly registered with the committee (Code: IR.BASU.REC.1402.017), ensuring compliance with established guidelines.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors made an equal contribution to the research process and writing the article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors are thankful to all the participants in this study.
References
- Zeng L, Zhou G, Yang W, Liu J. Guidelines for the diagnosis and treatment of knee osteoarthritis with integrative medicine based on traditional Chinese medicine. Frontiers in Medicine. 2023; 10:1260943. [DOI:10.3389/fmed.2023.1260943] [PMID] [PMCID]
- Riddle DL, Jiranek WA, McGlynn FJ. Yearly incidence of unicompartmental knee arthroplasty in the United States. The Journal of Arthroplasty. 2008; 23(3):408-12. [DOI:10.1016/j.arth.2007.04.012] [PMID]
- Zandiyeh P, Küpper JC, Mohtadi NGH, Goldsmith P, Ronsky JL. Effect of stochastic resonance on proprioception and kinesthesia in anterior cruciate ligament reconstructed patients. Journal of Biomechanics. 2019; 84:52-7. [DOI:10.1016/j.jbiomech.2018.12.018] [PMID]
- Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019; 393(10182):1745-59. [DOI:10.1016/S0140-6736(19)30417-9] [PMID]
- Kaufman KR, Hughes C, Morrey BF, Morrey M, An KN. Gait characteristics of patients with knee osteoarthritis. Journal of Biomechanics. 2001; 34(7):907-15. [DOI:10.1016/S0021-9290(01)00036-7] [PMID]
- Childs JD, Sparto PJ, Fitzgerald GK, Bizzini M, Irrgang JJ. Alterations in lower extremity movement and muscle activation patterns in individuals with knee osteoarthritis. Clinical Biomechanics. 2004; 19(1):44-9. [DOI:10.1016/j.clinbiomech.2003.08.007] [PMID]
- Al-Zahrani KS, Bakheit AM. A study of the gait characteristics of patients with chronic osteoarthritis of the knee. Disability and Rehabilitation. 2002; 24(5):275-80. [DOI:10.1080/09638280110087098] [PMID]
- Chen CP, Chen MJ, Pei YC, Lew HL, Wong PY, Tang SF. Sagittal plane loading response during gait in different age groups and in people with knee osteoarthritis. American Journal of Physical Medicine & Rehabilitation. 2003; 82(4):307-12. [DOI:10.1097/01.PHM.0000056987.33630.56] [PMID]
- Startzell JK, Owens DA, Mulfinger LM, Cavanagh PR. Stair negotiation in older people: A review. Journal of the American Geriatrics Society. 2000; 48(5):567-80. [DOI:10.1111/j.1532-5415.2000.tb05006.x] [PMID]
- Salsich GB, Brechter JH, Powers CM. Lower extremity kinetics during stair ambulation in patients with and without patellofemoral pain. Clinical Biomechanics. 2001; 16(10):906-12. [DOI:10.1016/S0268-0033(01)00085-7] [PMID]
- Svanström L. Falls on stairs: An epidemiological accident study. Scandinavian Journal of Social Medicine. 1974; 2(3):113-20. [DOI:10.1177/140349487400200302] [PMID]
- Bar-Haim S, Belokopytov M, Harries N, Frank A. A stair-climbing test for ambulatory assessment of children with cerebral palsy. Gait & Posture. 2004; 20(2):183-8. [DOI:10.1016/j.gaitpost.2003.09.002] [PMID]
- Hicks-Little CA, Peindl RD, Hubbard TJ, Scannell BP, Springer BD, Odum SM, et al. Lower extremity joint kinematics during stair climbing in knee osteoarthritis. Medicine and Science in Sports and Exercise. 2011; 43(3):516-24. [DOI:10.1249/MSS.0b013e3181f257be] [PMID]
- Hicks-Little CA, Peindl RD, Fehring TK, Odum SM, Hubbard TJ, Cordova ML. Temporal-spatial gait adaptations during stair ascent and descent in patients with knee osteoarthritis. The Journal of arthroplasty. 2012; 27(6):1183-9. [DOI:10.1016/j.arth.2012.01.018] [PMID]
- Asay JL, Mündermann A, Andriacchi TP. Adaptive patterns of movement during stair climbing in patients with knee osteoarthritis. Journal of Orthopaedic Research. 2009; 27(3):325-9. [DOI:10.1002/jor.20751] [PMID]
- Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and therapeutic criteria committee of the American Rheumatism Association. Arthritis and Rheumatism. 1986; 29(8):1039-49. [DOI:10.1002/art.1780290816] [PMID]
- Farrokhi S, O'Connell M, Gil AB, Sparto PJ, Fitzgerald GK. Altered gait characteristics in individuals with knee osteoarthritis and self-reported knee instability. The Journal of Orthopaedic and Sports Physical Therapy. 2015; 45(5):351-9. [DOI:10.2519/jospt.2015.5540] [PMID] [PMCID]
- Shen ZD, Yu HM, Wang JT, Shi GY, Sun Y. [Modified western ontario and mcmaster university osteoarthritis index scale used in patients with knee osteoarthritis (Chinese)]. Zhonghua Yi Xue Za Zhi. 2019; 99(7):537-41. [DOI:10.3760/cma.j.issn.0376-2491.2019.07.012] [PMID]
- Moissenet F, Bélaise C, Piche E, Michaud B, Begon M. An optimization method tracking EMG, ground reactions forces, and marker trajectories for musculo-Tendon forces estimation in equinus gait. Frontiers in Neurorobotics. 2019; 13:48. [DOI:10.3389/fnbot.2019.00048] [PMID] [PMCID]
- Protopapadaki A, Drechsler WI, Cramp MC, Coutts FJ, Scott OM. Hip, knee, ankle kinematics and kinetics during stair ascent and descent in healthy young individuals. Clinical Biomechanics. 2007; 22(2):203-10. [DOI:10.1016/j.clinbiomech.2006.09.010] [PMID]
- Lee HJ, Chou LS. Balance control during stair negotiation in older adults. Journal of Biomechanics. 2007; 40(11):2530-6. [DOI:10.1016/j.jbiomech.2006.11.001] [PMID]
- Hinman RS, Bennell KL, Metcalf BR, Crossley KM. Delayed onset of quadriceps activity and altered knee joint kinematics during stair stepping in individuals with knee osteoarthritis. Archives of Physical Medicine and Rehabilitation. 2002; 83(8):1080-6. [DOI:10.1053/apmr.2002.33068] [PMID]
- Hurwitz DE, Ryals AR, Block JA, Sharma L, Schnitzer TJ, Andriacchi TP. Knee pain and joint loading in subjects with osteoarthritis of the knee. Journal of Orthopaedic Research. 2000; 18(4):572-9. [DOI:10.1002/jor.1100180409] [PMID]
- Mian OS, Thom JM, Narici MV, Baltzopoulos V. Kinematics of stair descent in young and older adults and the impact of exercise training. Gait & Posture. 2007; 25(1):9-17. [DOI:10.1016/j.gaitpost.2005.12.014] [PMID]
- Owings TM, Grabiner MD. Variability of step kinematics in young and older adults. Gait & Posture. 2004; 20(1):26-9. [DOI:10.1016/S0966-6362(03)00088-2] [PMID]
- Sharma L, Hayes KW, Felson DT, Buchanan TS, Kirwan-Mellis G, Lou C, et al. Does laxity alter the relationship between strength and physical function in knee osteoarthritis? Arthritis and Rheumatism. 1999; 42(1):25-32. [DOI:10.1002/1529-0131(199901)42:13.0.CO;2-G] [PMID]
- DeVita P, Hortobágyi T. Obesity is not associated with increased knee joint torque and power during level walking.Journal of Biomechanics. 2003; 36(9):1355-62. [DOI:10.1016/S0021-9290(03)00119-2] [PMID]
- Sparrow WA, Tirosh O. Gait termination: A review of experimental methods and the effects of ageing and gait pathologies. Gait & Posture. 2005; 22(4):362-71. [DOI:10.1016/j.gaitpost.2004.11.005] [PMID]
- Guo Y, Liu Y, Huang X, Rong Y, He M, Wang Y, et al. The effects of shift work on sleeping quality, hypertension and diabetes in retired workers. Plos One. 2013; 8(8):e71107. [DOI:10.1371/journal.pone.0071107] [PMID] [PMCID]
- Yu B, Kienbacher T, Growney ES, Johnson ME, An KN. Reproducibility of the kinematics and kinetics of the lower extremity during normal stair-climbing. Journal of Orthopaedic Research. 1997; 15(3):348-52. [DOI:10.1002/jor.1100150306] [PMID]
- Nadeau S, McFadyen BJ, Malouin F. Frontal and sagittal plane analyses of the stair climbing task in healthy adults aged over 40 years: What are the challenges compared to level walking? Clinical Biomechanics. 2003; 18(10):950-9. [DOI:10.1016/S0268-0033(03)00179-7] [PMID]
Type of Study: Research |
Subject:
Special
Received: 2023/11/6 | Accepted: 2024/03/9 | Published: 2024/04/1
Received: 2023/11/6 | Accepted: 2024/03/9 | Published: 2024/04/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |







