Wed, Jul 9, 2025
Volume 14, Issue 2 (Spring 2024)
PTJ 2024, 14(2): 93-100 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sheikhalizade H, Imani F, Jafarnezhadgero A, Imani Brouj S. Sand Exercises Altered Muscular Frequency Content in Individuals With Anterior Cruciate Ligament Reconstruction and Pronated Feet During Walking. PTJ 2024; 14 (2) :93-100
URL: http://ptj.uswr.ac.ir/article-1-594-en.html
URL: http://ptj.uswr.ac.ir/article-1-594-en.html
1- Department of Sport Biomechanics, Faculty of Educational Sciences and Psychology, University of Mohaghegh Ardabili, Ardabil, Iran.
Keywords: Exercise, Frequency content, Electromyography, Pronated feet, Anterior cruciate ligament reconstruction
Full-Text [PDF 530 kb]
(637 Downloads)
| Abstract (HTML) (3067 Views)
Full-Text: (416 Views)
Introduction
The skeletal-muscular system of the human body is an interconnected set and changes in any part of it can affect other parts and cause problems in basic motor skills, such as walking [1, 2]. Walking activity is one of the main tasks of the lower body, by performing various actions, such as absorbing, the forces resulting from the impact of the foot on the ground, maintaining balance, and producing forward forces, plays an essential role in creating an integrated and properly coordinated pattern of walking [2-4]. A previous study has shown that natural walking requires neurally controlled commands, force generation by the muscles, and a specific range of motion for each case. This means that if it occurs in any of these cases, it can cause abnormal walking [5]. Abnormal walking causes various complications in the lower limbs—one of the factors that may cause injury while walking is foot pronation [6].
Pronation of the foot involves the reduction of the medial longitudinal arch along with the navicular bone on the medial surface of the foot, which can cause anatomical abnormalities [7]. This devaluation in the height of the internal longitudinal arch depends on the condition of the plantar bones and ligaments, leg and foot muscles, and plays an important role in maintaining balance and performing movement abilities and skills [7]. Foot pronation is a combination of heel eversion, foot abduction, and ankle dorsiflexion, which occurs in the subtalar and midtarsal joints and affects the longitudinal-internal arch of the foot [8, 9]. These additional movements caused the lack of shock absorption in these joints during transition movements [8, 9]. Excessive pronation during the support phase of walking leads to increased flexibility and, thus bringing instability of the subtalar and midtarsal joints [8, 9]. People with overpronation suffer from many biomechanical inefficiencies in the foot and ankle [10]. Foot pronation can cause biomechanical irregularities in a person’s performance, which also leads to Achilles tendon pain, leg pain, hamstring strain, and quadriceps muscle strain [11]; therefore, the pronated foot leads to impaired posture control, impaired absorption of pressures on the soles of the feet, the occurrence of lower limb injuries, and changes in the mobility of the ankle and foot joints, which, secondarily, probably causes changes in the electrical activity of the muscles [12-15]. Therefore, in addition to the changes in the standing position, the abnormalities of this part also affect the movement [7]. Overpronation of the foot is considered a major contributing factor in lower limb injuries [16]. It has been reported that between 0.6% and 8.5% of male players experience an injury to a ligament called the anterior cruciate ligament each year [9]. Knee injuries account for approximately 61% of sports injuries [17]. The pronation of the foot and internal rotation of the tibia are coupled with each other and create torsional forces [16]. This torsional stress may lead to ligament tears or dislocation-induced fractures [16]. The compensatory mechanism caused by muscle weakness in some other muscles can cause a disturbance in the ratio of muscle forces and then cause changes in the movement pattern [2].
In pronation, the fibularis, gastrocnemius medialis, soleus, iliotibial band, hamstrings, hip adductors, and iliopsoas muscles become functionally short (overactive), and the posterior and posterior and anterior calf muscles, vastus medialis, gluteus medius, and maximus, external rotators of the hip are inhibited [18, 19]. Evidence suggests that individuals with foot pronation exhibit increased levels of muscle electrical activity in certain muscles that are involved in the ankle joint, such as the tibialis posterior and anterior, dorsi flexors, and plantar flexors while displaying decreased levels of electrical activity in the evertor muscles, specifically the peroneus muscle [14, 20-22]. It seems logical that the change in the electrical activity of the muscles leads to a change in the function of the muscles and a decrease in their efficiency [2]. Effective rehabilitation programs for foot and ankle injuries have been successful in clinical trials, and programs focus on exercise therapy to improve joint range of motion, muscle strength, neuromuscular coordination, and gait mechanics [23].
Sand exercises can be included during treatment because they are free of cost and accessible to many people worldwide [24]. More importantly, training on the sand, which is an unstable and unpredictable surface, can have a positive effect on the biomechanics of human movement [24]. Greater electrical activity has been observed in muscles, such as gastrocnemius medialis, hamstrings (semi-membranous and biceps femoris), vastus lateralis and vastus medialis, rectus femoris, and the iliotibial band when running on sand compared to running on a hard surface [25]. Another study showed that due to the decrease in the elastic energy of the surface, more muscles are greater active while walking on sand surfaces [26]. An interventional study investigated the effect of eight weeks of exercise on the sand on walking kinetics and muscle activities in patients with pronated feet [24]. They observed lower vertical and lateral peak forces and increased electrical activity of lower limb muscles (e.g. vastus lateralis) after exercise. Accordingly, walking and running exercises on sand are recommended as an effective therapy for people with pronated feet.
To the authors’ knowledge, no study is available that examines the effects of walking on sand on the frequency content of electrical activity in subjects with anterior cruciate ligament injuries and pronated feet during walking. Therefore, this study determines the effect of exercises on the sand on the frequency content of electrical activity in people with anterior cruciate ligament injuries and pronated feet during walking.
Materials and Methods
This was a semi-experimental and laboratory-type study. The statistical sample size of the present study was 28 people (n=14 in each group). The statistical power of 0.8 was estimated at the significance level of 0.05 in the G*Power software. The statistical population of this research was males with the age range of 22 to 25 years who voluntarily participated in this research. The inclusion criteria were male gender, age range between 22 to 25 years, and at least a history of anterior cruciate ligament reconstruction for 6 months, anterior cruciate ligament reconstruction in one leg, having a pronated foot, passed six months after surgery, and ability to walk independently. The exclusion criteria were having a history of surgery or orthopedic disorders (except for anterior cruciate ligament reconstruction), the difference in the lower limbs, and using any braces.
According to the medical records of the subjects, all the people who were placed in the anterior cruciate ligament reconstruction group had a complete anterior cruciate ligament tear that was operated by arthroscopic surgery, and these people also had pronation. During the call, only 28 subjects had the conditions to enter the research in the anterior cruciate ligament injury group, who were selected with available sampling. The subjects’ dominant leg was determined by the soccer ball shot test. All subjects were right-footed. After justifying the subjects and mentioning the ethical considerations of the research, as well as mentioning the tips and training that did not interfere in the process of conducting research and data collection, the person was asked to wear sports clothes to prevent injury, and before performing the test, perform the initial heating. Then, the subjects walked on a 15-m path. Next, the experimental group performed the exercise protocol for 8 weeks, during which the control group did not do any exercises. Once more, after the completion of 8 weeks, the information on the electrical activity of the muscles was recorded in the act of walking. To record electromyography signals, an electromyogram device (Biometric Ltd, Nine Mile Point Ind Est, Newport, UK) was used. Before the electrode placement, excess hair was shaved and the skin was cleaned with alcohol and medical cotton. The placement of surface electrodes for recording electrical signals on selected muscles (tibialis anterior, gastrocnemius medialis, vastus medialis, vastus lateralis, biceps femoris, rectus femoris, semitendinosus, and gluteus medius) was determined according to the SENIAM protocol [27]. Surface electromyography signals were recorded with a sampling rate of 1000 Hz. The Biometrics DataLITE program, version 3.1 was used for data analysis, and the data were filtered by a 10-500 Hz low-pass filter.
Exercise protocol
For eight weeks, the experimental group engaged in walking and other activities on the sand. The program included jogging, striding, bounding, galloping, and short sprints. The group attended three sessions per week [28]. The exercise program was performed with bare feet. The start of each session included a 5-min warm-up and stretching, followed by a 5-min warm-up at the end [28]. The exercise duration was 50 min in each session [29]. A physiotherapist supervised each session to ensure proper technique and make necessary adjustments to the exercise program, including modifications or progressions. After the intervention, the experimental group was re-evaluated with the same strategies as the primary assessment. A check-up was planned for six days after the last exercise session to make sure that any immediate physiological responses to the exercise did not affect the measurements. The control group performed the same exercises at the futsal hall level and were re-evaluated after 8 weeks.
The normality of data distribution was assessed using the Shapiro-Wilk test. For statistical analysis, the two-way analysis of variance test was utilized. The SPSS software, version 26, was employed for all analyses.
Results
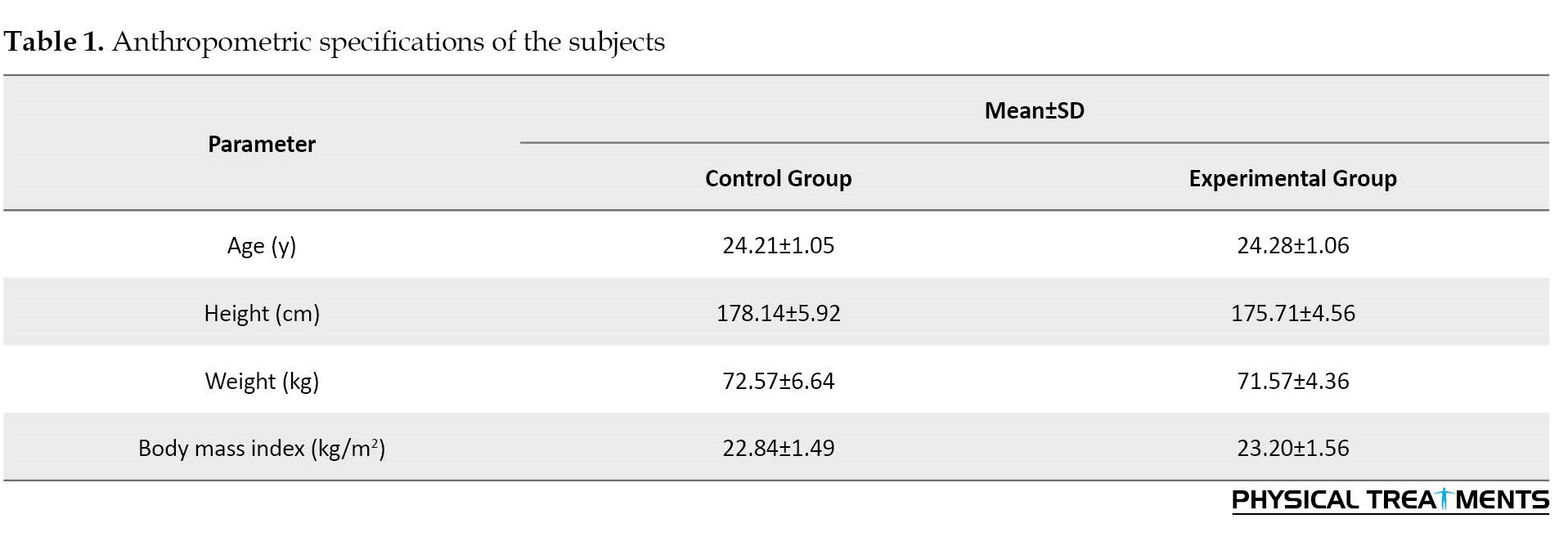
The anthropometric specifications are listed in Table 1.
The findings showed the main effect of time for the frequency content of the tibialis anterior, medial gastrocnemius, vastus medialis muscles during loading and push-off phases, the vastus lateralis muscle during the mid-stance, the rectus femoris at the mid-stance and push-off phases, semitendinosus muscle during the loading, mid-stance and push-off phases, biceps femoris muscle during the mid-stance and push-off phases, and gluteus medius muscle during the push-off phase (P<0.039, d=0.166-0.606; Table 2).
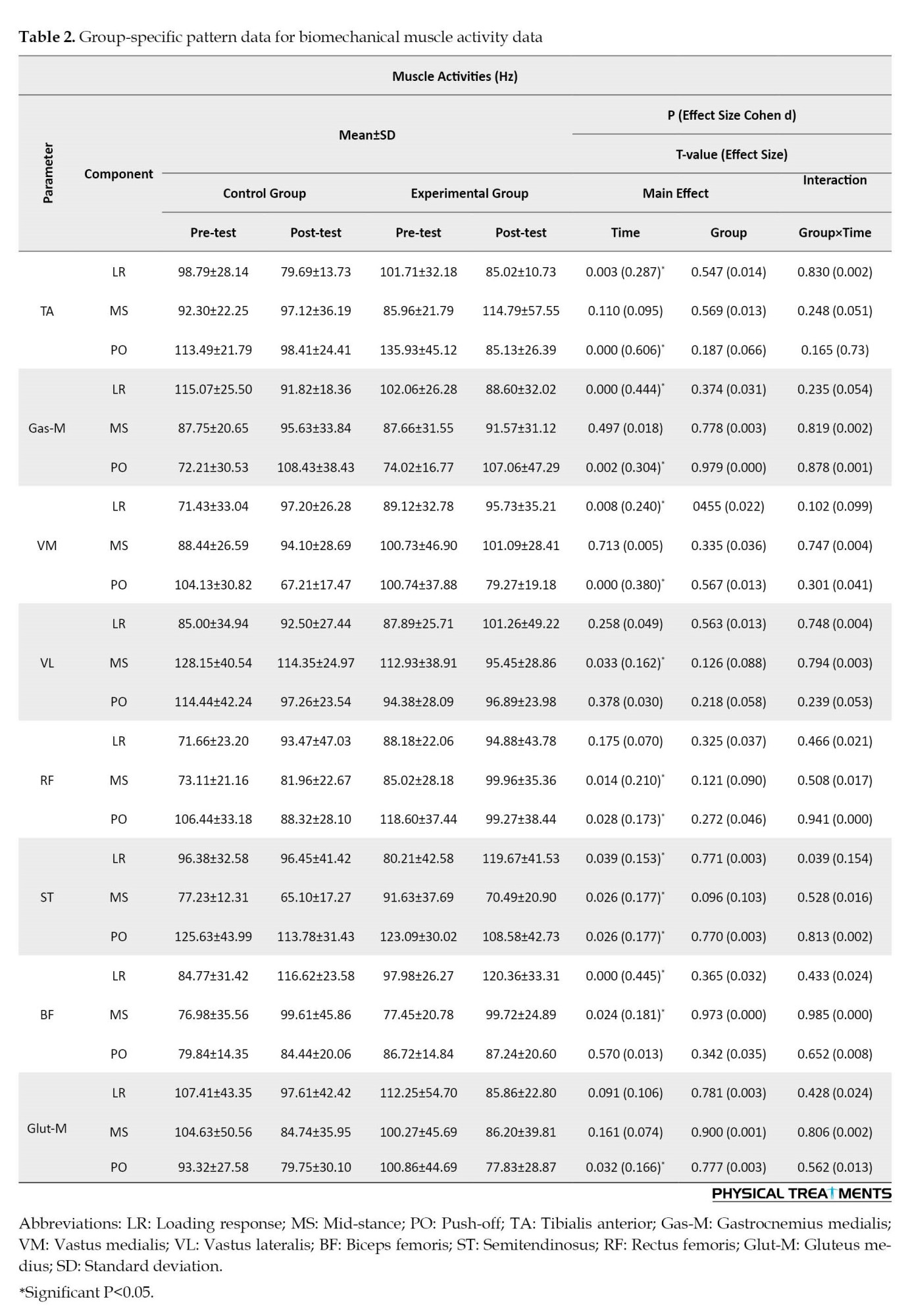
Significant group-by-time interactions were watched for semitendinosus (ST) activities during the loading phases (P=0.039, d=0.154; Table 2).
Discussion
This study determined the effect of exercises on the sand on the frequency content of electrical activity of the lower limb in people with anterior cruciate ligament injury and peroneal foot while walking. According to the findings, the frequency content of tibialis anterior muscle activity in the response phase of loading and pushing decreased in the post-test relative to the pre-test. In a study, Herbaut et al. (2017) investigated the efficacy of the lifespan of sports shoes on the biomechanical variables of children during running and showed the amount of ankle dorsiflexion in 41-62 and 88-100 (pushing). The percentage of the support phase was reduced when using used shoes; however, no significant difference was reported in the amount of ankle dorsiflexion and knee flexion during the two conditions of using new and used shoes, at the moment of heel contact [30]. Since the tibialis anterior muscle is the largest dorsiflexor muscle in the ankle area [31], the decrease in ankle dorsiflexion after the pushing phase test can lead to low activity of this muscle in this condition.
The findings of this study showed that exercises on the sand had a significant effect on the frequency content of the gastrocnemius medialis muscle during the push phase so the activity of this muscle increased after the test. The gastrocnemius medialis muscle is an anti-gravity muscle that plays an important role in walking [32]. This muscle is activated in the middle phase of support when bending the knee joint and its activity increases suddenly during the pushing phase, also in the early part of the swing phase when bending the knee joint to prevent the foot from hitting the ground [33]. People with genu-varum need more activity of the gastrocnemius medialis muscle compared to healthy people to maintain their posture because these people need more than healthy people to control the dynamic posture of the lower limb, which is the condition of the subtalar and midtarsal joints. Also, Madadi-Shad et al. (2020) reported that people with back pain compared to healthy people had less electrical activity in their gastrocnemius medialis muscle, which lower activity of this muscle caused a decrease in speed in these people [34]. Therefore, training on sand with an increase in the activity of the gastrocnemius medialis muscle has probably improved the control of the posture and increased the speed of people with pronation foot and anterior cruciate ligament reconstruction.
The findings of the research showed that during the response of loading and push-off, the amount of frequency content of the activity of the vastus medialis muscle during the pre-test and post-test was significant. Studies that have examined the electromyographic activity of the quadriceps muscle in the group with genu-varum have reported that there are changes in the activity of this muscle compared to healthy people, and during isometric and isokinetic contractions, the percentage of the motor neurons of the muscle is used. Four-headedness is more common in injured people than in healthy people [30]. Also, the effect of the group factor on the latissimus dorsi muscle showed a decrease in the activity frequency of this muscle during the mid-stance phase. In addition, the results showed that the frequency content of biceps muscle activity decreased after training compared to before it. Previous studies have shown that the co-contraction of the hamstring muscle group with the quadriceps muscle plays a major role in countering external varus and valgus forces on the knee. The biceps muscle counteracts the forces that enter the knee in the varus direction.
In people with hemiparesis, a common abnormality is stiff knee gait, in which the bending angle of the knee decreases during the swing phase due to hyperactivity of the right thigh. In these people, the amount of biceps muscle activity during walking is related to the increase in the knee bending angle [35]. In addition, the walking speed of people with strokes is related to the magnitude of the knee bending angle and its torque during walking [36, 37]. It is possible that training on the sand by increasing the activity of the quadriceps muscles and reducing the activity of the existing hamstring muscles has improved the walking speed of the studied subjects.
The findings showed that the interactive effect of time and group on the activity frequency of the semitendinosus muscle in the loading response phase has a statistically significant difference. Since the group of hamstring muscles is the antagonists of the anterior cruciate ligament, weakness in the activity of these muscles will be the cause of the injury of the anterior cruciate ligament [31]. Also, in addition to playing a role in bending the knee and facilitating the rotation of the tibia on the thigh, the semitendinosus muscle is responsible for ensuring the internal stability of the knee, and its weakness reduces the stability of the inner side of the knee [38]. Therefore, the 46.41% increase in the activity of the frequency content of the semitendinosus muscle after training on sand can probably be useful for the injury of people with anterior cruciate ligament reconstruction and reduce the burden on it. It is critical to recognize the limitations of this study. Primarily, the study only included male participants, therefore, the outcomes cannot be generalized to females. Moreover, kinematic data was not collected during the study. To better understand the impact of walking mileage on walking mechanics, future studies should analyze both kinematic and kinetic data.
Conclusion
According to the outcome obtained in this study, the frequency content of the electrical activity of the gastrocnemius medialis, vastus medialis, and rectus femoris muscles increased, and the frequency content of the electrical activity of the tibialis anterior, vastus lateralis, biceps femoris, and gluteus medius muscles decreased. Accordingly, training on sand can probably increase walking speed by reducing pain and increasing postural stability, and overall improve walking in people with anterior cruciate ligament injury.
Ethical Considerations
Compliance with ethical guidelines
The Ethics Committee affirmed the research protocol of Baqiyatallah University of Medical Sciences (Code: IR.BMSU.BAQ.REQ.1399.050). The research protocol of this study has been enrolled in the Iran Clinical Trial Organization (IRCT) (ID: IRCT20200912048696N1). Consent forms for taking part were signed by all of the informed individuals participating in the study.
Funding
This research did not get any grant from financing organizations within the public, commercial, or non-profit segments.
Authors' contributions
Conceptualization and writing the original draft: Hamed Sheikhalizade; Methodology: All authors; Supervision, review and editing: AmirAli Jafarnezhadgero.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank the participants in this research for their autonomic participation.
References
The skeletal-muscular system of the human body is an interconnected set and changes in any part of it can affect other parts and cause problems in basic motor skills, such as walking [1, 2]. Walking activity is one of the main tasks of the lower body, by performing various actions, such as absorbing, the forces resulting from the impact of the foot on the ground, maintaining balance, and producing forward forces, plays an essential role in creating an integrated and properly coordinated pattern of walking [2-4]. A previous study has shown that natural walking requires neurally controlled commands, force generation by the muscles, and a specific range of motion for each case. This means that if it occurs in any of these cases, it can cause abnormal walking [5]. Abnormal walking causes various complications in the lower limbs—one of the factors that may cause injury while walking is foot pronation [6].
Pronation of the foot involves the reduction of the medial longitudinal arch along with the navicular bone on the medial surface of the foot, which can cause anatomical abnormalities [7]. This devaluation in the height of the internal longitudinal arch depends on the condition of the plantar bones and ligaments, leg and foot muscles, and plays an important role in maintaining balance and performing movement abilities and skills [7]. Foot pronation is a combination of heel eversion, foot abduction, and ankle dorsiflexion, which occurs in the subtalar and midtarsal joints and affects the longitudinal-internal arch of the foot [8, 9]. These additional movements caused the lack of shock absorption in these joints during transition movements [8, 9]. Excessive pronation during the support phase of walking leads to increased flexibility and, thus bringing instability of the subtalar and midtarsal joints [8, 9]. People with overpronation suffer from many biomechanical inefficiencies in the foot and ankle [10]. Foot pronation can cause biomechanical irregularities in a person’s performance, which also leads to Achilles tendon pain, leg pain, hamstring strain, and quadriceps muscle strain [11]; therefore, the pronated foot leads to impaired posture control, impaired absorption of pressures on the soles of the feet, the occurrence of lower limb injuries, and changes in the mobility of the ankle and foot joints, which, secondarily, probably causes changes in the electrical activity of the muscles [12-15]. Therefore, in addition to the changes in the standing position, the abnormalities of this part also affect the movement [7]. Overpronation of the foot is considered a major contributing factor in lower limb injuries [16]. It has been reported that between 0.6% and 8.5% of male players experience an injury to a ligament called the anterior cruciate ligament each year [9]. Knee injuries account for approximately 61% of sports injuries [17]. The pronation of the foot and internal rotation of the tibia are coupled with each other and create torsional forces [16]. This torsional stress may lead to ligament tears or dislocation-induced fractures [16]. The compensatory mechanism caused by muscle weakness in some other muscles can cause a disturbance in the ratio of muscle forces and then cause changes in the movement pattern [2].
In pronation, the fibularis, gastrocnemius medialis, soleus, iliotibial band, hamstrings, hip adductors, and iliopsoas muscles become functionally short (overactive), and the posterior and posterior and anterior calf muscles, vastus medialis, gluteus medius, and maximus, external rotators of the hip are inhibited [18, 19]. Evidence suggests that individuals with foot pronation exhibit increased levels of muscle electrical activity in certain muscles that are involved in the ankle joint, such as the tibialis posterior and anterior, dorsi flexors, and plantar flexors while displaying decreased levels of electrical activity in the evertor muscles, specifically the peroneus muscle [14, 20-22]. It seems logical that the change in the electrical activity of the muscles leads to a change in the function of the muscles and a decrease in their efficiency [2]. Effective rehabilitation programs for foot and ankle injuries have been successful in clinical trials, and programs focus on exercise therapy to improve joint range of motion, muscle strength, neuromuscular coordination, and gait mechanics [23].
Sand exercises can be included during treatment because they are free of cost and accessible to many people worldwide [24]. More importantly, training on the sand, which is an unstable and unpredictable surface, can have a positive effect on the biomechanics of human movement [24]. Greater electrical activity has been observed in muscles, such as gastrocnemius medialis, hamstrings (semi-membranous and biceps femoris), vastus lateralis and vastus medialis, rectus femoris, and the iliotibial band when running on sand compared to running on a hard surface [25]. Another study showed that due to the decrease in the elastic energy of the surface, more muscles are greater active while walking on sand surfaces [26]. An interventional study investigated the effect of eight weeks of exercise on the sand on walking kinetics and muscle activities in patients with pronated feet [24]. They observed lower vertical and lateral peak forces and increased electrical activity of lower limb muscles (e.g. vastus lateralis) after exercise. Accordingly, walking and running exercises on sand are recommended as an effective therapy for people with pronated feet.
To the authors’ knowledge, no study is available that examines the effects of walking on sand on the frequency content of electrical activity in subjects with anterior cruciate ligament injuries and pronated feet during walking. Therefore, this study determines the effect of exercises on the sand on the frequency content of electrical activity in people with anterior cruciate ligament injuries and pronated feet during walking.
Materials and Methods
This was a semi-experimental and laboratory-type study. The statistical sample size of the present study was 28 people (n=14 in each group). The statistical power of 0.8 was estimated at the significance level of 0.05 in the G*Power software. The statistical population of this research was males with the age range of 22 to 25 years who voluntarily participated in this research. The inclusion criteria were male gender, age range between 22 to 25 years, and at least a history of anterior cruciate ligament reconstruction for 6 months, anterior cruciate ligament reconstruction in one leg, having a pronated foot, passed six months after surgery, and ability to walk independently. The exclusion criteria were having a history of surgery or orthopedic disorders (except for anterior cruciate ligament reconstruction), the difference in the lower limbs, and using any braces.
According to the medical records of the subjects, all the people who were placed in the anterior cruciate ligament reconstruction group had a complete anterior cruciate ligament tear that was operated by arthroscopic surgery, and these people also had pronation. During the call, only 28 subjects had the conditions to enter the research in the anterior cruciate ligament injury group, who were selected with available sampling. The subjects’ dominant leg was determined by the soccer ball shot test. All subjects were right-footed. After justifying the subjects and mentioning the ethical considerations of the research, as well as mentioning the tips and training that did not interfere in the process of conducting research and data collection, the person was asked to wear sports clothes to prevent injury, and before performing the test, perform the initial heating. Then, the subjects walked on a 15-m path. Next, the experimental group performed the exercise protocol for 8 weeks, during which the control group did not do any exercises. Once more, after the completion of 8 weeks, the information on the electrical activity of the muscles was recorded in the act of walking. To record electromyography signals, an electromyogram device (Biometric Ltd, Nine Mile Point Ind Est, Newport, UK) was used. Before the electrode placement, excess hair was shaved and the skin was cleaned with alcohol and medical cotton. The placement of surface electrodes for recording electrical signals on selected muscles (tibialis anterior, gastrocnemius medialis, vastus medialis, vastus lateralis, biceps femoris, rectus femoris, semitendinosus, and gluteus medius) was determined according to the SENIAM protocol [27]. Surface electromyography signals were recorded with a sampling rate of 1000 Hz. The Biometrics DataLITE program, version 3.1 was used for data analysis, and the data were filtered by a 10-500 Hz low-pass filter.
Exercise protocol
For eight weeks, the experimental group engaged in walking and other activities on the sand. The program included jogging, striding, bounding, galloping, and short sprints. The group attended three sessions per week [28]. The exercise program was performed with bare feet. The start of each session included a 5-min warm-up and stretching, followed by a 5-min warm-up at the end [28]. The exercise duration was 50 min in each session [29]. A physiotherapist supervised each session to ensure proper technique and make necessary adjustments to the exercise program, including modifications or progressions. After the intervention, the experimental group was re-evaluated with the same strategies as the primary assessment. A check-up was planned for six days after the last exercise session to make sure that any immediate physiological responses to the exercise did not affect the measurements. The control group performed the same exercises at the futsal hall level and were re-evaluated after 8 weeks.
The normality of data distribution was assessed using the Shapiro-Wilk test. For statistical analysis, the two-way analysis of variance test was utilized. The SPSS software, version 26, was employed for all analyses.
Results
The anthropometric specifications are listed in Table 1.
The findings showed the main effect of time for the frequency content of the tibialis anterior, medial gastrocnemius, vastus medialis muscles during loading and push-off phases, the vastus lateralis muscle during the mid-stance, the rectus femoris at the mid-stance and push-off phases, semitendinosus muscle during the loading, mid-stance and push-off phases, biceps femoris muscle during the mid-stance and push-off phases, and gluteus medius muscle during the push-off phase (P<0.039, d=0.166-0.606; Table 2).
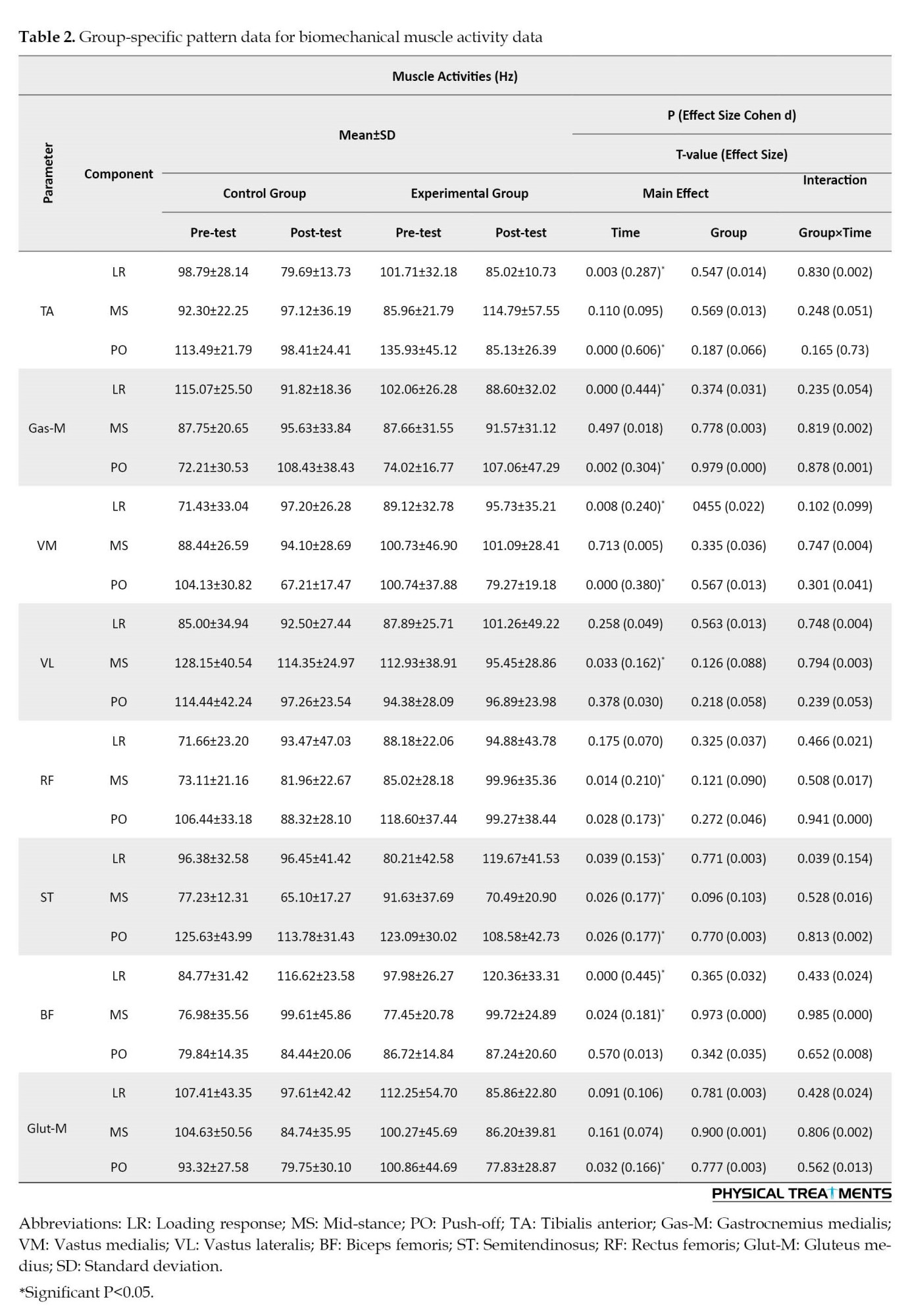
Significant group-by-time interactions were watched for semitendinosus (ST) activities during the loading phases (P=0.039, d=0.154; Table 2).
Discussion
This study determined the effect of exercises on the sand on the frequency content of electrical activity of the lower limb in people with anterior cruciate ligament injury and peroneal foot while walking. According to the findings, the frequency content of tibialis anterior muscle activity in the response phase of loading and pushing decreased in the post-test relative to the pre-test. In a study, Herbaut et al. (2017) investigated the efficacy of the lifespan of sports shoes on the biomechanical variables of children during running and showed the amount of ankle dorsiflexion in 41-62 and 88-100 (pushing). The percentage of the support phase was reduced when using used shoes; however, no significant difference was reported in the amount of ankle dorsiflexion and knee flexion during the two conditions of using new and used shoes, at the moment of heel contact [30]. Since the tibialis anterior muscle is the largest dorsiflexor muscle in the ankle area [31], the decrease in ankle dorsiflexion after the pushing phase test can lead to low activity of this muscle in this condition.
The findings of this study showed that exercises on the sand had a significant effect on the frequency content of the gastrocnemius medialis muscle during the push phase so the activity of this muscle increased after the test. The gastrocnemius medialis muscle is an anti-gravity muscle that plays an important role in walking [32]. This muscle is activated in the middle phase of support when bending the knee joint and its activity increases suddenly during the pushing phase, also in the early part of the swing phase when bending the knee joint to prevent the foot from hitting the ground [33]. People with genu-varum need more activity of the gastrocnemius medialis muscle compared to healthy people to maintain their posture because these people need more than healthy people to control the dynamic posture of the lower limb, which is the condition of the subtalar and midtarsal joints. Also, Madadi-Shad et al. (2020) reported that people with back pain compared to healthy people had less electrical activity in their gastrocnemius medialis muscle, which lower activity of this muscle caused a decrease in speed in these people [34]. Therefore, training on sand with an increase in the activity of the gastrocnemius medialis muscle has probably improved the control of the posture and increased the speed of people with pronation foot and anterior cruciate ligament reconstruction.
The findings of the research showed that during the response of loading and push-off, the amount of frequency content of the activity of the vastus medialis muscle during the pre-test and post-test was significant. Studies that have examined the electromyographic activity of the quadriceps muscle in the group with genu-varum have reported that there are changes in the activity of this muscle compared to healthy people, and during isometric and isokinetic contractions, the percentage of the motor neurons of the muscle is used. Four-headedness is more common in injured people than in healthy people [30]. Also, the effect of the group factor on the latissimus dorsi muscle showed a decrease in the activity frequency of this muscle during the mid-stance phase. In addition, the results showed that the frequency content of biceps muscle activity decreased after training compared to before it. Previous studies have shown that the co-contraction of the hamstring muscle group with the quadriceps muscle plays a major role in countering external varus and valgus forces on the knee. The biceps muscle counteracts the forces that enter the knee in the varus direction.
In people with hemiparesis, a common abnormality is stiff knee gait, in which the bending angle of the knee decreases during the swing phase due to hyperactivity of the right thigh. In these people, the amount of biceps muscle activity during walking is related to the increase in the knee bending angle [35]. In addition, the walking speed of people with strokes is related to the magnitude of the knee bending angle and its torque during walking [36, 37]. It is possible that training on the sand by increasing the activity of the quadriceps muscles and reducing the activity of the existing hamstring muscles has improved the walking speed of the studied subjects.
The findings showed that the interactive effect of time and group on the activity frequency of the semitendinosus muscle in the loading response phase has a statistically significant difference. Since the group of hamstring muscles is the antagonists of the anterior cruciate ligament, weakness in the activity of these muscles will be the cause of the injury of the anterior cruciate ligament [31]. Also, in addition to playing a role in bending the knee and facilitating the rotation of the tibia on the thigh, the semitendinosus muscle is responsible for ensuring the internal stability of the knee, and its weakness reduces the stability of the inner side of the knee [38]. Therefore, the 46.41% increase in the activity of the frequency content of the semitendinosus muscle after training on sand can probably be useful for the injury of people with anterior cruciate ligament reconstruction and reduce the burden on it. It is critical to recognize the limitations of this study. Primarily, the study only included male participants, therefore, the outcomes cannot be generalized to females. Moreover, kinematic data was not collected during the study. To better understand the impact of walking mileage on walking mechanics, future studies should analyze both kinematic and kinetic data.
Conclusion
According to the outcome obtained in this study, the frequency content of the electrical activity of the gastrocnemius medialis, vastus medialis, and rectus femoris muscles increased, and the frequency content of the electrical activity of the tibialis anterior, vastus lateralis, biceps femoris, and gluteus medius muscles decreased. Accordingly, training on sand can probably increase walking speed by reducing pain and increasing postural stability, and overall improve walking in people with anterior cruciate ligament injury.
Ethical Considerations
Compliance with ethical guidelines
The Ethics Committee affirmed the research protocol of Baqiyatallah University of Medical Sciences (Code: IR.BMSU.BAQ.REQ.1399.050). The research protocol of this study has been enrolled in the Iran Clinical Trial Organization (IRCT) (ID: IRCT20200912048696N1). Consent forms for taking part were signed by all of the informed individuals participating in the study.
Funding
This research did not get any grant from financing organizations within the public, commercial, or non-profit segments.
Authors' contributions
Conceptualization and writing the original draft: Hamed Sheikhalizade; Methodology: All authors; Supervision, review and editing: AmirAli Jafarnezhadgero.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank the participants in this research for their autonomic participation.
References
- Ledoux WR, Hillstrom HJ. The distributed plantar vertical force of neutrally aligned and pes planus feet. Gait & Posture. 2002; 15(1):1-9. [DOI:10.1016/S0966-6362(01)00165-5] [PMID]
- Tajdini kakavandi H, Sadeghi H, Abasi A. [Investigating ground reaction forces and electromyography muscle activity of lower extremity during the stance phase of walking in active male with and without genu varum deformity in kharazmi university in 2017: A descriptive study (Persian)]. Journal of Rafsanjan University of Medical Sciences. 2019; 18(7):675-88. [Link]
- Maiwald C, Arndt A, Nester C, Jones R, Lundberg A, Wolf P. The effect of intracortical bone pin application on kinetics and tibiocalcaneal kinematics of walking gait. Gait & Posture. 2017; 52:129-34. [DOI:10.1016/j.gaitpost.2016.10.023] [PMID]
- Rethlefsen SA, Blumstein G, Kay RM, Dorey F, Wren TA. Prevalence of specific gait abnormalities in children with cerebral palsy revisited: Influence of age, prior surgery, and Gross Motor Function Classification System level. Developmental Medicine & Child Neurology. 2017; 59(1):79-88. [DOI:10.1111/dmcn.13205] [PMID]
- Fasihi A, Siahkouhian M, Sheikhalizade H, Jafarnezhadgero A. Effect of fatigue at the heart rate deflection point on the frequency components of ground reaction forces during walking in individuals with pronated feet. The Scientific Journal of Rehabilitation Medicine. 2020; 9(2):228-38. [DOI:10.22037/jrm.2019.111901.2122]
- Piri E, Farzizade R, Barghamadi M. The effect of exercises in water and thera-band on the frequency spectrum of ground reaction forces in people with pronate foot during walking: A clinical triaL. Studies in Medical Sciences. 2022; 33(8):621-33. [DOI:10.52547/umj.33.8.621]
- Mantashloo Z, Sadeghi H, Khaleghi Tazji M. [Comparison of ground reaction forces and muscles electrical activity of the ankle during running in young men with pronation and normal foot (Persian)]. Journal of Rafsanjan University of Medical Sciences. 2017; 16(4):353-64. [Link]
- Valizade Orang A, Siahkoohian M, Jafarnezhadgero A, Jafarnezhadgero F. The effect of long-term use of motion control shoes on the ground reaction force components during running in runners with excessive pronated feet. Iranian Journal of Rehabilitation Research in Nursing. 2019; 6(2):48-55. [Link]
- Valizade-Orang A, Siahkoohian M, Jafarnezhadgero A, Bolboli L, Ghorbanlou F. [Investigating the effects of long-term use of motion control shoes on the frequency spectrum of ground reaction force during running in the runners with pronated feet (Persian)]. The Scientific Journal of Rehabilitation Medicine. 2020; 8(4):123-31. [DOI:10.22037/jrm.2019.111504.2040]
- Lee MS, Vanore JV, Thomas JL, Catanzariti AR, Kogler G, Kravitz SR, et al. Diagnosis and treatment of adult flatfoot. The Journal of Foot and Ankle Surgery. 2005; 44(2):78-113. [DOI:10.1053/j.jfas.2004.12.001] [PMID]
- Menz HB, Morris ME, Lord SR. Foot and ankle characteristics associated with impaired balance and functional ability in older people. The Journals of Gerontology. Series A: Biological Sciences and Medical Sciences. 2005; 60(12):1546-52. [DOI:10.1093/gerona/60.12.1546] [PMID]
- Williams DS 3rd, McClay IS, Hamill J. Arch structure and injury patterns in runners. Clinical Biomechanics. 2001; 16(4):341-7. [DOI:10.1016/S0268-0033(01)00005-5] [PMID]
- Dahle LK, Mueller M, Delitto A, Diamond JE. Visual assessment of foot type and relationship of foot type to lower extremity injury. Journal of Orthopaedic & Sports Physical Therapy. 1991; 14(2):70-4. [DOI:10.2519/jospt.1991.14.2.70] [PMID]
- Hunt AE, Smith RM. Mechanics and control of the flat versus normal foot during the stance phase of walking. Clinical Biomechanics (Bristol, Avon). 2004; 19(4):391-7. [DOI:10.1016/j.clinbiomech.2003.12.010] [PMID]
- Cote KP, Brunet ME, Gansneder BM, Shultz SJ. Effects of pronated and supinated foot postures on static and dynamic postural stability. Journal of Athletic Training. 2005; 40(1):41. [PMID]
- Mokhtari Malekabadi A, Jafarnezhadgero A, Gghorbanlou F. The effects of changing footstrike pattern on the amplitude and frequency spectrum of ground reaction forces during running in individuals with pronated feet. Physical Treatments-Specific Physical Therapy Journal. 2020; 10(4):205-12. [DOI:10.32598/ptj.10.4.348.2]
- Valizadeorang A, Ghorbanlou F, Jafarnezhadgero A, Alipoor Sarinasilou M. [Effect of knee brace on frequency spectrum of ground reaction forces during landing from two heights of 30 and 50 cm in athletes with anterior cruciate ligament injury (Persian)]. The Scientific Journal of Rehabilitation Medicine. 2019; 8(2):159-68. [DOI:10.22037/jrm.2018.111377.1950]
- Golchini A, Rahnama N. Effect of 12-week corrective exercises on postural sways in male students with pronation distortion syndrome. Research in Sport Medicine and Technology. 2020; 18:127-45. [DOI:10.32598/irj.18.2.937.1]
- Golchini A, Rahnama N. The effects of 12 weeks of systematic and functional corrective exercises on body posture of students suffering from pronation distortion syndrome. Iranian Rehabilitation Journal. 2020; 18(2):181-92. [DOI:10.32598/irj.18.2.937.1]
- Murley GS, Landorf KB, Menz HB, Bird AR. Effect of foot posture, foot orthoses and footwear on lower limb muscle activity during walking and running: A systematic review. Gait & Posture. 2009; 29(2):172-87. [DOI:10.1016/j.gaitpost.2008.08.015] [PMID]
- Gray EG, Basmajian JV. Electromyography and cinematography of leg and foot (“normal” and flat) during walking. The Anatomical Record. 1968; 161(1):1-15. [DOI:10.1002/ar.1091610101] [PMID]
- Jafarnezhadgero A, Fatollahi A, Sheykholeslami A, Dionisio VC, Akrami M. Long-term training on sand changes lower limb muscle activities during running in runners with over-pronated feet. Biomedical Engineering Online. 2021; 20(1):118. [DOI:10.1186/s12938-021-00955-8] [PMID]
- Chinn L, Hertel J. Rehabilitation of ankle and foot injuries in athletes. Clinics in Sports Medicine. 2010; 29(1):157-67. [DOI:10.1016/j.csm.2009.09.006] [PMID]
- Jafarnezhadgero AA, Fatollahi A, Granacher U. Eight weeks of exercising on sand has positive effects on biomechanics of walking and muscle activities in individuals with pronated feet: A randomized double-blinded controlled trial. Sports (Basel, Switzerland). 2022; 10(5):70. [DOI:10.3390/sports10050070] [PMID]
- Pinnington HC, Lloyd DG, Besier TF, Dawson B. Kinematic and electromyography analysis of submaximal differences running on a firm surface compared with soft, dry sand. European Journal of Applied Physiology. 2005; 94:242-53. [DOI:10.1007/s00421-005-1323-6] [PMID]
- Zamparo P, Perini R, Orizio C, Sacher M, Ferretti G. The energy cost of walking or running on sand. European Journal of Applied Physiology and Occupational Physiology. 1992; 65(2):183-7. [DOI:10.1007/BF00705078] [PMID]
- Farahpour N, Jafarnezhadgero A, Allard P, Majlesi M. Muscle activity and kinetics of lower limbs during walking in pronated feet individuals with and without low back pain. Journal of Electromyography and Kinesiology: Official Journal of the International Society of Electrophysiological Kinesiology. 2018; 39:35-41. [DOI:10.1016/j.jelekin.2018.01.006] [PMID]
- Durai DB, Shaju MF. Effect of sand running training on speed among school boys. International Journal of Physical Education, Sports and Health. 2019; 6(3):117-22. [Link]
- Anderson M, Barnum M. Foundations of athletic training: Prevention, assessment, and management. Philadelphia: Lippincott Williams & Wilkins; 2021. [Link]
- Herbaut A, Chavet P, Roux M, Guéguen N, Barbier F, Simoneau-Buessinger E. The influence of shoe aging on children running biomechanics. Gait & Posture. 2017; 56:123-8. [DOI:10.1016/j.gaitpost.2017.05.011] [PMID]
- Gellert C. Course title: Human movement matrix: Shoulder [internet]. 2016 [Updated 2024 May]. Available from: [Link]
- Namavarian N, Rezasoltani A, Rekabizadeh M. [A study on the function of the knee muscles in genu varum and genu valgum (Persian)]. Modern Rehabilitation. 2014; 8(3):19. [Link]
- Kakavandi HT, Sadeghi H, Abbasi A. The effects of genu varum deformity on the pattern and amount of Electromyography muscle activity lower extremity during the stance phase of walking. Journal of Clinical Physiotherapy Research. 2017; 2(3):110-8. [DOI:10.22037/jcpr.v2i3.17703]
- Madadi-Shad M, Jafarnezhadgero AA, Sheikhalizade H, Dionisio VC. Effect of a corrective exercise program on gait kinetics and muscle activities in older adults with both low back pain and pronated feet: A double-blind, randomized controlled trial. Gait & Posture. 2020; 76:339-45. [DOI:10.1016/j.gaitpost.2019.12.026] [PMID]
- Fujita K, Hori H, Kobayashi Y. Contribution of muscle activity at different gait phases for improving walking performance in chronic stroke patients with hemiparesis. Journal of physical therapy science. 2018; 30(11):1381-5. [DOI:10.1589/jpts.30.1381] [PMID]
- Olney SJ, Griffin MP, McBride ID. Temporal, kinematic, and kinetic variables related to gait speed in subjects with hemiplegia: A regression approach. Physical Therapy. 1994; 74(9):872-85. [DOI:10.1093/ptj/74.9.872] [PMID]
- Kim CM, Eng JJ. The relationship of lower-extremity muscle torque to locomotor performance in people with stroke. Physical Therapy. 2003; 83(1):49-57. [DOI:10.1093/ptj/83.1.49]
- Jafarnezhadgero AA, Anvari SM, Valizade Orang A. [Influence of sport shoe ageing on frequency domain of lower limb muscles in individuals with genu varum and healthy group during walking (Persian)]. Iranian Journal of Rehabilitation Research. 2020; 6(3):25-33. [Link]
Type of Study: Research |
Subject:
General
Received: 2023/08/9 | Accepted: 2024/01/29 | Published: 2024/04/1
Received: 2023/08/9 | Accepted: 2024/01/29 | Published: 2024/04/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |