Sun, Feb 22, 2026
Volume 10, Issue 2 (Spring 2020)
PTJ 2020, 10(2): 99-106 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Abshenas E, Karimi Zadeh Ardakani M, Takhtaei M, Naderi Beni M. Comparison of Functional Stability of Shoulder Girdle Between Individuals With Symmetric and Asymmetric Scapula. PTJ 2020; 10 (2) :99-106
URL: http://ptj.uswr.ac.ir/article-1-432-en.html
URL: http://ptj.uswr.ac.ir/article-1-432-en.html
1- Department of Health and Sport Medicine, Faculty of Physical Education and Sport Sciences, University of Tehran, Tehran, Iran.
2- Department of Motor Behavior, Faculty of Physical Education and Sport Sciences, University of Tehran, Tehran, Iran.
2- Department of Motor Behavior, Faculty of Physical Education and Sport Sciences, University of Tehran, Tehran, Iran.
Full-Text [PDF 1062 kb]
(2185 Downloads)
| Abstract (HTML) (4529 Views)
Subsequently, the subjects with minimal clothing were present at the test site, and the distance from the inferior-medial angle of scapula to the nearest spinous process was measured using the Kibler’s Lateral Scapular Slide Test (LSST) at 0, 45, and 90 degrees of shoulder abduction (Figure 1).
.jpg)
Statistical method: Data were analyzed by SPSS V. 22 and EXCEL 2016 software using the Kolmogorov-Smirnov test for examining data normality. An independent t-test was used to compare the data with normal distribution between the two groups, whereas the Mann-Whitney test was applied for data with no normal distribution at the significance level of 0.05.
3. Results
According to the results of the Kolmogorov-Smirnov test, all data showed normal distribution, except the results of the Davis test. Therefore, the Mann-Whitney U test was used for assessing the results of the Davis test, because data had no normal distribution.
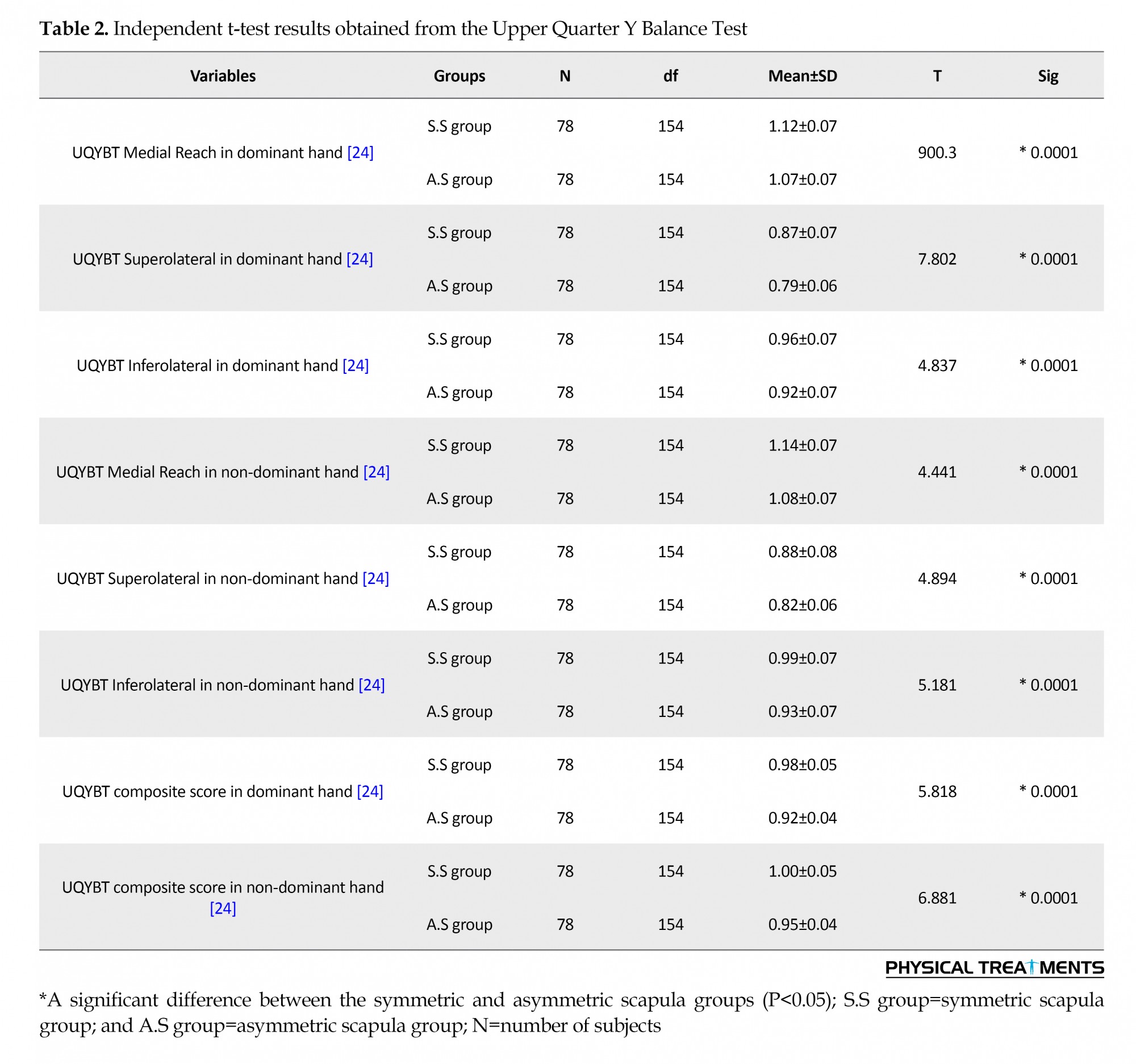
The independent t-test was used to compare the results of the groups obtained from the UQYBT with a normal distribution. According to the results of the independent t-test in Table 2, there was a significant difference between the groups with symmetric and asymmetric scapula in the normalized scores of each direction and the total score of each hand (P=0.0001).
Due to the non-normal distribution of data for the Davis test, the Mann-Whitney U test was used to compare between groups. The results of the Mann-Whitney U test in Table 3 indicated that a significant difference between the groups with symmetric and asymmetric scapulae in Davis test scores (P=0.0001).
4. Discussion
The results of this study showed that the functional stability of the shoulder girdle in the symmetric scapular group was significantly better than those in the asymmetric scapular group in all three directions. Also, in the superior and non-superior hands of both groups, the highest access score was achieved in the middle, inferolateral, and superolateral directions, respectively, which was consistent with previous studies. The reason for this finding may be the fact that the person’s hand in the middle direction is in the access direction and is likely to score higher, whereas, in the superolateral direction, the person’s hand is in its farthest position from the access point [21, 22, 25, 26].
So far, functional stability of the shoulder girdle has been evaluated several disorders, including shoulder impingement syndrome, anterior shoulder instability, and even some musculoskeletal abnormalities, such as round shoulder [27]. Hazar et al. (2014) showed that there was a significant difference between the two groups with and without shoulder impingement in the middle-inferior and lateral directions of the UQYBT, but there was no significant difference in the superolateral directions in the two groups [27].
In another study, Zandi et al. reported that healthy volleyball players had better performance stability in the shoulder girdle area in all three middle, inferior-lateral, and superolateral directions, as well as the score of UQYBT compared with volleyball players with anterior glenohumeral instability [25]. Due to glenohumeral instability, abnormalities in the function of mechanical receptors lead to the inhibition of the stabilizing neuro-muscular responses that may eventually cause repeated and progressive damage to the joint by dysfunction in the deep sensory system.
In a study by Beyranvand et al. (2017), they reported that some musculoskeletal abnormalities, such as rounded shoulders can also decrease the functional stability of shoulder girdle muscles by changing in their activities, leading to decreasing subjects’ access scores on the UQYBT [28]. They concluded that changes in the functional stability of the shoulder girdle might pave the way for possible future injuries.
One of the main roles of the scapula is its acting as a muscular connecting point, especially for the scapular stabilizer muscles, where the displacement of the scapula can affect the muscular function of this area, especially the stabilizer muscle [8]. Odom et al. stated that the position of the scapula is very important for the production of muscle strength and stability in the area [9]. Payne also believed that the weakness of the scapular stabilizer muscles is the reason for the biomechanical displacement of the scapula [29].
The inability of the scapula to perform its functions properly reduces its physiological and biomechanical performance, which may result in poor performance and increased damage to the shoulder area [5]. Concerning the causes of these consequences, it has been suggested that changes in the position of the scapula and the direction of the force around it may impair the feedback of the joint spindle receptors, and by reducing the optimal performance of joint afferents, modify the motility patterns, which must act on the accurate feedback of the deep sensory receptors. In such circumstances, the muscle patterns lose the ability to function in a coordinated manner and cannot manage muscle contraction [24, 30, 31]. Besides, in this situation, the performance of the scapular stabilizer muscles loses its optimal state, which leads to functional instability with reduced muscle activity and lack of muscle coordination in the functional area of the shoulder girdle.
5. Conclusion
No study has yet been conducted comparing the functional stability of the scapula girdle between individuals with the asymmetric and symmetric scapula. According to the findings of this study, scapular asymmetry and disruption of the scapular position can decrease functional stability and optimal performance quality in this area. Also, asymmetry in the scapulae can be examined to predict shoulder injuries.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Department of Health and Sport Medicine of Tehran University of Medical Sciences (Code: IR.UT.SPORT.REC.1398.029).All ethical principles are considered in this article. The participants were informed about the purpose of the research and its implementation stages; they were also assured about the confidentiality of their information; moreover, they were free to leave the study whenever they wished, and if desired, the research results would be available to them.
Funding
This research was extracted from the research project (No.30938/1), Funded by the University of Tehran.
Authors' contributions
All authors contribute in preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the sincere cooperation of the Vice-Chancellor of Research at the University of Tehran.
References
Voight ML, Thomson BC. The role of the scapula in the rehabilitation of shoulder injuries. Journal of Athletic Training. 2000; 35(3):364-72. [PMID] [PMCID]
Gumina S, Carbone S, Postacchini F. Scapular dyskinesis and SICK scapula syndrome in patients with chronic type III acromioclavicular dislocation. Arthroscopy. 2009; 25(1):40-5. [DOI:10.1016/j.arthro.2008.08.019] [PMID]
Terry GC, Chopp TM. Functional anatomy of the shoulder. Journal of Athletic Training. 2000; 35(3):248-55. [PMID] [PMCID]
Kibler WB, Ludewig PM, McClure PW, Michener LA, Bak K, Sciascia AD. Clinical implications of scapular dyskinesis in shoulder injury: The 2013 consensus statement from the ‘scapular summit’. British Journal of Sports Medicine. 2013; 47(14):877-85. [DOI:10.1136/bjsports-2013-092425]
Garrett WE, Speer KP, Kirkendall DT. Principles and practice of orthopaedic sports medicine. Philadelphia: Lippincott Williams & Wilkins; 2000. https://books.google.com/books?id=xtVpQgAACAAJ&dq
Meyer KE, Saether EE, Soiney EK, Shebeck MS, Paddock KL, Ludewig PM. Three-dimensional scapular kinematics during the throwing motion. Journal of Applied Biomechanics. 2008; 24(1):24-34. [DOI:10.1123/jab.24.1.24] [PMID]
Houglum PA. Therapeutic exercise for athletic injuries. Champaign: Human Kinetics; 2002. https://books.google.com/books?id=z358QgAACAAJ&dq
Kibler WB. The role of the scapula in athletic shoulder function. The American Journal of Sports Medicine. 1998; 26(2):325-37. [DOI:10.1177/03635465980260022801] [PMID]
Odom CJ, Taylor Ab, Hurd CE, Denegar CR. Measurement of scapular asymmetry and assessment of shoulder dysfunction using the lateral scapular slide test: A reliability and validity study. Physical Therapy. 2001; 81(2):799-809. [DOI:10.1093/ptj/81.2.799] [PMID]
Mottram SL. Dynamic stability of the scapula. Manual Therapy. 1997; 2(3):123-31. [DOI:10.1054/math.1997.0292] [PMID]
DePalma MJ, Johnson EW. Detecting and treating shoulder impingement syndrome: The role of scapulothoracic dyskinesis. The Physician and Sportsmedicine. 2003; 31(7):25-32. [DOI:10.1080/00913847.2003.11440616] [PMID]
Nodehi Moghadam A, Rouhbakhsh Z, Ebrahimi I, Salavati M, Jafari D, Mohammadi Z. [Shoulder girdle muscles endurance in subjects with and without impingement syndrome (Persian)]. Archive of Rehabilitation. 2011; 12(2):56-63. http://rehabilitationj.uswr.ac.ir/article-1-965-en.html
Fırat T, Türker T. Is the long sarcomere length responsible for non-traumatic supraspinatus tendinopathy? Potential novel pathophysiology and implications for physiotherapy. Pathophysiology. 2012; 19(3):179-83. [DOI:10.1016/j.pathophys.2012.04.008] [PMID]
Day JM, Bush H, Nitz AJ, Uhl TL. Scapular muscle performance in individuals with lateral epicondylalgia. Journal of Orthopaedic & Sports Physical Therapy. 2015; 45(5):414-24. [DOI:10.2519/jospt.2015.5290] [PMID]
Ebaugh DD, McClure PW, Karduna AR. Effects of shoulder muscle fatigue caused by repetitive overhead activities on scapulothoracic and glenohumeral kinematics. Journal of Electromyography and Kinesiology. 2006; 16(3):224-35. [DOI:10.1016/j.jelekin.2005.06.015] [PMID]
Moore SD, Uhl TL, Kibler WB. Improvements in shoulder endurance following a baseball-specific strengthening program in high school baseball players. Sports Health. 2013; 5(3):233-8. [DOI:10.1177/1941738113477604] [PMID] [PMCID]
Pollock A, Farmer SE, Brady MC, Langhorne P, Mead GE, Mehrholz J, et al. Interventions for improving upper limb function after stroke. Cochrane Database of Systematic Reviews. 2014; 2014(11):CD010820. [DOI:10.1002/14651858.CD010820.pub2] [PMID] [PMCID]
Kibler W. Clinical examination of the shoulder. In: Pettrone FA, editor. Athletic Injuries of the Shoulder. New York: McGraw-Hill; 1995. https://books.google.com/books?id=A15sAAAAMAAJ&q
T’Jonck LT, Lysens R, Grasse G. Measurements of scapular position and rotation: A reliability study. Physiotherapy Research International. 1996; 1(3):148-58. [DOI:10.1002/pri.55] [PMID]
Cook G. Movement: Functional movement systems: Screening, assessment, corrective strategies. Mumbai: On Target Publications: 2010. https://books.google.com/books?id=iOadmwEACAAJ&dq
Westrick RB, Miller JM, Carow SD, Gerber JP. Exploration of the y-balance test for assessment of upper quarter closed kinetic chain performance. International Journal of Sports Physical Therapy. 2012; 7(2):139-47. [PMID] [PMCID]
Butler RJ, Myers HS, Black D, Kiesel KB, Plisky PJ, Moorman CT, et al. Bilateral differences in the upper quarter function of high school aged baseball and softball players. International Journal of Sports Physical Therapy. 2014; 9(4):518-24. [PMID] [PMCID]
Lewis J, Green A, Reichard Z, Wright C. Scapular position: The validity of skin surface palpation. Manual Therapy. 2002; 7(1):26-30. [DOI:10.1054/math.2001.0405] [PMID]
Myers JB, Ju YY, Hwang JH, McMahon PJ, Rodosky MW, Lephart SM, et al. Reflexive muscle activation alterations in shoulders with anterior glenohumeral instability. The American Journal of Sports Medicine. 2004; 32(4):1013-21. [DOI:10.1177/0363546503262190] [PMID]
Zandi S, Rajabi R, Minoonejad H, Mohseni-Bandpei M. [Upper quarter functional stability in female volleyball players with and without anterior shoulder instability, with consideration of arm dominance (Persian)]. Archives of Rehabilitation. 2016; 16(4):346-55. http://rehabilitationj.uswr.ac.ir/article-1-1774-en.html
Beyranvand R, Mirnasouri R, Mostofi S, Salari S. [The effect of low back pain on functional stability of the upper limb in gymnast athletes in Khoramabad 2017 (Persian)]. Journal of Rafsanjan University of Medical Sciences. 2018; 17(8):759-68. http://journal.rums.ac.ir/article-1-4166-en.html
Hazar Z, Ulug N, Yuksel I. Upper quarter y-balance test score of patients with shoulder impingement syndrome. Orthopaedic Journal of Sports Medicine. 2014; 2(3 Suppl):2325967114S00275. [DOI:10.1177/2325967114S00275] [PMCID]
Beyranvand R, Mirnasouri R, Mollahoseini S, Mostofi S. The functional stability of the upper limbs in healthy and rounded shoulder gymnasts. Science of Gymnastics Journal. 2017; 9(3):279-90. https://bit.ly/2OY0fM8
Paine RM, Voight M. The role of the scapula. Journal of Orthopaedic & Sports Physical Therapy. 1993; 18(1):386-91. [DOI:10.2519/jospt.1993.18.1.386] [PMID]
Guido Jr JA, Stemm J. Reactive neuromuscular training: A multi-level approach to rehabilitation of the unstable shoulder. North American Journal of Sports Physical Therapy. 2007; 2(2):97-103. [PMID] [PMCID]
Myers JB, Lephart SM. Sensorimotor deficits contributing to glenohumeral instability. Clinical Orthopaedics and Related Research. 2002; 400:98-104. [DOI:10.1097/00003086-200207000-00013] [PMID]
Full-Text: (1711 Views)
1. Introduction
it and healthy body posture requires coordination of different parts of the body, and scapula and more generally shoulder girdle is one of the parts playing a key role in maintaining good body posture [1].
The shoulder girdle is a complex musculoskeletal system that allows for extensive upper extremity movement and function [2], which acts as a stabilizer and fixed point for moving muscular head. It also enables the transfer of power from the limb to the trunk and allows performing a wide range of movements [2-4].
The connection between the scapula and the chest wall through the stabilization of muscles allows for a complex three-dimensional motion that causes extensive upper extremity mobility [4]. The role of the scapula has received considerable attention in recent years because it plays an important role in producing smooth and coordinated shoulder girdle movements [1]. Kibler acknowledges that the role of the scapula in many movements is to obtain the proper motions and positions to facilitate shoulder function [5]. In other words, appropriate scapular movements are vital to the normal mechanics of the shoulder [6]. One of the main roles of the scapula is acting as a base for muscle attachment and its displacement can affect the function of the muscles around the shoulder girdle, especially the scapular stabilizer muscles [5, 7, 8]. Also, the position of the scapula is directly related to the production of muscle forces [9] and the range of motion of the shoulder girdle [1].
The inability of the scapula bone to perform its functions causes it to lose its physiological and biomechanical efficacy; therefore, the shoulder function will lose its effectiveness. This can lead to poor performance and increased shoulder injuries [5]. It seems that the displacement of the scapula can affect the function and production of the shoulder girdle muscular force, especially the scapular stabilizer muscles [10].
According to Kibler, decreasing the asymmetry of the scapula position indicates the increasing role of the scapular muscle stabilizer in controlling the approaching motion of the scapula during abduction [8]. It has also been stated that asymmetry of 1.5 cm or more in each of the three zero (neutral), 45, and 90-degree abduction modes is considered abnormal for clinical evaluation [8].
Imbalance of the agonist and antagonist muscles of the glenohumeral joint can cause damage to the shoulder joint and subsequent problems, including impingement syndrome [11, 12]. Muscular endurance is also the ability of a muscle to perform a sustained activity that is performed as isometric or isotonic contraction [13]. Muscular endurance in the shoulder area is responsible for the prevention of pain and many problems in the area [14-16]. The muscular stability and endurance of the shoulder girdle have always been emphasized due to the important connection between the trunk and the upper extremity. The stability of the shoulder girdle is crucial for optimal upper extremity motor function [17].
The position of the scapula is critical to the quality of performance of this area; therefore, by the scapular displacement, the probability of the functional stability reduction and subsequent injury is increased. Due to the very high importance of stability and endurance of the shoulder girdle in maintaining the health of this area, the current research was conducted to compare shoulder area stability and endurance using the Davis and Upper Quarter Y Balance Test (UQYBT) tests in subjects with the symmetric and asymmetric scapula.
2. Materials and Methods
Research Design
This descriptive cross-sectional study was conducted on 156 male students of Tehran University who were selected by cluster sampling. The research was carried out in a university dormitory complex. Buildings were assigned numbers and were chosen by lot, and then rooms were randomly selected, and each resident was haphazardly selected from predetermined numbers and was subsequently evaluated. Assessments were conducted on these residents. This research was ethically reviewed and approved by the Department of Health and Sports Medicine of Tehran University of Medical Sciences.
At first, a brief description of the purpose of the research and its implementation was described for the subjects. Then, personal information form (age, sex, height, and weight) (Table 1), injury history, and consent form were completed for all subjects and those with no history of acute shoulder injury entered the measurement phase.
it and healthy body posture requires coordination of different parts of the body, and scapula and more generally shoulder girdle is one of the parts playing a key role in maintaining good body posture [1].
The shoulder girdle is a complex musculoskeletal system that allows for extensive upper extremity movement and function [2], which acts as a stabilizer and fixed point for moving muscular head. It also enables the transfer of power from the limb to the trunk and allows performing a wide range of movements [2-4].
The connection between the scapula and the chest wall through the stabilization of muscles allows for a complex three-dimensional motion that causes extensive upper extremity mobility [4]. The role of the scapula has received considerable attention in recent years because it plays an important role in producing smooth and coordinated shoulder girdle movements [1]. Kibler acknowledges that the role of the scapula in many movements is to obtain the proper motions and positions to facilitate shoulder function [5]. In other words, appropriate scapular movements are vital to the normal mechanics of the shoulder [6]. One of the main roles of the scapula is acting as a base for muscle attachment and its displacement can affect the function of the muscles around the shoulder girdle, especially the scapular stabilizer muscles [5, 7, 8]. Also, the position of the scapula is directly related to the production of muscle forces [9] and the range of motion of the shoulder girdle [1].
The inability of the scapula bone to perform its functions causes it to lose its physiological and biomechanical efficacy; therefore, the shoulder function will lose its effectiveness. This can lead to poor performance and increased shoulder injuries [5]. It seems that the displacement of the scapula can affect the function and production of the shoulder girdle muscular force, especially the scapular stabilizer muscles [10].
According to Kibler, decreasing the asymmetry of the scapula position indicates the increasing role of the scapular muscle stabilizer in controlling the approaching motion of the scapula during abduction [8]. It has also been stated that asymmetry of 1.5 cm or more in each of the three zero (neutral), 45, and 90-degree abduction modes is considered abnormal for clinical evaluation [8].
Imbalance of the agonist and antagonist muscles of the glenohumeral joint can cause damage to the shoulder joint and subsequent problems, including impingement syndrome [11, 12]. Muscular endurance is also the ability of a muscle to perform a sustained activity that is performed as isometric or isotonic contraction [13]. Muscular endurance in the shoulder area is responsible for the prevention of pain and many problems in the area [14-16]. The muscular stability and endurance of the shoulder girdle have always been emphasized due to the important connection between the trunk and the upper extremity. The stability of the shoulder girdle is crucial for optimal upper extremity motor function [17].
The position of the scapula is critical to the quality of performance of this area; therefore, by the scapular displacement, the probability of the functional stability reduction and subsequent injury is increased. Due to the very high importance of stability and endurance of the shoulder girdle in maintaining the health of this area, the current research was conducted to compare shoulder area stability and endurance using the Davis and Upper Quarter Y Balance Test (UQYBT) tests in subjects with the symmetric and asymmetric scapula.
2. Materials and Methods
Research Design
This descriptive cross-sectional study was conducted on 156 male students of Tehran University who were selected by cluster sampling. The research was carried out in a university dormitory complex. Buildings were assigned numbers and were chosen by lot, and then rooms were randomly selected, and each resident was haphazardly selected from predetermined numbers and was subsequently evaluated. Assessments were conducted on these residents. This research was ethically reviewed and approved by the Department of Health and Sports Medicine of Tehran University of Medical Sciences.
At first, a brief description of the purpose of the research and its implementation was described for the subjects. Then, personal information form (age, sex, height, and weight) (Table 1), injury history, and consent form were completed for all subjects and those with no history of acute shoulder injury entered the measurement phase.
Subsequently, the subjects with minimal clothing were present at the test site, and the distance from the inferior-medial angle of scapula to the nearest spinous process was measured using the Kibler’s Lateral Scapular Slide Test (LSST) at 0, 45, and 90 degrees of shoulder abduction (Figure 1).
.jpg)
This test was developed and applied by Kibler to assess the scapular asymmetry and evaluate the ability of the scapular fixator in three positions of 0, 45, and 90 degrees of shoulder abduction [18].
LSST test is performed as follows: the subject stands behind the examiner. In this position, first, the inner edge of the inferior angle of the scapula is found and marked with a marker. The inferior angle of the scapula can be a reference point in the measurement [19]. In the present study, the scapular position was measured in the following three positions:
First position or zero-degree arm abduction: In this position, the hands are next to the body (neutral). In this condition, the inner edge of the inferior angle of the scapula was first marked with a marker, and then the nearest vertebrae spinal process and its location were marked. The tape head was then placed on the marked spinal process and its distance to the inferior scapular angle was measured.
Second position or 45-degree arm abduction: In this position, the subject was asked to place his palms on the head of the thigh so that his thumb was backward and the other fingers forward. The inferior angle of the scapula was then specified in this position, and its distance to the spinal process of the previous vertebrae was measured.
Also, to compare the different access scores separately in different directions, these scores were normalized with upper limb length, and normalized access scores for each direction were used for comparison. Inter-rater reliability (r=0.80) and intra-rater reliability (r=1.00) were reported at a high level [21].
Davis test: Davis test was used to test the upper body agility and stabilization. In this test, two test strips were attached on the ground in 90 cm distance, and the subjects were asked to take a swimming position with each hand on one strip. Then, they were asked to touch the right strip with their left hands and left strip with right hands for 15 s at maximum speed consecutively (Figure 3).
The subjects performed the test three times and an average of three attempts was recorded as their records. It should be noted that the surface touch of the scapula is considered a valid method to determine the actual location of the scapula [23].LSST test is performed as follows: the subject stands behind the examiner. In this position, first, the inner edge of the inferior angle of the scapula is found and marked with a marker. The inferior angle of the scapula can be a reference point in the measurement [19]. In the present study, the scapular position was measured in the following three positions:
First position or zero-degree arm abduction: In this position, the hands are next to the body (neutral). In this condition, the inner edge of the inferior angle of the scapula was first marked with a marker, and then the nearest vertebrae spinal process and its location were marked. The tape head was then placed on the marked spinal process and its distance to the inferior scapular angle was measured.
Second position or 45-degree arm abduction: In this position, the subject was asked to place his palms on the head of the thigh so that his thumb was backward and the other fingers forward. The inferior angle of the scapula was then specified in this position, and its distance to the spinal process of the previous vertebrae was measured.
Third position or 90-degree arm abduction: In this position, the hands were raised from the sides of the body so that they were parallel to the ground. Then, the maximal internal rotation of the humerus was performed until the thumb was toward the ground. In this condition, the inferior angle of the scapula was determined and its distance to the spinal process of the previous vertebrae was measured [20].
Subjects with the asymmetry of greater than 1.5 cm in each of the three positions were assigned to the asymmetric scapular group and those with the asymmetry of less than 1 cm in the symmetric scapular group [18].
UQYBT: This test was performed using the Y device having a plate for placing the support hand. Some graded rods were attached to it on three sides, with a movable indicator mounted on each rod. By moving the indicator by the free hand, the level of achievement to it in that side was specified. In this test, the subject was asked to place the palms (elbows in extension) and the toes (without shoes) in the starting position (legs open shoulder width) and keep the spine and lower extremity in the same direction. In this position, the subject should maintain the position with his or her free hand and achieve the middle, inferolateral, and superolateral directions as far as possible (Figure 2).
.jpg)
To compare with other subjects, accessions with upper extremity length (the seventh cervical vertebra to the end of the longest finger at 90° shoulder abduction and elbow extension, wrist and finger extension) were normalized [20].
The access procedure was performed in all three directions consecutively, and the process was performed 3 times [21]. To calculate the combined score, the scores are given in the following formula [20]:
Composite score=(middle access+inferolateral access+superolateral access) / (Limb length×3) [22]Subjects with the asymmetry of greater than 1.5 cm in each of the three positions were assigned to the asymmetric scapular group and those with the asymmetry of less than 1 cm in the symmetric scapular group [18].
UQYBT: This test was performed using the Y device having a plate for placing the support hand. Some graded rods were attached to it on three sides, with a movable indicator mounted on each rod. By moving the indicator by the free hand, the level of achievement to it in that side was specified. In this test, the subject was asked to place the palms (elbows in extension) and the toes (without shoes) in the starting position (legs open shoulder width) and keep the spine and lower extremity in the same direction. In this position, the subject should maintain the position with his or her free hand and achieve the middle, inferolateral, and superolateral directions as far as possible (Figure 2).
.jpg)
To compare with other subjects, accessions with upper extremity length (the seventh cervical vertebra to the end of the longest finger at 90° shoulder abduction and elbow extension, wrist and finger extension) were normalized [20].
The access procedure was performed in all three directions consecutively, and the process was performed 3 times [21]. To calculate the combined score, the scores are given in the following formula [20]:
Also, to compare the different access scores separately in different directions, these scores were normalized with upper limb length, and normalized access scores for each direction were used for comparison. Inter-rater reliability (r=0.80) and intra-rater reliability (r=1.00) were reported at a high level [21].
Davis test: Davis test was used to test the upper body agility and stabilization. In this test, two test strips were attached on the ground in 90 cm distance, and the subjects were asked to take a swimming position with each hand on one strip. Then, they were asked to touch the right strip with their left hands and left strip with right hands for 15 s at maximum speed consecutively (Figure 3).
Statistical method: Data were analyzed by SPSS V. 22 and EXCEL 2016 software using the Kolmogorov-Smirnov test for examining data normality. An independent t-test was used to compare the data with normal distribution between the two groups, whereas the Mann-Whitney test was applied for data with no normal distribution at the significance level of 0.05.
3. Results
According to the results of the Kolmogorov-Smirnov test, all data showed normal distribution, except the results of the Davis test. Therefore, the Mann-Whitney U test was used for assessing the results of the Davis test, because data had no normal distribution.
The independent t-test was used to compare the results of the groups obtained from the UQYBT with a normal distribution. According to the results of the independent t-test in Table 2, there was a significant difference between the groups with symmetric and asymmetric scapula in the normalized scores of each direction and the total score of each hand (P=0.0001).
Due to the non-normal distribution of data for the Davis test, the Mann-Whitney U test was used to compare between groups. The results of the Mann-Whitney U test in Table 3 indicated that a significant difference between the groups with symmetric and asymmetric scapulae in Davis test scores (P=0.0001).
4. Discussion
The results of this study showed that the functional stability of the shoulder girdle in the symmetric scapular group was significantly better than those in the asymmetric scapular group in all three directions. Also, in the superior and non-superior hands of both groups, the highest access score was achieved in the middle, inferolateral, and superolateral directions, respectively, which was consistent with previous studies. The reason for this finding may be the fact that the person’s hand in the middle direction is in the access direction and is likely to score higher, whereas, in the superolateral direction, the person’s hand is in its farthest position from the access point [21, 22, 25, 26].
So far, functional stability of the shoulder girdle has been evaluated several disorders, including shoulder impingement syndrome, anterior shoulder instability, and even some musculoskeletal abnormalities, such as round shoulder [27]. Hazar et al. (2014) showed that there was a significant difference between the two groups with and without shoulder impingement in the middle-inferior and lateral directions of the UQYBT, but there was no significant difference in the superolateral directions in the two groups [27].
In another study, Zandi et al. reported that healthy volleyball players had better performance stability in the shoulder girdle area in all three middle, inferior-lateral, and superolateral directions, as well as the score of UQYBT compared with volleyball players with anterior glenohumeral instability [25]. Due to glenohumeral instability, abnormalities in the function of mechanical receptors lead to the inhibition of the stabilizing neuro-muscular responses that may eventually cause repeated and progressive damage to the joint by dysfunction in the deep sensory system.
In a study by Beyranvand et al. (2017), they reported that some musculoskeletal abnormalities, such as rounded shoulders can also decrease the functional stability of shoulder girdle muscles by changing in their activities, leading to decreasing subjects’ access scores on the UQYBT [28]. They concluded that changes in the functional stability of the shoulder girdle might pave the way for possible future injuries.
One of the main roles of the scapula is its acting as a muscular connecting point, especially for the scapular stabilizer muscles, where the displacement of the scapula can affect the muscular function of this area, especially the stabilizer muscle [8]. Odom et al. stated that the position of the scapula is very important for the production of muscle strength and stability in the area [9]. Payne also believed that the weakness of the scapular stabilizer muscles is the reason for the biomechanical displacement of the scapula [29].
The inability of the scapula to perform its functions properly reduces its physiological and biomechanical performance, which may result in poor performance and increased damage to the shoulder area [5]. Concerning the causes of these consequences, it has been suggested that changes in the position of the scapula and the direction of the force around it may impair the feedback of the joint spindle receptors, and by reducing the optimal performance of joint afferents, modify the motility patterns, which must act on the accurate feedback of the deep sensory receptors. In such circumstances, the muscle patterns lose the ability to function in a coordinated manner and cannot manage muscle contraction [24, 30, 31]. Besides, in this situation, the performance of the scapular stabilizer muscles loses its optimal state, which leads to functional instability with reduced muscle activity and lack of muscle coordination in the functional area of the shoulder girdle.
5. Conclusion
No study has yet been conducted comparing the functional stability of the scapula girdle between individuals with the asymmetric and symmetric scapula. According to the findings of this study, scapular asymmetry and disruption of the scapular position can decrease functional stability and optimal performance quality in this area. Also, asymmetry in the scapulae can be examined to predict shoulder injuries.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Department of Health and Sport Medicine of Tehran University of Medical Sciences (Code: IR.UT.SPORT.REC.1398.029).All ethical principles are considered in this article. The participants were informed about the purpose of the research and its implementation stages; they were also assured about the confidentiality of their information; moreover, they were free to leave the study whenever they wished, and if desired, the research results would be available to them.
Funding
This research was extracted from the research project (No.30938/1), Funded by the University of Tehran.
Authors' contributions
All authors contribute in preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank the sincere cooperation of the Vice-Chancellor of Research at the University of Tehran.
References
Voight ML, Thomson BC. The role of the scapula in the rehabilitation of shoulder injuries. Journal of Athletic Training. 2000; 35(3):364-72. [PMID] [PMCID]
Gumina S, Carbone S, Postacchini F. Scapular dyskinesis and SICK scapula syndrome in patients with chronic type III acromioclavicular dislocation. Arthroscopy. 2009; 25(1):40-5. [DOI:10.1016/j.arthro.2008.08.019] [PMID]
Terry GC, Chopp TM. Functional anatomy of the shoulder. Journal of Athletic Training. 2000; 35(3):248-55. [PMID] [PMCID]
Kibler WB, Ludewig PM, McClure PW, Michener LA, Bak K, Sciascia AD. Clinical implications of scapular dyskinesis in shoulder injury: The 2013 consensus statement from the ‘scapular summit’. British Journal of Sports Medicine. 2013; 47(14):877-85. [DOI:10.1136/bjsports-2013-092425]
Garrett WE, Speer KP, Kirkendall DT. Principles and practice of orthopaedic sports medicine. Philadelphia: Lippincott Williams & Wilkins; 2000. https://books.google.com/books?id=xtVpQgAACAAJ&dq
Meyer KE, Saether EE, Soiney EK, Shebeck MS, Paddock KL, Ludewig PM. Three-dimensional scapular kinematics during the throwing motion. Journal of Applied Biomechanics. 2008; 24(1):24-34. [DOI:10.1123/jab.24.1.24] [PMID]
Houglum PA. Therapeutic exercise for athletic injuries. Champaign: Human Kinetics; 2002. https://books.google.com/books?id=z358QgAACAAJ&dq
Kibler WB. The role of the scapula in athletic shoulder function. The American Journal of Sports Medicine. 1998; 26(2):325-37. [DOI:10.1177/03635465980260022801] [PMID]
Odom CJ, Taylor Ab, Hurd CE, Denegar CR. Measurement of scapular asymmetry and assessment of shoulder dysfunction using the lateral scapular slide test: A reliability and validity study. Physical Therapy. 2001; 81(2):799-809. [DOI:10.1093/ptj/81.2.799] [PMID]
Mottram SL. Dynamic stability of the scapula. Manual Therapy. 1997; 2(3):123-31. [DOI:10.1054/math.1997.0292] [PMID]
DePalma MJ, Johnson EW. Detecting and treating shoulder impingement syndrome: The role of scapulothoracic dyskinesis. The Physician and Sportsmedicine. 2003; 31(7):25-32. [DOI:10.1080/00913847.2003.11440616] [PMID]
Nodehi Moghadam A, Rouhbakhsh Z, Ebrahimi I, Salavati M, Jafari D, Mohammadi Z. [Shoulder girdle muscles endurance in subjects with and without impingement syndrome (Persian)]. Archive of Rehabilitation. 2011; 12(2):56-63. http://rehabilitationj.uswr.ac.ir/article-1-965-en.html
Fırat T, Türker T. Is the long sarcomere length responsible for non-traumatic supraspinatus tendinopathy? Potential novel pathophysiology and implications for physiotherapy. Pathophysiology. 2012; 19(3):179-83. [DOI:10.1016/j.pathophys.2012.04.008] [PMID]
Day JM, Bush H, Nitz AJ, Uhl TL. Scapular muscle performance in individuals with lateral epicondylalgia. Journal of Orthopaedic & Sports Physical Therapy. 2015; 45(5):414-24. [DOI:10.2519/jospt.2015.5290] [PMID]
Ebaugh DD, McClure PW, Karduna AR. Effects of shoulder muscle fatigue caused by repetitive overhead activities on scapulothoracic and glenohumeral kinematics. Journal of Electromyography and Kinesiology. 2006; 16(3):224-35. [DOI:10.1016/j.jelekin.2005.06.015] [PMID]
Moore SD, Uhl TL, Kibler WB. Improvements in shoulder endurance following a baseball-specific strengthening program in high school baseball players. Sports Health. 2013; 5(3):233-8. [DOI:10.1177/1941738113477604] [PMID] [PMCID]
Pollock A, Farmer SE, Brady MC, Langhorne P, Mead GE, Mehrholz J, et al. Interventions for improving upper limb function after stroke. Cochrane Database of Systematic Reviews. 2014; 2014(11):CD010820. [DOI:10.1002/14651858.CD010820.pub2] [PMID] [PMCID]
Kibler W. Clinical examination of the shoulder. In: Pettrone FA, editor. Athletic Injuries of the Shoulder. New York: McGraw-Hill; 1995. https://books.google.com/books?id=A15sAAAAMAAJ&q
T’Jonck LT, Lysens R, Grasse G. Measurements of scapular position and rotation: A reliability study. Physiotherapy Research International. 1996; 1(3):148-58. [DOI:10.1002/pri.55] [PMID]
Cook G. Movement: Functional movement systems: Screening, assessment, corrective strategies. Mumbai: On Target Publications: 2010. https://books.google.com/books?id=iOadmwEACAAJ&dq
Westrick RB, Miller JM, Carow SD, Gerber JP. Exploration of the y-balance test for assessment of upper quarter closed kinetic chain performance. International Journal of Sports Physical Therapy. 2012; 7(2):139-47. [PMID] [PMCID]
Butler RJ, Myers HS, Black D, Kiesel KB, Plisky PJ, Moorman CT, et al. Bilateral differences in the upper quarter function of high school aged baseball and softball players. International Journal of Sports Physical Therapy. 2014; 9(4):518-24. [PMID] [PMCID]
Lewis J, Green A, Reichard Z, Wright C. Scapular position: The validity of skin surface palpation. Manual Therapy. 2002; 7(1):26-30. [DOI:10.1054/math.2001.0405] [PMID]
Myers JB, Ju YY, Hwang JH, McMahon PJ, Rodosky MW, Lephart SM, et al. Reflexive muscle activation alterations in shoulders with anterior glenohumeral instability. The American Journal of Sports Medicine. 2004; 32(4):1013-21. [DOI:10.1177/0363546503262190] [PMID]
Zandi S, Rajabi R, Minoonejad H, Mohseni-Bandpei M. [Upper quarter functional stability in female volleyball players with and without anterior shoulder instability, with consideration of arm dominance (Persian)]. Archives of Rehabilitation. 2016; 16(4):346-55. http://rehabilitationj.uswr.ac.ir/article-1-1774-en.html
Beyranvand R, Mirnasouri R, Mostofi S, Salari S. [The effect of low back pain on functional stability of the upper limb in gymnast athletes in Khoramabad 2017 (Persian)]. Journal of Rafsanjan University of Medical Sciences. 2018; 17(8):759-68. http://journal.rums.ac.ir/article-1-4166-en.html
Hazar Z, Ulug N, Yuksel I. Upper quarter y-balance test score of patients with shoulder impingement syndrome. Orthopaedic Journal of Sports Medicine. 2014; 2(3 Suppl):2325967114S00275. [DOI:10.1177/2325967114S00275] [PMCID]
Beyranvand R, Mirnasouri R, Mollahoseini S, Mostofi S. The functional stability of the upper limbs in healthy and rounded shoulder gymnasts. Science of Gymnastics Journal. 2017; 9(3):279-90. https://bit.ly/2OY0fM8
Paine RM, Voight M. The role of the scapula. Journal of Orthopaedic & Sports Physical Therapy. 1993; 18(1):386-91. [DOI:10.2519/jospt.1993.18.1.386] [PMID]
Guido Jr JA, Stemm J. Reactive neuromuscular training: A multi-level approach to rehabilitation of the unstable shoulder. North American Journal of Sports Physical Therapy. 2007; 2(2):97-103. [PMID] [PMCID]
Myers JB, Lephart SM. Sensorimotor deficits contributing to glenohumeral instability. Clinical Orthopaedics and Related Research. 2002; 400:98-104. [DOI:10.1097/00003086-200207000-00013] [PMID]
Type of Study: Applicable |
Subject:
General
Received: 2020/01/12 | Accepted: 2020/05/18 | Published: 2020/07/9
Received: 2020/01/12 | Accepted: 2020/05/18 | Published: 2020/07/9
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |