Mon, Jan 5, 2026
Volume 13, Issue 4 (Autumn 2023)
PTJ 2023, 13(4): 245-252 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mazidavi A, Karimi N, Khorasani B, Baraghoosh P, Biglarian A. Effects of Muscle Energy Technique on Pain and Range of Motion in Chronic Low Back Pain Subjects with Lateral Flexion Restriction. PTJ 2023; 13 (4) :245-252
URL: http://ptj.uswr.ac.ir/article-1-583-en.html
URL: http://ptj.uswr.ac.ir/article-1-583-en.html
1- Department of Physiotherapy, Faculty of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Clinical Sciences, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
3- Department of Biostatistics and Epidemiology, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Clinical Sciences, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
3- Department of Biostatistics and Epidemiology, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
Keywords: Chronic low back pain, Lateral flexion, Muscle energy technique, Quadratus lumborum muscle, Manual therapy, Randomized clinical trial
Full-Text [PDF 526 kb]
(1501 Downloads)
| Abstract (HTML) (3384 Views)
Full-Text: (1812 Views)
1. Introduction
Low back pain (LBP) is one of the most common musculoskeletal problems [1, 2], and the leading cause of activity limitation and absenteeism [3]. Sixty to eighty percent of LBP patients report pain or disability a year later, and up to 40% report chronic pain [4, 5]. The impact of LBP on individuals and society, including pain, disability, and associated diagnostic and treatment costs, underscores the importance of prevention and effective treatment [6]. Various factors contribute to the development of chronic LBP. Physical factors, such as reduced muscle strength and endurance are prognostic factors for chronic LBP. The strength and endurance of the trunk muscles play a crucial role in reducing pain, enhancing stability, and maintaining spinal function [7, 8]. Chronic LBP has been associated with changes in trunk muscle responses and increased muscle fatigability [9]. Patients with chronic LBP and healthy individuals experiencing fatigue may utilize similar neuromuscular strategies to protect the spine, which can lead to back injuries. Delayed activation and higher levels of muscle activity have been associated with LBP [9]. Quadratus lumborum (QL) is a deep trunk muscle, and its tightness can trigger symptoms of significant low back tightness and discomfort [10]. Various treatments have been proposed for alleviating LBP, such as stretching exercises [11], heat therapy [12], massage therapy [13], proprioceptive neuromuscular facilitation [14], myofascial release [15], and muscle energy technique (MET) [16].
MET is a manual therapy that utilizes gentle muscle contractions of the patient to relax muscles, lengthen them, and restore normal joint motion [17, 18]. This technique was pioneered in 1948 by Fred Mitchell, Doctor of Osteopathic Medicine, to enhance musculoskeletal function by mobilizing joints and stretching tight muscles and fascia. Its primary aims are pain reduction, improved circulation, and enhanced lymphatic drainage [19]. MET operates based on the principle of reciprocal inhibition, which suggests that when indirect pressure is applied, muscles on one side of a joint will relax in response to the contraction of muscles on the opposite side [18]. The objective of MET is to promote muscle relaxation and lengthening, consequently enhancing joint range of motion (ROM). It is generally recognized as a gentle manual therapy technique for addressing limited motion in the spine and extremities [20]. MET is commonly applied to patients experiencing muscle spasms, as the process of lengthening shortened or spastic muscles can lead to improved ligament function. This technique involves alternating intervals of resisted muscle contractions and assisted stretching, collectively working to alleviate limitations in muscular activity [20]. Numerous studies have explored the impact of MET on lower back pain (LBP). MET might be a valuable approach for reducing non-specific lumbopelvic pain (LPP) over 24 hours [20]. Several studies have investigated the effects of MET on LBP, with one study proposing that MET could be a beneficial method for reducing non-specific lumbopelvic pain within a 24-hour timeframe [20]. Another study discovered that when combined with supervised motor control and resistance exercises, MET may be more effective in reducing disability and enhancing function in patients with acute LBP compared to neuromuscular re-education and resistance training [21]. Sharma et al. investigated the effects of MET on pain and disability in subjects with SI joint dysfunction. Their findings revealed that both MET and mobilization are effective in treating chronic LBP caused by sacroiliac joint dysfunction [22]. Patil et al. investigated the effectiveness of MET in QL in acute LBP. The findings suggested that MET combined with interferential therapy could be an effective treatment option for patients with acute LBP [23]. A review article suggested that the MET procedure can be effective in the management of chronic mechanical LBP [24]. However, there remains a lack of research on its clinical benefits and specific impact on the QL muscle in terms of reducing pain intensity and increasing spinal ROM. Therefore, the purpose of this research was to investigate the effect of MET on QL muscle regarding pain and lumbar ROM in patients suffering from chronic LBP characterized by restricted lateral movement. The hypothesis was that MET can improve pain and lumbar ROM in chronic LBP subjects with restricted lateral movement.
2. Materials and Methods
Source of data
The data were collected from the physiotherapy department of Milad Hospital in Tehran, Iran, from 2018 to 2019.
Subjects
This study was a single-blind randomized clinical trial. The sample included both male and female participants (a heterogeneous group) clinically diagnosed with chronic LBP with lateral flexion restriction and referred to the physiotherapy outpatient department of Milad Hospital for physiotherapy treatment. With a 90% Cl, 90% statistical power, and considering a 20% dropout rate, it was determined that each group would require 54 participants.
Inclusion criteria
1) Age range of 20 to 50 years; 2) Both male and female individuals with a clinical diagnosis of non-specific chronic LBP; 3) Participants experiencing lumbar pain and discomfort at the attachment points of the QL, specifically the iliac crest and lower ribs; 4) Individuals with limited unilateral flexion; 5) Participants willing to take part in the study; 6) Individuals who have not undergone physiotherapy within the past three months
Exclusion criteria
1) Participants with specific causes of LBP, such as intervertebral disc prolapse with instability, radicular symptoms, lumbar spondylosis, spondylolisthesis, lumbar canal stenosis, malignancies, and sensory deficits; 2) Participants with conditions, like osteoporosis, kidney and gastrointestinal disorders, and psychiatric issues as self-reported by the patients; 3) Individuals with a history of spinal surgery or spinal fractures; 4) Participants with differences in leg length (measured using the tape measurement method) [25]
Procedure
The study recruited participants with chronic LBP who were referred to the physiotherapy outpatient department and screened for suitability based on inclusion and exclusion criteria. Those willing to participate signed an informed consent form, and their demographic data were collected, along with their initial assessment of pain intensity and ROM of the lumbar spine. Pain intensity was assessed using a 100-mm visual analog scale (VAS) for back pain before and after treatment. Participants were instructed to mark a point on a 10 cm line to indicate the intensity of their pain, where zero represented the absence of pain, and ten indicated the most severe pain imaginable [26]. A standard plastic goniometer was used to measure the ROM of the lumbar lateral flexion angle before and after treatment. Each measurement was repeated three times to allow for the evaluation of intratester reliability. The examiner palpated and marked bony landmarks (the spinous process of the S1 vertebra and the spinous process of the C7 vertebra) for goniometer alignment in a standing erect position. The stationary arm was aligned vertically, the axis was set at the S1 spinous process, and the moving arm was aligned with the C7 spinous process. By using a random number table [27], 102 participants were randomly allocated to two groups of 51: Control and intervention. The control group received conventional physiotherapy, while the intervention group received MET using Chaitow’s method of post-isometric relaxation in addition to conventional physiotherapy [28].
Conventional physiotherapy
The patients allocated to the conventional physiotherapy group were provided with a combination of methods, including the application of a hot pack (10 minutes), and transcutaneous electrical nerve stimulation (TENS) (frequency: 2Hz and pulse duration: 200 μs; 20 minutes). The physiotherapist applied these methods to the patients in three sessions during a week. All participants received conventional physiotherapy lasting for 0.5 hours.
MET procedure
The intervention group received additional isometric contraction using post-isometric relaxation as part of MET [28]. This was achieved by holding the contraction for 5 seconds, followed by a 5-second rest period, and repeating this process three times during each session on the restricted side. The sessions were held three times in one week. The procedure was conducted with the therapist standing behind the side-lying patient. The patient abducted the uppermost leg until the therapist could palpate QL activity. Then, the patient was instructed to hold the leg with a mild degree of force (<20% of available strength) isometrically. After 5 seconds of contraction, the patient allowed the leg to hang slightly behind them. Then, the patient completely relaxed for 5 seconds. The therapist then passively moved to a new restricted barrier and held the stretch for 30 minutes.
Statistical analysis
Analyses were conducted on subjects who completed the entire process. Statistical tests were performed using IBM SPSS software, version 22. Central tendency and dispersion indices were employed to describe both qualitative and quantitative variables. The Kolmogorov-Smirnov test was employed to evaluate the normality of the data distribution. An analysis of covariance (ANCOVA) was employed to assess the effect of MET on pain and ROM. A significance level of 0.05 was adopted for all statistical tests.
3. Results
Initially, there were 108 patients enrolled in the study, but two patients were excluded because they did not meet the inclusion criteria, and four patients voluntarily withdrew from the study, resulting in a final sample size of 102 patients. These patients were randomly divided into the control (n=51) and intervention (n=51) groups using a table of random numbers. In the intervention group, five patients did not complete the treatment, and the remaining 46 patients were analyzed. The mean age of the patients was 37.74±7.07 years in the control group and 39.87±6.3 years in the intervention group (Table 1).
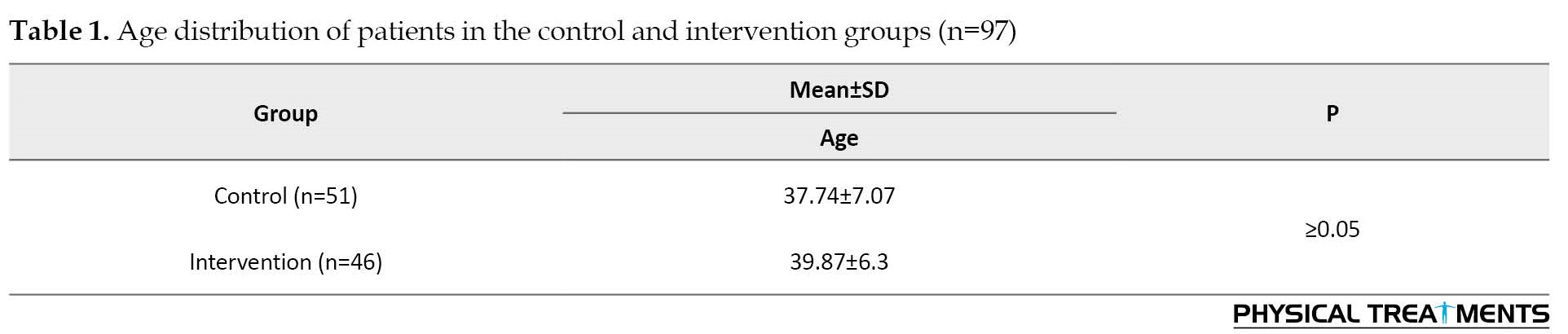
The Kolmogorov-Smirnov test results revealed that all variables examined in the study followed a normal distribution. A comparison of the background variables before the treatment revealed no significant differences between the two groups according to the distribution of their age and gender (P≥0.05) (Tables 1 and 2).
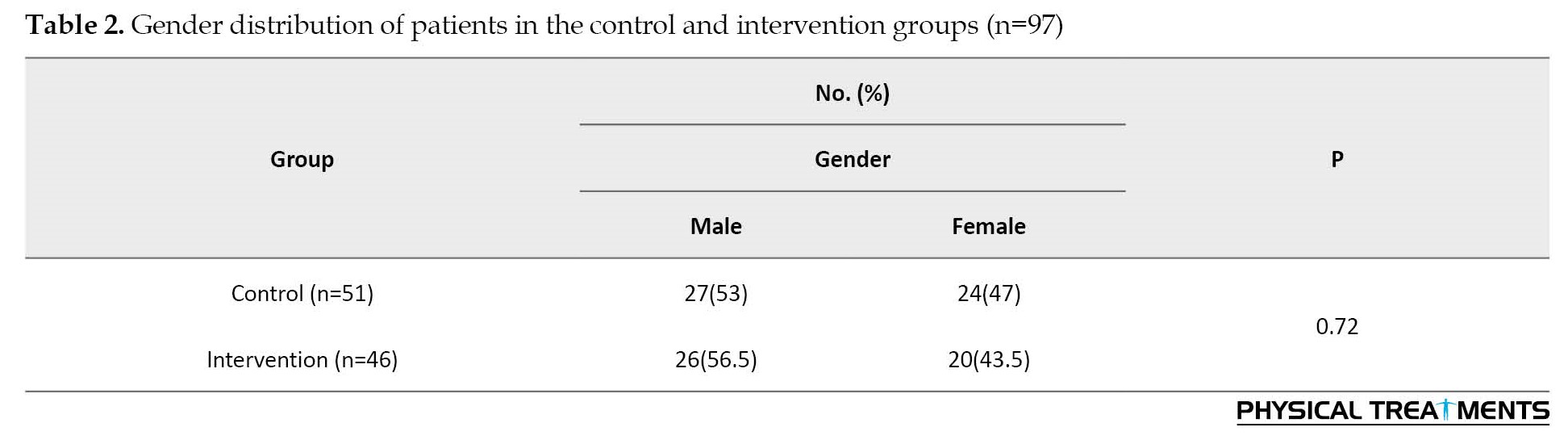
In the control group, among 51 participants, 27 were male (53%), and 24 were female (47%). In the intervention group, among 46 participants, 26 were male (56.5%), and 20 were female (43.5%) (Table 2).
The mean scores for pain and ROM in the control and intervention groups before the treatment are presented in Table 3.
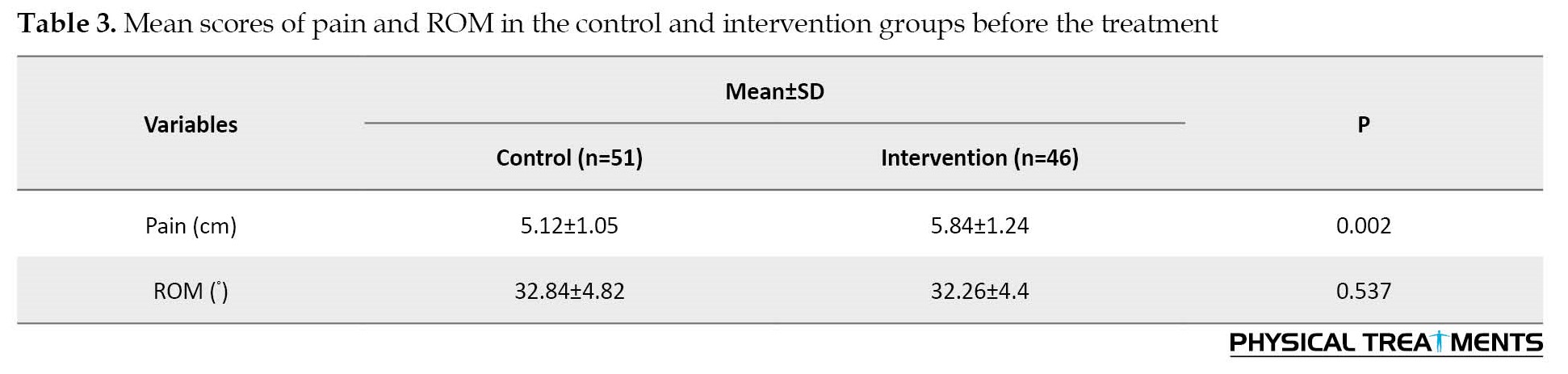
In the control group, the mean pain score and ROM were 5.12±1.05 and 32.84±4.82, respectively. In the intervention group, the mean pain score and ROM were 5.84±1.24 and 32.26±4.4, respectively. Before the treatment, there was a significant difference in pain scores between the two groups (P=0.002). However, the comparison of ROM scores between the two groups showed no statistically significant difference in ROM scores before the treatment (P=0.537).
The mean pain scores and ROM in the control and intervention groups after the treatment are reported in Table 4.
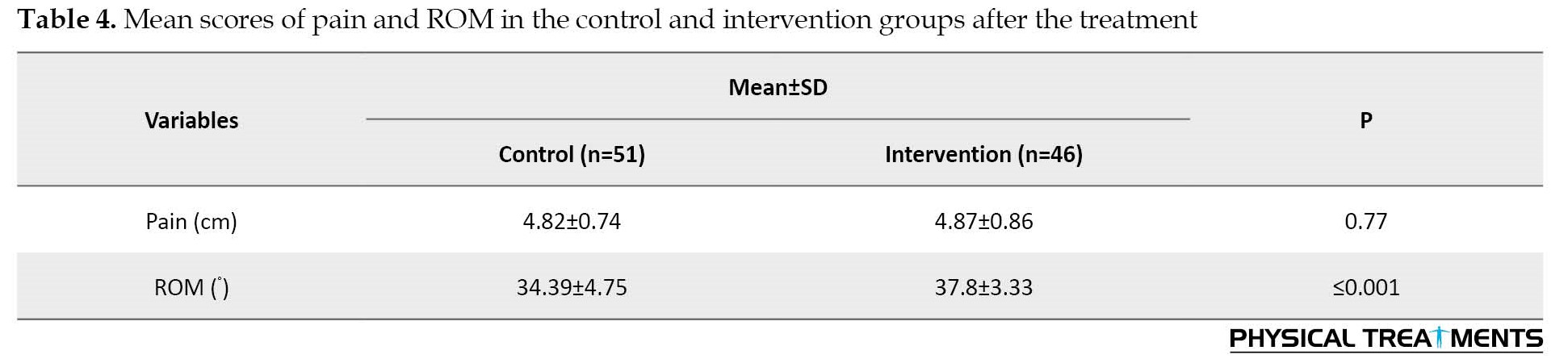
The control group had a mean pain score and ROM of 4.82±0.74 and 34.39±4.75, respectively. In the intervention group, the mean pain score and ROM were 4.87±0.86 and 37.8±3.33, respectively. Following the treatment, there was no significant difference in the mean pain scores between the two groups (P=0.77). Conversely, the mean scores of ROM in the intervention group showed a significant difference compared to the control group (P≤0.001).
Table 5 presents the comparison of pre-treatment and post-treatment scores of pain and ROM in the control and intervention groups.
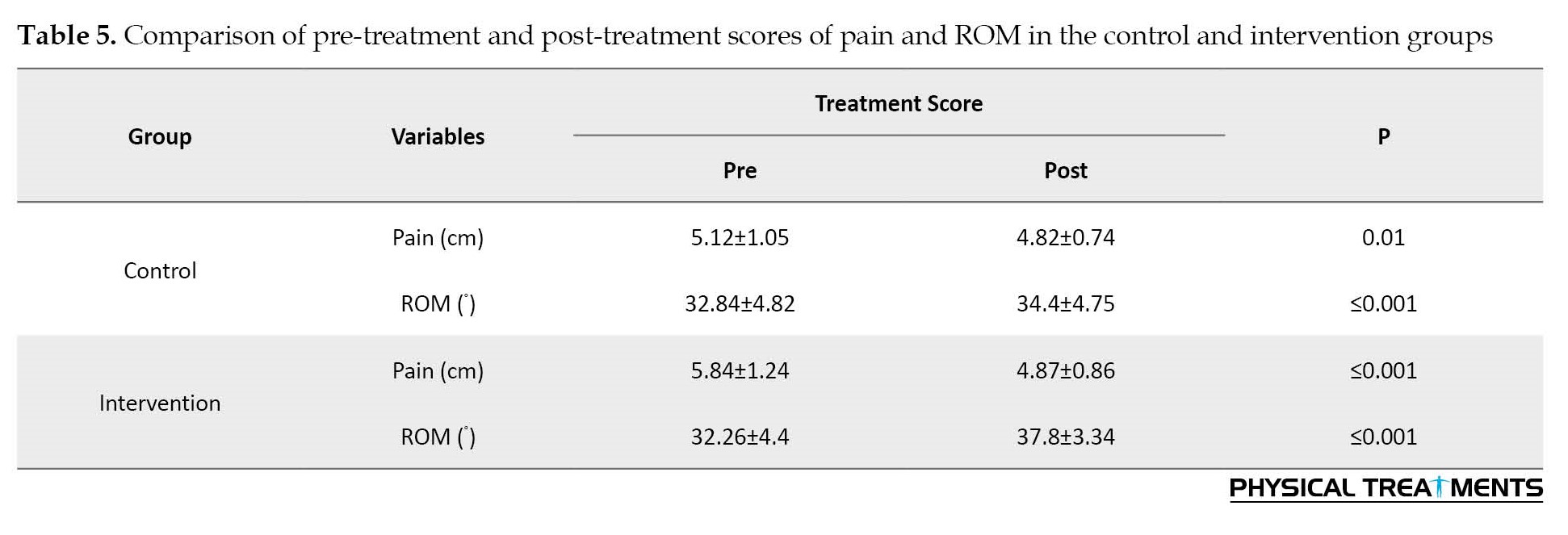
In the control group, the mean pre-test pain score was 5.12±1.05, which significantly decreased to 4.82±0.74 in the post-test phase (p=0.01). Similarly, the ROM scores in the control group displayed a significant improvement, with a pre-test score of 32.84±4.82 increasing to 34.4±4.75 in the post-test phase (P≤0.001). Participants of the intervention group reported a mean pre-test pain score of 5.84±1.24, which significantly reduced to 4.87±0.86 after the intervention (P≤0.001). Moreover, the ROM scores in the intervention significantly increased, with the pre-test score of 32.26±4.4 increasing to 37.8±3.34 in the post-test phase (P≤0.001).
4. Discussion
In this randomized clinical trial, the combination of manual therapy (MET) and conventional physiotherapy demonstrated positive effects on pain reduction and ROM in chronic LBP patients. MET is effective in patients with chronic LBP [20-24], which is supported by the findings of the present study. The neurophysiological mechanisms of muscles can explain these effects. According to Chaitow’s method, post-isometric relaxation refers to the subsequent reduction in tone of the agonist muscle (QL) following an isometric contraction. This response is mediated by Golgi tendon organ receptors, which inhibit muscle contraction in response to muscle overstretching [28].
Selkow et al. showed that restoring the full stretch length of muscles reduces muscle tension and subsequent pain [20], which is aligned with the results of our study. Our results indicated that MET improved muscle flexibility and consequently, ROM in the lumbar region. After stretching, muscle resistance decreases, and a viscoelastic response occurs [29]. Furthermore, muscle contraction stimulates contractile receptors, activating the periaqueductal gray matter in the midbrain, the non-opioid serotonergic pathway, and the noradrenergic descending inhibitory pathway, ultimately decreasing the sensation of pain [30, 31].
Previous studies have demonstrated that manual application of MET increases rhythmic muscle contractions and improves blood and lymphatic circulation in the muscles [31]. This process helps remove pro-inflammatory markers and contraction-induced secretions, thereby reducing the stimulation of pain receptors [33, 34]. In the MET method, the patient actively cooperates by contracting the muscles, inhaling and exhaling, and performing joint movements in specific directions. This technique directly targets the muscles, leading to a decrease in muscle hypertonicity [28]. In our study, the patient contracted the muscle first and then relaxed it, resulting in increased ROM of the lumbar joints. Ylinen et al. assessed the impact of stretching exercises versus manual therapy for the treatment of chronic neck pain. Their findings indicated that both stretching exercises and manual therapy significantly reduced neck pain and improved the level of disability among women experiencing non-specific neck pain [35].
Sharma et al. studied the effect of two techniques, ischemic compression, and MET, on trigger points in the upper trapezius. Their results showed that after four weeks of treatment, the MET group exhibited greater improvement in ROM compared to the other group, although no significant difference was found in pain reduction. Based on these findings, they concluded that MET was more effective in reducing pain and improving ROM [22].
Recent studies on the effects of MET on various muscles have consistently reported pain reduction, increased pain threshold, and improved ROM, measured by the VAS and other assessment tools. Overall, our study findings support the effectiveness of both conventional physiotherapy and MET in managing pain and increasing ROM in the QL muscle.
The application of MET, through the lengthening of sarcomeres and increased muscle blood flow, effectively reduces pain and improves ROM in patients with chronic LBP. Due to its cost-effectiveness, safety, and beneficial effects, therapists can consider integrating MET with other treatment methods. Further research is recommended to explore the effectiveness of MET on the QL muscle, with longer treatment periods for more definitive results. Additionally, three sessions of MET targeting this muscle are recommended to reduce pain and increase ROM in individuals with chronic LBP.
5. Conclusion
This study indicated that both treatments (conventional physiotherapy and MET) were effective in reducing pain. However, the intervention group showed a significant improvement in ROM compared to the control group. We suggest that the addition of MET to conventional physiotherapy can result in better flexibility. These findings highlight the potential benefits of combining MET with conventional physiotherapy on the QL muscle in chronic LBP subjects with lateral flexion restriction, as it can lead to reduced pain and improved ROM in the lumbar area.
Limitations and future research
One of the limitations of this article is that the study protocol involved performing the MET in a small number of sessions, whereas it may be more appropriate to investigate the effects of the MET in more than three sessions. The participants were limited to chronic LBP subjects with lateral flexion restriction. The results may not apply to individuals with different characteristics or conditions, limiting the generalizability of the results. We only evaluated the immediate effects of the treatment without assessing the long-term outcomes. Chronic LBP often requires long-term management; thus, it would be valuable to examine the sustainability of the observed improvements. Future research should investigate the effects of multiple MET treatments on the lumbar spine and whether other MET treatments enhance the observed changes in pain and ROM.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences (Code: 97/801/آ/4186).
Funding
This study received support from a research project at the University of Social Welfare and Rehabilitation Sciences.
Authors' contributions
All authors contributed equally to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors are grateful to the Physiotherapy Department of Milad Hospital and the Physiotherapy Department of the University of Social Welfare and Rehabilitation Sciences for their support throughout their research. The authors also thank the patients who took part in this research.
References
Low back pain (LBP) is one of the most common musculoskeletal problems [1, 2], and the leading cause of activity limitation and absenteeism [3]. Sixty to eighty percent of LBP patients report pain or disability a year later, and up to 40% report chronic pain [4, 5]. The impact of LBP on individuals and society, including pain, disability, and associated diagnostic and treatment costs, underscores the importance of prevention and effective treatment [6]. Various factors contribute to the development of chronic LBP. Physical factors, such as reduced muscle strength and endurance are prognostic factors for chronic LBP. The strength and endurance of the trunk muscles play a crucial role in reducing pain, enhancing stability, and maintaining spinal function [7, 8]. Chronic LBP has been associated with changes in trunk muscle responses and increased muscle fatigability [9]. Patients with chronic LBP and healthy individuals experiencing fatigue may utilize similar neuromuscular strategies to protect the spine, which can lead to back injuries. Delayed activation and higher levels of muscle activity have been associated with LBP [9]. Quadratus lumborum (QL) is a deep trunk muscle, and its tightness can trigger symptoms of significant low back tightness and discomfort [10]. Various treatments have been proposed for alleviating LBP, such as stretching exercises [11], heat therapy [12], massage therapy [13], proprioceptive neuromuscular facilitation [14], myofascial release [15], and muscle energy technique (MET) [16].
MET is a manual therapy that utilizes gentle muscle contractions of the patient to relax muscles, lengthen them, and restore normal joint motion [17, 18]. This technique was pioneered in 1948 by Fred Mitchell, Doctor of Osteopathic Medicine, to enhance musculoskeletal function by mobilizing joints and stretching tight muscles and fascia. Its primary aims are pain reduction, improved circulation, and enhanced lymphatic drainage [19]. MET operates based on the principle of reciprocal inhibition, which suggests that when indirect pressure is applied, muscles on one side of a joint will relax in response to the contraction of muscles on the opposite side [18]. The objective of MET is to promote muscle relaxation and lengthening, consequently enhancing joint range of motion (ROM). It is generally recognized as a gentle manual therapy technique for addressing limited motion in the spine and extremities [20]. MET is commonly applied to patients experiencing muscle spasms, as the process of lengthening shortened or spastic muscles can lead to improved ligament function. This technique involves alternating intervals of resisted muscle contractions and assisted stretching, collectively working to alleviate limitations in muscular activity [20]. Numerous studies have explored the impact of MET on lower back pain (LBP). MET might be a valuable approach for reducing non-specific lumbopelvic pain (LPP) over 24 hours [20]. Several studies have investigated the effects of MET on LBP, with one study proposing that MET could be a beneficial method for reducing non-specific lumbopelvic pain within a 24-hour timeframe [20]. Another study discovered that when combined with supervised motor control and resistance exercises, MET may be more effective in reducing disability and enhancing function in patients with acute LBP compared to neuromuscular re-education and resistance training [21]. Sharma et al. investigated the effects of MET on pain and disability in subjects with SI joint dysfunction. Their findings revealed that both MET and mobilization are effective in treating chronic LBP caused by sacroiliac joint dysfunction [22]. Patil et al. investigated the effectiveness of MET in QL in acute LBP. The findings suggested that MET combined with interferential therapy could be an effective treatment option for patients with acute LBP [23]. A review article suggested that the MET procedure can be effective in the management of chronic mechanical LBP [24]. However, there remains a lack of research on its clinical benefits and specific impact on the QL muscle in terms of reducing pain intensity and increasing spinal ROM. Therefore, the purpose of this research was to investigate the effect of MET on QL muscle regarding pain and lumbar ROM in patients suffering from chronic LBP characterized by restricted lateral movement. The hypothesis was that MET can improve pain and lumbar ROM in chronic LBP subjects with restricted lateral movement.
2. Materials and Methods
Source of data
The data were collected from the physiotherapy department of Milad Hospital in Tehran, Iran, from 2018 to 2019.
Subjects
This study was a single-blind randomized clinical trial. The sample included both male and female participants (a heterogeneous group) clinically diagnosed with chronic LBP with lateral flexion restriction and referred to the physiotherapy outpatient department of Milad Hospital for physiotherapy treatment. With a 90% Cl, 90% statistical power, and considering a 20% dropout rate, it was determined that each group would require 54 participants.
Inclusion criteria
1) Age range of 20 to 50 years; 2) Both male and female individuals with a clinical diagnosis of non-specific chronic LBP; 3) Participants experiencing lumbar pain and discomfort at the attachment points of the QL, specifically the iliac crest and lower ribs; 4) Individuals with limited unilateral flexion; 5) Participants willing to take part in the study; 6) Individuals who have not undergone physiotherapy within the past three months
Exclusion criteria
1) Participants with specific causes of LBP, such as intervertebral disc prolapse with instability, radicular symptoms, lumbar spondylosis, spondylolisthesis, lumbar canal stenosis, malignancies, and sensory deficits; 2) Participants with conditions, like osteoporosis, kidney and gastrointestinal disorders, and psychiatric issues as self-reported by the patients; 3) Individuals with a history of spinal surgery or spinal fractures; 4) Participants with differences in leg length (measured using the tape measurement method) [25]
Procedure
The study recruited participants with chronic LBP who were referred to the physiotherapy outpatient department and screened for suitability based on inclusion and exclusion criteria. Those willing to participate signed an informed consent form, and their demographic data were collected, along with their initial assessment of pain intensity and ROM of the lumbar spine. Pain intensity was assessed using a 100-mm visual analog scale (VAS) for back pain before and after treatment. Participants were instructed to mark a point on a 10 cm line to indicate the intensity of their pain, where zero represented the absence of pain, and ten indicated the most severe pain imaginable [26]. A standard plastic goniometer was used to measure the ROM of the lumbar lateral flexion angle before and after treatment. Each measurement was repeated three times to allow for the evaluation of intratester reliability. The examiner palpated and marked bony landmarks (the spinous process of the S1 vertebra and the spinous process of the C7 vertebra) for goniometer alignment in a standing erect position. The stationary arm was aligned vertically, the axis was set at the S1 spinous process, and the moving arm was aligned with the C7 spinous process. By using a random number table [27], 102 participants were randomly allocated to two groups of 51: Control and intervention. The control group received conventional physiotherapy, while the intervention group received MET using Chaitow’s method of post-isometric relaxation in addition to conventional physiotherapy [28].
Conventional physiotherapy
The patients allocated to the conventional physiotherapy group were provided with a combination of methods, including the application of a hot pack (10 minutes), and transcutaneous electrical nerve stimulation (TENS) (frequency: 2Hz and pulse duration: 200 μs; 20 minutes). The physiotherapist applied these methods to the patients in three sessions during a week. All participants received conventional physiotherapy lasting for 0.5 hours.
MET procedure
The intervention group received additional isometric contraction using post-isometric relaxation as part of MET [28]. This was achieved by holding the contraction for 5 seconds, followed by a 5-second rest period, and repeating this process three times during each session on the restricted side. The sessions were held three times in one week. The procedure was conducted with the therapist standing behind the side-lying patient. The patient abducted the uppermost leg until the therapist could palpate QL activity. Then, the patient was instructed to hold the leg with a mild degree of force (<20% of available strength) isometrically. After 5 seconds of contraction, the patient allowed the leg to hang slightly behind them. Then, the patient completely relaxed for 5 seconds. The therapist then passively moved to a new restricted barrier and held the stretch for 30 minutes.
Statistical analysis
Analyses were conducted on subjects who completed the entire process. Statistical tests were performed using IBM SPSS software, version 22. Central tendency and dispersion indices were employed to describe both qualitative and quantitative variables. The Kolmogorov-Smirnov test was employed to evaluate the normality of the data distribution. An analysis of covariance (ANCOVA) was employed to assess the effect of MET on pain and ROM. A significance level of 0.05 was adopted for all statistical tests.
3. Results
Initially, there were 108 patients enrolled in the study, but two patients were excluded because they did not meet the inclusion criteria, and four patients voluntarily withdrew from the study, resulting in a final sample size of 102 patients. These patients were randomly divided into the control (n=51) and intervention (n=51) groups using a table of random numbers. In the intervention group, five patients did not complete the treatment, and the remaining 46 patients were analyzed. The mean age of the patients was 37.74±7.07 years in the control group and 39.87±6.3 years in the intervention group (Table 1).
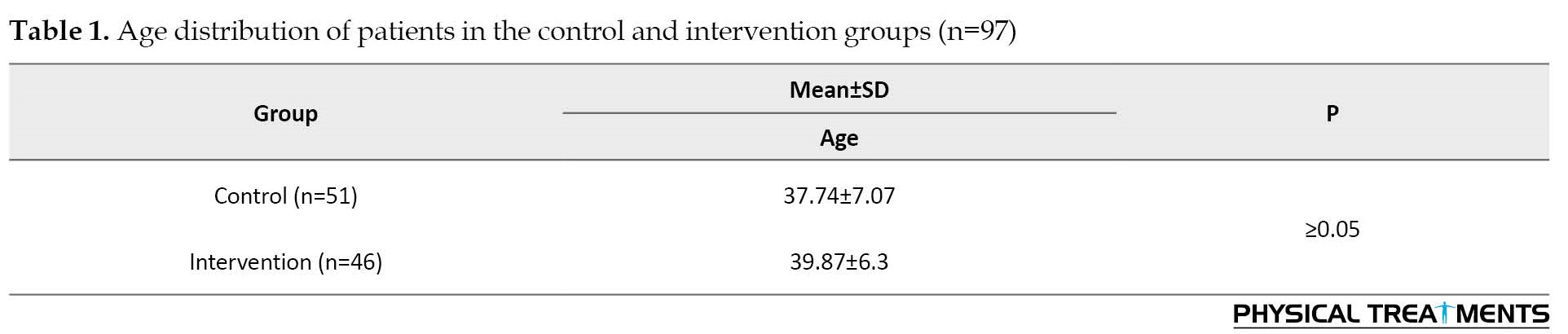
The Kolmogorov-Smirnov test results revealed that all variables examined in the study followed a normal distribution. A comparison of the background variables before the treatment revealed no significant differences between the two groups according to the distribution of their age and gender (P≥0.05) (Tables 1 and 2).
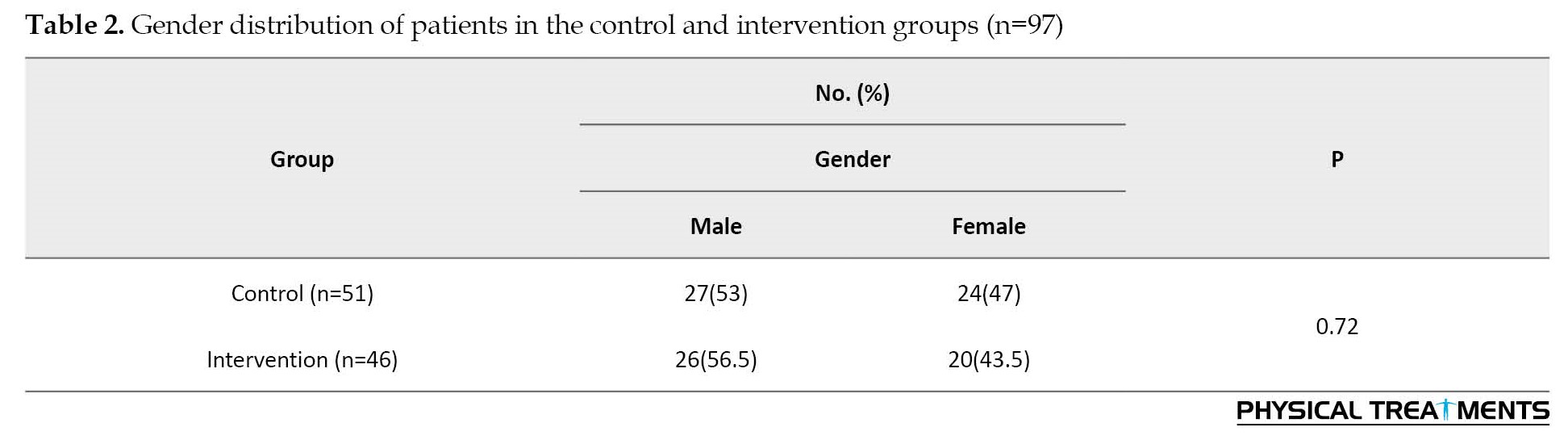
In the control group, among 51 participants, 27 were male (53%), and 24 were female (47%). In the intervention group, among 46 participants, 26 were male (56.5%), and 20 were female (43.5%) (Table 2).
The mean scores for pain and ROM in the control and intervention groups before the treatment are presented in Table 3.
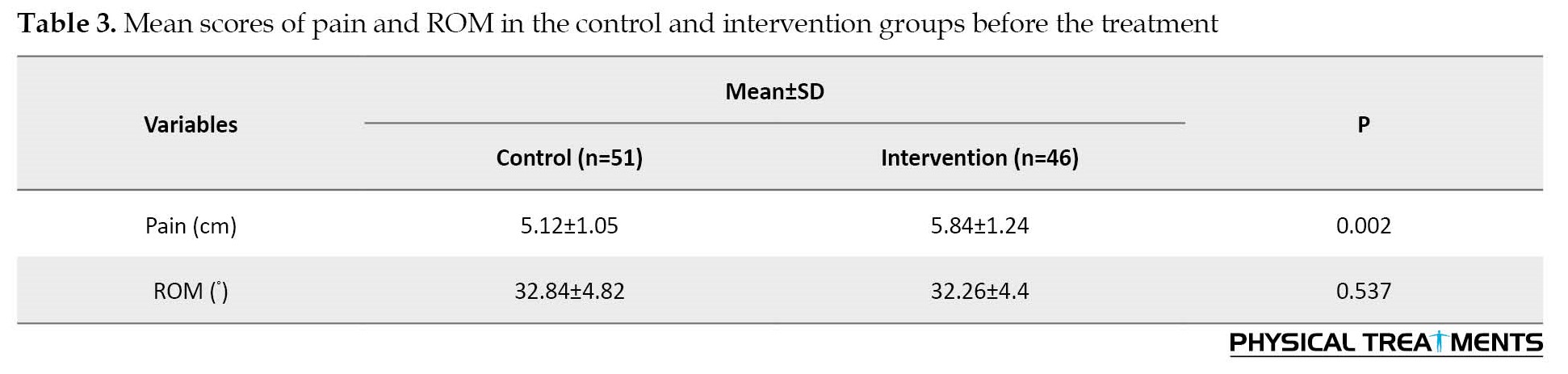
In the control group, the mean pain score and ROM were 5.12±1.05 and 32.84±4.82, respectively. In the intervention group, the mean pain score and ROM were 5.84±1.24 and 32.26±4.4, respectively. Before the treatment, there was a significant difference in pain scores between the two groups (P=0.002). However, the comparison of ROM scores between the two groups showed no statistically significant difference in ROM scores before the treatment (P=0.537).
The mean pain scores and ROM in the control and intervention groups after the treatment are reported in Table 4.
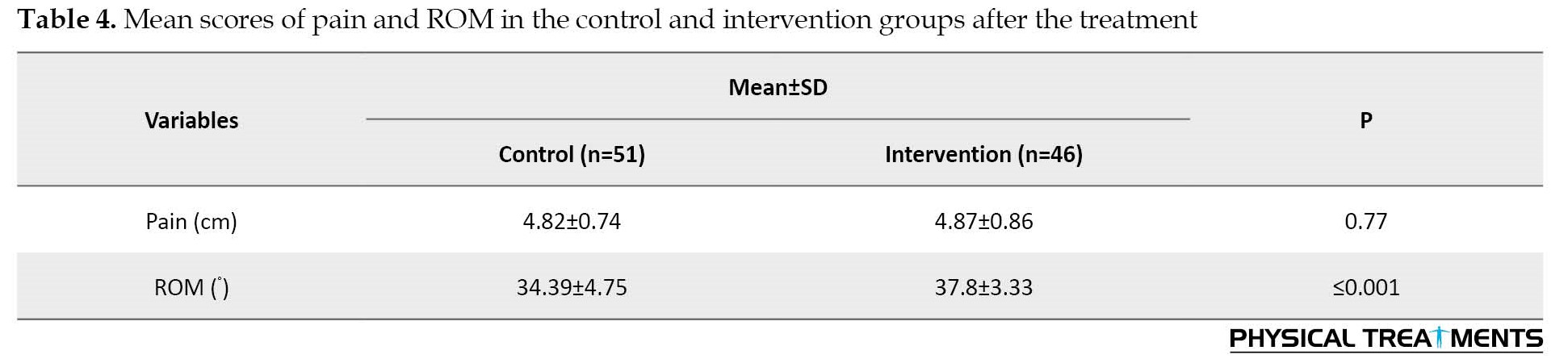
The control group had a mean pain score and ROM of 4.82±0.74 and 34.39±4.75, respectively. In the intervention group, the mean pain score and ROM were 4.87±0.86 and 37.8±3.33, respectively. Following the treatment, there was no significant difference in the mean pain scores between the two groups (P=0.77). Conversely, the mean scores of ROM in the intervention group showed a significant difference compared to the control group (P≤0.001).
Table 5 presents the comparison of pre-treatment and post-treatment scores of pain and ROM in the control and intervention groups.
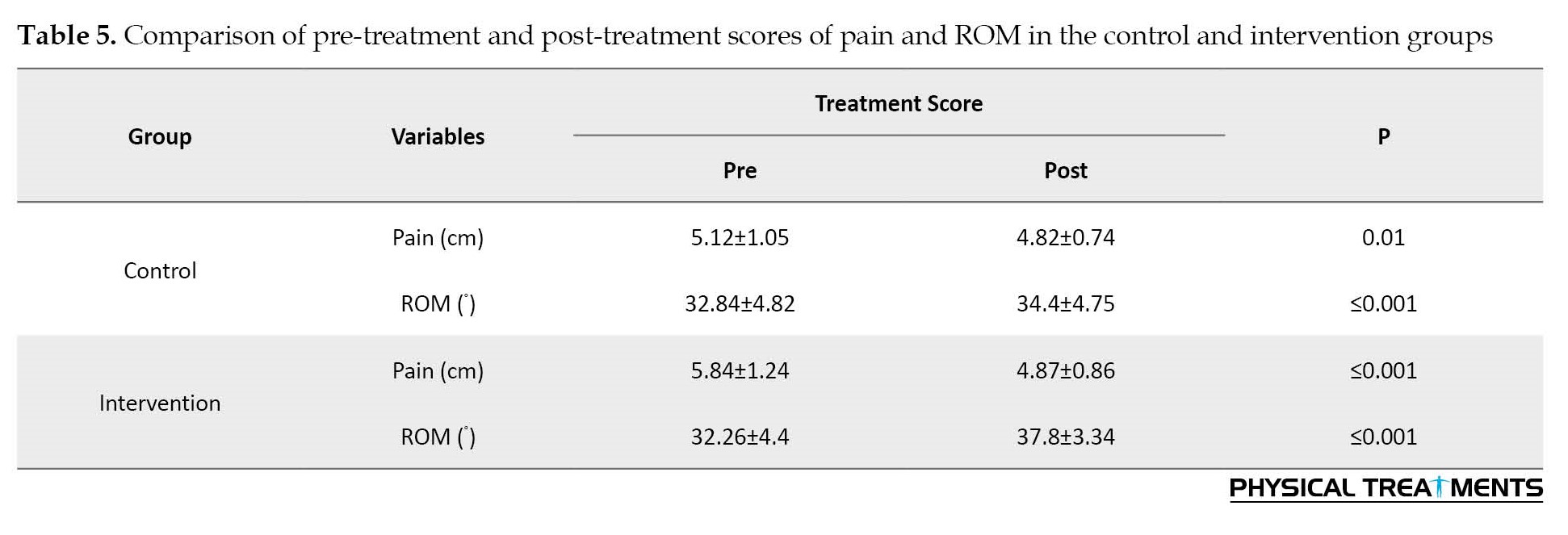
In the control group, the mean pre-test pain score was 5.12±1.05, which significantly decreased to 4.82±0.74 in the post-test phase (p=0.01). Similarly, the ROM scores in the control group displayed a significant improvement, with a pre-test score of 32.84±4.82 increasing to 34.4±4.75 in the post-test phase (P≤0.001). Participants of the intervention group reported a mean pre-test pain score of 5.84±1.24, which significantly reduced to 4.87±0.86 after the intervention (P≤0.001). Moreover, the ROM scores in the intervention significantly increased, with the pre-test score of 32.26±4.4 increasing to 37.8±3.34 in the post-test phase (P≤0.001).
4. Discussion
In this randomized clinical trial, the combination of manual therapy (MET) and conventional physiotherapy demonstrated positive effects on pain reduction and ROM in chronic LBP patients. MET is effective in patients with chronic LBP [20-24], which is supported by the findings of the present study. The neurophysiological mechanisms of muscles can explain these effects. According to Chaitow’s method, post-isometric relaxation refers to the subsequent reduction in tone of the agonist muscle (QL) following an isometric contraction. This response is mediated by Golgi tendon organ receptors, which inhibit muscle contraction in response to muscle overstretching [28].
Selkow et al. showed that restoring the full stretch length of muscles reduces muscle tension and subsequent pain [20], which is aligned with the results of our study. Our results indicated that MET improved muscle flexibility and consequently, ROM in the lumbar region. After stretching, muscle resistance decreases, and a viscoelastic response occurs [29]. Furthermore, muscle contraction stimulates contractile receptors, activating the periaqueductal gray matter in the midbrain, the non-opioid serotonergic pathway, and the noradrenergic descending inhibitory pathway, ultimately decreasing the sensation of pain [30, 31].
Previous studies have demonstrated that manual application of MET increases rhythmic muscle contractions and improves blood and lymphatic circulation in the muscles [31]. This process helps remove pro-inflammatory markers and contraction-induced secretions, thereby reducing the stimulation of pain receptors [33, 34]. In the MET method, the patient actively cooperates by contracting the muscles, inhaling and exhaling, and performing joint movements in specific directions. This technique directly targets the muscles, leading to a decrease in muscle hypertonicity [28]. In our study, the patient contracted the muscle first and then relaxed it, resulting in increased ROM of the lumbar joints. Ylinen et al. assessed the impact of stretching exercises versus manual therapy for the treatment of chronic neck pain. Their findings indicated that both stretching exercises and manual therapy significantly reduced neck pain and improved the level of disability among women experiencing non-specific neck pain [35].
Sharma et al. studied the effect of two techniques, ischemic compression, and MET, on trigger points in the upper trapezius. Their results showed that after four weeks of treatment, the MET group exhibited greater improvement in ROM compared to the other group, although no significant difference was found in pain reduction. Based on these findings, they concluded that MET was more effective in reducing pain and improving ROM [22].
Recent studies on the effects of MET on various muscles have consistently reported pain reduction, increased pain threshold, and improved ROM, measured by the VAS and other assessment tools. Overall, our study findings support the effectiveness of both conventional physiotherapy and MET in managing pain and increasing ROM in the QL muscle.
The application of MET, through the lengthening of sarcomeres and increased muscle blood flow, effectively reduces pain and improves ROM in patients with chronic LBP. Due to its cost-effectiveness, safety, and beneficial effects, therapists can consider integrating MET with other treatment methods. Further research is recommended to explore the effectiveness of MET on the QL muscle, with longer treatment periods for more definitive results. Additionally, three sessions of MET targeting this muscle are recommended to reduce pain and increase ROM in individuals with chronic LBP.
5. Conclusion
This study indicated that both treatments (conventional physiotherapy and MET) were effective in reducing pain. However, the intervention group showed a significant improvement in ROM compared to the control group. We suggest that the addition of MET to conventional physiotherapy can result in better flexibility. These findings highlight the potential benefits of combining MET with conventional physiotherapy on the QL muscle in chronic LBP subjects with lateral flexion restriction, as it can lead to reduced pain and improved ROM in the lumbar area.
Limitations and future research
One of the limitations of this article is that the study protocol involved performing the MET in a small number of sessions, whereas it may be more appropriate to investigate the effects of the MET in more than three sessions. The participants were limited to chronic LBP subjects with lateral flexion restriction. The results may not apply to individuals with different characteristics or conditions, limiting the generalizability of the results. We only evaluated the immediate effects of the treatment without assessing the long-term outcomes. Chronic LBP often requires long-term management; thus, it would be valuable to examine the sustainability of the observed improvements. Future research should investigate the effects of multiple MET treatments on the lumbar spine and whether other MET treatments enhance the observed changes in pain and ROM.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences (Code: 97/801/آ/4186).
Funding
This study received support from a research project at the University of Social Welfare and Rehabilitation Sciences.
Authors' contributions
All authors contributed equally to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors are grateful to the Physiotherapy Department of Milad Hospital and the Physiotherapy Department of the University of Social Welfare and Rehabilitation Sciences for their support throughout their research. The authors also thank the patients who took part in this research.
References
- Balagué F, Mannion AF, Pellisé F, Cedraschi C. Non-specific low back pain. The lancet. 2012; 379(9814):482-91. [DOI:10.1016/S0140-6736(11)60610-7] [PMID]
- Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, et al. A systematic review of the global prevalence of low back pain. Arthritis & Rheumatism. 2012; 64(6):2028-37. [DOI:10.1002/art.34347] [PMID]
- Wu A, March L, Zheng X, Huang J, Wang X, Zhao J, et al. Global low back pain prevalence and years lived with disability from 1990 to 2017: Estimates from the Global Burden of Disease Study 2017. Annals of Translational Medicine. 2020; 8(6):299. [DOI:10.21037/atm.2020.02.175] [PMID]
- Hestbaek L, Leboeuf-Yde C, Manniche C. Low back pain: What is the long-term course? A review of studies of general patient populations. European Spine Journal. 2003; 12(2):149-65. [DOI:10.1007/s00586-002-0508-5] [PMID]
- Dunn KM, Jordan K, Croft PR. Characterizing the course of low back pain: A latent class analysis. American Journal of Epidemiology. 2006; 163(8):754-61. [DOI:10.1093/aje/kwj100] [PMID]
- Deyo RA, Cherkin D, Conrad D, Volinn E. Cost, controversy, crisis: Low back pain and the health of the public. Annual Review of Public Health. 1991; 12:141-56. [DOI:10.1146/annurev.pu.12.050191.001041] [PMID]
- Safdari S, Khayambashi K, Ghasemi GA, Falah A, Sakhavat E. [Effects of selected core stabilization exercise protocol on pain and functional disability in patients with chronic non-specific low back pain (Persian)]. Journal of Research in Rehabilitation Sciences. 2014; 10(1):56-66. [Link]
- Hwangbo G, Lee CW, Kim SG, Kim HS. The effects of trunk stability exercise and a combined exercise program on pain, flexibility, and static balance in chronic low back pain patients. Journal of Physical Therapy Science. 2015; 27(4):1153-5. [DOI:10.1589/jpts.27.1153] [PMID]
- Jubany J, Danneels L, Angulo-Barroso R. The influence of fatigue and chronic low back pain on muscle recruitment patterns following an unexpected external perturbation. BMC Musculoskeletal Disorders. 2017; 18(1):161. [DOI:10.1186/s12891-017-1523-3] [PMID]
- No author. Quadratus lumborum exercises & stretches [internet]. 2021 [Updated 2023 December]. Available from: [Link]
- França FR, Burke TN, Caffaro RR, Ramos LA, Marques AP. Effects of muscular stretching and segmental stabilization on functional disability and pain in patients with chronic low back pain: A randomized, controlled trial. Journal of Manipulative and Physiological Therapeutics. 2012; 35(4):279-85. [DOI:10.1016/j.jmpt.2012.04.012] [PMID]
- Freiwald J, Magni A, Fanlo-Mazas P, Paulino E, Sequeira de Medeiros L, Moretti B, et al. A role for superficial heat therapy in the management of non-specific, mild-to-moderate low back pain in current clinical practice: A narrative review. Life. 2021; 11(8):780. [DOI:10.3390/life11080780] [PMID]
- Furlan AD, Giraldo M, Baskwill A, Irvin E, Imamura M. Massage for low‐back pain. Cochrane Database of Systematic Reviews. 2015; 2015(9):CD001929. [DOI:10.1002/14651858.CD001929.pub3] [PMID]
- Anggiat L, Manurung NSA, Manik JWH. Proprioceptive neuromuscular facilitation approach for low back pain: A review study. International Journal of Sport, Exercise and Health Research. 2022; 6(1):81-7. [DOI:10.31254/sportmed.6113]
- Wu Z, Wang Y, Ye X, Chen Z, Zhou R, Ye Z, et al. Myofascial release for chronic low back pain: A systematic review and meta-analysis. Frontiers in Medicine. 2021; 8:697986.[DOI:10.3389/fmed.2021.697986] [PMID]
- Thomas E, Cavallaro AR, Mani D, Bianco A, Palma A. The efficacy of muscle energy techniques in symptomatic and asymptomatic subjects: A systematic review. Chiropractic & Manual Therapies. 2019; 27:35. [DOI:10.1186/s12998-019-0258-7] [PMID]
- No author. Muscle energy techniques. [internet]. 2023 [Updated 2023 December]. Available from: [Link]
- No author. What is muscle energy technique? [internet]. 2021 [Updated 2023 December]. Available from: [Link]
- Goodridge JP. Muscle energy technique: Definition, explanation, methods of procedure. The Journal of the American Osteopathic Association. 1981; 81(12):67-74. [DOI:10.1515/jom-1981-811211]
- Selkow NM, Grindstaff TL, Cross KM, Pugh K, Hertel J, Saliba S. Short-term effect of muscle energy technique on pain in individuals with non-specific lumbopelvic pain: A pilot study. Journal of Manual & Manipulative Therapy. 2009; 17(1):14E-8. [DOI:10.1179/jmt.2009.17.1.14E] [PMID]
- Wilson E, Payton O, Donegan-Shoaf L, Dec K. Muscle energy technique in patients with acute low back pain: a pilot clinical trial. Journal of Orthopaedic & Sports Physical Therapy. 2003; 33(9):502-12. [DOI:10.2519/jospt.2003.33.9.502] [PMID]
- Sharma D, Sen S. Effects of muscle energy technique on pain and disability in subjects with SI joint dysfunction.International Journal of Physiotherapy and Research. 2014; 2(1):305-11. [Link]
- Patil PN, Chandu B, Metgud S, Khatri S. Effectiveness of muscle energy technique on quadratus lumborum in acute low back pain-randomized controlled trial. Indian Journal of Physiotherapy and Occupational Therapy. 2010; 4(1):54-8. [Link]
- Ahmed UA, Nadasan T, Van Oosterwijck J, Maharaj SS. The effect of muscles energy technique in the management of chronic mechanical low back pain: A scoping review. Journal of Back and Musculoskeletal Rehabilitation. 2021; 34(2):179-93. [DOI:10.3233/BMR-200011] [PMID]
- Farahmand B, Ebrahimi Takamjani E, Yazdi HR, Saeedi H, Kamali M, Bagherzadeh Cham M. A systematic review on the validity and reliability of tape measurement method in leg length discrepancy. Med J Islam Repub Iran. 2019; 33:46. [DOI:10.34171/mjiri.33.46] [PMID]
- Jensen MP, Chen C, Brugger AM. Interpretation of visual analog scale ratings and change scores: A reanalysis of two clinical trials of postoperative pain. The Journal of Pain. 2003; 4(7):407-14. [DOI:10.1016/S1526-5900(03)00716-8] [PMID]
- No author. Table of random numbers [internet]. 2023 [Updated 2023 December]. Available from: [Link]
- Chaitow L, Crenshaw K. Muscle energy techniques. Amsterdam: Elsevier Health Sciences; 2006. [Link]
- Mahieu NN, McNair P, De Muynck M, Stevens V, Blanckaert I, Smits N, et al. Effect of static and ballistic stretching on the muscle-tendon tissue properties. Med Sci Sports Exerc. 2007; 39(3):494-501. [DOI:10.1249/01.mss.0000247004.40212.f7] [PMID]
- Rickards LD. Therapeutic needling in osteopathic practice: An evidence-informed perspective. International Journal of Osteopathic Medicine. 2009; 12(1):2-13. [DOI:10.1016/j.ijosm.2009.01.003]
- Akbari A, Naroii S, Eshgi M, Farahani A. [A comparison between muscle energy technique with low-level laser in reducing neck and shoulder pain and disability in subjects with trapezius and levator scapula myofascial trigger points (Persian)]. Journal of Advances in Medical and Biomedical Research. 2012; 20(79):69-82. [Link]
- Fryer G. Muscle energy technique: An evidence-informed approach. International Journal of Osteopathic Medicine. 2011; 14(1):3-9. [DOI:10.1016/j.ijosm.2010.04.004]
- Dommerholt J, Mayoral del Moral O, Gröbli C. Trigger point dry needling. Journal of Manual & Manipulative Therapy. 2006; 14(4):70E-87E. [DOI:10.1179/jmt.2006.14.4.70E]
- Bukhari SN, Khan T. Comparison between effects of ischemic compression therapy and deep friction massage therapy for trigger points in neck and upper back. Journal Riphah College of Rehabilitation Sciences. 2020; 8(01):S29-32. [Link]
- Ylinen J, Kautiainen H, Wirén K, Häkkinen A. Stretching exercises vs manual therapy in treatment of chronic neck pain: A randomized, controlled cross-over trial. Journal of Rehabilitation Medicine. 2007; 39(2):126-32. [DOI:10.2340/16501977-0015] [PMID]
Type of Study: Research |
Subject:
Sport injury and corrective exercises
Received: 2023/06/11 | Accepted: 2023/07/26 | Published: 2023/10/14
Received: 2023/06/11 | Accepted: 2023/07/26 | Published: 2023/10/14
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






