Tue, Jul 16, 2024
Volume 9, Issue 1 (Winter 2019)
PTJ 2019, 9(1): 47-58 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mousavi S H, Minoonejad H, Seidi F, Rajabi R. Comparing the Effect of 8-Week Corrective Exercises With Versus Without Myofascial Release on Correcting Forward Shoulder Deformity. PTJ 2019; 9 (1) :47-58
URL: http://ptj.uswr.ac.ir/article-1-379-en.html
URL: http://ptj.uswr.ac.ir/article-1-379-en.html
1- Department of Health and Sports Medicine, Faculty of Physical Education and Sport Sciences, University of Tehran, Tehran, Iran.
Full-Text [PDF 1261 kb]
(1975 Downloads)
| Abstract (HTML) (3084 Views)
4. Discussion
In this randomized controlled trial on 45 samples, 15 performed corrective exercises, and 15 received a combination of corrective exercises and MFR therapy for 8 weeks under the direct supervision of the researcher (three time per week, each session one hour). The results showed no significant difference between the two exercises groups in terms of SFP angle with the control group that received no intervention. In the group received the combinational intervention, SFP angle reduced by 6 degrees and the group received only corrective exercises reported a 4 degrees reduction in SFP angle.
Full-Text: (4677 Views)
1. Introduction
The proper physical condition requires the correct placement of the spines and joints so that the muscles and ligaments act naturally [1]. Adoption of inappropriate postures in life leads to muscle imbalance and postural changes [2]. The Forward Shoulder Posture (FSP) is one of the many postural deviations that accounts for 80% of shoulder deformities [3]. It is known as scapular protraction and elevation with a forward position of the shoulder, causing a funnel chest [4]. This deformity is probably due to the shortened and tight anterior muscles and the weakness and elongation of the posterior muscles of the shoulder girdle [5].
It seems that the weakness of the muscles holding the spine can weaken the static and dynamic postural balance [6]. Abnormal changes in balance and muscle strength (length-tension relationship) increase the motor recruitment time consequences (a couple) and movement disorder of the scapular joint for internal rotation. These changes also decrease the posterior tilt and the upward scapular rotation, which leads to FSP [7]. Based on many references, FSP will be diagnosed if the angle between the vertical line and the line linked C7 spinous process with the acromion process be more than 52 degrees [8-10].
Physiological complications of FSP vary from person to person in terms of prevalence and severity. The muscle imbalance caused by FSP can restrict chest expansion during respiration and result in hard breathing [9]. The anterior pectoral muscle stiffness because of long-term contraction leads to forward rotation of shoulder girdle, out of the anatomic plate, and besides limiting the range of motion of shoulder and arm joints, causes the narrowing of the dorsal neural tube and the pressure on the dorsal and suprascapular nerves, creating neurological symptoms [11]. Moreover, the subacromial space reduces, and the subject is susceptible to subacromial impingement syndrome [12].
Research has shown several ways to correct this deformity, including manual therapy, postural re-education, using taping and orthoses, and exercise therapy [13-15]. The goals of implementing all these methods, especially exercise therapy (corrective movements) for correcting FSP deformity is to improve the range of motion, increase the flexibility, increase the strength of the weakened muscles, and in general, eliminate muscle imbalance (establishing a balance between muscles involved in deformity).
Researchers have always sought to find combined corrective exercises for greater efficacy to correct FSP. For example, Morningstar proposed a rehabilitative procedure using chiropractic and spinal manipulative therapy to correct FSP [16]. Rahnema et al. in a study on examining the effect of 8-week regular corrective exercises on the spinal cord of female students, reported that these exercises were a safe and useful way to improve spine abnormalities and reduce future problems and discomforts [17]. In their study, muscle stretching and strength exercises were carried out as well as proprioceptive neuromuscular facilitation for better and faster performance through effective stimulation of receptors. In another study, Zandi et al. [18] by comparing three programs of corrective exercises, postural re-education, and their combination on FSP found out that the combination of corrective exercises with postural re-education had a significant effect on reducing the FSP angle.
Muscle shortness and connective tissue stiffness are common musculoskeletal problems which may be caused by various reasons such as illness, trauma, insufficient mobility, or scarring. Reduced soft tissue flexibility and movement limitation can lead to changes in motor patterns and musculoskeletal disorders [19]. Many of the methods used to maintain flexibility in the muscles emphasize the use of different stretching exercises [20]. Other methods that are commonly used to improve muscle flexibility include heat [20, 21], massage [22], proprioceptive neuromuscular facilitation [23], muscle energy techniques [24] and Myofascial Release (MFR) techniques [25].
MFR techniques are manual techniques used by health-care professionals or by the patient [called Self-Myofascial Release (SMR)] to influence the fascia. Although it is still unknown how these techniques work, their therapeutic effects have been clinically proven [25]. These techniques stretch the restricted fascia. A gentle pressure for 90-120 s in the restricted tissue increases its flexibility, and then the first release occurs. After that, the therapist takes the tissue to a new area and keeps it in hand. After several releases, the tissue becomes softer. The claimed effects for MFR techniques are similar to the effects of massage and soft-tissue mobilization techniques which include changing blood circulation, dilatation of the capillaries, stimulation of the nervous system, and changes in skin temperature and metabolism [26].
Several studies have shown that manual therapies can correct the spinal alignment, facilitate the movement of intervertebral joints, stretch the shortened tissues, and release adhesions around the joints. Therefore, these techniques are expected to be effective in improving spinal abnormalities. One of the studies used manual therapy to treat abnormalities was conducted by Łukasik et al. [27]. They compared the effectiveness of MFR techniques with massage therapy on 18 patients (12 females and 6 males) with the upper crossed syndrome.
They were divided into two groups of MFR (8 females, 1 male) and massage (4 females, 5 males). The therapy lasted for two weeks, 30 min per day. They concluded that both methods could increase cervical spine height (suprasternal height) and chest mobility (mobility of thoracic spine) in samples. Likewise, Kamali et al. compared manual therapy and exercise therapy in people with postural hyperkyphosis and reported that the angle of thoracic kyphosis significantly decreased and thoracic extensor muscle strength increased in both groups [28]. Shojaei et al. investigated the effect of MFR by using rolling foam training on lumbar lordosis in older men and concluded that it had a significant impact on the reduction of lumbar lordosis [29]. As can be seen, the majority of these studies compared the effect of MFR technique with other corrective exercises of musculoskeletal abnormalities.
Considering the beneficial effects of MFR technique on reducing muscle tightness and eliminating muscle imbalances, its combination with other corrective exercises can be more effective in correcting FSP. In the literature review, we found no study that investigated the effect of MFR technique combined with exercise therapy. In this regard, this study aimed to evaluate the effect of the 8-week combined protocol of MFR technique and corrective exercises on FSP and to find out which of these methods were more effective in correcting FSP. Comparison of the long-term effects of each of them during a 4-week follow-up period was another objective of this study.
2. Materials and Methods
This research is a quasi-experimental study. The study population consisted of all non-athlete male students aged 18-28 years at the Islamic Azad University of Zanjan, Iran, who had FSP. These students were identified from the general physical education classes by the researcher and introduced to the examiner. Then, based on inclusion criteria, 45 samples were selected for the study and randomly assigned in three groups of CE (Corrective Exercises only), CE+MFR (Corrective Exercises + MFR therapy), and control. The inclusion criteria were having FSP angle>52° [9, 30], forward head posture angle>46° [9, 30], thoracic kyphosis angle>42° [31, 32], being 18-28 years old, and giving informed consent to participate voluntarily.
On the other hand, the exclusion criteria were having a history of bone fracture, operation, or joint diseases in the spine, shoulder, and pelvis; having lower crossed syndrome; doing regular physical activity; being championship and membership in sports teams; having specific job conditions (which can exacerbate the deformity and avoid correcting posture at workplace); unwilling to participate or continue with participation during exercises; not participating in two consecutive training sessions or three alternate training sessions; and not attending in meetings to measure the dependent variables before or after the intervention.
After completing the consent form and collecting standard demographic information about height, weight, and age (using a measuring tape and a digital scale) from all subjects, they all took the pretest to assess their FSP angle using photographic analysis. This method has been used in numerous studies with good reliability (0.91) [33, 34, 35]. For angle measurement, first, the two anatomical landmarks of the right side acromion tubercle and the C7 spinous process were determined. To identify the C7 spinous process, the examiner stood behind the subject and asked to bend his head forward.
Two prominences were felt at the base of the neck, which were C6 and C7 spinous processes. Then, while palpating the prominences, the subject was asked to return his head to a natural position (extension). In this case, one of prominences (C6) disappeared, and only one remained (C7) [10, 31]. A prominent landmark was used to mark the place of C7. After that, the subject was asked to stand at a determined place near the wall (at a distance of 23 cm) with the left arm toward the wall. The digital camera tripod was then placed at a distance of 265 cm from the wall, and its height was adjusted at the right shoulder level of the subject. The subject was asked to bend forward three times and raise his hands over his head three times and then stand naturally and relaxed and look at an imaginary point on the opposite wall (eyes on the horizon).
After a 5-sec pause, the examiner took a photo from the profile view. The photo was transferred into a computer, and by using AutoCAD software, the degree of FSP angle was measured [9]. A flexible ruler was used to measure the degree of kyphosis angle. The photographic analysis also was used to measure Forward Head Posture (FHP) angle [8-10, 32, 33, 36]. The Standard Error Measurement (SEM) was calculated to determine the reliability of the FSP angle [37]. To do this, FSP angle of 15 subjects was measured for three days and for three times, and its SEM was reported as 0.6°, which indicates the high accuracy of the measurement.
The control subjects continued their daily routine without doing any specific exercises, while CE+MFR group performed corrective exercises plus MFR therapy, and CE group performed only corrective exercises for 8 weeks (3 sessions per week and each session for 60 min) under the direct supervision of the examiner. For CE+MFR group, training protocol included four parts of warming up, MFR therapy, main exercises, and cooling down. For the CE group, the same protocol was used but had no MFR therapy. The exercises performed in this study were adapted from the comprehensive exercises of Katzman et al. study [38].
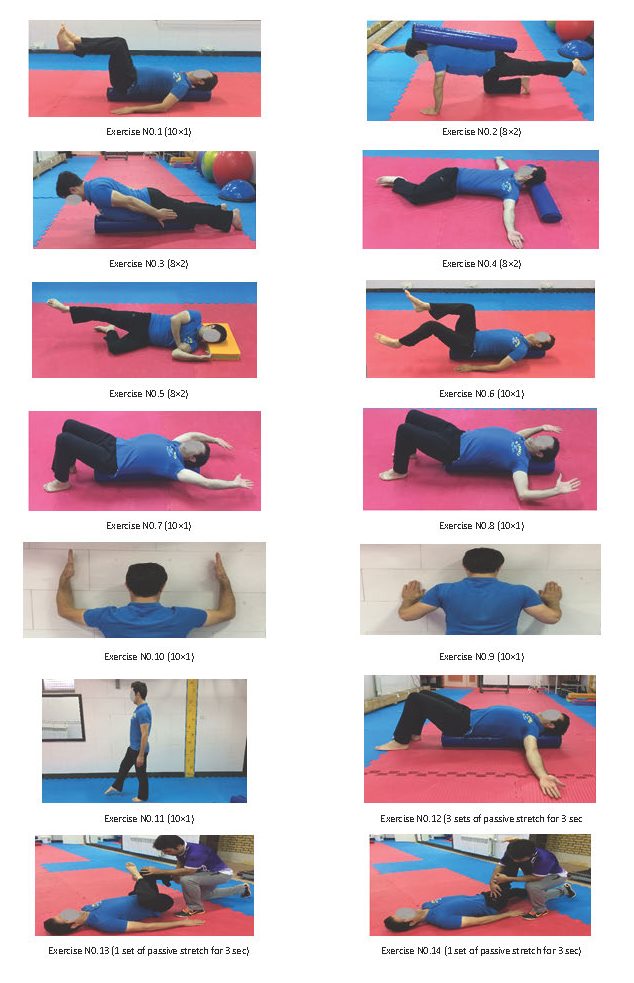
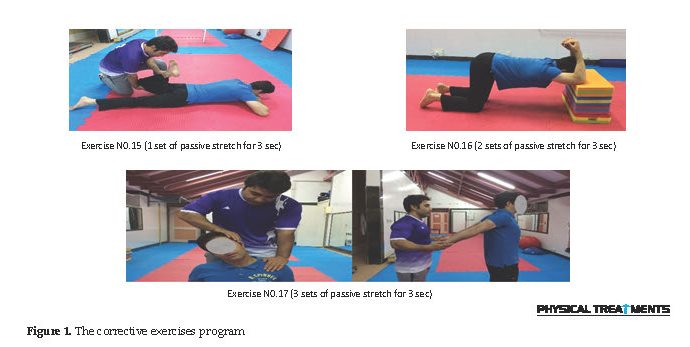
As shown in Figure 1, the exercise program consisted of three parts of spinal strengthening exercises, spinal alignment exercises, and spinal mobility exercises. The general purpose of this program was to correct musculoskeletal impairments; these exercises were presented in a multidimensional form and three parts. The exercises in the first part aimed to increase trunk stability/mobility, to strengthen lower trapezius muscle, spinal extensor muscles, multifidus muscle, and the transversus abdominis muscle, to empower posterior lumbar/hip extensor muscles, to strengthen and increase the spine mobility during spine rotation and extension, and to empower gluteus medius muscle for keeping stability in standing position. The exercises in this part included supine transversus abdominis on the foam roller (No. 1), quadruped arm and leg lift (No. 2), prone trunk lift to neutral (No. 3), side-lying thoracic rotation/extension (No. 4), and side-lying hip abduction/external rotation (No. 5).
The exercises in the second part aimed to increase heart rate and the temperature of core muscles, shoulder and chest flexibility, trunk stability and the shoulder/spine mobility, and to strengthen lower trapezius and serratus anterior muscles and scapular stability. The exercises in this part were marching on the foam roller (No. 6), unilateral overhead reaching on roller (No. 7), bilateral pull-down supine on roller (No. 8), shoulder flexion/thoracic extension at wall (No. 9), wall push-ups (No. 10), and single-leg stance (No. 11).
Finally, the exercises in the third part aimed to stretch pectoralis major muscle and increase the expansiveness of rib cage and anterior chest wall; to increase the length of the posterior hip, gluteal, hamstring, gastrocnemius-soleus, quadriceps, trapezius muscles; and to increase spine extension. The third part exercises were chest/spine stretching supine/roller (No. 12), gluteal stretching (No. 13), supine straight-leg raise, prone hip (No. 14), quadriceps stretch (No. 15), quadruped thoracic extension stretch (No. 16), and neck/chest stretch standing (No. 17).
The intensity of exercises was determined based on the Borg scale from 15 to 16 (70-80% of the perceived exertion). This intensity has been recommended to gain strength. Studies also have shown that this intensity rate is effective in improving endurance in the upper and lower limb muscles in adults. A progressive 8-week protocol was used for all strength practices (quadriceps, hands, upper trunk, and so on). At first, without resistance, and then when the subjects got adapted to the exercises, the intensity of the exercises increased with using Thera-Band or wrist weights. The subjects reported the intensity of the tasks with expressions like “a little hard” (moderate intensity 50-60%) and “hard” (higher than moderate intensity 70-80%). If the subjects rated the intensity level less than “a little hard,” the intensity level would be increased, but if they rated it more than “hard”, the intensity level would be reduced.
The goal was to perform one set of each task in a range of 70-80% so that the subjects can perform 8 repetitions well. Wrist weights were used to increase the resistance. The weights increased by 0.5 kg each time. Thera-Band was used to increase the intensity of stretching exercises. Thera-Band resistance increased from yellow to red, green, and finally, blue. The increase in resistance continued until reaching from the perceived exertion of “a little hard” to “hard” [38].
For MFR therapy, the “cross-hand release” technique was used. This technique is conducted on anterior chest (pectoral area), and the posterior part, especially the upper part. For releasing, cross hands are applied on the area with gentle pressure and then moved in the opposite direction to feel the end of tissue barrier according to the technique proposed by Duncan and then waiting there until it releases [39]. According to Duncan, since collagen bands need about 90-120 sec to be released, at least 90 sec is required for cross-hand release. Accordingly, we applied MFR therapy twice each time for 90 seconds on the determined areas.
In the end, all groups went under assessment, and their FSP angle was measured similar to the pretest phase. After 4 weeks, the effect of exercises was followed up to examine their long-term effect. The collected data were analyzed in SPSS V. 20 using descriptive and inferential statistics. After testing the normality of data distribution by Kolmogorov-Smirnov test, the repeated measures ANOVA was carried out for assessing intra-group differences, and ANCOVA for inter-group changes. The significance level was set at P<0.05.
3. Results
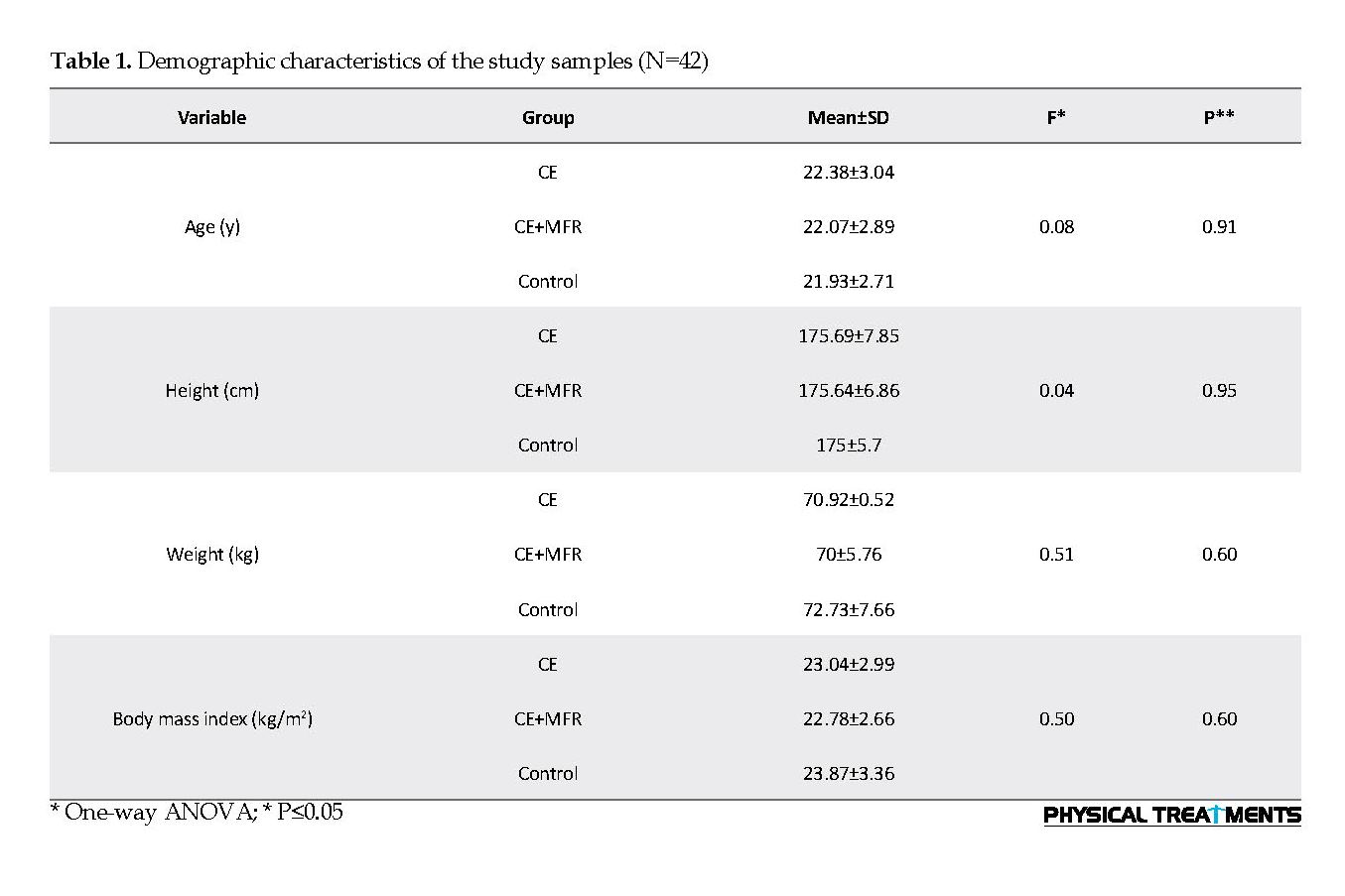
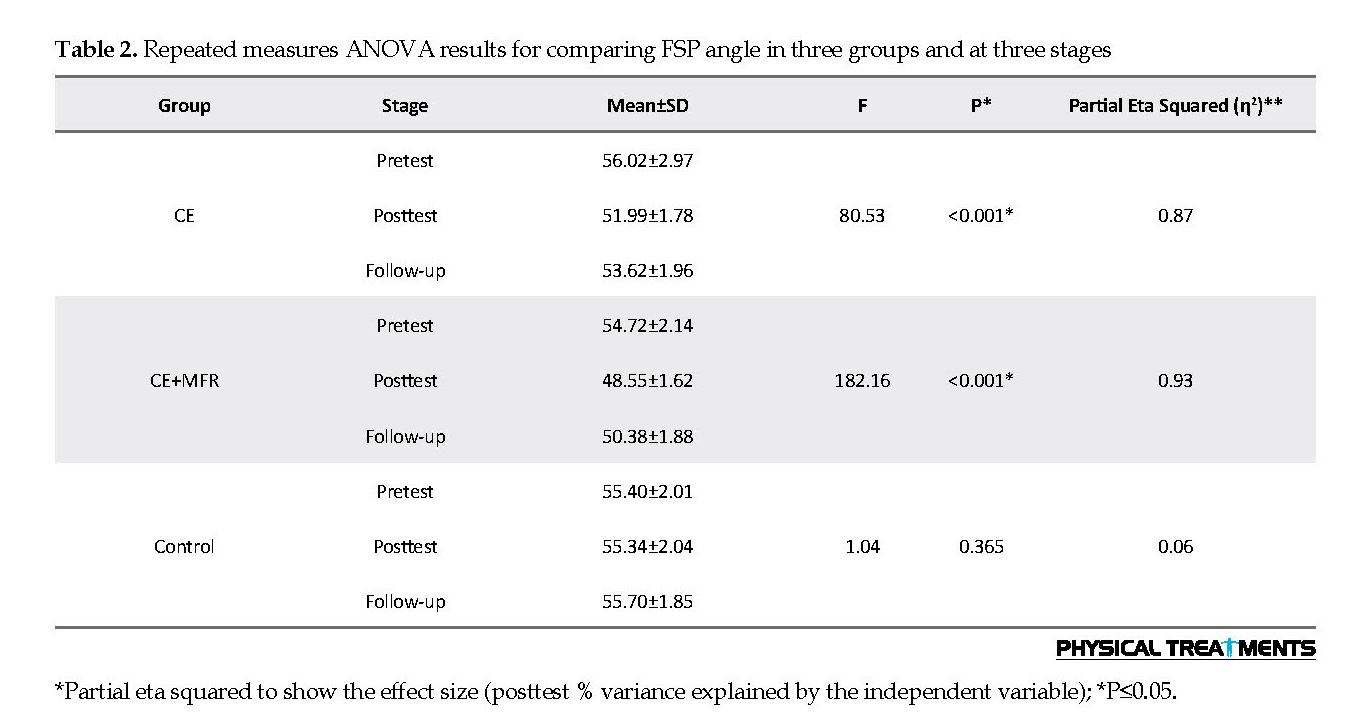
Table 1 presents the demographic characteristics of the participants. The results of the 1-way ANOVA showed no significant difference between the three study groups in terms of height, weight, age, and body mass index (P>0.05). For comparison of FSP angles in the pretest, posttest, and follow-up (intra-group variation) between three groups, the repeated measures ANOVA was used. The results shown in Table 2 indicate a significant difference between CE and CE+MFR groups in FSP angle (P≤0.05).
The proper physical condition requires the correct placement of the spines and joints so that the muscles and ligaments act naturally [1]. Adoption of inappropriate postures in life leads to muscle imbalance and postural changes [2]. The Forward Shoulder Posture (FSP) is one of the many postural deviations that accounts for 80% of shoulder deformities [3]. It is known as scapular protraction and elevation with a forward position of the shoulder, causing a funnel chest [4]. This deformity is probably due to the shortened and tight anterior muscles and the weakness and elongation of the posterior muscles of the shoulder girdle [5].
It seems that the weakness of the muscles holding the spine can weaken the static and dynamic postural balance [6]. Abnormal changes in balance and muscle strength (length-tension relationship) increase the motor recruitment time consequences (a couple) and movement disorder of the scapular joint for internal rotation. These changes also decrease the posterior tilt and the upward scapular rotation, which leads to FSP [7]. Based on many references, FSP will be diagnosed if the angle between the vertical line and the line linked C7 spinous process with the acromion process be more than 52 degrees [8-10].
Physiological complications of FSP vary from person to person in terms of prevalence and severity. The muscle imbalance caused by FSP can restrict chest expansion during respiration and result in hard breathing [9]. The anterior pectoral muscle stiffness because of long-term contraction leads to forward rotation of shoulder girdle, out of the anatomic plate, and besides limiting the range of motion of shoulder and arm joints, causes the narrowing of the dorsal neural tube and the pressure on the dorsal and suprascapular nerves, creating neurological symptoms [11]. Moreover, the subacromial space reduces, and the subject is susceptible to subacromial impingement syndrome [12].
Research has shown several ways to correct this deformity, including manual therapy, postural re-education, using taping and orthoses, and exercise therapy [13-15]. The goals of implementing all these methods, especially exercise therapy (corrective movements) for correcting FSP deformity is to improve the range of motion, increase the flexibility, increase the strength of the weakened muscles, and in general, eliminate muscle imbalance (establishing a balance between muscles involved in deformity).
Researchers have always sought to find combined corrective exercises for greater efficacy to correct FSP. For example, Morningstar proposed a rehabilitative procedure using chiropractic and spinal manipulative therapy to correct FSP [16]. Rahnema et al. in a study on examining the effect of 8-week regular corrective exercises on the spinal cord of female students, reported that these exercises were a safe and useful way to improve spine abnormalities and reduce future problems and discomforts [17]. In their study, muscle stretching and strength exercises were carried out as well as proprioceptive neuromuscular facilitation for better and faster performance through effective stimulation of receptors. In another study, Zandi et al. [18] by comparing three programs of corrective exercises, postural re-education, and their combination on FSP found out that the combination of corrective exercises with postural re-education had a significant effect on reducing the FSP angle.
Muscle shortness and connective tissue stiffness are common musculoskeletal problems which may be caused by various reasons such as illness, trauma, insufficient mobility, or scarring. Reduced soft tissue flexibility and movement limitation can lead to changes in motor patterns and musculoskeletal disorders [19]. Many of the methods used to maintain flexibility in the muscles emphasize the use of different stretching exercises [20]. Other methods that are commonly used to improve muscle flexibility include heat [20, 21], massage [22], proprioceptive neuromuscular facilitation [23], muscle energy techniques [24] and Myofascial Release (MFR) techniques [25].
MFR techniques are manual techniques used by health-care professionals or by the patient [called Self-Myofascial Release (SMR)] to influence the fascia. Although it is still unknown how these techniques work, their therapeutic effects have been clinically proven [25]. These techniques stretch the restricted fascia. A gentle pressure for 90-120 s in the restricted tissue increases its flexibility, and then the first release occurs. After that, the therapist takes the tissue to a new area and keeps it in hand. After several releases, the tissue becomes softer. The claimed effects for MFR techniques are similar to the effects of massage and soft-tissue mobilization techniques which include changing blood circulation, dilatation of the capillaries, stimulation of the nervous system, and changes in skin temperature and metabolism [26].
Several studies have shown that manual therapies can correct the spinal alignment, facilitate the movement of intervertebral joints, stretch the shortened tissues, and release adhesions around the joints. Therefore, these techniques are expected to be effective in improving spinal abnormalities. One of the studies used manual therapy to treat abnormalities was conducted by Łukasik et al. [27]. They compared the effectiveness of MFR techniques with massage therapy on 18 patients (12 females and 6 males) with the upper crossed syndrome.
They were divided into two groups of MFR (8 females, 1 male) and massage (4 females, 5 males). The therapy lasted for two weeks, 30 min per day. They concluded that both methods could increase cervical spine height (suprasternal height) and chest mobility (mobility of thoracic spine) in samples. Likewise, Kamali et al. compared manual therapy and exercise therapy in people with postural hyperkyphosis and reported that the angle of thoracic kyphosis significantly decreased and thoracic extensor muscle strength increased in both groups [28]. Shojaei et al. investigated the effect of MFR by using rolling foam training on lumbar lordosis in older men and concluded that it had a significant impact on the reduction of lumbar lordosis [29]. As can be seen, the majority of these studies compared the effect of MFR technique with other corrective exercises of musculoskeletal abnormalities.
Considering the beneficial effects of MFR technique on reducing muscle tightness and eliminating muscle imbalances, its combination with other corrective exercises can be more effective in correcting FSP. In the literature review, we found no study that investigated the effect of MFR technique combined with exercise therapy. In this regard, this study aimed to evaluate the effect of the 8-week combined protocol of MFR technique and corrective exercises on FSP and to find out which of these methods were more effective in correcting FSP. Comparison of the long-term effects of each of them during a 4-week follow-up period was another objective of this study.
2. Materials and Methods
This research is a quasi-experimental study. The study population consisted of all non-athlete male students aged 18-28 years at the Islamic Azad University of Zanjan, Iran, who had FSP. These students were identified from the general physical education classes by the researcher and introduced to the examiner. Then, based on inclusion criteria, 45 samples were selected for the study and randomly assigned in three groups of CE (Corrective Exercises only), CE+MFR (Corrective Exercises + MFR therapy), and control. The inclusion criteria were having FSP angle>52° [9, 30], forward head posture angle>46° [9, 30], thoracic kyphosis angle>42° [31, 32], being 18-28 years old, and giving informed consent to participate voluntarily.
On the other hand, the exclusion criteria were having a history of bone fracture, operation, or joint diseases in the spine, shoulder, and pelvis; having lower crossed syndrome; doing regular physical activity; being championship and membership in sports teams; having specific job conditions (which can exacerbate the deformity and avoid correcting posture at workplace); unwilling to participate or continue with participation during exercises; not participating in two consecutive training sessions or three alternate training sessions; and not attending in meetings to measure the dependent variables before or after the intervention.
After completing the consent form and collecting standard demographic information about height, weight, and age (using a measuring tape and a digital scale) from all subjects, they all took the pretest to assess their FSP angle using photographic analysis. This method has been used in numerous studies with good reliability (0.91) [33, 34, 35]. For angle measurement, first, the two anatomical landmarks of the right side acromion tubercle and the C7 spinous process were determined. To identify the C7 spinous process, the examiner stood behind the subject and asked to bend his head forward.
Two prominences were felt at the base of the neck, which were C6 and C7 spinous processes. Then, while palpating the prominences, the subject was asked to return his head to a natural position (extension). In this case, one of prominences (C6) disappeared, and only one remained (C7) [10, 31]. A prominent landmark was used to mark the place of C7. After that, the subject was asked to stand at a determined place near the wall (at a distance of 23 cm) with the left arm toward the wall. The digital camera tripod was then placed at a distance of 265 cm from the wall, and its height was adjusted at the right shoulder level of the subject. The subject was asked to bend forward three times and raise his hands over his head three times and then stand naturally and relaxed and look at an imaginary point on the opposite wall (eyes on the horizon).
After a 5-sec pause, the examiner took a photo from the profile view. The photo was transferred into a computer, and by using AutoCAD software, the degree of FSP angle was measured [9]. A flexible ruler was used to measure the degree of kyphosis angle. The photographic analysis also was used to measure Forward Head Posture (FHP) angle [8-10, 32, 33, 36]. The Standard Error Measurement (SEM) was calculated to determine the reliability of the FSP angle [37]. To do this, FSP angle of 15 subjects was measured for three days and for three times, and its SEM was reported as 0.6°, which indicates the high accuracy of the measurement.
The control subjects continued their daily routine without doing any specific exercises, while CE+MFR group performed corrective exercises plus MFR therapy, and CE group performed only corrective exercises for 8 weeks (3 sessions per week and each session for 60 min) under the direct supervision of the examiner. For CE+MFR group, training protocol included four parts of warming up, MFR therapy, main exercises, and cooling down. For the CE group, the same protocol was used but had no MFR therapy. The exercises performed in this study were adapted from the comprehensive exercises of Katzman et al. study [38].
As shown in Figure 1, the exercise program consisted of three parts of spinal strengthening exercises, spinal alignment exercises, and spinal mobility exercises. The general purpose of this program was to correct musculoskeletal impairments; these exercises were presented in a multidimensional form and three parts. The exercises in the first part aimed to increase trunk stability/mobility, to strengthen lower trapezius muscle, spinal extensor muscles, multifidus muscle, and the transversus abdominis muscle, to empower posterior lumbar/hip extensor muscles, to strengthen and increase the spine mobility during spine rotation and extension, and to empower gluteus medius muscle for keeping stability in standing position. The exercises in this part included supine transversus abdominis on the foam roller (No. 1), quadruped arm and leg lift (No. 2), prone trunk lift to neutral (No. 3), side-lying thoracic rotation/extension (No. 4), and side-lying hip abduction/external rotation (No. 5).
The exercises in the second part aimed to increase heart rate and the temperature of core muscles, shoulder and chest flexibility, trunk stability and the shoulder/spine mobility, and to strengthen lower trapezius and serratus anterior muscles and scapular stability. The exercises in this part were marching on the foam roller (No. 6), unilateral overhead reaching on roller (No. 7), bilateral pull-down supine on roller (No. 8), shoulder flexion/thoracic extension at wall (No. 9), wall push-ups (No. 10), and single-leg stance (No. 11).
Finally, the exercises in the third part aimed to stretch pectoralis major muscle and increase the expansiveness of rib cage and anterior chest wall; to increase the length of the posterior hip, gluteal, hamstring, gastrocnemius-soleus, quadriceps, trapezius muscles; and to increase spine extension. The third part exercises were chest/spine stretching supine/roller (No. 12), gluteal stretching (No. 13), supine straight-leg raise, prone hip (No. 14), quadriceps stretch (No. 15), quadruped thoracic extension stretch (No. 16), and neck/chest stretch standing (No. 17).
The intensity of exercises was determined based on the Borg scale from 15 to 16 (70-80% of the perceived exertion). This intensity has been recommended to gain strength. Studies also have shown that this intensity rate is effective in improving endurance in the upper and lower limb muscles in adults. A progressive 8-week protocol was used for all strength practices (quadriceps, hands, upper trunk, and so on). At first, without resistance, and then when the subjects got adapted to the exercises, the intensity of the exercises increased with using Thera-Band or wrist weights. The subjects reported the intensity of the tasks with expressions like “a little hard” (moderate intensity 50-60%) and “hard” (higher than moderate intensity 70-80%). If the subjects rated the intensity level less than “a little hard,” the intensity level would be increased, but if they rated it more than “hard”, the intensity level would be reduced.
The goal was to perform one set of each task in a range of 70-80% so that the subjects can perform 8 repetitions well. Wrist weights were used to increase the resistance. The weights increased by 0.5 kg each time. Thera-Band was used to increase the intensity of stretching exercises. Thera-Band resistance increased from yellow to red, green, and finally, blue. The increase in resistance continued until reaching from the perceived exertion of “a little hard” to “hard” [38].
For MFR therapy, the “cross-hand release” technique was used. This technique is conducted on anterior chest (pectoral area), and the posterior part, especially the upper part. For releasing, cross hands are applied on the area with gentle pressure and then moved in the opposite direction to feel the end of tissue barrier according to the technique proposed by Duncan and then waiting there until it releases [39]. According to Duncan, since collagen bands need about 90-120 sec to be released, at least 90 sec is required for cross-hand release. Accordingly, we applied MFR therapy twice each time for 90 seconds on the determined areas.
In the end, all groups went under assessment, and their FSP angle was measured similar to the pretest phase. After 4 weeks, the effect of exercises was followed up to examine their long-term effect. The collected data were analyzed in SPSS V. 20 using descriptive and inferential statistics. After testing the normality of data distribution by Kolmogorov-Smirnov test, the repeated measures ANOVA was carried out for assessing intra-group differences, and ANCOVA for inter-group changes. The significance level was set at P<0.05.
3. Results
Table 1 presents the demographic characteristics of the participants. The results of the 1-way ANOVA showed no significant difference between the three study groups in terms of height, weight, age, and body mass index (P>0.05). For comparison of FSP angles in the pretest, posttest, and follow-up (intra-group variation) between three groups, the repeated measures ANOVA was used. The results shown in Table 2 indicate a significant difference between CE and CE+MFR groups in FSP angle (P≤0.05).
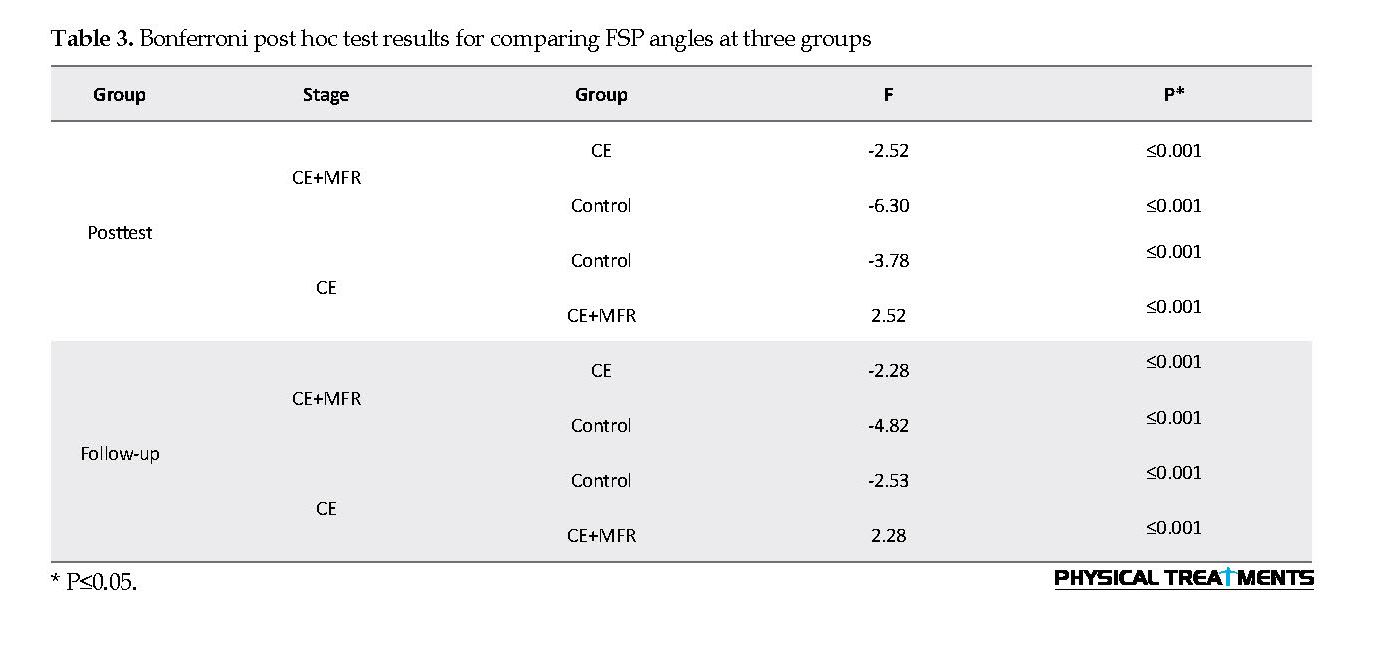
The Bonferroni post hoc test was used because of the significance of repeated measures ANOVA for pairwise comparison of FSP angles at different measurement phases. Its results showed that in the CE (mean difference=4.03, P=0.001) and CE+MFR groups (mean difference=6.17, P=0.001), the posttest FSP angle was significantly different from the pretest FSP angle, and the FSP angle reduced after the 8-week intervention. The FSP angle at the follow-up period in the CE (mean difference=2.40, P=0.001) and CE+MFR groups (mean difference= 4.33, P=0.001) also showed a significant reduction compared to pretest score.
For comparing the effect of corrective exercises alone and corrective exercises plus MFR on FSP angles at posttest and follow-up period, ANCOVA was used by considering pretest as covariate variable. The results showed significant differences between the three groups at posttest (F=117, P=0.001, η2=0.86) and follow-up (F=62.05, P=0.001, η2=0.76).
Because of the significance of repeated measures ANOVA for pairwise comparison of changes, we used the Bonferroni post hoc test (Table 3). The results of this test showed that at posttest, the FSP angle in the CE+MFR group was significantly less than that of the CE and control groups (P≤0.001). Also, the FSP angle in the CE group was significantly less than that of the control group (P≤0.001). Besides, the Bonferroni test results showed that the subjects’ FSP angle in the follow-up test group in the CE+MFR group was significantly less than the CE and the control groups (P≤0.001). Also, FSP angle was significantly less than that in the control group (P≤0.001).
4. Discussion
In this randomized controlled trial on 45 samples, 15 performed corrective exercises, and 15 received a combination of corrective exercises and MFR therapy for 8 weeks under the direct supervision of the researcher (three time per week, each session one hour). The results showed no significant difference between the two exercises groups in terms of SFP angle with the control group that received no intervention. In the group received the combinational intervention, SFP angle reduced by 6 degrees and the group received only corrective exercises reported a 4 degrees reduction in SFP angle.
However, based on ANOVA results, the combinational intervention had a greater and more significant effect on reducing SFP angle compared to corrective exercises alone. After 4-week follow-up, no significant difference was found between the two groups in SFP angle compared to posttest results. This finding indicates the lasting effect of exercises in both exercise groups 4 weeks after the completion of the tasks compared to the control group.
To the best of our knowledge, no study has investigated the combination of corrective exercises with MFR technique on FSP, so the results of this study cannot be compared directly with the results of other studies. However, as noted, many studies have examined the effects of corrective exercises on this deformity. In this regard, the results of this study regarding the effectiveness of corrective exercises on FSP correction are consistent with the findings of Seidi, Hajihosseini et al., Ruivo et al., Lynch et al., and Kluemper et al. [9, 30, 40-42]. All of these studies have reported the significant effect of corrective exercises on FSP correction. Also, it should be noted that most previous studies were used the interventional exercises alone, and no study has ever tried to test the effect of corrective exercises combined with myofascial release technique in treating FSP.
In the exercise protocol of this study, the strength exercises were used to increase the power of straightening muscles of the spine in patients with FSP, because these exercises strengthen spinal muscles and play an essential role in maintaining the posture and can help to improve the FSP. On the other hand, the results of previous studies have shown that combining spinal strength exercises with stretching exercises can reduce the degree of FSP angle in the affected people [8, 33]. It is proven that trunk muscles are involved in controlling the movement and stability of the spine, but the deep and core muscles play a vital role in controlling intervertebral movements. They also provide spinal stability in dynamic conditions.
Accordingly, in this study, in addition to empowering the posterior extensor muscles, deep and core muscles of the body were strengthened too, and pectoral muscles were stretched so that the chest expansion and the mobility of thoracic spine be considered. Furthermore, the exercises were performed in a closed kinetic chain and during weight bearing on a foam roller to be closer to the natural condition of the body [38]. Researchers have stated that, following strength training in skeletal muscles, some changes may occur, including an increase in total amount of contractile proteins, especially myosin fibers, and increase in the amount and strength of connective tissues, capillary density, and the number of fibers via longitudinal fiber splitting. These alterations increase muscle strength and endurance. They also stated that stretching exercises would act as a coordinator of agonist and antagonist muscle activities [43]. Therefore, it seems that the tasks performed in this study may lengthen the anterior chest wall muscle and strengthen the posterior and core muscles, followed by reducing the degree of FSP in the patients.
To the best of our knowledge, no study has investigated the combination of corrective exercises with MFR technique on FSP, so the results of this study cannot be compared directly with the results of other studies. However, as noted, many studies have examined the effects of corrective exercises on this deformity. In this regard, the results of this study regarding the effectiveness of corrective exercises on FSP correction are consistent with the findings of Seidi, Hajihosseini et al., Ruivo et al., Lynch et al., and Kluemper et al. [9, 30, 40-42]. All of these studies have reported the significant effect of corrective exercises on FSP correction. Also, it should be noted that most previous studies were used the interventional exercises alone, and no study has ever tried to test the effect of corrective exercises combined with myofascial release technique in treating FSP.
In the exercise protocol of this study, the strength exercises were used to increase the power of straightening muscles of the spine in patients with FSP, because these exercises strengthen spinal muscles and play an essential role in maintaining the posture and can help to improve the FSP. On the other hand, the results of previous studies have shown that combining spinal strength exercises with stretching exercises can reduce the degree of FSP angle in the affected people [8, 33]. It is proven that trunk muscles are involved in controlling the movement and stability of the spine, but the deep and core muscles play a vital role in controlling intervertebral movements. They also provide spinal stability in dynamic conditions.
Accordingly, in this study, in addition to empowering the posterior extensor muscles, deep and core muscles of the body were strengthened too, and pectoral muscles were stretched so that the chest expansion and the mobility of thoracic spine be considered. Furthermore, the exercises were performed in a closed kinetic chain and during weight bearing on a foam roller to be closer to the natural condition of the body [38]. Researchers have stated that, following strength training in skeletal muscles, some changes may occur, including an increase in total amount of contractile proteins, especially myosin fibers, and increase in the amount and strength of connective tissues, capillary density, and the number of fibers via longitudinal fiber splitting. These alterations increase muscle strength and endurance. They also stated that stretching exercises would act as a coordinator of agonist and antagonist muscle activities [43]. Therefore, it seems that the tasks performed in this study may lengthen the anterior chest wall muscle and strengthen the posterior and core muscles, followed by reducing the degree of FSP in the patients.
According to the Janda theory, the main reason for FSP is muscle imbalance [44]. Based on this theory, in FSP, the muscle imbalance causes shoulders to move away from each other and lifts lower angles, and as a result, shoulders move forward. Therefore, for reduction of FSP angle, the main focus in our exercises was on correcting the scapula position.
In this regard, our exercises aimed to strengthen scapular stabilizing muscles, including rhomboid, lower trapezius, and serratus anterior so as while maintaining the stability of the shoulder, coordinate couple forces and main mover muscles of the scapula, and avoid abnormal positioning of the scapula and then reduce the FSP angle. Hence, our exercise program is based on the basic principles of comprehensive corrective exercises (simultaneous attention to the total physical condition of the subjects, observing the correct alignment of all limbs, creating a concurrent contraction in the involved muscles, enabling the nervous system to maintain the correct posture and in general, attention to muscle-skeletal-neural chains during training) had acceptable effectiveness on both CE and CE+MFR groups, eventually caused intra-group changes and reduced FSP angle at posttest stage compared to the pretest and follow-up results.
In the group received corrective exercises with MFR therapy, we observed more reduction of FSP angle compared to the group received corrective exercises only. Probably one of the main reasons for this result is the application of MFR therapy.
So far, many studies have indicated the usefulness of MFR techniques. Therefore, the researcher now tries to review the benefits of myofascial release based on scientific evidence and discuss the possible reasons for the effectiveness of combination therapy.
The word “Myofascia” consists of two parts; “Myo” means muscle and “fascia” means band. Myofascia, which is also considered a connective tissue, is an embryonic web-like tissue that covers the entire human body and is closely related to all different structures of the body. Besides surrounding body structures, it also has the responsibility to protect them. Fascia, as the largest system in the human body, is a single sheet of connective tissue that extends from the sole of the feet to the skull and from interior to the exterior of the body [39]. Since fascia tissue has many sensory receptors (almost ten times that of muscle tissue), it is also referred to as signal sender system. In this regard, this tissue has a high mechanical sensitivity to the tensions or pressures on it [45].
Concerning many receptors in the fascia, it has an integrated, sensitive, and precise function like the nervous system and with a wide range of roles throughout the body. It is clear that by making any changes in this tissue, we will see widespread changes in different parts of human movement patterns. This phenomenon can be explained by the myofascial chain reaction theory [44]. Based on this theory, fascia can directly and profoundly affect the function of other parts of the body. Thus, with the slightest change in fascia due to the nature of its reaction against physical and neurological damage, the connective tissue is being deformed, hardened, and thickened. Poor physical condition and subsequent musculoskeletal abnormalities can cause these changes in fascia, and as a result, the body loses its physiological adaptive capacity [44].
One of the most prominent features of fascia is its inner elasticity. It allows the fascia to resist against deformation when pressures and forces are applied on it, and in addition to stabilization and general strengthening of the body, it can easily return to its original shape after relieving the pressure [39]. When the force is exerted to the fascia, its viscoelastic nature allows it to extend against the pressure. Over time, fascia deforms slowly in proportion to the exerted force, and the so-called “creep” occurs in it.
The MFR techniques are applied with continuous (90 to 120 sec) and gentle pressure. These techniques extend the elements of elastic and reticular fibers, which is continued until the release is stopped. During the release, the “ground substance” starts to flow [46]. This substance in fascia tissue has a strong hydrophilic property and therefore, like a gel-like tissue, allows other elements (collagen and elastin) to glide over it and move [39] easily. This viscous substance is a part of the connective tissue cells that is deformed due to the positive influence of MFR techniques.
It seems that the MFR technique in this study (cross-hand technique) applied on pectoral and thoracic muscles was able to break down cross-linkages (plastic deformation) and circulate ground substance and hence, increase the flexibility of fascia tissue [46]. In this regard, we observed a more significant reduction in FSP angle among those received combinational exercises compared to those with corrective exercises only.
In this study, the researcher attempted to correct these deformities in young people with the consideration of previous national and international studies on the effect of training intervention on FPS correction which mainly recommended concurrent using of strength and stretching exercises along with postural exercises and combining them with other methods such as MFR therapy (as an effective and recommended method along with corrective exercises). By adapting exercises proposed by Katzman et al. [38] and combining them with MFR therapy, we sought to diversify and use combinational techniques, and due to the significant reduction of FSP angle in the posttest and follow-up stages, we can conclude that the program was successful.
As a result, according to the findings of the present study, it is suggested that MFR therapy be used as an effective method in combination with corrective exercises to correct FSP deformity.
Ethical Considerations
Compliance with ethical guidelines
This study has been approved by the National Ethics Committee of Biomedical Research (Code: IR.UT.SPORT.REC.1397.004).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
All authors contributed in designing, running, and writing all parts of the research.
Conflict of interests
The authors declared no conflict of interest.
References
Houglum PA. Therapeutic exercise for athletic injuries. Champaign: Human Kinetics; 2001.
Penha PJ, João SMA, Casarotto RA, Amino CJ, Penteado DC. Postural assessment of girls between 7 and 10 years of age. Clinics. 2005; 60(1):9-16. [DOI:10.1590/S1807-59322005000100004] [PMID]
Neuman D. Kinesiology of the musculoskeletal system: Foundation for rehabilition. London: Mosby; 2010.
Kendall FP, McCreary EK, Provance PG, Rodgers M, Romani WA. Muscles: Testing and function, with posture and pain: Includes a bonus primal anatomy. Philadelphia: Lippincott Williams & Wilkins; 2005.
Savadatti R, Gaude GS. Effect of forward shoulder posture on forced vital capacity-A co-relational study. Indian Journal of Physical Therapy and Occupational Therapy.2011; 5(2):119-23.
Shavandi N SS, Heidarpor R, Sheikh Hoseini R. [The effect of a 7 weeks corrective exercise on thoracic kyphosis in hyper-kyphotic students (Persian)]. Journal of Kurdistan University of Medical Sciences. 2011;13(4): 42-50.
Najafi M, Behpour Q, Qayini S, Younes H. [Effect of tensile-selective corrective exercises on shoulder dislocation in front of elementary school students (Persian)]. Journal of Rehabilitation Sciences. 2012;1(2):54-60.
Hajihosseini E, Norasteh A A, Shamsi A, Daneshmandi H. [The effect of 6 weeks strength training, stretching and comprehensive corrective exercises on forward head incorrect posture (Persian)]. Journal of Modern Rehabilitation. 2016; 9(S1):38-48
Seidi F. [The effect of a 12-week corrective exercises program on forward head and shoulder deformities (Persian)]. Studies in Sport Medicine. 2011; (14):31-44.
Rajabi R. [Laboratory corrective movements (Persian)]. Tehran: University of Tehran; 2016.
Oyama S. Profiling physical characteristics of the swimmer’s shoulder: comparison to baseball pitchers and non-overhead athletes [PhD. dessertation]. Pittsburgh: University of Pittsburgh; 2006.
Hammer W. Posture evaluations, forward head and forward shoulder. Dyna Chir-pract. 2010; 17(18):1-2.
Harman K, Hubley-Kozey CL, Butler H. Effectiveness of an exercise program to improve forward head posture in normal adults: A randomized, controlled 10-week trial. Journal of Manual & Manipulative Therapy. 2005; 13(3):163-76. [DOI:10.1179/106698105790824888]
Andersen CH, Andersen LL, Mortensen OS, Zebis MK, Sjøgaard G. Protocol for shoulder function training reducing musculoskeletal pain in shoulder and neck: A randomized controlled trial. BMC Musculoskeletal Disorders. 2011; 12:14. [DOI:10.1186/1471-2474-12-14] [PMID] [PMCID]
Morningstar MW, Strauchman MN, Weeks DA. Spinal manipulation and anterior headweighting for the correction of forward head posture and cervical hypolordosis: A pilot study. Journal of Chiropractic Medicine. 2003; 2(2):51-4. [DOI:10.1016/S0899-3467(07)60042-1]
Morningstar M. Cervical curve restoration and forward head posture reduction for the treatment of mechanical thoracic pain using the pettibon corrective and rehabilitative procedures. Journal of Chiropractic Medicine. 2002; 1(3):113-5. [DOI:10.1016/S0899-3467(07)60013-5]
Rhanema N, Bambaeichi E, Taghian F, Nazarian AB, Abdolahi M. [Effect of 8 weeks of regular regimens on spinal cord (rectus, spinal scoliosis and lumbar lordosis) in female students (Persian)]. Journal of Isfahan Medical School. 2009; 27(101):676-86.
Zandi S. [Comparison of the effect of a period of corrective exercises on the rehearsal of postural habits and their combination in correcting upper crossover syndrome in 10-11 years old girls (Persian)] [MA. thesis]. Tehran: University of Tehran; 2010.
Prentice WE. Rehabilitation techniques for sports medicine and athletic training. New York: McGraw-Hill; 2004.
Knight CA, Rutledge CR, Cox ME, Acosta M, Hall SJ. Effect of superficial heat, deep heat, and active exercise warm-up on the extensibility of the plantar flexors. Physical Therapy. 2001; 81(6):1206-14. [DOI:10.1093/ptj/81.6.1206]
Funk D, Swank AM, Adams KJ, Treolo D. Efficacy of moist heat pack application over static stretching on hamstring flexibility. The Journal of Strength & Conditioning Research. 2001; 15(1):123-6. [DOI:10.1519/1533-4287(2001)0152.0.CO;2]
Barlow A, Clarke R, Johnson N, Seabourne B, Thomas D, Gal J. Effect of massage of the hamstring muscle group on performance of the sit and reach test. British Journal of Sports Medicine. 2004; 38(3):349-51. [DOI:10.1136/bjsm.2002.003673] [PMID] [PMCID]
Funk DC, Swank AM, Mikla BM, Fagan TA, Farr BK. Impact of prior exercise on hamstring flexibility: A comparison of proprioceptive neuromuscular facilitation and static stretching. The Journal of Strength & Conditioning Research. 2003; 17(3):489-92. [DOI:10.1519/00124278-200308000-00010]
Spernoga SG, Uhl TL, Arnold BL, Gansneder BM. Duration of maintained hamstring flexibility after a one-time, modified hold-relax stretching protocol. Journal of Athletic Training. 2001; 36(1):44-8. [PMID] [PMCID]
Kain J, Martorello L, Swanson E, Sego S. Comparison of an indirect tri-planar Myofascial Release (MFR) technique and a hot pack for increasing range of motion. Journal of Bodywork and Movement Therapies. 2011; 15(1):7-63. [DOI:10.1016/j.jbmt.2009.12.002] [PMID]
Izadkhah S NN, Maarufi N, Kocheili Y, Shabedin H. [Comparison of myofascial release and muscle energy technique effects on hamstring muscle flexibility (Persian)]. Journal of Modern Rehabilitation. 2016; 9(5):131-9.
Łukasik E, Targosiński P, Szymański M, Letkiewicz-Ryłów O, Styczeń P, Wychowański M. Comparing the effectiveness of myofascial techniques with massage in persons with upper crossed syndrome (preliminary report). Advances in Rehabilitation. 2017; 31(2):53-67. [DOI:10.1515/rehab-2015-0067]
Kamali F, Shirazi S, Ebrahimi S, Mirshamsi M, Ghanbari A. Comparison of manual therapy and exercise therapy for postural hyperkyphosis: A randomized clinical trial. Physiotherapy Theory and Practice. 2016; 32(2):92-7. [DOI:10.3109/09593985.2015.1110739] [PMID]
Shojaei P, Hemmatfar A, Behpour N. [The effect of eight weeks of rolling foam training on lumbar lordosis in older men (Persian)]. Journal of Applied Research Sport Science Without Borders. 2017; 1(4):75-88.
Hajihosseini E, Norasteh A, Shamsi A, Daneshmandi H. The effects of strengthening, stretching and comprehensive exercises on forward shoulder posture correction. Physical Treatments-Specific Physical Therapy Journal. 2014; 4(3):123-32.
Rajabi R. [Thoracic Kyphosis, Review of Literature, epidemiology. etiology, cause, evaluation and new corrective methods (Persian)]. Tehran: Tehran University; 2013.
Seidi F, Rajabi R, Ebrahimi E, Alizadeh MH, Minoonejad H. The efficiency of corrective exercise interventions on thoracic hyper-kyphosis angle. Journal of Back and Musculoskeletal Rehabilitation. 2014; 27(1):7-16. [DOI:10.3233/BMR-130411] [PMID]
Seidi F, Rajabi R, Ebrahimi E, Alizadeh MH, Daneshmandi H. [The effect of a 10-week selected corrective exercise program on postural thoracic kyphosis deformity (Persian)]. Sport Medicine (Harakat). 2013; 10:5-22.
Daneshmandi H, Mogharabi Mozafari M. [The effect of eight weeks of comprehensive corrective training on upper cross_syndrome (Persian)]. Journal of Research in Sports Medicine and Technology. 2014; 12(7):75-86.
Thigpen CA, Padua DA, Michener LA, Guskiewicz K, Giuliani C, Keener JD, et al. Head and shoulder posture affect scapular mechanics and muscle activity in overhead tasks. Journal of Electromyography and kinesiology. 2010; 20(4):701-9. [DOI:10.1016/j.jelekin.2009.12.003] [PMID]
Seidi F, Rajabi R, Alizadeh MH, Daneshmandi H. [The effect of a 10-week selected corrective exercise program on postural thoracic kyphosis deformity (Persian)]. Journal of Sport Medicine. 2013; 5(1):5-22. [DOI:10.22059/JSMED.2013.32159]
Hakimipour M, Rajabi R, Minoonejad H, Soltani A. [Reliability of foot photo box in measuring selected footprint indicesا (Persian)]. Journal of Applied Exercise Phycology. 2016; 4(8):122-14.
Katzman W, Vittinghoff E, Kado D, Lane N, Ensrud K, Shipp K. Thoracic kyphosis and rate of incident vertebral fractures: The fracture intervention trial. Osteoporosis International. 2016; 27(3):899-903. [DOI:10.1007/s00198-015-3478-2] [PMID] [PMCID]
Duncan R. Myofascial release. Campaign: Human kinetics. 2014.
Ruivo RM, Pezarat-Correia P, Carita AI. Effects of a Resistance And Stretching Training Program On Forward Head And Protracted Shoulder Posture In Adolescents. Journal of Manipulative and Physiological Therapeutics. 2017; 40(1):1-10. [DOI:10.1016/j.jmpt.2016.10.005] [PMID]
Lynch SS, Thigpen CA, Mihalik JP, Prentice WE, Padua D. The effects of an exercise intervention on forward head and rounded shoulder postures in elite swimmers. British Journal of Sports Medicine. 2010; 44(5):376-81. [DOI:10.1136/bjsm.2009.066837] [PMID]
Kluemper M, Uhl T, Hazelrigg H. Effect of stretching and strengthening shoulder muscles on forward shoulder posture in competitive swimmers. Journal of Sport Rehabilitation. 2006; 15(1):58-70. [DOI:10.1123/jsr.15.1.58]
Jang HJ, Kim MJ, Kim SY. Effect of thorax correction exercises on flexed posture and chest function in older women with age-related hyperkyphosis. Journal of Physical Therapy Science. 2015; 27(4):1161-4. [DOI:10.1589/jpts.27.1161] [PMID] [PMCID]
Frank C, Page P, Lardner R. Assessment and treatment of muscle imbalance: the Janda approach. Campaign: Human kinetics; 2009.
Langevin HM. Connective tissue: A body-wide signaling network? Medical Hypotheses. 2006; 66(6):1074-7. [DOI:10.1016/j.mehy.2005.12.032] [PMID]
Keirns M. Myofascial release in sports medicine. Champaign: Human Kinetics. 2000; 11(3):38-52.
In this regard, our exercises aimed to strengthen scapular stabilizing muscles, including rhomboid, lower trapezius, and serratus anterior so as while maintaining the stability of the shoulder, coordinate couple forces and main mover muscles of the scapula, and avoid abnormal positioning of the scapula and then reduce the FSP angle. Hence, our exercise program is based on the basic principles of comprehensive corrective exercises (simultaneous attention to the total physical condition of the subjects, observing the correct alignment of all limbs, creating a concurrent contraction in the involved muscles, enabling the nervous system to maintain the correct posture and in general, attention to muscle-skeletal-neural chains during training) had acceptable effectiveness on both CE and CE+MFR groups, eventually caused intra-group changes and reduced FSP angle at posttest stage compared to the pretest and follow-up results.
In the group received corrective exercises with MFR therapy, we observed more reduction of FSP angle compared to the group received corrective exercises only. Probably one of the main reasons for this result is the application of MFR therapy.
So far, many studies have indicated the usefulness of MFR techniques. Therefore, the researcher now tries to review the benefits of myofascial release based on scientific evidence and discuss the possible reasons for the effectiveness of combination therapy.
The word “Myofascia” consists of two parts; “Myo” means muscle and “fascia” means band. Myofascia, which is also considered a connective tissue, is an embryonic web-like tissue that covers the entire human body and is closely related to all different structures of the body. Besides surrounding body structures, it also has the responsibility to protect them. Fascia, as the largest system in the human body, is a single sheet of connective tissue that extends from the sole of the feet to the skull and from interior to the exterior of the body [39]. Since fascia tissue has many sensory receptors (almost ten times that of muscle tissue), it is also referred to as signal sender system. In this regard, this tissue has a high mechanical sensitivity to the tensions or pressures on it [45].
Concerning many receptors in the fascia, it has an integrated, sensitive, and precise function like the nervous system and with a wide range of roles throughout the body. It is clear that by making any changes in this tissue, we will see widespread changes in different parts of human movement patterns. This phenomenon can be explained by the myofascial chain reaction theory [44]. Based on this theory, fascia can directly and profoundly affect the function of other parts of the body. Thus, with the slightest change in fascia due to the nature of its reaction against physical and neurological damage, the connective tissue is being deformed, hardened, and thickened. Poor physical condition and subsequent musculoskeletal abnormalities can cause these changes in fascia, and as a result, the body loses its physiological adaptive capacity [44].
One of the most prominent features of fascia is its inner elasticity. It allows the fascia to resist against deformation when pressures and forces are applied on it, and in addition to stabilization and general strengthening of the body, it can easily return to its original shape after relieving the pressure [39]. When the force is exerted to the fascia, its viscoelastic nature allows it to extend against the pressure. Over time, fascia deforms slowly in proportion to the exerted force, and the so-called “creep” occurs in it.
The MFR techniques are applied with continuous (90 to 120 sec) and gentle pressure. These techniques extend the elements of elastic and reticular fibers, which is continued until the release is stopped. During the release, the “ground substance” starts to flow [46]. This substance in fascia tissue has a strong hydrophilic property and therefore, like a gel-like tissue, allows other elements (collagen and elastin) to glide over it and move [39] easily. This viscous substance is a part of the connective tissue cells that is deformed due to the positive influence of MFR techniques.
It seems that the MFR technique in this study (cross-hand technique) applied on pectoral and thoracic muscles was able to break down cross-linkages (plastic deformation) and circulate ground substance and hence, increase the flexibility of fascia tissue [46]. In this regard, we observed a more significant reduction in FSP angle among those received combinational exercises compared to those with corrective exercises only.
In this study, the researcher attempted to correct these deformities in young people with the consideration of previous national and international studies on the effect of training intervention on FPS correction which mainly recommended concurrent using of strength and stretching exercises along with postural exercises and combining them with other methods such as MFR therapy (as an effective and recommended method along with corrective exercises). By adapting exercises proposed by Katzman et al. [38] and combining them with MFR therapy, we sought to diversify and use combinational techniques, and due to the significant reduction of FSP angle in the posttest and follow-up stages, we can conclude that the program was successful.
As a result, according to the findings of the present study, it is suggested that MFR therapy be used as an effective method in combination with corrective exercises to correct FSP deformity.
Ethical Considerations
Compliance with ethical guidelines
This study has been approved by the National Ethics Committee of Biomedical Research (Code: IR.UT.SPORT.REC.1397.004).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
All authors contributed in designing, running, and writing all parts of the research.
Conflict of interests
The authors declared no conflict of interest.
References
Houglum PA. Therapeutic exercise for athletic injuries. Champaign: Human Kinetics; 2001.
Penha PJ, João SMA, Casarotto RA, Amino CJ, Penteado DC. Postural assessment of girls between 7 and 10 years of age. Clinics. 2005; 60(1):9-16. [DOI:10.1590/S1807-59322005000100004] [PMID]
Neuman D. Kinesiology of the musculoskeletal system: Foundation for rehabilition. London: Mosby; 2010.
Kendall FP, McCreary EK, Provance PG, Rodgers M, Romani WA. Muscles: Testing and function, with posture and pain: Includes a bonus primal anatomy. Philadelphia: Lippincott Williams & Wilkins; 2005.
Savadatti R, Gaude GS. Effect of forward shoulder posture on forced vital capacity-A co-relational study. Indian Journal of Physical Therapy and Occupational Therapy.2011; 5(2):119-23.
Shavandi N SS, Heidarpor R, Sheikh Hoseini R. [The effect of a 7 weeks corrective exercise on thoracic kyphosis in hyper-kyphotic students (Persian)]. Journal of Kurdistan University of Medical Sciences. 2011;13(4): 42-50.
Najafi M, Behpour Q, Qayini S, Younes H. [Effect of tensile-selective corrective exercises on shoulder dislocation in front of elementary school students (Persian)]. Journal of Rehabilitation Sciences. 2012;1(2):54-60.
Hajihosseini E, Norasteh A A, Shamsi A, Daneshmandi H. [The effect of 6 weeks strength training, stretching and comprehensive corrective exercises on forward head incorrect posture (Persian)]. Journal of Modern Rehabilitation. 2016; 9(S1):38-48
Seidi F. [The effect of a 12-week corrective exercises program on forward head and shoulder deformities (Persian)]. Studies in Sport Medicine. 2011; (14):31-44.
Rajabi R. [Laboratory corrective movements (Persian)]. Tehran: University of Tehran; 2016.
Oyama S. Profiling physical characteristics of the swimmer’s shoulder: comparison to baseball pitchers and non-overhead athletes [PhD. dessertation]. Pittsburgh: University of Pittsburgh; 2006.
Hammer W. Posture evaluations, forward head and forward shoulder. Dyna Chir-pract. 2010; 17(18):1-2.
Harman K, Hubley-Kozey CL, Butler H. Effectiveness of an exercise program to improve forward head posture in normal adults: A randomized, controlled 10-week trial. Journal of Manual & Manipulative Therapy. 2005; 13(3):163-76. [DOI:10.1179/106698105790824888]
Andersen CH, Andersen LL, Mortensen OS, Zebis MK, Sjøgaard G. Protocol for shoulder function training reducing musculoskeletal pain in shoulder and neck: A randomized controlled trial. BMC Musculoskeletal Disorders. 2011; 12:14. [DOI:10.1186/1471-2474-12-14] [PMID] [PMCID]
Morningstar MW, Strauchman MN, Weeks DA. Spinal manipulation and anterior headweighting for the correction of forward head posture and cervical hypolordosis: A pilot study. Journal of Chiropractic Medicine. 2003; 2(2):51-4. [DOI:10.1016/S0899-3467(07)60042-1]
Morningstar M. Cervical curve restoration and forward head posture reduction for the treatment of mechanical thoracic pain using the pettibon corrective and rehabilitative procedures. Journal of Chiropractic Medicine. 2002; 1(3):113-5. [DOI:10.1016/S0899-3467(07)60013-5]
Rhanema N, Bambaeichi E, Taghian F, Nazarian AB, Abdolahi M. [Effect of 8 weeks of regular regimens on spinal cord (rectus, spinal scoliosis and lumbar lordosis) in female students (Persian)]. Journal of Isfahan Medical School. 2009; 27(101):676-86.
Zandi S. [Comparison of the effect of a period of corrective exercises on the rehearsal of postural habits and their combination in correcting upper crossover syndrome in 10-11 years old girls (Persian)] [MA. thesis]. Tehran: University of Tehran; 2010.
Prentice WE. Rehabilitation techniques for sports medicine and athletic training. New York: McGraw-Hill; 2004.
Knight CA, Rutledge CR, Cox ME, Acosta M, Hall SJ. Effect of superficial heat, deep heat, and active exercise warm-up on the extensibility of the plantar flexors. Physical Therapy. 2001; 81(6):1206-14. [DOI:10.1093/ptj/81.6.1206]
Funk D, Swank AM, Adams KJ, Treolo D. Efficacy of moist heat pack application over static stretching on hamstring flexibility. The Journal of Strength & Conditioning Research. 2001; 15(1):123-6. [DOI:10.1519/1533-4287(2001)0152.0.CO;2]
Barlow A, Clarke R, Johnson N, Seabourne B, Thomas D, Gal J. Effect of massage of the hamstring muscle group on performance of the sit and reach test. British Journal of Sports Medicine. 2004; 38(3):349-51. [DOI:10.1136/bjsm.2002.003673] [PMID] [PMCID]
Funk DC, Swank AM, Mikla BM, Fagan TA, Farr BK. Impact of prior exercise on hamstring flexibility: A comparison of proprioceptive neuromuscular facilitation and static stretching. The Journal of Strength & Conditioning Research. 2003; 17(3):489-92. [DOI:10.1519/00124278-200308000-00010]
Spernoga SG, Uhl TL, Arnold BL, Gansneder BM. Duration of maintained hamstring flexibility after a one-time, modified hold-relax stretching protocol. Journal of Athletic Training. 2001; 36(1):44-8. [PMID] [PMCID]
Kain J, Martorello L, Swanson E, Sego S. Comparison of an indirect tri-planar Myofascial Release (MFR) technique and a hot pack for increasing range of motion. Journal of Bodywork and Movement Therapies. 2011; 15(1):7-63. [DOI:10.1016/j.jbmt.2009.12.002] [PMID]
Izadkhah S NN, Maarufi N, Kocheili Y, Shabedin H. [Comparison of myofascial release and muscle energy technique effects on hamstring muscle flexibility (Persian)]. Journal of Modern Rehabilitation. 2016; 9(5):131-9.
Łukasik E, Targosiński P, Szymański M, Letkiewicz-Ryłów O, Styczeń P, Wychowański M. Comparing the effectiveness of myofascial techniques with massage in persons with upper crossed syndrome (preliminary report). Advances in Rehabilitation. 2017; 31(2):53-67. [DOI:10.1515/rehab-2015-0067]
Kamali F, Shirazi S, Ebrahimi S, Mirshamsi M, Ghanbari A. Comparison of manual therapy and exercise therapy for postural hyperkyphosis: A randomized clinical trial. Physiotherapy Theory and Practice. 2016; 32(2):92-7. [DOI:10.3109/09593985.2015.1110739] [PMID]
Shojaei P, Hemmatfar A, Behpour N. [The effect of eight weeks of rolling foam training on lumbar lordosis in older men (Persian)]. Journal of Applied Research Sport Science Without Borders. 2017; 1(4):75-88.
Hajihosseini E, Norasteh A, Shamsi A, Daneshmandi H. The effects of strengthening, stretching and comprehensive exercises on forward shoulder posture correction. Physical Treatments-Specific Physical Therapy Journal. 2014; 4(3):123-32.
Rajabi R. [Thoracic Kyphosis, Review of Literature, epidemiology. etiology, cause, evaluation and new corrective methods (Persian)]. Tehran: Tehran University; 2013.
Seidi F, Rajabi R, Ebrahimi E, Alizadeh MH, Minoonejad H. The efficiency of corrective exercise interventions on thoracic hyper-kyphosis angle. Journal of Back and Musculoskeletal Rehabilitation. 2014; 27(1):7-16. [DOI:10.3233/BMR-130411] [PMID]
Seidi F, Rajabi R, Ebrahimi E, Alizadeh MH, Daneshmandi H. [The effect of a 10-week selected corrective exercise program on postural thoracic kyphosis deformity (Persian)]. Sport Medicine (Harakat). 2013; 10:5-22.
Daneshmandi H, Mogharabi Mozafari M. [The effect of eight weeks of comprehensive corrective training on upper cross_syndrome (Persian)]. Journal of Research in Sports Medicine and Technology. 2014; 12(7):75-86.
Thigpen CA, Padua DA, Michener LA, Guskiewicz K, Giuliani C, Keener JD, et al. Head and shoulder posture affect scapular mechanics and muscle activity in overhead tasks. Journal of Electromyography and kinesiology. 2010; 20(4):701-9. [DOI:10.1016/j.jelekin.2009.12.003] [PMID]
Seidi F, Rajabi R, Alizadeh MH, Daneshmandi H. [The effect of a 10-week selected corrective exercise program on postural thoracic kyphosis deformity (Persian)]. Journal of Sport Medicine. 2013; 5(1):5-22. [DOI:10.22059/JSMED.2013.32159]
Hakimipour M, Rajabi R, Minoonejad H, Soltani A. [Reliability of foot photo box in measuring selected footprint indicesا (Persian)]. Journal of Applied Exercise Phycology. 2016; 4(8):122-14.
Katzman W, Vittinghoff E, Kado D, Lane N, Ensrud K, Shipp K. Thoracic kyphosis and rate of incident vertebral fractures: The fracture intervention trial. Osteoporosis International. 2016; 27(3):899-903. [DOI:10.1007/s00198-015-3478-2] [PMID] [PMCID]
Duncan R. Myofascial release. Campaign: Human kinetics. 2014.
Ruivo RM, Pezarat-Correia P, Carita AI. Effects of a Resistance And Stretching Training Program On Forward Head And Protracted Shoulder Posture In Adolescents. Journal of Manipulative and Physiological Therapeutics. 2017; 40(1):1-10. [DOI:10.1016/j.jmpt.2016.10.005] [PMID]
Lynch SS, Thigpen CA, Mihalik JP, Prentice WE, Padua D. The effects of an exercise intervention on forward head and rounded shoulder postures in elite swimmers. British Journal of Sports Medicine. 2010; 44(5):376-81. [DOI:10.1136/bjsm.2009.066837] [PMID]
Kluemper M, Uhl T, Hazelrigg H. Effect of stretching and strengthening shoulder muscles on forward shoulder posture in competitive swimmers. Journal of Sport Rehabilitation. 2006; 15(1):58-70. [DOI:10.1123/jsr.15.1.58]
Jang HJ, Kim MJ, Kim SY. Effect of thorax correction exercises on flexed posture and chest function in older women with age-related hyperkyphosis. Journal of Physical Therapy Science. 2015; 27(4):1161-4. [DOI:10.1589/jpts.27.1161] [PMID] [PMCID]
Frank C, Page P, Lardner R. Assessment and treatment of muscle imbalance: the Janda approach. Campaign: Human kinetics; 2009.
Langevin HM. Connective tissue: A body-wide signaling network? Medical Hypotheses. 2006; 66(6):1074-7. [DOI:10.1016/j.mehy.2005.12.032] [PMID]
Keirns M. Myofascial release in sports medicine. Champaign: Human Kinetics. 2000; 11(3):38-52.
Type of Study: Research |
Subject:
Special
Received: 2018/06/14 | Accepted: 2018/10/16 | Published: 2019/01/1
Received: 2018/06/14 | Accepted: 2018/10/16 | Published: 2019/01/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |