Thu, Aug 28, 2025
Volume 9, Issue 2 (Spring 2019)
PTJ 2019, 9(2): 85-96 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sedaghatnezhad P, Rahnama L, Shams M, Karimi N. Uphill Walking Effect on the Disability of Patients With Knee Osteoarthritis. PTJ 2019; 9 (2) :85-96
URL: http://ptj.uswr.ac.ir/article-1-407-en.html
URL: http://ptj.uswr.ac.ir/article-1-407-en.html
1- Department of Physiotherapy, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Physical Therapy, University of North Georgia, Georgia, USA.
2- Department of Physical Therapy, University of North Georgia, Georgia, USA.
Full-Text [PDF 602 kb]
(1966 Downloads)
| Abstract (HTML) (3838 Views)
Table 2 presents the mean±SD of the subscales of the KOOS questionnaire at three assessment times; pre-test (before the treatment), post-test (after ten sessions of treatment), and follow-up (20 days after the treatment completion). According to the data of this table in both control and intervention groups, the lowest score recorded in all subscales was in the pre-test stage. All mean scores of subscales in both groups were similar in the pre-test (P>0.05) except for the sport and recreation activities (P=0.02) (Table 3). Therefore, to prevent the effect of the difference between the two groups in terms of this subscale on the test results, the changes in this difference were studied during the test stages.
Symptom Subscale
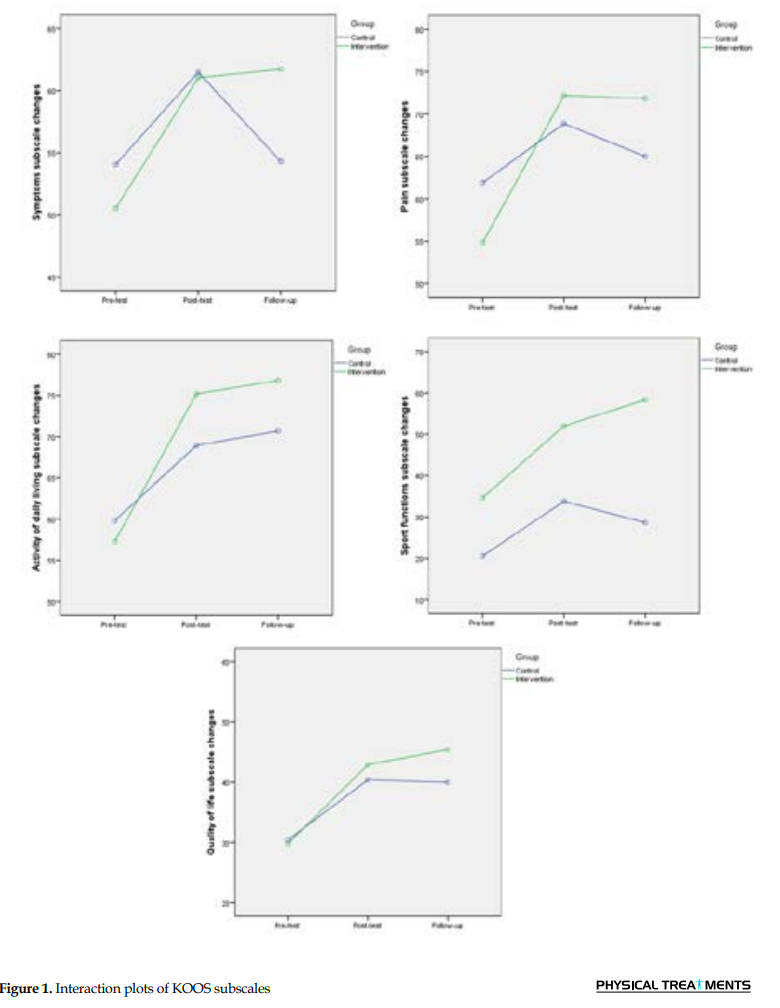
The results of the repeated measures ANOVA show a significant interaction effect of time by the group on the symptom subscale (F=4.14, P=0.03, ES=2.22), i.e. the changing procedure in this subscale is significant between the two groups during the study. According to Figure 1, the mean score of the symptom subscale in the intervention group was less than that of the control group in the pre-test, and the mean scores of the two groups were approximately the same in the post-test. Therefore, an increase in the score of this subscale in the intervention group was more than that of the control group. Also, in the follow-up and pre-test stages, the mean scores of the control group were almost the same, but in the intervention group, the increase in the scores continued from post-test to the follow-up stage. The results of the Bonferroni posthoc test showed that in the control group, the changes in this subscale were not significant in the post-test (P=0.09) and follow-up (P=0.94) compared to the pre-test. However, in the intervention group, the changes in the symptom subscale in both post-test (T=3.34, P=0.01, ES=0.86) and follow-up (T=4.06, P=0.003, ES=0.95) were significant compared to the pre-test. It means that only the treatment program of the intervention group caused a significant change in the scores of the symptom subscale and the persistency of change. The mean score of this subscale between the two groups was not significantly different in the post-test (P=0.91) and follow-up (P=0.11). Tables 3 and 4 present the results of within-group and between-group pairwise comparisons, respectively.
Pain Subscale
The results of repeated measures ANOVA show the significant interaction effect of time by the group on pain subscale (F=3.3, P=0.04, ES=0.86), i.e. the changing procedure of this subscale is significant between the two groups during the study. According to Figure 1, the mean score of the pain subscale in the intervention group was less than that of the control group in the pre-test and more in the post-test. Therefore, the increase in the score of this subscale in the intervention group is more than that of the control group. Also, in the follow-up and pre-test stages, the mean scores of the control group were almost the same, but it was almost constant in the intervention group from post-test to follow-up. The results of the Bonferroni posthoc test showed that in the control group, changes in this subscale were not significant in the post-test (P=0.18) and follow-up (P=0.5) compared to the pre-test. In the intervention group, changes in the pain subscale in both post-test (T=5.98, P<0.001, ES=1.02) and follow-up (T=4.39, P=0.001, ES=1.01) were significant compared to the pre-test. That is, only the treatment program in the intervention group has significantly changed the score of pain subscale and the persistency of change. The mean score of this subscale between the two groups was not significantly different in the post-test (P=0.58) and follow-up (P=0.34).
Activities of daily living subscale
The results of repeated measures ANOVA show that the interaction effect of time by the group has a significant effect on the subscale of activities of daily living (F=3.44, P=0.04, ES=0.82). According to Figure 1, the mean score of this subscale in the pre-test in the intervention group was slightly lower than that of the control group and was more than the control group in the post-test. Therefore, the gradient of an increase in the mean score of this subscale in the intervention group is greater than that of the control group. The results of the Bonferroni posthoc test showed that in the control group, changes in this subscale in the post-test (T=3.7, P=0.01, ES=0.61) and follow-up (T=4.33, P=0.001, ES=0.74) were significant compared to the pre-test. Also, in the intervention group, the changes in the subscales of activities of daily living in both post-test (T=5.38, P<0.001, ES=0.9) and follow-up (T=6.71, P<0.001, ES=0.94) were significant compared to the pre-test. Overall, the treatment program of both groups has significantly changed the scores of activities of daily living subscale and the persistency of this change. The mean score of this subscale between the two groups was not significantly different in the post-test (P=0.31) and follow-up (P=0.33).
Sport and recreation functions
The results of repeated measures ANOVA show that the interaction effect of time by the group is significant for the subscales of sport and recreation functions (F=3.66, P=0.03, ES=1.06). As shown in Figure 1, in all stages of the measurement, i.e. pre-test (T=2.36, P=0.02, ES=0.86), post-test (T=2.49, P=0.02, ES=1.11), and follow-up (T=4.5, P<0.001, ES=1.64), the mean score of the intervention group is greater than that of the control group. Considering the significant difference in the pre-test between the two groups, the changes in this difference were studied in different stages. The changes in this difference were not significant in the post-test compared to the pre-test (P=0.64), but in follow-up (T=2.62, P=0.02, ES=0.65), these changes were significant compared to the pre-test. Therefore, the treatment program of the intervention group increased the subscales of sport and recreation functions after 20 days of competition of the intervention.
Quality of life Subscale
Figure 1 shows similar changes in the quality of life subscale in response to treatment over time in the two groups; the time by group interaction on this subscale was not significant (P=0.47). The results of repeated measures ANOVA showed a significant effect of time on the quality of life subscale (F=16.53, P<0.001, ES=0.48), meaning that during the study, the score of this subscale has changed. The results of ANOVA showed that in the control group, changes in this subscale in the post-test (T=2.78, P=0.04, ES=0.6) and follow-up (T=3.52, P=0.02, ES=0.67) were significant compared to the pre-test. In the intervention group, the changes in the quality of life subscale in both post-test (T=3.33, P=0.005, ES=0.81) and follow-up 4.31, P<0.001, ES=1.06) were significant compared to the pre-test. Overall, the treatment program of both groups has significantly changed the scores of quality of life subscale and the persistency of this change. The main effect of the group in this subscale was not significant (P=0.63), meaning that the results of the treatment were the same in both groups.
4. Discussion
Disability is not only a consequence of a disease or injury but also a factor affecting people’s communication with the environment. Disability is one of the major consequences of lower extremities osteoarthritis, and since knee osteoarthritis is very common, its disability has a significant impact on the individual and the community. Considering that one of the goals of treatment in patients suffering from knee osteoarthritis is to minimize their disability, the present study investigated the effect of adding walking on the uphill treadmill to the routine physiotherapy program of patients with knee osteoarthritis on the disability of these patients.
The results of this study showed that adding uphill treadmill walking to the routine physiotherapy program would improve all subscales of the KOOS questionnaire and, thus, reduce the disability of people with knee osteoarthritis so that the recovery would be persistent up to 20 days. However, physiotherapy treatment in the control group did not improve pain, symptoms, and sport and recreation functions subscales.
The findings of this study about the effect of physiotherapy and exercise program on the disability of patients suffering from knee osteoarthritis are in line with the results of the studies by Ardakani, Miri, Esfandiari et al. and Ahadi et al. indicating the the significant improvement of subscales of KOOS questionnaire following stretching and strengthening exercises of hamstring and quadriceps muscles, adding dry needling to the physiotherapy program, and using orthoses with lateral wedge and physiotherapy, respectively, in patients with patellofemoral pain syndrome or knee osteoarthritis [36-39].
The results of this study indicate that the symptom subscale of KOOS questionnaire changes following the physiotherapy alone was not significant. The results also confirm Miri’s study that observed an insignificant change in the symptom subscale of the KOOS questionnaire after the usual physiotherapy treatment in patients with patellofemoral pain syndrome [37].
Patients with knee osteoarthritis tend to avoid physical activity to relieve pain. In the short term, avoiding physical activity helps patients to relieve pain, but in the long term, the reduction in activity levels leads to muscle weakness. Joint stability and its ability to withstand the applied loads reduce because of the muscle weakness, which ultimately leads to the patient’s disability and the avoidance of physical activities [40]. Another reason for disability is the reduction of a joint range of motion caused by the shortness of the joint capsule, muscles, and muscle spasm [41, 42]. Quadriceps muscle weakness in patients with knee pain is also associated with disability [43]. Evidence suggests that muscle weakness is associated with functional impairment following the muscle-strengthening programs, improving inability and reducing disability occurred [43, 44]. Among the reasons mentioned for disability (pain, limitation of range of motion, and muscle weakness), just muscle weakness factor has improved in the control group by strengthening exercise and has improved the subscales of activity of daily living and quality of life of this group of participants. However, in the intervention group, the three factors have improved, including a decrease in knee pain (increasing the score of the pain subscale), an increase in the limited range of motion of the knee joint because of stretching of the soft tissue of the posterior joint while walking on the uphill treadmill, and also strengthening muscles following strengthening exercise during treatment sessions. Therefore, all subscales in this group showed a significant increase.
Regarding the changes in the subscale of sport and recreation functions that became significant in the intervention group after 20 days, the patients were not sure of their knee improvement immediately after completing their treatment sessions and thought that jumping and other physical activities would return the disease symptoms; so, they avoided these movements. But, after 20 days and given the persistent improvement in the pain and symptom subscales in this group, they believed that they were able to perform these movements, and the previous symptoms of the disease would not return.
According to the findings, adding walking on the uphill surface to the physiotherapy treatment program of patients with knee osteoarthritis has a significant effect on reducing their disability and its persistency. Therefore, it is suggested that physiotherapists use walking on the uphill treadmill along with a physiotherapy program to promote the results of rehabilitation programs for patients with knee osteoarthritis. Considering that this study was conducted on patients with grade 2 or 3 knee joint osteoarthritis on the scale of Kellgren and Lawrence, it is suggested that further research be conducted on patients with a higher degree of osteoarthritis. Also, if possible, the study will be conducted for a longer follow-up period.
Ethical Considerations
Compliance with ethical guidelines
The Research Ethics Committee of the University of Social Welfare and Rehabilitation Sciences (approval number: IR.USWR.REC.1396.183) approved this study. We informed the participants about the study procedure, and they signed the informed consent form.
Funding
This paper was extracted from the MSc. thesis of the first author, Parisa Sedaghatnezhad, in the Department of Physiotherapy, University of Social Welfare and Rehabilitation Sciences.
Authors' contributions
All authors contributed in prepairing this article.
Conflict of interest
The authors declared no conflict of interest.
References
Full-Text: (4799 Views)
1. Introduction
Osteoarthritis is a degenerative disease that destroys joint surfaces [1]. The most common joints affected by this disease are knees, hips, hands, and spines [2]. The knee joint osteoarthritis is the most common osteoarthritis of peripheral joints in Iran [3]. It affects not only articular cartilage but also joint capsules, meniscus, ligaments, and muscles around the joint [4, 5]. The prevalence of osteoarthritis increases with age and is more prevalent in females. Besides, obesity or heavy physical activities are also a risk for knee osteoarthritis [6]. The most common symptoms of this disease are chronic pain and morning stiffness, which decrease the functional ability of the individual [7]. Painkillers and anti-inflammatory drugs, physiotherapy, applying orthosis, weight loss, and intra-articular injection are some remedies of these symptoms. In severe osteoarthritis, the physician suggests operation with many complications and costs [8]. This disease imposes a lot of costs on society and the individual.
In 2016, the results of a study had shown that in Iran, $360 were spent annually for each person suffering from knee osteoarthritis for visiting physicians, performing laboratory tests, imaging, and taking a drug. In addition, indirect costs arise from the absence of paid work, the adaptation of home, and the purchase of assistive devices [9]. Therefore, because of the high prevalence of osteoarthritis, its effect on individual function, the high cost of disease, and complications in surgical procedures, it is important to find a non-invasive method for treating these patients.
In the chronic osteoarthritis, because of the pain, the individuals keep their knees slightly flexed during rest and activity [10]. Bending the knee increases the stiffness of the posterior joint muscles and connective tissues and causes flexion contracture in the knee [11]. The complications of flexion contracture of the knee are the displacement of the center of knee joint pressure to the posterior, an increase in the flexor moment arm length, and finally, an increase at this moment [12]. As a result, the quadriceps muscle works intensively to overcome this moment, which increases the compressive force on the patellofemoral joint and degrades the joint [11]. Also, when the knee suffers from flexor shortness, the activity of the gastrocnemius and soleus muscles, which are the knee flexor, increases and the stiffness of these muscles increases, too [11]. Therefore, the ankle dorsiflexion is limited, leads to excessive subtalar joint pronation, tibial internal rotation, femoral internal rotation, and increases in the Q-angle [13].
Another change in the gait of people suffering from knee osteoarthritis is an increase in the knee adduction moment. The increase is due to the higher prevalence of osteoarthritis in the internal compartment of the tibiofemoral joint than in the external compartment. It reduces joint spacing in the internal side and displaces the ground reaction force vector to this direction, resulting in the varus deformity of the knee [14]. This process continues as a cycle so that an increase at the adduction moment intensifies joint degradation and, in turn, results in a further reduction in the knee joint space in the internal side of the knee and an increase in the adduction moment [15].
Uphill walking is a functional stretching method of the posterior knee joint muscles that correct flexor shortness and restores the knee joint center of pressure to the anterior. It also reduces the activity of the quadriceps muscle and the compression force on the patellofemoral joint, which reduces knee pain. Other advantages of walking on the upward surface are improving the limited plantar flexion of the ankle, reducing the pronation of subtalar joint, reducing the internal tibial and femoral rotation, and ultimately reducing knee joint degeneration [16]. Studies have shown that walking on the upward surface reduces the internal knee extension moment (equivalent to an external knee flexion moment or in short, knee flexion moment) and the adduction moment of the knee joint, lower extremities joints loading, the tibiofemoral joint compression, the knee varus angle. It also increases the activity of extensor muscles of the hip, knee, and ankle [17-20].
The mentioned studies are performed on healthy people, and according to the studies, the effect of uphill walking is not investigated in patients suffering from knee osteoarthritis. Therefore, this study aims at comparing the effect of routine physiotherapy with and without uphill walking on the disability of patients suffering from knee osteoarthritis. The study question is, “does uphill walking decrease the disability of patients with knee osteoarthritis?”
2. Materials and Methods
The present study, with the registration number of IRCT20171115034920N1, is a part of a clinical trial registered at the Iranian Clinical Trial Center. This study was performed on 30 patients aged 40 to 65 years (25 females and 5 males) with grade 2 or 3 osteoarthritis of the knee on the “Kellgren and Lawrence” scale, who were referred to a physiotherapy clinic in Tehran. Therefore, the researcher used the non-probability and convenience sampling method. Because of the lack of a similar previous study, given α=0.05, β=0.2, and mean difference of 2.4 cm based on a visual analog scale (VAS) parameter in a previous orthotic study on the knee osteoarthritis patients by Rodrigues et al. a sample size of 30 patients was estimated for both groups [21]. At the end of the study, to test sample sufficiency, the power of the test was above 90%.
The inclusion criteria of the study included developing knee osteoarthritis according to the American College of Rheumatology criteria, being classified in grade 2 or 3 according to the Kellgren and Lawrence classification scale, being 40 to 65 years old, having a body mass index (BMI) less than 30 kg/m2, having a minimum pain intensity of 30 mm on the VAS during one week before entering the study, having at least 2 degrees limitation in the knee extension, and experiencing gradual onset of the symptoms of the disease [22-28]. The patients with knee joint physiotherapy six months or intra-articular injection of the knees three months before entering the study, those unable to walk without assistive devices, and those with the history of injury to knee ligaments, patella dislocation, bursitis, systemic arthritis, knee operation, heel spur, or lumbar disc problem were excluded from the study [11, 24, 29, 30, 31].
The Persian version of the Knee injury and Osteoarthritis Outcome Score (KOOS) questionnaire was used to assess the disability of the patients. This is a valid and reliable questionnaire for evaluating the results of knee joint treatments in Iranian patients with knee joint disorder [32]. The questionnaire contains 42 items categorized into five subscales, including subscales of symptoms, pain, the activity of daily living, sport and recreation functions, and quality of life. There are five options for each question with answers scoring from zero to four points. The score of each subscale is calculated as a percentage; zero indicates the maximum problem, and 100 indicates no problem. There is no overall score in this questionnaire. The participants completed the questionnaire three times; at the beginning of the study, after ten sessions of the treatment, and also after 20 days of completion of the treatment.
At first, the volunteers with knee osteoarthritis, who were referred to the physiotherapy clinic for treating this disease, were assessed in terms of inclusion and exclusion criteria. The knee radiographs were examined by an orthopedic specialist, and those with grade 2 or 3 knee osteoarthritis based on the Kellgren and Lawrence scale (that is, their knee joint space was narrowed, osteophyte was grown around the joint, and sclerosis was low if any) were allowed to participate in the study. The height and weight of individuals were also measured, and their BMI was calculated. In this study, a BMI of less than 30 kg/m2 was desirable. Afterward, the patients were asked to complete the background information questionnaire to provide information on age, the history of physiotherapy, intra-articular injection of the knee, other illnesses, injury, medications, and minimum pain intensity on the VAS one week before the study.
Then, the patients were asked to complete the KOOS questionnaire. They were also asked to avoid activities imposing a lot of load on the knee joint during the study, or not to start a new treatment for the knee problem. The patients were randomly divided into control and intervention groups with 15 patients in each group based on a simple random assignment method. Initially, randomization was done for the assignment of even numbers to the control or the intervention group, and the result was the assignment of this set of numbers to the intervention group. Then, some numbers were assigned in the order of the entry of the subjects to the study so that the first person received number one. Since this number was odd, that person entered the control group, and the process continued for all 30 participants. The main researcher selected and grouped the samples. Therefore, the patients of each group were unaware of the presence of the other group.
Both the control and intervention groups underwent ten sessions of physiotherapy for knee osteoarthritis, which were done in the following way:
Firstly, an ultrasound (NOVIN-210B) with a frequency of 1MHz and an intensity of 1W/cm2 was used continuously for 6 minutes (three minutes for the anterior and three minutes for the posterior part of the knee joint). It was followed by conventional Transcutaneous Electrical Nerve Stimulation (TENS), (NOVIN-620F: frequency =100 Hz, duration =50 μs) to the extent that the patient felt it completely and in comfortable manner with 4 pads on the superior, inferior, medial, and lateral of the patella (cross mode) along with two hot packs, one on the anterior and the other on the posterior of the knee for 20 minutes [33]. Similar exercises were assigned to the patients to strengthen the quadriceps muscles, the hip abductor muscles, and triceps surae, including quadriceps setting in supine, hip abduction in side-lying, and heel raise on two legs in standing position. Each exercise was performed in two sets; ten repetitions in each set and five repetitions were added each session to eventually reach 30 repetitions.
After completing the physiotherapy session, the control group left the clinic. However, the subjects in the intervention group walked on a treadmill with an 8-degree slope (ascending) in every ten sessions with the following procedure. To familiarize the intervention group with uphill walking, the subjects in the intervention group were allowed to walk on the treadmill with +8-degree slope at a speed of 1.1 m/s for two minutes at the first session. Subsequently, when the patients were prepared to walk on the treadmill, they first walked on a treadmill for two minutes with a 0-degree slope at a speed of 1.1 m/s for warm-up; then, the slope increased to 8 degrees. The patients in the intervention group were asked to walk on a treadmill for 15 minutes, twice each session, once before starting physiotherapy and once after that. The patients walked on the treadmill without the shoe, and they were not allowed to take the treadmill’s handles.
Determining the treadmill slope was based on the studies of Haggerty et al. and Lange et al. who recommended a slope of 10% to 15% (5.74 to 9 degrees) in knee rehabilitation [16, 34]. Determining the treadmill speed was also based on the results of a study by Zeni et al. who showed that the mean speed selected by patients with knee osteoarthritis was 1.13 (0.9-1.4) m/s [35].
The KOOS questionnaire was completed once after the completion of ten sessions of physiotherapy and once 20 days after the completion of the treatment sessions. SPSS V. 22 was used to analyze the data. Mean±SD and percentage were reported as descriptive statistics. The Shapiro-Wilk test was used to examine the data distribution. Then the normally distributed variables were compared, using the independent t-test and non-normally distributed variables by Mann-Whitney U test between groups at baseline. The repeated measures analysis of variance (ANOVA) was used to examine the effect of treatment on KOOS subscales. The within-group factor of this analysis was time (pre-test, post-test, and follow-up), and the between-group factor was the group (control and intervention groups). If the time by group interaction were significant, Bonferroni posthoc test would be used and within-group and between-group changes would be reported. If the interaction effect were not significant, the significance of the main effects of time and group would be discussed. If any of the main effects were significant, ANOVA would be used to determine within-group changes. If the main effect of the group were significant, then, ANOVA would be used to examine the changes.
The significance level, the test statistics, and the Effect Size (ES) of the tests were reported in the text, and the mean difference between the groups or within each group, as well as the 95% confidence interval of the mean difference, was reported in the tables. To measure the effect size, Cohen’s d was used. If Cohen’s d is 0.2 to 0.4, it indicates a low effect, 0.5 to 0.7 indicates a moderate effect, and above 0.8 indicates a high effect. The α value was set at 0.05.
3. Results
A total of 30 patients with grade 2 or 3 knee osteoarthritis participated in this study and were randomly divided into control and intervention groups, with 15 patients in each group. The mean±SD age of the control group was 59.6±7.43 and the intervention group was 53.8±7.43 years, respectively. All 30 participants completed the study. Table 1 presents the demographic characteristics of the samples based on the groups. According to Table 1 , there was no statistically significant difference between the two groups in terms of the demographic characteristics (P<0.05).
Osteoarthritis is a degenerative disease that destroys joint surfaces [1]. The most common joints affected by this disease are knees, hips, hands, and spines [2]. The knee joint osteoarthritis is the most common osteoarthritis of peripheral joints in Iran [3]. It affects not only articular cartilage but also joint capsules, meniscus, ligaments, and muscles around the joint [4, 5]. The prevalence of osteoarthritis increases with age and is more prevalent in females. Besides, obesity or heavy physical activities are also a risk for knee osteoarthritis [6]. The most common symptoms of this disease are chronic pain and morning stiffness, which decrease the functional ability of the individual [7]. Painkillers and anti-inflammatory drugs, physiotherapy, applying orthosis, weight loss, and intra-articular injection are some remedies of these symptoms. In severe osteoarthritis, the physician suggests operation with many complications and costs [8]. This disease imposes a lot of costs on society and the individual.
In 2016, the results of a study had shown that in Iran, $360 were spent annually for each person suffering from knee osteoarthritis for visiting physicians, performing laboratory tests, imaging, and taking a drug. In addition, indirect costs arise from the absence of paid work, the adaptation of home, and the purchase of assistive devices [9]. Therefore, because of the high prevalence of osteoarthritis, its effect on individual function, the high cost of disease, and complications in surgical procedures, it is important to find a non-invasive method for treating these patients.
In the chronic osteoarthritis, because of the pain, the individuals keep their knees slightly flexed during rest and activity [10]. Bending the knee increases the stiffness of the posterior joint muscles and connective tissues and causes flexion contracture in the knee [11]. The complications of flexion contracture of the knee are the displacement of the center of knee joint pressure to the posterior, an increase in the flexor moment arm length, and finally, an increase at this moment [12]. As a result, the quadriceps muscle works intensively to overcome this moment, which increases the compressive force on the patellofemoral joint and degrades the joint [11]. Also, when the knee suffers from flexor shortness, the activity of the gastrocnemius and soleus muscles, which are the knee flexor, increases and the stiffness of these muscles increases, too [11]. Therefore, the ankle dorsiflexion is limited, leads to excessive subtalar joint pronation, tibial internal rotation, femoral internal rotation, and increases in the Q-angle [13].
Another change in the gait of people suffering from knee osteoarthritis is an increase in the knee adduction moment. The increase is due to the higher prevalence of osteoarthritis in the internal compartment of the tibiofemoral joint than in the external compartment. It reduces joint spacing in the internal side and displaces the ground reaction force vector to this direction, resulting in the varus deformity of the knee [14]. This process continues as a cycle so that an increase at the adduction moment intensifies joint degradation and, in turn, results in a further reduction in the knee joint space in the internal side of the knee and an increase in the adduction moment [15].
Uphill walking is a functional stretching method of the posterior knee joint muscles that correct flexor shortness and restores the knee joint center of pressure to the anterior. It also reduces the activity of the quadriceps muscle and the compression force on the patellofemoral joint, which reduces knee pain. Other advantages of walking on the upward surface are improving the limited plantar flexion of the ankle, reducing the pronation of subtalar joint, reducing the internal tibial and femoral rotation, and ultimately reducing knee joint degeneration [16]. Studies have shown that walking on the upward surface reduces the internal knee extension moment (equivalent to an external knee flexion moment or in short, knee flexion moment) and the adduction moment of the knee joint, lower extremities joints loading, the tibiofemoral joint compression, the knee varus angle. It also increases the activity of extensor muscles of the hip, knee, and ankle [17-20].
The mentioned studies are performed on healthy people, and according to the studies, the effect of uphill walking is not investigated in patients suffering from knee osteoarthritis. Therefore, this study aims at comparing the effect of routine physiotherapy with and without uphill walking on the disability of patients suffering from knee osteoarthritis. The study question is, “does uphill walking decrease the disability of patients with knee osteoarthritis?”
2. Materials and Methods
The present study, with the registration number of IRCT20171115034920N1, is a part of a clinical trial registered at the Iranian Clinical Trial Center. This study was performed on 30 patients aged 40 to 65 years (25 females and 5 males) with grade 2 or 3 osteoarthritis of the knee on the “Kellgren and Lawrence” scale, who were referred to a physiotherapy clinic in Tehran. Therefore, the researcher used the non-probability and convenience sampling method. Because of the lack of a similar previous study, given α=0.05, β=0.2, and mean difference of 2.4 cm based on a visual analog scale (VAS) parameter in a previous orthotic study on the knee osteoarthritis patients by Rodrigues et al. a sample size of 30 patients was estimated for both groups [21]. At the end of the study, to test sample sufficiency, the power of the test was above 90%.
The inclusion criteria of the study included developing knee osteoarthritis according to the American College of Rheumatology criteria, being classified in grade 2 or 3 according to the Kellgren and Lawrence classification scale, being 40 to 65 years old, having a body mass index (BMI) less than 30 kg/m2, having a minimum pain intensity of 30 mm on the VAS during one week before entering the study, having at least 2 degrees limitation in the knee extension, and experiencing gradual onset of the symptoms of the disease [22-28]. The patients with knee joint physiotherapy six months or intra-articular injection of the knees three months before entering the study, those unable to walk without assistive devices, and those with the history of injury to knee ligaments, patella dislocation, bursitis, systemic arthritis, knee operation, heel spur, or lumbar disc problem were excluded from the study [11, 24, 29, 30, 31].
The Persian version of the Knee injury and Osteoarthritis Outcome Score (KOOS) questionnaire was used to assess the disability of the patients. This is a valid and reliable questionnaire for evaluating the results of knee joint treatments in Iranian patients with knee joint disorder [32]. The questionnaire contains 42 items categorized into five subscales, including subscales of symptoms, pain, the activity of daily living, sport and recreation functions, and quality of life. There are five options for each question with answers scoring from zero to four points. The score of each subscale is calculated as a percentage; zero indicates the maximum problem, and 100 indicates no problem. There is no overall score in this questionnaire. The participants completed the questionnaire three times; at the beginning of the study, after ten sessions of the treatment, and also after 20 days of completion of the treatment.
At first, the volunteers with knee osteoarthritis, who were referred to the physiotherapy clinic for treating this disease, were assessed in terms of inclusion and exclusion criteria. The knee radiographs were examined by an orthopedic specialist, and those with grade 2 or 3 knee osteoarthritis based on the Kellgren and Lawrence scale (that is, their knee joint space was narrowed, osteophyte was grown around the joint, and sclerosis was low if any) were allowed to participate in the study. The height and weight of individuals were also measured, and their BMI was calculated. In this study, a BMI of less than 30 kg/m2 was desirable. Afterward, the patients were asked to complete the background information questionnaire to provide information on age, the history of physiotherapy, intra-articular injection of the knee, other illnesses, injury, medications, and minimum pain intensity on the VAS one week before the study.
Then, the patients were asked to complete the KOOS questionnaire. They were also asked to avoid activities imposing a lot of load on the knee joint during the study, or not to start a new treatment for the knee problem. The patients were randomly divided into control and intervention groups with 15 patients in each group based on a simple random assignment method. Initially, randomization was done for the assignment of even numbers to the control or the intervention group, and the result was the assignment of this set of numbers to the intervention group. Then, some numbers were assigned in the order of the entry of the subjects to the study so that the first person received number one. Since this number was odd, that person entered the control group, and the process continued for all 30 participants. The main researcher selected and grouped the samples. Therefore, the patients of each group were unaware of the presence of the other group.
Both the control and intervention groups underwent ten sessions of physiotherapy for knee osteoarthritis, which were done in the following way:
Firstly, an ultrasound (NOVIN-210B) with a frequency of 1MHz and an intensity of 1W/cm2 was used continuously for 6 minutes (three minutes for the anterior and three minutes for the posterior part of the knee joint). It was followed by conventional Transcutaneous Electrical Nerve Stimulation (TENS), (NOVIN-620F: frequency =100 Hz, duration =50 μs) to the extent that the patient felt it completely and in comfortable manner with 4 pads on the superior, inferior, medial, and lateral of the patella (cross mode) along with two hot packs, one on the anterior and the other on the posterior of the knee for 20 minutes [33]. Similar exercises were assigned to the patients to strengthen the quadriceps muscles, the hip abductor muscles, and triceps surae, including quadriceps setting in supine, hip abduction in side-lying, and heel raise on two legs in standing position. Each exercise was performed in two sets; ten repetitions in each set and five repetitions were added each session to eventually reach 30 repetitions.
After completing the physiotherapy session, the control group left the clinic. However, the subjects in the intervention group walked on a treadmill with an 8-degree slope (ascending) in every ten sessions with the following procedure. To familiarize the intervention group with uphill walking, the subjects in the intervention group were allowed to walk on the treadmill with +8-degree slope at a speed of 1.1 m/s for two minutes at the first session. Subsequently, when the patients were prepared to walk on the treadmill, they first walked on a treadmill for two minutes with a 0-degree slope at a speed of 1.1 m/s for warm-up; then, the slope increased to 8 degrees. The patients in the intervention group were asked to walk on a treadmill for 15 minutes, twice each session, once before starting physiotherapy and once after that. The patients walked on the treadmill without the shoe, and they were not allowed to take the treadmill’s handles.
Determining the treadmill slope was based on the studies of Haggerty et al. and Lange et al. who recommended a slope of 10% to 15% (5.74 to 9 degrees) in knee rehabilitation [16, 34]. Determining the treadmill speed was also based on the results of a study by Zeni et al. who showed that the mean speed selected by patients with knee osteoarthritis was 1.13 (0.9-1.4) m/s [35].
The KOOS questionnaire was completed once after the completion of ten sessions of physiotherapy and once 20 days after the completion of the treatment sessions. SPSS V. 22 was used to analyze the data. Mean±SD and percentage were reported as descriptive statistics. The Shapiro-Wilk test was used to examine the data distribution. Then the normally distributed variables were compared, using the independent t-test and non-normally distributed variables by Mann-Whitney U test between groups at baseline. The repeated measures analysis of variance (ANOVA) was used to examine the effect of treatment on KOOS subscales. The within-group factor of this analysis was time (pre-test, post-test, and follow-up), and the between-group factor was the group (control and intervention groups). If the time by group interaction were significant, Bonferroni posthoc test would be used and within-group and between-group changes would be reported. If the interaction effect were not significant, the significance of the main effects of time and group would be discussed. If any of the main effects were significant, ANOVA would be used to determine within-group changes. If the main effect of the group were significant, then, ANOVA would be used to examine the changes.
The significance level, the test statistics, and the Effect Size (ES) of the tests were reported in the text, and the mean difference between the groups or within each group, as well as the 95% confidence interval of the mean difference, was reported in the tables. To measure the effect size, Cohen’s d was used. If Cohen’s d is 0.2 to 0.4, it indicates a low effect, 0.5 to 0.7 indicates a moderate effect, and above 0.8 indicates a high effect. The α value was set at 0.05.
3. Results
A total of 30 patients with grade 2 or 3 knee osteoarthritis participated in this study and were randomly divided into control and intervention groups, with 15 patients in each group. The mean±SD age of the control group was 59.6±7.43 and the intervention group was 53.8±7.43 years, respectively. All 30 participants completed the study. Table 1 presents the demographic characteristics of the samples based on the groups. According to Table 1 , there was no statistically significant difference between the two groups in terms of the demographic characteristics (P<0.05).
Table 2 presents the mean±SD of the subscales of the KOOS questionnaire at three assessment times; pre-test (before the treatment), post-test (after ten sessions of treatment), and follow-up (20 days after the treatment completion). According to the data of this table in both control and intervention groups, the lowest score recorded in all subscales was in the pre-test stage. All mean scores of subscales in both groups were similar in the pre-test (P>0.05) except for the sport and recreation activities (P=0.02) (Table 3). Therefore, to prevent the effect of the difference between the two groups in terms of this subscale on the test results, the changes in this difference were studied during the test stages.
Symptom Subscale
The results of the repeated measures ANOVA show a significant interaction effect of time by the group on the symptom subscale (F=4.14, P=0.03, ES=2.22), i.e. the changing procedure in this subscale is significant between the two groups during the study. According to Figure 1, the mean score of the symptom subscale in the intervention group was less than that of the control group in the pre-test, and the mean scores of the two groups were approximately the same in the post-test. Therefore, an increase in the score of this subscale in the intervention group was more than that of the control group. Also, in the follow-up and pre-test stages, the mean scores of the control group were almost the same, but in the intervention group, the increase in the scores continued from post-test to the follow-up stage. The results of the Bonferroni posthoc test showed that in the control group, the changes in this subscale were not significant in the post-test (P=0.09) and follow-up (P=0.94) compared to the pre-test. However, in the intervention group, the changes in the symptom subscale in both post-test (T=3.34, P=0.01, ES=0.86) and follow-up (T=4.06, P=0.003, ES=0.95) were significant compared to the pre-test. It means that only the treatment program of the intervention group caused a significant change in the scores of the symptom subscale and the persistency of change. The mean score of this subscale between the two groups was not significantly different in the post-test (P=0.91) and follow-up (P=0.11). Tables 3 and 4 present the results of within-group and between-group pairwise comparisons, respectively.
Pain Subscale
The results of repeated measures ANOVA show the significant interaction effect of time by the group on pain subscale (F=3.3, P=0.04, ES=0.86), i.e. the changing procedure of this subscale is significant between the two groups during the study. According to Figure 1, the mean score of the pain subscale in the intervention group was less than that of the control group in the pre-test and more in the post-test. Therefore, the increase in the score of this subscale in the intervention group is more than that of the control group. Also, in the follow-up and pre-test stages, the mean scores of the control group were almost the same, but it was almost constant in the intervention group from post-test to follow-up. The results of the Bonferroni posthoc test showed that in the control group, changes in this subscale were not significant in the post-test (P=0.18) and follow-up (P=0.5) compared to the pre-test. In the intervention group, changes in the pain subscale in both post-test (T=5.98, P<0.001, ES=1.02) and follow-up (T=4.39, P=0.001, ES=1.01) were significant compared to the pre-test. That is, only the treatment program in the intervention group has significantly changed the score of pain subscale and the persistency of change. The mean score of this subscale between the two groups was not significantly different in the post-test (P=0.58) and follow-up (P=0.34).
Activities of daily living subscale
The results of repeated measures ANOVA show that the interaction effect of time by the group has a significant effect on the subscale of activities of daily living (F=3.44, P=0.04, ES=0.82). According to Figure 1, the mean score of this subscale in the pre-test in the intervention group was slightly lower than that of the control group and was more than the control group in the post-test. Therefore, the gradient of an increase in the mean score of this subscale in the intervention group is greater than that of the control group. The results of the Bonferroni posthoc test showed that in the control group, changes in this subscale in the post-test (T=3.7, P=0.01, ES=0.61) and follow-up (T=4.33, P=0.001, ES=0.74) were significant compared to the pre-test. Also, in the intervention group, the changes in the subscales of activities of daily living in both post-test (T=5.38, P<0.001, ES=0.9) and follow-up (T=6.71, P<0.001, ES=0.94) were significant compared to the pre-test. Overall, the treatment program of both groups has significantly changed the scores of activities of daily living subscale and the persistency of this change. The mean score of this subscale between the two groups was not significantly different in the post-test (P=0.31) and follow-up (P=0.33).
Sport and recreation functions
The results of repeated measures ANOVA show that the interaction effect of time by the group is significant for the subscales of sport and recreation functions (F=3.66, P=0.03, ES=1.06). As shown in Figure 1, in all stages of the measurement, i.e. pre-test (T=2.36, P=0.02, ES=0.86), post-test (T=2.49, P=0.02, ES=1.11), and follow-up (T=4.5, P<0.001, ES=1.64), the mean score of the intervention group is greater than that of the control group. Considering the significant difference in the pre-test between the two groups, the changes in this difference were studied in different stages. The changes in this difference were not significant in the post-test compared to the pre-test (P=0.64), but in follow-up (T=2.62, P=0.02, ES=0.65), these changes were significant compared to the pre-test. Therefore, the treatment program of the intervention group increased the subscales of sport and recreation functions after 20 days of competition of the intervention.
Quality of life Subscale
Figure 1 shows similar changes in the quality of life subscale in response to treatment over time in the two groups; the time by group interaction on this subscale was not significant (P=0.47). The results of repeated measures ANOVA showed a significant effect of time on the quality of life subscale (F=16.53, P<0.001, ES=0.48), meaning that during the study, the score of this subscale has changed. The results of ANOVA showed that in the control group, changes in this subscale in the post-test (T=2.78, P=0.04, ES=0.6) and follow-up (T=3.52, P=0.02, ES=0.67) were significant compared to the pre-test. In the intervention group, the changes in the quality of life subscale in both post-test (T=3.33, P=0.005, ES=0.81) and follow-up 4.31, P<0.001, ES=1.06) were significant compared to the pre-test. Overall, the treatment program of both groups has significantly changed the scores of quality of life subscale and the persistency of this change. The main effect of the group in this subscale was not significant (P=0.63), meaning that the results of the treatment were the same in both groups.
4. Discussion
Disability is not only a consequence of a disease or injury but also a factor affecting people’s communication with the environment. Disability is one of the major consequences of lower extremities osteoarthritis, and since knee osteoarthritis is very common, its disability has a significant impact on the individual and the community. Considering that one of the goals of treatment in patients suffering from knee osteoarthritis is to minimize their disability, the present study investigated the effect of adding walking on the uphill treadmill to the routine physiotherapy program of patients with knee osteoarthritis on the disability of these patients.
The results of this study showed that adding uphill treadmill walking to the routine physiotherapy program would improve all subscales of the KOOS questionnaire and, thus, reduce the disability of people with knee osteoarthritis so that the recovery would be persistent up to 20 days. However, physiotherapy treatment in the control group did not improve pain, symptoms, and sport and recreation functions subscales.
The findings of this study about the effect of physiotherapy and exercise program on the disability of patients suffering from knee osteoarthritis are in line with the results of the studies by Ardakani, Miri, Esfandiari et al. and Ahadi et al. indicating the the significant improvement of subscales of KOOS questionnaire following stretching and strengthening exercises of hamstring and quadriceps muscles, adding dry needling to the physiotherapy program, and using orthoses with lateral wedge and physiotherapy, respectively, in patients with patellofemoral pain syndrome or knee osteoarthritis [36-39].
The results of this study indicate that the symptom subscale of KOOS questionnaire changes following the physiotherapy alone was not significant. The results also confirm Miri’s study that observed an insignificant change in the symptom subscale of the KOOS questionnaire after the usual physiotherapy treatment in patients with patellofemoral pain syndrome [37].
Patients with knee osteoarthritis tend to avoid physical activity to relieve pain. In the short term, avoiding physical activity helps patients to relieve pain, but in the long term, the reduction in activity levels leads to muscle weakness. Joint stability and its ability to withstand the applied loads reduce because of the muscle weakness, which ultimately leads to the patient’s disability and the avoidance of physical activities [40]. Another reason for disability is the reduction of a joint range of motion caused by the shortness of the joint capsule, muscles, and muscle spasm [41, 42]. Quadriceps muscle weakness in patients with knee pain is also associated with disability [43]. Evidence suggests that muscle weakness is associated with functional impairment following the muscle-strengthening programs, improving inability and reducing disability occurred [43, 44]. Among the reasons mentioned for disability (pain, limitation of range of motion, and muscle weakness), just muscle weakness factor has improved in the control group by strengthening exercise and has improved the subscales of activity of daily living and quality of life of this group of participants. However, in the intervention group, the three factors have improved, including a decrease in knee pain (increasing the score of the pain subscale), an increase in the limited range of motion of the knee joint because of stretching of the soft tissue of the posterior joint while walking on the uphill treadmill, and also strengthening muscles following strengthening exercise during treatment sessions. Therefore, all subscales in this group showed a significant increase.
Regarding the changes in the subscale of sport and recreation functions that became significant in the intervention group after 20 days, the patients were not sure of their knee improvement immediately after completing their treatment sessions and thought that jumping and other physical activities would return the disease symptoms; so, they avoided these movements. But, after 20 days and given the persistent improvement in the pain and symptom subscales in this group, they believed that they were able to perform these movements, and the previous symptoms of the disease would not return.
According to the findings, adding walking on the uphill surface to the physiotherapy treatment program of patients with knee osteoarthritis has a significant effect on reducing their disability and its persistency. Therefore, it is suggested that physiotherapists use walking on the uphill treadmill along with a physiotherapy program to promote the results of rehabilitation programs for patients with knee osteoarthritis. Considering that this study was conducted on patients with grade 2 or 3 knee joint osteoarthritis on the scale of Kellgren and Lawrence, it is suggested that further research be conducted on patients with a higher degree of osteoarthritis. Also, if possible, the study will be conducted for a longer follow-up period.
Ethical Considerations
Compliance with ethical guidelines
The Research Ethics Committee of the University of Social Welfare and Rehabilitation Sciences (approval number: IR.USWR.REC.1396.183) approved this study. We informed the participants about the study procedure, and they signed the informed consent form.
Funding
This paper was extracted from the MSc. thesis of the first author, Parisa Sedaghatnezhad, in the Department of Physiotherapy, University of Social Welfare and Rehabilitation Sciences.
Authors' contributions
All authors contributed in prepairing this article.
Conflict of interest
The authors declared no conflict of interest.
References
- Loeser RF, Goldring SR, Scanzello CR, Goldring MB. Osteoarthritis: A disease of the joint as an organ. Arthritis & Rheumatology. 2012; 64(6):1697-707. [DOI:10.1002/art.34453] [PMID] [PMCID]
- Palazzo C, Nguyen C, Lefevre-Colau M-M, Rannou F, Poiraudeau S. Risk factors and burden of osteoarthritis. Annals of Physical and Rehabilitation Medicine. 2016; 59(3):134-8. [DOI:10.1016/j.rehab.2016.01.006] [PMID]
- Mousavi SME. [The identification of influential factors in knee osteoarthritis and its prevalence among referals to orthopedic clinics in Tehran (Persian)]. Archives of Rehabilitation. 2001; 2(1):14-20.
- Heidari B. Knee osteoarthritis prevalence, risk factors, pathogenesis and features: Part I. Caspian Journal of Internal Medicine. 2011; 2(2):205-12.
- Felson DT. Osteoarthritis of the knee. The New England Journal of Medicine. 2006; 354(8):841-8. [DOI:10.1056/NEJMcp051726] [PMID]
- Wittenauer R, Smith L, Aden K. Background paper 6.12 osteoarthritis. World Health Organisation. 2013.
- Zhang W, Doherty M, Peat G, Bierma-Zeinstra SM, Arden N, Bresnihan B, et al. EULAR evidence based recommendations for the diagnosis of knee osteoarthritis. Annals of the Rheumatic Diseases. 2009; 63(3):483-9. [DOI:10.1136/ard.2009.113100] [PMID]
- Zhang W, Moskowitz R, Nuki G, Abramson S, Altman R, Arden N, et al. OARSI recommendations for the management of hip and knee osteoarthritis, part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis and Cartilage. 2008; 16(2):137-62. [DOI:10.1016/j.joca.2007.12.013] [PMID]
- Mobini M, Mohammadpour RA, Tahmasbi B, Karimi T. Cost comparison of illness in patients with rheumatoid arthritis, osteoarthritis and fibromyalgia syndrome. Rheumatology Research. 2017; 2(2):65-70. [DOI:10.22631/rr.2017.69997.1020]
- Koh IJ, Chang CB, Kang YG, Seong SC, Kim TK. Incidence, predictors, and effects of residual flexion contracture on clinical outcomes of total knee arthroplasty. The Journal of Arthroplasty. 2013; 28(4):585-90. [DOI:10.1016/j.arth.2012.07.014] [PMID]
- Piva SR, Goodnite EA, Childs JD. Strength around the hip and flexibility of soft tissues in individuals with and without patellofemoral pain syndrome. The Journal of Orthopaedic and Sports Physical Therapy. 2005; 35(12):793-801. [DOI:10.2519/jospt.2005.35.12.793] [PMID]
- Elbaz A, Magram-Flohr I, Segal G, Mor A, Debi R, Kalichman L. Association between knee osteoarthritis and functional changes in ankle joint and achilles tendon. The Journal of Foot and Ankle Surgery. 2017; 56(2):238-41. [DOI:10.1053/j.jfas.2016.11.017] [PMID]
- Waryasz GR, McDermott AY. Patellofemoral Pain Syndrome (PFPS): A systematic review of anatomy and potential risk factors. Dynamic Medicine. 2008; 7(1):9. [DOI:10.1186/1476-5918-7-9] [PMID] [PMCID]
- Baliunas A, Hurwitz D, Ryals A, Karrar A, Case J, Block J, et al. Increased knee joint loads during walking are present in subjects with knee osteoarthritis. Osteoarthritis Cartilage. 2002; 10(7):573-9. [DOI:10.1053/joca.2002.0797] [PMID]
- Jones RK, Chapman GJ, Findlow AH, Forsythe L, Parkes MJ, Sultan J, et al. A new approach to prevention of knee osteoarthritis: Reducing medial load in the contralateral knee. The Journal of Rheumatology. 2013; 40(3):309-15. [DOI:10.3899/jrheum.120589] [PMID]
- Lange GW, Hintermeister RA, Schlegel T, Dillman CJ, Steadman JR. Electromyographic and kinematic analysis of graded treadmill walking and the implications for knee rehabilitation. The Journal of Orthopaedic and Sports Physical Therapy. 1996; 23(5):294-301. [DOI:10.2519/jospt.1996.23.5.294] [PMID]
- Ehlen KA, Reiser RF, Browning RC. Energetics and biomechanics of inclined treadmill walking in obese adults. Medicine and Science in Sports & Exercise. 2011; 43(7):1251-9. [DOI:10.1249/MSS.0b013e3182098a6c] [PMID]
- Haight DJ, Lerner ZF, Board WJ, Browning RC. A comparison of slow, uphill and fast, level walking on lower extremity biomechanics and tibiofemoral joint loading in obese and nonobese adults. Journal of Orthopaedic Research. 2014; 32(2):324-30. [DOI:10.1002/jor.22497] [PMID]
- Naderi S, Mohammadipour F, Amir Seyfaddini M. The effects of different walking inclinations on knee angle in the frontal plane of patients with varus malalignment. Physical Treatments Journal. 2014; 4(3):139-44.
- Franz JR, Kram R. The effects of grade and speed on leg muscle activations during walking. Gait Posture. 2012; 35(1):143-7. [DOI:10.1016/j.gaitpost.2011.08.025] [PMID] [PMCID]
- Rodrigues PT, Ferreira AF, Pereira RM, Bonfa E, Borba EF, Fuller R. Effectiveness of medial‐wedge insole treatment for valgus knee osteoarthritis. Arthritis Care & Research. 2008; 59(5):603-8. [DOI:10.1002/art.23560] [PMID]
- Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, et al. Development of criteria for the classification and reporting of osteoarthritis: Classification of osteoarthritis of the knee. Arthritis Rheum. 1986; 29(8):1039-49. [DOI:10.1002/art.1780290816] [PMID]
- Callaghan MJ, Parkes MJ, Felson DT. The effect of knee braces on quadriceps strength and inhibition in subjects with patellofemoral osteoarthritis. The Journal of Orthopaedic and Sports Physical Therapy. 2016; 46(1):19-25. [DOI:10.2519/jospt.2016.5093] [PMID]
- Anwer S, Alghadir A. Effect of isometric quadriceps exercise on muscle strength, pain, and function in patients with knee osteoarthritis: A randomized controlled study. Journal of Physical Therapy Science. 2014; 26(5):745-8. [DOI:10.1589/jpts.26.745] [PMID] [PMCID]
- Hamidi M, Samavati Sharif M, Aghayari A. [Comparison the severity of the knee osteoarthritis and its consequence in veteran endurance runners and non-athletes (Persian)]. Journal of Sport Medicine. 2014; 6(2):103-17.
- Barton CJ, Bonanno D, Levinger P, Menz HB. Foot and ankle characteristics in patellofemoral pain syndrome: A case control and reliability study. The Journal of Orthopaedic and Sports Physical Therapy. 2010; 40(5):286-96. [DOI:10.2519/jospt.2010.3227] [PMID]
- Feland JB, Myrer JW, Schulthies SS, Fellingham GW, Measom GW. The effect of duration of stretching of the hamstring muscle group for increasing range of motion in people aged 65 years or older. Physical Therapy. 2001; 81(5):1110-7.
- Rahimi M, Salavati M, Ebrahimi Takamjani E, Mohammadi L. [Evaluation of comparison of hamstring and rectus femoris muscles stiffness and peak torque between anterior knee pain patients and healthy subjects (Persian)]. Journal of Modern Rehabilitation. 2013; 7(1):21-8.
- Ng M, Leung MC, Poon D. The effects of electro-acupuncture and transcutaneous electrical nerve stimulation on patients with painful osteoarthritic knees: A randomized controlled trial with follow-up evaluation. The Journal of Alternative & Complementary Medicine. 2003; 9(5):641-9. [DOI:10.1089/107555303322524490] [PMID]
- Elbaz A, Magram-Flohr I, Segal G, Mor A, Debi R, Kalichman L. Association between knee osteoarthritis and functional changes in ankle joint and achilles tendon. The Journal of Foot and Ankle Surgery. 2017; 56(2):238-41. [DOI:10.1053/j.jfas.2016.11.017] [PMID]
- Ganiyu S, Bello UM. Comparison of the effects of acupuncture and acupuncture-like transcutaneous electrical nerve stimulation among adult Nigerian adult with osteoarthritis of the knee. Journal of Alternative, Complementary & Integrative Medicine. 2016; 2(009). [DOI:10.24966/ACIM-7562/100009]
- Saraei-Pour S, Salavati M, Akhbari B, Kazem-Nezhad A. [Translation and adaptation of knee injury and osteoarthritis outcome score (KOOS) into Persian and testing Persian version reliability among iranians with osteoarthritis (Persian)]. Archives of Rehabilitation. 2007; 8(1):42-6.
- Mahmoudi Aghdam S, Khademi Kalantari K, Akbarzadeh Baghban A, Rezaee M, Rahimi A, Sadat Naeimee S. [Effect of joint traction on functional improvement and quality of life in patients with severe knee osteoarthritis (Persian)]. The Scientific Journal of Rehabilitation Medicine. 2012; 1(2):1-6.
- Haggerty M, Dickin DC, Popp J, Wang H. The influence of incline walking on joint mechanics. Gait Posture. 2014; 39(4):1017-21. [DOI:10.1016/j.gaitpost.2013.12.027] [PMID]
- Zeni JA, Higginson JS. Differences in gait parameters between healthy subjects and persons with moderate and severe knee osteoarthritis: A result of altered walking speed? Clinical Biomechanics. 2009; 24(4):372-8. [DOI:10.1016/j.clinbiomech.2009.02.001] [PMID] [PMCID]
- Ardakani S. [Effects of two home programs of stretch and stretch-strength exercise in patients with patellofemoral pain syndrome (Persian)]. [Msc thesis] Isfahan: University of Isfahan; 2011.
- Miri Abyaneh H, Mosallnezhad Z. [Investigating the effect of add superficial dry needling to routine physiotherapy in patients with patellofemaral pain syndrome (Persian)]. [Msc . thesis] Tehran: University of Social Welfare and Rehabilitation Sciences; 2014.
- Esfandiari E, Kamyab M, Foroughi N, Yazdi HR. [The effect of lateral wedge insole with and without sub-talar strap on pain, function, and quality of life in medial knee osteoarthritis (Persian)]. Modern Rehabilitation. 2012; 6(1):17-25.
- Ahadi T, Saleki M, Razi M, Raeisi Gh, Forough B. [Comparison of physical modality and knee isometric exercise training on symptom of knee osteoarthritis (Persian)]. Journal of Gorgan University of Medical Sciences. 2011; 12(4):12-7.
- Steultjens M, Dekker J, Bijlsma J. Avoidance of activity and disability in patients with osteoarthritis of the knee: The mediating role of muscle strength. Arthritis and Rheumatism. 2002; 46(7):1784-8. [DOI:10.1002/art.10383] [PMID]
- Steultjens M, Dekker J, Van Baar M, Oostendorp R, Bijlsma J. Range of joint motion and disability in patients with osteoarthritis of the knee or hip. Rheumatology. 2000; 39(9):955-61. [DOI:10.1093/rheumatology/39.9.955] [PMID]
- Dekker J, Boot B, van der Woude LH, Bijlsma J. Pain and disability in osteoarthritis: A review of biobehavioral mechanisms. Journal of Behavioral Medicine. 1992; 15(2):189-214. [DOI:10.1007/BF00848325] [PMID]
- O’Reilly SC, Jones A, Muir KR, Doherty M. Quadriceps weakness in knee osteoarthritis: The effect on pain and disability. Annals of the Rheumatic Diseases. 1998; 57(10):588-94. [DOI:10.1136/ard.57.10.588] [PMID] [PMCID]
- Sanchez-Ramirez DC, van der Leeden M, van der Esch M, Roorda LD, Verschueren S, van Dieën J, et al. Increased knee muscle strength is associated with decreased activity limitations in established knee osteoarthritis: Two-year follow-up study in the Amsterdam osteoarthritis cohort. Journal of Rehabilitation Medicine. 2015; 47(7):647-54. [DOI:10.2340/16501977-1973] [PMID]
Type of Study: Research |
Subject:
General
Received: 2019/07/5 | Accepted: 2019/08/7 | Published: 2019/11/12
Received: 2019/07/5 | Accepted: 2019/08/7 | Published: 2019/11/12
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |