Sun, Dec 7, 2025
Volume 10, Issue 1 (Winter 2020)
PTJ 2020, 10(1): 23-32 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mansori M H, Moghadas Tabrizi Y, Karimizadeh Ardakani M. Effects of a Four-Week Vestibular Exercise Program on Postural Control, Risk of Falling, and Quality of Life in Visually-impaired Individuals. PTJ 2020; 10 (1) :23-32
URL: http://ptj.uswr.ac.ir/article-1-421-en.html
URL: http://ptj.uswr.ac.ir/article-1-421-en.html
1- Department of Sports Medicine and Health, Faculty of Physical Education and Sport Sciences, University of Tehran, Tehran, Iran.
Full-Text [PDF 581 kb]
(4663 Downloads)
| Abstract (HTML) (5718 Views)
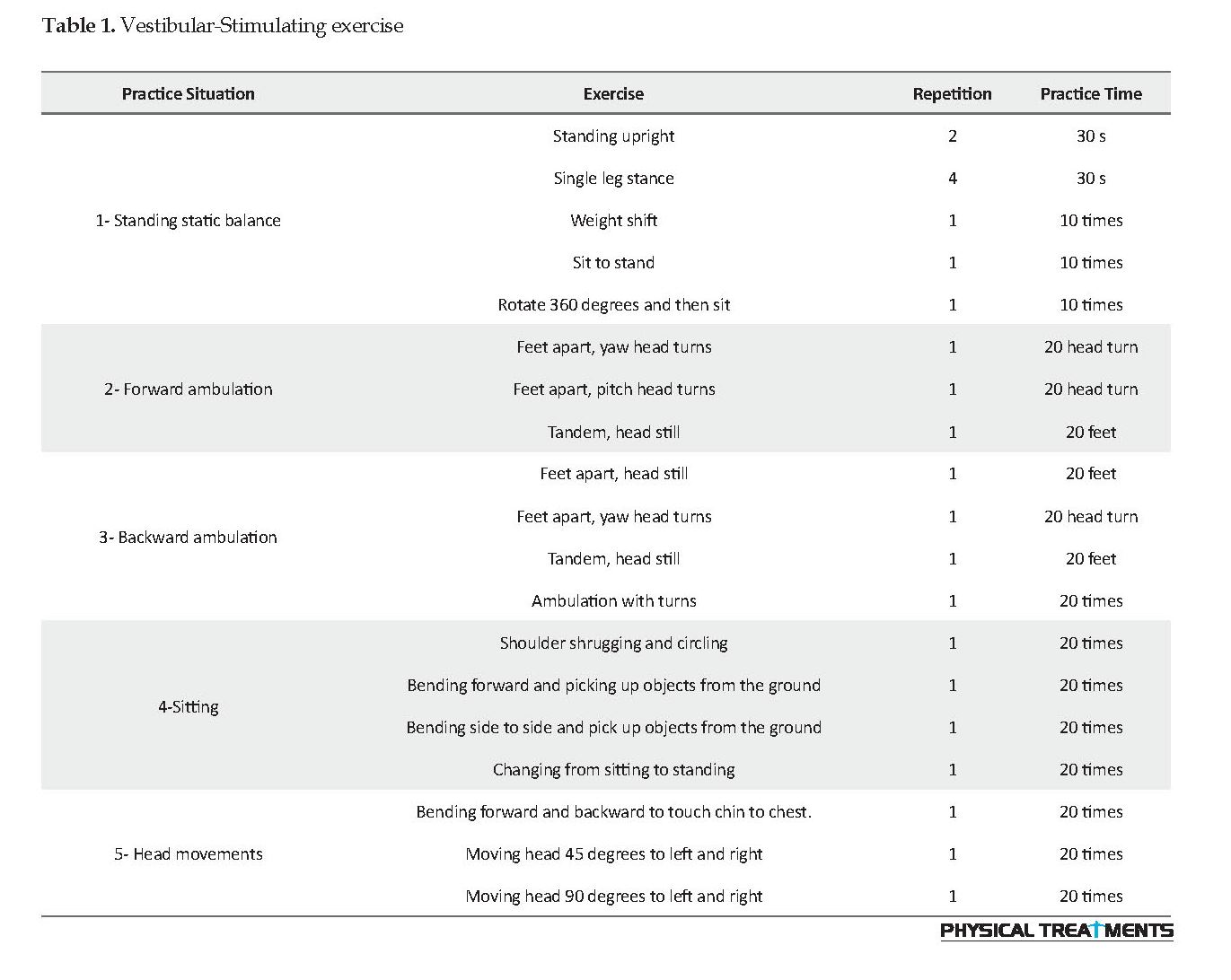
During this time, the control group performed their routine daily activities (Table 1). In addition to using sports coaches alongside the blind people to keep them safe during the exercises, any unexpected event that could endanger the study samples was prevented by verbal feedback along with the samples at all stages of the researcher’s practice. The subjects attempted to perform the actual exercises with physical feedback.
Descriptive and inferential statistics were used to analyze the collected data. Shapiro-Wilk test was implemented to check the normal distribution of data. Analysis of Covariance (ANCOVA) was also used to investigate the differences in scores of postural control indices, risk of falls, and quality of life between the two groups. Moreover, Paired Samples t-test was applied to investigate the intra-group differences at a significance level of 0.05. All statistical measures were performed by SPSS.
3. Results
The study participants’ characteristics, including height, weight, and age, and the results of the homogeneity of the groups are described in Table 2.
.jpg)
As per Table 2, the Independent Samples t-test results indicated no significant difference between the two groups in terms of height, weight, and age (P>0.05), and the two groups were homogeneous in all the above cases.
Given the normality of the data, determined by the Shapiro-Wilk test, ANCOVA and Paired Samples t-test were used to evaluate the impact of the exercises and their comparison. ANCOVA was used to compare the risk of falling, quality of life, and postural control index between the two groups at posttest (Table 3).
.jpg)
The ANCOVA results indicated a significant difference between the experimental and control groups in static and dynamic parameters of biodex, the risk of falling test, and overall quality of life (P<0.05). The achieved mean scores specified that the experimental group subjects had a performance than the controls. Paired Samples t-test was used for comparing postural control, risk of falling, and quality of life within the study groups and between the pretest and posttest values (Table 4).
.jpg)
Full-Text: (4229 Views)
1. Introduction
Balance or postural stability indicates the body’s ability to maintain the center of gravity of the body within the range of support or the ability to maintain a posture to perform a movement or respond to an external perturbation [1]. The human body is fundamentally unstable in a standing position. The center of gravity displacements affects the fluctuations of the human body. The exact location of the center of gravity is not directly understood for the human Central Nervous System (CNS); however, it requires the integration of input information from different senses (input data from visual, vestibular and somatosensory systems, e.g., proprioception, joints, and skin receptors) [2].
Postural control is a complex process, in which the balance disorder could be caused by somatosensory, visual, vestibular, musculoskeletal, or cognitive problems, like the fear of falling. A new theory that has created the basis of researchers’ work in terms of motion and balance is the theory of systems. According to this theory, the ability to maintain and control the body’s position in space results from a complex interaction that occurs between various musculoskeletal and nervous systems; the importance of each system varies according to the purpose of movement and environmental conditions [3]. Impairments in either of these segments could lead to postural control disorders and so on.
Moreover, all of these sensory areas are involved in individuals with visual impairment [4]. Vision plays a central role in maintaining postural stability. Visual impairment reduces the ability to balance and causes disorders, falls, job disabilities, and recurring injuries [5]. A healthy person’s body fluctuations with their eyes closed while standing are increased by 20% to 70% relative to the when their eyes are open. Vision also significantly affects motor control and balance in humans and is more important than other sources of sensory input to the CNS [6]. In addition to changes in postural control, the lack of vision results in increased social dependency, restricted daily living activities, reduced self-esteem, and increased risk of falling. A study on falls in the elderly reported that the blind elderly are at greater risks of falling than their deaf counterparts [7].
Various studies have indicated that visual impairment affects one’s quality of life and reduces their social activities and independence [8]. Masaki concluded that blind youth gained lower scores in most variables of quality of life questionnaire, compared to the norm values of quality of life in the Japanese community; the quality of their daily lives was below the norm of society [9]. The results of previous research on balance deficits and compensating strategies for blind people are contradictory [10]. A reason for this may be because blind people can compensate for their visual impairment by gaining confidence from the stability of proprioception and the vestibular system.
This process may be more active in visually-impaired people because the vestibular system plays a vital role as sensory receptors when other neural resources are reduced or eliminated [11]. A reason for this may be because blind people can compensate for their disability through other sensory factors involved in postural control (proprioception and vestibular system). These senses may play a more significant role in maintaining the body’s vertical alignment in the blind; thus, they compensate for the lack of vision system [12]. The vestibular system determines the primary source of such essential information [10].
Therefore, it is critical to find and use new methods to encourage social relationships between people with visual impairment and exercise at home [13].
One of these balance exercises is vestibular stimulation exercises [14]. Various studies have reported a positive effect of the vestibular system rehabilitation program on balance in people with Multiple Sclerosis (MS) [4, 15], intellectual disabilities [16], Down syndrome [17], Parkinson’s disease [18], and so on. These findings suggested a potential in developing a similar exercise program for individuals without such vestibular abnormalities. The vestibular system transmits information on the movement of head and direction of gravity to the CNS and causes rapid muscle responses, called automated body posture responses. Accordingly, in case of imbalance, ankle extensor muscles are activated 80 to 150 MS after the onset of imbalance by otoliths, i.e., involved in the creation of automatic postural responses that provide proper balance [19].
Studies have revealed that vestibular rehabilitation is a key treatment for balance disorders [20]. According to prior research, the risk of falls and loss of balance is higher in people with visual impairments, compared to the healthy population. Afferent sensory information through the vestibular or sensory system is provided for visually-impaired individuals who receive 80% of the sensory perception in different situations [21]. Furthermore, vestibular rehabilitation exercises involve balance control centers, such as the vestibular system, vision, and proprioception [22].
Exercise therapy is a cost-benefit and effective method of reducing functional disorders. According to studies, a proper rehabilitation program that includes strengthening the balance of muscular strength and repetitive movements could have a greater effect on medication, than the treatment of positional vertigo and balance disorders [23]. Among these methods, vestibular rehabilitation is a useful non-invasive method in treating unilateral, bilateral, and control balance disorders or in reducing symptoms, such as dizziness, nausea, vomiting, and so on [4].
However, it is unclear whether the vestibular stimulation exercises could compensate for the lack of vision in visually-impaired individuals. In addition, the effect of vestibular stimulation exercises to stimulate and improve the vestibular system, create new movement patterns, as well as postural stabilization and postural control in individuals with visual impairments is also examined. Such research may help us better understand the mechanisms in maintaining balance, postural control, and performance improvement in individuals with visual impairment; accordingly, appropriate and diverse training could be suggested to this community. Therefore, the present study aimed to investigate the effect of vestibular exercises on the quality of life, risk of falling, and postural control individuals with visual impairments.
2. Participants and Methods
Research Design: The present study was conducted in the Faculty of Physical Education, University of Tehran, in Tehran City, Iran, in 2018. This was a quasi-experimental research with a pretest-posttest and one control group design. In this study, the minimum sample, size according to previous research, was estimated using the G*power software with a test power of 80%, confidence interval of 95%, and effect size of 0.3 for each group of 12 subjects. The statistical sample consisted of 24 blind students of Tehran University with the age range of 20-30 years who were selected by convenience and purposive sampling method. After referring to the learning Center of the University of Tehran, the study samples were determined. Then, those with complete congenital and acquired blindness were enrolled by studying the academic records of students.
Individuals who voluntarily intended to participate in the research, according to the inclusion criteria, were selected by explaining the research process to them. The inclusion criteria were as follows: male gender, absolute blindness, ability to walk independently, the lack of pain and injury in the lumbar region, trunk, and lower limbs, the absence of apparent musculoskeletal disorders of the lower extremities, voluntary participation in research, understanding the research guidelines [24] and no sensory disorder, other than blindness [25-27]. Exclusion criteria consisted of any pain during exercise, dizziness, and nausea during exercise [26], as well as the lack of satisfaction about continuing to research and collaborating with the researcher.
Eligible individuals were invited for a meeting to become familiarized with the research process. During the session, the study participants were provided with test instructions and a training program. All individuals became familiar with the research process and goals before starting the research process. Then, they signed a consent form approved by the Faculty of Physical Education of Tehran University. The study subjects were randomly divided into control (n=12) and experimental (n=12) groups. The experimental group performed a 4-week vestibular exercise program for 3 weekly sessions of 50 minutes [14].
Timed Up and Go (TUG) Test [28], Biodex Balance System [29], and the quality of life questionnaire of 36-Item Short-Form Health Survey (SF-36) [30] were used to respectively assess the risk of falls, postural control, and quality of life of the study samples before and after conducting the exercise intervention. The tests were performed by the researcher in the same condition as well as the same time of day, from each subject.
The Timed Up and Go (TUG) Test: This test was designed by Matthias in 1986 with a rating scale of one to 5. The TUG test consists of sitting on a chair, standing, and walking up to three meters, as well as returning and sitting on a chair. The assessment criterion of this test is the length of time that a person performs this movement from the moment they rise from the seat until returning the first sitting position, i.e., measured with a stopwatch. The validity and reliability of this test were reported to be favorable [Intraclass Correlation Coefficient (ICC)=0.97-0.98] [28].
Biodex Balance System: Biodex Medical System Inc. model, made by the USA, was used to evaluate static and dynamic balance in the study participants. Biodex Balance System could perform balance test and balance training and three types of static and dynamic tests, as well as stability range. The stability indices provided by the system indicate the degree of deviation of the plane from the horizontal position. These indices include the overall stability index, anterior-posterior index, and medial-lateral stability index [29]. Additionally, the validity and reliability of the biodex device in assessing the balance of blind individuals have been supported by Aidug et al. [25, 31]. Before each test, the study subjects rested for 5 minutes in a sitting position. During the test, the subjects were dressed in light and loose-fitting clothing and placed on the device screen bare feet.
Before each measurement, the appropriate position of the legs and stature was monitored by the researcher. Each test was repeated for 20 seconds and three times, with a rest interval of 10 seconds. The study subjects were requested to stand on the balance plate with the help of the device’s handles in which feet distance from each other was as much as 10% of the height, and the person felt comfortable. The spatial position of the heels was recorded by determining the location of the heels on the calibrated plate and the angle of the foot axis (along with the second finger). The position of the legs was determined using the angles available on the device screen.
These values were recorded and applied for other test conditions. In all balance tests, the study participant had to stand on a plate in which its degree of stability was adjustable from 1 to 12 for 20 seconds; they had to maintain their balance by holding the device screen horizontally. In this test, each individual had to hold the center of gravity in the center circle of the plate. In the present study, static surfaces were used to evaluate static balance in a two-legged standing position with eyes closed, and dynamic surfaces in level 8 were used to evaluate dynamic balance [25]. To increase the sample safety, two instructor assistants helped during tests on the back and side of the subject to prevent any sudden falls. The study samples were also presented at the beginning of the measurement that they could use the device’s knobs at any time to counteract their falling.
Quality of Life Questionnaire: The SF-36 questionnaire was used and validated in Tehran, Iran, to measure the quality of life of the study subjects. Internal consistency in subscales other than vitality, using Cronbach’s alpha coefficient, was obtained as the range of 0.77 to 0.9 [30]. The scale consists of 36 items that include 8 subscales, including physical functioning, physical role functioning, bodily pain, general health, emotional role functioning, social performance, mental health, and vitality. The obtainable score for each item is between 0 and 100, and the score for each subscale is obtained by calculating the mean score of its subscales [32]. To fill out the questionnaire, the researcher would read the questions to the subject; then complete the questionnaire according to the subject’s answer.
The experimental group performed 4 weeks (3 50-min sessions per week) using the vestibular stimulation exercise protocol (Table 1) [14].
Balance or postural stability indicates the body’s ability to maintain the center of gravity of the body within the range of support or the ability to maintain a posture to perform a movement or respond to an external perturbation [1]. The human body is fundamentally unstable in a standing position. The center of gravity displacements affects the fluctuations of the human body. The exact location of the center of gravity is not directly understood for the human Central Nervous System (CNS); however, it requires the integration of input information from different senses (input data from visual, vestibular and somatosensory systems, e.g., proprioception, joints, and skin receptors) [2].
Postural control is a complex process, in which the balance disorder could be caused by somatosensory, visual, vestibular, musculoskeletal, or cognitive problems, like the fear of falling. A new theory that has created the basis of researchers’ work in terms of motion and balance is the theory of systems. According to this theory, the ability to maintain and control the body’s position in space results from a complex interaction that occurs between various musculoskeletal and nervous systems; the importance of each system varies according to the purpose of movement and environmental conditions [3]. Impairments in either of these segments could lead to postural control disorders and so on.
Moreover, all of these sensory areas are involved in individuals with visual impairment [4]. Vision plays a central role in maintaining postural stability. Visual impairment reduces the ability to balance and causes disorders, falls, job disabilities, and recurring injuries [5]. A healthy person’s body fluctuations with their eyes closed while standing are increased by 20% to 70% relative to the when their eyes are open. Vision also significantly affects motor control and balance in humans and is more important than other sources of sensory input to the CNS [6]. In addition to changes in postural control, the lack of vision results in increased social dependency, restricted daily living activities, reduced self-esteem, and increased risk of falling. A study on falls in the elderly reported that the blind elderly are at greater risks of falling than their deaf counterparts [7].
Various studies have indicated that visual impairment affects one’s quality of life and reduces their social activities and independence [8]. Masaki concluded that blind youth gained lower scores in most variables of quality of life questionnaire, compared to the norm values of quality of life in the Japanese community; the quality of their daily lives was below the norm of society [9]. The results of previous research on balance deficits and compensating strategies for blind people are contradictory [10]. A reason for this may be because blind people can compensate for their visual impairment by gaining confidence from the stability of proprioception and the vestibular system.
This process may be more active in visually-impaired people because the vestibular system plays a vital role as sensory receptors when other neural resources are reduced or eliminated [11]. A reason for this may be because blind people can compensate for their disability through other sensory factors involved in postural control (proprioception and vestibular system). These senses may play a more significant role in maintaining the body’s vertical alignment in the blind; thus, they compensate for the lack of vision system [12]. The vestibular system determines the primary source of such essential information [10].
Therefore, it is critical to find and use new methods to encourage social relationships between people with visual impairment and exercise at home [13].
One of these balance exercises is vestibular stimulation exercises [14]. Various studies have reported a positive effect of the vestibular system rehabilitation program on balance in people with Multiple Sclerosis (MS) [4, 15], intellectual disabilities [16], Down syndrome [17], Parkinson’s disease [18], and so on. These findings suggested a potential in developing a similar exercise program for individuals without such vestibular abnormalities. The vestibular system transmits information on the movement of head and direction of gravity to the CNS and causes rapid muscle responses, called automated body posture responses. Accordingly, in case of imbalance, ankle extensor muscles are activated 80 to 150 MS after the onset of imbalance by otoliths, i.e., involved in the creation of automatic postural responses that provide proper balance [19].
Studies have revealed that vestibular rehabilitation is a key treatment for balance disorders [20]. According to prior research, the risk of falls and loss of balance is higher in people with visual impairments, compared to the healthy population. Afferent sensory information through the vestibular or sensory system is provided for visually-impaired individuals who receive 80% of the sensory perception in different situations [21]. Furthermore, vestibular rehabilitation exercises involve balance control centers, such as the vestibular system, vision, and proprioception [22].
Exercise therapy is a cost-benefit and effective method of reducing functional disorders. According to studies, a proper rehabilitation program that includes strengthening the balance of muscular strength and repetitive movements could have a greater effect on medication, than the treatment of positional vertigo and balance disorders [23]. Among these methods, vestibular rehabilitation is a useful non-invasive method in treating unilateral, bilateral, and control balance disorders or in reducing symptoms, such as dizziness, nausea, vomiting, and so on [4].
However, it is unclear whether the vestibular stimulation exercises could compensate for the lack of vision in visually-impaired individuals. In addition, the effect of vestibular stimulation exercises to stimulate and improve the vestibular system, create new movement patterns, as well as postural stabilization and postural control in individuals with visual impairments is also examined. Such research may help us better understand the mechanisms in maintaining balance, postural control, and performance improvement in individuals with visual impairment; accordingly, appropriate and diverse training could be suggested to this community. Therefore, the present study aimed to investigate the effect of vestibular exercises on the quality of life, risk of falling, and postural control individuals with visual impairments.
2. Participants and Methods
Research Design: The present study was conducted in the Faculty of Physical Education, University of Tehran, in Tehran City, Iran, in 2018. This was a quasi-experimental research with a pretest-posttest and one control group design. In this study, the minimum sample, size according to previous research, was estimated using the G*power software with a test power of 80%, confidence interval of 95%, and effect size of 0.3 for each group of 12 subjects. The statistical sample consisted of 24 blind students of Tehran University with the age range of 20-30 years who were selected by convenience and purposive sampling method. After referring to the learning Center of the University of Tehran, the study samples were determined. Then, those with complete congenital and acquired blindness were enrolled by studying the academic records of students.
Individuals who voluntarily intended to participate in the research, according to the inclusion criteria, were selected by explaining the research process to them. The inclusion criteria were as follows: male gender, absolute blindness, ability to walk independently, the lack of pain and injury in the lumbar region, trunk, and lower limbs, the absence of apparent musculoskeletal disorders of the lower extremities, voluntary participation in research, understanding the research guidelines [24] and no sensory disorder, other than blindness [25-27]. Exclusion criteria consisted of any pain during exercise, dizziness, and nausea during exercise [26], as well as the lack of satisfaction about continuing to research and collaborating with the researcher.
Eligible individuals were invited for a meeting to become familiarized with the research process. During the session, the study participants were provided with test instructions and a training program. All individuals became familiar with the research process and goals before starting the research process. Then, they signed a consent form approved by the Faculty of Physical Education of Tehran University. The study subjects were randomly divided into control (n=12) and experimental (n=12) groups. The experimental group performed a 4-week vestibular exercise program for 3 weekly sessions of 50 minutes [14].
Timed Up and Go (TUG) Test [28], Biodex Balance System [29], and the quality of life questionnaire of 36-Item Short-Form Health Survey (SF-36) [30] were used to respectively assess the risk of falls, postural control, and quality of life of the study samples before and after conducting the exercise intervention. The tests were performed by the researcher in the same condition as well as the same time of day, from each subject.
The Timed Up and Go (TUG) Test: This test was designed by Matthias in 1986 with a rating scale of one to 5. The TUG test consists of sitting on a chair, standing, and walking up to three meters, as well as returning and sitting on a chair. The assessment criterion of this test is the length of time that a person performs this movement from the moment they rise from the seat until returning the first sitting position, i.e., measured with a stopwatch. The validity and reliability of this test were reported to be favorable [Intraclass Correlation Coefficient (ICC)=0.97-0.98] [28].
Biodex Balance System: Biodex Medical System Inc. model, made by the USA, was used to evaluate static and dynamic balance in the study participants. Biodex Balance System could perform balance test and balance training and three types of static and dynamic tests, as well as stability range. The stability indices provided by the system indicate the degree of deviation of the plane from the horizontal position. These indices include the overall stability index, anterior-posterior index, and medial-lateral stability index [29]. Additionally, the validity and reliability of the biodex device in assessing the balance of blind individuals have been supported by Aidug et al. [25, 31]. Before each test, the study subjects rested for 5 minutes in a sitting position. During the test, the subjects were dressed in light and loose-fitting clothing and placed on the device screen bare feet.
Before each measurement, the appropriate position of the legs and stature was monitored by the researcher. Each test was repeated for 20 seconds and three times, with a rest interval of 10 seconds. The study subjects were requested to stand on the balance plate with the help of the device’s handles in which feet distance from each other was as much as 10% of the height, and the person felt comfortable. The spatial position of the heels was recorded by determining the location of the heels on the calibrated plate and the angle of the foot axis (along with the second finger). The position of the legs was determined using the angles available on the device screen.
These values were recorded and applied for other test conditions. In all balance tests, the study participant had to stand on a plate in which its degree of stability was adjustable from 1 to 12 for 20 seconds; they had to maintain their balance by holding the device screen horizontally. In this test, each individual had to hold the center of gravity in the center circle of the plate. In the present study, static surfaces were used to evaluate static balance in a two-legged standing position with eyes closed, and dynamic surfaces in level 8 were used to evaluate dynamic balance [25]. To increase the sample safety, two instructor assistants helped during tests on the back and side of the subject to prevent any sudden falls. The study samples were also presented at the beginning of the measurement that they could use the device’s knobs at any time to counteract their falling.
Quality of Life Questionnaire: The SF-36 questionnaire was used and validated in Tehran, Iran, to measure the quality of life of the study subjects. Internal consistency in subscales other than vitality, using Cronbach’s alpha coefficient, was obtained as the range of 0.77 to 0.9 [30]. The scale consists of 36 items that include 8 subscales, including physical functioning, physical role functioning, bodily pain, general health, emotional role functioning, social performance, mental health, and vitality. The obtainable score for each item is between 0 and 100, and the score for each subscale is obtained by calculating the mean score of its subscales [32]. To fill out the questionnaire, the researcher would read the questions to the subject; then complete the questionnaire according to the subject’s answer.
The experimental group performed 4 weeks (3 50-min sessions per week) using the vestibular stimulation exercise protocol (Table 1) [14].
During this time, the control group performed their routine daily activities (Table 1). In addition to using sports coaches alongside the blind people to keep them safe during the exercises, any unexpected event that could endanger the study samples was prevented by verbal feedback along with the samples at all stages of the researcher’s practice. The subjects attempted to perform the actual exercises with physical feedback.
Descriptive and inferential statistics were used to analyze the collected data. Shapiro-Wilk test was implemented to check the normal distribution of data. Analysis of Covariance (ANCOVA) was also used to investigate the differences in scores of postural control indices, risk of falls, and quality of life between the two groups. Moreover, Paired Samples t-test was applied to investigate the intra-group differences at a significance level of 0.05. All statistical measures were performed by SPSS.
3. Results
The study participants’ characteristics, including height, weight, and age, and the results of the homogeneity of the groups are described in Table 2.
.jpg)
As per Table 2, the Independent Samples t-test results indicated no significant difference between the two groups in terms of height, weight, and age (P>0.05), and the two groups were homogeneous in all the above cases.
Given the normality of the data, determined by the Shapiro-Wilk test, ANCOVA and Paired Samples t-test were used to evaluate the impact of the exercises and their comparison. ANCOVA was used to compare the risk of falling, quality of life, and postural control index between the two groups at posttest (Table 3).
.jpg)
The ANCOVA results indicated a significant difference between the experimental and control groups in static and dynamic parameters of biodex, the risk of falling test, and overall quality of life (P<0.05). The achieved mean scores specified that the experimental group subjects had a performance than the controls. Paired Samples t-test was used for comparing postural control, risk of falling, and quality of life within the study groups and between the pretest and posttest values (Table 4).
.jpg)
According to Table 4, vestibular training significantly differed in the static and dynamic parameters of biodex, risk of falling test scores, and the overall quality of life score between pretest and posttest phases in the experimental group (P<0.05). However, no significant difference was observed among the research variables between the pretest and posttest phases (P>0.05).
4. Discussion
Balance is essential for individuals with visual impairments and helps maintain their physical condition in space [33]. Balance disorders have been the subject of numerous studies; the results of such studies have been used to develop and extend diverse exercises to address such disorders. Due to the lack of vision in the blind, the total amount of motor information storage and proper movement patterns in the CNS is reduced and generally affect the overall balance performance of the person. Studies have suggested that individuals with visual impairment perform poorer in postural control tests than their healthy counterparts [34].
According to the literature, the major problem of blind people is motor independence and balance, which also affects their quality of life. It has also affected all postural control indices in the Biodex Balance System in the study participants. In the experimental group, there was a significant difference between the pretest-posttest scores of postural control indices and the risk of falling across all subscales of quality of life (P<0.05), in addition to the improvement of the overall quality of life score. However, no significant difference was observed in the noted variables between the pretest and posttest values in the control group (P<0.05). The present study findings were consistent with those of Wizomirska [10], Sanderman [35], Samoudi [18], and Van Ching Chan [14], who found that vestibular exercises impacted balance and other factors in the disabled group.
Vestibular exercises are balance-based and used in people with vestibular system defects or those with impairments in vision or body functions [10]. Vestibular rehabilitation includes integrated sensory stimulation and vestibular stimulation therapies; it refers to implementing exercises, like repositioning techniques, as well as exercises to improve muscle strength and balance [17]. The effect of a 4-week vestibular exercise on the balance of individuals with positional vertigo was examined by Van Ching Chan et al. on 26 subjects (in two control and experimental groups of 13 with the mean age of 56 y) for 3 weekly sessions of 50 minutes. One-leg stance test and dynamic walking index were used before and after the intervention to evaluate the study sample’s balance.
It was concluded that there was a statistically significant difference in both tests in the first two weeks of the training program and at the end of the training program [14]. Besides, Sanderman (2016) explored vestibular stimulation exercises on balance in children with Down syndrome. In total, 18 patients were assigned to a control group consisting of 10 subjects and one experimental group consisting of 8 subjects. Vestibular exercises were performed for 6 weeks and twice a week for 1 hour to assess changes in coordination, balance, walking speed, agility, strength, proprioception, and upper extremity coordination in the study subjects. In the mentioned study, the single-leg standing and walking in a straight-line test were used to assess balance.
The relevant results revealed a significant difference in upper extremity coordination, static balance, and walking speed in the group performing the vestibular exercises. It was also emphasized that if an exercise intervention program is regularly applied to a specific group at younger ages, it can increase athletic and social participation, and improve the quality of life [35].
Mackias et al. investigated the effects of vestibular therapy on reducing falls in the elderly; they concluded that if rehabilitation treatment were performed immediately after the problem development, recovery would be much more successful and a better rate of balance would be achieved [20]. The present research findings were in line with domestic investigations, including Ghiasi [36], Qasemi [23], and Farzin [4].
The effect of vestibular exercises on balance, walking, and quality of life in individuals with vertigo caused by environmental injuries was examined by Qasemi et al. (2010). They used the Berg Balance Scale, Dynamic Gait Index, and Beck inventory; they observed significant effects of all of these variables at the end of training and even one month of lasting effect after completing the exercises [23]. The effect of vestibular exercises on the balance of people with unilateral vestibular problems was investigated in a study by Korena and associates. They concluded that exercise improves one’s ability to perform daily tasks and enhances quality of life by increasing the rate of control and balance [37]. Accordingly, vestibular rehabilitation might provide the necessary stimuli for reorganization and central sensory integration; thus, it enhances proper body postural control through three mechanisms of replacement, adaptation, and habituation [15].
Such a measure allows the brain to maintain balance with signals coming from the inner ear, as well as relying on signals initiating from the eyes, knees, legs, and neck to improve balance and reduce the risk of falls [38]. The CNS processes input signals and integrates those with other sensory information to estimate head awareness. In this case, the outputs of the central vestibular system are transmitted to ocular muscles and the spinal cord producing two major oculars -vestibular and spinal-vestibular reflexes which activates anti-gravity muscles, i.e., extensors, and inhibits flexor muscles. Thus, it plays an important role in creating appropriate postural responses and movement strategies in organs, such as ankle, thigh, and leg [39].
Other benefits of this physiotherapy include increasing balance, the relaxation of neck and shoulder muscles, affecting balance mechanisms in the neck, and reducing the risk of falling. Consequently, it leads to increased self-esteem, participation in social activities, the improvement of ocular -vestibular and spinal-vestibular reflex functions, effective identification of appropriate postural movement strategies, and the improvement of natural postural strategies and gait. This especially occurs in patients who suffer from vertigo in case of moving their heads, using alternative strategies by the somatosensory system, residual vestibular and vision functions, increased mobility and endurance of walking, anxiety reduction (that may occur as a result of sensory mismatch due to abnormal signals from the vestibular system), improved general physical conditions and general coordination, as well as supporting natural and automatic movements, increased motivation, socialization, and positive psychological effects [39, 40].
According to the results of the present study and the concurrent research, it can be concluded that due to the manipulation and stimulation of the vestibular system and possibly the reliance of the blind on this sense in balance and motor function, these subjects demonstrated better performance during the stimulation and rehabilitation of the vestibular system at the same conditions in the posttest phase, compared to the control group, and their oscillations decreased. Thus, in support of previous research, concerning the blind people’s reliance on other senses (vestibular system and somatosensory), their balance and motor function are improved by reinforcing each of these senses, especially the vestibular system.
A limitation in this research was the lack of psychological state control for the samples, which could have affected the research results to some extent; same-gender samples, the lack of access to samples, and the small sample size were other study limitations. Another limitation in this research was considering one type of training program, i.e., not compared with other exercises; this could create another subject of study for researchers to compare vestibular training with different exercises.
Furthermore, for further research, is the following points are recommended. A similar study with a relatively high sample size be conducted on blind people to achieve more comprehensive and generalizable data. Performing similar research on females considering their age and technical level. Comparing different training methods on balance and risk of falling, and the motor function of blind people is recommended. It is also suggested that balance strategies be explored and compared during sudden disturbances of the level of trust between the people with and without visual impairment. Balance training protocols are based on strengthening each of the visual, sensory, and atrial systems; therefore, the role of these senses should be compared on the motor and balance function of the blind people.
5. Conclusion
According to the current study findings, there was a significant difference between the mean scores of the postural control index, the risk of falling, and the quality of life of blind people with disabilities in the experimental and control groups. This rehabilitation program leads to a significant improvement in these individuals. Given the numerous benefits of this rehabilitation and its domestic low-cost and easy application, it is suggested that this rehabilitation program be implemented on different visually-impaired groups. Teachers and coaches of students with visual impairment are recommended to use vestibular stimulation exercises implemented in the present study along with other exercises to increase physical fitness in schools.
Ethical Considerations
Compliance with ethical guidelines
All ethical principle were considered in this article and the present study was approved by the Ethics Committee of the Faculty of Physical Education of Tehran University (Code: IR.UT. SPORT.REC.1398.035).
Funding
The present paper was extracted from the MSc thesis of the first Department of Sports Medicine and Health, Faculty of Physical Education and Sport Sciences, University of Tehran.
Authors' contributions
Original idea, writing the manuscript, protocol development, abstract, and data analysis: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank Vice-Chancellor of Research at the University of Tehran.
References
Mohammadi F. [Assessment of CNS function on postural control with and without Somatosensory and Vestibular perturbation in globall players in comparison with non-athlete blind and sighted subjects (Persian)] [MA. Thesis]. Tehran: University of Tehran; 2008.
Popa T, Bonifazi M, Della Volpe R, Rossi A, Mazzocchio R. Adaptive changes in postural strategy selection in chronic low back pain. Experimental Brain Research. 2007; 177(3):411-8. [DOI:10.1007/s00221-006-0683-4] [PMID]
Shumway-Cook A, Woollacott MH. Motor control: Theory and practical applications. Philadelphia: Lippincott Williams & Wilkins; 2000.
Farzin F, Golpayegani M, Faraji F, Shahrjerdi S, Ghasemi P. [The effect of vestibular rehabilitation on dizzines and balance in patient with multiple sclerosis (Persian)]. Journal of Arak University of Medical Sciences. 2018; 21(2):65-74.
Blomqvist S, Rehn B. Validity and reliability of the Dynamic One Leg Stance (DOLS) in people with vision loss. Advances in Physiotherapy. 2007; 9(3):129-35. [DOI:10.1080/14038190701395671]
Paul M, Biswas SK, Sandhu JS. Role of sports vision and eye hand coordination training in performance of table tennis players. Brazilian Journal of Biomotricity. 2011; 5(2):106-16.
Soares AV, Oliveira CS, Knabben RJ, Domenech SC, Borges Junior NG. Postural control in blind subjects. Einstein (Sao Paulo). 2011; 9(4):470-6. [DOI:10.1590/s1679-45082011ao2046] [PMID]
West SK, Munoz B, Rubin GS, Schein OD, Bandeen-Roche K, Zeger S, et al. Function and visual impairment in a population-based study of older adults. The SEE project. Salisbury Eye Evaluation. Investigative Ophthalmology & Visual Science. 1997; 38(1):72-82.
Masaki I. Reduced health-related quality of life among Japanese college students with visual impairment. Biopsychosocial Medicine. 2015; 9:18. [DOI:10.1186/s13030-015-0045-1] [PMID] [PMCID]
Wiszomirska I, Kaczmarczyk K, Błażkiewicz M, Wit A. The impact of a vestibular-stimulating exercise regimen on postural stability in women over 60. Journal of Exercise Science & Fitness. 2015; 13(2):72-8.
Friedrich M, Grein H-J, Wicher C, Schuetze J, Mueller A, Lauenroth A, et al. Influence of pathologic and simulated visual dysfunctions on the postural system. Experimental Brain Research. 2008; 186(2):305-14. [DOI:10.1007/s00221-007-1233-4] [PMID]
Bacsi AM, Colebatch JG. Evidence for reflex and perceptual vestibular contributions to postural control. Experimental Brain Research. 2005; 160(1):22-8. [DOI:10.1007/s00221-004-1982-2] [PMID]
Çolak T, Bamaç B, Aydin M, Meriç B, Özbek A. Physical fitness levels of blind and visually impaired goalball team players. Isokinetics And Exercise Science. 2004; 12(4):247-52. [DOI:10.3233/IES-2004-0182]
Chang WC, Yang YR, Hsu LC, Chern CM, Wang RY. Balance improvement in patients with benign paroxysmal positional vertigo. Clinical Rehabilitation. 2008; 22(4):338-47. [DOI:10.1177/0269215507082741] [PMID]
Hebert JR, Corboy JR, Manago MM, Schenkman M. Effects of vestibular rehabilitation on multiple sclerosis-related fatigue and upright postural control: A randomized controlled trial. Physical Therapy. 2011; 91(8):1166-83. [DOI:10.2522/ptj.20100399] [PMID]
Badke MB, Miedaner JA, Grove CR, Shea TA, Pyle GM. Effects of vestibular and balance rehabilitation on sensory organization and dizziness handicap. Annals of Otology, Rhinology & Laryngology. 2005; 114(1):48-54. [DOI:10.1177/000348940511400109] [PMID]
Carter K, Sunderman S, Burnett SW. The effect of vestibular stimulation exercises on balance, coordination, and agility in children with Down syndrome. American Journal of Psychiatry and Neuroscience. 2018; 6(2):28-32. [DOI:10.11648/j.ajpn.20180602.11]
Samoudi G, Jivegård M, Mulavara AP, Bergquist F. Effects of stochastic vestibular galvanic stimulation and LDOPA on balance and motor symptoms in patients with Parkinson’s disease. Brain Stimulation. 2015; 8(3):474-80. [DOI:10.1016/j.brs.2014.11.019] [PMID] [PMCID]
Herdman S, Clendaniel RA. Vestibular rehabilitation. Philadelphia: F.A. Davis Company; 2014.
Macias JD, Massingale S, Gerkin RD. Efficacy of vestibular rehabilitation therapy in reducing falls. Otolaryngology-Head and Neck Surgery. 2005; 133(3):323-5. [DOI:10.1016/j.otohns.2005.04.024] [PMID]
Legood R, Scuffham P, Cryer C. Are we blind to injuries in the visually impaired? A review of the literature. Injury Prevention. 2002; 8(2):155-60. [DOI:10.1136/ip.8.2.155] [PMID] [PMCID]
Zanardini FH1, Zeigelboim BS, Jurkiewicz AL, Marques JM, Martins-Bassetto J. [Vestibular rehabilitation in elderly patients with dizziness (Portuguese)]. Pro-fono Revista de Atualização Cientifica. 2007; 19(2):177-84. [DOI:10.1590/S0104-56872007000200006] [PMID]
Ghasemi E, Shayegannejad V, Ghorbani A, Momeni N, Khani F. The effectiveness of exercise-therapy on improvement of balance, gait, quality of life and depression in elderly patients with vertigo due to peripheral disturbances of vestibular system. Journal of Research in Rehabilitation Sciences. 2010: 4(2):109-16.
Letafatkar K, Alizadeh M, Kordi M. The effect of exhausting exercise induced fatigue on the double-leg balance of elite male athletes. Journal of Social Sciences. 2009; 5(4):445-51. [DOI:10.3844/jssp.2009.445.451]
Aydoğ E, Aydoğ S, Cakci A, Doral M. Dynamic postural stability in blind athletes using the biodex stability system. International Journal of Sports Medicine. 2006; 27(05):415-8. [DOI:10.1055/s-2005-865777] [PMID]
Nithya Devi R. Effect of Cawthorne-Cooksey exercises along with breathing and proprioception exercises on balance, disability and postural control in vertigo patients. [PhD dissrtation]. Coimbatore: KG College of Physiotherapy; 2012.
Gaerlan MG. The role of visual, vestibular, and somatosensory systems in postural balance. Las Vegas: University of Nevada Las Vegas; 2010.
Raji P. Functional balance tests. Audiol. 2012; 21(4):1-9.
Malekzadeh H, Seidi F, Rajabi R. [Effect of circadian rhythms on knee joint position sense in men college soccer players (Persian)]. Journal of Research in Rehabilitation Sciences. 2015; 11(2):179-90.
Montazeri A, Goshtasebi A, Vahdaninia M, Gandek B. The Short Form Health Survey (SF-36): Translation and validation study of the Iranian version. Quality of Life Research. 2005; 14(3):875-82. [DOI:10.1007/s11136-004-1014-5] [PMID]
Cachupe WJ, Shifflett B, Kahanov L, Wughalter EH. Reliability of biodex balance system measures. Measurement in Physical Education and Exercise Science. 2001; 5(2):97-108. [DOI:10.1207/S15327841MPEE0502_3]
Khajavi D, Farrokhi A, Jaberi-Moghaddam AA, Kazemnejad A. [Effect of Strength and balance training program on maintaining balance and quality of life in older male adults with fear of fall (Persian)]. Iranian Journal of Ageing. 2016; 11(2):270-9. [DOI:10.21859/sija-1102270]
Wiszomirska I, Kaczmarczyk K, Błażkiewicz M, Wit A. The impact of a vestibular-stimulating exercise regime on postural stability in people with visual impairment. BioMed Research International. 2015; 2015:136969. [DOI:10.1155/2015/136969] [PMID] [PMCID]
King S, Wang J, Priesol AJ, Lewis RF. Central integration of canal and otolith signals is abnormal in vestibular migraine. Frontiers in Neurology. 2014; 5:233. [DOI:10.3389/fneur.2014.00233] [PMID] [PMCID]
Sunderman S. The effect of vestibular stimulation exercises on balance in children with Down syndrome. Medicine & Science in Sport & Exercise. 2016; 48(55):400. [DOI:10.1249/01.mss.0000486207.93485.39]
Ghiasi, k. The Impact of Eight Weeks Vestibular Exercises on Dynamic Balance in Students with Hearing Impairment. Isfahan: National Conference on Modern Research in Sport Science; 2018.
Corna S, Nardone A, Prestinari A, Galante M, Grasso M, Schieppati M. Comparison of Cawthorne-Cooksey exercises and sinusoidal support surface translations to improve balance in patients with unilateral vestibular deficit. Archives of Physical Medicine and Rehabilitation. 2003; 84(8):1173-84. [DOI:10.1016/S0003-9993(03)00130-8]
Ribeiro AdSB, Pereira JS. Balance improvement and reduction of likelihood of falls in older women after Cawthorne and Cooksey exercises. Brazilian Journal of Otorhinolaryngology. 2005; 71(1):38-46. [DOI:10.1016/S1808-8694(15)31283-0]
Simoceli L, Bittar RSM, Sznifer J. Adaptation exercises of vestibulo-ocular reflex on balance in the elderly. Journal of Otolaryngology of the World. 2008; 12(2):183-8.
Tavanai E, Hajiabolhassan F. Cervicogenic vertigo: Etiology, diagnosis and treatment. Auditory and Vestibular Research. 2013; 22(3):1-13.
4. Discussion
Balance is essential for individuals with visual impairments and helps maintain their physical condition in space [33]. Balance disorders have been the subject of numerous studies; the results of such studies have been used to develop and extend diverse exercises to address such disorders. Due to the lack of vision in the blind, the total amount of motor information storage and proper movement patterns in the CNS is reduced and generally affect the overall balance performance of the person. Studies have suggested that individuals with visual impairment perform poorer in postural control tests than their healthy counterparts [34].
According to the literature, the major problem of blind people is motor independence and balance, which also affects their quality of life. It has also affected all postural control indices in the Biodex Balance System in the study participants. In the experimental group, there was a significant difference between the pretest-posttest scores of postural control indices and the risk of falling across all subscales of quality of life (P<0.05), in addition to the improvement of the overall quality of life score. However, no significant difference was observed in the noted variables between the pretest and posttest values in the control group (P<0.05). The present study findings were consistent with those of Wizomirska [10], Sanderman [35], Samoudi [18], and Van Ching Chan [14], who found that vestibular exercises impacted balance and other factors in the disabled group.
Vestibular exercises are balance-based and used in people with vestibular system defects or those with impairments in vision or body functions [10]. Vestibular rehabilitation includes integrated sensory stimulation and vestibular stimulation therapies; it refers to implementing exercises, like repositioning techniques, as well as exercises to improve muscle strength and balance [17]. The effect of a 4-week vestibular exercise on the balance of individuals with positional vertigo was examined by Van Ching Chan et al. on 26 subjects (in two control and experimental groups of 13 with the mean age of 56 y) for 3 weekly sessions of 50 minutes. One-leg stance test and dynamic walking index were used before and after the intervention to evaluate the study sample’s balance.
It was concluded that there was a statistically significant difference in both tests in the first two weeks of the training program and at the end of the training program [14]. Besides, Sanderman (2016) explored vestibular stimulation exercises on balance in children with Down syndrome. In total, 18 patients were assigned to a control group consisting of 10 subjects and one experimental group consisting of 8 subjects. Vestibular exercises were performed for 6 weeks and twice a week for 1 hour to assess changes in coordination, balance, walking speed, agility, strength, proprioception, and upper extremity coordination in the study subjects. In the mentioned study, the single-leg standing and walking in a straight-line test were used to assess balance.
The relevant results revealed a significant difference in upper extremity coordination, static balance, and walking speed in the group performing the vestibular exercises. It was also emphasized that if an exercise intervention program is regularly applied to a specific group at younger ages, it can increase athletic and social participation, and improve the quality of life [35].
Mackias et al. investigated the effects of vestibular therapy on reducing falls in the elderly; they concluded that if rehabilitation treatment were performed immediately after the problem development, recovery would be much more successful and a better rate of balance would be achieved [20]. The present research findings were in line with domestic investigations, including Ghiasi [36], Qasemi [23], and Farzin [4].
The effect of vestibular exercises on balance, walking, and quality of life in individuals with vertigo caused by environmental injuries was examined by Qasemi et al. (2010). They used the Berg Balance Scale, Dynamic Gait Index, and Beck inventory; they observed significant effects of all of these variables at the end of training and even one month of lasting effect after completing the exercises [23]. The effect of vestibular exercises on the balance of people with unilateral vestibular problems was investigated in a study by Korena and associates. They concluded that exercise improves one’s ability to perform daily tasks and enhances quality of life by increasing the rate of control and balance [37]. Accordingly, vestibular rehabilitation might provide the necessary stimuli for reorganization and central sensory integration; thus, it enhances proper body postural control through three mechanisms of replacement, adaptation, and habituation [15].
Such a measure allows the brain to maintain balance with signals coming from the inner ear, as well as relying on signals initiating from the eyes, knees, legs, and neck to improve balance and reduce the risk of falls [38]. The CNS processes input signals and integrates those with other sensory information to estimate head awareness. In this case, the outputs of the central vestibular system are transmitted to ocular muscles and the spinal cord producing two major oculars -vestibular and spinal-vestibular reflexes which activates anti-gravity muscles, i.e., extensors, and inhibits flexor muscles. Thus, it plays an important role in creating appropriate postural responses and movement strategies in organs, such as ankle, thigh, and leg [39].
Other benefits of this physiotherapy include increasing balance, the relaxation of neck and shoulder muscles, affecting balance mechanisms in the neck, and reducing the risk of falling. Consequently, it leads to increased self-esteem, participation in social activities, the improvement of ocular -vestibular and spinal-vestibular reflex functions, effective identification of appropriate postural movement strategies, and the improvement of natural postural strategies and gait. This especially occurs in patients who suffer from vertigo in case of moving their heads, using alternative strategies by the somatosensory system, residual vestibular and vision functions, increased mobility and endurance of walking, anxiety reduction (that may occur as a result of sensory mismatch due to abnormal signals from the vestibular system), improved general physical conditions and general coordination, as well as supporting natural and automatic movements, increased motivation, socialization, and positive psychological effects [39, 40].
According to the results of the present study and the concurrent research, it can be concluded that due to the manipulation and stimulation of the vestibular system and possibly the reliance of the blind on this sense in balance and motor function, these subjects demonstrated better performance during the stimulation and rehabilitation of the vestibular system at the same conditions in the posttest phase, compared to the control group, and their oscillations decreased. Thus, in support of previous research, concerning the blind people’s reliance on other senses (vestibular system and somatosensory), their balance and motor function are improved by reinforcing each of these senses, especially the vestibular system.
A limitation in this research was the lack of psychological state control for the samples, which could have affected the research results to some extent; same-gender samples, the lack of access to samples, and the small sample size were other study limitations. Another limitation in this research was considering one type of training program, i.e., not compared with other exercises; this could create another subject of study for researchers to compare vestibular training with different exercises.
Furthermore, for further research, is the following points are recommended. A similar study with a relatively high sample size be conducted on blind people to achieve more comprehensive and generalizable data. Performing similar research on females considering their age and technical level. Comparing different training methods on balance and risk of falling, and the motor function of blind people is recommended. It is also suggested that balance strategies be explored and compared during sudden disturbances of the level of trust between the people with and without visual impairment. Balance training protocols are based on strengthening each of the visual, sensory, and atrial systems; therefore, the role of these senses should be compared on the motor and balance function of the blind people.
5. Conclusion
According to the current study findings, there was a significant difference between the mean scores of the postural control index, the risk of falling, and the quality of life of blind people with disabilities in the experimental and control groups. This rehabilitation program leads to a significant improvement in these individuals. Given the numerous benefits of this rehabilitation and its domestic low-cost and easy application, it is suggested that this rehabilitation program be implemented on different visually-impaired groups. Teachers and coaches of students with visual impairment are recommended to use vestibular stimulation exercises implemented in the present study along with other exercises to increase physical fitness in schools.
Ethical Considerations
Compliance with ethical guidelines
All ethical principle were considered in this article and the present study was approved by the Ethics Committee of the Faculty of Physical Education of Tehran University (Code: IR.UT. SPORT.REC.1398.035).
Funding
The present paper was extracted from the MSc thesis of the first Department of Sports Medicine and Health, Faculty of Physical Education and Sport Sciences, University of Tehran.
Authors' contributions
Original idea, writing the manuscript, protocol development, abstract, and data analysis: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank Vice-Chancellor of Research at the University of Tehran.
References
Mohammadi F. [Assessment of CNS function on postural control with and without Somatosensory and Vestibular perturbation in globall players in comparison with non-athlete blind and sighted subjects (Persian)] [MA. Thesis]. Tehran: University of Tehran; 2008.
Popa T, Bonifazi M, Della Volpe R, Rossi A, Mazzocchio R. Adaptive changes in postural strategy selection in chronic low back pain. Experimental Brain Research. 2007; 177(3):411-8. [DOI:10.1007/s00221-006-0683-4] [PMID]
Shumway-Cook A, Woollacott MH. Motor control: Theory and practical applications. Philadelphia: Lippincott Williams & Wilkins; 2000.
Farzin F, Golpayegani M, Faraji F, Shahrjerdi S, Ghasemi P. [The effect of vestibular rehabilitation on dizzines and balance in patient with multiple sclerosis (Persian)]. Journal of Arak University of Medical Sciences. 2018; 21(2):65-74.
Blomqvist S, Rehn B. Validity and reliability of the Dynamic One Leg Stance (DOLS) in people with vision loss. Advances in Physiotherapy. 2007; 9(3):129-35. [DOI:10.1080/14038190701395671]
Paul M, Biswas SK, Sandhu JS. Role of sports vision and eye hand coordination training in performance of table tennis players. Brazilian Journal of Biomotricity. 2011; 5(2):106-16.
Soares AV, Oliveira CS, Knabben RJ, Domenech SC, Borges Junior NG. Postural control in blind subjects. Einstein (Sao Paulo). 2011; 9(4):470-6. [DOI:10.1590/s1679-45082011ao2046] [PMID]
West SK, Munoz B, Rubin GS, Schein OD, Bandeen-Roche K, Zeger S, et al. Function and visual impairment in a population-based study of older adults. The SEE project. Salisbury Eye Evaluation. Investigative Ophthalmology & Visual Science. 1997; 38(1):72-82.
Masaki I. Reduced health-related quality of life among Japanese college students with visual impairment. Biopsychosocial Medicine. 2015; 9:18. [DOI:10.1186/s13030-015-0045-1] [PMID] [PMCID]
Wiszomirska I, Kaczmarczyk K, Błażkiewicz M, Wit A. The impact of a vestibular-stimulating exercise regimen on postural stability in women over 60. Journal of Exercise Science & Fitness. 2015; 13(2):72-8.
Friedrich M, Grein H-J, Wicher C, Schuetze J, Mueller A, Lauenroth A, et al. Influence of pathologic and simulated visual dysfunctions on the postural system. Experimental Brain Research. 2008; 186(2):305-14. [DOI:10.1007/s00221-007-1233-4] [PMID]
Bacsi AM, Colebatch JG. Evidence for reflex and perceptual vestibular contributions to postural control. Experimental Brain Research. 2005; 160(1):22-8. [DOI:10.1007/s00221-004-1982-2] [PMID]
Çolak T, Bamaç B, Aydin M, Meriç B, Özbek A. Physical fitness levels of blind and visually impaired goalball team players. Isokinetics And Exercise Science. 2004; 12(4):247-52. [DOI:10.3233/IES-2004-0182]
Chang WC, Yang YR, Hsu LC, Chern CM, Wang RY. Balance improvement in patients with benign paroxysmal positional vertigo. Clinical Rehabilitation. 2008; 22(4):338-47. [DOI:10.1177/0269215507082741] [PMID]
Hebert JR, Corboy JR, Manago MM, Schenkman M. Effects of vestibular rehabilitation on multiple sclerosis-related fatigue and upright postural control: A randomized controlled trial. Physical Therapy. 2011; 91(8):1166-83. [DOI:10.2522/ptj.20100399] [PMID]
Badke MB, Miedaner JA, Grove CR, Shea TA, Pyle GM. Effects of vestibular and balance rehabilitation on sensory organization and dizziness handicap. Annals of Otology, Rhinology & Laryngology. 2005; 114(1):48-54. [DOI:10.1177/000348940511400109] [PMID]
Carter K, Sunderman S, Burnett SW. The effect of vestibular stimulation exercises on balance, coordination, and agility in children with Down syndrome. American Journal of Psychiatry and Neuroscience. 2018; 6(2):28-32. [DOI:10.11648/j.ajpn.20180602.11]
Samoudi G, Jivegård M, Mulavara AP, Bergquist F. Effects of stochastic vestibular galvanic stimulation and LDOPA on balance and motor symptoms in patients with Parkinson’s disease. Brain Stimulation. 2015; 8(3):474-80. [DOI:10.1016/j.brs.2014.11.019] [PMID] [PMCID]
Herdman S, Clendaniel RA. Vestibular rehabilitation. Philadelphia: F.A. Davis Company; 2014.
Macias JD, Massingale S, Gerkin RD. Efficacy of vestibular rehabilitation therapy in reducing falls. Otolaryngology-Head and Neck Surgery. 2005; 133(3):323-5. [DOI:10.1016/j.otohns.2005.04.024] [PMID]
Legood R, Scuffham P, Cryer C. Are we blind to injuries in the visually impaired? A review of the literature. Injury Prevention. 2002; 8(2):155-60. [DOI:10.1136/ip.8.2.155] [PMID] [PMCID]
Zanardini FH1, Zeigelboim BS, Jurkiewicz AL, Marques JM, Martins-Bassetto J. [Vestibular rehabilitation in elderly patients with dizziness (Portuguese)]. Pro-fono Revista de Atualização Cientifica. 2007; 19(2):177-84. [DOI:10.1590/S0104-56872007000200006] [PMID]
Ghasemi E, Shayegannejad V, Ghorbani A, Momeni N, Khani F. The effectiveness of exercise-therapy on improvement of balance, gait, quality of life and depression in elderly patients with vertigo due to peripheral disturbances of vestibular system. Journal of Research in Rehabilitation Sciences. 2010: 4(2):109-16.
Letafatkar K, Alizadeh M, Kordi M. The effect of exhausting exercise induced fatigue on the double-leg balance of elite male athletes. Journal of Social Sciences. 2009; 5(4):445-51. [DOI:10.3844/jssp.2009.445.451]
Aydoğ E, Aydoğ S, Cakci A, Doral M. Dynamic postural stability in blind athletes using the biodex stability system. International Journal of Sports Medicine. 2006; 27(05):415-8. [DOI:10.1055/s-2005-865777] [PMID]
Nithya Devi R. Effect of Cawthorne-Cooksey exercises along with breathing and proprioception exercises on balance, disability and postural control in vertigo patients. [PhD dissrtation]. Coimbatore: KG College of Physiotherapy; 2012.
Gaerlan MG. The role of visual, vestibular, and somatosensory systems in postural balance. Las Vegas: University of Nevada Las Vegas; 2010.
Raji P. Functional balance tests. Audiol. 2012; 21(4):1-9.
Malekzadeh H, Seidi F, Rajabi R. [Effect of circadian rhythms on knee joint position sense in men college soccer players (Persian)]. Journal of Research in Rehabilitation Sciences. 2015; 11(2):179-90.
Montazeri A, Goshtasebi A, Vahdaninia M, Gandek B. The Short Form Health Survey (SF-36): Translation and validation study of the Iranian version. Quality of Life Research. 2005; 14(3):875-82. [DOI:10.1007/s11136-004-1014-5] [PMID]
Cachupe WJ, Shifflett B, Kahanov L, Wughalter EH. Reliability of biodex balance system measures. Measurement in Physical Education and Exercise Science. 2001; 5(2):97-108. [DOI:10.1207/S15327841MPEE0502_3]
Khajavi D, Farrokhi A, Jaberi-Moghaddam AA, Kazemnejad A. [Effect of Strength and balance training program on maintaining balance and quality of life in older male adults with fear of fall (Persian)]. Iranian Journal of Ageing. 2016; 11(2):270-9. [DOI:10.21859/sija-1102270]
Wiszomirska I, Kaczmarczyk K, Błażkiewicz M, Wit A. The impact of a vestibular-stimulating exercise regime on postural stability in people with visual impairment. BioMed Research International. 2015; 2015:136969. [DOI:10.1155/2015/136969] [PMID] [PMCID]
King S, Wang J, Priesol AJ, Lewis RF. Central integration of canal and otolith signals is abnormal in vestibular migraine. Frontiers in Neurology. 2014; 5:233. [DOI:10.3389/fneur.2014.00233] [PMID] [PMCID]
Sunderman S. The effect of vestibular stimulation exercises on balance in children with Down syndrome. Medicine & Science in Sport & Exercise. 2016; 48(55):400. [DOI:10.1249/01.mss.0000486207.93485.39]
Ghiasi, k. The Impact of Eight Weeks Vestibular Exercises on Dynamic Balance in Students with Hearing Impairment. Isfahan: National Conference on Modern Research in Sport Science; 2018.
Corna S, Nardone A, Prestinari A, Galante M, Grasso M, Schieppati M. Comparison of Cawthorne-Cooksey exercises and sinusoidal support surface translations to improve balance in patients with unilateral vestibular deficit. Archives of Physical Medicine and Rehabilitation. 2003; 84(8):1173-84. [DOI:10.1016/S0003-9993(03)00130-8]
Ribeiro AdSB, Pereira JS. Balance improvement and reduction of likelihood of falls in older women after Cawthorne and Cooksey exercises. Brazilian Journal of Otorhinolaryngology. 2005; 71(1):38-46. [DOI:10.1016/S1808-8694(15)31283-0]
Simoceli L, Bittar RSM, Sznifer J. Adaptation exercises of vestibulo-ocular reflex on balance in the elderly. Journal of Otolaryngology of the World. 2008; 12(2):183-8.
Tavanai E, Hajiabolhassan F. Cervicogenic vertigo: Etiology, diagnosis and treatment. Auditory and Vestibular Research. 2013; 22(3):1-13.
Type of Study: Applicable |
Subject:
Sport injury and corrective exercises
Received: 2019/07/19 | Accepted: 2020/01/1 | Published: 2020/05/31
Received: 2019/07/19 | Accepted: 2020/01/1 | Published: 2020/05/31
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |