Wed, Jul 16, 2025
Volume 11, Issue 3 (Summer 2021)
PTJ 2021, 11(3): 181-188 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Youssef M. Neuromuscular Electric Stimulation Versus Traditional Treatment on Harris Hip Score in Cases of Avascular Necrosis of Femoral Head After Kidney Transplantation. PTJ 2021; 11 (3) :181-188
URL: http://ptj.uswr.ac.ir/article-1-463-en.html
URL: http://ptj.uswr.ac.ir/article-1-463-en.html
Physical Therapy, Cairo University Hospitals, Giza, Egypt.
Keywords: Avascular necrosis, Femoral head, Physical activity, Neuromuscular electric stimulation, Exercise, Infrared
Full-Text [PDF 534 kb]
(1380 Downloads)
| Abstract (HTML) (2957 Views)
Full-Text: (1090 Views)
1. Introduction
Avascular Necrosis (AVN) is also called aseptic necrosis of bone, ischemic bone necrosis, osteochondritis dessecans, and osteonecrosis [1]. Femoral condyles, tibial plateau, talus, and humeral head may be affected. Its prevalence is 6% to 15% and rises by 52% in patients under high-dose corticosteroids. Also, AVN is seen in 85% of cases [2, 3].
After transplantation, inactivity and postoperative malnutrition result in low Body Mass Index (BMI) and muscle atrophy. There is a history of metabolic bone disease, mass accompanied by immunosuppressive medication such as high dosages of corticosteroids, cellular hypertrophy, and toxicity. Elevated lipid levels cause microemboli, and along with endothelial cell changes, venous stasis occurs. These changes lead to increased intra-osseous pressure and bone necrosis [4].
The ischemia occurs very soon in renal transplant patients, often within 12 weeks of transplantation. Symptoms may not appear that soon, but within two years, most patients are diagnosed [5, 6]. This disease mainly affects the femoral head. Once osteonecrosis begins, 80% of the femoral head will ruin if not treated [7].
The patients started to complain in the third, fourth, and fifth decade of their life; men are more affected than women with a ratio of 4:1. At the beginning of femoral head AVN, it is asymptomatic, but with the progression of the disease, patients experience pain, reduced Range Of Motion (ROM), and limping during the hip joint activity [1, 8]. By activity, the pain will appear insidiously, and with disease progression, pain occurs at rest and affect ROM and function [9].
In the latter stages, as joint deformity and muscle wasting develop, active and passive ROM is lost, most frequently in abduction, flexion, and internal rotation of the affected hip. Positive Trendelenburg sign and click is heard when the patient is asked to rise from a seat or after external rotation of the abducted hip [10].
Conservative treatment options include bed rest, reduced weight-bearing, analgesics, deep heat modalities, braces, and ROM exercises. Unfortunately, pain is not entirely relieved [11]. Hip MRI is the most reliable tool in the diagnosis of AVN and also helps to determine its stage [12].
2. Materials and Methods
All study procedures were done following the ethical standards of the 2000 revision of the Helsinki Declaration. All patients were asked to sign an informed consent for study participation after a full explanation of the procedures.
Study subjects
This study was conducted on 20 patients (13 men and 7 women) admitted to Cairo University Hospitals. All patients had kidney transplantation surgery 1-4 years ago and were under immunosuppressive corticosteroid treatment after surgery. They were 37 to 45 years old. The patients were diagnosed according to their clinical manifestations and confirmed by MRI. All patients had AVN of femoral head grades from II to IV. The patients were randomly divided into two groups: the first group was treated by Neuromuscular Electric Stimulation (NMES) along with stretching and strengthening exercises, and the second group by Traditional Treatment (TT) with stretching and strengthening exercises. The exclusion criteria were diabetic patients, extensive destruction of the femoral head and joint, and obese patients with a BMI of ≥35 kg/m2.
Evaluative procedures:
ROM (Range of Motion): By goniometer, we compared the range of motion of the affected hip with the normal side to detect subtle limitations or painful movements [13].
Muscle Testing: Manual muscle test was used to assess the strength of hip flexors, extensors, internal and external rotators of the hip joint, and particular muscle groups that are the source of pain [14].
Harris Hip Score (HHS): It is a pain scale and assesses sitting, limping, ascending stairs, support, putting on shoes and socks, enter public transportation, distance walked, range of motion, absence of deformity, total HHS. The evaluation was used before and after the application of treatment of both groups [15, 16].
Treatment procedures
Group 1: The patients received a 30-min session of NMES around their hip joints. One electrode is placed on the greater trochanter of the femoral head and the other on the gluteus maximus muscle for 30 min using the Healthtronic three channels model (BM 1006). The electrode size is 10×9.4 cm. Electric stimulation is the process of using an electrical impulse to contract and relax the gluteus maximus muscle. The current intensity was adjusted according to the patient’s tolerability. The device was set for 20 s of stimulation followed by 4 s relaxation.
The session was followed by another 30 min of stretching and strengthening exercises of the affected lower limb and active exercise for the normal limb. Strengthening exercises involve hip joint muscles, knee flexors and extensors, ankle dorsiflexors, and plantar flexors. Each exercise was done in 5 sets, with 10 repetitions in each set [17]. The patient can relax whenever they want. The resting period between each exercise is 1-2 min. The stretching exercise for external rotators and abductors are done with 30 repetitions interrupted with a resting period when the patient wants. Stretching positions are taught to do at home, too. The intervention was done 3 sessions a week for 3 months.
Group 2: TT consists of infrared and exercises. Infrared as a method of heating improves circulation by providing vasodilatation so that it can relieve pain. It is applied on the hip joint for 20 min at 0.45 to 0.60 cm, according to the patient’s sensation of warmth [11].
Statistical analysis
All the obtained data are presented as the Mean±SD. They were analyzed using the independent t-test. The statistical significance was set at a confidence level of 95% (P<0.05). Pre- and post-treatment analyses were done in Minitab version 13.1.
3. Results
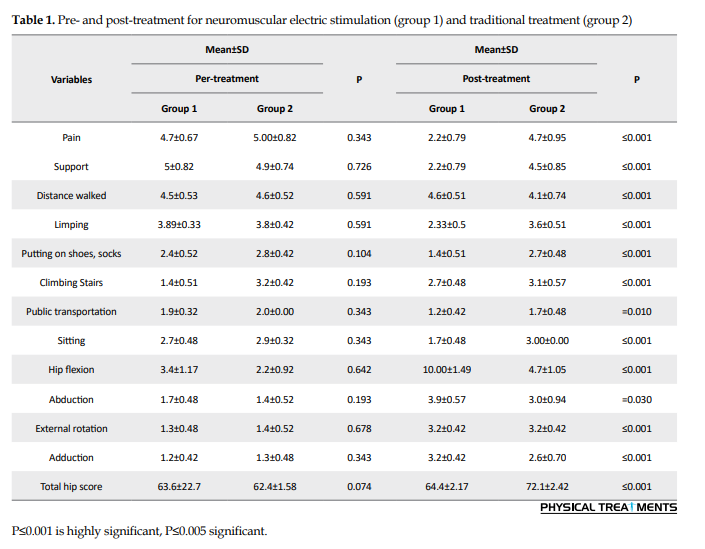
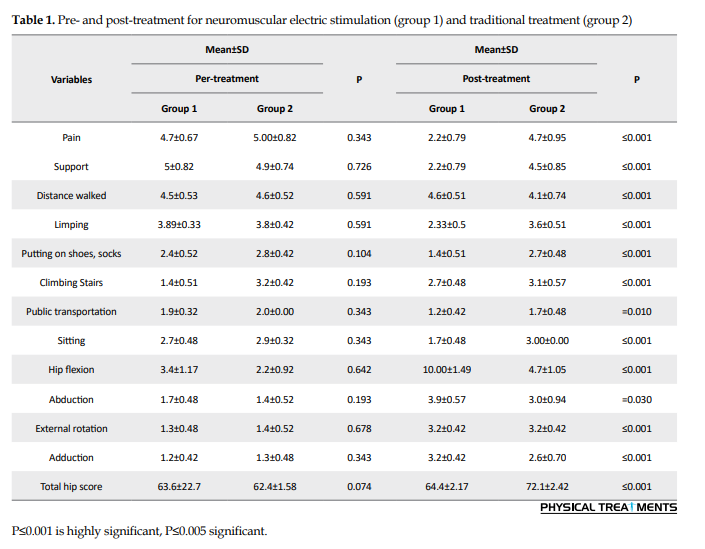
A total of 20 patients consisting of 13 men (65%) and 7 women (35%) participated in this study. They were between 37 and 45 years old. Before treatment, no significant differences were found between study groups regarding pain (P=0.343), support (P=0.727), distance walked (P=0.591), limping (P=0.591), putting on shoes and socks (P=0.104), climbing stairs (P=0.193), public transportation (P=0.343), sitting (P=0.343), flexion, (P=0.6420), abduction, (P=0.193), external rotation (P=0.678), adduction (P=0.343), and total Harris hip score (P=0.074).
However, after treatment, significant differences were found between the two groups regarding pain (P< 0.001), support (P<0.001), distance walked (P<0.001), limping (P<0.001), putting on shoes and socks, (P<0.001), climbing stairs (P<0.001), sitting (P<0.001), flexion, (P<0.001), external rotation (P<0.001), public transportation (P=0.010), abduction, (P=0.030), adduction (P<0.001), and total hip score (P=0.016).
4. Discussion
To the best of our knowledge, this is the first study that compares TT of physical therapy with new methods like NMES. Also, it is the first study that measures the effect of different Physical Therapy (PT) modalities on HHS. There are no significant differences between the groups in the component of HHS before the treatment in pain, support, distance walked, limping, putting on shoes and socks, climbing stairs, abduction, adduction, external rotation, hip flexion, public transportation, sitting, and total hip score. However, after three months of treatments, there were significant differences in all components of HHS in the NMES group and non-significant differences in the TT group (Table 1).
Premkumar et al. [6] conducted a meta-analysis to find the effect of TT for AVN of the femoral head. They reported that 80% of 819 patients had a negative outcome followed for 34 months without weight-bearing. So, they concluded that the TT is ineffective in the treatment of AVN of the femoral head. Unfortunately, traditional drugs and PT methods continue to be used despite their ineffectiveness.
Kaushik et al. [18] found that preventing the weight-bearing (with a cane, crutches, or walker), with the modification of activity, and traditional PT is ineffective in treating late-stage AVN (the third and fourth stage). Also, it failed to prevent disease progression, even in the early stages (Steinberg stage I and II).
Bogdan et al. [8] found that conservative treatment of 30 sessions of hyperbaric oxygen therapy, using non-steroidal anti-inflammatory drugs, cold packs, ROM exercises, and bed rest cannot relieve pain. However, in some early cases (Steinberg Stage-I, II), low weight-bearing, restricting activities, or using crutches can stop the damage due to AVN and allow natural healing. Still, these patients have an 85% risk of femoral head collapse. When the involved segment is smaller than 15%, the protected weight-bearing may be effective and located far from the weight-bearing region. ROM and strengthening exercises can maintain joint function as it prevents muscle weakness and keeps joint mobility, but it did not prevent disease progression. This finding agrees with the present study TT has increased only 1 point in Harris hip score, which indicates the improvement of patient’s activity of daily living as presented in Table 1.
Several studies documented the effect of NMES in reducing pain in spinal cord injury [19, 20], neck pain [21], patellofemoral pain [22], shoulder pain [23], and pain associated with endometriosis [24]. AVN is characterized by inflammatory changes and ischemia, which occur in the first stage and progresses to pain and edema. During the early stage, NMES increases cell membrane adenosine receptors which have an anti-inflammatory effect accompanied by a decrease in the production of free radicles and consequently lowering the pain [25]. NMES reduces the anti-inflammatory effect, thereby decreasing the breakdown of the cartilage, increasing angiogenesis, and improving bone formation through an increase in osteoblasts and decrease in the osteoclasts [26, 27].
Stimulation of the femoral head anteriorly and posteriorly for a long period induces the recovery of bone ischemia through 1) increase in the production of growth factors and increase osteoblasts activity, 2) formation of new vessels that stop the extension of necrosis to another area, and 3) decrease in the parathyroid hormones leading to decrease the activity of the osteoclasts [28]. So NMES may be an excellent tool that helps in treating patients with AVN of the femoral head. Some studies stated that physical therapy could be used in combination with core decompression and even replace it. A study compared core compression and bone grafting associated with PT with core compression and bone graft alone. The results revealed hip progression 70% with 5 points improvement in HHS compared to 79% progression and 3 points improvement in Harris score in decompression group. This finding supports the present study results, as HHS increased 8 points in the NMES group and 1 point in the TT group.
Marchese et al. [14] conducted a study on 38 patients with sickle cell disease (17 received hip core decompression with physical therapy and 21 received physical therapy alone). The physical therapy protocol comprises the weight-bearing limitation of toe-touch weight bearing on the affected hip for the initial 6 weeks of the study. If the patient’s one hip has osteonecrosis, he or she was asked to use a crutch or a walker. And if both hips were affected, the patient was asked to use a wheelchair during mobility. The researchers stated the relation between pain, ROM, and functional mobility. Also, stretching and strengthening exercises were administered once or twice a week to assist with the home exercise program for 3 months. That study reported that PT alone seems to be as effective as hip core decompression followed by PT. In the NMES group, there is a decrease in pain scale accompanied by an increase in the ROM and activity of daily living (Table 1). However, the TT group showed no significant difference in any component of HHS.
Neumayr et al. [29] compared the results of core decompression followed by a PT program with a physical therapy program alone on 38 patients (46 hips) with sickle cell disease and Steinberg Stage-I, -II, or -III. No intraoperative and postoperative complications occurred in 17 patients who received decompression combined with PT and 21 patients who received PT alone. After three years of follow-up, the hip survival rate was 82%, with 18.1 points improvement in HHS in the group treated with decompression and physical therapy and 86% hip survival and 15.7 points improvement in HHS in the group treated with PT alone. These findings support and explain the results of the present study. NMES created a significant difference in all evaluation parameters (Table 1); in other words, total HHS increased 8 points in the NMES group while only 1 point in the TT group.
5. Conclusion
The study revealed that NMES is more effective than TT in relieving pain and empowering the muscles around the hip. These effects improved Harris hip score and activity of daily living in patients treated with NMES.
Ethical Considerations
Compliance with ethical guidelines
All the participants were informed about the purpose of the research and its implementation stages. They were also assured about the confidentiality of their information and were free to leave the study whenever they wished, and if desired, the research results would be available to them. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975. Informed consent was obtained from all patients.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Conflict of interest
The author declared no conflict of interest.
Refrences:
Avascular Necrosis (AVN) is also called aseptic necrosis of bone, ischemic bone necrosis, osteochondritis dessecans, and osteonecrosis [1]. Femoral condyles, tibial plateau, talus, and humeral head may be affected. Its prevalence is 6% to 15% and rises by 52% in patients under high-dose corticosteroids. Also, AVN is seen in 85% of cases [2, 3].
After transplantation, inactivity and postoperative malnutrition result in low Body Mass Index (BMI) and muscle atrophy. There is a history of metabolic bone disease, mass accompanied by immunosuppressive medication such as high dosages of corticosteroids, cellular hypertrophy, and toxicity. Elevated lipid levels cause microemboli, and along with endothelial cell changes, venous stasis occurs. These changes lead to increased intra-osseous pressure and bone necrosis [4].
The ischemia occurs very soon in renal transplant patients, often within 12 weeks of transplantation. Symptoms may not appear that soon, but within two years, most patients are diagnosed [5, 6]. This disease mainly affects the femoral head. Once osteonecrosis begins, 80% of the femoral head will ruin if not treated [7].
The patients started to complain in the third, fourth, and fifth decade of their life; men are more affected than women with a ratio of 4:1. At the beginning of femoral head AVN, it is asymptomatic, but with the progression of the disease, patients experience pain, reduced Range Of Motion (ROM), and limping during the hip joint activity [1, 8]. By activity, the pain will appear insidiously, and with disease progression, pain occurs at rest and affect ROM and function [9].
In the latter stages, as joint deformity and muscle wasting develop, active and passive ROM is lost, most frequently in abduction, flexion, and internal rotation of the affected hip. Positive Trendelenburg sign and click is heard when the patient is asked to rise from a seat or after external rotation of the abducted hip [10].
Conservative treatment options include bed rest, reduced weight-bearing, analgesics, deep heat modalities, braces, and ROM exercises. Unfortunately, pain is not entirely relieved [11]. Hip MRI is the most reliable tool in the diagnosis of AVN and also helps to determine its stage [12].
2. Materials and Methods
All study procedures were done following the ethical standards of the 2000 revision of the Helsinki Declaration. All patients were asked to sign an informed consent for study participation after a full explanation of the procedures.
Study subjects
This study was conducted on 20 patients (13 men and 7 women) admitted to Cairo University Hospitals. All patients had kidney transplantation surgery 1-4 years ago and were under immunosuppressive corticosteroid treatment after surgery. They were 37 to 45 years old. The patients were diagnosed according to their clinical manifestations and confirmed by MRI. All patients had AVN of femoral head grades from II to IV. The patients were randomly divided into two groups: the first group was treated by Neuromuscular Electric Stimulation (NMES) along with stretching and strengthening exercises, and the second group by Traditional Treatment (TT) with stretching and strengthening exercises. The exclusion criteria were diabetic patients, extensive destruction of the femoral head and joint, and obese patients with a BMI of ≥35 kg/m2.
Evaluative procedures:
ROM (Range of Motion): By goniometer, we compared the range of motion of the affected hip with the normal side to detect subtle limitations or painful movements [13].
Muscle Testing: Manual muscle test was used to assess the strength of hip flexors, extensors, internal and external rotators of the hip joint, and particular muscle groups that are the source of pain [14].
Harris Hip Score (HHS): It is a pain scale and assesses sitting, limping, ascending stairs, support, putting on shoes and socks, enter public transportation, distance walked, range of motion, absence of deformity, total HHS. The evaluation was used before and after the application of treatment of both groups [15, 16].
Treatment procedures
Group 1: The patients received a 30-min session of NMES around their hip joints. One electrode is placed on the greater trochanter of the femoral head and the other on the gluteus maximus muscle for 30 min using the Healthtronic three channels model (BM 1006). The electrode size is 10×9.4 cm. Electric stimulation is the process of using an electrical impulse to contract and relax the gluteus maximus muscle. The current intensity was adjusted according to the patient’s tolerability. The device was set for 20 s of stimulation followed by 4 s relaxation.
The session was followed by another 30 min of stretching and strengthening exercises of the affected lower limb and active exercise for the normal limb. Strengthening exercises involve hip joint muscles, knee flexors and extensors, ankle dorsiflexors, and plantar flexors. Each exercise was done in 5 sets, with 10 repetitions in each set [17]. The patient can relax whenever they want. The resting period between each exercise is 1-2 min. The stretching exercise for external rotators and abductors are done with 30 repetitions interrupted with a resting period when the patient wants. Stretching positions are taught to do at home, too. The intervention was done 3 sessions a week for 3 months.
Group 2: TT consists of infrared and exercises. Infrared as a method of heating improves circulation by providing vasodilatation so that it can relieve pain. It is applied on the hip joint for 20 min at 0.45 to 0.60 cm, according to the patient’s sensation of warmth [11].
Statistical analysis
All the obtained data are presented as the Mean±SD. They were analyzed using the independent t-test. The statistical significance was set at a confidence level of 95% (P<0.05). Pre- and post-treatment analyses were done in Minitab version 13.1.
3. Results
A total of 20 patients consisting of 13 men (65%) and 7 women (35%) participated in this study. They were between 37 and 45 years old. Before treatment, no significant differences were found between study groups regarding pain (P=0.343), support (P=0.727), distance walked (P=0.591), limping (P=0.591), putting on shoes and socks (P=0.104), climbing stairs (P=0.193), public transportation (P=0.343), sitting (P=0.343), flexion, (P=0.6420), abduction, (P=0.193), external rotation (P=0.678), adduction (P=0.343), and total Harris hip score (P=0.074).
However, after treatment, significant differences were found between the two groups regarding pain (P< 0.001), support (P<0.001), distance walked (P<0.001), limping (P<0.001), putting on shoes and socks, (P<0.001), climbing stairs (P<0.001), sitting (P<0.001), flexion, (P<0.001), external rotation (P<0.001), public transportation (P=0.010), abduction, (P=0.030), adduction (P<0.001), and total hip score (P=0.016).
4. Discussion
To the best of our knowledge, this is the first study that compares TT of physical therapy with new methods like NMES. Also, it is the first study that measures the effect of different Physical Therapy (PT) modalities on HHS. There are no significant differences between the groups in the component of HHS before the treatment in pain, support, distance walked, limping, putting on shoes and socks, climbing stairs, abduction, adduction, external rotation, hip flexion, public transportation, sitting, and total hip score. However, after three months of treatments, there were significant differences in all components of HHS in the NMES group and non-significant differences in the TT group (Table 1).
Premkumar et al. [6] conducted a meta-analysis to find the effect of TT for AVN of the femoral head. They reported that 80% of 819 patients had a negative outcome followed for 34 months without weight-bearing. So, they concluded that the TT is ineffective in the treatment of AVN of the femoral head. Unfortunately, traditional drugs and PT methods continue to be used despite their ineffectiveness.
Kaushik et al. [18] found that preventing the weight-bearing (with a cane, crutches, or walker), with the modification of activity, and traditional PT is ineffective in treating late-stage AVN (the third and fourth stage). Also, it failed to prevent disease progression, even in the early stages (Steinberg stage I and II).
Bogdan et al. [8] found that conservative treatment of 30 sessions of hyperbaric oxygen therapy, using non-steroidal anti-inflammatory drugs, cold packs, ROM exercises, and bed rest cannot relieve pain. However, in some early cases (Steinberg Stage-I, II), low weight-bearing, restricting activities, or using crutches can stop the damage due to AVN and allow natural healing. Still, these patients have an 85% risk of femoral head collapse. When the involved segment is smaller than 15%, the protected weight-bearing may be effective and located far from the weight-bearing region. ROM and strengthening exercises can maintain joint function as it prevents muscle weakness and keeps joint mobility, but it did not prevent disease progression. This finding agrees with the present study TT has increased only 1 point in Harris hip score, which indicates the improvement of patient’s activity of daily living as presented in Table 1.
Several studies documented the effect of NMES in reducing pain in spinal cord injury [19, 20], neck pain [21], patellofemoral pain [22], shoulder pain [23], and pain associated with endometriosis [24]. AVN is characterized by inflammatory changes and ischemia, which occur in the first stage and progresses to pain and edema. During the early stage, NMES increases cell membrane adenosine receptors which have an anti-inflammatory effect accompanied by a decrease in the production of free radicles and consequently lowering the pain [25]. NMES reduces the anti-inflammatory effect, thereby decreasing the breakdown of the cartilage, increasing angiogenesis, and improving bone formation through an increase in osteoblasts and decrease in the osteoclasts [26, 27].
Stimulation of the femoral head anteriorly and posteriorly for a long period induces the recovery of bone ischemia through 1) increase in the production of growth factors and increase osteoblasts activity, 2) formation of new vessels that stop the extension of necrosis to another area, and 3) decrease in the parathyroid hormones leading to decrease the activity of the osteoclasts [28]. So NMES may be an excellent tool that helps in treating patients with AVN of the femoral head. Some studies stated that physical therapy could be used in combination with core decompression and even replace it. A study compared core compression and bone grafting associated with PT with core compression and bone graft alone. The results revealed hip progression 70% with 5 points improvement in HHS compared to 79% progression and 3 points improvement in Harris score in decompression group. This finding supports the present study results, as HHS increased 8 points in the NMES group and 1 point in the TT group.
Marchese et al. [14] conducted a study on 38 patients with sickle cell disease (17 received hip core decompression with physical therapy and 21 received physical therapy alone). The physical therapy protocol comprises the weight-bearing limitation of toe-touch weight bearing on the affected hip for the initial 6 weeks of the study. If the patient’s one hip has osteonecrosis, he or she was asked to use a crutch or a walker. And if both hips were affected, the patient was asked to use a wheelchair during mobility. The researchers stated the relation between pain, ROM, and functional mobility. Also, stretching and strengthening exercises were administered once or twice a week to assist with the home exercise program for 3 months. That study reported that PT alone seems to be as effective as hip core decompression followed by PT. In the NMES group, there is a decrease in pain scale accompanied by an increase in the ROM and activity of daily living (Table 1). However, the TT group showed no significant difference in any component of HHS.
Neumayr et al. [29] compared the results of core decompression followed by a PT program with a physical therapy program alone on 38 patients (46 hips) with sickle cell disease and Steinberg Stage-I, -II, or -III. No intraoperative and postoperative complications occurred in 17 patients who received decompression combined with PT and 21 patients who received PT alone. After three years of follow-up, the hip survival rate was 82%, with 18.1 points improvement in HHS in the group treated with decompression and physical therapy and 86% hip survival and 15.7 points improvement in HHS in the group treated with PT alone. These findings support and explain the results of the present study. NMES created a significant difference in all evaluation parameters (Table 1); in other words, total HHS increased 8 points in the NMES group while only 1 point in the TT group.
5. Conclusion
The study revealed that NMES is more effective than TT in relieving pain and empowering the muscles around the hip. These effects improved Harris hip score and activity of daily living in patients treated with NMES.
Ethical Considerations
Compliance with ethical guidelines
All the participants were informed about the purpose of the research and its implementation stages. They were also assured about the confidentiality of their information and were free to leave the study whenever they wished, and if desired, the research results would be available to them. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975. Informed consent was obtained from all patients.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Conflict of interest
The author declared no conflict of interest.
Refrences:
- Liu D, Ahmet A, Ward L, Krishnamoorthy P, Mandelcorn ED, Leigh R, et al., A practical guide to the monitoring and management of complications of systemic corticosteroid therapy. Allergy, Asthma & Clinical Immunology. 2013; 9(1):30. [DOI:10.1186/1710-1492-9-30] [PMID] [PMCID]
- Reid A, Brady A, Blake C, Mongey AB, Veale DJ, Fitz Gerald O, et al. Randomised controlled trial examining the effect of exercise in people with rheumatoid arthritis taking anti-TNFα therapy medication. BMC Musculoskeletal Disorders. 2011; 12:11. [DOI:10.1186/1471-2474-12-11] [PMID] [PMCID]
- Zhang R, Chouhan KK. Metabolic bone diseases in kidney transplant recipients. World Journal of Nephrology. 2012; 1(5):127-33. [PMID]
- Sayed-Noor AS. Joint arthroplasties other than the hip in solid organ transplant recipients. The Open Orthopaedics Journal. 2009; 3:27-31. [DOI:10.2174/1874325000903010027] [PMID] [PMCID]
- Nowicki P, Chaudhary H. Total hip replacement in renal transplant Patients. The Journal of Bone and Joint Surgery. 2007; 89(12):1561-6. [DOI:10.1302/0301-620X.89B12.19400] [PMID]
- Piyakunmala K, Sangkomkamhang T, Chareonchonvanitch K. Is magnetic resonance imaging necessary for normal plain radiography evaluation of contralateral non-traumatic asymptomatic femoral head in high osteonecrosis risk patient. Journal of the Medical Association of Thailand. 2009; 92 (Suppl 6): S147-51. [PMID]
- Ansari S, Dhungel K, Ahmad K. Avascular necrosis of the femoral head: A case report with emphasis on imaging findings. Nepalese Journal of Radiology. 2012; 2(2):3-10. https://www.researchgate.net/publication/272774719_Avascular_Necrosis_of_the_Femoral_Head_A_Case_Report_with_Emphasis_on_Imaging_Findings
- Bogdan H, Cristescu V, Dragusaun M. Avascular necrosis of the femoral head. Maedica. 2009; 4(1):26-34. https://www.maedica.ro/articles/2009/2009_Vol4(7)_No1/2009_Vol4(7)_No1_pg26-34.pdf
- Chan KL, Mok CC. Glucocorticoid-induced avascular bone necrosis: Diagnosis and management. The Open Orthopaedics Journal. 2012; 6:449-57. [DOI:10.2174/1874325001206010449] [PMID] [PMCID]
- Cabrita HA, Santos AL, Gobbi RG, Lima AL, Oliveira PR, Ejnisman L, et al. Avascular necrosis of the femoral head in HIV-infected patients: Preliminary results from surgical treatment for ceramic-ceramic joint replacement. Revista Brasileira de Ortopedia. 2015; 47(5):626-30. [DOI:10.1016/S2255-4971(15)30014-8] [PMID]
- Stoica Z, Dumitrescu D, Popescu M, Gheonea I, Gabor M, Bogdan N. Imaging of avascular necrosis of femoral head: Familiar methods and newer trends. Current Health Sciences Journal. 2009; 35(1):23-8. [PMID]
- Ahmet M., Ferdi Y, Zaheer, A., et al., Bilateral avascular necrosis of the knee due to corticosteroid therapy in a patient with posterior inferior cerebellar anterovenous malformation. Turkish Journal of Physical Medicine and Rehabilitation. 2012; 58:243-52. https://www.researchgate.net/publication/260797176_Bilateral_Avascular_Necrosis_of_the_Knee_Due_to_Corticosteroid_Therapy_in_a_Patient_With_Posterior_Inferior_Cerebellar_Anterovenous_Malformation
- Brooker BJ, Keith PP. Osteonecrosis: The perils of steroids. A review of the literature and case report. Case Reports in Clinical Medicine. 2012; 1(2):26-37. [DOI:10.4236/crcm.2012.12008]
- Marchese VG, Connolly BH, Able C, Booten AR, Bowen P, Porter BM, et al. Relationships among severity of osteonecrosis, pain, range of motion, and functional mobility in children, adolescents, and young adults with acute lymphoblastic leukemia. Physical Therapy. 2008; 88(3):341-50. [DOI:10.2522/ptj.20070108] [PMID]
- Marchetti P, Binazzi R, Vaccari V, Girolami M, Morici F, Impallomeni C, et al. Long-term results with cementless Fitek (or Fitmore) cups. The Journal of Arthroplasty. 2005; 20(6):730-7. [DOI:10.1016/j.arth.2004.11.019] [PMID]
- Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: Treatment by mold arthroplasty. An end-result study using a new method of result evaluation. The Journal of Bone and Joint Surgery. 1969; 51(4):737-55. [DOI:10.2106/00004623-196951040-00012] [PMID]
- Ferri A, Scaglioni G, Pousson M, Capodaglio P, Van Hoecke J, Narici MV. Strength and power changes of the human plantar flexorsand knee extensors in response to resistance training in old age. Acta Physiologica Scandinavica. 2003; 177(1):69-78. [DOI:10.1046/j.1365-201X.2003.01050.x] [PMID]
- Kaushik AP, Das A, Cui Q. Osteonecrosis of the femoral head: An update in year 2012. World Journal of Orthopedics. 2012; 3(5):49-57. [DOI:10.5312/wjo.v3.i5.49] [PMID] [PMCID]
- Li YP, Cui X, Liu SC, Zhang SH, Zhao YH. Neuromuscular electrical stimulation for treating postpartum low back pain. Medicine. 2018; 97(28):e11426. [DOI:10.1097/MD.0000000000011426] [PMID] [PMCID]
- Chen FC, Shao HL, Han FL. A pilot study of neuromuscular electrical stimulation for neuropathic pain caused by spinal cord injury. Medicine. 2018; 97(31):e11658. [DOI:10.1097/MD.0000000000011658] [PMID] [PMCID]
- Miao Q, Qiang JH, Jin YL. Effectiveness of percutaneous neuromuscular electrical stimulation for neck pain relief in patients with cervical spondylosis. Medicine. 2018; 97(26):e11080. [DOI:10.1097/MD.0000000000011080] [PMID] [PMCID]
- Martimbianco ALC, Torloni MR, Andriolo BN, Porfírio GJ, Riera R. Neuromuscular Electrical Stimulation (NMES) for patellofemoral pain syndrome. The Cochrane Database of Systematic Reviews. 2017; 12(12):CD011289. [DOI:10.1002/14651858.CD011289.pub2] [PMID] [PMCID]
- Zhou M, Li F, Lu W, Wu J, Pei S. Efficiency of neuromuscular electrical stimulation and transcutaneous nerve stimulation on hemiplegic shoulder pain: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation. 2018; 99(9):1730-9. [DOI:10.1016/j.apmr.2018.04.020] [PMID]
- Bi XL, Xie CX. Effect of neuromuscular electrical stimulation for endometriosis-associated pain: A retrospective study. Medicine. 2018; 97(26):e11266. [DOI:10.1097/MD.0000000000011266] [PMID] [PMCID]
- Varani K, Gessi S, Merighi S, Iannotta V, Cattabriga E, Spisani S, et al. Effect of low frequency electromagnetic fields on A2A adenosine receptors in human neutrophils. British Journal of Pharmacology. 2002; 136(1):57-66. [DOI:10.1038/sj.bjp.0704695] [PMID] [PMCID]
- Massari L, Fini M, Cadossi R, Setti S, Traina GC. Biophysical stimulation with pulsed electromagnetic fields in osteonecrosis of the femoral head. The Journal of Bone and Joint Surgery. 2006; 88(Suppl 3):56-60. [DOI:10.2106/JBJS.F.00536] [PMID]
- Leo M, Milena F, Ruggero C, Stefania S, Giancarlo T. Biophysical stimulation in osteonecrosis of the femoral head. Indian Journal of Orthopaedics. 2009; 43(1):17-21. [DOI:10.4103/0019-5413.45319] [PMID] [PMCID]
- Al-Jabri T, Tan JYQ, Tong GY, Shenoy R, Kayani B, Parratt T, et al. The role of electrical stimulation in the management of avascular necrosis of the femoral head in adults: A systematic review. BMC Musculoskeletal Disorders. 2017; 18(1):319. [DOI:10.1186/s12891-017-1663-5] [PMID] [PMCID]
- Neumayr LD, Aguilar C, Earles AN, Jergesen HE, Haberkern CM, Kammen BF, et al. Physical therapy alone compared with core decompression and physical therapy for femoral head osteonecrosis in sickle cell disease: Results of a multicenter study at a mean of three years after treatment. The Journal of Bone and Joint Surgery. 2006; 88(12):2573-82. [DOI:10.2106/00004623-200612000-00003] [PMID]
Type of Study: Research |
Subject:
General
Received: 2020/07/3 | Accepted: 2021/04/20 | Published: 2021/07/1
Received: 2020/07/3 | Accepted: 2021/04/20 | Published: 2021/07/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |