Thu, Sep 18, 2025
Volume 14, Issue 1 (Winter 2024)
PTJ 2024, 14(1): 43-52 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Saki F, Shayesteh A, Ramezani F. Short-term Effects of Kinesio Taping Application on Outcomes of Athletes With Shin Splints. PTJ 2024; 14 (1) :43-52
URL: http://ptj.uswr.ac.ir/article-1-609-en.html
URL: http://ptj.uswr.ac.ir/article-1-609-en.html
1- Department of Exercise Rehabilitation, Faculty of Sport Sciences, Bu-Ali Sina University, Hamedan, Iran.
Keywords: Athletic tape, Injury, Postural balance, Preventive therapy, Medial tibial stress syndrome
Full-Text [PDF 867 kb]
(1786 Downloads)
| Abstract (HTML) (3533 Views)
Full-Text: (1302 Views)
Introduction
Shin splints (SS), or medial tibial stress syndrome (MTSS), commonly affects athletes engaged in running and jumping activities [1], causing pain in the muscles, tendons, and bone tissue around the shin bone [2]. The main symptom is experiencing pain along the inner edge of the shin bone, which hinders an athlete’s performance and overall well-being [2]. To address this issue, various treatments, including physical therapy modalities [3], leg orthosis [4, 5], and kinesio taping (KT) [6, 7] have been utilized. KT is an elastic tape that provides support to the injured area, promotes better blood circulation, reduces pain, enhances proprioception, facilitates muscle activation, and corrects biomechanical alignment [8-10].
Postural control and plantar pressure parameters play a crucial role in the performance of athletes, especially those suffering from SS. The body’s postural control involves the maintenance of the body’s position in space for stability and orientation. It is particularly vital for athletes in determining their motor skills, agility, and athletic performance. Feet bear the literal weight of our physical activities, and the distribution of forces and pressures across different foot areas, especially during movement, significantly impacts athletic performance, injury risk, and recovery. Several studies have demonstrated the impact of plantar pressures during running, and walking, and in the incidence of exercise-induced leg pain [1, 7, 11, 12]. Increased medial plantar forces have been linked in previous studies to exercise-induced leg pain, while Sharma et al. [13] hypothesized that the same may contribute to MTSS, commonly known as SS. The study by Sharma et al. [13] highlighted how plantar pressure variance can serve as a potential predictor for SS because a significant percentage of military recruits developing MTSS had higher rearfoot peak plantar forces and pressures. By monitoring and understanding these factors, conditions, such as SS can be predicted and managed and effective preventative and rehabilitative strategies can be developed for athletes. This underpins the importance of postural control and plantar pressure parameters amongst athletes, specifically those dealing with SS, influencing not just their performance but their overall well-being.
The hypothesis of this research stems from a study [14] that unveiled an acute effect of taping on plantar pressure characteristics in athletes suffering exercise-induced leg pain. Parallelly, other studies have advocated the effectiveness of KT in managing pain stemming from conditions, such as knee pain [15-18] and shoulder pain [19, 20]. This placebo-controlled trial aims to bridge the gap in the existing literature by providing insights into the short-term effects of KT on pain, postural control, and plantar pressure parameters of athletes with SS. We further effort to determine the extent to which this taping method may alleviate shin splint-related pain and contribute to the overall performance of the athletes.
Materials and Methods
Research design
This study was designed as a placebo-controlled research, aiming to investigate the effects of kinesio tape on male runners with SS in Hamedan City, Iran. The statistical population of this study consisted of purposefully selected male runner athletes aged between 20 and 32 years. The statistical sample included 32 athletes with SS, with 16 participants assigned to each group; KT and placebo control (PC) groups. To ensure eligibility, athletes had to complete a SS pain questionnaire [21] based on the criteria established by Yates and White.
Participants
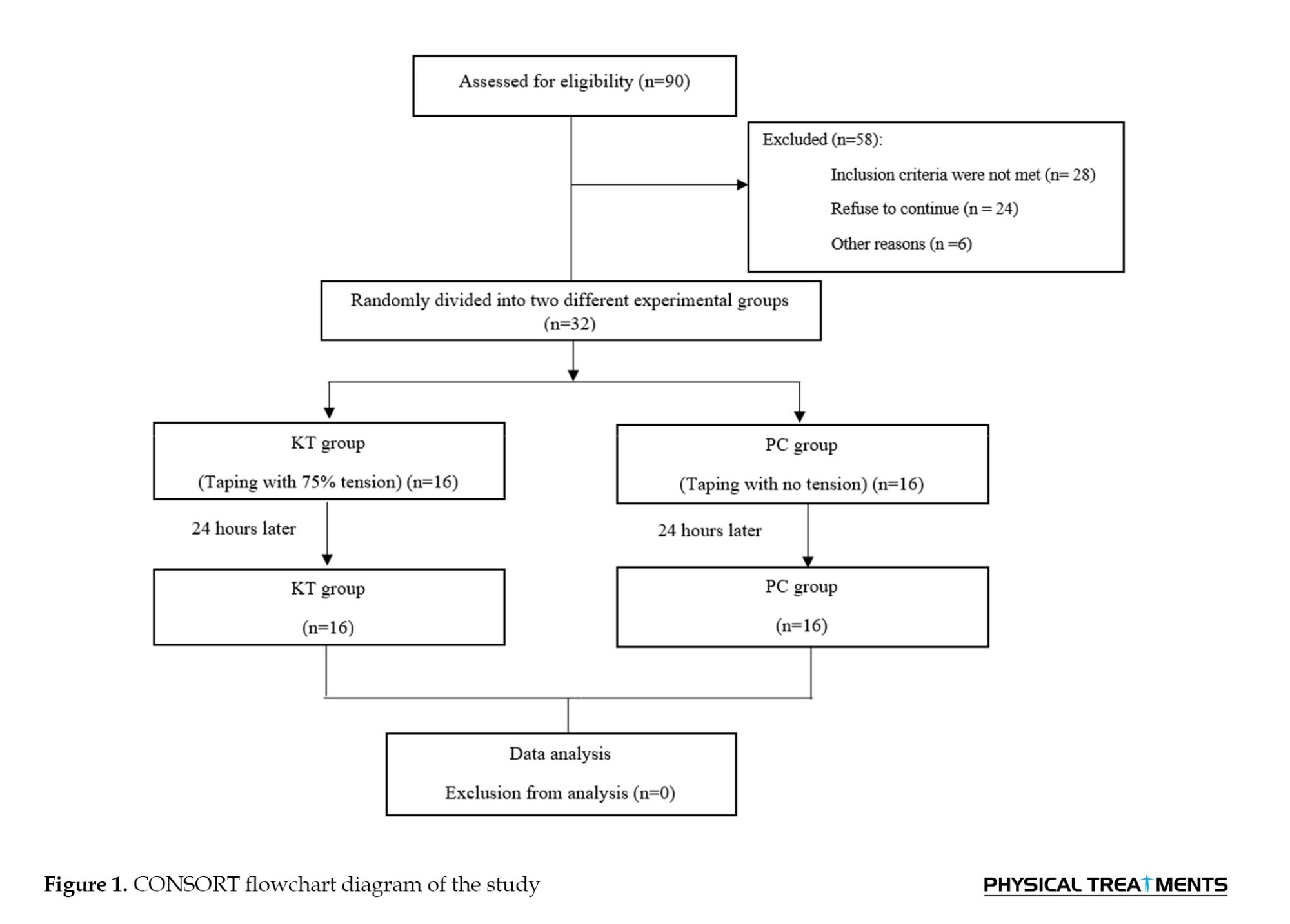
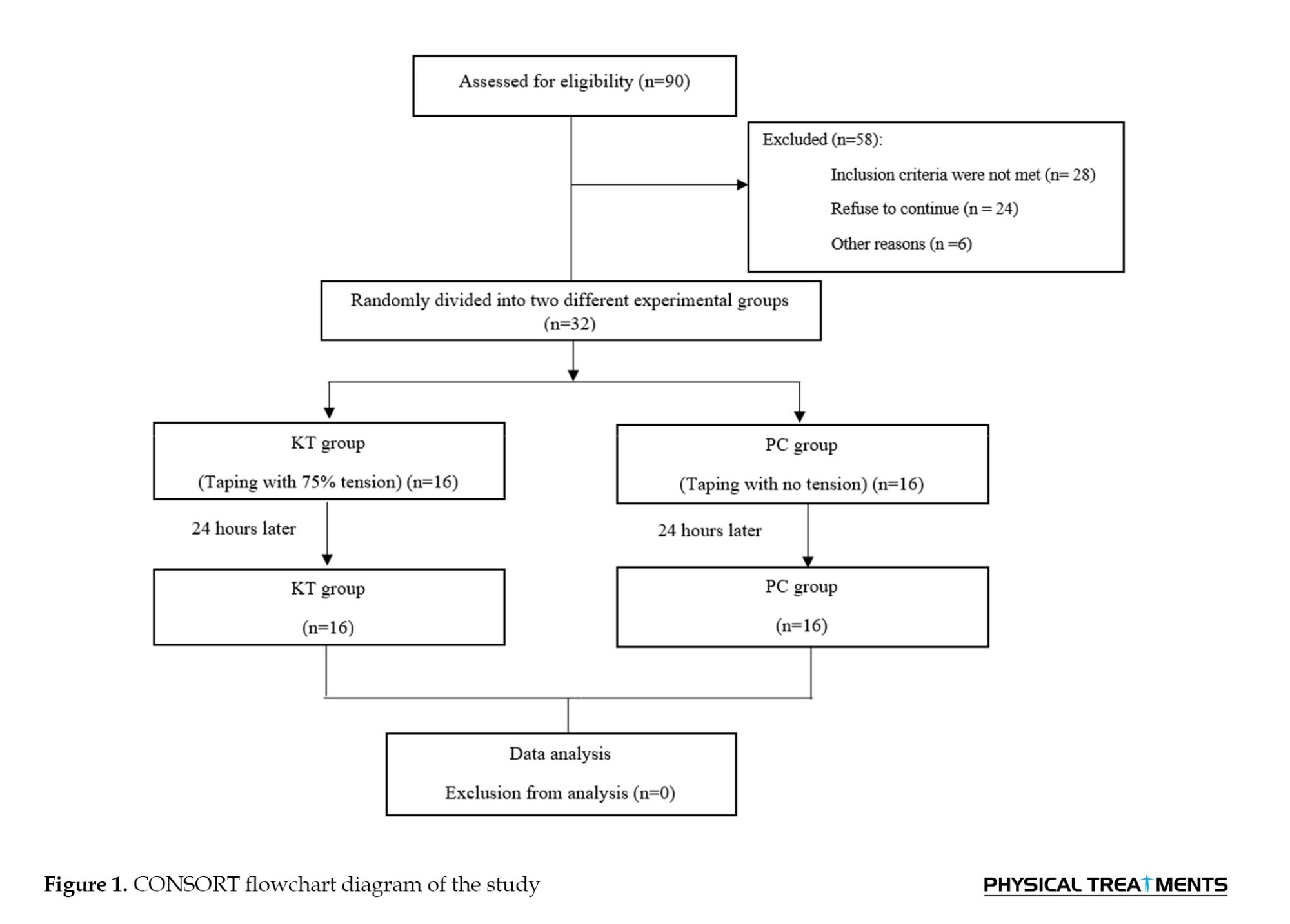
The study’s inclusion criteria included athletes who are runners and experience pain on the inner edge of the lower leg as a result of training that continues for several hours or days after training. It also included tenderness when pressure is applied to the lower inner edge of the leg’s posterior third, diffuse pain extending five centimeters over two-thirds of the lower inner-posterior part of the leg, itching in the front muscles of the leg, pain onset upon palpation of the lower inner-posterior part of the leg, pain lasting for more than a few days, pain relief during warm-up, increased pain with higher training intensity, and an uneven sensation when touching the inside blade of the shin bone [22]. The exclusion criteria included individuals with a history of fractures or surgery in the trunk and lower extremities, as well as a history of sensitivity to tape from previous skin exposure. It also excludes individuals with balance disorders unrelated to the condition being studied and those who have participated in lower leg and ankle rehabilitation programs within the past six months (Figure 1).
To ensure the subjects’ consent to participate in this research, a written consent form was provided to them. All the potential risks of the test were explained to the subjects. The people present in the research were free to participate or not participate in the test, and after declaring their cooperation, they could withdraw from the research at any time.
Procedures
All the measurements were performed for each participant at baseline and after 24 hours in the Sports Sciences Laboratory of Bu-Ali Sina University. The demographic data were collected in the pre-test session. After the pre-test assessments, the subjects were randomly assigned to the KT and PC groups. The Random Number Generator software was utilized for the randomization process, which was carried out by an individual distinct from the examiner and therapists. Initially, all participants did a pre-test session, and their pain, postural control, and plantar pressure parameters were assessed. Then after the pre-test session, the KT was applied to their leg. The subjects were asked to keep the tape on and come back after 24 hours. Then, in the post-test, the variables were re-evaluated.
Intervention
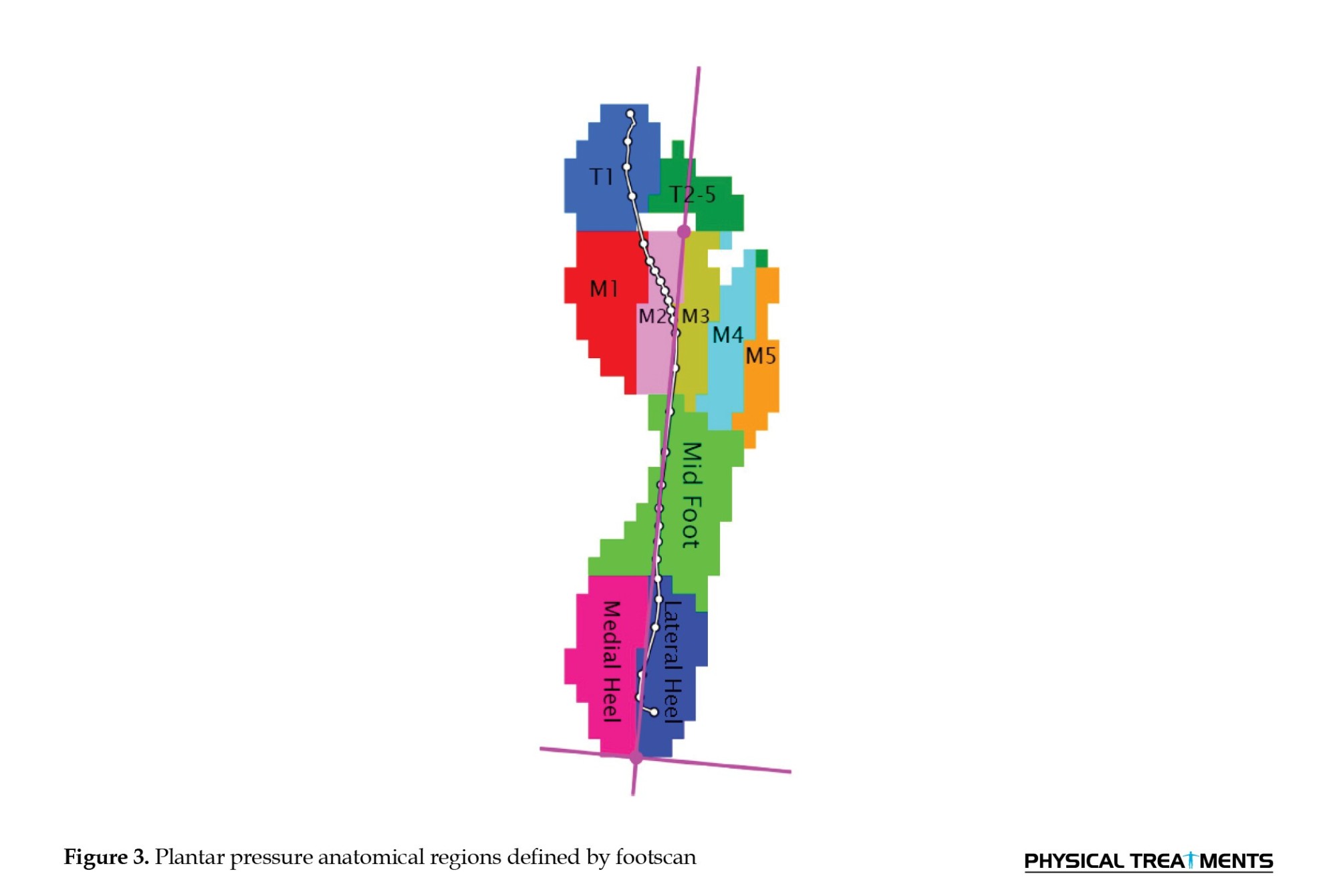
The KT group used kinesio tape on their lower leg. They followed the technique described by Griebert et al. [7], which involved shaving hair from the inner part of the tibia and cleaning the area with alcohol. A Y-shaped tape was applied, with the tail of the Y-tape placed in the upper third of the tibia. Each half of the Y-tape was applied to the front and back of the medial malleolus and ended under the arch of the foot (Figure 2). The tape was applied with 75% tension, except for the ends which were applied without any tension. The PC group received a similar application technique but without any tension.

Pain
The visual analog scale (VAS) is a valuable tool to assess subjective qualities or attitudes that are difficult to quantify directly, such as pain levels [23]. It includes a straight horizontal or vertical line with a fixed length, accompanied by a line scale ranging from 0 to 10 (where 0 signifies no pain and 10 denotes the most excruciating pain imaginable). By marking the line at the point they consider reflective of their current condition, respondents establish their visual analog scale (VAS) score. This score is determined by measuring the distance from the left or bottom end of the line to the respondent’s marked point.
Plantar pressure assessment protocol
Plantar pressure data were recorded at a sampling frequency of 300 Hz by using a foot scan system (RSscan International, Belgium, 0.5×0.5×0.02 m, 4363 sensors). For postural control assessment, participants were asked to stand on a foot scan plate with bare feet while the weight was equally distributed between the feet, arms at sides, and eyes facing straight ahead. The duration of the test was 20 s with 3 repetitions and 1 minute of rest between trials [24].
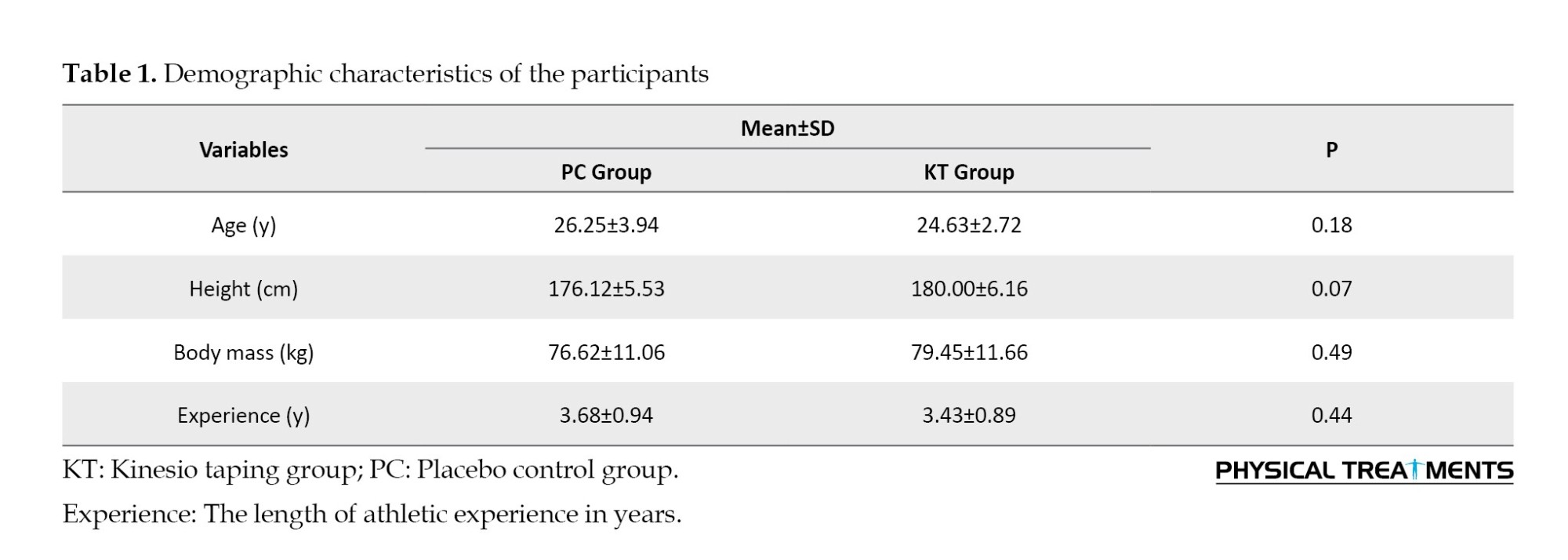
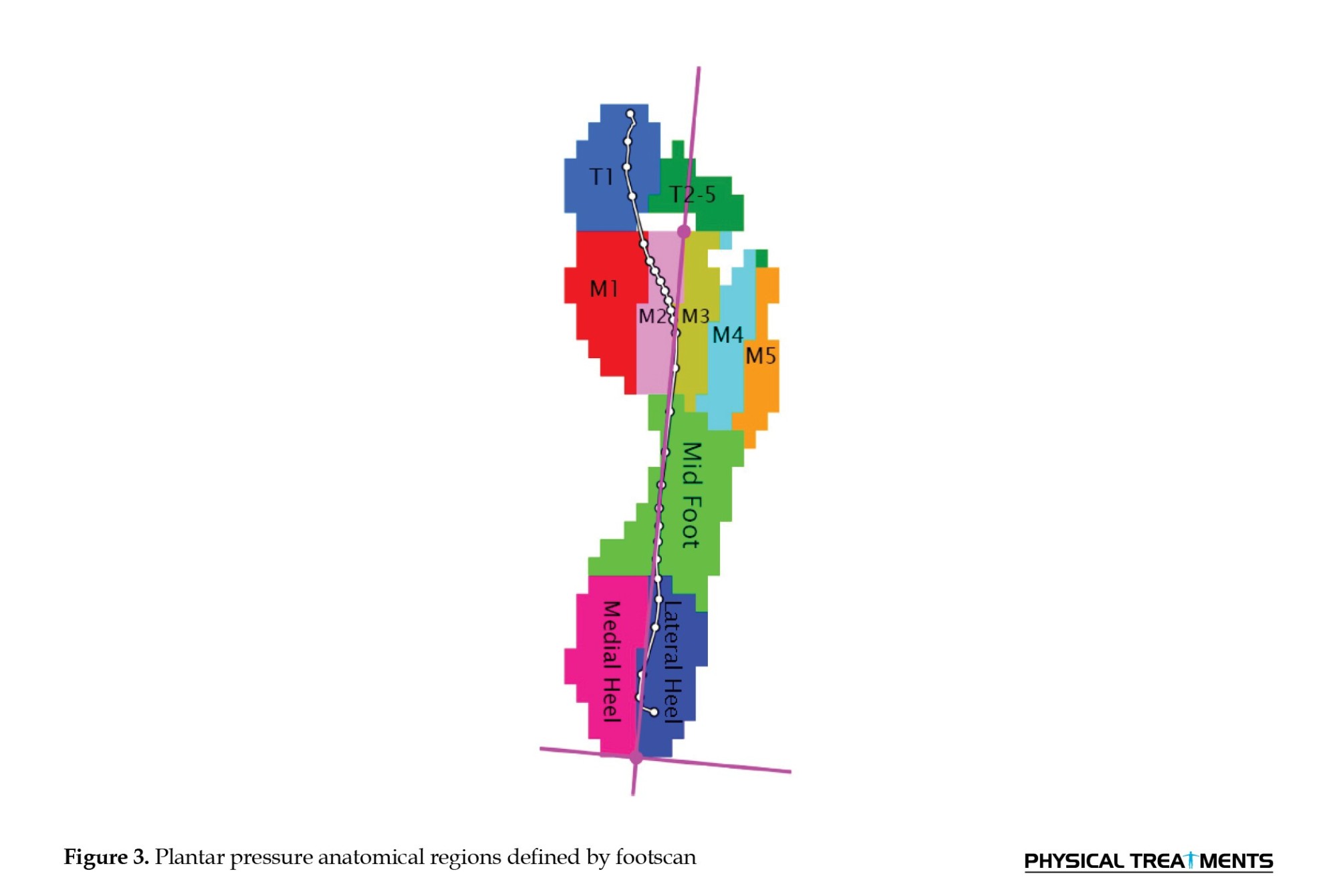
To dynamically assess plantar pressure, the participants walked at a self-selected speed along the gait pathway. The foot scan plate was placed in the middle of a 12-m gait pathway. Then the subjects were asked to start walking in a normal state with bare feet and pass over the foot scan plate. Before the test, the subjects were asked to practice the foot scan for three minutes. Walking speed was not controlled to produce a natural gait pattern. If the foot contact with the foot scan plate was not complete, the subject intentionally and artificially crossed over the foot scan, and the subject used an unusual stepping pattern, his trail was not recorded. All subjects performed three valid trials. An average of three valid trials from the affected foot was recorded. Data were extracted during the stance phases of gait. The stance phase of gait was determined as heel contact with the ground until toe lift. The studied variables were travel distance (TD), the center of pressure displacement in mediolateral (COP ML) and anterior-posterior (COP AP) directions, and the ellipse area. Plantar pressure parameters were peak pressure in ten areas of the foot. These areas include respectively, big toe (T1), second to fifth toes (T2-5), first metatarsal bone (M1), second metatarsal head (M2), third metatarsal head (M3), fourth metatarsal head (M4), fifth metatarsal head (M5), middle part of the foot (MID), medial part of the heel (MH) and lateral part of the heel (LH) (Figure 3).
Statistical analysis
The study’s statistical analysis was done using G*Power software, version 3.1.9.2 to determine the sample size. A minimum of 24 participants was determined to be necessary (medium effect size of 0.35 [14], an α level of 0.05, and a power of 0.8), and due to the dropout with 32 individuals included in the sample size. SPSS software, version 26 was used for the statistical analysis, assessing the normality of the data and the homogeneity of the variances. An independent t-test was conducted to compare demographic information between the groups and a mixed repeated measure analysis of variance (ANOVA) was employed to assess any interaction between the groups (KT and PC) and time (pre and post-intervention). Pairwise comparisons were performed using Bonferroni corrections. The effect size was calculated using partial eta squared, with values of 0.10, 0.25, and 0.40 considered as small, medium, and large, respectively. Statistical significance was determined at P<0.05.
Results
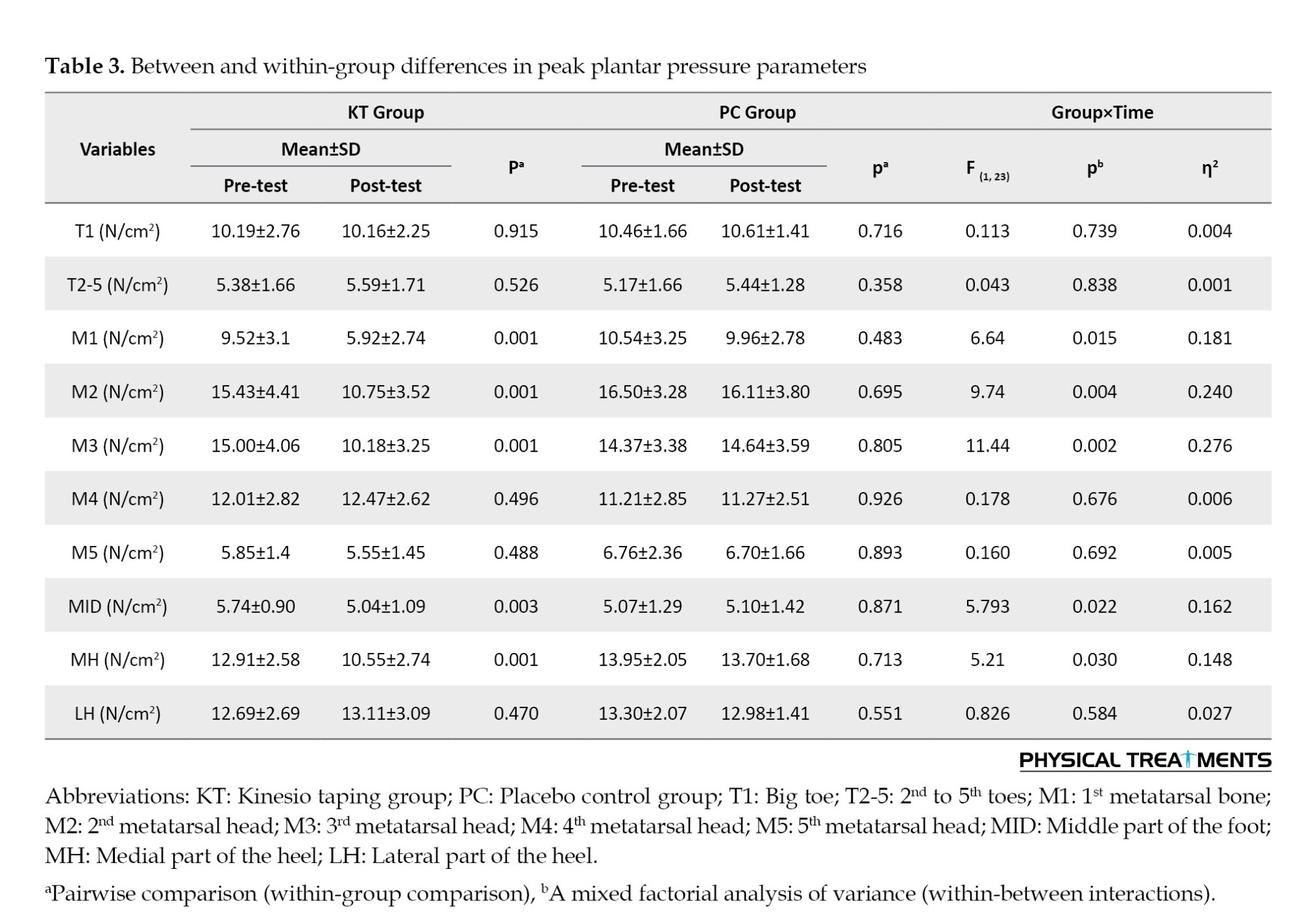
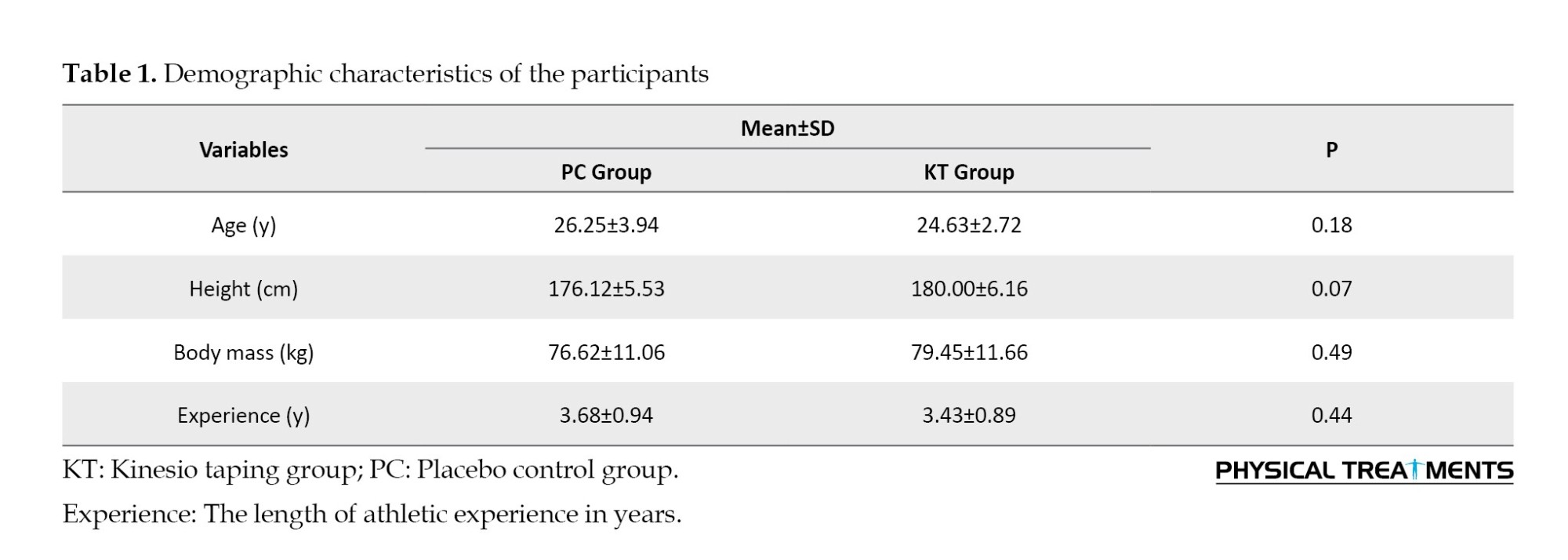
Parametric tests were employed for analysis due to the normal data distribution (P>0.05). Table 1 presents the demographic characteristics of each group and the outcomes of the independent t-test. No significant distinctions were observed among the groups regarding mean age, height, body mass, and experience (P>0.05; independent t-test).
Results from a mixed repeated measure ANOVA showed a significant interaction effect of group×time on pain (P=0.001, η2=0.432), ellipse area (P=0.041, η2=0.132), and COP in the ML direction (P=0.002, η2=0.280). However, no statistically significant interaction effects of group×time were observed on travel distance and COP in the AP direction (Table 2). Pairwise comparisons indicated that pain, ellipse area, and COP in the ML direction were significantly lower in the post-test compared to the pre-test after KT intervention (P<0.05). No significant differences were observed in COP in the AP direction and travel distance (TD) from pre-test to post-test in the KT group.

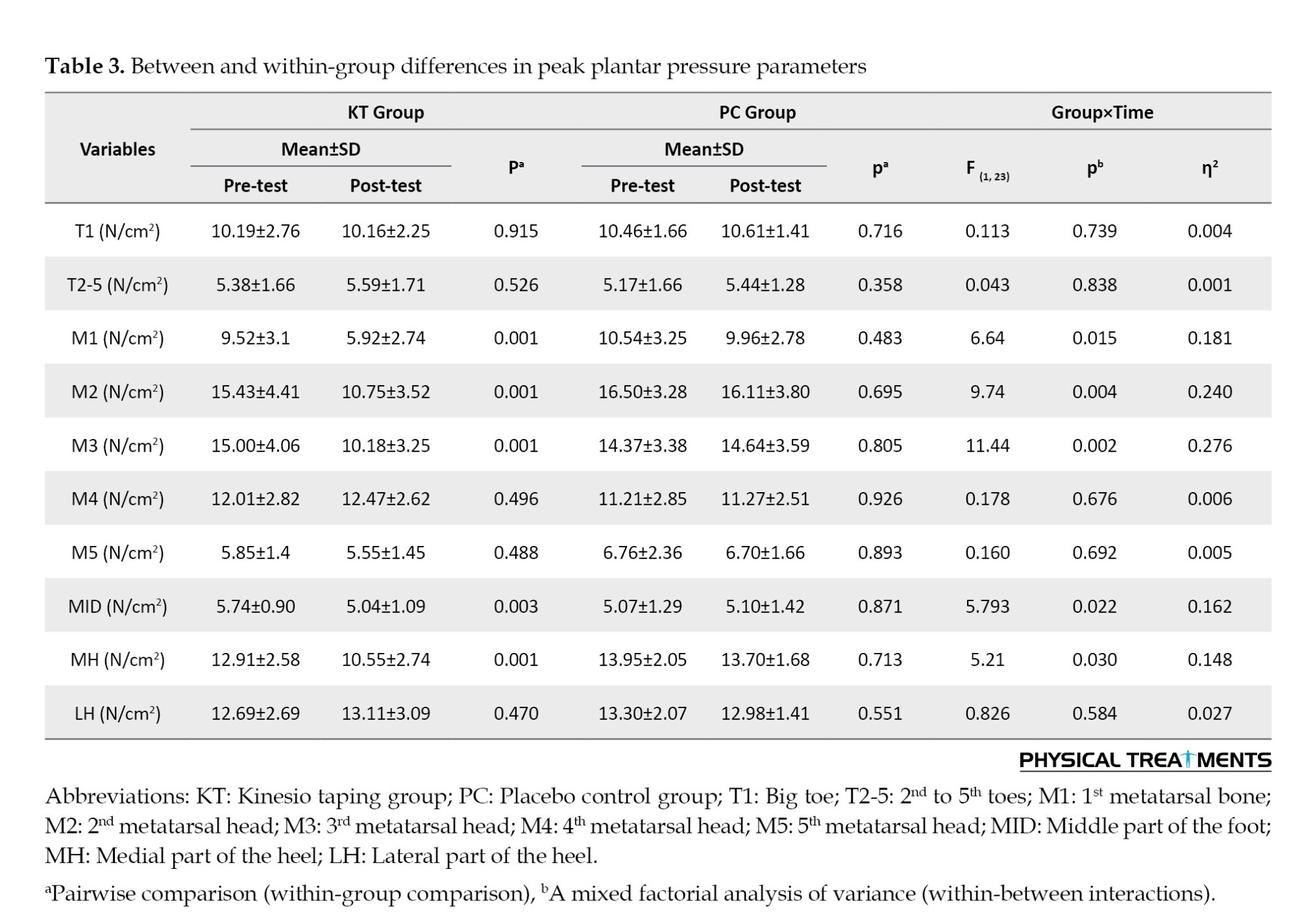
Results from a mixed repeated measure ANOVA revealed significant interaction effects of group×time on M1 (P=0.015, η2=0.181), M2 (P=0.004, η2=0.240), M3 (P=0.002, η2=0.276), MID (P=0.022, η2=0.162), and MH (P=0.030, η2=0.148). However, no significant interaction effects of group×time were found for other plantar pressure parameters (T1, T2-5, M4, M5, and LH) (Table 3).
Discussion
This study was conducted to investigate the short-term effects of using KT on pain, postural control, and plantar pressure in athletes with SS. The results suggest that KT provides immediate pain relief and demonstrates improvements in postural control and redistribution of plantar pressure. However, it is essential to note that it does not completely remove the underlying cause of SS.
The reduction in perceived pain among athletes is consistent with previous research that has identified the analgesic effects of KT [6, 25]. These pain-relieving effects may be attributed to neural suppression that can alter the sensory inputs responsible for pain perception [20, 26]. Additionally, KT appears to facilitate an immediate physiological response that helps normalize muscle function and improve lymphatic circulation, making it an effective conservative management option for athletes with SS [20]. Furthermore, the KT method used in this study may control stress and strain on the muscles, tendons, and bones of the lower leg, specifically targeting the tibialis posterior and soleus muscles that attach to the medial tibial border, thereby reducing pain associated with SS. Several studies have demonstrated that interventions, such as supportive shoes, orthotics, insoles, and KT, can help reduce pain and prevent SS in athletes [6, 27-29]. These interventions aim to provide stability and cushioning for the foot, prevent excessive pronation, and correct biomechanical alignment. By doing so, they may decrease stress on the lower leg, improve shock absorption, and optimize pressure distribution throughout the foot. The anti-pronation KT group showed a larger decrease in pain intensity than the space correction KT group in a study comparing it to taping for space correction [6, 14]. Nevertheless, several other studies have discovered no significant distinction in pain relief or prevention of shin splints between anti-pronation interventions and placebo or control interventions [14, 27]. These studies propose that foot pronation may not be a significant risk factor for shin splints and that other factors such as training load, volume, intensity, surface area, technique, muscle strength, flexibility, and fatigue could have a more crucial role in its development.
This study demonstrated an impressive improvement in both ellipse area and COP displacement, indicating enhanced balance, stability, and control over movements following the application of the KT. The reduction in ellipse area suggests that participants gained better command over their foot pressure, which is crucial for runners and athletes in terms of stability, balance, injury prevention, and energy efficiency. Decreasing in COP displacement was observed in both the ML and AP directions in the KT group. The reduction was particularly significant in the ML direction, while it approached significance in the AP direction. This result suggests that the COP ML displacement is more sensitive to external disturbances or internal disruptions compared to COP AP. This sensitivity can be attributed to the body’s lower inertia and muscle strength in the frontal plane compared to the sagittal plane [30, 31]. The decrease in COP ML displacement indicates a reduction in lateral movements and an increase in forward movements in runners, highlighting their improved balance and body control due to the KT [32]. This improvement may be attributed to the tactile stimulation provided by the tape, which enhances proprioceptive feedback and aids in increasing postural control [33]. Furthermore, the results suggest that KT may have a beneficial role in managing SS. The tape’s elevation of superficial tissues promotes healing by facilitating the removal of waste products from the area and stimulating nerve endings that help relax the muscles. Additionally, KT may effectively modulate foot motion and reduce overpronation [14].
A reduction in peak pressure was observed in the M1, M2, M3, MID, and MH, suggesting a more balanced distribution of plantar pressure. The use of KT may have contributed to gait changes by correcting biomechanical factors associated with musculoskeletal pathology, resulting in optimal pressure redistribution and pain relief [14, 33]. This enables athletes to return to a more natural foot pattern. Previous studies have identified foot pronation as a risk factor for developing SS [1, 12]. KT reduces the peak stress on the midfoot of people with SS during walking [7]. The mechanisms by which KT affects SS seem to involve the modification of leg biomechanics, activation pattern of leg muscles, facilitation of proprioception, and pain relief [20, 26, 33]. Previous studies have shown that KT has a greater effect on pain and physical performance compared to space correction taping [28]. Therefore, it can be considered an effective preventive and therapeutic solution for individuals with SS. Clinicians often use the low-dye tape technique to address pain and musculoskeletal injuries in the lower limbs [34]. According to a review study, this technique can bring about positive biomechanical impacts, such as raising the internal longitudinal arch, reducing heel protrusion and internal rotation of the tibia, and altering pressure distribution while standing or walking. Additionally, the tape may provide neuromuscular benefits, such as decreased activation of the tibialis anterior and tibialis posterior muscles when walking [34]. These biomechanical and neuromuscular changes observed immediately after using low-dye tape and KT suggest that their use can reduce the stress applied to the tibia and, consequently, prevent and treat MTSS. Another study has shown that low-dye tape reduces the contact area of the inner part of the foot, increases the arch of the foot, and decreases the activity of the tibialis anterior and tibialis posterior muscles [35]. This supports the use of tape as a suitable method for treating and preventing MTSS in athletes and military personnel.
Conclusion
In summary, the results of this study provide compelling evidence of the beneficial impact of KT on various aspects of foot function. The positive effects demonstrated in pain reduction, postural control enhancement, and plantar pressure distribution highlight the potential of this intervention for promoting overall balance and preventing injuries. Moreover, the potential benefits of managing shin splints underscore the practical applications of KT in athletic settings. However, further investigations are warranted to gain a comprehensive understanding of the mechanisms underlying these improvements and to explore the full range of practical applications in diverse populations and conditions. By expanding upon these initial findings, future research can provide valuable insights and guide sports therapists and athletes in maximizing the benefits of KT.
However, it is essential to note that while KT may provide short-term relief and functional improvement, it is not a definitive solution for SS. This relief is temporary and should be supplemented with comprehensive training and rehabilitation programs for complete recovery. Although our research provided valuable insights, certain limitations should be considered. Future longitudinal studies should enroll larger cohorts and evaluate the long-term effects of KT to validate our results. Additionally, while walking was chosen as the activity for observing the effect of KT on plantar loading, further studies should investigate whether these differences exist during specific exercise maneuvers that may be more representative of the population as a whole.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the study Ethics Committee of BU-Ali Sina University (Code: IR.BASU.REC.1398.046) and was registered in the Iranian Registry of Clinical Trials IRCT (Code: IRCT20210629051737N1). Informed consent was obtained from all subjects involved in the study.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, methodology, project administration, resources and formal analysis: Farzaneh Saki and Amir Shayesteh; Investigation: Amir Shayesteh; Data curation: All authors; Writing: Farzaneh Saki and Farzaneh Ramezani; Supervision: Farzaneh Saki.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank all the participants for their participation in this study.
References
Shin splints (SS), or medial tibial stress syndrome (MTSS), commonly affects athletes engaged in running and jumping activities [1], causing pain in the muscles, tendons, and bone tissue around the shin bone [2]. The main symptom is experiencing pain along the inner edge of the shin bone, which hinders an athlete’s performance and overall well-being [2]. To address this issue, various treatments, including physical therapy modalities [3], leg orthosis [4, 5], and kinesio taping (KT) [6, 7] have been utilized. KT is an elastic tape that provides support to the injured area, promotes better blood circulation, reduces pain, enhances proprioception, facilitates muscle activation, and corrects biomechanical alignment [8-10].
Postural control and plantar pressure parameters play a crucial role in the performance of athletes, especially those suffering from SS. The body’s postural control involves the maintenance of the body’s position in space for stability and orientation. It is particularly vital for athletes in determining their motor skills, agility, and athletic performance. Feet bear the literal weight of our physical activities, and the distribution of forces and pressures across different foot areas, especially during movement, significantly impacts athletic performance, injury risk, and recovery. Several studies have demonstrated the impact of plantar pressures during running, and walking, and in the incidence of exercise-induced leg pain [1, 7, 11, 12]. Increased medial plantar forces have been linked in previous studies to exercise-induced leg pain, while Sharma et al. [13] hypothesized that the same may contribute to MTSS, commonly known as SS. The study by Sharma et al. [13] highlighted how plantar pressure variance can serve as a potential predictor for SS because a significant percentage of military recruits developing MTSS had higher rearfoot peak plantar forces and pressures. By monitoring and understanding these factors, conditions, such as SS can be predicted and managed and effective preventative and rehabilitative strategies can be developed for athletes. This underpins the importance of postural control and plantar pressure parameters amongst athletes, specifically those dealing with SS, influencing not just their performance but their overall well-being.
The hypothesis of this research stems from a study [14] that unveiled an acute effect of taping on plantar pressure characteristics in athletes suffering exercise-induced leg pain. Parallelly, other studies have advocated the effectiveness of KT in managing pain stemming from conditions, such as knee pain [15-18] and shoulder pain [19, 20]. This placebo-controlled trial aims to bridge the gap in the existing literature by providing insights into the short-term effects of KT on pain, postural control, and plantar pressure parameters of athletes with SS. We further effort to determine the extent to which this taping method may alleviate shin splint-related pain and contribute to the overall performance of the athletes.
Materials and Methods
Research design
This study was designed as a placebo-controlled research, aiming to investigate the effects of kinesio tape on male runners with SS in Hamedan City, Iran. The statistical population of this study consisted of purposefully selected male runner athletes aged between 20 and 32 years. The statistical sample included 32 athletes with SS, with 16 participants assigned to each group; KT and placebo control (PC) groups. To ensure eligibility, athletes had to complete a SS pain questionnaire [21] based on the criteria established by Yates and White.
Participants
The study’s inclusion criteria included athletes who are runners and experience pain on the inner edge of the lower leg as a result of training that continues for several hours or days after training. It also included tenderness when pressure is applied to the lower inner edge of the leg’s posterior third, diffuse pain extending five centimeters over two-thirds of the lower inner-posterior part of the leg, itching in the front muscles of the leg, pain onset upon palpation of the lower inner-posterior part of the leg, pain lasting for more than a few days, pain relief during warm-up, increased pain with higher training intensity, and an uneven sensation when touching the inside blade of the shin bone [22]. The exclusion criteria included individuals with a history of fractures or surgery in the trunk and lower extremities, as well as a history of sensitivity to tape from previous skin exposure. It also excludes individuals with balance disorders unrelated to the condition being studied and those who have participated in lower leg and ankle rehabilitation programs within the past six months (Figure 1).
To ensure the subjects’ consent to participate in this research, a written consent form was provided to them. All the potential risks of the test were explained to the subjects. The people present in the research were free to participate or not participate in the test, and after declaring their cooperation, they could withdraw from the research at any time.
Procedures
All the measurements were performed for each participant at baseline and after 24 hours in the Sports Sciences Laboratory of Bu-Ali Sina University. The demographic data were collected in the pre-test session. After the pre-test assessments, the subjects were randomly assigned to the KT and PC groups. The Random Number Generator software was utilized for the randomization process, which was carried out by an individual distinct from the examiner and therapists. Initially, all participants did a pre-test session, and their pain, postural control, and plantar pressure parameters were assessed. Then after the pre-test session, the KT was applied to their leg. The subjects were asked to keep the tape on and come back after 24 hours. Then, in the post-test, the variables were re-evaluated.
Intervention
The KT group used kinesio tape on their lower leg. They followed the technique described by Griebert et al. [7], which involved shaving hair from the inner part of the tibia and cleaning the area with alcohol. A Y-shaped tape was applied, with the tail of the Y-tape placed in the upper third of the tibia. Each half of the Y-tape was applied to the front and back of the medial malleolus and ended under the arch of the foot (Figure 2). The tape was applied with 75% tension, except for the ends which were applied without any tension. The PC group received a similar application technique but without any tension.

Pain
The visual analog scale (VAS) is a valuable tool to assess subjective qualities or attitudes that are difficult to quantify directly, such as pain levels [23]. It includes a straight horizontal or vertical line with a fixed length, accompanied by a line scale ranging from 0 to 10 (where 0 signifies no pain and 10 denotes the most excruciating pain imaginable). By marking the line at the point they consider reflective of their current condition, respondents establish their visual analog scale (VAS) score. This score is determined by measuring the distance from the left or bottom end of the line to the respondent’s marked point.
Plantar pressure assessment protocol
Plantar pressure data were recorded at a sampling frequency of 300 Hz by using a foot scan system (RSscan International, Belgium, 0.5×0.5×0.02 m, 4363 sensors). For postural control assessment, participants were asked to stand on a foot scan plate with bare feet while the weight was equally distributed between the feet, arms at sides, and eyes facing straight ahead. The duration of the test was 20 s with 3 repetitions and 1 minute of rest between trials [24].
To dynamically assess plantar pressure, the participants walked at a self-selected speed along the gait pathway. The foot scan plate was placed in the middle of a 12-m gait pathway. Then the subjects were asked to start walking in a normal state with bare feet and pass over the foot scan plate. Before the test, the subjects were asked to practice the foot scan for three minutes. Walking speed was not controlled to produce a natural gait pattern. If the foot contact with the foot scan plate was not complete, the subject intentionally and artificially crossed over the foot scan, and the subject used an unusual stepping pattern, his trail was not recorded. All subjects performed three valid trials. An average of three valid trials from the affected foot was recorded. Data were extracted during the stance phases of gait. The stance phase of gait was determined as heel contact with the ground until toe lift. The studied variables were travel distance (TD), the center of pressure displacement in mediolateral (COP ML) and anterior-posterior (COP AP) directions, and the ellipse area. Plantar pressure parameters were peak pressure in ten areas of the foot. These areas include respectively, big toe (T1), second to fifth toes (T2-5), first metatarsal bone (M1), second metatarsal head (M2), third metatarsal head (M3), fourth metatarsal head (M4), fifth metatarsal head (M5), middle part of the foot (MID), medial part of the heel (MH) and lateral part of the heel (LH) (Figure 3).
Statistical analysis
The study’s statistical analysis was done using G*Power software, version 3.1.9.2 to determine the sample size. A minimum of 24 participants was determined to be necessary (medium effect size of 0.35 [14], an α level of 0.05, and a power of 0.8), and due to the dropout with 32 individuals included in the sample size. SPSS software, version 26 was used for the statistical analysis, assessing the normality of the data and the homogeneity of the variances. An independent t-test was conducted to compare demographic information between the groups and a mixed repeated measure analysis of variance (ANOVA) was employed to assess any interaction between the groups (KT and PC) and time (pre and post-intervention). Pairwise comparisons were performed using Bonferroni corrections. The effect size was calculated using partial eta squared, with values of 0.10, 0.25, and 0.40 considered as small, medium, and large, respectively. Statistical significance was determined at P<0.05.
Results
Parametric tests were employed for analysis due to the normal data distribution (P>0.05). Table 1 presents the demographic characteristics of each group and the outcomes of the independent t-test. No significant distinctions were observed among the groups regarding mean age, height, body mass, and experience (P>0.05; independent t-test).
Results from a mixed repeated measure ANOVA showed a significant interaction effect of group×time on pain (P=0.001, η2=0.432), ellipse area (P=0.041, η2=0.132), and COP in the ML direction (P=0.002, η2=0.280). However, no statistically significant interaction effects of group×time were observed on travel distance and COP in the AP direction (Table 2). Pairwise comparisons indicated that pain, ellipse area, and COP in the ML direction were significantly lower in the post-test compared to the pre-test after KT intervention (P<0.05). No significant differences were observed in COP in the AP direction and travel distance (TD) from pre-test to post-test in the KT group.

Results from a mixed repeated measure ANOVA revealed significant interaction effects of group×time on M1 (P=0.015, η2=0.181), M2 (P=0.004, η2=0.240), M3 (P=0.002, η2=0.276), MID (P=0.022, η2=0.162), and MH (P=0.030, η2=0.148). However, no significant interaction effects of group×time were found for other plantar pressure parameters (T1, T2-5, M4, M5, and LH) (Table 3).
Discussion
This study was conducted to investigate the short-term effects of using KT on pain, postural control, and plantar pressure in athletes with SS. The results suggest that KT provides immediate pain relief and demonstrates improvements in postural control and redistribution of plantar pressure. However, it is essential to note that it does not completely remove the underlying cause of SS.
The reduction in perceived pain among athletes is consistent with previous research that has identified the analgesic effects of KT [6, 25]. These pain-relieving effects may be attributed to neural suppression that can alter the sensory inputs responsible for pain perception [20, 26]. Additionally, KT appears to facilitate an immediate physiological response that helps normalize muscle function and improve lymphatic circulation, making it an effective conservative management option for athletes with SS [20]. Furthermore, the KT method used in this study may control stress and strain on the muscles, tendons, and bones of the lower leg, specifically targeting the tibialis posterior and soleus muscles that attach to the medial tibial border, thereby reducing pain associated with SS. Several studies have demonstrated that interventions, such as supportive shoes, orthotics, insoles, and KT, can help reduce pain and prevent SS in athletes [6, 27-29]. These interventions aim to provide stability and cushioning for the foot, prevent excessive pronation, and correct biomechanical alignment. By doing so, they may decrease stress on the lower leg, improve shock absorption, and optimize pressure distribution throughout the foot. The anti-pronation KT group showed a larger decrease in pain intensity than the space correction KT group in a study comparing it to taping for space correction [6, 14]. Nevertheless, several other studies have discovered no significant distinction in pain relief or prevention of shin splints between anti-pronation interventions and placebo or control interventions [14, 27]. These studies propose that foot pronation may not be a significant risk factor for shin splints and that other factors such as training load, volume, intensity, surface area, technique, muscle strength, flexibility, and fatigue could have a more crucial role in its development.
This study demonstrated an impressive improvement in both ellipse area and COP displacement, indicating enhanced balance, stability, and control over movements following the application of the KT. The reduction in ellipse area suggests that participants gained better command over their foot pressure, which is crucial for runners and athletes in terms of stability, balance, injury prevention, and energy efficiency. Decreasing in COP displacement was observed in both the ML and AP directions in the KT group. The reduction was particularly significant in the ML direction, while it approached significance in the AP direction. This result suggests that the COP ML displacement is more sensitive to external disturbances or internal disruptions compared to COP AP. This sensitivity can be attributed to the body’s lower inertia and muscle strength in the frontal plane compared to the sagittal plane [30, 31]. The decrease in COP ML displacement indicates a reduction in lateral movements and an increase in forward movements in runners, highlighting their improved balance and body control due to the KT [32]. This improvement may be attributed to the tactile stimulation provided by the tape, which enhances proprioceptive feedback and aids in increasing postural control [33]. Furthermore, the results suggest that KT may have a beneficial role in managing SS. The tape’s elevation of superficial tissues promotes healing by facilitating the removal of waste products from the area and stimulating nerve endings that help relax the muscles. Additionally, KT may effectively modulate foot motion and reduce overpronation [14].
A reduction in peak pressure was observed in the M1, M2, M3, MID, and MH, suggesting a more balanced distribution of plantar pressure. The use of KT may have contributed to gait changes by correcting biomechanical factors associated with musculoskeletal pathology, resulting in optimal pressure redistribution and pain relief [14, 33]. This enables athletes to return to a more natural foot pattern. Previous studies have identified foot pronation as a risk factor for developing SS [1, 12]. KT reduces the peak stress on the midfoot of people with SS during walking [7]. The mechanisms by which KT affects SS seem to involve the modification of leg biomechanics, activation pattern of leg muscles, facilitation of proprioception, and pain relief [20, 26, 33]. Previous studies have shown that KT has a greater effect on pain and physical performance compared to space correction taping [28]. Therefore, it can be considered an effective preventive and therapeutic solution for individuals with SS. Clinicians often use the low-dye tape technique to address pain and musculoskeletal injuries in the lower limbs [34]. According to a review study, this technique can bring about positive biomechanical impacts, such as raising the internal longitudinal arch, reducing heel protrusion and internal rotation of the tibia, and altering pressure distribution while standing or walking. Additionally, the tape may provide neuromuscular benefits, such as decreased activation of the tibialis anterior and tibialis posterior muscles when walking [34]. These biomechanical and neuromuscular changes observed immediately after using low-dye tape and KT suggest that their use can reduce the stress applied to the tibia and, consequently, prevent and treat MTSS. Another study has shown that low-dye tape reduces the contact area of the inner part of the foot, increases the arch of the foot, and decreases the activity of the tibialis anterior and tibialis posterior muscles [35]. This supports the use of tape as a suitable method for treating and preventing MTSS in athletes and military personnel.
Conclusion
In summary, the results of this study provide compelling evidence of the beneficial impact of KT on various aspects of foot function. The positive effects demonstrated in pain reduction, postural control enhancement, and plantar pressure distribution highlight the potential of this intervention for promoting overall balance and preventing injuries. Moreover, the potential benefits of managing shin splints underscore the practical applications of KT in athletic settings. However, further investigations are warranted to gain a comprehensive understanding of the mechanisms underlying these improvements and to explore the full range of practical applications in diverse populations and conditions. By expanding upon these initial findings, future research can provide valuable insights and guide sports therapists and athletes in maximizing the benefits of KT.
However, it is essential to note that while KT may provide short-term relief and functional improvement, it is not a definitive solution for SS. This relief is temporary and should be supplemented with comprehensive training and rehabilitation programs for complete recovery. Although our research provided valuable insights, certain limitations should be considered. Future longitudinal studies should enroll larger cohorts and evaluate the long-term effects of KT to validate our results. Additionally, while walking was chosen as the activity for observing the effect of KT on plantar loading, further studies should investigate whether these differences exist during specific exercise maneuvers that may be more representative of the population as a whole.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the study Ethics Committee of BU-Ali Sina University (Code: IR.BASU.REC.1398.046) and was registered in the Iranian Registry of Clinical Trials IRCT (Code: IRCT20210629051737N1). Informed consent was obtained from all subjects involved in the study.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, methodology, project administration, resources and formal analysis: Farzaneh Saki and Amir Shayesteh; Investigation: Amir Shayesteh; Data curation: All authors; Writing: Farzaneh Saki and Farzaneh Ramezani; Supervision: Farzaneh Saki.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank all the participants for their participation in this study.
References
- Hamstra-Wright KL, Bliven KC, Bay C. Risk factors for medial tibial stress syndrome in physically active individuals such as runners and military personnel: A systematic review and meta-analysis. British Journal of Sports Medicine. 2015; 49(6):362-9. [DOI:10.1136/bjsports-2014-093462] [PMID]
- Mita T. A review and analysis of current treatment approaches used by athletic trainers for medial tibial stress syndrome. [MSc thesis]. Fargo: North Dakota State University; 2021. [Link]
- Moen MH, Holtslag L, Bakker E, Barten C, Weir A, Tol JL, et al. The treatment of medial tibial stress syndrome in athletes; A randomized clinical trial. Sports Medicine, Arthroscopy, Rehabilitation, Therapy & Technology. 2012; 4:12.[DOI:10.1186/1758-2555-4-12] [PMID]
- Naderi A, Degens H, Sakinepoor A. Arch-support foot-orthoses normalize dynamic in-shoe foot pressure distribution in medial tibial stress syndrome. European Journal of Sport Science. 2019; 19(2):247-57. [DOI:10.1080/17461391.2018.1503337] [PMID]
- Naderi A, Bagheri S, Ramazanian Ahoor F, Moen MH, Degens H. Foot orthoses enhance the effectiveness of exercise, shockwave, and ice therapy in the management of medial tibial stress syndrome. Clinical Journal of Sport Medicine. 2022; 32(3):e251-60. [DOI:10.1097/JSM.0000000000000926] [PMID]
- Kachanathu SJ, Algarni FS, Nuhmani S, Alenazi AM, Hafez AR, Algarni AD. Functional outcomes of kinesio taping versus standard orthotics in the management of shin splint. The Journal of Sports Medicine and Physical Fitness. 2018; 58(11):1666-70. [DOI:10.23736/S0022-4707.17.07520-X] [PMID]
- Griebert MC, Needle AR, McConnell J, Kaminski TW. Lower-leg Kinesio tape reduces rate of loading in participants with medial tibial stress syndrome. Physical Therapy in Sport. 2016; 18:62-7. [DOI:10.1016/j.ptsp.2014.01.001] [PMID]
- Huang CY, Hsieh TH, Lu SC, Su FC. Effect of the Kinesio tape to muscle activity and vertical jump performance in healthy inactive people. Biomedical Engineering Online. 2011; 10:70. [DOI:10.1186/1475-925X-10-70] [PMID]
- Spanos S, Brunswic M, Billis E. The effect of taping on the proprioception of the ankle in a non-weight bearing position, amongst injured athletes. The Foot. 2008; 18(1):25-33. [DOI:10.1016/j.foot.2007.07.003]
- Guo S, Liu P, Feng B, Xu Y, Wang Y. Efficacy of kinesiology taping on the management of shin splints: A systematic review. The Physician and Sportsmedicine. 2022; 50(5):369-377. [DOI:10.1080/00913847.2021.1949253] [PMID]
- Willems TM, Witvrouw E, De Cock A, De Clercq D. Gait-related risk factors for exercise-related lower-leg pain during shod running. Medicine & Science in Sports & Exercise. 2007; 39(2):330-9. [DOI:10.1249/01.mss.0000247001.94470.21] [PMID]
- Newman P, Witchalls J, Waddington G, Adams R. Risk factors associated with medial tibial stress syndrome in runners: A systematic review and meta-analysis. Open Access Journal of Sports Medicine. 2013; 4:229-41. [DOI:10.2147/OAJSM.S39331] [PMID]
- Sharma J, Golby J, Greeves J, Spears IR. Biomechanical and lifestyle risk factors for medial tibia stress syndrome in army recruits: A prospective study. Gait & Posture. 2011; 33(3):361-5. [DOI:10.1016/j.gaitpost.2010.12.002] [PMID]
- Park J, Kim T. Acute effect of taping on plantar pressure characteristics in athletes with exercise-induced leg pain: A description and comparison of groups. The Physician and Sportsmedicine. 2019; 47(2):212-9. [DOI:10.1080/00913847.2018.1547085] [PMID]
- Campolo M, Babu J, Dmochowska K, Scariah S, Varughese J. A comparison of two taping techniques (kinesio and mcconnell) and their effect on anterior knee pain during functional activities. International Journal of Sports Physical Therapy. 2013; 8(2):105-10. [PMID]
- Osorio JA, Vairo GL, Rozea GD, Bosha PJ, Millard RL, Aukerman DF, et al. The effects of two therapeutic patellofemoral taping techniques on strength, endurance, and pain responses. Physical Therapy in Sport. 2013; 14(4):199-206. [DOI:10.1016/j.ptsp.2012.09.006] [PMID]
- Tsai CT, Chang WD, Lee JP. Effects of short-term treatment with kinesiotaping for plantar fasciitis. Journal of Musculoskeletal Pain. 2010; 18(1):71-80. [DOI:10.3109/10582450903495882]
- Aytar A, Nihan O, Ozgur S, Gul B, Pınar O, Metin K. Initial effects of kinesio® taping in patients with patellofemoral pain syndrome: A randomized, double-blind study. Isokinetics and Exercise Science. 2011; 19(2):135-42. [DOI:10.3233/IES-2011-0413]
- Kaya E, Zinnuroglu M, Tugcu I. Kinesio taping compared to physical therapy modalities for the treatment of shoulder impingement syndrome. Clinical Rheumatology. 2011; 30(2):201-7. [DOI:10.1007/s10067-010-1475-6] [PMID]
- Thelen MD, Dauber JA, Stoneman PD. The clinical efficacy of kinesio tape for shoulder pain: A randomized, double-blinded, clinical trial. Journal of Orthopaedic & Sports Physical Therapy. 2008; 38(7):389-95. [DOI:10.2519/jospt.2008.2791] [PMID]
- Yates B, White S. The incidence and risk factors in the development of medial tibial stress syndrome among naval recruits. The American Journal of Sports Medicine. 2004; 32(3):772-80. [DOI:10.1177/0095399703258776] [PMID]
- Winters M. The diagnosis and management of medial tibial stress syndrome: An evidence update. Der Unfallchirurg. 2020; 123(Suppl 1):15-9. [DOI:10.1007/s00113-019-0667-z] [PMID]
- Delgado DA, Lambert BS, Boutris N, McCulloch PC, Robbins AB, Moreno MR, et al. Validation of Digital Visual Analog Scale Pain Scoring with a traditional paper-based Visual Analog Scale in adults. Journal of the American Academy of Orthopaedic Surgeons. Global Research & Reviews. 2018; 2(3):e088. [DOI:10.5435/JAAOSGlobal-D-17-00088] [PMID]
- Jafarnezhadgero AA, Oliveira AS, Mousavi SH, Madadi-Shad M. Combining valgus knee brace and lateral foot wedges reduces external forces and moments in osteoarthritis patients. Gait & Posture. 2018; 59:104-10. [DOI:10.1016/j.gaitpost.2017.09.040] [PMID]
- Bhusari N, Deshmukh M. Shin Splint: A review. Cureus. 2023; 15(1):e33905. [DOI:10.7759/cureus.33905] [PMID]
- Zhang, G. and R. Wang, Progress and prospect in research about kinesio taping on human performance and the related mechanism. Chinese Sport Science and Technology. 2015; 51(1):73-80. [Link]
- Sharma U, Sinha AGK. Comparison of effectiveness of kinesio taping with nonelastic taping and no taping in players with acute shin splints. Physiotherapy-The Journal of Indian Association of Physiotherapists. 2017; 11(1):21. [Link]
- Nayak S, Manjunatha A, Kumar Thakur P. Effect of elastic anti pronation taping technique along with Cryotherapy in decreasing pain and increasing ankle dorsiflexion range of motion in female subjects with medial tibia stress syndrome. National Journal of Clinical Orthopaedics. 2020; 4(3):15-8. [DOI:10.33545/orthor.2020.v4.i3a.228]
- calf stretching for individuals with medial tibial stress syndrome. Foot & Ankle Specialist. 2010; 3(1):15-20. [DOI:10.1177/1938640009355659] [PMID]
- Paterna M, Dvir Z, De Benedictis C, Maffiodo D, Franco W, Ferraresi C, et al. Center of pressure displacement due to graded controlled perturbations to the trunk in standing subjects: The force-impulse paradigm. European Journal of Applied Physiology. 2022; 122(2):425-35. [DOI:10.1007/s00421-021-04844-9] [PMID]
- Choi H, Kim WS. Anterior-posterior displacement of center of pressure measured by insole foot pressure measurement system in subacute recovery stage of post-stroke hemiplegia. Technology and Health Care. 2018; 26(4):649-57.[DOI:10.3233/THC-181310] [PMID]
- Hohmann E, Reaburn P, Tetsworth K, Imhoff A. Plantar pressures during long distance running: An investigation of 10 marathon runners. Journal of Sports Science & Medicine. 2016; 15(2):254-62. [PMID]
- Williams S, Whatman C, Hume PA, Sheerin K. Kinesio taping in treatment and prevention of sports injuries: A meta-analysis of the evidence for its effectiveness. Sports Medicine. 2012; 42(2):153-64. [DOI:10.2165/11594960-000000000-00000] [PMID]
- Franettovich M, Chapman A, Blanch P, Vicenzino B. A physiological and psychological basis for anti-pronation taping from a critical review of the literature. Sports Medicine. 2008; 38(8):617-31. [DOI:10.2165/00007256-200838080-00001] [PMID]
- Franettovich M, Chapman AR, Blanch P, Vicenzino B. Augmented low-Dye tape alters foot mobility and neuromotor control of gait in individuals with and without exercise related leg pain. Journal of Foot and Ankle Research. 2010; 3:5. [DOI:10.1186/1757-1146-3-5] [PMID]
Type of Study: Research |
Subject:
General
Received: 2023/11/5 | Accepted: 2023/12/3 | Published: 2024/01/1
Received: 2023/11/5 | Accepted: 2023/12/3 | Published: 2024/01/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






