Sat, Nov 8, 2025
Volume 12, Issue 4 (Autumn 2022)
PTJ 2022, 12(4): 291-302 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ansari A, Karimizadeh Ardakani M, Akoochakian M. Effects of Weight-bearing Exercise on a Mini-trampoline, and Foot-ankle Therapeutic Exercise Program on Foot-ankle Functionality in People With Diabetic Peripheral Neuropathy. PTJ 2022; 12 (4) :291-302
URL: http://ptj.uswr.ac.ir/article-1-559-en.html
URL: http://ptj.uswr.ac.ir/article-1-559-en.html
1- Department of Sport Sciences, Kish International Campus, University of Tehran, Kish, Iran.
2- Department of Health and Sports Medicine, Faculty of Physical Education and Sport Sciences, University of Tehran, Tehran, Iran.
2- Department of Health and Sports Medicine, Faculty of Physical Education and Sport Sciences, University of Tehran, Tehran, Iran.
Keywords: Diabetic peripheral neuropathy, Mini-trampoline, Ankle therapeutic exercise program, Plantar functionality
Full-Text [PDF 538 kb]
(1216 Downloads)
| Abstract (HTML) (4261 Views)
Full-Text: (977 Views)
1. Introduction
Diabetes is the most common endocrine disease, one of the leading causes of death in most countries, and unquestionably one of the most pressing health issues in the world today [1, 2, 3]. Diabetes causes a broad spectrum of complications. The most common long-term complication of this disease is peripheral neuropathy. According to the national diabetes information center, more than 50% of those with diabetes have some form of neuropathy, even if they have no symptoms. Diabetic peripheral neuropathy (DPN) is a neurological disorder that affects the sensitivity and excitability of the nerves of the feet and hands [4, 5] resulting in a stabbing or burning sensation, numbness, and tingling in lower limbs [6, 7, 8,]. Foot disorders are the main problem related to diabetic neuropathy, leading to a significant deal of pain and social costs for patients [9, 10,]. Numbness in one or both feet is frequently the early symptom. Therefore, people with DPN are more likely to develop foot ulcers and are at a higher risk of having their foot amputated at the ankle or below knee level [11].
DPN also causes musculoskeletal dysfunction due to sensory-motor disorders which include changes in the joints surrounding the tissues, as well as a decrease in function and strength of feet due to atrophy of the inner lower foot muscles. Furthermore, it causes decreased mobility of the ankle and the first metatarsophalangeal joint, which can result in high plantar pressure under the metatarsal heads and loss of function of the toes, particularly the big toe. These effects are the primary contributors to the formation of deformities and high pressures on the soles of the feet, which affect the stability of foot dynamics and cause changes in the biomechanics of walking, such as a reduction in walking speed and ankle dorsi and plantar flexion, as well as a decrease in torque force around the ankle joint, a delay in muscle activation in the legs and thighs, and an increase in torque force in the hip joint [7]. As a result of these changes, patients with DPN typically exhibit more disturbance in posture and walking, along with difficulties performing daily activities [12, 13].
A growing body of evidence supports the impact of exercise on neuropathy management. Exercise improves glucose control and increases insulin sensitivity throughout the body. It lowers circulating fat levels, stimulating angiogenesis and increasing perfusion, physical performance, and balance, and lowering depression, anxiety, and the risk of falling in DNP patients [14]. Strength, stretching, balance, and resistance training programs have been shown to improve muscle strength, endurance, and flexibility, and can lead to increased range of motion (ROM) and muscle strength [15-19].
Proper foot and ankle exercises are among the other appropriate exercises investigated in this study. On the one hand, these exercises have beneficial results in reducing negative factors of diabetic foot pathogenesis and may lead to increased nerve speed of the lower limbs and muscle strengthening, improved ROM of the ankle, redistributed sole and plantar pressure during walking, and as a result, a better physiological pattern. More positive effects, such as increased skin sensitivity and intraepidermal nerve fiber density can be achieved by performing appropriate ankle exercises in diabetic patients, which can delay the usual process of DPN, skin damage, and wounding [20].
On the other hand, increased weight-bearing activities can result in increased pressure on the soles of the feet and, as a result, foot ulcers. Therefore, the American Diabetes Association advises people with diabetic neuropathy to exercise properly and to limit activities that require bearing body weight. Trampoline exercise has recently been shown to improve balance control in the elderly [21], as well as athletic performance, rehabilitation, injury recovery, and foot function in athletes with ankle instability [22].
Exercises on the mini-trampoline and ankle therapeutic exercises at home can be effective in improving patients’ quality of life as a simple, affordable, low-risk, and quick-improvement treatment program that focuses on the use of segmental exercises for foot function. However, to our knowledge, no earlier study has been conducted to evaluate the effects of a foot and ankle treatment program capable of personalizing special foot treatment exercises at home aimed at preventing and treating musculoskeletal defects and complications in patients with diabetic neuropathy. Therefore, more research in this field is required to strengthen the level of evidence based on the use of specific ankle therapeutic exercises to reduce risk factors and prevent further complications.
Thus, this study aims to examine whether providing appropriate solutions based on therapeutic strategies for musculoskeletal abnormalities related to DPN, including self-care instructions and home exercises (ankle therapeutic exercises and weight-bearing exercises on a mini-trampoline), can improve the health and performance of the foot and ankle ROM.
2. Materials and Methods
The current study is a clinical trial study with two experimental groups and one control group. The statistical population of this study includes 48 women who suffered from type 2 diabetes for at least 7 years with an average age of 50 to 65 years and a history of moderate or severe peripheral neuropathy with decreased sensation in the feet that had been previously diagnosed by a medical doctor. The sample size was estimated using G Power software. The software was programmed with the assumption of a large effect size (80%), at a level of 5% error probability and 95% power. The total sample size calculated by the software for three groups was 48 people with 16 subjects in each group. This study was conducted at the Parsian diabetes clinic in Tehran.
After receiving informed consent, volunteers who met the eligibility criteria were randomly assigned into two intervention groups and one control group. During the exercise intervention period, all three groups received foot care training and medical team recommendations, which included, foot hygiene, daily washing and careful drying of the feet, especially between the toes, use of non-elastic and seamless socks, trimming the nails in a square shape, preventing unsupervised removal of calluses or blisters, not wearing shoes or slippers without socks, and seeking medical attention if problems with the feet are discovered. During the study, subjects in all three groups did not receive any other concurrent care, such as physiotherapy, acupuncture, or any other non-conventional medical intervention. Cramping, moderate to severe pain, fatigue, dizziness, fear, or any condition that exposed the patient to discomfort were all reasons for stopping the session.
To validate the training protocols, all participants underwent two measurement sessions (before and after the intervention) to measure the flexion and extension angles of the first metatarsophalangeal joint with a goniometer, the ROM of the ankle with an electro goniometer, and the isometric strength of the foot with a hand-held dynamometer. The researcher performed all measurements in the presence of a medical doctor and physiotherapist.
Research instruments
All participants completed the Brazilian version of the Michigan neuropathy screening instrument (MNSI) questionnaire to determine the presence of DPN. In this research, the Brazilian-Portuguese version of the foot health status questionnaire (FHSQ-BR) was used to assess foot health [23, 24]. Flexion and extension angles (first) ([metatarsophalangeal joints] MTPJ) were measured with a goniometer using the dynamic ROM measurement method. For analysis, the mean values of three maximum flexion and maximum extension records were calculated [14]. An electro-goniometer (model DSI [Danesh Salar Iranian]) with a measurement accuracy of 1 degree was used to evaluate the ROM of the ankle flexion and extension, and the mean scores of three records of maximum flexion and maximum extension were calculated for analysis [23, 24]. The strength peak muscle force (kg) was measured by a maximum isometric voluntary contraction in ankle dorsi and plantar flexion and hallux dorsi and plantar flexion using a hand-held push-pull dynamometer. Each muscle group should be tested with a 3-5 s contraction. Three repetitions were performed for each foot muscle group, with a minimum of 10 s of rest between each, and the mean scores of three measurements were used for data analysis [25, 26].
Exercise protocols
The first experimental group exercised on a mini-trampoline at home [14]. The mini-trampoline training program consisted of four levels of progression over eight weeks. The participants were instructed to perform each exercise with 10 repetitions for two weeks, at least three times per week, and hold the position for up to 10 s in static exercises. The exercise program was performed daily in three sets with 5-minute rest intervals between them. To warm up and cool down, participants were asked to stretch quadriceps, hamstrings, biceps, and soleus muscles. Each muscle was stretched 3 times with a 20 s rest between each. In addition, the participants were asked to wear appropriate footwear and inspect their feet after the exercises. Discontinuation criteria for each session included cramping, moderate to severe pain, fatigue, dizziness, or any condition that exposed the patient to any discomfort [14].
The ankle exercise-therapy program was carried out by the second experimental group. This program included exercises to strengthen the internal and external foot and ankle muscles [27]. Six exercises were performed, four exercises for the inner foot muscles and two exercises for the outer foot and ankle muscles. Exercises were done using tools, such as cotton ball, pencils, balls, and chairs. The interphalangeal, metatarsophalangeal, and ankle joints were targeted in this protocol, with emphasis on the following muscle groups, medial plantar side (abductor hallucis, flexor hallucis brevis, and adductor hallucis), lateral plantar side (abductor digiti minimi, flexor digiti minimi, and opponens digiti minimi), median plantar side (flexor digitorum brevis, quadratus plantar, lumbrical muscle, plantar interosseous muscle, and dorsal interosseous muscle) and dorsal plantar side (extensor digitorum brevis, and extensor hallucis brevis). Foot exercises were performed first in a sitting position and one set of 30 repetitions, then in a standing position and standing on one foot if the exercise was very simple for the patient. In addition, after completing the exercises, the patient could complete a table indicating the perceived exertion using a Likert scale. If the exertion scale was between 0 and 5, the individual should progress to the next stage of the exercise for the next session (e.g. from sitting to standing or using a different tool). If the exertion scale was between 6 and 8, the exercise volume and intensity level should be maintained. If the exertion level was between 9 and 10, the number of repetitions should be reduced or the position should be modified (for example, switching from a standing position to a sitting one). This program was followed by the participants for eight weeks, three times a week and a total of twenty-four sessions.
Statistical analysis
The analysis of the covariance (ANCOVA) test was used to assess the efficacy of mini-trampoline exercise and ankle exercise therapy and interventions. The pre-test score of the groups was considered as a covariance or control variable in this test, and its effect was neutralized. The post-hoc comparison test of Bonferroni was also used to compare the post-test of three groups. The pre and post-test times for each group’s mean scores were compared separately using a paired or paired t-test. SPSS software, version 27 was used to analyze the data.
3. Results
Table 1 presents the characteristics of the current research participants, including age, height, weight, body mass index, history of diabetes, duration of neuropathy, and hemoglobin A1c (HBA1C) (P>0.05).
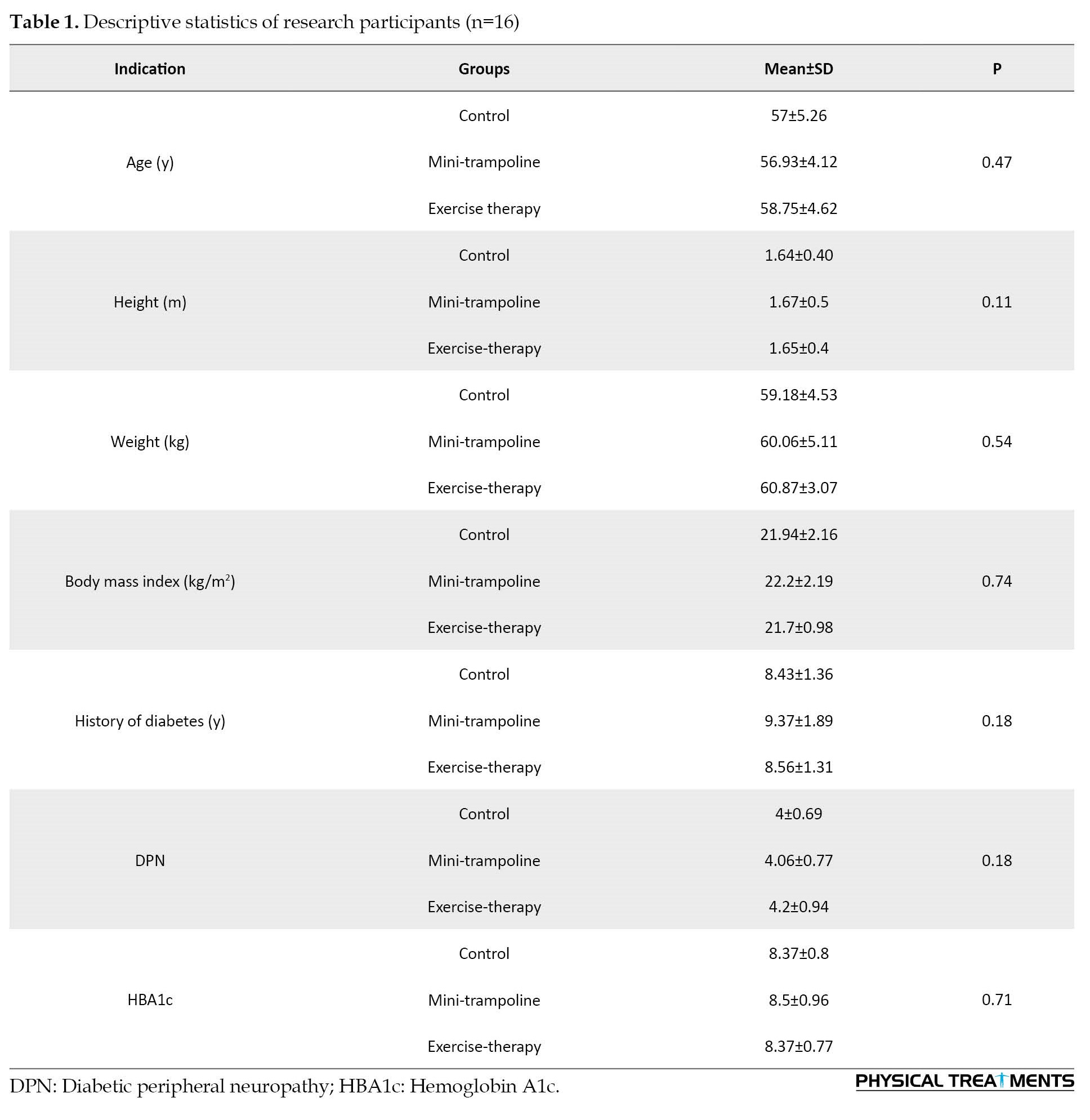
Table 2 presents the results of ANCOVA used to investigate and compare the effectiveness of both mini-trampoline exercise and ankle exercise therapy interventions on foot mobility.
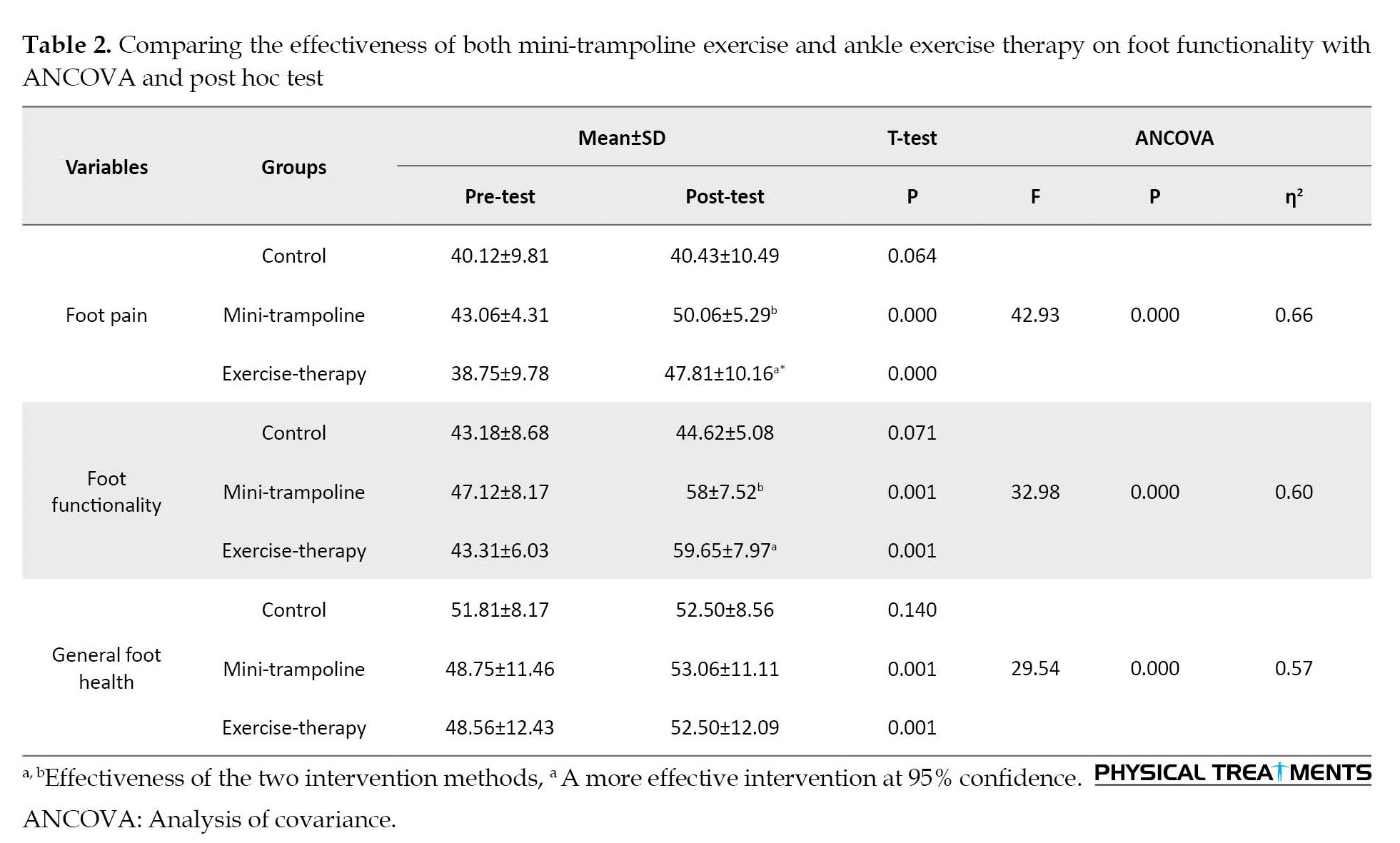
The results of ANCOVA revealed that mini-trampoline exercise and therapeutic exercise interventions were significantly effective on plantar mobility at a confidence level of at least 95% (P<0.05) (Table 2). Also, the paired t-test results revealed a difference between the pre-test and post-test mean scores in the two intervention groups for all variables listed in Table 2 (P<0.05), but no significant difference was found in the control group between the pre-test and post-test mean scores (P>0.05). Post hoc Bonferroni test showed that therapeutic exercise intervention was more effective than mini-trampoline intervention regarding two variables of foot pain and foot functionality (P<0.05).
Table 3 presents the results of ANCOVA used to investigate and compare the effectiveness of mini-trampoline interventions and ankle exercise therapy on ankle range of motion.
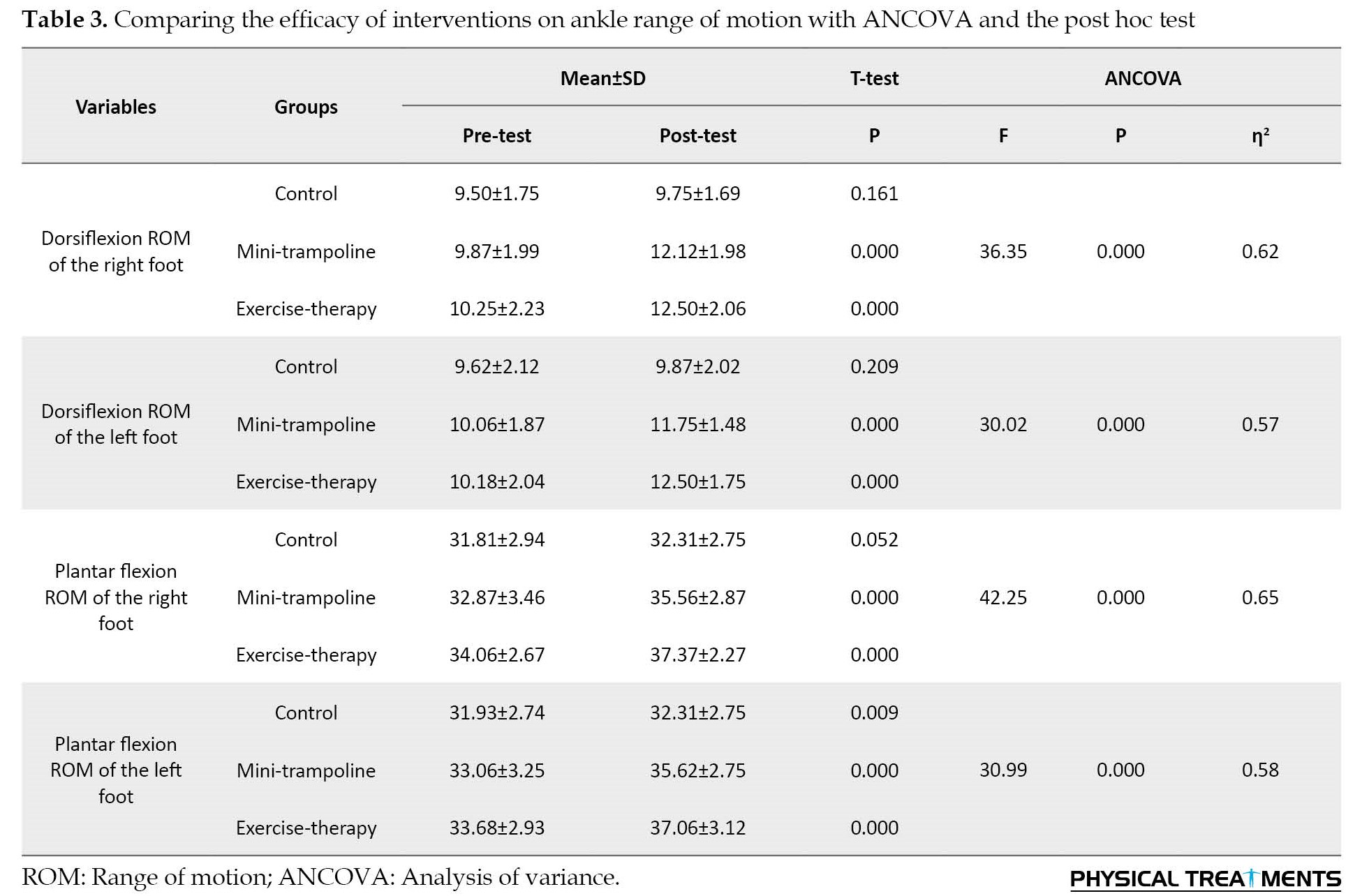
The results of ANCOVA demonstrated that mini-trampoline and ankle exercise therapy interventions were significantly effective on the ankle range of motion at the 95% confidence level (P<0.05) (Table 3). Furthermore, the paired t-test results revealed a difference between the pre-test and post-test mean scores in the two intervention groups for all variables mentioned in Table 3 (P<0.05), while no significant difference was observed between the pre and post-test mean scores in the control group (P>0.05). The post hoc Bonferroni test showed no difference in the effectiveness of the two interventions on ankle range of motion (P<0.05).
Table 4 presents the results of ANCOVA used to investigate and compare the effectiveness of mini-trampoline interventions and ankle exercise therapy on the range of motion of the first metatarsal joint.
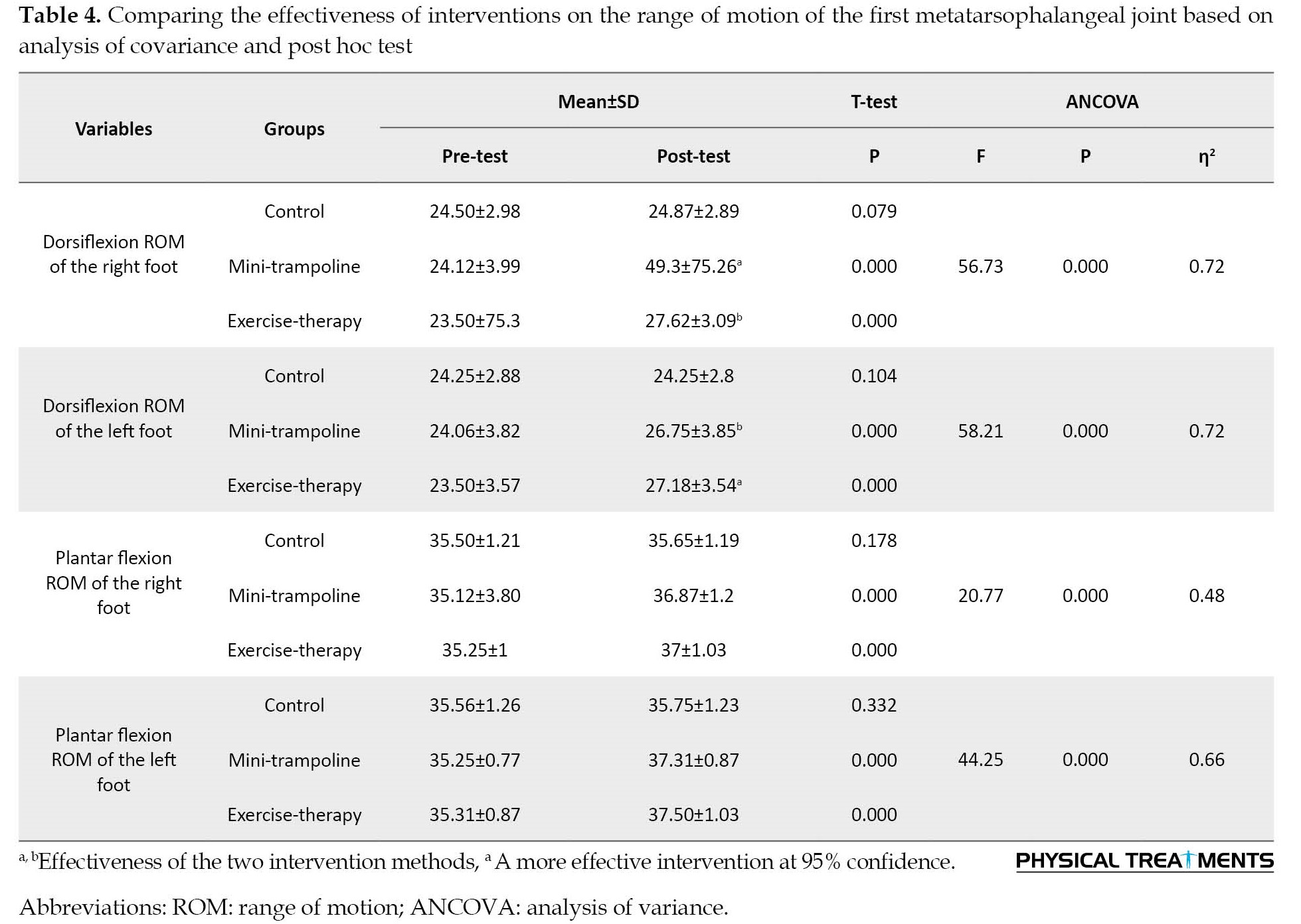
The results of ANCOVA revealed that, at a confidence level of at least 95%, both mini-trampoline and ankle therapeutic exercise interventions were effective on the first metatarsophalangeal joint’s range of motion (P<0.05) (Table 4). In addition, the paired t-test results showed a difference between the pre and post-test mean scores in the two intervention groups for all variables listed in Table 4 (P<0.05). However, no significant difference was observed between the pre-test and post-test mean sores in the control group (P>0.05). The Bonferroni’s post hoc test revealed that the mini-trampoline intervention was more effective than the ankle therapeutic exercise regarding the variables of dorsiflexion ROM of the both right and left foot (P<0.05).
Table 5 presents the results of ANCOVA to investigate and compare the effectiveness of mini-trampoline exercise and ankle exercise therapy interventions regarding the range of ankle strength.
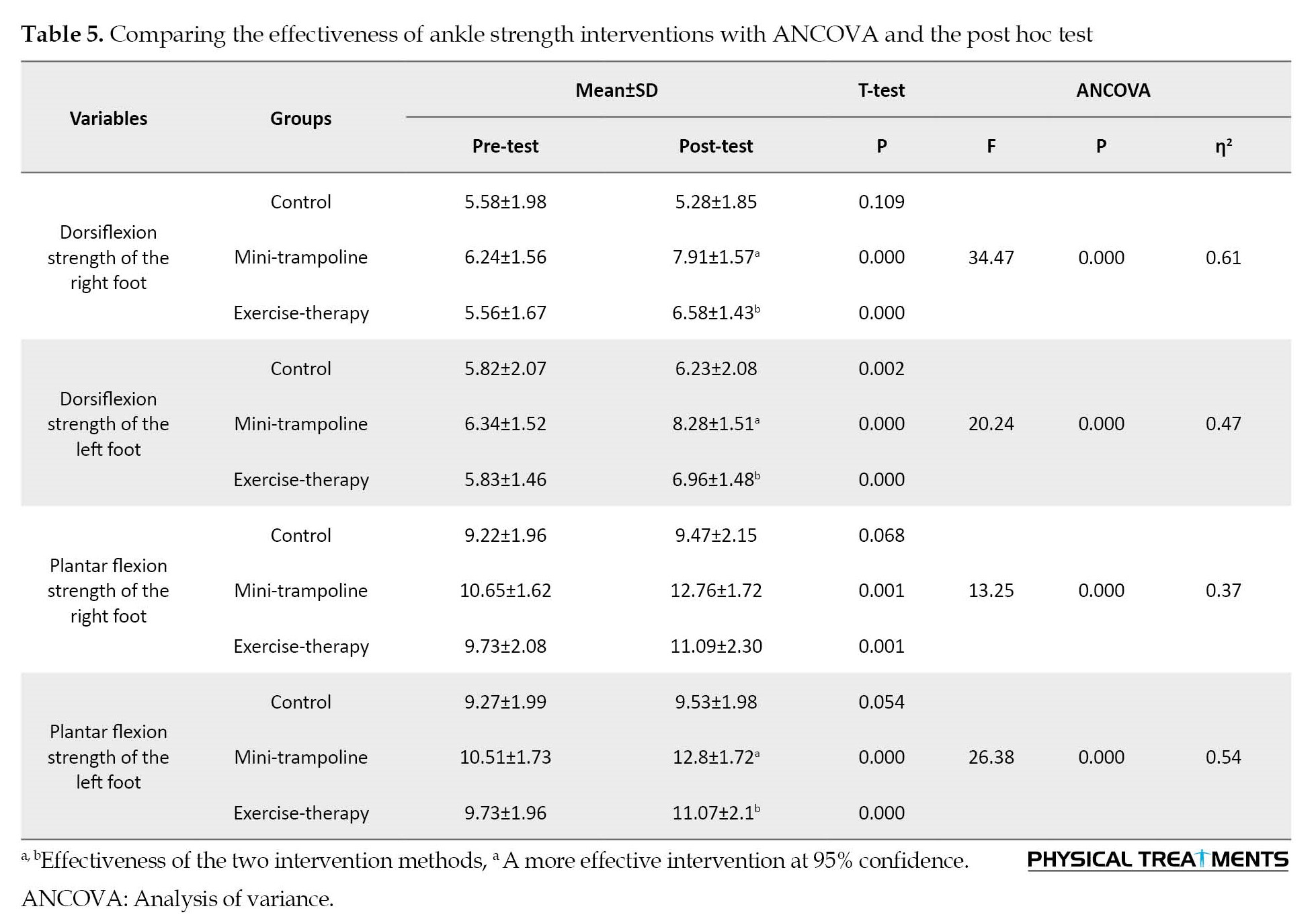
The results of ANCOVA showed that at the confidence level of at least 95%, two mini-trampoline interventions and ankle therapeutic exercise were significantly effective on ankle strength variables (P<0.05) (Table 5). Also, the results of the paired t-test showed a difference between the pre-test and post-test mean scores in both intervention groups in all the variables listed in Table 5 (P<0.05). In the control group, the pre-test and post-test mean values were not significantly different except for one variable (Dorsiflexion strength of the left foot) (P>0.05). The post hoc Bonferroni test showed no difference between the two intervention groups in the plantar flexion strength of the right foot, but in the three variables of the dorsiflexion strength of the right and left foot and the plantar flexion strength of the left foot, the mini-trampoline intervention was more effective than the ankle exercise therapy intervention (P<0.05).
Table 6 presents the results of ANCOVA to investigate and compare the effectiveness of mini-trampoline exercise and ankle exercise therapy interventions on the strength of the hallux.
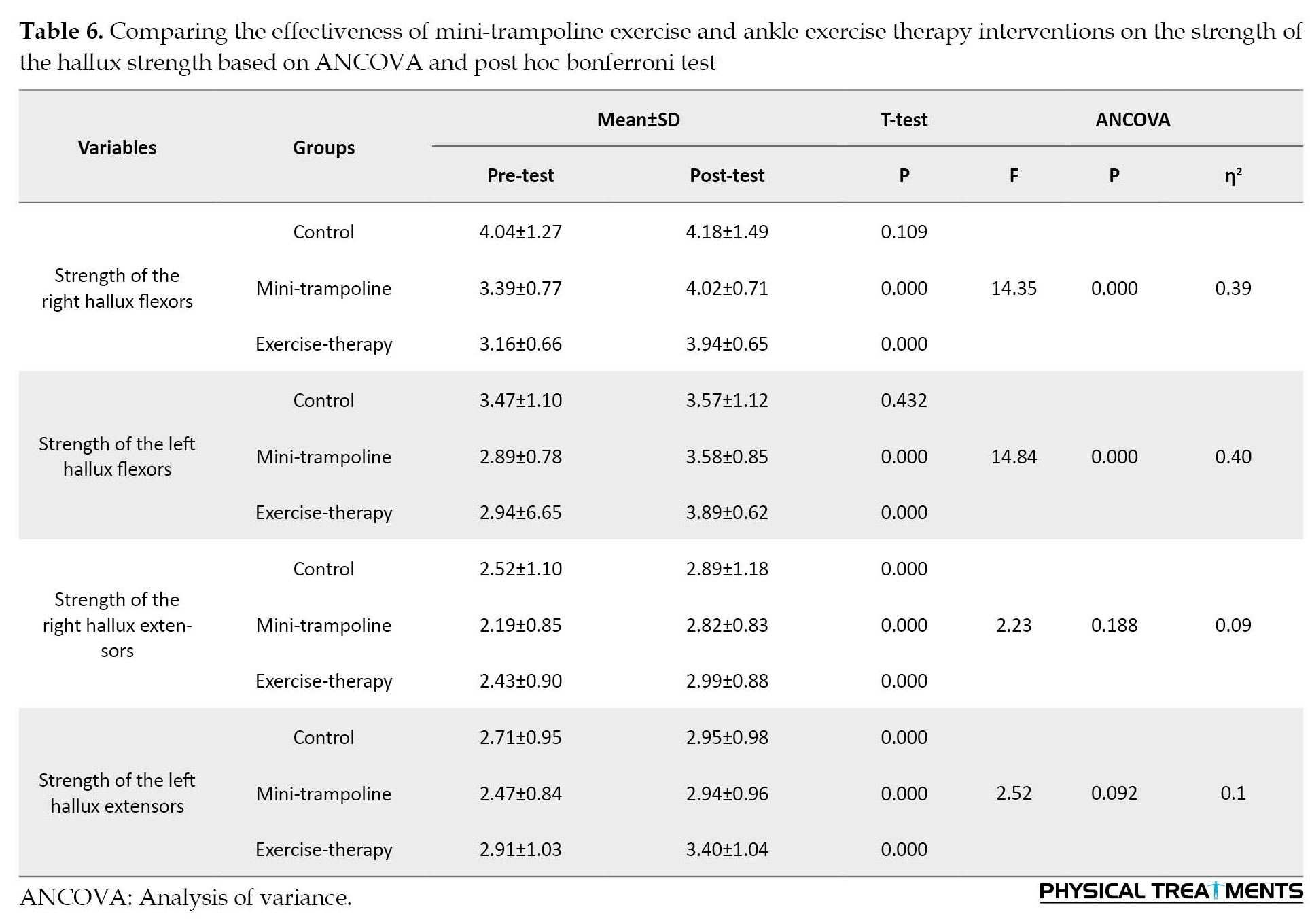
The results of ANCOVA showed that at the confidence level of at least 95%, both mini-trampoline exercise and ankle therapeutic exercise interventions were significantly effective on the two variables of the hallux strength (P<0.05) (Table 6). The efficacy of any of the two interventions for right and left hallux extension strength was not confirmed (P>0.05). The paired t-test results revealed a difference in both intervention groups’ pre and post-test mean scores in the right and left hallux flexion strength (P<0.05). However, no significant difference was observed between the pre and post-test mean scores in the control group (P>0.05). Post hoc Bonferroni test showed that the effectiveness of both interventions on the strength variables of the hallux was similar and no significant difference was observed (P>0.05).
4. Discussion
The findings showed that weight-bearing exercises on the mini-trampoline and ankle exercise therapy program in the interventional groups compared to the control group resulted in a significant improvement in foot sole mobility, ankle ROM, first metatarsophalangeal joint ROM, isometric strength of ankle dorsiflexion and plantarflexion and hallux dorsiflexion and plantarflexion. These results were consistent with the results of studies conducted by other researches [14, 24, 29, 30].
Kanchanasamut et al. (2017) investigated the effect of a weight-bearing exercise program on a mini-trampoline on foot mobility, plantar pressure, and sensation in diabetic foot neuropathy. This study included 24 patients with diabetic neuropathy in one control and two experimental groups. The control group only received the foot care program, while the experimental group participated in exercises for eight weeks. The results showed that weight-bearing exercises for eight weeks improve the perception of vibration [14].
Sartor et al. (2014) analyzed the effect of functional, strengthening, and stretching exercises on foot function in patients with diabetic neuropathy. A total of 55 patients with diabetic neuropathy participated in this research. The control group received medication, as well as medical care, and foot care instructions, and the experimental group performed exercises for 12 weeks. The results revealed changes in the rocking motion of the foot during walking, improved distribution of plantar pressure, and better functional status of the ankle [28].
The study entitled “exercise therapy improves plantar pressure distribution in patients with diabetic peripheral neuropathy” conducted by Fayed et al. (2016) included forty women with DPN. The control group received treatment and medical care, while the experimental group received medical treatment as well as physiotherapy interventions and stretching, strengthening, balance, and walking exercises. The findings demonstrated that physiotherapy intervention can significantly prevent the occurrence of diabetic ulcers in patients with diabetic neuropathy. The outstanding changes in this study were supported by pressure distribution, peak plantar pressure, and foot contact area [29].
Cerrahoglu et al. (2016) evaluated the effect of ROM and plantar pressure on diabetic patients with and without neuropathy on foot care exercises. The study included 76 diabetic patients, and the exercise groups followed their respective training programs for four weeks. The findings demonstrated that a home exercise program can be an effective preventive method to improve ROM in the foot joints and plantar pressure distribution in diabetic patients, regardless of the presence or absence of neuropathy [30].
All previous studies have shown that exercise programs and treatment protocols are effective in improving musculoskeletal health, balance, preventing further complications, and increasing patients’ independence in performing daily activities. However, the mentioned exercises typically target larger joints and lower limb muscles, with a primary focus on walking training, whereas both protocols in the current study target musculoskeletal defects of distal and smaller joints and muscles, as well as intrinsic and extrinsic muscles which are the most damaged in neuropathic patients and their functions and biomechanics are affected under dynamic conditions. In neuropathy patients, movement disorders in the distal muscles are seen with a 15%-20% decrease in the maximum ankle isokinetic moment, as well as atrophy of the inner foot muscles. In addition, the greater the plantar overload under the corresponding part during walking, the lower the lateral mobility of the forefoot in the first metatarsophalangeal joint, inversion, and eversion of the subtalar joint. As a result, the target of the relevant exercise protocols in the present study was the interphalangeal, metatarsophalangeal, ankle joints, and muscle groups on the medial plantar side, lateral plantar side, median plantar side, and dorsal plantar side, which resulted in increased mechanical properties of the calcaneal tendon, reduced foot fat, increased isometric muscle strength of the toes and hallux, increased the ankle extensor torque and strength, increased the ROM of the ankle in the sagittal plane, increased the conduction speed of the peroneal motor nerve and the sural sensory nerve, reduced plantar numbness, expanded peripheral microvasculature and changed vascular function, as well as improved sensory and motor afferent function [14, 15, 17, 18, 20]. As a result, mini-trampoline and ankle therapeutic exercises can be used as a simple, affordable, low-risk, and quick-improvement treatment program that focuses on the integration of peripheral strengthening using segmental exercises for foot function, which improves diabetic patient’s quality of life.
5. Conclusion
According to the findings, the exercise protocols used in this study, which were completely focused on the musculoskeletal dysfunction caused by DPN, can be effective in reducing musculoskeletal dysfunctions caused by this problem, and included in patients’ daily activities as a self-care strategy to minimize the harmful consequences of DPN.
Study limitations
The small sample size and short-term follow-up of the exercise program’s effects were the study’s main shortcomings. It is suggested that further comparative studies using exercise routines and a larger sample size should be conducted to evaluate their impact on the management of DPN. Furthermore, given the paucity of studies designing exercise programs such as mini-trampoline and ankle therapy exercise programs to prevent and control diabetes in women with peripheral neuropathy, it is recommended to conduct more research in this area.
Ethical Considerations
Compliance with ethical guidelines
The Research Ethics Committee of the Institute of Sports Sciences approved all research processes and methods in terms of ethical considerations (Code: IR.SSRI.REC 1400.1311). Also, written informed consent was obtained from all participants.
Funding
The paper was extracted from the PhD thesis of Ashraf Ansari, approved by Department of Sport Injury and Corrective Exercise, Tehran University.
Authors' contributions
Conceptualization, methodology, resources, visualization, original data preparation and analysis, writing- original draft, review and editing: Ashraf Ansari; Supervision: Mohammad Karimizadeh Ardakani and Mahdieh Akoochakian
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors express their deepest gratitude to all the subjects who participated in this research.
References
Diabetes is the most common endocrine disease, one of the leading causes of death in most countries, and unquestionably one of the most pressing health issues in the world today [1, 2, 3]. Diabetes causes a broad spectrum of complications. The most common long-term complication of this disease is peripheral neuropathy. According to the national diabetes information center, more than 50% of those with diabetes have some form of neuropathy, even if they have no symptoms. Diabetic peripheral neuropathy (DPN) is a neurological disorder that affects the sensitivity and excitability of the nerves of the feet and hands [4, 5] resulting in a stabbing or burning sensation, numbness, and tingling in lower limbs [6, 7, 8,]. Foot disorders are the main problem related to diabetic neuropathy, leading to a significant deal of pain and social costs for patients [9, 10,]. Numbness in one or both feet is frequently the early symptom. Therefore, people with DPN are more likely to develop foot ulcers and are at a higher risk of having their foot amputated at the ankle or below knee level [11].
DPN also causes musculoskeletal dysfunction due to sensory-motor disorders which include changes in the joints surrounding the tissues, as well as a decrease in function and strength of feet due to atrophy of the inner lower foot muscles. Furthermore, it causes decreased mobility of the ankle and the first metatarsophalangeal joint, which can result in high plantar pressure under the metatarsal heads and loss of function of the toes, particularly the big toe. These effects are the primary contributors to the formation of deformities and high pressures on the soles of the feet, which affect the stability of foot dynamics and cause changes in the biomechanics of walking, such as a reduction in walking speed and ankle dorsi and plantar flexion, as well as a decrease in torque force around the ankle joint, a delay in muscle activation in the legs and thighs, and an increase in torque force in the hip joint [7]. As a result of these changes, patients with DPN typically exhibit more disturbance in posture and walking, along with difficulties performing daily activities [12, 13].
A growing body of evidence supports the impact of exercise on neuropathy management. Exercise improves glucose control and increases insulin sensitivity throughout the body. It lowers circulating fat levels, stimulating angiogenesis and increasing perfusion, physical performance, and balance, and lowering depression, anxiety, and the risk of falling in DNP patients [14]. Strength, stretching, balance, and resistance training programs have been shown to improve muscle strength, endurance, and flexibility, and can lead to increased range of motion (ROM) and muscle strength [15-19].
Proper foot and ankle exercises are among the other appropriate exercises investigated in this study. On the one hand, these exercises have beneficial results in reducing negative factors of diabetic foot pathogenesis and may lead to increased nerve speed of the lower limbs and muscle strengthening, improved ROM of the ankle, redistributed sole and plantar pressure during walking, and as a result, a better physiological pattern. More positive effects, such as increased skin sensitivity and intraepidermal nerve fiber density can be achieved by performing appropriate ankle exercises in diabetic patients, which can delay the usual process of DPN, skin damage, and wounding [20].
On the other hand, increased weight-bearing activities can result in increased pressure on the soles of the feet and, as a result, foot ulcers. Therefore, the American Diabetes Association advises people with diabetic neuropathy to exercise properly and to limit activities that require bearing body weight. Trampoline exercise has recently been shown to improve balance control in the elderly [21], as well as athletic performance, rehabilitation, injury recovery, and foot function in athletes with ankle instability [22].
Exercises on the mini-trampoline and ankle therapeutic exercises at home can be effective in improving patients’ quality of life as a simple, affordable, low-risk, and quick-improvement treatment program that focuses on the use of segmental exercises for foot function. However, to our knowledge, no earlier study has been conducted to evaluate the effects of a foot and ankle treatment program capable of personalizing special foot treatment exercises at home aimed at preventing and treating musculoskeletal defects and complications in patients with diabetic neuropathy. Therefore, more research in this field is required to strengthen the level of evidence based on the use of specific ankle therapeutic exercises to reduce risk factors and prevent further complications.
Thus, this study aims to examine whether providing appropriate solutions based on therapeutic strategies for musculoskeletal abnormalities related to DPN, including self-care instructions and home exercises (ankle therapeutic exercises and weight-bearing exercises on a mini-trampoline), can improve the health and performance of the foot and ankle ROM.
2. Materials and Methods
The current study is a clinical trial study with two experimental groups and one control group. The statistical population of this study includes 48 women who suffered from type 2 diabetes for at least 7 years with an average age of 50 to 65 years and a history of moderate or severe peripheral neuropathy with decreased sensation in the feet that had been previously diagnosed by a medical doctor. The sample size was estimated using G Power software. The software was programmed with the assumption of a large effect size (80%), at a level of 5% error probability and 95% power. The total sample size calculated by the software for three groups was 48 people with 16 subjects in each group. This study was conducted at the Parsian diabetes clinic in Tehran.
After receiving informed consent, volunteers who met the eligibility criteria were randomly assigned into two intervention groups and one control group. During the exercise intervention period, all three groups received foot care training and medical team recommendations, which included, foot hygiene, daily washing and careful drying of the feet, especially between the toes, use of non-elastic and seamless socks, trimming the nails in a square shape, preventing unsupervised removal of calluses or blisters, not wearing shoes or slippers without socks, and seeking medical attention if problems with the feet are discovered. During the study, subjects in all three groups did not receive any other concurrent care, such as physiotherapy, acupuncture, or any other non-conventional medical intervention. Cramping, moderate to severe pain, fatigue, dizziness, fear, or any condition that exposed the patient to discomfort were all reasons for stopping the session.
To validate the training protocols, all participants underwent two measurement sessions (before and after the intervention) to measure the flexion and extension angles of the first metatarsophalangeal joint with a goniometer, the ROM of the ankle with an electro goniometer, and the isometric strength of the foot with a hand-held dynamometer. The researcher performed all measurements in the presence of a medical doctor and physiotherapist.
Research instruments
All participants completed the Brazilian version of the Michigan neuropathy screening instrument (MNSI) questionnaire to determine the presence of DPN. In this research, the Brazilian-Portuguese version of the foot health status questionnaire (FHSQ-BR) was used to assess foot health [23, 24]. Flexion and extension angles (first) ([metatarsophalangeal joints] MTPJ) were measured with a goniometer using the dynamic ROM measurement method. For analysis, the mean values of three maximum flexion and maximum extension records were calculated [14]. An electro-goniometer (model DSI [Danesh Salar Iranian]) with a measurement accuracy of 1 degree was used to evaluate the ROM of the ankle flexion and extension, and the mean scores of three records of maximum flexion and maximum extension were calculated for analysis [23, 24]. The strength peak muscle force (kg) was measured by a maximum isometric voluntary contraction in ankle dorsi and plantar flexion and hallux dorsi and plantar flexion using a hand-held push-pull dynamometer. Each muscle group should be tested with a 3-5 s contraction. Three repetitions were performed for each foot muscle group, with a minimum of 10 s of rest between each, and the mean scores of three measurements were used for data analysis [25, 26].
Exercise protocols
The first experimental group exercised on a mini-trampoline at home [14]. The mini-trampoline training program consisted of four levels of progression over eight weeks. The participants were instructed to perform each exercise with 10 repetitions for two weeks, at least three times per week, and hold the position for up to 10 s in static exercises. The exercise program was performed daily in three sets with 5-minute rest intervals between them. To warm up and cool down, participants were asked to stretch quadriceps, hamstrings, biceps, and soleus muscles. Each muscle was stretched 3 times with a 20 s rest between each. In addition, the participants were asked to wear appropriate footwear and inspect their feet after the exercises. Discontinuation criteria for each session included cramping, moderate to severe pain, fatigue, dizziness, or any condition that exposed the patient to any discomfort [14].
The ankle exercise-therapy program was carried out by the second experimental group. This program included exercises to strengthen the internal and external foot and ankle muscles [27]. Six exercises were performed, four exercises for the inner foot muscles and two exercises for the outer foot and ankle muscles. Exercises were done using tools, such as cotton ball, pencils, balls, and chairs. The interphalangeal, metatarsophalangeal, and ankle joints were targeted in this protocol, with emphasis on the following muscle groups, medial plantar side (abductor hallucis, flexor hallucis brevis, and adductor hallucis), lateral plantar side (abductor digiti minimi, flexor digiti minimi, and opponens digiti minimi), median plantar side (flexor digitorum brevis, quadratus plantar, lumbrical muscle, plantar interosseous muscle, and dorsal interosseous muscle) and dorsal plantar side (extensor digitorum brevis, and extensor hallucis brevis). Foot exercises were performed first in a sitting position and one set of 30 repetitions, then in a standing position and standing on one foot if the exercise was very simple for the patient. In addition, after completing the exercises, the patient could complete a table indicating the perceived exertion using a Likert scale. If the exertion scale was between 0 and 5, the individual should progress to the next stage of the exercise for the next session (e.g. from sitting to standing or using a different tool). If the exertion scale was between 6 and 8, the exercise volume and intensity level should be maintained. If the exertion level was between 9 and 10, the number of repetitions should be reduced or the position should be modified (for example, switching from a standing position to a sitting one). This program was followed by the participants for eight weeks, three times a week and a total of twenty-four sessions.
Statistical analysis
The analysis of the covariance (ANCOVA) test was used to assess the efficacy of mini-trampoline exercise and ankle exercise therapy and interventions. The pre-test score of the groups was considered as a covariance or control variable in this test, and its effect was neutralized. The post-hoc comparison test of Bonferroni was also used to compare the post-test of three groups. The pre and post-test times for each group’s mean scores were compared separately using a paired or paired t-test. SPSS software, version 27 was used to analyze the data.
3. Results
Table 1 presents the characteristics of the current research participants, including age, height, weight, body mass index, history of diabetes, duration of neuropathy, and hemoglobin A1c (HBA1C) (P>0.05).
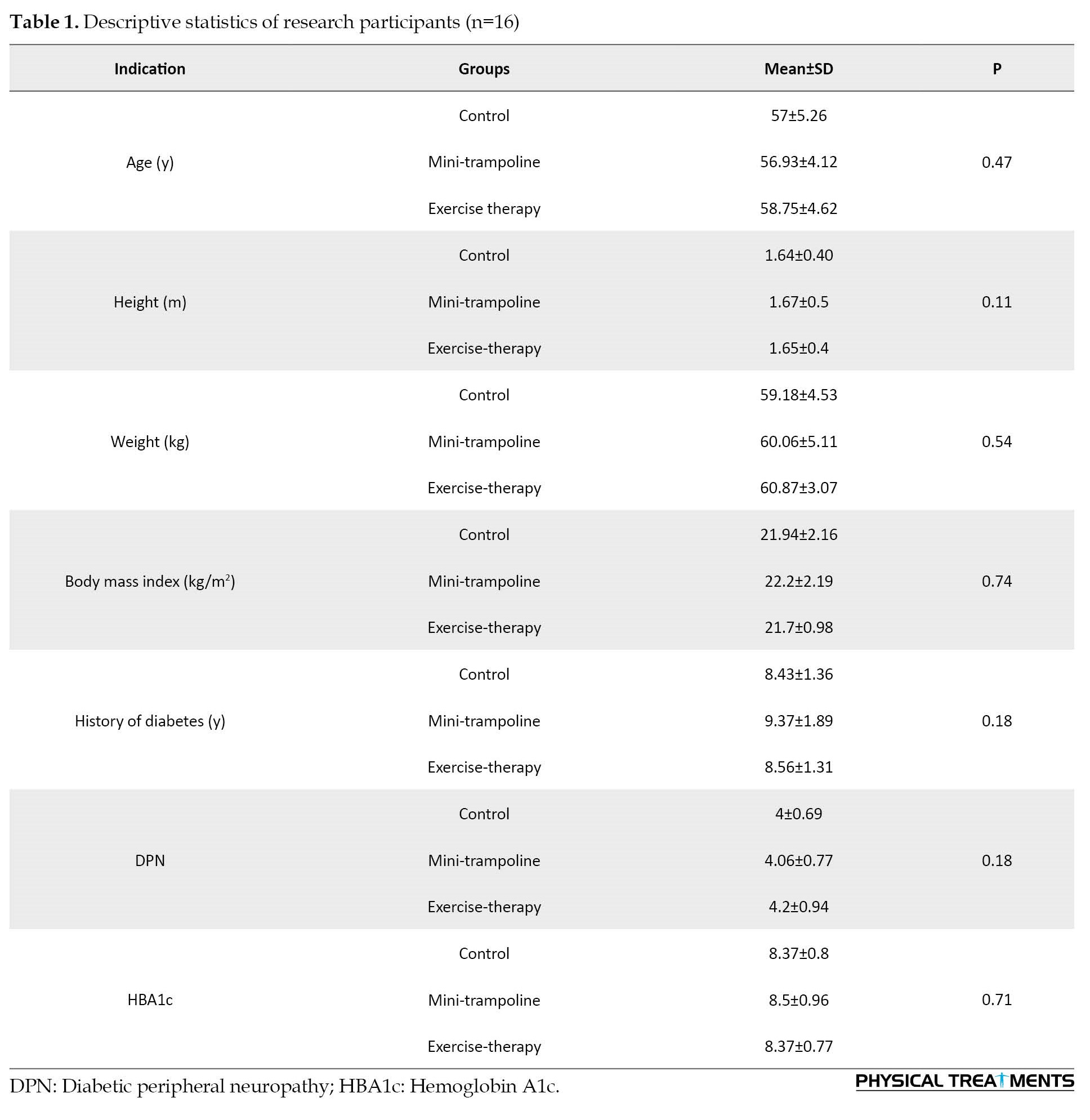
Table 2 presents the results of ANCOVA used to investigate and compare the effectiveness of both mini-trampoline exercise and ankle exercise therapy interventions on foot mobility.
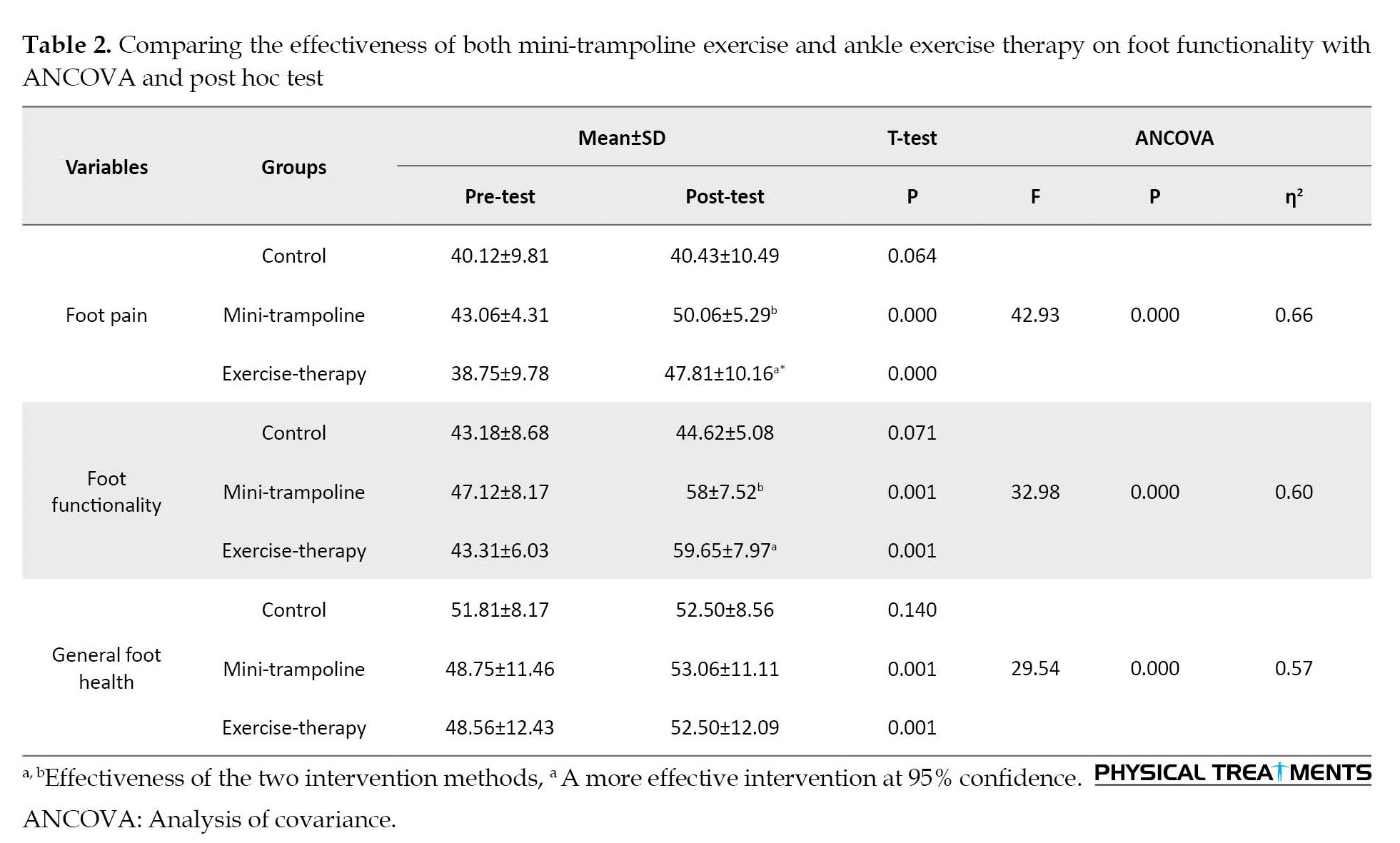
The results of ANCOVA revealed that mini-trampoline exercise and therapeutic exercise interventions were significantly effective on plantar mobility at a confidence level of at least 95% (P<0.05) (Table 2). Also, the paired t-test results revealed a difference between the pre-test and post-test mean scores in the two intervention groups for all variables listed in Table 2 (P<0.05), but no significant difference was found in the control group between the pre-test and post-test mean scores (P>0.05). Post hoc Bonferroni test showed that therapeutic exercise intervention was more effective than mini-trampoline intervention regarding two variables of foot pain and foot functionality (P<0.05).
Table 3 presents the results of ANCOVA used to investigate and compare the effectiveness of mini-trampoline interventions and ankle exercise therapy on ankle range of motion.
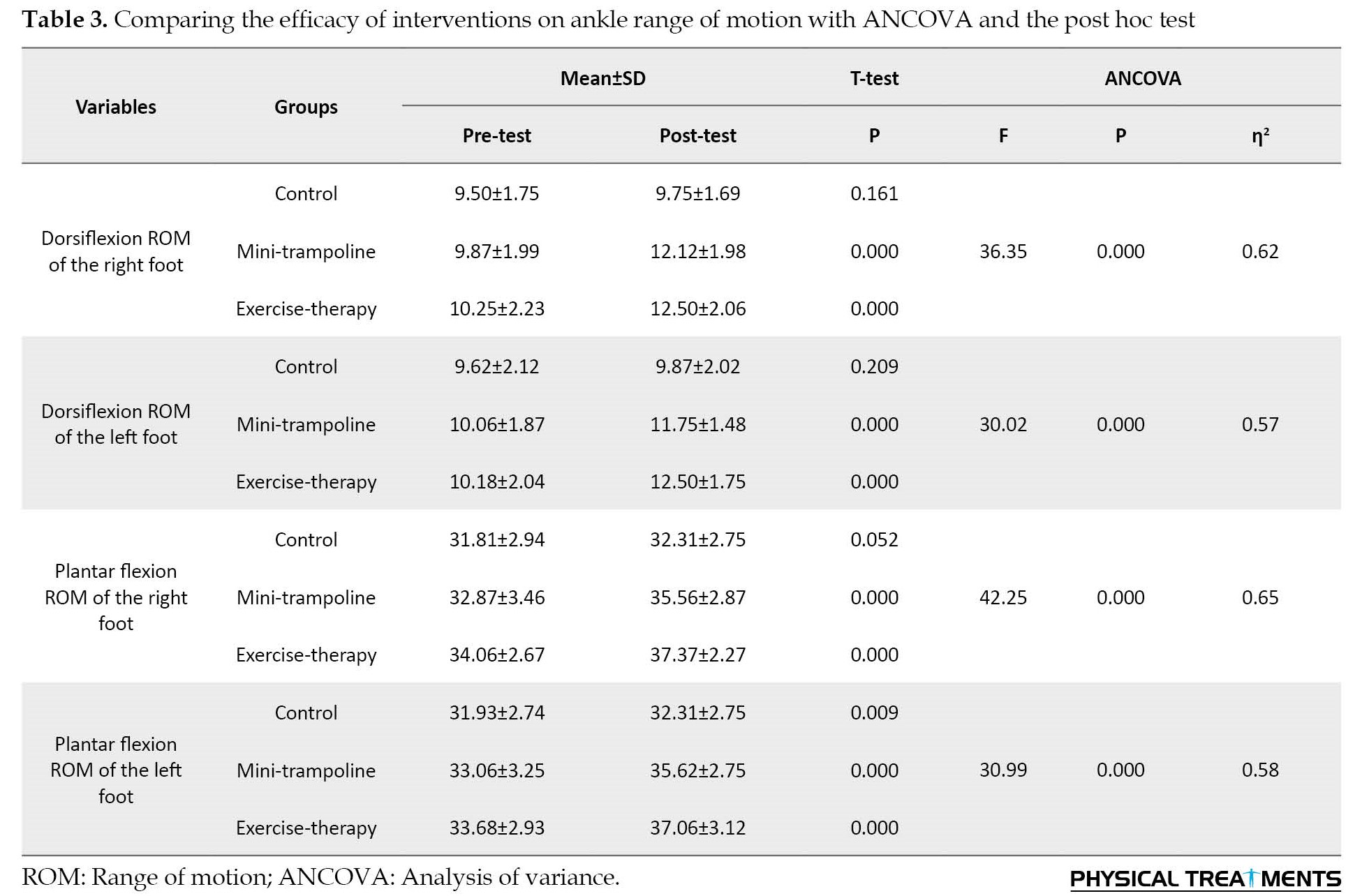
The results of ANCOVA demonstrated that mini-trampoline and ankle exercise therapy interventions were significantly effective on the ankle range of motion at the 95% confidence level (P<0.05) (Table 3). Furthermore, the paired t-test results revealed a difference between the pre-test and post-test mean scores in the two intervention groups for all variables mentioned in Table 3 (P<0.05), while no significant difference was observed between the pre and post-test mean scores in the control group (P>0.05). The post hoc Bonferroni test showed no difference in the effectiveness of the two interventions on ankle range of motion (P<0.05).
Table 4 presents the results of ANCOVA used to investigate and compare the effectiveness of mini-trampoline interventions and ankle exercise therapy on the range of motion of the first metatarsal joint.
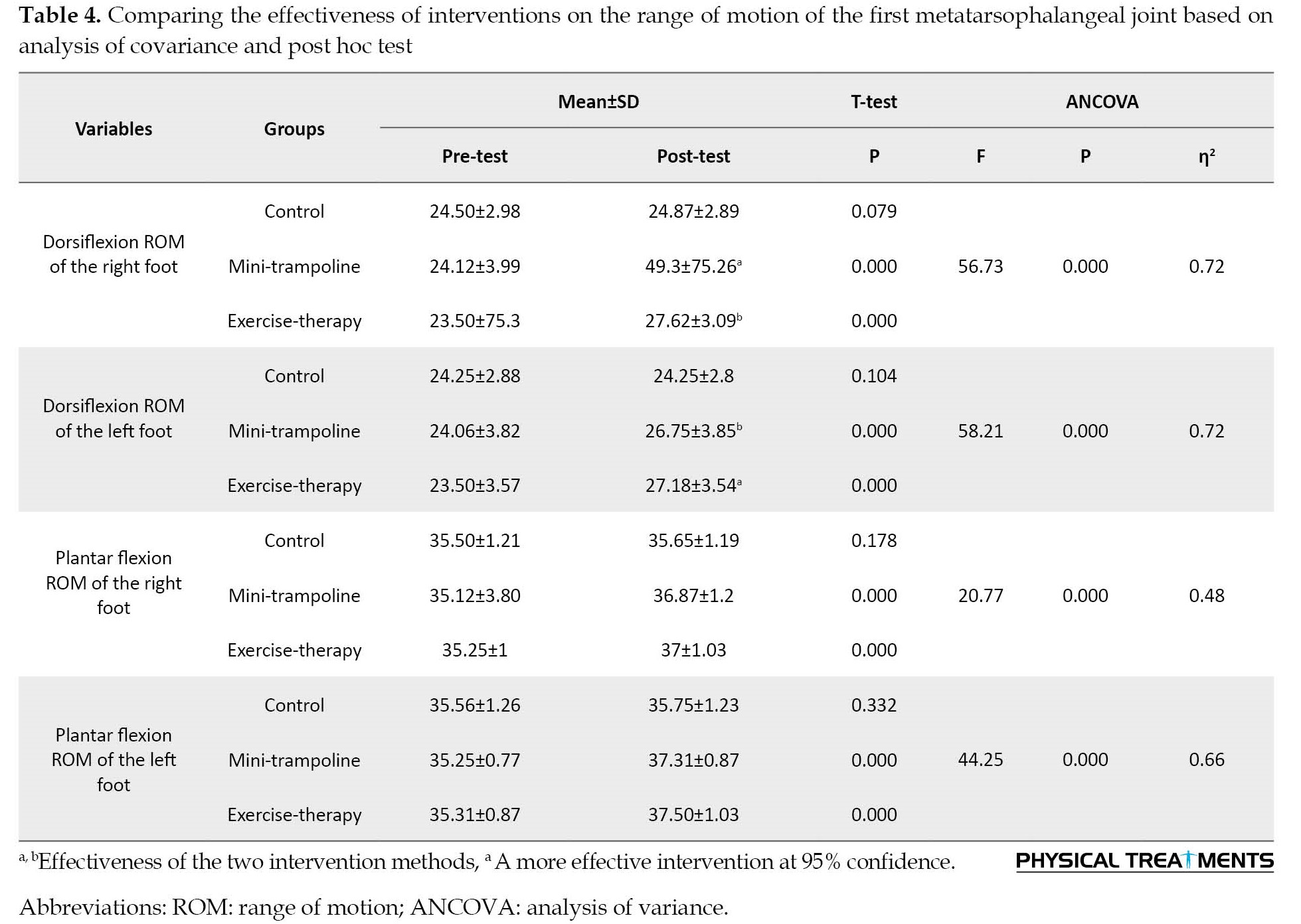
The results of ANCOVA revealed that, at a confidence level of at least 95%, both mini-trampoline and ankle therapeutic exercise interventions were effective on the first metatarsophalangeal joint’s range of motion (P<0.05) (Table 4). In addition, the paired t-test results showed a difference between the pre and post-test mean scores in the two intervention groups for all variables listed in Table 4 (P<0.05). However, no significant difference was observed between the pre-test and post-test mean sores in the control group (P>0.05). The Bonferroni’s post hoc test revealed that the mini-trampoline intervention was more effective than the ankle therapeutic exercise regarding the variables of dorsiflexion ROM of the both right and left foot (P<0.05).
Table 5 presents the results of ANCOVA to investigate and compare the effectiveness of mini-trampoline exercise and ankle exercise therapy interventions regarding the range of ankle strength.
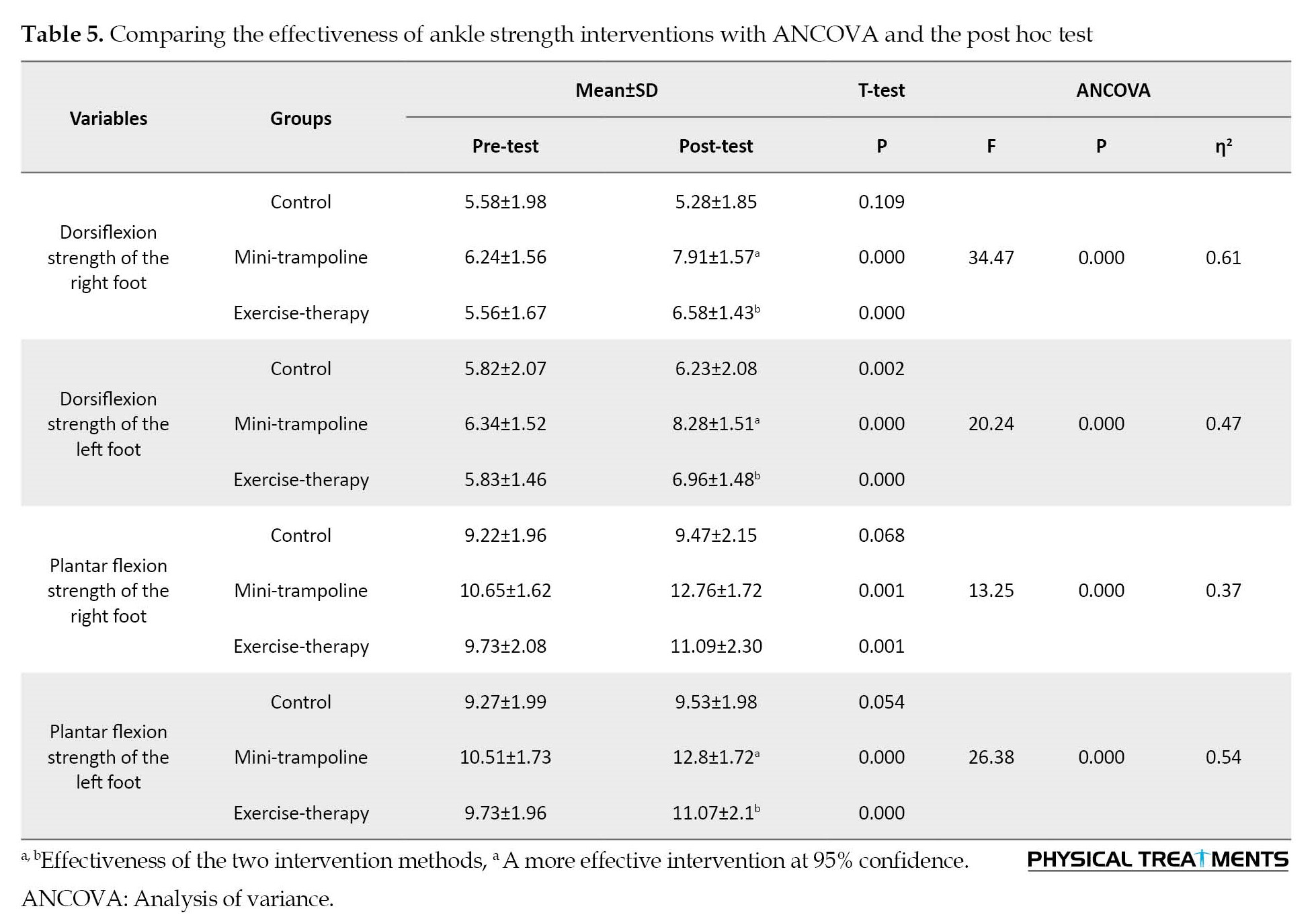
The results of ANCOVA showed that at the confidence level of at least 95%, two mini-trampoline interventions and ankle therapeutic exercise were significantly effective on ankle strength variables (P<0.05) (Table 5). Also, the results of the paired t-test showed a difference between the pre-test and post-test mean scores in both intervention groups in all the variables listed in Table 5 (P<0.05). In the control group, the pre-test and post-test mean values were not significantly different except for one variable (Dorsiflexion strength of the left foot) (P>0.05). The post hoc Bonferroni test showed no difference between the two intervention groups in the plantar flexion strength of the right foot, but in the three variables of the dorsiflexion strength of the right and left foot and the plantar flexion strength of the left foot, the mini-trampoline intervention was more effective than the ankle exercise therapy intervention (P<0.05).
Table 6 presents the results of ANCOVA to investigate and compare the effectiveness of mini-trampoline exercise and ankle exercise therapy interventions on the strength of the hallux.
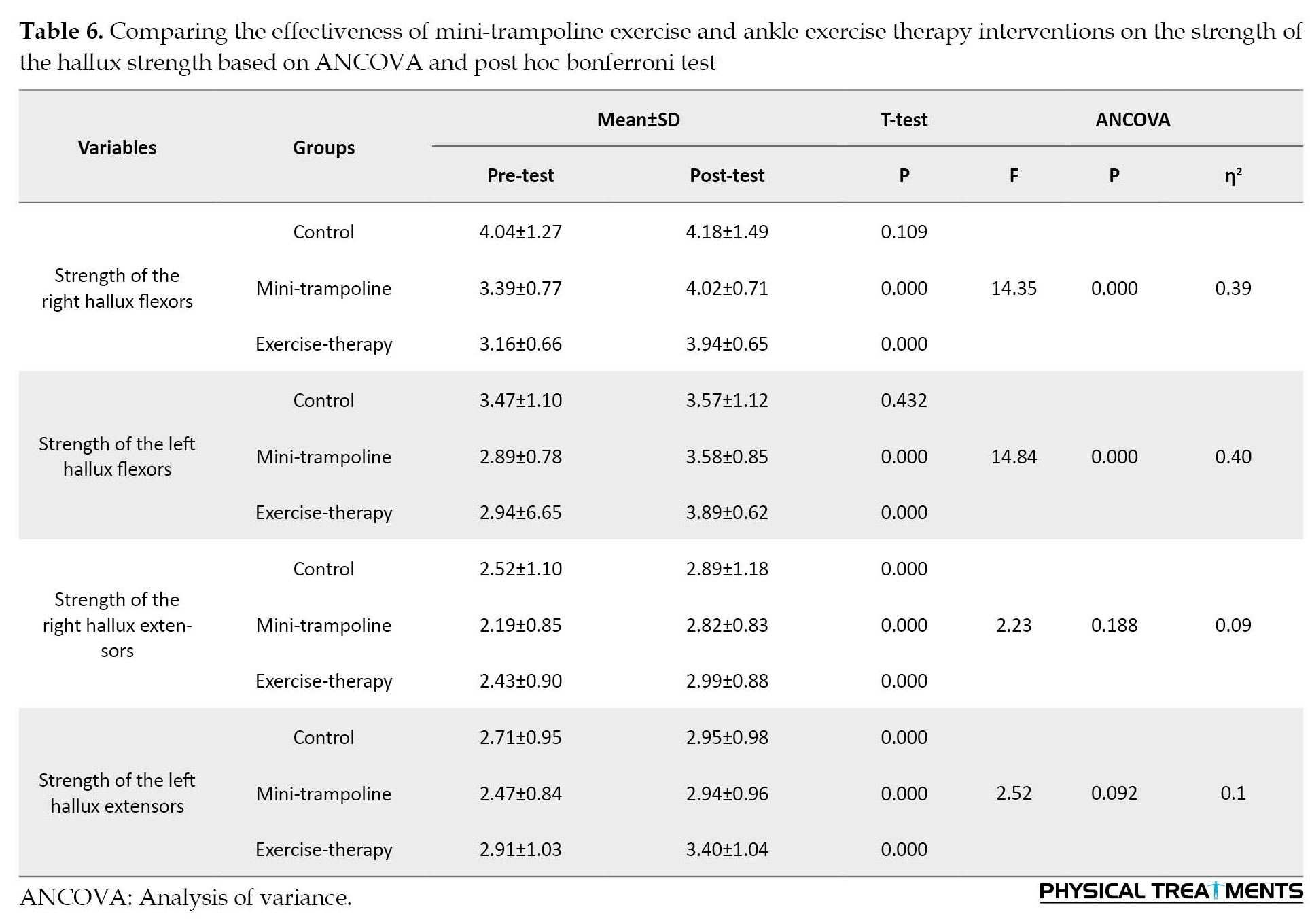
The results of ANCOVA showed that at the confidence level of at least 95%, both mini-trampoline exercise and ankle therapeutic exercise interventions were significantly effective on the two variables of the hallux strength (P<0.05) (Table 6). The efficacy of any of the two interventions for right and left hallux extension strength was not confirmed (P>0.05). The paired t-test results revealed a difference in both intervention groups’ pre and post-test mean scores in the right and left hallux flexion strength (P<0.05). However, no significant difference was observed between the pre and post-test mean scores in the control group (P>0.05). Post hoc Bonferroni test showed that the effectiveness of both interventions on the strength variables of the hallux was similar and no significant difference was observed (P>0.05).
4. Discussion
The findings showed that weight-bearing exercises on the mini-trampoline and ankle exercise therapy program in the interventional groups compared to the control group resulted in a significant improvement in foot sole mobility, ankle ROM, first metatarsophalangeal joint ROM, isometric strength of ankle dorsiflexion and plantarflexion and hallux dorsiflexion and plantarflexion. These results were consistent with the results of studies conducted by other researches [14, 24, 29, 30].
Kanchanasamut et al. (2017) investigated the effect of a weight-bearing exercise program on a mini-trampoline on foot mobility, plantar pressure, and sensation in diabetic foot neuropathy. This study included 24 patients with diabetic neuropathy in one control and two experimental groups. The control group only received the foot care program, while the experimental group participated in exercises for eight weeks. The results showed that weight-bearing exercises for eight weeks improve the perception of vibration [14].
Sartor et al. (2014) analyzed the effect of functional, strengthening, and stretching exercises on foot function in patients with diabetic neuropathy. A total of 55 patients with diabetic neuropathy participated in this research. The control group received medication, as well as medical care, and foot care instructions, and the experimental group performed exercises for 12 weeks. The results revealed changes in the rocking motion of the foot during walking, improved distribution of plantar pressure, and better functional status of the ankle [28].
The study entitled “exercise therapy improves plantar pressure distribution in patients with diabetic peripheral neuropathy” conducted by Fayed et al. (2016) included forty women with DPN. The control group received treatment and medical care, while the experimental group received medical treatment as well as physiotherapy interventions and stretching, strengthening, balance, and walking exercises. The findings demonstrated that physiotherapy intervention can significantly prevent the occurrence of diabetic ulcers in patients with diabetic neuropathy. The outstanding changes in this study were supported by pressure distribution, peak plantar pressure, and foot contact area [29].
Cerrahoglu et al. (2016) evaluated the effect of ROM and plantar pressure on diabetic patients with and without neuropathy on foot care exercises. The study included 76 diabetic patients, and the exercise groups followed their respective training programs for four weeks. The findings demonstrated that a home exercise program can be an effective preventive method to improve ROM in the foot joints and plantar pressure distribution in diabetic patients, regardless of the presence or absence of neuropathy [30].
All previous studies have shown that exercise programs and treatment protocols are effective in improving musculoskeletal health, balance, preventing further complications, and increasing patients’ independence in performing daily activities. However, the mentioned exercises typically target larger joints and lower limb muscles, with a primary focus on walking training, whereas both protocols in the current study target musculoskeletal defects of distal and smaller joints and muscles, as well as intrinsic and extrinsic muscles which are the most damaged in neuropathic patients and their functions and biomechanics are affected under dynamic conditions. In neuropathy patients, movement disorders in the distal muscles are seen with a 15%-20% decrease in the maximum ankle isokinetic moment, as well as atrophy of the inner foot muscles. In addition, the greater the plantar overload under the corresponding part during walking, the lower the lateral mobility of the forefoot in the first metatarsophalangeal joint, inversion, and eversion of the subtalar joint. As a result, the target of the relevant exercise protocols in the present study was the interphalangeal, metatarsophalangeal, ankle joints, and muscle groups on the medial plantar side, lateral plantar side, median plantar side, and dorsal plantar side, which resulted in increased mechanical properties of the calcaneal tendon, reduced foot fat, increased isometric muscle strength of the toes and hallux, increased the ankle extensor torque and strength, increased the ROM of the ankle in the sagittal plane, increased the conduction speed of the peroneal motor nerve and the sural sensory nerve, reduced plantar numbness, expanded peripheral microvasculature and changed vascular function, as well as improved sensory and motor afferent function [14, 15, 17, 18, 20]. As a result, mini-trampoline and ankle therapeutic exercises can be used as a simple, affordable, low-risk, and quick-improvement treatment program that focuses on the integration of peripheral strengthening using segmental exercises for foot function, which improves diabetic patient’s quality of life.
5. Conclusion
According to the findings, the exercise protocols used in this study, which were completely focused on the musculoskeletal dysfunction caused by DPN, can be effective in reducing musculoskeletal dysfunctions caused by this problem, and included in patients’ daily activities as a self-care strategy to minimize the harmful consequences of DPN.
Study limitations
The small sample size and short-term follow-up of the exercise program’s effects were the study’s main shortcomings. It is suggested that further comparative studies using exercise routines and a larger sample size should be conducted to evaluate their impact on the management of DPN. Furthermore, given the paucity of studies designing exercise programs such as mini-trampoline and ankle therapy exercise programs to prevent and control diabetes in women with peripheral neuropathy, it is recommended to conduct more research in this area.
Ethical Considerations
Compliance with ethical guidelines
The Research Ethics Committee of the Institute of Sports Sciences approved all research processes and methods in terms of ethical considerations (Code: IR.SSRI.REC 1400.1311). Also, written informed consent was obtained from all participants.
Funding
The paper was extracted from the PhD thesis of Ashraf Ansari, approved by Department of Sport Injury and Corrective Exercise, Tehran University.
Authors' contributions
Conceptualization, methodology, resources, visualization, original data preparation and analysis, writing- original draft, review and editing: Ashraf Ansari; Supervision: Mohammad Karimizadeh Ardakani and Mahdieh Akoochakian
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors express their deepest gratitude to all the subjects who participated in this research.
References
- Kidney disease: Improving global outcomes (KDIGO). Kdigo 2022 clinical practice guideline for diabetes management in chronic kidney disease. Kidney International. 2022; 102 (Suppl 5S), S1–127. [Link]
- Centers for Disease Control and Prevention. National diabetes statistics report. Atlanta: Centers for Disease Control and Prevention; 2022. [Link]
- Kanaley JA, Colberg SR, Corcoran MH, Malin SK, Rodriguez NR, Crespo CJ, et al. Exercise/physical activity in individuals with type 2 diabetes: A consensus statement from the american college of sports medicine. Medicine and Science in Sports and Exercise. 2022; 54(2):353-68. [DOI:10.1249/MSS.0000000000002800] [PMID] [PMCID]
- American Diabetes Association. Classification and diagnosis of diabetes: Standards of medical care in diabetes-2021. Diabetes Care. 2021; 441(1 Suppl): S15-33. [DOI:10.2337/dc21-S002] [PMID]
- Chitneni A, Rupp A, Ghorayeb J, Abd-Elsayed A. Early detection of diabetic peripheral neuropathy by fMRI: An evidence-based review. Brain Sciences. 2022; 12(5):557. [DOI:10.3390/brainsci12050557] [PMID] [PMCID]
- Kiyani M, Yang Z, Charalambous LT, Adil SM, Lee HJ, Yang S, et al. Painful diabetic peripheral neuropathy: Health care costs and complications from 2010 to 2015. Neurology Clinical Practice. 2020; 10(1):47-57. [DOI:10.1212/CPJ.0000000000000671] [PMID] [PMCID]
- Di Stefano G, Di Lionardo A, Di Pietro G, Truini A. Neuropathic pain related to peripheral neuropathies according to the IASP grading system criteria. Brain Sciences. 2020; 11(1):1. [DOI:10.3390/brainsci11010001] [PMID] [PMCID]
- Holmes CJ, Hastings MK. The application of exercise training for diabetic peripheral neuropathy. Journal of Clinical Medicine. 2021; 10(21):5042. [DOI:jcm10215042, 2021] [PMID] [PMCID]
- Alam U, Riley DR, Jugdey RS, Azmi S, Rajbhandari S, D'Août K, et al. Diabetic neuropathy and gait: A review. Diabetes Therapy. 2017; 8(6):1253-64. [DOI:10.1007/s13300-017-0295-y] [PMID] [PMCID]
- Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. The New England Journal of Medicine. 2017; 376(24):2367-75. [DOI:10.1056/NEJMra1615439] [PMID]
- Ahmad I, Noohu MM, Verma S, Singla D, Hussain ME. Effect of sensorimotor training on balance measures and proprioception among middle and older age adults with diabetic peripheral neuropathy. Gait & Posture. 2019; 74:114-20. [DOI:10.1016/j.gaitpost.2019.08.018] [PMID]
- American Diabetes Association. Standards of medical care in diabetes-2019 abridged for primary care providers. Clinical Diabetes. 2019; 37(1):11-34. [PMID]
- Sumikawa M, Kuwamura Y, Sumikawa Y, Fujiwara T, Kamiya C. Effect of foot self-care behavior according to severity of diabetic neuropathy in japanese patients with diabetes. Health. 2018; 10(09):1192. [DOI:10.4236/health.2018.109091]
- Kanchanasamut W, Pensri P. Effects of weight-bearing exercise on a mini-trampoline on foot mobility, plantar pressure and sensation of diabetic neuropathic feet; a preliminary study. Diabetic Foot and Ankle. 2017; 8(1):1287239. [DOI:10.1080/2000625X.2017.1287239] [PMID] [PMCID]
- Rayman G, Vas P, Dhatariya k, Driver V, Hartemann A, Londahl M, et al. Guidelines on use of interventions to enhance healing of chronic foot ulcers in diabetes (IWGDF 2019 update). Diabetes/Metabolism Research and Reviews. 2020; 36:e3283. [DOI:10.1002/dmrr.3283]
- Tran MM, Haley MN. Does exercise improve healing of diabetic foot ulcers? A systematic review. Journal of Foot and Ankle Research. 2021; 14(1):19. [DOI:10.1186/s 13047-021-00456-w] [PMID] [PMCID]
- Aagaard TV, Moeini S, Skou ST, Madsen UR, Brorson S. Benefits and harms of exercise therapy for patients with diabetic foot ulcers: A systematic review. The International Journal of Lower Extremity Wounds. 2022; 21(3):219-33. [DOI: 10.1177/1534734620954066] [PMID]
- Awaluddin SW, Ardi M, Zabitha RA. The effects of foot exercise to distal sensorimotor on diabetic peripheral neuropathy. Indian Journal of Forensic Medicine & Toxicology. 2019; 13(4). [DOI:10.5958/0973-9130.2019.00570.X]
- Szyguła R, Wierzbicka M, Sondel G. Influence of 8-week aerobic training on the skin microcirculation in patients with ischaemic heart disease. Journal of Aging Research. 2020; 2020:4602067. [DOI:10.1155/2020/4602067] [PMID] [PMCID]
- Monteiro RL, Ferreira JSSP, Silva ÉQ, Donini A, Cruvinel-Júnior RH, Verissímo JL, et al. Feasibility and preliminary efficacy of a foot-ankle exercise program aiming to improve foot-ankle functionality and gait biomechanics in people with diabetic neuropathy: A randomized controlled trial. Sensors (Basel). 2020; 20(18):5129. [DOI:10.3390/s20185129] [PMID] [PMCID]
- Sadeghi M, Ghasemi G, Karimi M. Effect of 12-week rebound therapy exercise on static stability of patients with spinal cord injury. Journal of Sport Rehabilitation. 2019; 28(5):464-7. [DOI:10.1123/jsr.2017-0303] [PMID]
- Giagazoglou P, Kokaridas D, Sidiropoulou M, Patsiaouras A, Karra C, Neofotistou K. Effects of a trampoline exercise intervention on motor performance and balance ability of children with intellectual disabilities. Research in Developmental Disabilities. 2013; 34(9):2701-7. [DOI:10.1016/j.ridd.2013.05.034] [PMID]
- Ferreira JSSP, Cruvinel Junior RH, Silva EQ, Veríssimo JL, Monteiro RL, Pereira DS, et al. Study protocol for a randomized controlled trial on the effect of the diabetic foot guidance system (SOPeD) for the prevention and treatment of foot musculoskeletal dysfunctions in people with diabetic neuropathy: The footcare (FOCA) trial I. Trials. 2020; 21(1):73. [DOI:10.1186/S13063-019-4017-9,2020] [PMID] [PMCID]
- Monteiro RL, Sartor CD, Ferreira JSSP, Dantas MGB, Bus SA, Sacco ICN. Protocol for evaluating the effects of a foot-ankle therapeutic exercise program on daily activity, foot-ankle functionality, and biomechanics in people with diabetic polyneuropathy: A randomized controlled trial. BMC Musculoskeletal Disorders. 2018; 19(1):400. [DOI:10.1186/s12891-018-2323-0] [PMID] [PMCID]
- Healy A, Naemi R, Sundar L, Chatzistergos P, Ramachandran A, Chockalingam N. Hallux plantar flexor strength in people with diabetic neuropathy: Validation of a simple clinical test. Diabetes Research and Clinical Practice. 2018; 144:1-9. [DOI:10.1016/j.diabres.2018.07.038] [PMID]
- Błażkiewicz M, Sundar L, Healy A, Ramachandran A, Chockalingam N, Naemi R. Assessment of lower leg muscle force distribution during isometric ankle dorsi and plantar flexion in patients with diabetes: A preliminary study. Journal of Diabetes and its Complications. 2015; 29(2):282-7. [DOI:10.1016/j.jdiacomp.2014.10.007] [PMID]
- Silva EQ, Suda EY, Santos DP, Veríssimo JL, Ferreira JSSP, Cruvinel Júnior RH, et al. Effect of an educational booklet for prevention and treatment of foot musculoskeletal dysfunctions in people with diabetic neuropathy: The footcare (FOCA) trial II, a study protocol of a randomized controlled trial. Trials. 2020; 21(1):180. [DOI: 10.1186/s13063-020-4115-8] [PMID] [PMCID]
- Sartor CD, Hasue RH, Cacciari LP, Butugan MK, Watari R, Pássaro AC, et al. Effects of strengthening, stretching and functional training on foot function in patients with diabetic neuropathy: Results of a randomized controlled trial. BMC Musculoskeletal Disorders. 2014; 15:137. [DOI:10.1186/1471-2474-15-137] [PMID] [PMCID]
- Fayed EE, Badr NM, Ismail S, Hakim SA. Exercise therapy improves planter pressure distribution in patients with diabetic peripheral neuropathy. International Journal of PharmTech Research. 2016; 9(5):151-9. [Link]
- Cerrahoglu L, Koşan U, Sirin TC, Ulusoy A. Range of motion and plantar pressure evaluation for the effects of self-care foot exercises on diabetic patients with and without neuropathy. Journal of the American Podiatric Medical Association. 2016; 106(3):189-200. [DOI:10.7547/14-095] [PMID]
Type of Study: Research |
Subject:
Sport injury and corrective exercises
Received: 2023/02/5 | Accepted: 2023/02/28 | Published: 2022/10/20
Received: 2023/02/5 | Accepted: 2023/02/28 | Published: 2022/10/20
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |