Fri, Nov 7, 2025
Volume 14, Issue 1 (Winter 2024)
PTJ 2024, 14(1): 1-10 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Parvaneh Sarand A, Norasteh A A. Return to Sport After Shoulder Arthroplasty: A Systematic Review. PTJ 2024; 14 (1) :1-10
URL: http://ptj.uswr.ac.ir/article-1-596-en.html
URL: http://ptj.uswr.ac.ir/article-1-596-en.html
1- Department of Physiotherapy, Faculty of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of Sports Injury and Corrective Exercise, Faculty of Physical Education & Sport Sciences, University of Guilan, Rasht, Iran.
2- Department of Sports Injury and Corrective Exercise, Faculty of Physical Education & Sport Sciences, University of Guilan, Rasht, Iran.
Full-Text [PDF 592 kb]
(1142 Downloads)
| Abstract (HTML) (2435 Views)
Full-Text: (872 Views)
Introduction
Over the past few decades, shoulder arthroplasty has become a reliable and successful treatment for end-stage glenohumeral arthritis and post-traumatic sequelae [1, 2, 3] to relieve pain and restore mobility to the joint [3, 4]. The number of individuals opting for shoulder arthroplasty is on the rise, thanks to the development of more sophisticated implants and surgical techniques [5]. As life expectancy continues to increase, many elderly people are looking to maintain an active lifestyle, even after undergoing shoulder arthroplasty, to enjoy a higher quality of life [5]. However, engaging in sports or intense physical activity after arthroplasty carries certain risks, such as dislocation, polyethylene wear, and loosening of the implants [6].
Some different kinds of arthroplasty include reversed shoulder arthroplasty (RSA) [7], reversed total shoulder arthroplasty (RTSA) [8], total shoulder arthroplasty (TSA) [9], shoulder hemiarthroplasty (HSA) [10], humeral hemiarthroplasty (HHA) [11], humeral head resurfacing (HHR) [12] with biologic or prosthetic glenoid resurfacing (TSR) [12]. Increased shoulder arthroplasty was used for different diseases, such as osteoarthritis (OA), post-traumatic arthritis, inflammatory arthritis, osteonecrosis, rotator cuff dysfunction, and comminuted fractures [13].
The significance of participating in sports after shoulder arthroplasty has increased due to a heightened focus on physical fitness, making it more clinically relevant [13]. An increasing segment of the aging population, undergoing joint replacement surgery, expresses interest in sports and physical activities. If joint arthroplasty is required, their participation in sports activities may be limited. After different joint arthroplasties, previous studies have shown a return to sport (RTS) [14-22]. Since shoulder arthroplasty is a successful treatment, more attention has been paid to the patient’s aim of RTS [3, 10]. A common inquiry among patients undergoing shoulder arthroplasty is whether they can resume their pre-surgery activities, including questions about the types of sports or work they can expect post-procedure [3, 10].
The patient questionnaire consisted of closed-ended questions, prompting participants to express their agreement with the surgeon’s evaluation of their operated shoulder by marking a circle. This approach resulted in high levels of agreement with the surgeon’s assessment [23]. The assessment incorporated a 0-10 pain scale (0 indicating no pain and 10 indicating severe pain). Participants reported their current pain medication usage, categorized as none, over-the-counter, narcotic, or a combination of over-the-counter and narcotic. The range of motion was evaluated through a diagram, specifying forward flexion in degrees, external rotation in degrees, and internal rotation on a scale of 1-8. Strength was measured on a 10-point scale, ranging from 0 (complete paralysis) to 10 (normal strength) [23]. Lastly, RTS criteria are mostly evaluated quantitatively by the physical activity and sport-related questionnaires [4, 7-10, 13, 24-35]. However, much research is needed to complete the information in this field.
Given the significance of RTS, this study was conducted to thoroughly review the RTS outcomes following shoulder arthroplasty.
Materials and Methods
This is a systematic review based on guidelines for preferred reporting items.
Search strategy
This review thoroughly examines RTS following shoulder arthroplasty. It involves searching databases, such as Web of Science, PEDRO, Google Scholar, PubMed, SCOPUS, and CINAHL using two sets of keyword groups, (group 1) “return to sport” or “return to play” or “return to competition” or “return to physical activity”; and (group 2) “shoulder arthroplasty” or “shoulder replacement”. The two sets of combinations were investigated in the title, abstract, and keywords of studies published in journals indexed in the databases, covering the period from January 2000 to May 2023. Additionally, a manual search and a comprehensive review of article sources were conducted to identify articles that may not have been captured through electronic searches.
Eligibility criteria
The inclusion criteria included individuals, including athletes, who underwent various types of shoulder arthroplasty for reasons, such as rotator cuff tear, arthropathy, inflammation, glenohumeral OA, inflammatory OA, and fracture. Other criteria included a history of sports participation, a follow-up duration of >1 year, age >65 years, English-language articles, and the inclusion of full-text studies with cross-sectional and cohort designs.
The exclusion criteria included non-English articles, follow-up durations of <1 year, age <65 years, revision surgery cases, unwilling or deceased patients, those lacking a history of sports participation, individuals unreachable after multiple telephone calls, those diagnosed with fracture sequelae or other shoulder injuries, such as fractures of the proximal humerus, and articles briefly published in congresses and seminars.
Study selection
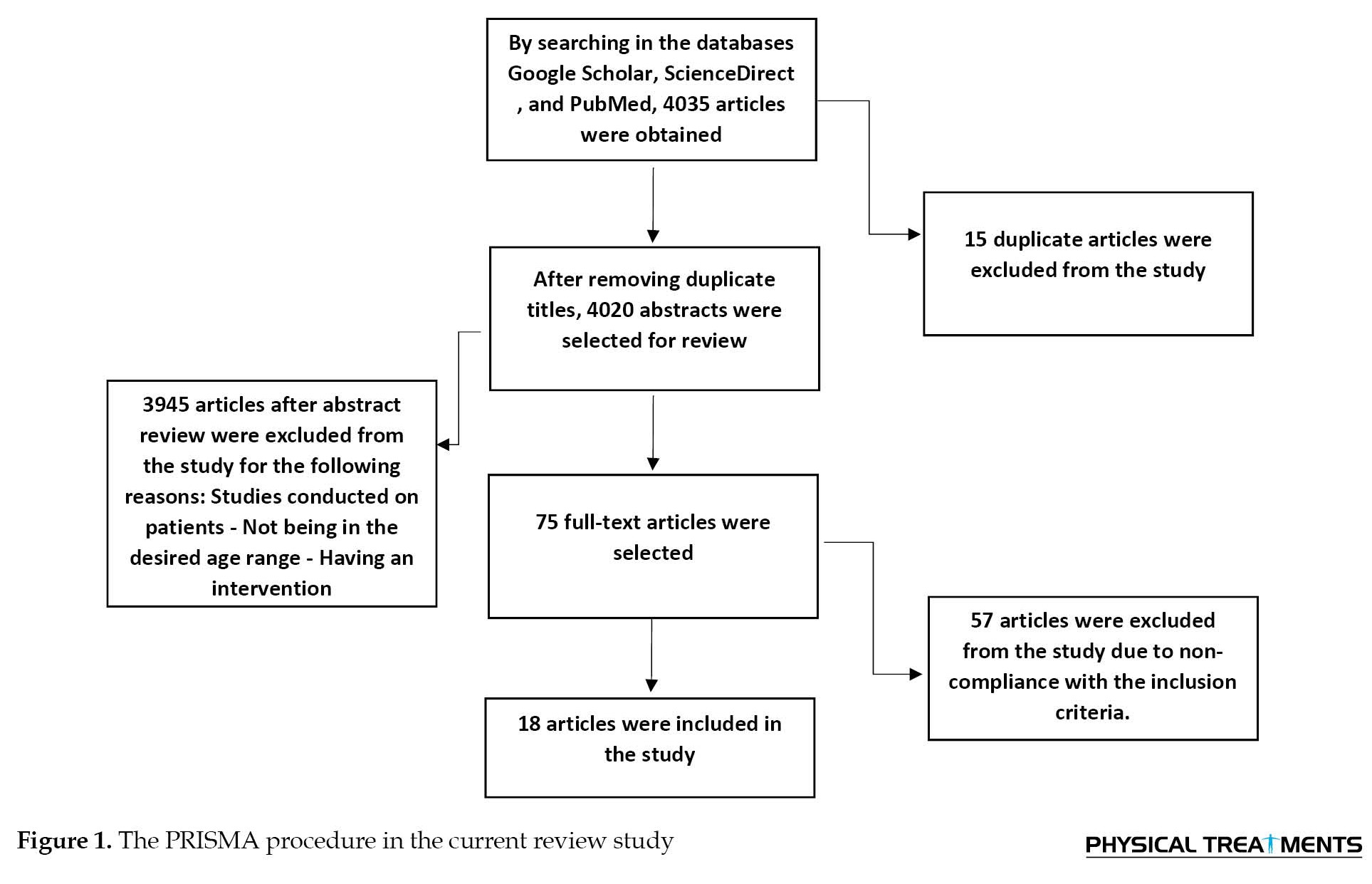
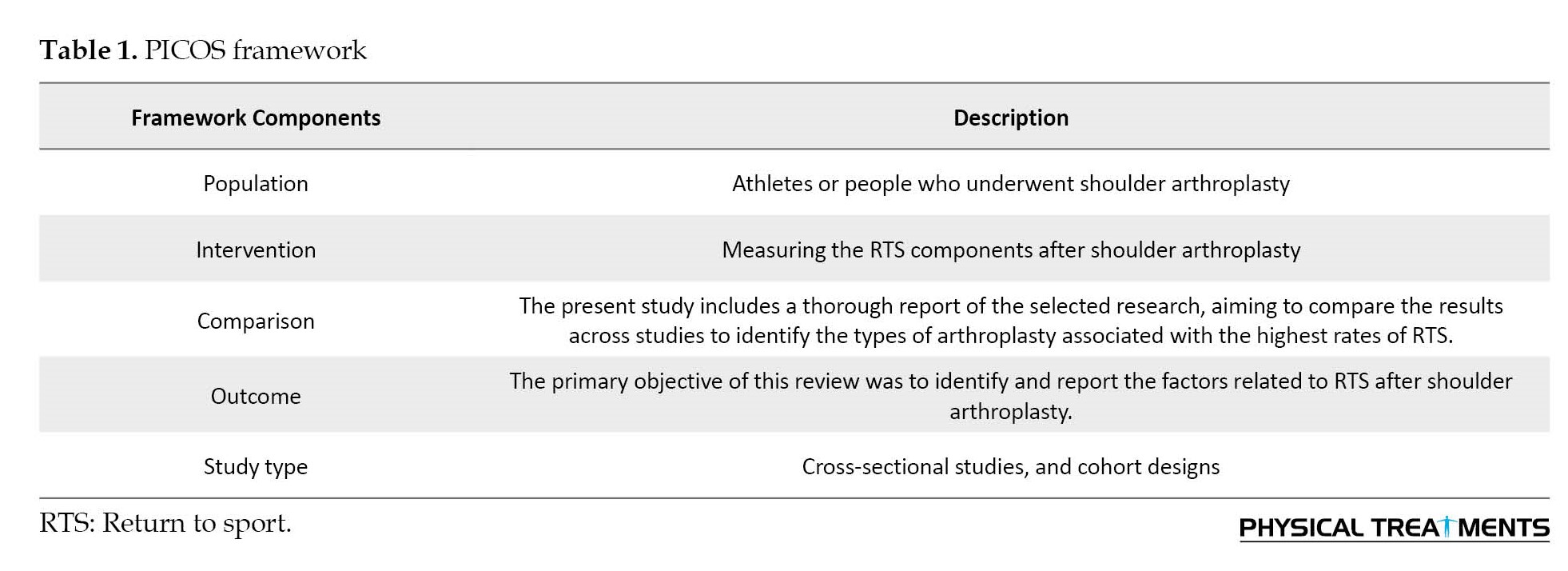
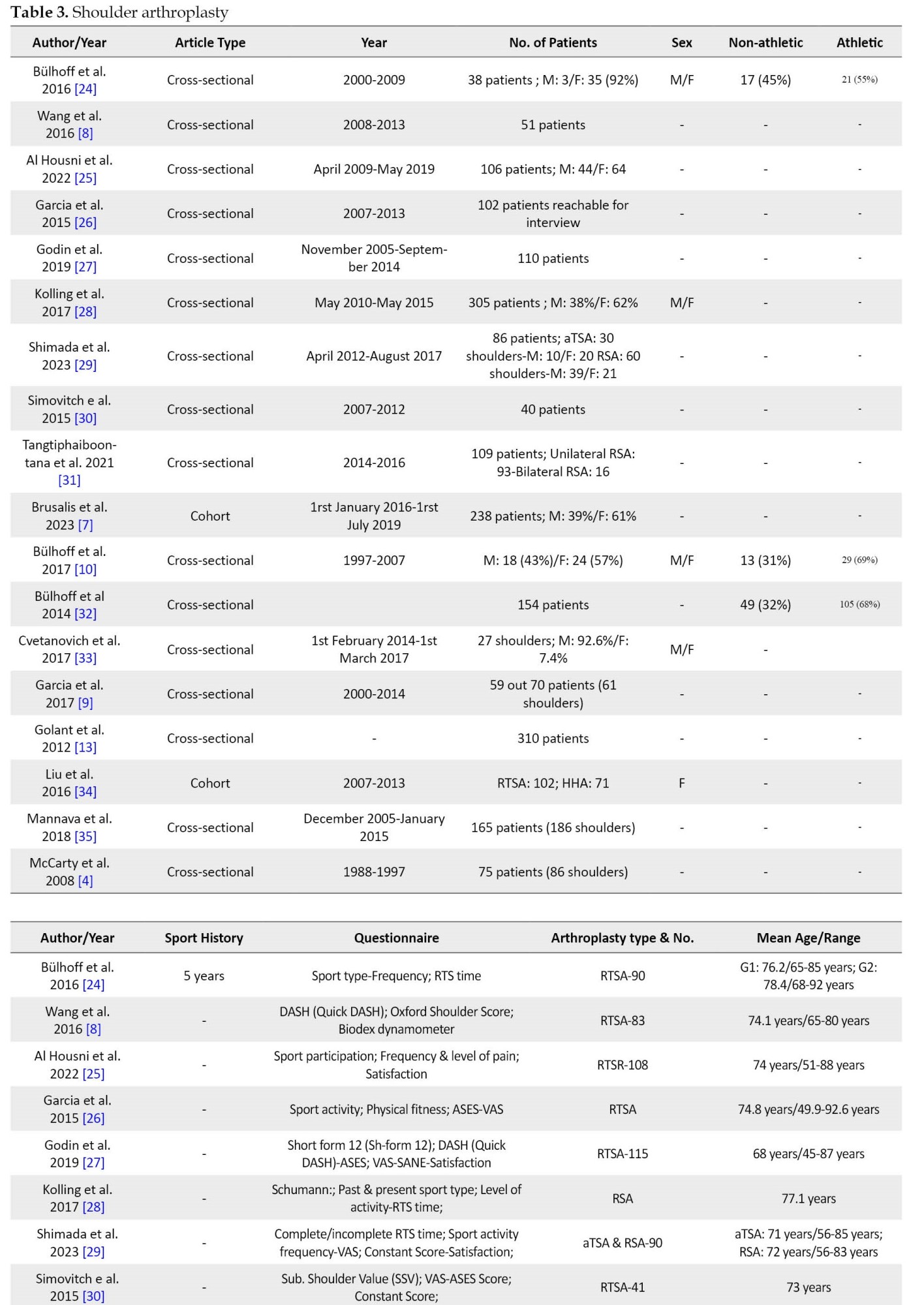
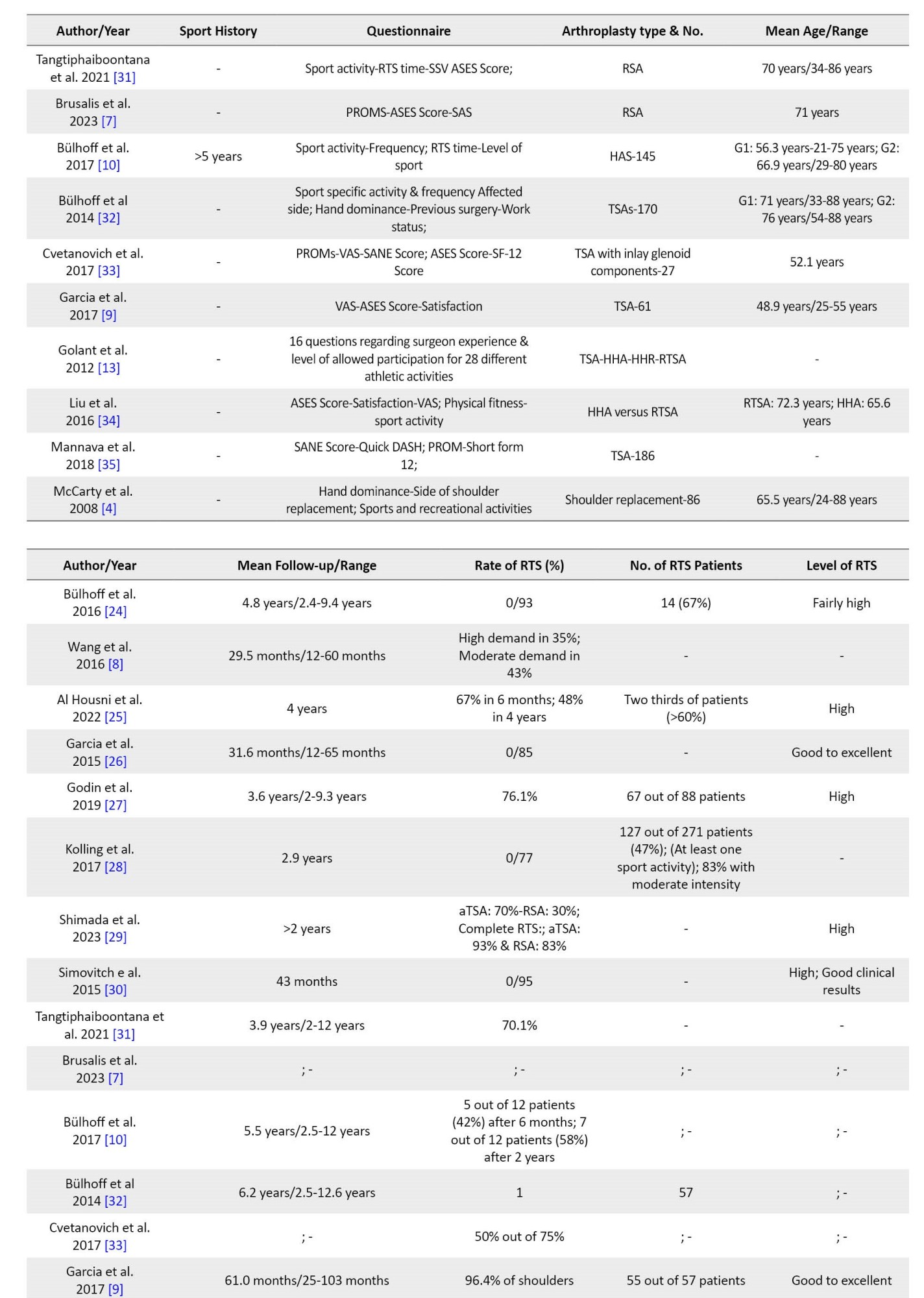
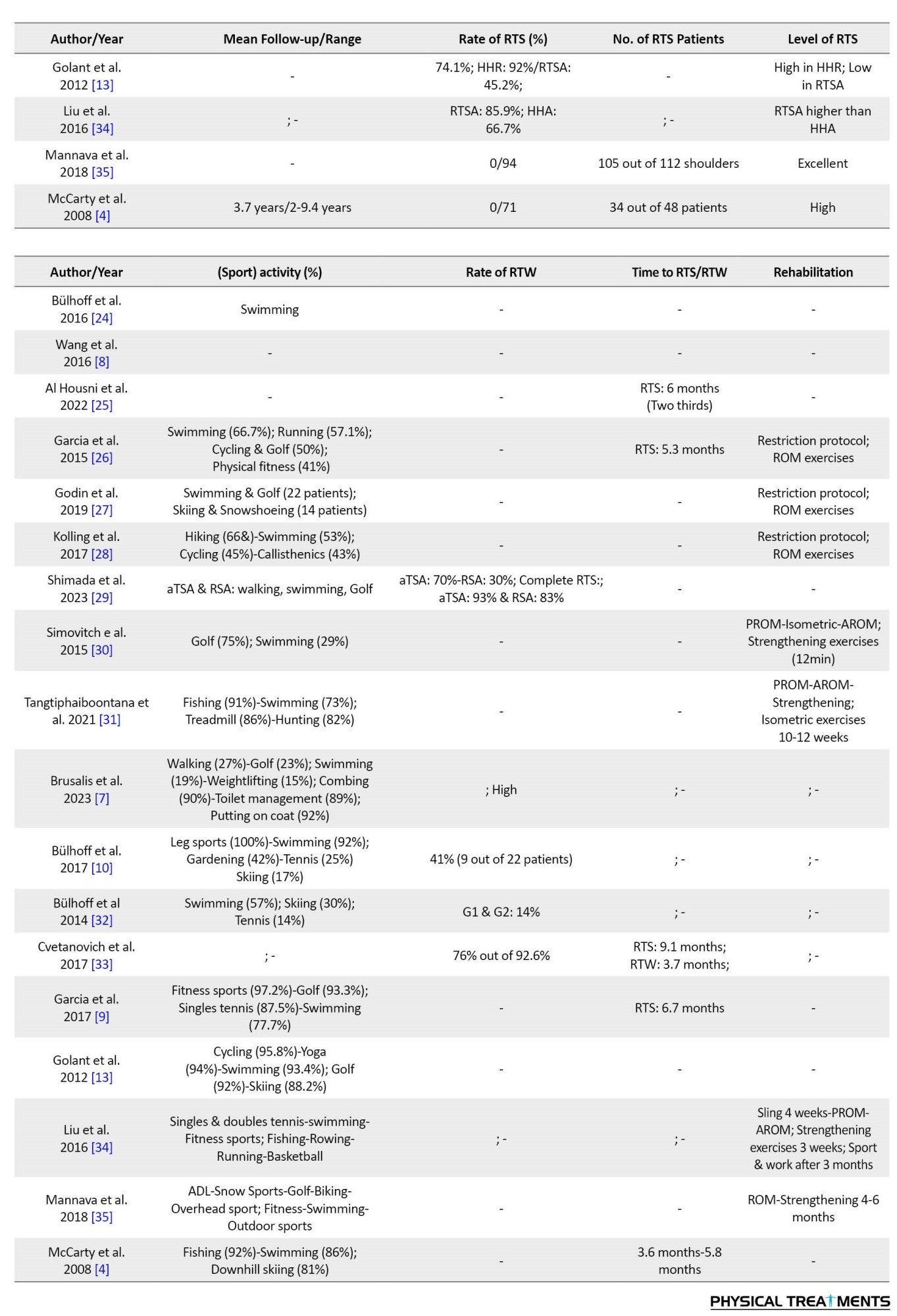
The search was conducted in English, with all texts screened by researchers. A total of 4 035 articles were obtained from databases using relevant keywords. Initial screening of article titles resulted in the removal of 15 duplicates. Subsequent examination of abstracts led to the exclusion of 3 945 articles that did not meet the inclusion criteria. Full-text assessment was performed on 75 articles, with 57 articles excluded for various reasons, such as being in languages other than English (e.g. Chinese, Hindi, Italian, Spanish) or not being relevant to the RTS after shoulder arthroplasty. Ultimately, 18 articles, meeting all criteria, were included in the review, and their results were comprehensively reported. A senior researcher independently verified the final list of selected articles to ensure alignment with the study’s objectives. Figure 1 shows the study selection process, and Table 1 presents the population, intervention, comparison, outcome, and study (PICOS)-type framework based on the specified research question.
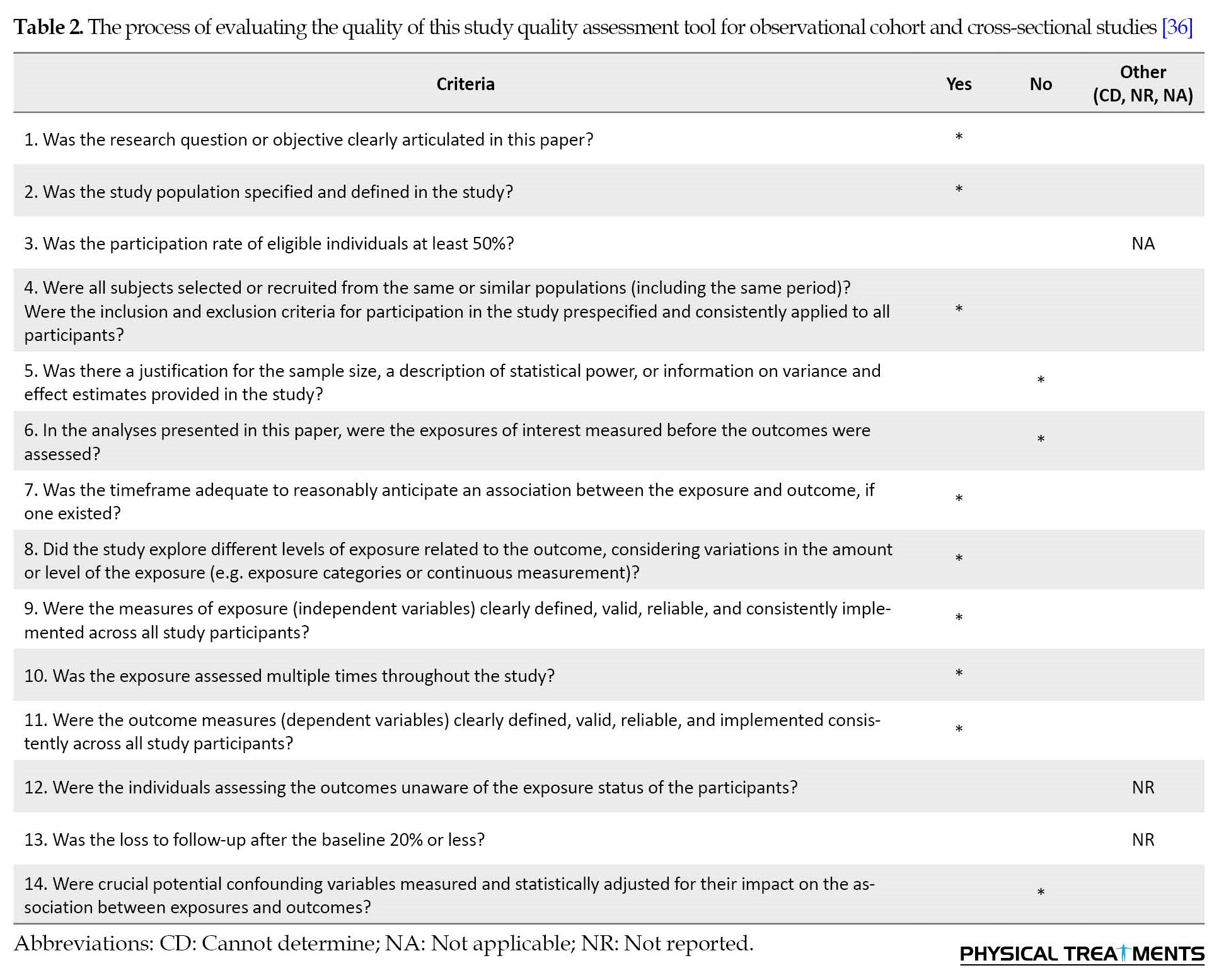
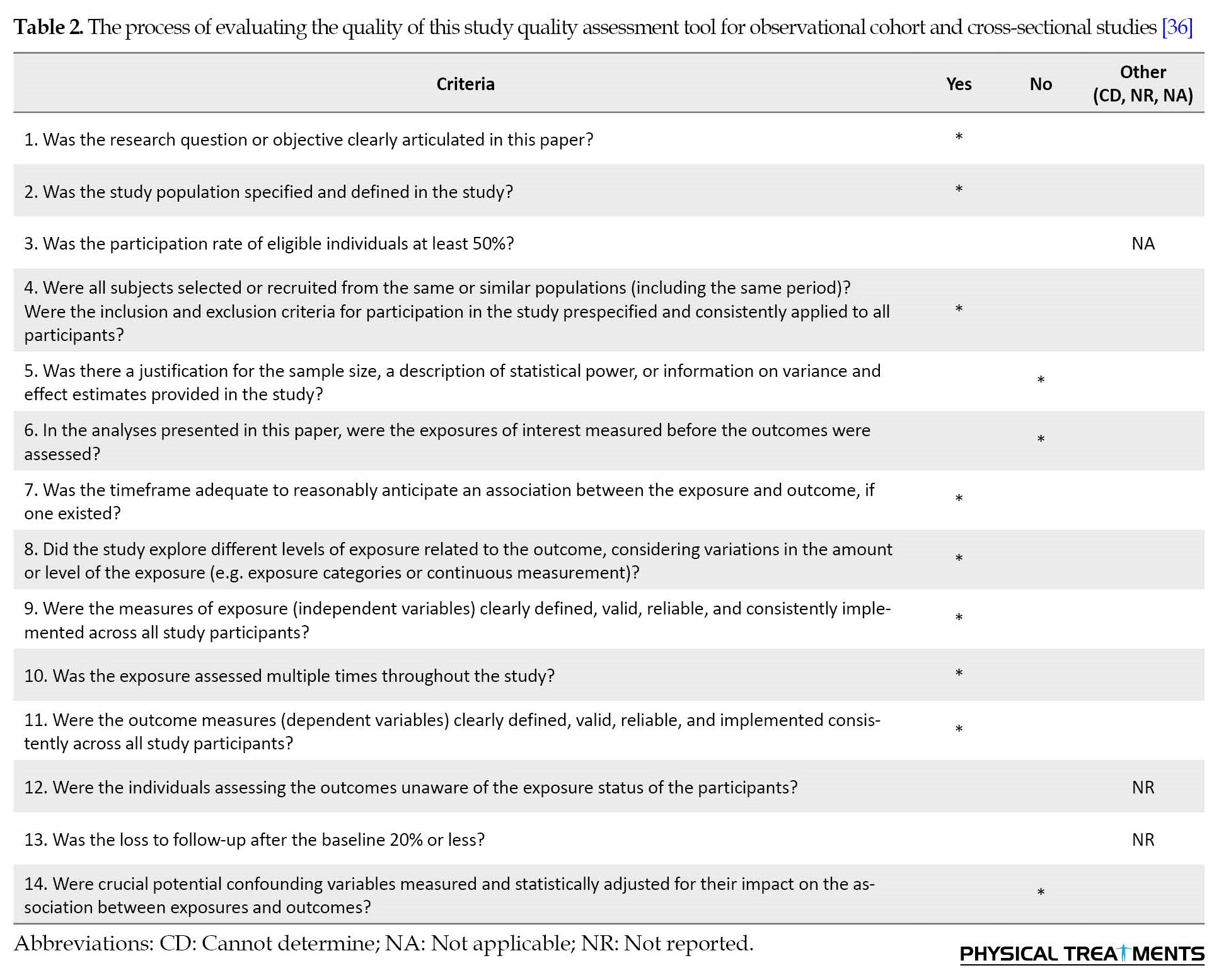
Through searches in databases, including Web of Science, PEDRO, Google Scholar, PubMed, SCOPUS, and CINAHL, 4 035 articles were initially obtained. Following the removal of duplicate titles, 4 020 abstracts were reviewed. Subsequently, 15 articles were excluded based on abstract assessment, leaving 75 full-text articles for further examination. After a thorough review of the full-text articles, 57 were excluded, and 18 were ultimately included in the study. Table 2 shows the evaluation process for the study’s quality, and Figure 1 shows the process of assessing and selecting research articles.
Results
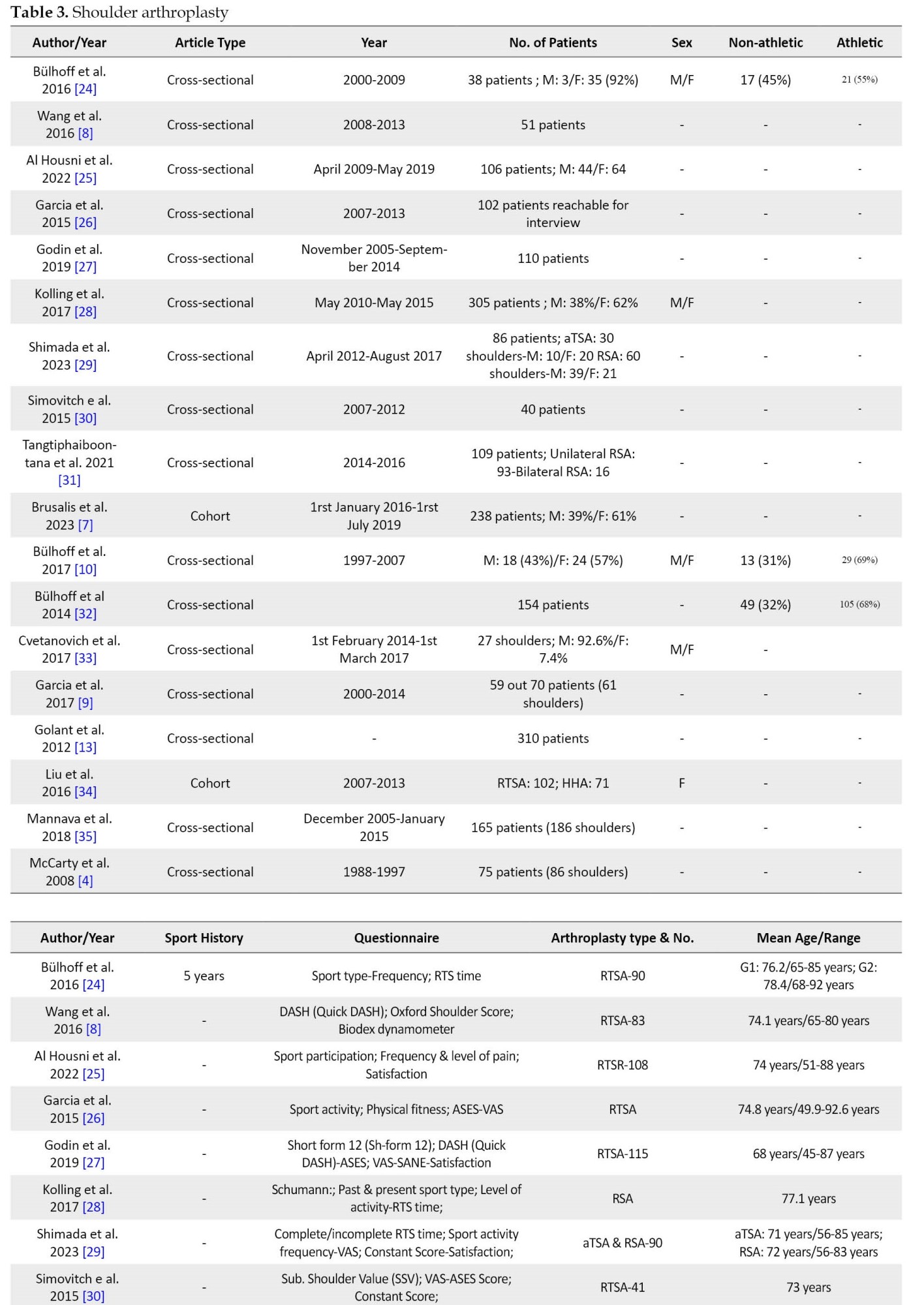
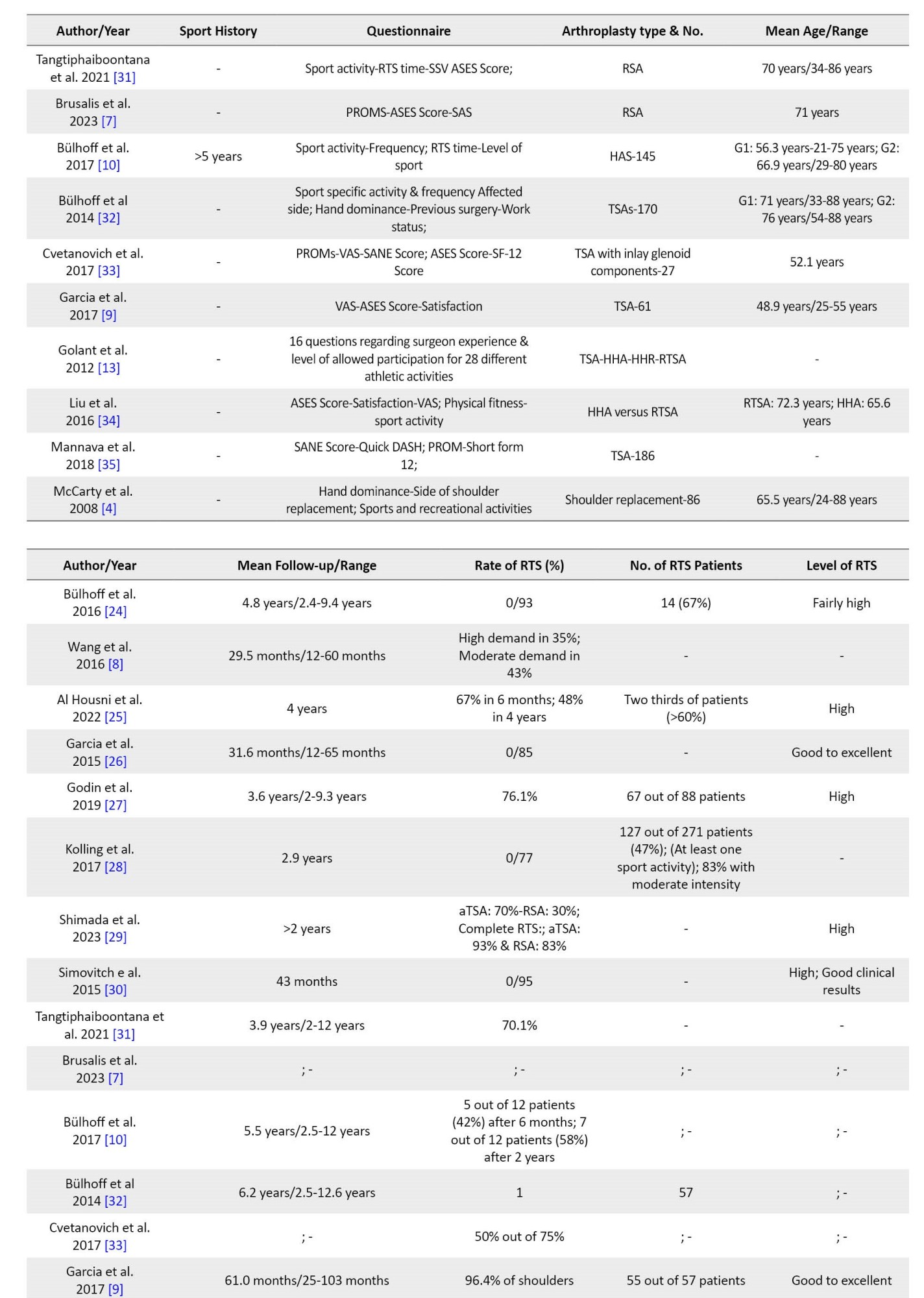
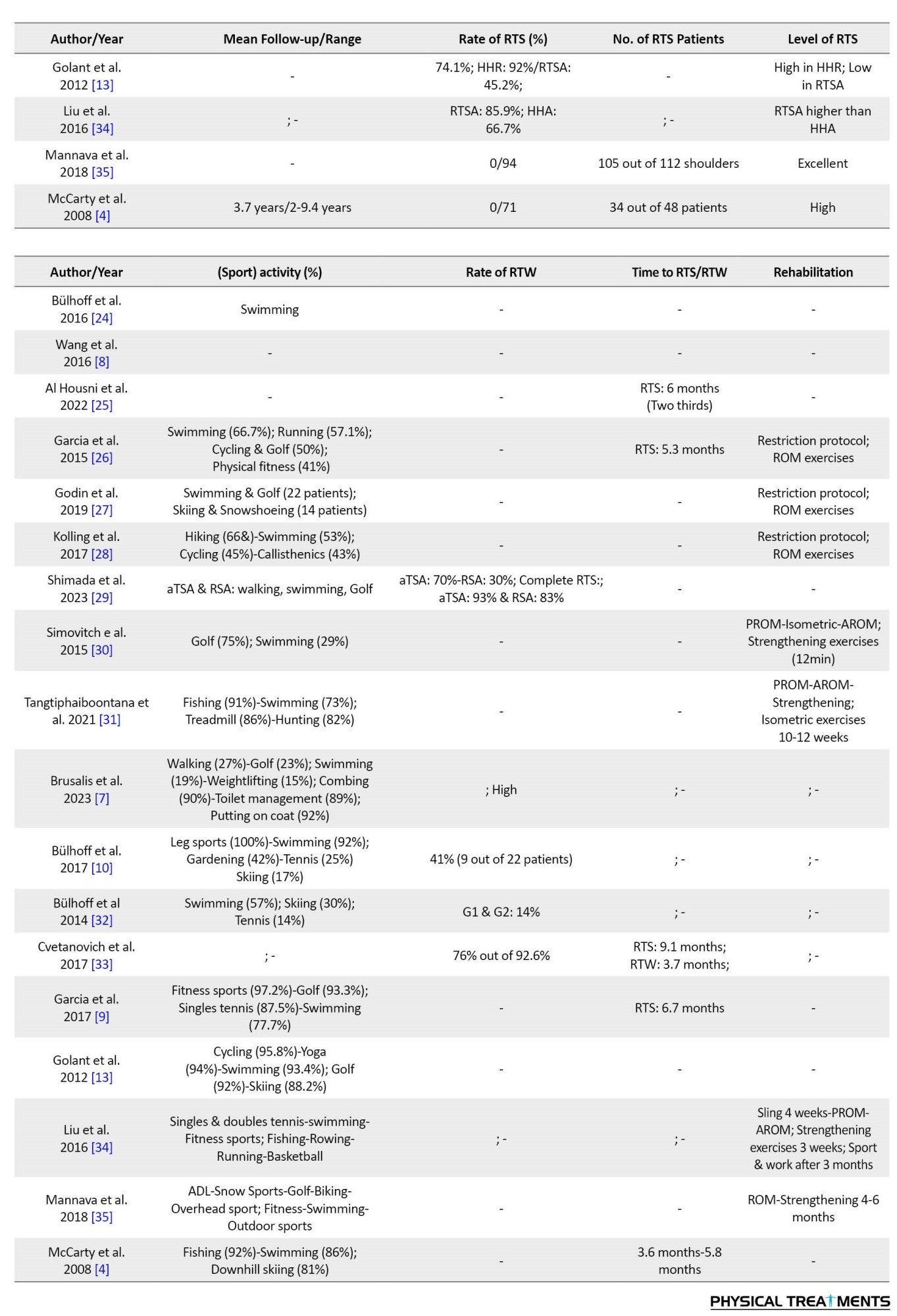
By summarizing the results obtained from the review of the studies, it was found that different kinds of shoulder arthroplasty were used in these studies. Eighteen different shoulder arthroplasty articles were reported with 18 different columns, including the author and year (stating the related authors’ name and the year that the article was conducted), article type (stating the type of article whether it’s cross-sectional or cohort), year range (stating the range of time that the information of the patients has been collected), number of patients (No. of patients) (stating the patients’ number who participated in the related study), sports history (stating the history of the sport of the patients), sex (stating the patients’ related gender to determine whether they were male, female, or bisexual, mean age (stating the mean age of the individuals in the related study), arthroplasty type and No. (stating the type of arthroplasty in terms of surgery, such as RSA, TSA, and so forth, also stating the related number of arthroplasties that have been done until that time), questionnaire (stating the elements and components of the related questionnaires), mean follow-up (stating the average follow-up times of the patients in the related study), rate of RTS (stating the return to sport rate with the percentage), No. of RTS patients (stating the number of patients who returned to their sports), level of RTS (stating the RTS magnitude or size), sports activity (stating the different kinds of sports that patients returned after arthroplasty), rate of return to work (RTW) (stating the return to work or physical activity rate with the percentage), time to RTS and RTW (stating the time range that patients return to sport and work), and rehabilitation (stating the rehabilitation protocols that some studies conducted after arthroplasty before RTS. Table 3 presents the studies concerning shoulder arthroplasty.
Discussion and Conclusion
This study was conducted to report factors related to RTS after shoulder arthroplasty. The main results of the article were the high proportion of RTS rate, level, and number of patients after shoulder arthroplasty, especially the types TSA and RTSA.
All articles were between 2008-2023. From 1988 to 2019, out of 18 articles, 16 were cross-sectional studies and 2 were cohort studies. Two articles reported that the sport history was 5 and <5 years and in terms of sex, 4 out of 5 articles were both male and female and 1 was just female. Besides, except for 5 out of 18 articles in mean follow-up, all mean age and follow-up time have been reported.
From an arthroplasty-type perspective, 7 out of 18 articles were RTSA, 6 were TSA, 4 were RSA, and others were HSA, HHA, and HHR, respectively. As a result, RTSA was the most common and popular treatment method among 18 articles that patients underwent during their surgery.
Additionally, the tools used to evaluate all patients were mostly the patient-reported outcome measures evaluating patients’ sports type, frequency, RTS time, sports participation, level of sport and pain, sports activity, hand dominance, previous surgery, work status, physical fitness, and side of the shoulder replacement, additionally, various reliable questionnaires, such as disability of arm, shoulder, and hand (DASH) (quick DASH), Oxford shoulder score, satisfaction, American Shoulder and Elbow Surgeons shoulder score (ASES score), visual analog scale (VAS), short form 12 (SF-12), single assessment numeric evaluation (SANE), constant score, subjective shoulder value (SSV), and shoulder activity scale (SAS), were utilized in the study.
Seven out of 18 articles used a post-operative rehabilitation protocol. The protocol consisted of some restriction protocol, including external rotation until 30 degrees for 2-3 weeks, sling, active range of motion (AROM) and passive range of motion (PROM) exercises, isometric exercises for 10-12 weeks, strengthening exercises for 12 minutes of 3 weeks and then started their sport or work after 3-6 months.
Last but not least, this review also reported the rate, level, time to return, the number of RTS patients, and sports activities after different shoulder arthroplasties. Seventeen out of 18 articles reported the RTS rate above 80%. Eleven out of 18 articles reported the level of RTS was high and excellent. Five out of 18 articles reported the time to RTS between 5.3 months to 9.1 months. Also, the number of RTS patients reported in 8 articles and the highest one was 55 out of 57 patients. Moreover, the rate and time of RTW are also reported in some articles. The RTW rate was reported in 5 studies and the highest was 93% in TSA and 83% in RSA. Time to RTW was reported to be 3.7 months in just one study. In terms of the sports activity after the RTS report, 15 out of 18 articles mentioned some sports activities that the patients participated in swimming, leg sports, tennis, golf, skiing, and so forth. Among these, swimming (100%) was the most common and popular sport in which patients could take part after shoulder arthroplasty.
As previously noted, the rate and level of RTS after shoulder arthroplasty are deemed significant. For instance, in a particular study, 6 patients (29%) cited the continuation of sports participation as the primary reason for undergoing shoulder replacement surgery [3, 24]. Recent evidence also suggests that in approximately 70% of cases, patients may return to recreational sports activities they were looking forward to [3, 26, 31]. However, much research is needed to complete the information in this field.
We hope this comprehensive systematic review provides insight into sports physiotherapists, athletic trainers, clinicians, practitioners, and coaches and trainers to help patients increase their quality of life and have successful RTS after shoulder arthroplasty.
Ethical Considerations
Compliance with ethical guidelines
This article is a review with no human or animal sample.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization: Ali Parvaneh Sarand; Methodology, investigation, writing, resources: All authors; Supervision: Ali Asghar Norasteh.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors appreciate all individuals who contributed to the completion of this article.
References
Over the past few decades, shoulder arthroplasty has become a reliable and successful treatment for end-stage glenohumeral arthritis and post-traumatic sequelae [1, 2, 3] to relieve pain and restore mobility to the joint [3, 4]. The number of individuals opting for shoulder arthroplasty is on the rise, thanks to the development of more sophisticated implants and surgical techniques [5]. As life expectancy continues to increase, many elderly people are looking to maintain an active lifestyle, even after undergoing shoulder arthroplasty, to enjoy a higher quality of life [5]. However, engaging in sports or intense physical activity after arthroplasty carries certain risks, such as dislocation, polyethylene wear, and loosening of the implants [6].
Some different kinds of arthroplasty include reversed shoulder arthroplasty (RSA) [7], reversed total shoulder arthroplasty (RTSA) [8], total shoulder arthroplasty (TSA) [9], shoulder hemiarthroplasty (HSA) [10], humeral hemiarthroplasty (HHA) [11], humeral head resurfacing (HHR) [12] with biologic or prosthetic glenoid resurfacing (TSR) [12]. Increased shoulder arthroplasty was used for different diseases, such as osteoarthritis (OA), post-traumatic arthritis, inflammatory arthritis, osteonecrosis, rotator cuff dysfunction, and comminuted fractures [13].
The significance of participating in sports after shoulder arthroplasty has increased due to a heightened focus on physical fitness, making it more clinically relevant [13]. An increasing segment of the aging population, undergoing joint replacement surgery, expresses interest in sports and physical activities. If joint arthroplasty is required, their participation in sports activities may be limited. After different joint arthroplasties, previous studies have shown a return to sport (RTS) [14-22]. Since shoulder arthroplasty is a successful treatment, more attention has been paid to the patient’s aim of RTS [3, 10]. A common inquiry among patients undergoing shoulder arthroplasty is whether they can resume their pre-surgery activities, including questions about the types of sports or work they can expect post-procedure [3, 10].
The patient questionnaire consisted of closed-ended questions, prompting participants to express their agreement with the surgeon’s evaluation of their operated shoulder by marking a circle. This approach resulted in high levels of agreement with the surgeon’s assessment [23]. The assessment incorporated a 0-10 pain scale (0 indicating no pain and 10 indicating severe pain). Participants reported their current pain medication usage, categorized as none, over-the-counter, narcotic, or a combination of over-the-counter and narcotic. The range of motion was evaluated through a diagram, specifying forward flexion in degrees, external rotation in degrees, and internal rotation on a scale of 1-8. Strength was measured on a 10-point scale, ranging from 0 (complete paralysis) to 10 (normal strength) [23]. Lastly, RTS criteria are mostly evaluated quantitatively by the physical activity and sport-related questionnaires [4, 7-10, 13, 24-35]. However, much research is needed to complete the information in this field.
Given the significance of RTS, this study was conducted to thoroughly review the RTS outcomes following shoulder arthroplasty.
Materials and Methods
This is a systematic review based on guidelines for preferred reporting items.
Search strategy
This review thoroughly examines RTS following shoulder arthroplasty. It involves searching databases, such as Web of Science, PEDRO, Google Scholar, PubMed, SCOPUS, and CINAHL using two sets of keyword groups, (group 1) “return to sport” or “return to play” or “return to competition” or “return to physical activity”; and (group 2) “shoulder arthroplasty” or “shoulder replacement”. The two sets of combinations were investigated in the title, abstract, and keywords of studies published in journals indexed in the databases, covering the period from January 2000 to May 2023. Additionally, a manual search and a comprehensive review of article sources were conducted to identify articles that may not have been captured through electronic searches.
Eligibility criteria
The inclusion criteria included individuals, including athletes, who underwent various types of shoulder arthroplasty for reasons, such as rotator cuff tear, arthropathy, inflammation, glenohumeral OA, inflammatory OA, and fracture. Other criteria included a history of sports participation, a follow-up duration of >1 year, age >65 years, English-language articles, and the inclusion of full-text studies with cross-sectional and cohort designs.
The exclusion criteria included non-English articles, follow-up durations of <1 year, age <65 years, revision surgery cases, unwilling or deceased patients, those lacking a history of sports participation, individuals unreachable after multiple telephone calls, those diagnosed with fracture sequelae or other shoulder injuries, such as fractures of the proximal humerus, and articles briefly published in congresses and seminars.
Study selection
The search was conducted in English, with all texts screened by researchers. A total of 4 035 articles were obtained from databases using relevant keywords. Initial screening of article titles resulted in the removal of 15 duplicates. Subsequent examination of abstracts led to the exclusion of 3 945 articles that did not meet the inclusion criteria. Full-text assessment was performed on 75 articles, with 57 articles excluded for various reasons, such as being in languages other than English (e.g. Chinese, Hindi, Italian, Spanish) or not being relevant to the RTS after shoulder arthroplasty. Ultimately, 18 articles, meeting all criteria, were included in the review, and their results were comprehensively reported. A senior researcher independently verified the final list of selected articles to ensure alignment with the study’s objectives. Figure 1 shows the study selection process, and Table 1 presents the population, intervention, comparison, outcome, and study (PICOS)-type framework based on the specified research question.
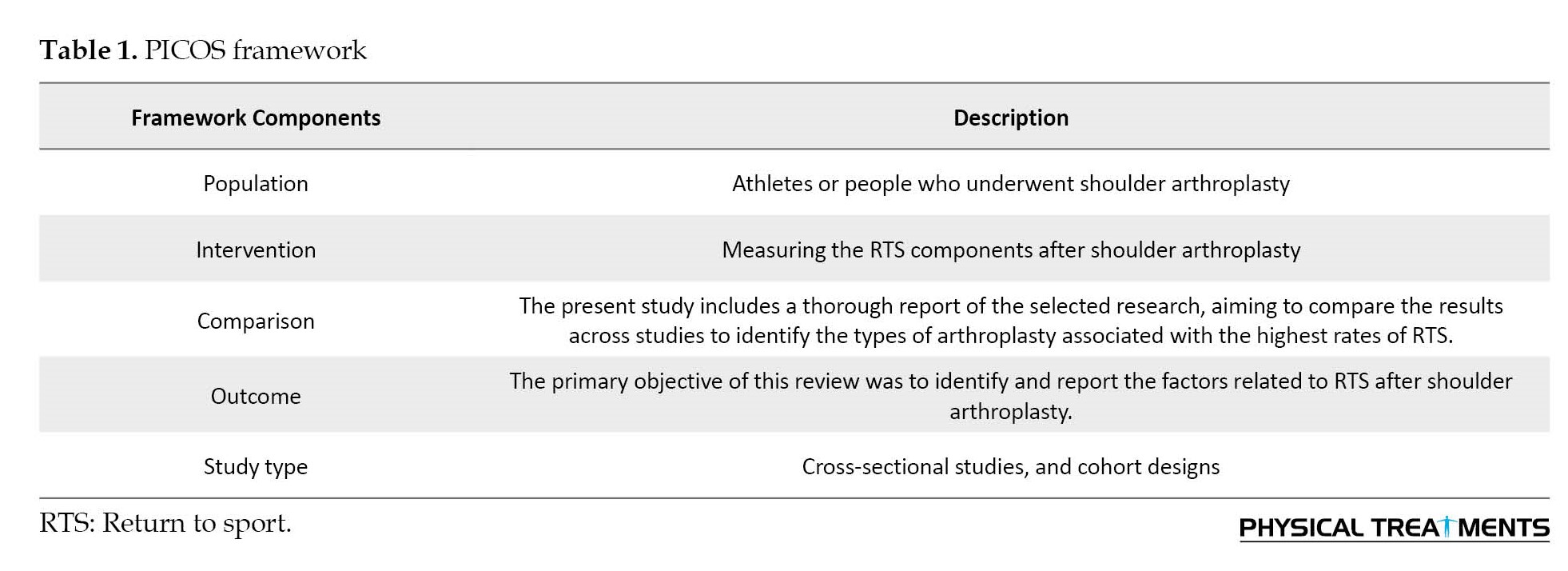
Through searches in databases, including Web of Science, PEDRO, Google Scholar, PubMed, SCOPUS, and CINAHL, 4 035 articles were initially obtained. Following the removal of duplicate titles, 4 020 abstracts were reviewed. Subsequently, 15 articles were excluded based on abstract assessment, leaving 75 full-text articles for further examination. After a thorough review of the full-text articles, 57 were excluded, and 18 were ultimately included in the study. Table 2 shows the evaluation process for the study’s quality, and Figure 1 shows the process of assessing and selecting research articles.
Results
By summarizing the results obtained from the review of the studies, it was found that different kinds of shoulder arthroplasty were used in these studies. Eighteen different shoulder arthroplasty articles were reported with 18 different columns, including the author and year (stating the related authors’ name and the year that the article was conducted), article type (stating the type of article whether it’s cross-sectional or cohort), year range (stating the range of time that the information of the patients has been collected), number of patients (No. of patients) (stating the patients’ number who participated in the related study), sports history (stating the history of the sport of the patients), sex (stating the patients’ related gender to determine whether they were male, female, or bisexual, mean age (stating the mean age of the individuals in the related study), arthroplasty type and No. (stating the type of arthroplasty in terms of surgery, such as RSA, TSA, and so forth, also stating the related number of arthroplasties that have been done until that time), questionnaire (stating the elements and components of the related questionnaires), mean follow-up (stating the average follow-up times of the patients in the related study), rate of RTS (stating the return to sport rate with the percentage), No. of RTS patients (stating the number of patients who returned to their sports), level of RTS (stating the RTS magnitude or size), sports activity (stating the different kinds of sports that patients returned after arthroplasty), rate of return to work (RTW) (stating the return to work or physical activity rate with the percentage), time to RTS and RTW (stating the time range that patients return to sport and work), and rehabilitation (stating the rehabilitation protocols that some studies conducted after arthroplasty before RTS. Table 3 presents the studies concerning shoulder arthroplasty.
Discussion and Conclusion
This study was conducted to report factors related to RTS after shoulder arthroplasty. The main results of the article were the high proportion of RTS rate, level, and number of patients after shoulder arthroplasty, especially the types TSA and RTSA.
All articles were between 2008-2023. From 1988 to 2019, out of 18 articles, 16 were cross-sectional studies and 2 were cohort studies. Two articles reported that the sport history was 5 and <5 years and in terms of sex, 4 out of 5 articles were both male and female and 1 was just female. Besides, except for 5 out of 18 articles in mean follow-up, all mean age and follow-up time have been reported.
From an arthroplasty-type perspective, 7 out of 18 articles were RTSA, 6 were TSA, 4 were RSA, and others were HSA, HHA, and HHR, respectively. As a result, RTSA was the most common and popular treatment method among 18 articles that patients underwent during their surgery.
Additionally, the tools used to evaluate all patients were mostly the patient-reported outcome measures evaluating patients’ sports type, frequency, RTS time, sports participation, level of sport and pain, sports activity, hand dominance, previous surgery, work status, physical fitness, and side of the shoulder replacement, additionally, various reliable questionnaires, such as disability of arm, shoulder, and hand (DASH) (quick DASH), Oxford shoulder score, satisfaction, American Shoulder and Elbow Surgeons shoulder score (ASES score), visual analog scale (VAS), short form 12 (SF-12), single assessment numeric evaluation (SANE), constant score, subjective shoulder value (SSV), and shoulder activity scale (SAS), were utilized in the study.
Seven out of 18 articles used a post-operative rehabilitation protocol. The protocol consisted of some restriction protocol, including external rotation until 30 degrees for 2-3 weeks, sling, active range of motion (AROM) and passive range of motion (PROM) exercises, isometric exercises for 10-12 weeks, strengthening exercises for 12 minutes of 3 weeks and then started their sport or work after 3-6 months.
Last but not least, this review also reported the rate, level, time to return, the number of RTS patients, and sports activities after different shoulder arthroplasties. Seventeen out of 18 articles reported the RTS rate above 80%. Eleven out of 18 articles reported the level of RTS was high and excellent. Five out of 18 articles reported the time to RTS between 5.3 months to 9.1 months. Also, the number of RTS patients reported in 8 articles and the highest one was 55 out of 57 patients. Moreover, the rate and time of RTW are also reported in some articles. The RTW rate was reported in 5 studies and the highest was 93% in TSA and 83% in RSA. Time to RTW was reported to be 3.7 months in just one study. In terms of the sports activity after the RTS report, 15 out of 18 articles mentioned some sports activities that the patients participated in swimming, leg sports, tennis, golf, skiing, and so forth. Among these, swimming (100%) was the most common and popular sport in which patients could take part after shoulder arthroplasty.
As previously noted, the rate and level of RTS after shoulder arthroplasty are deemed significant. For instance, in a particular study, 6 patients (29%) cited the continuation of sports participation as the primary reason for undergoing shoulder replacement surgery [3, 24]. Recent evidence also suggests that in approximately 70% of cases, patients may return to recreational sports activities they were looking forward to [3, 26, 31]. However, much research is needed to complete the information in this field.
We hope this comprehensive systematic review provides insight into sports physiotherapists, athletic trainers, clinicians, practitioners, and coaches and trainers to help patients increase their quality of life and have successful RTS after shoulder arthroplasty.
Ethical Considerations
Compliance with ethical guidelines
This article is a review with no human or animal sample.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization: Ali Parvaneh Sarand; Methodology, investigation, writing, resources: All authors; Supervision: Ali Asghar Norasteh.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors appreciate all individuals who contributed to the completion of this article.
References
- Young A, Walch G, Boileau P, Favard L, Gohlke F, Loew M, et al. A multicentre study of the long-term results of using a flat-back polyethylene glenoid component in shoulder replacement for primary osteoarthritis. The Journal of Bone and Joint Surgery. British volume, 2011; 93(2):210-6. [DOI:10.1302/0301-620X.93B2.25086] [PMID]
- Raiss P, Schmitt M, Bruckner T, Kasten P, Pape G, Loew M, et al. Results of cemented total shoulder replacement with a minimum follow-up of ten years. The Journal of Bone and Joint Surgery. American volume. 2012; ;94(23):e1711-10.[DOI:10.2106/JBJS.K.00580] [PMID]
- Norasteh A A, Zolghadr H. Functional tests & their reliability for return to sport after shoulder injuries: A review study. Journal of Research in Orthopedic Science. 2022; 9(2):69-78. [DOI:10.32598/JROSJ.9.2.867.1]
- McCarty EC, Marx RG, Maerz D, Altchek D, Warren RF. Sports participation after shoulder replacement surgery. The American Journal of Sports Medicine. 2008; 36(8):1577-81. [DOI:10.1177/0363546508317126] [PMID]
- Kim SH, Wise BL, Zhang Y, Szabo RM. Increasing incidence of shoulder arthroplasty in the United States. The Journal of Bone and Joint Surgery. American Volume. 2011; 93(24):2249-54. [DOI:10.2106/JBJS.J.01994] [PMID]
- Zuckerman JD, Rokito A. Frozen shoulder: A consensus definition. Journal of Shoulder and Elbow Surgery. 2011; 20(2):322-5. [DOI:10.1016/j.jse.2010.07.008] [PMID]
- Brusalis CM, White AE, Finocchiaro A, Dines DM, Dines JS, Kontaxis A, et al. What specific activities are patients performing two years after primary reverse total shoulder arthroplasty? Seminars in Arthroplasty. 2023; 33(2):360-5.[DOI:10.1053/j.sart.2022.12.011]
- Wang A, Doyle T, Cunningham G, Brutty M, Campbell P, Bharat C, et al. Isokinetic shoulder strength correlates with level of sports participation and functional activity after reverse total shoulder arthroplasty. Journal of Shoulder and Elbow Surgery. 2016; 25(9):1464-9. [DOI:10.1016/j.jse.2016.01.025] [PMID]
- Garcia GH, Liu JN, Sinatro A, Wu HH, Dines JS, Warren RF, et al. High satisfaction and return to sports after total shoulder arthroplasty in patients aged 55 years and younger. The American Journal of Sports Medicine. 2017; 45(7):1664-9. [DOI:10.1177/0363546517695220] [PMID]
- Bülhoff M, Sowa B, Bruckner T, Zeifang F, Rais P. Return to sports and work after partial shoulder replacement surgery. Der Orthopäde. 2017; 46(8):711-6. [DOI:10.1007/s00132-017-3414-6] [PMID]
- Seah SJ, Puah KL, Lie DT. Can radiographic parameters predict favourable outcomes in proximal humeral hemiarthroplasty for fractures?-A case series. Journal of Orthopaedic Reports. 2023; 2(1):100118. [DOI:10.1016/j.jorep.2022.100118]
- Khokhar O, Khan S, Cash T, Khokhar H, Waseem M. O115 Is humeral head resurfacing still a valid treatment for younger patients? 10-15-year patient follow up data for the global conservative anatomic prosthesis. British Journal of Surgery. 2023; 110(Supplement_3):znad101.115. [DOI:10.1093/bjs/znad101.115]
- Golant A, Christoforou D, Zuckerman JD, Kwon YW. Return to sports after shoulder arthroplasty: A survey of surgeons’ preferences. Journal of Shoulder and Elbow Surgery. 2012; 21(4):554-60. [DOI:10.1016/j.jse.2010.11.021] [PMID]
- Antonelli B, Teng R, Breslow RG, Jamison M, Hepinstall M, Schwarzkopf R, et al. Few runners return to running after total joint arthroplasty, while others initiate running. Global Research & Reviews. 2023; 7(4):e23.00019. [DOI:10.5435/JAAOSGlobal-D-23-00019]
- Gschwend N, Frei T, Morscher E, Nigg B, Loehr J. Alpine and cross-country skiing after total hip replacement: 2 cohorts of 50 patients each, one active, the other inactive in skiing, followed for 5-10 years. Acta orthopaedica Scandinavica. 2000; 71(3):243-9. [DOI:10.1080/000164700317411825] [PMID]
- Huch K, Müller KA, Stürmer T, Brenner H, Puhl W, Günther KP. Sports activities 5 years after total knee or hip arthroplasty: The Ulm Osteoarthritis Study. Annals of the Rheumatic Diseases. 2005; 64(12):1715-20. [DOI:10.1136/ard.2004.033266] [PMID]
- Jensen KL, Rockwood CA Jr. Shoulder arthroplasty in recreational golfers. Journal of Shoulder and Elbow Surgery. 1998; 7(4):362-7. [DOI:10.1016/S1058-2746(98)90024-6] [PMID]
- Mallon WJ, Callaghan JJ. Total hip arthroplasty in active golfers. The Journal of Arthroplasty. 1992; 7( Suppl):339-46. [DOI:10.1016/S0883-5403(07)80022-2] [PMID]
- Mallon WJ, Callaghan JJ. Total knee arthroplasty in active golfers. The Journal of Arthroplasty. 1993; 8(3):299-306. [DOI:10.1016/S0883-5403(06)80093-8] [PMID]
- McGrory BJ, Stuart MJ, Sim FH. Participation in sports after hip and knee arthroplasty: Review of literature and survey of surgeon preferences. Mayo Clinic Proceedings. 1995. 70(4):342-8. [DOI:10.4065/70.4.342] [PMID]
- Mont MA, Rajadhyaksha AD, Marxen JL, Silberstein CE, Hungerford DS. Tennis after total knee arthroplasty. The American Journal of Sports Medicine. 2002; 30(2):163-6. [DOI:10.1177/03635465020300020301] [PMID]
- Ritter MA, Meding JB. Total hip arthroplasty: Can the patient play sports again? Orthopedics. 1987; 10(10):1447-52. [DOI:10.3928/0147-7447-19871001-15] [PMID]
- Smith AM, Barnes SA, Sperling JW, Farrell CM, Cummings JD, Cofield RH. Patient and physician-assessed shoulder function after arthroplasty. The Journal of Bone and Joint Surgery. American volume. 2006; 88(3):508-13. [PMID]
- Bülhoff M, Sowa B, Bruckner T, Zeifang F, Raiss P. Activity levels after reverse shoulder arthroplasty. Archives of Orthopaedic and Trauma Surgery. 2016; 136(9):1189-93. [DOI:10.1007/s00402-016-2494-9] [PMID]
- Al Housni HSA, Lam PH, Latif JW, Murrell GAC. Sports participation after reverse total shoulder replacement. Orthopaedic Journal of Sports Medicine. 2022; 10(11):23259671221136304. [DOI:10.1177/23259671221136304] [PMID]
- Garcia GH, Taylor SA, DePalma BJ, Mahony GT, Grawe BM, Nguyen J, et al. Patient activity levels after reverse total shoulder arthroplasty: What are patients doing? The American Journal of Sports Medicine. 2015; 43(11):2816-21. [DOI:10.1177/0363546515597673] [PMID]
- Godin JA, Pogorzelski J, Horan MP, Lacheta L, Hussain ZB, Altintas B, et al. Impact of age and subscapularis tendon reparability on return to recreational sports activities and 2-year outcomes after reverse total shoulder arthroplasty. Orthopaedic Journal of Sports Medicine. 2019; 7(10):2325967119875461. [DOI:10.1177/2325967119875461] [PMID]
- Kolling C, Borovac M, Audigé L, Mueller AM, Schwyzer HK. Return to sports after reverse shoulder arthroplasty-the Swiss perspective. International Orthopaedics. 2018; 42(5):1129-35. [DOI:10.1007/s00264-017-3715-8] [PMID]
- Shimada Y, Matsuki K, Sugaya H, Takahashi N, Tokai M, Hashimoto E, et al. Return to sports and physical work after anatomical and reverse shoulder arthroplasty. Journal of Shoulder and Elbow Surgery. 2023; 32(7):1445-51. [DOI:10.1016/j.jse.2022.12.025] [PMID]
- Simovitch RW, Gerard BK, Brees JA, Fullick R, Kearse JC. Outcomes of reverse total shoulder arthroplasty in a senior athletic population. Journal of Shoulder and Elbow Surgery. 2015; 24(9):1481-5. [DOI:10.1016/j.jse.2015.03.011] [PMID]
- Tangtiphaiboontana J, Mara KC, Jensen AR, Camp CL, Morrey ME, Sanchez-Sotelo J. Return to sports after primary reverse shoulder arthroplasty: Outcomes at Mean 4-Year follow-up. Orthopaedic Journal of Sports Medicine. 2021; 9(6):23259671211012393. [DOI:10.1177/23259671211012393] [PMID]
- Bülhoff M, Sattler P, Bruckner T, Loew M, Zeifang F, Raiss P. Do patients return to sports and work after total shoulder replacement surgery? The American Journal of Sports Medicine. 2015; 43(2):423-7. [DOI:10.1177/0363546514557940] [PMID]
- Cvetanovich GL, Naylor AJ, O'Brien MC, Waterman BR, Garcia GH, Nicholson GP. Anatomic total shoulder arthroplasty with an inlay glenoid component: Clinical outcomes and return to activity. Journal of Shoulder and Elbow Surgery. 2020; 29(6):1188-96. [DOI:10.1016/j.jse.2019.10.003] [PMID]
- Liu JN, Garcia GH, Mahony G, Wu HH, Dines DM, Warren RF, et al. Sports after shoulder arthroplasty: A comparative analysis of hemiarthroplasty and reverse total shoulder replacement. Journal of Shoulder and Elbow Surgery. 2016; 25(6):920-6. [DOI:10.1016/j.jse.2015.11.003] [PMID]
- Mannava S, Horan MP, Frangiamore SJ, Hussain ZB, Fritz EM, Godin JA, et al. Return to recreational sporting activities following total shoulder arthroplasty. Orthopaedic Journal of Sports Medicine. 2018; 6(7):2325967118782672. [DOI:10.1177/2325967118782672] [PMID]
- Downes MJ, Brennan ML, Williams HC, Dean RS. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open. 2016; 6(12):e011458. [DOI:10.1136/bmjopen-2016-011458] [PMID]
Type of Study: Research |
Subject:
Sport injury and corrective exercises
Received: 2023/08/31 | Accepted: 2023/12/3 | Published: 2024/01/1
Received: 2023/08/31 | Accepted: 2023/12/3 | Published: 2024/01/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |