Tue, Jul 1, 2025
Volume 14, Issue 2 (Spring 2024)
PTJ 2024, 14(2): 101-114 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ansari A, Karimizadeh Ardakani M, Akoochakian M. Effectiveness of Rebounder and Foot-ankle Exercises on Biomechanics and Quality of Life in Peripheral Neuropathy Patients. PTJ 2024; 14 (2) :101-114
URL: http://ptj.uswr.ac.ir/article-1-598-en.html
URL: http://ptj.uswr.ac.ir/article-1-598-en.html
1- Department of Sport Injury and Corrective Exercise, Kish International Campus, University of Tehran, Kish, Iran.
2- Department of Health and Sports Medicine, Faculty of Physical Education and Sport Sciences, University of Tehran, Tehran, Iran.
3- Department of Sport Science, Kish International Campus, University of Tehran, Kish, Iran.
2- Department of Health and Sports Medicine, Faculty of Physical Education and Sport Sciences, University of Tehran, Tehran, Iran.
3- Department of Sport Science, Kish International Campus, University of Tehran, Kish, Iran.
Full-Text [PDF 621 kb]
(724 Downloads)
| Abstract (HTML) (2598 Views)
Full-Text: (1052 Views)
Introduction
Currently, more than 500 million adults are living with diabetes worldwide, with nearly half of them suffering from various kinds of neuropathy [1-4]. In line with the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), diabetes implications are growing rapidly and diabetic peripheral neuropathy (DPN) is the maximum common microvascular consequence, influencing as much as 70% of sufferers from diabetes [5]. DPN is caused by hyperglycemia and decreased blood supply to peripheral nerves, which commonly affect the lower extremities [6, 7]; in addition, in advanced cases, it affects the upper limbs. Diabetes-related neuropathy is responsible for 40% to 70% of traumatic lower extremity amputations. Lower limb injuries account for about 20% of the causes of hospitalization in people with diabetes, and 85% are attributable to amputation of the lower limb in patients with diabetes before the development of a wound, the main factors associated with which are foot deformity and trauma. Sensorimotor neuropathy, one of DPN’s symptoms, causes a gradual loss of tactile sensation and pain sensitivity, often known as the loss of protective sensation of the feet, which makes the feet more vulnerable to damage and increases the risk of ulceration [8]. More than half of diabetic neuropathy patients experience severe pain that interferes with work and social activities. Furthermore, the psychosocial impacts of diabetic neuropathy impair a person’s quality of life (QoL) [9]. Diabetic neuropathy, which has a detrimental influence on postural balance, alterations in walking kinematics, and deficiencies in proprioception, raises the risk of falling, which is most closely associated with depressive symptoms in diabetic patients [1-3].
The progression of DPN causes biomechanical, sensory, and motor complications that result in diabetic foot problems, loss of overall foot function, an increased proportion of fat tissue in foot muscles, leg muscle dysfunction, such as reduced joint mobility, intrinsic foot muscle atrophy, distal muscle weakness, and a decrease in the mechanical properties of the calcaneal tendon [10].
These induce a loss of balance between the flexor and extensor muscles, resulting in joint abnormalities such as claw fingers, hammer toes, overlapping fingers, metatarsal head protrusion, and hallux valgus (b:union:). Such abnormalities result in pressure point changes in the soles of the feet, as well as overload and skin reactions with localized hyperkeratosis (callus), which escalates to sole ulcers with continued walking. Healthy people have a higher plantar pressure peak in the posterior area of the foot (up to 6 kg/cm2) in static conditions; however, people with DPN may have different balance and plantar load distribution, which causes an increase in plantar pressure in some areas of the foot and damage to other areas, making them prone to injury [8].
According to the materials given, if treatment interventions targeted at preventing and alleviating the implications of DPN are not broadly adopted, the incidence of plantar ulcers is likely to rise. The American Diabetes Association (ADA) recommends wound reduction, proper education, self-management for foot care, medication, and nutritional therapies for patients to prevent diabetic foot problems and lower limb amputations. Furthermore, studies have demonstrated that neuro-musculoskeletal alterations produced by way of diabetes, which include deformity, muscle fatigue, limited range of motion, connective tissue stiffness, negative stability, and coordination may be healed or averted with exercise treatment [11].
Exercise therapy also allows patients to preserve as much residual biomechanical capacity as possible to interact safely with the ground while walking and standing, which may help prevent tissue degradation. For older populations, multicomponent exercise interventions, such as resistance, balance, and endurance training, as well as group and home-based exercise activities and Tai Chi, have so far shown beneficial effects on functional parameters and are the best strategies for the frail elderly, because they prevent the risk of falling and promote several physical health attributes, including balance, strength and cardiorespiratory fitness. They are also beneficial in improving the level of any bodily movement and living standards, as well as reducing the mortality rate [11-13].
One of the relevant exercises in this study is the foot and ankle exercise, which leads to enhancing the mechanical residences of the coccygeal tendon, reducing the fats in the foot muscle groups, increasing the isometric muscle energy of the toes and hallux, ankle extensor strength, range of movement of the ankle inside the sagittal plane, the conduction speed of the peroneal motor nerve and the sural sensory nerve, reducing sole numbness, dilating the peripheral microcirculatory vessels and changing the vascular features, better performance of sensory afferents and motor efferents, and somatosensory integration [14]. They can also adjust foot and ankle mechanics, and reduce pressure variations when walking, boost foot strength and performance, and minimize leg sensation loss, resulting in increased vibration perception and mobility of the foot and ankle joints [15, 16].
Other training protocols employed in this study included trampoline training or rebound therapy, a new training method that mechanically stimulates the neuromuscular system. Exercise on a rebounder has been demonstrated to improve elderly people’s balance control, and rehabilitation, and improve foot function in athletes with ankle instability, Parkinson disease, cerebral palsy, and stroke [17].
Bouncing on a rebounder subjects a person to different gravitational forces that enliven all body cells, including insulin receptors, and working muscles’ glucose uptake, and insulin resistance. Rebound therapy is related to a lower chance of musculoskeletal impairments as it reduces ground reaction forces, which puts no stress on weight-bearing joints, and equally distributes gravitational forces across all body parts.
There is evidence that standing and walking on a trampoline actively stretches the articular ligaments and muscle tendons of the ankles and toes and stretches the plantar fascia which leads to an increase in the degree of flexion and extension of the toes. Exercise on a flexible and elastic surface requires contraction of the muscles of the core, legs, and feet without causing complications in the sole, improves perception of sensations, and increases intraepidermal nerve fiber branches. Consequentially, foot ulcers can be avoided by lowering diabetic nerve damage symptoms such as numbness, discomfort, tingling, burning, and excessive plantar pressure, along with boosting foot and ankle strength [18-21].
The studies supporting the beneficial effects of foot workouts are of poor quality and ignore programs to strengthen the entire body, that is, the distal muscle group, which includes the extrinsic muscles of the ankle and the intrinsic muscles of the foot, as well as increasing flexibility. As a result, providing systematic therapeutic foot exercises that are focused on the main musculoskeletal abnormalities of the lower extremity and have a distinct focus from general exercises can complement traditional treatments for diabetic foot.
Accordingly, this study demonstrates if presenting appropriate solutions primarily based on healing techniques for DPN-related musculoskeletal abnormalities, together with self-care commands and domestic exercises (therapeutic ankle exercise and weight-bearing activities on a rebounder) can enhance the biomechanical factors and satisfaction of existence in patients suffering from peripheral neuropathy of the foot.
Materials and Methods
This was a clinical trial study. Women diagnosed with type 2 diabetes for a minimum 7 years accompanied by moderate or severe peripheral neuropathy for at least one year, with a 50- to 65-year-old average, who could walk independently, with decreased sensation in the leg that was previously diagnosed by a doctor, were eligible to take part in the study. The investigation was conducted in the Omid Novin Corrective Exercises Center (Tehran City, Iran, 2022), with volunteers drawn from patients who had been referred to the Parsian Clinic in Tehran.
The participants should not have a medical history of neurological or orthopedic illnesses (heart attack, stroke, poliomyelitis, rheumatoid arthritis, or severe osteoarthritis) that could mislead neuropathy evaluation, liver failure, kidney failure or dialysis, angina, embolism, cardiac arrhythmia, surgery, and other conditions that may cause neuropathy evaluation to be misled. Cardiac bypass, angioplasty, and amputation of a limb or part of a foot, current or previous foot ulcer, high or low blood pressure, visible reduction of the dorsalis pedis and tibialis posterior arteries diagnosed by the doctor.
Following the initial screening and meeting the eligibility criteria, 48 women with diabetes were randomly and equally divided into one control and two intervention groups using sealed envelopes with 16 patients per group. Measurements were made by a single-blinded assessor.
During the intervention period, all three groups received an instructional booklet containing foot exercises and foot care instructions, as well as recommendations regarding DPN complications by the medical team, including daily foot assessment, foot cleanliness, daily foot washing, and thorough drying. Using non-elastic and seamless socks, trimming the nails in a square shape, preventing unsupervised eradication of calluses or blisters, not wearing shoes or slippers without socks, and looking out for medical care if issues with the feet are discovered.
In the course of the trial, members in each of the three groups were no longer able to get hold of any other concurrent care, inclusive of physical therapy, acupuncture, or non-conventional clinical treatments. In cases where remedies were probably essential, the affected person ought to notify the researchers. Cramping, mild to extreme pain, exhaustion, dizziness, panic, or any other situation that exposed the patient to pain were all reasons for session discontinuation. During a meeting a few days before the start of the training protocol, the participants fulfilled the eligibility requirements, and were given a summary of the aims of the research, the benefits of participating in this study, and the steps of the trial. The consent form was filled out and signed by all of the participants, as well as the therapist. The demographic information of each person, including height, weight, age, body mass index, period span of diabetes and leg numbness, hemoglobin A1C, a questionnaire related to DPN symptoms, foot health and function, fall efficacy scale-international questionnaire, and basic symptoms, was then collected at the Center for Corrective Movements in Tehran before the exercise intervention.
Two measuring sessions were held to validate the results of the training methods. Before and after the exercise intervention, plantar pressure distribution and the risk of falling were assessed using a foot scanner, and functional reach test, respectively. Dynamic balance and QoL were also evaluated before the intervention and after the training intervention was completed. The participants were randomly distributed into two experimental groups and one control group. One of the interventional groups finished rebound activities, while the other completed an eight-week ankle-strengthening workout course at home.
Other than medications, self-care, and foot care advice from the educational booklet, the control group did not get any special intervention. All members of the control group received the foot exercises protocol if the intervention’s efficacy was demonstrated after the study.
Research instruments
The participants completed the Michigan neuropathy screening instrument (Brazilian version) to detect the existence of diabetic peripheral neuropathy. The mentioned questionnaire contains 15 questions about foot and leg sensitivity, with answers written by the participants. The answer “yes” to questions 1, 2, 3, 5, 8, 9, 11, 12, 14, 15, and “no” to questions 7 and 13 will result in a score of 1. Question 4 assesses the lack of blood circulation, while question 10 evaluates the general weakness and is excluded from the score. Total scores range from 0-13, with a score of 13 indicating severe DPN.
In our study, the foot health status questionnaire (Brazilian-Portuguese version) was used to indicate the participants’ foot health. Part I examines the following four aspects of foot health: Foot pain, footwear, foot function, and general foot health. Part II has multiple-choice questions with affirmative sentence possibilities, and the appropriate numbers are finally determined, part III gathers general demographic data. As the second part refers to general health, only the first part’s scores will be used in this study. Each part is scored from 0-100, with 100 being the ideal situation and 0 representing the most terrible [22, 23].
The QoL questionnaire was applied to evaluate the individuals’ health-related QoL. This questionnaire provides the evaluator with an index that reveals the individual’s health status. This questionnaire is based on a classification system that describes participant’s health in the following five dimensions: Mobility, non-medical care, routine activities, pain/discomfort, and anxiety/despair. Each aspect has three stages of severity, in which stage 1 shows no problems, stage 2 indicates mild to moderate problems, and stage 3 indicates intense problems. The QoL questionnaire produces values ranging from -0.59 to 1.00, indicating the patient’s health state (a score of 1 indicates perfect health) [24, 25].
The functional reach test and the falls efficacy scale-international were utilized to evaluate the existence and severity of balance impairment and fall risk. This questionnaire is scored on a scale of 1 to 10, with 1 indicating good self-confidence, 10 indicating low self-confidence, and a total score of 70 or above indicating that the person is scared of falling [26, 27].
In the functional reach test, the participant was instructed to stand next to, but touching the wall with bare feet, as the lateral area of the foot is perpendicular against the wall and both feet are parallel to each other in a comfortable position, while the shoulder flexion angle is 90 degrees, the elbow is extended and a closed fist. A paper meter parallel to the floor and aligned with the height of the patient’s acromion is attached to the wall.
The starting position is recorded where the third metacarpal head is on the tape. The participants are then asked to bend forward from their dominant side as far as they can without taking a step, losing balance, flexing the hip, or moving the feet forward. The displacement is measured on the tape meter. Three measurements will be taken and the average will be utilized for statistical analysis. The greater the displacement, the superior the functional balance [28].
To record and analyze plantar pressure, foot scan model 3 Body View (Made in America) was used. The participant was instructed to walk 3 times naturally and barefoot on the screen, and the mean value of three measured peak plantar pressures was used for data analysis. The plantar area was divided into five sections for assessment (under hallux, medial forefoot, lateral forefoot, midfoot, and heel) [29].
A dynamic balance device (made by Danesh Salar Iranian Co., Iran) was used to measure dynamic balance. This device contains two hardware pieces: A Certain part for the person’s standing and the other for displaying information related to maintaining balance). The movement of the participants in the frontal plane is in the lateral direction (medial-lateral) and according to the visual stimulus. This device has biofeedback and balance stability range adjustment.
The participants walk on the unstable plate of the balance structure and keep their balance using a handle in front of them. To maintain balance, they should progressively separate their hand from the support and never rely on it during the test. Their balance record will be reported at a specified time [30].
All the measurements were carried out by a single-blinded assessor along with a physiotherapist. The investigator who is responsible for all before and after intervention measurements is a PhD candidate in sports injury and corrective exercises at the University of Tehran (Kish International Campus, Kish, Iran).
Exercise protocols
The participants in the intervention groups received a training booklet in two parts. The first section contains instructional materials to guide people in changing their health behaviors around autonomous foot care, as well as information about diabetic neuropathy, footwear, and the advantages of foot and ankle activity. The second section contains training protocols.
The first conventional group practiced on a rebounder at home [29]. This training program was comprised of four levels of progression in which the intensity of the exercises expanded step by step by eliminating basic tasks and adding more complicated activities to the program over 8 weeks. The members were requested to execute each level of the training program for a minimum of two weeks (three times per week), with 10 repetitions of each exercise and holding the static exercises for up to 10 s.
The training program was carried out in three sets per day, with 5-min rest intervals between sets. The subjects were instructed to stretch the quadriceps, hamstrings, biceps, and soleus muscles for pre-exercise warm-up and cool-down, stretching every mentioned muscle three times for 20 s each time. Subjects were also required to put on appropriate shoes and examine their feet after the exercises. Cramping, moderate to severe aches, weariness, and dizziness that expose the participants to any uneasiness are the termination criteria for each session [29].
The second experimental group performed the ankle exercise-therapy program. The internal and exterior muscles of the foot and ankle were strengthened as part of this program [5]. There were six activities altogether: Four for the inner leg muscles and two for the outer leg and ankle muscles. Cotton balls, pencils, balls, and chairs were used in the exercises. The interphalangeal, metatarsophalangeal, and lower leg joints were the focus of this treatment protocol. This protocol targets the following muscle groups: The medial plantar side (abductor hallucis, flexor hallucis brevis, and adductor hallucis), lateral plantar side (abductor digiti minimi, flexor digiti minimi, and opponens digiti minimi), medial plantar side (flexor digitorum brevis), plantar interosseous muscles, lumbrical muscle, square plantar muscle, and dorsum interosseous muscles), and dorsum side (extensor hallucis brevis and extensor digitorum brevis). In one set of 30 repetitions, leg workouts were performed initially in a sitting position.
If the patients find an exercise too easy, they can perform it in standing and then standing on one leg position. The patients can also increase the number of exercises; upon completion, they fill out a table that displays the perceived effort for each exercise on a Likert scale. If the effort falls between 0 and 5, the person should proceed to the next exercise step (e.g. moving from sitting to standing or using a different object) during the next session. If the effort falls between 6 and 8, the training volume and intensity level should be maintained. On the off chance that the effort falls in the range of 9 and 10, the number of reiterations ought to be diminished or the activity pose changed (e.g. from a standing position to a sitting one). During 8 weeks, this program was followed 3 times a week, resulting in 24 sessions in total.
Statistical data analysis
The analysis of the covariance (ANCOVA) test allowed us to examine the effectiveness of rebounder and ankle exercise therapy interventions. The groups’ pre-test results were taken into account as covariance or control variables, and their impact was neutralized. The post hoc comparison test of Bonferroni was also utilized to analyze the post-test of all three groups. Each group’s average post-test and pre-test times were looked at independently utilizing a paired or paired t-test. The data were analyzed with SPSS software, version 27.
Results
The characteristics of the present research individuals including age, body mass index, height, weight, records of diabetes, period after a neuropathy diagnosis, and hemoglobin A1C are detailed in Table 1 (P>0.05).

In Table 2, the findings of covariance analysis were reported to evaluate and compare the effectiveness of mini-trampoline therapies and ankle exercise therapy on right foot pressure.

The analysis of covariance’s findings (Table 2) demonstrated that two mini-trampoline interventions and therapeutic exercises were statistically effective in reducing the peak pressure of the medial forefoot area and the peak pressure of the lateral forefoot area, respectively (P<0.05). Additionally, the paired t-test findings represented that there was a contrast between the pre-test and post-test averages in these two variables for the two intervention groups (P<0.05). None of the variable averages in the control group showed a statistically significant difference between pre-test and post-test (P>0.05). Exercise therapy and the mini-trampoline intervention were equally effective, according to the Bonferroni post hoc analysis (P>0.05).
The covariance analysis findings are presented in Table 3 to investigate and compare the efficacy of rebounder interventions and exercise therapy on left foot pressure.

Table 4 has provided the results of covariance analysis to investigate and compare the effectiveness of rebounder interventions and exercise therapy on the risk of falling variable.
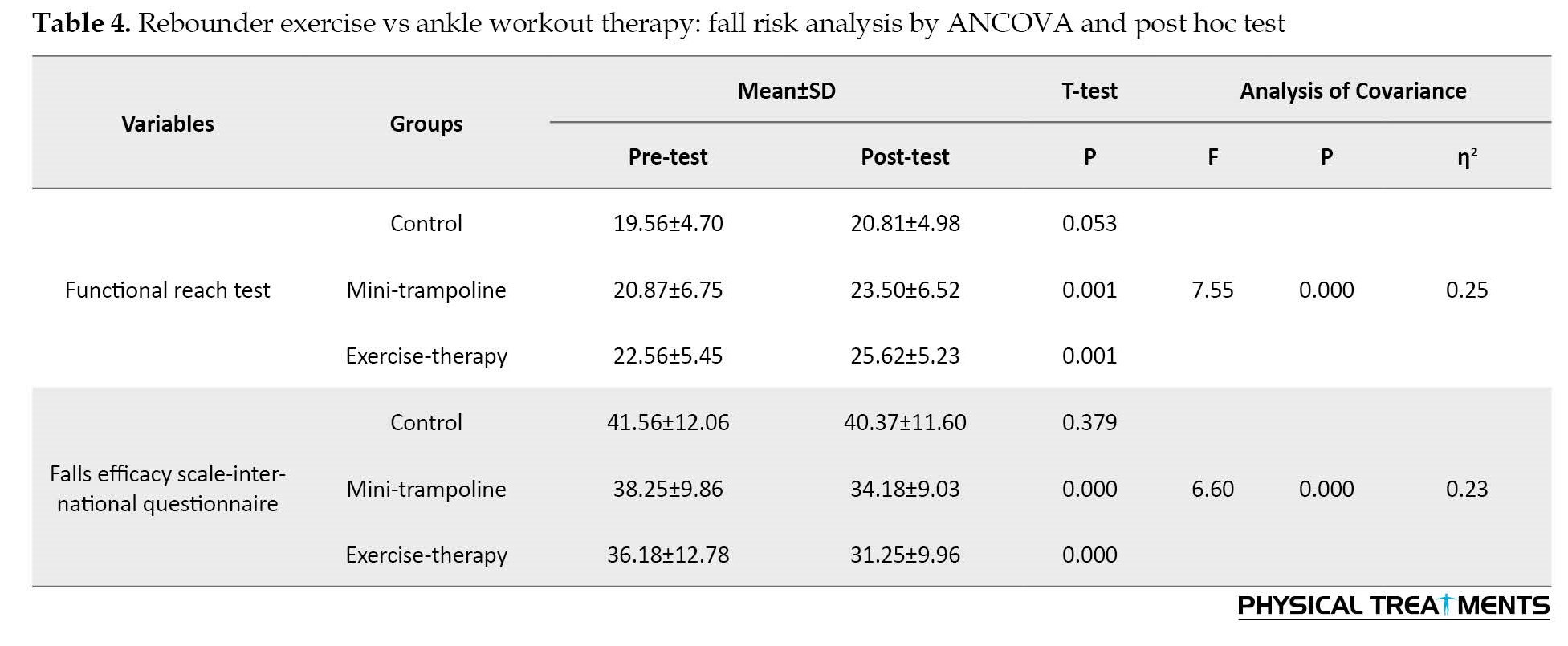
The analysis of covariance (Table 4) discovered that statistically at a confidence level of at least 95%, two mini-trampoline therapies, and therapeutic exercises were effective on fall risk variables, that is, the functional reach test and the fall questionnaire (P<0.05). Furthermore, the paired t-test findings revealed that there was a difference between the pre-test and post-test means in both variables in the two experimental groups (P<0.05). On the functional reach test and the fall questionnaire, the Bonferroni post hoc test results revealed no difference in effectiveness between the two intervention modalities (P<0.05).
The results of covariance analysis are reported in Table 5 to examine and compare the effectiveness of rebounder and exercise therapy interventions on dynamic balance.

The analysis of covariance results in Table 5 showed that two mini-trampoline therapies and therapeutic exercise significantly improved dynamic balance (P<0.05) with a confidence level of at least 95%. The paired t-test findings revealed a difference in the dynamic balance scale pre-test and post-test averages in the two intervention groups (P<0.05), but not in the control group (P>0.05). The post hoc Bonferroni test revealed that the therapeutic exercise approach was significantly more efficacious on dynamic balance than the mini-trampoline method (P<0.05).
hows the findings of a covariance analysis used to analyze and compare the effects of rebound therapies and exercise therapy on QoL.
The findings of the analysis of covariance (Table 6) revealed that two mini-trampoline and exercise therapy interventions significantly improved the quality of living (P<0.05) at a confidence level of at least 95%.

The paired t-test findings showed a difference between the pre-test and post-test means in the QoL score in the two intervention groups (P<0.05), but not in the control group (P>0.05). The post hoc Bonferroni test results found that the efficiency of the two treatment approaches on QoL was not statistically different (P<0.05).
Discussion
After eight weeks of performing weight-bearing exercises on a rebounder and the ankle exercise therapy program, the findings of the research showed that these two exercises in the experimental groups compared to the control group caused a significant enhancement in the two components of the peak pressure of the medial forefoot area and the peak pressure of the area lateral forefoot right and left foot, fall risk, dynamic balance and QoL.
The development of diabetic peripheral neuropathy impairs the integrity of tiny joints and internal muscles of the feet which are the main causes of deformity and high plantar pressures [5-10]. Improving the feeling of the soles of the feet and the perception of vibration is one of the changes that have been reported as a result of some exercise activities.
These results were consistent with the findings of Kankanasamut et al. [29], Sartor et al. [31], Fayed et al. [32], Cerrahoglu et al. [33], Jorgetto et al. [8], Jiang et al. [3], Prokai et al. [1], de Oliveira Lima et al. [34], and Monterio et al [10].
Kankanasamut et al. [29] demonstrated that eight weeks of weight-bearing exercises increases vibration perception. Sartor et al. [31] studied the effect of functional, strengthening, and stretching exercises on foot function in diabetic neuropathy patients. A change in the feet rocking motion during walking implies an improvement in plantar stress distribution and an improved functional state of the ankle.
Fayed et al. [32] investigated the effect of physical activity treatments on plantar pressure distribution in people with diabetic peripheral neuropathy, along with medicinal treatment, patients underwent physiotherapy interventions, such as stretching, strengthening, balance, and walking workouts. The outcomes supported that physiotherapy mediation may prohibit the development of ulcers in diabetic neuropathy patients, as evidenced by significant changes in pressure distribution, plantar peak, and foot contact area. Cerrahoglu et al. [33] instructed diabetic patients with and without neuropathy on ankle and foot workouts and communicated with patients weekly to promote program adherence.
These strategies suggest that a home activity plan can be an advantageous preventive approach for diabetic individuals to boost the range of motion in lower limb joints and lower peak pressure while walking. Tudpor et al. [35] studied the use of short-leg workouts to prevent falls in diabetic individuals.
Monterio et al. [10] showed that foot and ankle therapeutic exercises significantly improved brisk walking speed, ankle range of motion, and vibration perception. The interphalangeal, metatarsophalangeal, and ankle joints, and the muscle groups on the medial, lateral, dorsal, and median plantar side are the focus of the relevant exercise protocols in this research, which explains the findings and is consistent with the research previously mentioned which results in an improvement in the sagittal plane range of motion of the ankle, an increase in the mechanical properties of the coccygeal tendon, a decrease in fat in the leg muscles, an increase in the torque force, ankle extensor power, and the isometric muscle strength of the toes and hallux, as well as the redistribution of the plantar pressure during walking [5, 15, 16].
Patients suffering from DPN regularly experience increased postural and gait disturbances and are more likely to fall. Numerous problems, including neuromuscular issues of the foot, particularly the internal muscles of the foot, and weakening of the distal muscles, are responsible for such balance and walking disorders. In contrast with the control group, the consequences of the current study demonstrate a significant decrease in the risk of falling; the patients reported acting more easily and confidently as a result of completing the treatment program, indicating the psychological effects of the significant fall risk reduction.
The study’s findings are compared to those of the control group, and they are consistent with those of Tudpor et al. [35], who investigated how short-term leg exercises could reduce the chance of falling in diabetes patients. According to the findings, short leg exercises improve dynamic posture control and lessen muscular atrophy.
These explanations have been confirmed by de Oliveira Lima et al. [34] who have investigated the efficacy of physical activities on balance, fear of falling, and the risk of falling in patients with peripheral neuropathy and discovered that a mixture of activities, for instance, walking, balance, and functional training improves balance, fear of falling, and standard of living in DPN patients but not their risk of falling.
Prokai et al. [1] demonstrated that a 12-week exercise program on the sand, including strengthening, stretching, balance, and walking exercises is a safe and effective method for improving plantar flexion strength, ankle flexibility, and balance, which manifests in better walking performance in patients suffering from diabetic peripheral neuropathy.
When interpreting the results of this study and considering the results of the preceding literature, it is worth noting that the improvement in balance observed in the exercise group may be attributable to the lack of coordination between ankle muscles strength, resulting in a biomechanical imbalance which is corrected by ankle treatment exercises. Performing these particular exercises promotes the mobility of the foot-ankle complex and maximizes the strength of the foot and lower leg muscles which leads to the enhancement of plantar flexor muscle strength and the production of hip torque force, as well as balances the biomechanics of the ankle. As a result, increasing the information received from the lower limbs leads to maintaining more accurate control of the posture, better nerve feedback, and enhancement of balance and walking patterns. Therefore, strengthening muscles, achieving neuromuscular coordination through exercise, and properly summoning motor units after exercises all contribute to improving balance and lowering the risk of falling [22, 23].
Since all patients in the experimental groups were able to finish the intervention without injury or complaints, home exercises with a training manual can be utilized as an alternative treatment and part of self-care habits, because they may improve patient adherence to treatment and even reduce the waiting time in outpatient programs, alleviate the symptoms and severity of DPN, increase the functional status of the foot, attain functional balance and make useful biomechanical changes and prevent further complications in rehabilitation programs.
Conclusion
The current study showed that exercise on the rebounder and therapeutic ankle exercises that contribute to the reduction or alleviation of DPN-induced musculoskeletal and sensory deficits can be used as a program focused on integrating peripheral strengthening using segmental exercises for leg functionality to treat and prevent leg and foot functional problems in this populace, as well as to improve their independence in daily activities. Therefore, we urge researchers to conduct extra clinical studies to validate the efficacy of particular physical activities for ankle treatment. These studies’ findings may support the use of exercise therapy in the treatment and prevention of diabetes, particularly about the long-term consequences of neuropathy.
Study limitations and recommendations for future research
The study’s main flaws were the limited sample size and short-term follow-up on the physical activity program’s advantages. To determine their effect on DPN management, it is recommended that similar studies be carried out with a bigger sample size. More research in this field is advised given the dearth of studies evaluating the efficacy of exercise regimens like ankle therapeutics and mini-trampoline for the prevention and control of diabetes in women with peripheral neuropathy.
Ethical Considerations
Compliance with ethical guidelines
The Sport Sciences Research Institute’ Ethics Committee authorized all research methodologies and procedures based on ethical concerns (Code: IR.SSRI.REC 1400.1311). In addition, before beginning the research process, all participants in this study provided informed consent.
Funding
This paper is an extract from the PhD dissertation of Ashraf Ansari approved by Department of Sport Injury and Corrective Exercise, Kish Campus of University of Tehran.
Authors' contributions
Conceptualization, methodology, software, validation, formal analysis, investigation, resources, project administration, data curation and writing: Ashraf Ansari; Supervision: Mohammad Karimizadeh Ardakani and Mahdieh Akoochakian.
Conflict of interest
The authors declared no conflict of interest.
References
Currently, more than 500 million adults are living with diabetes worldwide, with nearly half of them suffering from various kinds of neuropathy [1-4]. In line with the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), diabetes implications are growing rapidly and diabetic peripheral neuropathy (DPN) is the maximum common microvascular consequence, influencing as much as 70% of sufferers from diabetes [5]. DPN is caused by hyperglycemia and decreased blood supply to peripheral nerves, which commonly affect the lower extremities [6, 7]; in addition, in advanced cases, it affects the upper limbs. Diabetes-related neuropathy is responsible for 40% to 70% of traumatic lower extremity amputations. Lower limb injuries account for about 20% of the causes of hospitalization in people with diabetes, and 85% are attributable to amputation of the lower limb in patients with diabetes before the development of a wound, the main factors associated with which are foot deformity and trauma. Sensorimotor neuropathy, one of DPN’s symptoms, causes a gradual loss of tactile sensation and pain sensitivity, often known as the loss of protective sensation of the feet, which makes the feet more vulnerable to damage and increases the risk of ulceration [8]. More than half of diabetic neuropathy patients experience severe pain that interferes with work and social activities. Furthermore, the psychosocial impacts of diabetic neuropathy impair a person’s quality of life (QoL) [9]. Diabetic neuropathy, which has a detrimental influence on postural balance, alterations in walking kinematics, and deficiencies in proprioception, raises the risk of falling, which is most closely associated with depressive symptoms in diabetic patients [1-3].
The progression of DPN causes biomechanical, sensory, and motor complications that result in diabetic foot problems, loss of overall foot function, an increased proportion of fat tissue in foot muscles, leg muscle dysfunction, such as reduced joint mobility, intrinsic foot muscle atrophy, distal muscle weakness, and a decrease in the mechanical properties of the calcaneal tendon [10].
These induce a loss of balance between the flexor and extensor muscles, resulting in joint abnormalities such as claw fingers, hammer toes, overlapping fingers, metatarsal head protrusion, and hallux valgus (b:union:). Such abnormalities result in pressure point changes in the soles of the feet, as well as overload and skin reactions with localized hyperkeratosis (callus), which escalates to sole ulcers with continued walking. Healthy people have a higher plantar pressure peak in the posterior area of the foot (up to 6 kg/cm2) in static conditions; however, people with DPN may have different balance and plantar load distribution, which causes an increase in plantar pressure in some areas of the foot and damage to other areas, making them prone to injury [8].
According to the materials given, if treatment interventions targeted at preventing and alleviating the implications of DPN are not broadly adopted, the incidence of plantar ulcers is likely to rise. The American Diabetes Association (ADA) recommends wound reduction, proper education, self-management for foot care, medication, and nutritional therapies for patients to prevent diabetic foot problems and lower limb amputations. Furthermore, studies have demonstrated that neuro-musculoskeletal alterations produced by way of diabetes, which include deformity, muscle fatigue, limited range of motion, connective tissue stiffness, negative stability, and coordination may be healed or averted with exercise treatment [11].
Exercise therapy also allows patients to preserve as much residual biomechanical capacity as possible to interact safely with the ground while walking and standing, which may help prevent tissue degradation. For older populations, multicomponent exercise interventions, such as resistance, balance, and endurance training, as well as group and home-based exercise activities and Tai Chi, have so far shown beneficial effects on functional parameters and are the best strategies for the frail elderly, because they prevent the risk of falling and promote several physical health attributes, including balance, strength and cardiorespiratory fitness. They are also beneficial in improving the level of any bodily movement and living standards, as well as reducing the mortality rate [11-13].
One of the relevant exercises in this study is the foot and ankle exercise, which leads to enhancing the mechanical residences of the coccygeal tendon, reducing the fats in the foot muscle groups, increasing the isometric muscle energy of the toes and hallux, ankle extensor strength, range of movement of the ankle inside the sagittal plane, the conduction speed of the peroneal motor nerve and the sural sensory nerve, reducing sole numbness, dilating the peripheral microcirculatory vessels and changing the vascular features, better performance of sensory afferents and motor efferents, and somatosensory integration [14]. They can also adjust foot and ankle mechanics, and reduce pressure variations when walking, boost foot strength and performance, and minimize leg sensation loss, resulting in increased vibration perception and mobility of the foot and ankle joints [15, 16].
Other training protocols employed in this study included trampoline training or rebound therapy, a new training method that mechanically stimulates the neuromuscular system. Exercise on a rebounder has been demonstrated to improve elderly people’s balance control, and rehabilitation, and improve foot function in athletes with ankle instability, Parkinson disease, cerebral palsy, and stroke [17].
Bouncing on a rebounder subjects a person to different gravitational forces that enliven all body cells, including insulin receptors, and working muscles’ glucose uptake, and insulin resistance. Rebound therapy is related to a lower chance of musculoskeletal impairments as it reduces ground reaction forces, which puts no stress on weight-bearing joints, and equally distributes gravitational forces across all body parts.
There is evidence that standing and walking on a trampoline actively stretches the articular ligaments and muscle tendons of the ankles and toes and stretches the plantar fascia which leads to an increase in the degree of flexion and extension of the toes. Exercise on a flexible and elastic surface requires contraction of the muscles of the core, legs, and feet without causing complications in the sole, improves perception of sensations, and increases intraepidermal nerve fiber branches. Consequentially, foot ulcers can be avoided by lowering diabetic nerve damage symptoms such as numbness, discomfort, tingling, burning, and excessive plantar pressure, along with boosting foot and ankle strength [18-21].
The studies supporting the beneficial effects of foot workouts are of poor quality and ignore programs to strengthen the entire body, that is, the distal muscle group, which includes the extrinsic muscles of the ankle and the intrinsic muscles of the foot, as well as increasing flexibility. As a result, providing systematic therapeutic foot exercises that are focused on the main musculoskeletal abnormalities of the lower extremity and have a distinct focus from general exercises can complement traditional treatments for diabetic foot.
Accordingly, this study demonstrates if presenting appropriate solutions primarily based on healing techniques for DPN-related musculoskeletal abnormalities, together with self-care commands and domestic exercises (therapeutic ankle exercise and weight-bearing activities on a rebounder) can enhance the biomechanical factors and satisfaction of existence in patients suffering from peripheral neuropathy of the foot.
Materials and Methods
This was a clinical trial study. Women diagnosed with type 2 diabetes for a minimum 7 years accompanied by moderate or severe peripheral neuropathy for at least one year, with a 50- to 65-year-old average, who could walk independently, with decreased sensation in the leg that was previously diagnosed by a doctor, were eligible to take part in the study. The investigation was conducted in the Omid Novin Corrective Exercises Center (Tehran City, Iran, 2022), with volunteers drawn from patients who had been referred to the Parsian Clinic in Tehran.
The participants should not have a medical history of neurological or orthopedic illnesses (heart attack, stroke, poliomyelitis, rheumatoid arthritis, or severe osteoarthritis) that could mislead neuropathy evaluation, liver failure, kidney failure or dialysis, angina, embolism, cardiac arrhythmia, surgery, and other conditions that may cause neuropathy evaluation to be misled. Cardiac bypass, angioplasty, and amputation of a limb or part of a foot, current or previous foot ulcer, high or low blood pressure, visible reduction of the dorsalis pedis and tibialis posterior arteries diagnosed by the doctor.
Following the initial screening and meeting the eligibility criteria, 48 women with diabetes were randomly and equally divided into one control and two intervention groups using sealed envelopes with 16 patients per group. Measurements were made by a single-blinded assessor.
During the intervention period, all three groups received an instructional booklet containing foot exercises and foot care instructions, as well as recommendations regarding DPN complications by the medical team, including daily foot assessment, foot cleanliness, daily foot washing, and thorough drying. Using non-elastic and seamless socks, trimming the nails in a square shape, preventing unsupervised eradication of calluses or blisters, not wearing shoes or slippers without socks, and looking out for medical care if issues with the feet are discovered.
In the course of the trial, members in each of the three groups were no longer able to get hold of any other concurrent care, inclusive of physical therapy, acupuncture, or non-conventional clinical treatments. In cases where remedies were probably essential, the affected person ought to notify the researchers. Cramping, mild to extreme pain, exhaustion, dizziness, panic, or any other situation that exposed the patient to pain were all reasons for session discontinuation. During a meeting a few days before the start of the training protocol, the participants fulfilled the eligibility requirements, and were given a summary of the aims of the research, the benefits of participating in this study, and the steps of the trial. The consent form was filled out and signed by all of the participants, as well as the therapist. The demographic information of each person, including height, weight, age, body mass index, period span of diabetes and leg numbness, hemoglobin A1C, a questionnaire related to DPN symptoms, foot health and function, fall efficacy scale-international questionnaire, and basic symptoms, was then collected at the Center for Corrective Movements in Tehran before the exercise intervention.
Two measuring sessions were held to validate the results of the training methods. Before and after the exercise intervention, plantar pressure distribution and the risk of falling were assessed using a foot scanner, and functional reach test, respectively. Dynamic balance and QoL were also evaluated before the intervention and after the training intervention was completed. The participants were randomly distributed into two experimental groups and one control group. One of the interventional groups finished rebound activities, while the other completed an eight-week ankle-strengthening workout course at home.
Other than medications, self-care, and foot care advice from the educational booklet, the control group did not get any special intervention. All members of the control group received the foot exercises protocol if the intervention’s efficacy was demonstrated after the study.
Research instruments
The participants completed the Michigan neuropathy screening instrument (Brazilian version) to detect the existence of diabetic peripheral neuropathy. The mentioned questionnaire contains 15 questions about foot and leg sensitivity, with answers written by the participants. The answer “yes” to questions 1, 2, 3, 5, 8, 9, 11, 12, 14, 15, and “no” to questions 7 and 13 will result in a score of 1. Question 4 assesses the lack of blood circulation, while question 10 evaluates the general weakness and is excluded from the score. Total scores range from 0-13, with a score of 13 indicating severe DPN.
In our study, the foot health status questionnaire (Brazilian-Portuguese version) was used to indicate the participants’ foot health. Part I examines the following four aspects of foot health: Foot pain, footwear, foot function, and general foot health. Part II has multiple-choice questions with affirmative sentence possibilities, and the appropriate numbers are finally determined, part III gathers general demographic data. As the second part refers to general health, only the first part’s scores will be used in this study. Each part is scored from 0-100, with 100 being the ideal situation and 0 representing the most terrible [22, 23].
The QoL questionnaire was applied to evaluate the individuals’ health-related QoL. This questionnaire provides the evaluator with an index that reveals the individual’s health status. This questionnaire is based on a classification system that describes participant’s health in the following five dimensions: Mobility, non-medical care, routine activities, pain/discomfort, and anxiety/despair. Each aspect has three stages of severity, in which stage 1 shows no problems, stage 2 indicates mild to moderate problems, and stage 3 indicates intense problems. The QoL questionnaire produces values ranging from -0.59 to 1.00, indicating the patient’s health state (a score of 1 indicates perfect health) [24, 25].
The functional reach test and the falls efficacy scale-international were utilized to evaluate the existence and severity of balance impairment and fall risk. This questionnaire is scored on a scale of 1 to 10, with 1 indicating good self-confidence, 10 indicating low self-confidence, and a total score of 70 or above indicating that the person is scared of falling [26, 27].
In the functional reach test, the participant was instructed to stand next to, but touching the wall with bare feet, as the lateral area of the foot is perpendicular against the wall and both feet are parallel to each other in a comfortable position, while the shoulder flexion angle is 90 degrees, the elbow is extended and a closed fist. A paper meter parallel to the floor and aligned with the height of the patient’s acromion is attached to the wall.
The starting position is recorded where the third metacarpal head is on the tape. The participants are then asked to bend forward from their dominant side as far as they can without taking a step, losing balance, flexing the hip, or moving the feet forward. The displacement is measured on the tape meter. Three measurements will be taken and the average will be utilized for statistical analysis. The greater the displacement, the superior the functional balance [28].
To record and analyze plantar pressure, foot scan model 3 Body View (Made in America) was used. The participant was instructed to walk 3 times naturally and barefoot on the screen, and the mean value of three measured peak plantar pressures was used for data analysis. The plantar area was divided into five sections for assessment (under hallux, medial forefoot, lateral forefoot, midfoot, and heel) [29].
A dynamic balance device (made by Danesh Salar Iranian Co., Iran) was used to measure dynamic balance. This device contains two hardware pieces: A Certain part for the person’s standing and the other for displaying information related to maintaining balance). The movement of the participants in the frontal plane is in the lateral direction (medial-lateral) and according to the visual stimulus. This device has biofeedback and balance stability range adjustment.
The participants walk on the unstable plate of the balance structure and keep their balance using a handle in front of them. To maintain balance, they should progressively separate their hand from the support and never rely on it during the test. Their balance record will be reported at a specified time [30].
All the measurements were carried out by a single-blinded assessor along with a physiotherapist. The investigator who is responsible for all before and after intervention measurements is a PhD candidate in sports injury and corrective exercises at the University of Tehran (Kish International Campus, Kish, Iran).
Exercise protocols
The participants in the intervention groups received a training booklet in two parts. The first section contains instructional materials to guide people in changing their health behaviors around autonomous foot care, as well as information about diabetic neuropathy, footwear, and the advantages of foot and ankle activity. The second section contains training protocols.
The first conventional group practiced on a rebounder at home [29]. This training program was comprised of four levels of progression in which the intensity of the exercises expanded step by step by eliminating basic tasks and adding more complicated activities to the program over 8 weeks. The members were requested to execute each level of the training program for a minimum of two weeks (three times per week), with 10 repetitions of each exercise and holding the static exercises for up to 10 s.
The training program was carried out in three sets per day, with 5-min rest intervals between sets. The subjects were instructed to stretch the quadriceps, hamstrings, biceps, and soleus muscles for pre-exercise warm-up and cool-down, stretching every mentioned muscle three times for 20 s each time. Subjects were also required to put on appropriate shoes and examine their feet after the exercises. Cramping, moderate to severe aches, weariness, and dizziness that expose the participants to any uneasiness are the termination criteria for each session [29].
The second experimental group performed the ankle exercise-therapy program. The internal and exterior muscles of the foot and ankle were strengthened as part of this program [5]. There were six activities altogether: Four for the inner leg muscles and two for the outer leg and ankle muscles. Cotton balls, pencils, balls, and chairs were used in the exercises. The interphalangeal, metatarsophalangeal, and lower leg joints were the focus of this treatment protocol. This protocol targets the following muscle groups: The medial plantar side (abductor hallucis, flexor hallucis brevis, and adductor hallucis), lateral plantar side (abductor digiti minimi, flexor digiti minimi, and opponens digiti minimi), medial plantar side (flexor digitorum brevis), plantar interosseous muscles, lumbrical muscle, square plantar muscle, and dorsum interosseous muscles), and dorsum side (extensor hallucis brevis and extensor digitorum brevis). In one set of 30 repetitions, leg workouts were performed initially in a sitting position.
If the patients find an exercise too easy, they can perform it in standing and then standing on one leg position. The patients can also increase the number of exercises; upon completion, they fill out a table that displays the perceived effort for each exercise on a Likert scale. If the effort falls between 0 and 5, the person should proceed to the next exercise step (e.g. moving from sitting to standing or using a different object) during the next session. If the effort falls between 6 and 8, the training volume and intensity level should be maintained. On the off chance that the effort falls in the range of 9 and 10, the number of reiterations ought to be diminished or the activity pose changed (e.g. from a standing position to a sitting one). During 8 weeks, this program was followed 3 times a week, resulting in 24 sessions in total.
Statistical data analysis
The analysis of the covariance (ANCOVA) test allowed us to examine the effectiveness of rebounder and ankle exercise therapy interventions. The groups’ pre-test results were taken into account as covariance or control variables, and their impact was neutralized. The post hoc comparison test of Bonferroni was also utilized to analyze the post-test of all three groups. Each group’s average post-test and pre-test times were looked at independently utilizing a paired or paired t-test. The data were analyzed with SPSS software, version 27.
Results
The characteristics of the present research individuals including age, body mass index, height, weight, records of diabetes, period after a neuropathy diagnosis, and hemoglobin A1C are detailed in Table 1 (P>0.05).

In Table 2, the findings of covariance analysis were reported to evaluate and compare the effectiveness of mini-trampoline therapies and ankle exercise therapy on right foot pressure.

The analysis of covariance’s findings (Table 2) demonstrated that two mini-trampoline interventions and therapeutic exercises were statistically effective in reducing the peak pressure of the medial forefoot area and the peak pressure of the lateral forefoot area, respectively (P<0.05). Additionally, the paired t-test findings represented that there was a contrast between the pre-test and post-test averages in these two variables for the two intervention groups (P<0.05). None of the variable averages in the control group showed a statistically significant difference between pre-test and post-test (P>0.05). Exercise therapy and the mini-trampoline intervention were equally effective, according to the Bonferroni post hoc analysis (P>0.05).
The covariance analysis findings are presented in Table 3 to investigate and compare the efficacy of rebounder interventions and exercise therapy on left foot pressure.

Table 4 has provided the results of covariance analysis to investigate and compare the effectiveness of rebounder interventions and exercise therapy on the risk of falling variable.
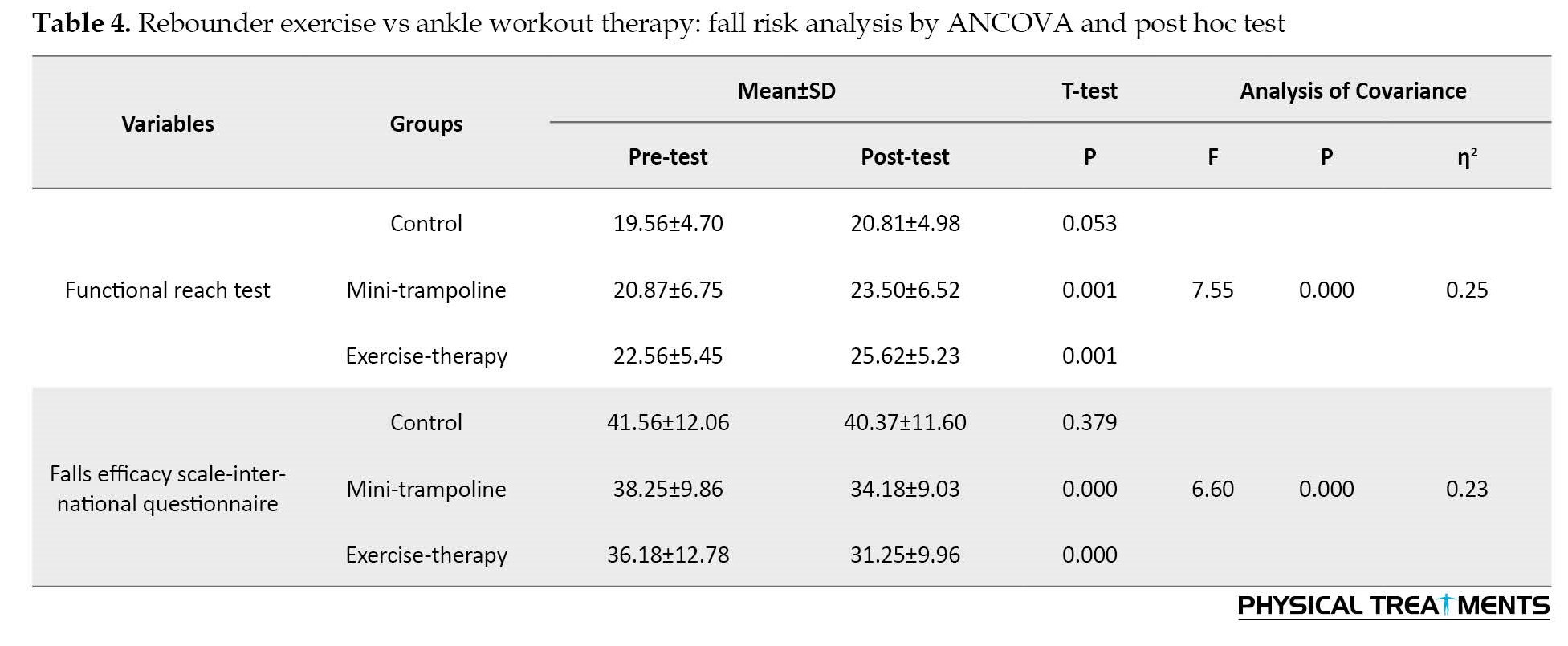
The analysis of covariance (Table 4) discovered that statistically at a confidence level of at least 95%, two mini-trampoline therapies, and therapeutic exercises were effective on fall risk variables, that is, the functional reach test and the fall questionnaire (P<0.05). Furthermore, the paired t-test findings revealed that there was a difference between the pre-test and post-test means in both variables in the two experimental groups (P<0.05). On the functional reach test and the fall questionnaire, the Bonferroni post hoc test results revealed no difference in effectiveness between the two intervention modalities (P<0.05).
The results of covariance analysis are reported in Table 5 to examine and compare the effectiveness of rebounder and exercise therapy interventions on dynamic balance.

The analysis of covariance results in Table 5 showed that two mini-trampoline therapies and therapeutic exercise significantly improved dynamic balance (P<0.05) with a confidence level of at least 95%. The paired t-test findings revealed a difference in the dynamic balance scale pre-test and post-test averages in the two intervention groups (P<0.05), but not in the control group (P>0.05). The post hoc Bonferroni test revealed that the therapeutic exercise approach was significantly more efficacious on dynamic balance than the mini-trampoline method (P<0.05).
hows the findings of a covariance analysis used to analyze and compare the effects of rebound therapies and exercise therapy on QoL.
The findings of the analysis of covariance (Table 6) revealed that two mini-trampoline and exercise therapy interventions significantly improved the quality of living (P<0.05) at a confidence level of at least 95%.

The paired t-test findings showed a difference between the pre-test and post-test means in the QoL score in the two intervention groups (P<0.05), but not in the control group (P>0.05). The post hoc Bonferroni test results found that the efficiency of the two treatment approaches on QoL was not statistically different (P<0.05).
Discussion
After eight weeks of performing weight-bearing exercises on a rebounder and the ankle exercise therapy program, the findings of the research showed that these two exercises in the experimental groups compared to the control group caused a significant enhancement in the two components of the peak pressure of the medial forefoot area and the peak pressure of the area lateral forefoot right and left foot, fall risk, dynamic balance and QoL.
The development of diabetic peripheral neuropathy impairs the integrity of tiny joints and internal muscles of the feet which are the main causes of deformity and high plantar pressures [5-10]. Improving the feeling of the soles of the feet and the perception of vibration is one of the changes that have been reported as a result of some exercise activities.
These results were consistent with the findings of Kankanasamut et al. [29], Sartor et al. [31], Fayed et al. [32], Cerrahoglu et al. [33], Jorgetto et al. [8], Jiang et al. [3], Prokai et al. [1], de Oliveira Lima et al. [34], and Monterio et al [10].
Kankanasamut et al. [29] demonstrated that eight weeks of weight-bearing exercises increases vibration perception. Sartor et al. [31] studied the effect of functional, strengthening, and stretching exercises on foot function in diabetic neuropathy patients. A change in the feet rocking motion during walking implies an improvement in plantar stress distribution and an improved functional state of the ankle.
Fayed et al. [32] investigated the effect of physical activity treatments on plantar pressure distribution in people with diabetic peripheral neuropathy, along with medicinal treatment, patients underwent physiotherapy interventions, such as stretching, strengthening, balance, and walking workouts. The outcomes supported that physiotherapy mediation may prohibit the development of ulcers in diabetic neuropathy patients, as evidenced by significant changes in pressure distribution, plantar peak, and foot contact area. Cerrahoglu et al. [33] instructed diabetic patients with and without neuropathy on ankle and foot workouts and communicated with patients weekly to promote program adherence.
These strategies suggest that a home activity plan can be an advantageous preventive approach for diabetic individuals to boost the range of motion in lower limb joints and lower peak pressure while walking. Tudpor et al. [35] studied the use of short-leg workouts to prevent falls in diabetic individuals.
Monterio et al. [10] showed that foot and ankle therapeutic exercises significantly improved brisk walking speed, ankle range of motion, and vibration perception. The interphalangeal, metatarsophalangeal, and ankle joints, and the muscle groups on the medial, lateral, dorsal, and median plantar side are the focus of the relevant exercise protocols in this research, which explains the findings and is consistent with the research previously mentioned which results in an improvement in the sagittal plane range of motion of the ankle, an increase in the mechanical properties of the coccygeal tendon, a decrease in fat in the leg muscles, an increase in the torque force, ankle extensor power, and the isometric muscle strength of the toes and hallux, as well as the redistribution of the plantar pressure during walking [5, 15, 16].
Patients suffering from DPN regularly experience increased postural and gait disturbances and are more likely to fall. Numerous problems, including neuromuscular issues of the foot, particularly the internal muscles of the foot, and weakening of the distal muscles, are responsible for such balance and walking disorders. In contrast with the control group, the consequences of the current study demonstrate a significant decrease in the risk of falling; the patients reported acting more easily and confidently as a result of completing the treatment program, indicating the psychological effects of the significant fall risk reduction.
The study’s findings are compared to those of the control group, and they are consistent with those of Tudpor et al. [35], who investigated how short-term leg exercises could reduce the chance of falling in diabetes patients. According to the findings, short leg exercises improve dynamic posture control and lessen muscular atrophy.
These explanations have been confirmed by de Oliveira Lima et al. [34] who have investigated the efficacy of physical activities on balance, fear of falling, and the risk of falling in patients with peripheral neuropathy and discovered that a mixture of activities, for instance, walking, balance, and functional training improves balance, fear of falling, and standard of living in DPN patients but not their risk of falling.
Prokai et al. [1] demonstrated that a 12-week exercise program on the sand, including strengthening, stretching, balance, and walking exercises is a safe and effective method for improving plantar flexion strength, ankle flexibility, and balance, which manifests in better walking performance in patients suffering from diabetic peripheral neuropathy.
When interpreting the results of this study and considering the results of the preceding literature, it is worth noting that the improvement in balance observed in the exercise group may be attributable to the lack of coordination between ankle muscles strength, resulting in a biomechanical imbalance which is corrected by ankle treatment exercises. Performing these particular exercises promotes the mobility of the foot-ankle complex and maximizes the strength of the foot and lower leg muscles which leads to the enhancement of plantar flexor muscle strength and the production of hip torque force, as well as balances the biomechanics of the ankle. As a result, increasing the information received from the lower limbs leads to maintaining more accurate control of the posture, better nerve feedback, and enhancement of balance and walking patterns. Therefore, strengthening muscles, achieving neuromuscular coordination through exercise, and properly summoning motor units after exercises all contribute to improving balance and lowering the risk of falling [22, 23].
Since all patients in the experimental groups were able to finish the intervention without injury or complaints, home exercises with a training manual can be utilized as an alternative treatment and part of self-care habits, because they may improve patient adherence to treatment and even reduce the waiting time in outpatient programs, alleviate the symptoms and severity of DPN, increase the functional status of the foot, attain functional balance and make useful biomechanical changes and prevent further complications in rehabilitation programs.
Conclusion
The current study showed that exercise on the rebounder and therapeutic ankle exercises that contribute to the reduction or alleviation of DPN-induced musculoskeletal and sensory deficits can be used as a program focused on integrating peripheral strengthening using segmental exercises for leg functionality to treat and prevent leg and foot functional problems in this populace, as well as to improve their independence in daily activities. Therefore, we urge researchers to conduct extra clinical studies to validate the efficacy of particular physical activities for ankle treatment. These studies’ findings may support the use of exercise therapy in the treatment and prevention of diabetes, particularly about the long-term consequences of neuropathy.
Study limitations and recommendations for future research
The study’s main flaws were the limited sample size and short-term follow-up on the physical activity program’s advantages. To determine their effect on DPN management, it is recommended that similar studies be carried out with a bigger sample size. More research in this field is advised given the dearth of studies evaluating the efficacy of exercise regimens like ankle therapeutics and mini-trampoline for the prevention and control of diabetes in women with peripheral neuropathy.
Ethical Considerations
Compliance with ethical guidelines
The Sport Sciences Research Institute’ Ethics Committee authorized all research methodologies and procedures based on ethical concerns (Code: IR.SSRI.REC 1400.1311). In addition, before beginning the research process, all participants in this study provided informed consent.
Funding
This paper is an extract from the PhD dissertation of Ashraf Ansari approved by Department of Sport Injury and Corrective Exercise, Kish Campus of University of Tehran.
Authors' contributions
Conceptualization, methodology, software, validation, formal analysis, investigation, resources, project administration, data curation and writing: Ashraf Ansari; Supervision: Mohammad Karimizadeh Ardakani and Mahdieh Akoochakian.
Conflict of interest
The authors declared no conflict of interest.
References
- Prókai J, Murlasits Z, Bánhidi M, Csóka L, Gréci V, Atlasz T, et al., The effects of a 12-week-long sand exercise training program on neuromechanical and functional parameters in type II Diabetic patients with neuropathy. International Journal of Environmental Research and Public Health. 2023; 20(7):5413. [DOI:10.3390/ijerph20075413] [PMID]
- Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Research and Clinical Practice. 2022; 183:109119. [DOI:10.1016/j.diabres.2021.109119] [PMID]
- Jiang X, Deng F, Rui S, Ma Y, Wang M, Deng B, et al. The evaluation of gait and balance for patients with early diabetic peripheral neuropathy: A cross-sectional study. Risk Management and Healthcare Policy. 2022; 15:543-52. [DOI:10.2147/RMHP.S361698] [PMID]
- Kocak MZ, Aktas G, Erkus E, Yis OM, Duman TT, Atak BM, et al. Neuregulin-4 is associated with plasma glucose and increased risk of type 2 diabetes mellitus. Swiss Medical Weekly. 2019; 149:w20139. [DOI:10.4414/smw.2019.20139] [PMID]
- Silva EQ, Suda EY, Santos DP, Veríssimo JL, Ferreira JSSP, Cruvinel Júnior RH, et al. Effect of an educational booklet for prevention and treatment of foot musculoskeletal dysfunctions in people with diabetic neuropathy: The FOotCAre (FOCA) trial II, a study protocol of a randomized controlled trial. Trials. 2020; 21(1):180. [DOI:10.1186/s13063-020-4115-8] [PMID]
- Ali M, Anwar S, Perveen W, Akhtar M, Hashmi R, Jabeen Z. Effects of neurodynamic exercises on the management of diabetic peripheral neuropathy of the upper limb: A case series. Physiotherapy Quarterly. 2023; 31(3):53-6. [DOI:10.5114/pq.2021.111834]
- Kanaley JA, Colberg SR, Corcoran MH, Malin SK, Rodriguez NR, Crespo CJ, et al. Exercise/physical activity in individuals with type 2 diabetes: A consensus statement from the American College of Sports Medicine. Medicine and Science in Sports and Exercise. 2022; 54(2):353-68. [DOI:10.1249/MSS.0000000000002800] [PMID]
- Jorgetto JV, DdS O, Gamba MA, Kusahara DM. Biomechanical profile of people with diabetic neuropathy attended in primary care in East Paulista, Brazil. Research Square. 2021.[DOI:10.21203/rs.3.rs-203954/v1]
- Preston FG, Riley DR, Azmi S, Alam U. Painful diabetic peripheral neuropathy: Practical guidance and challenges for clinical management. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy. 2023; 16:1595-612. [DOI:10.2147/DMSO.S370050] [PMID]
- Monteiro RL, Ferreira JSSP, Silva ÉQ, Cruvinel-Júnior RH, Veríssimo JL, Bus SA, et al. Foot-ankle therapeutic exercise program can improve gait speed in people with diabetic neuropathy: A randomized controlled trial. Scientific Reports. 2022; 12(1):7561. [DOI:10.1038/s41598-022-11745-0] [PMID]
- Hernando-Garijo I, Medrano-de-la-Fuente R, Mingo-Gómez MT, Lahuerta Martín S, Ceballos-Laita L, Jiménez-Del-Barrio S. Effects of exercise therapy on diabetic neuropathy: A systematic review and meta-analysis. Physiotherapy Theory and Practice. 2023; 21:1-14. [DOI:10.1080/09593985.2023.2227975] [PMID]
- Holmes CJ, Hastings MK. The application of exercise training for diabetic peripheral neuropathy. Journal of clinical Medicine. 2021; 10(21):5042. [DOI:10.3390/jcm10215042] [PMID]
- Streckmann F, Balke M, Cavaletti G, Toscanelli A, Bloch W, Décard BF, et al. Exercise and neuropathy: Systematic review with meta-analysis. Sports Medicine. 2022; 52(5):1043-65. [DOI:10.1007/s40279-021-01596-6] [PMID]
- AlKhotani RY, Al-Dubai SA, Almeshaly MS, Alautabi AS, Maqulah SF, AlGhamdi ZJ, et al. The association between physical activity and peripheral neuropathy in diabetic patients: A cross-sectional multicenter study from Saudi Arabia. Cureus. 2023; 15(2):e34504. [DOI:10.7759/cureus.34504]
- Monteiro RL, Ferreira JSSP, Silva ÉQ, Donini A, Cruvinel-Júnior RH, Verissímo JL, et al. Feasibility and preliminary efficacy of a foot-ankle exercise program aiming to improve foot-ankle functionality and gait biomechanics in people with diabetic neuropathy: A randomized controlled trial. Sensors (Basel). 2020; 20(18):5129. [DOI:10.3390/s20185129] [PMID]
- Silva ÉQ, Veríssimo JL, Ferreira JS, Cruvinel-Júnior RH, Monteiro RL, Suda EY, et al. Effects of a home-based foot–ankle exercise program with educational booklet for foot dysfunctions in people with diabetic neuropathy: Results of the FOCA-II randomized controlled clinical trial. Applied Sciences. 2023; 13(3):1423. [DOI:10.3390/app13031423]
- Miklitsch C, Krewer C, Freivogel S, Steube D. Effects of a predefined mini-trampoline training programme on balance, mobility and activities of daily living after stroke: A randomized controlled pilot study. Clinical Rehabilitation. 2013; 27(10):939-47. [DOI:10.1177/0269215513485591] [PMID]
- Sadeghi M, Ghasemi G, Karimi M. Effect of 12-week rebound therapy exercise on static stability of patients with spinal cord injury. Journal of Sport Rehabilitation. 2019; 28(5):464-7. [DOI:10.1123/jsr.2017-0303] [PMID]
- Giagazoglou P, Kokaridas D, Sidiropoulou M, Patsiaouras A, Karra C, Neofotistou K. Effects of a trampoline exercise intervention on motor performance and balance ability of children with intellectual disabilities. Research in Developmental Disabilities. 2013; 34(9):2701-7. [DOI:10.1016/j.ridd.2013.05.034] [PMID]
- Justina OA, Petronilla OC, Ikenna UC, Nneka IC, Gloria MU. Effects of rebound exercises on overweight and obese adults: A scoping review. Archives of Physiotherapy & Global Researches. 2021; 25(1): 7-16. [Link]
- Nuhu JM, Maharaj SS. Influence of a mini-trampoline rebound exercise program on insulin resistance, lipid profile and central obesity in individuals with type 2 diabetes. The Journal of Sports Medicine and Physical Fitness. 2017; 58(4):503-9. [DOI:10.23736/S0022-4707.17.07120-1] [PMID]
- Ferreira JSSP, Cruvinel Junior RH, Silva EQ, Veríssimo JL, Monteiro RL, Pereira DS, et al. Study protocol for a randomized controlled trial on the effect of the Diabetic Foot Guidance System (SOPeD) for the prevention and treatment of foot musculoskeletal dysfunctions in people with diabetic neuropathy: The FOotCAre (FOCA) trial I. Trials. 2020; 21(1):73. [DOI:10.1186/s13063-019-4017-9] [PMID]
- Monteiro RL, Sartor CD, Ferreira JSSP, Dantas MGB, Bus SA, Sacco ICN. Protocol for evaluating the effects of a foot-ankle therapeutic exercise program on daily activity, foot-ankle functionality, and biomechanics in people with diabetic polyneuropathy: A randomized controlled trial. BMC Musculoskeletal Disorders. 2018; 19(1):400. [DOI:10.1186/s12891-018-2323-0] [PMID]
- Safieddine M, Bruneau L, Soulaimana I, Debussche X, Lafarge S, Falissard B, et al. Quality of life assessment in diabetic patients: Validity of the creole version of the EQ-5D-5L in Re::union: Island. Frontiers in Psychology. 2023; 14:1185316. [DOI:10.3389/fpsyg.2023.1185316] [PMID]
- Xu RH, Wong EL, Cheung AW. Estimation of minimally important difference of the EQ-5D-5L utility scores among patients with either hypertension or diabetes or both: A cross-sectional study in Hong Kong. BMJ Open. 2020; 10(11):e039397. [DOI:10.1136/bmjopen-2020-039397] [PMID]
- Alasmari RS, Hassani HA, Almalky NA, Bokhari AF, Al Zahrani A, Hafez AA. Risk factors for fall among the elderly with diabetes mellitus type 2 in Jeddah, Saudi Arabia, 2022: A cross-sectional study. Annals of Medicine and Surgery. 2023; 85(3):412-7. [DOI:10.1097/MS9.0000000000000269] [PMID]
- Aslibeigi F, Zarrinkoob H, Erfanifar A, Akbarzadeh Baghban A, Denak F. Fear of falling and balance confidence in older adults with type 2 diabetes. Auditory and Vestibular Research. 2022; 31(4): 31(4):319-26. [DOI: 10.18502/avr.v31i4.10737]
- Pires IM, Garcia NM, Zdravevski E. Measurement of results of functional reach test with sensors: A systematic review. Electronics. 2020; 9(7):1078. [DOI:10.3390/electronics9071078]
- Kanchanasamut W, Pensri P. Effects of weight-bearing exercise on a mini-trampoline on foot mobility, plantar pressure and sensation of diabetic neuropathic feet; a preliminary study. Diabetic Foot & Ankle. 2017; 8(1):1287239. [DOI:10.1080/2000625X.2017.1287239] [PMID]
- Fattahi A, Zehtab Asghari H, Koreili Z. [A comparative study of Plantar Arch Index, weight distribution, equilibrium performance, and selected musculoskeletal disorders in active and non-active adolescences (Persian)]. Journal of Sport Biomechanics. 2020; 6(3):154-69. [Link]
- Sartor CD, Hasue RH, Cacciari LP, Butugan MK, Watari R, Pássaro AC, et al. Effects of strengthening, stretching and functional training on foot function in patients with diabetic neuropathy: Results of a randomized controlled trial. BMC Musculoskeletal Disorders. 2014; 15:137. [DOI:10.1186/1471-2474-15-137] [PMID]
- Fayed EE, Badr NM, Ismail S, Hakim SA. Exercise therapy improves planter pressure distribution in patients with diabetic peripheral neuropathy. International Journal of PharmTech Research. 2016; 9(5):151-9. [Link]
- Cerrahoglu L, Koşan U, Sirin TC, Ulusoy A. Range of motion and plantar pressure evaluation for the effects of self-care foot exercises on diabetic patients with and without neuropathy. Journal of the American Podiatric Medical Association. 2016; 106(3):189-200. [DOI:10.7547/14-095] [PMID]
- de Oliveira Lima RA, Piemonte GA, Nogueira CR, Dos Santos Nunes-Nogueira V. Efficacy of exercise on balance, fear of falling, and risk of falls in patients with diabetic peripheral neuropathy: A systematic review and meta-analysis. Archives of Endocrinology and Metabolism. 2021; 65(2):198-211. [PMID]
- Tudpor K, Traithip W. Fall prevention by short-foot exercise in diabetic patients. Indian Journal of Physiotherapy and Occupational Therapy - An International Journal. 2019; 13(2):69-74. [DOI:10.5958/0973-5674.2019.00048.0]
Type of Study: Research |
Subject:
Special
Received: 2023/09/3 | Accepted: 2024/01/30 | Published: 2024/04/1
Received: 2023/09/3 | Accepted: 2024/01/30 | Published: 2024/04/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






