Thu, Nov 13, 2025
Volume 8, Issue 1 (Spring 2018)
PTJ 2018, 8(1): 27-36 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mozafaripour E, Rajabi R, Minoonejad H. Anatomical Alignment of Lower Extremity in Subjects With Genu Valgum and Genu Varum Deformities. PTJ 2018; 8 (1) :27-36
URL: http://ptj.uswr.ac.ir/article-1-351-en.html
URL: http://ptj.uswr.ac.ir/article-1-351-en.html
1- Department of Sports Medicine and Health, Faculty of Physical Education & Sport Sciences, University of Tehran, Tehran, Iran.
Full-Text [PDF 784 kb]
(9101 Downloads)
| Abstract (HTML) (8477 Views)
The results also indicated that tibia vara value was significantly higher in the subjects with genu varum deformity than those with genu valgum deformity and the control group (P≤0.05). However, no significant differences were found between the tibial torsion and external rotation of hip in the study groups (P≥0.05). Prior to the study, a pilot study was conducted on 10 healthy subjects in order to determine the intra-rater reliability of the test. The results indicated high intra-rater reliability for all variables (ICC≤0.84).
4. Discussion
Results of the study indicated that the internal rotation of hip, Q angle, anteversion of hip, hip knee hyperextension and plantar arch index were significantly higher in the subjects with genu valgum deformity, compared to the subjects with genu varum deformity. The results also indicated that tibia vara value was significantly higher in the subjects with genu varum deformity than those with genu valgum deformity. However, no significant differences were found between the tibial torsion and external rotation of hip in the study groups.
Anteversion of hip
The present study indicated that the mean anteversion score of hip was higher in the subjects with genu valgum deformity than the subjects with genu varum deformity and control group (P≤0.05). However, there was no significant difference between the genu varum group and the controls (P≥0.05).
Anteversion of hip is the angle formed between the head and neck of femur with condylar axis of the hip. If this angle increases, femur loses its stability in the acetabulum and inclines toward the outer side of acetabulum. In order to recover this position and restore femur into acetabulum and increase stability, a person with increased anteversion gives a compensatory internal rotation to femur [24, 25]. It may disrupt the natural alignment of the knees and make the distal end of femur and subsequently the whole knee joint come closer to the midline of the body, forcing the knees to valgus position and causing genu valgum deformity-over time. Results of the present study are consistent with the findings of Magee (2013), who reported increased anteversion in the subjects with genu valgum deformity [25]. No study was found examining this factor in the subjects with these deformities.
Internal and external rotation
The results indicated that internal rotation was significantly higher in genu valgum group than the genu varum group (P≤0.05). However, there was no significant difference between the values of this variable in other groups (P≥0.05).
Lawrence et al. (2008) reported that the strength of external rotator muscles is associated with internal rotation of hip and these muscles control the internal rotation of hip by applying eccentric force and reduce it [26]. In consistent with our findings, other studies have also reported the direct relationship between reduced strength of these muscles and increased internal rotation and adduction of hip [27, 28]. Studies suggested that the increased internal rotation of hip in the people with genu valgum deformity is due to the weakness of external rotator muscles, and decreased strength of these muscles in such people reduces their control on the internal rotation of hip, leading to increased amount of this factor in this group.
Movements like the internal and external rotation of hip, which occur in opposite directions, are interdependent, and an increase in the range of motion of each will subsequently decrease the range of motion of the other one. According to the present study, the subjects with genu valgum deformity had more internal rotation of hip than the genu varum deformity group. Thus, such increase in the internal rotation of hip was expected to decrease external rotation of hip in this group. Although external rotation was higher in the subjects with genu varum deformity than those with genu valgum deformity, the difference was not statistically significant.
Q angle and plantar arch index
Results of the present study indicated that Q angle was significantly higher in the subjects with genu valgum deformity than those with genu varum deformity and the control group (P≤0.05). The obtained results also indicated that the mean score of plantar arch index was significantly higher in the subjects with genu valgum deformity than those with genu varum deformity (P≤0.05). Based on the theory of kinetic chain, the changes in one segment or part of body may cause changes in other parts of the body and affect their status. According to this theory, reduced plantar arch results in the internal rotation of tibia, making the knees undergo a valgus position and the hips rotate internally. For this reason and because of decreased plantar arch in the subjects with genu valgum deformity, their knees undergo valgus position and displace internally, leading to increased Q angle in them [29, 30].
Neumann et al. (2010), Magee (2008), Schamberger et al. (2012), and Riegger (1996) have noted flatfoot and increased Q angle in people with genu valgum deformity [11, 25, 31, 32].
Knee hyperextension
Results of the study indicated that knee hyperextension was significantly higher in the subjects with genu valgum deformity than those with genu varum deformity and the controls (P≤0.05). This suggests that knee joint has more extension in this group. This study indicated that the internal rotation of hip was found in the subjects with genu valgum deformity. This could likely make gluteal muscles undergo a stretched position in this group, which leads to the weakness of these muscles, resulting in further extension in knees of such subjects, compared to other groups [9, 19].
Tibial torsion
The obtained results indicated no significant differences between tibial torsion in the subjects with genu varum deformity and those with genu valgum and control group (P≥0.05). No study was found consistent with the present research, indicating a lack of significant difference in tibial torsion in the subjects with genu valgum deformity and those with genu varum deformity. However, some textbooks, described the compensatory internal or external rotation of tibia in the subjects with genu valgum and genu varum deformities [9-11, 31, 32]. However, the findings of the present study are inconsistent with the ideas of these authors.
Most researchers have suggested that in genu valgum and genu varum deformities, tibia will have compensatory torsion in the opposite direction of hip rotation [9, 25, 31]. The researcher, therefore, is expected to observe a compensatory external torsion in the subjects with genu valgum deformity due to increased internal rotation of hip. However, this was not the case and no difference was found between tibial torsion in the subjects with genu valgum deformity and those with genu varum deformity and control group.
The researchers have no compelling reason why there was no tibial compensatory process in the people with genu valgum deformity. Therefore, future studies should be conducted to clarify the issue. Finally, tibial torsion should be assessed and measured individually, in order to detect possible changes in tibial torsion in people with such deformities. Therefore, the mechanism of the changes occurred in the individual’s tibia, if any, could be revealed and the risks of probable damages threatening them could be identified.
Tibia vara
Based on this study, the mean score of tibia vara is significantly higher in the subjects with genu varum deformity than those with genu valgum deformity and control group (P≤0.05). Although the mean score of tibia vara was lower in the subjects with genu valgum deformity than the control group, no significant difference was found between these two groups (P≥0.05).
Tibia vara is the angle between the axis perpendicular to the plane and distal one-third of tibia, indicating curvature or arcuate shape of tibia [22]. One of the main causes of tibia vara in lower extremity is unbalanced mechanical stress exerted on the internal and external parts of tibia [33, 34]. When genu varum deformity occurs, legs get away from each other, subsequently making the proximal end of tibia distant from the midline of the body. In this condition, pressure on tibia is not distributed equally at its length and its inner part experiences more pressure than its outer parts [35].
The pressure on tibia and far distance of proximal one-third of tibia from the midline of the body may increase the amount of curvature or increase tibia vara in the people with genu varum deformity. It should be noted that increased tibia vara may occur during childhood due to some nutritional problems and some diseases like Blount’s disease [34, 36]. In this case, increased curvature of tibia may make the knees of the child distant from each other and expose the child to a risk of genu varum deformity. Finally, it can be argued that increased tibia vara is a characteristic change observed with genu varum deformity, whether genu varum deformity increases tibia vara or vice versa.
Based on the study results, the changes occurring in lower extremity alignment in the subjects with genu valgum deformity include increased anteversion, increased hip internal rotation ( compared to the subjects with genu varum), increased Q angle, increased knee hyperextension, and more flatfoot (compared to the subjects with genu varum). In addition, the changes occurring in lower extremity alignment of the people with genu varum deformity include decreased internal rotation of hip (compared to the subjects with genu valgum), increased tibia vara, and high arch (compared to the subjects with genu valgum). The main limitation of the present study is the lack of related articles. Therefore, the required information was gained by related books of Orthopedic and kinesiology.
The present research is among the few studies examining the changes of lower extremity alignment in genu valgum and genu varum deformities. Thus, the obtained data can be used as a reference in prescription of exercise in this population.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles were considered in this article. The participants were informed about the purpose of the research and its implementation stages; they were also assured about the confidentiality of their information; Moreover, They were allowed to leave the study whenever they wish, and if desired, the results of the research would be available to them.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors contributions
Conceptualization, Methodology, and Investigation: All authors; Writing-Original Draft: Esmaeil Mozafaripour; Writing-Review & Editing: Reza Rajabi and Hooman Minoonejad; Funding Acquisition and Resources: All authors; Supervision: Reza Rajabi and Hooman Minoonejad.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
Authors appreciate Tehran University authorities for their cooperation in conducting this study.
References
Full-Text: (6325 Views)
1. Introduction
Changes in lower extremity alignment have always been considered as an important risk factor in the development of acute and chronic injuries of lower extremity such as patellofemoral pain syndrome, Anterior Cruciate Ligament (ACL) injury, stress fracture, and plantar fasciitis [1, 2]. It is believed that biomechanical changes combined with the above-mentioned changes lead to changes in the amount and direction of forces applied to the joint, changes in proprioception, and muscle activation patterns. These factors decrease lower extremity neuromuscular control , exposing this part of the body to injury [3].
The lower extremity injuries related to changes in lower extremity alignment have been widely investigated in previous studies [4-8]. The relationships between such changes and injuries of this segment are clearly documented in the existing studies. Genu varum and genu valgum deformities are frequent anomalies of lower extremity that are associated with many anatomical changes in knee joint and its adjacent segments, which expose the people with such anomalies to acute and chronic injuries.
Data are insufficient on anatomical changes occurring in this joint and its adjacent joints and segments following such an anomaly. For example, Sahrmann et al. (2010) has noted internal rotation of hip, external rotation of tibia, and probability of supination or pronation of foot as changes in the subjects with genu valgum, and internal rotation of hip, knee hyperextension, tibia vara, and supination of foot as changes in the subjects with genu varum [9]. Similarly, Levangie and Norkin (2011) recognized the internal rotation of hip, external rotation of tibia, and pronated foot for the changes in lower extremity alignment in genu varum deformity. However, they disregarded the subsequent changes of genu valgum deformity [10].
Regarding the changes in genu valgum, Neumann (2010) noted internal rotation of tibia and pronation of foot as the concomitant changes. However, they overlooked the changes in lower extremity in the subjects with genu varum deformity [11]. According to the literature, there is no consensus among researchers about the changes in lower extremity alignment in the subjects with such deformities. Also, investigations failed to thoroughly examine the subsequent changes of these deformities. Therefore, the present study aimed to investigate the changes in lower extremity alignment in the subjects with genu varum and genu valgum deformities.
We also compared the samples with the healthy population as well as with each other, in order to determine the subsequent changes of these deformities. As a result, lower extremity alignment was investigated by foot arch index, tibia vara, the rotation of tibia, knee hyperextension, Q angle, the internal and external rotation of hip, and anteversion of hip in the study groups.
2. Materials and Methods
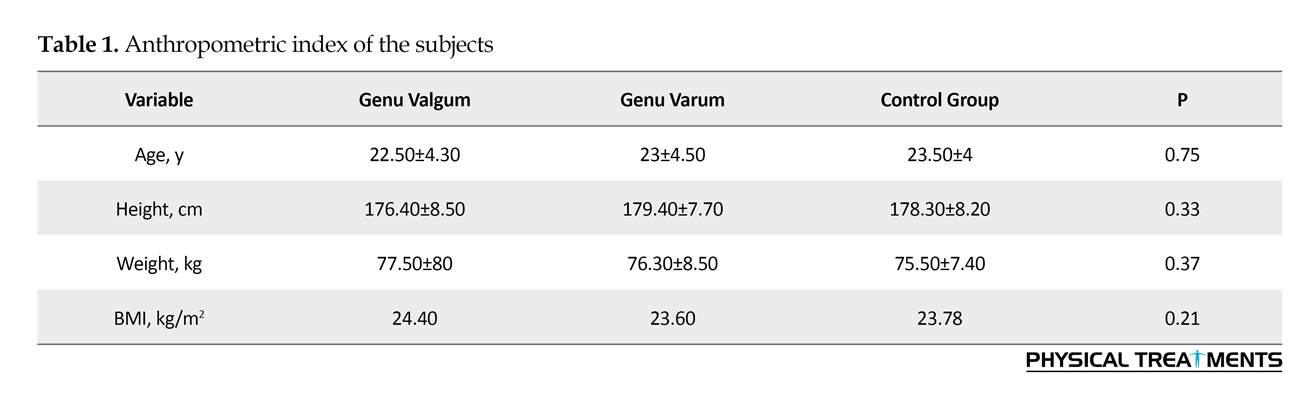
The statistical sample of the study comprised 120 students aged 18-26 years from Tehran University. The subjects were assigned into 3 groups based on inclusion criteria and by convenience sampling method (40 to genu varum, 40 to genu valgum, and 40 to healthy subject groups). The anthropometric characteristics of the subjects are presented in Table 1. Exclusion criteria included histories of surgery, fracture or dislocation in lower extremity, pain in any part of the body on the test day, severe muscular soreness in lower extremity on the test day, evident anomaly in the hip and spinal column of the subjects, such as increased kyphosis, increased lordosis and scoliosis, and apparent difference in the length of leg, greater than 2 cm in each subject [12, 13].
Each subject signed the consent form prior to study participation. Furthermore, this study was approved by the Ethics Committee of Tehran University. For evaluating and assigning the subjects to genu varum and genu valgum groups, they were requested to stand barefoot against the wall in anatomical position, with heels, hips and upper backs contacting the wall. Then, they were requested to bring their legs close to each other. The subject was assigned to genu varum group if the distance between internal condyles of knee was more than 3 cm and subject was assigned to genu valgum group if the distance between the internal malleoli of ankle was more than 3 cm. The subject was assigned to the healthy group, if the distance between malleoli and internal condyles was less than 3 cm [14, 15].
Lower extremity alignment was measured for the anteversion of hip, internal rotation of hip, external rotation of hip, Q angle, knee hyperextension, tibial torsion, tibia vara, and foot arch index. All measurements were done by goniometer and each variable was measured three times and an average of three measurements was recorded. All measurements related to the variables were performed by a single examiner to eliminate inter-rater bias. Prior to the study, a pilot study was conducted on 10 healthy subjects in order to determine the intra-rater reliability of the test.
Assessment tools
Anteversion of hip
Craig’s Test was used to measure the anteversion of hip. The subjects were requested to lie prone and hold the knee at 90º flexion. Then, the examiner touched the posterior part of greater trochanter and passively rotated the subject’s hip until the greater trochanter was parallel with the examination table (at this moment, the femur neck was parallel with surface of table). The angle between the vertical line and shaft of tibia was recorded as the extent of anteversion of hip for each subject [8, 16] (Figure 1).
Changes in lower extremity alignment have always been considered as an important risk factor in the development of acute and chronic injuries of lower extremity such as patellofemoral pain syndrome, Anterior Cruciate Ligament (ACL) injury, stress fracture, and plantar fasciitis [1, 2]. It is believed that biomechanical changes combined with the above-mentioned changes lead to changes in the amount and direction of forces applied to the joint, changes in proprioception, and muscle activation patterns. These factors decrease lower extremity neuromuscular control , exposing this part of the body to injury [3].
The lower extremity injuries related to changes in lower extremity alignment have been widely investigated in previous studies [4-8]. The relationships between such changes and injuries of this segment are clearly documented in the existing studies. Genu varum and genu valgum deformities are frequent anomalies of lower extremity that are associated with many anatomical changes in knee joint and its adjacent segments, which expose the people with such anomalies to acute and chronic injuries.
Data are insufficient on anatomical changes occurring in this joint and its adjacent joints and segments following such an anomaly. For example, Sahrmann et al. (2010) has noted internal rotation of hip, external rotation of tibia, and probability of supination or pronation of foot as changes in the subjects with genu valgum, and internal rotation of hip, knee hyperextension, tibia vara, and supination of foot as changes in the subjects with genu varum [9]. Similarly, Levangie and Norkin (2011) recognized the internal rotation of hip, external rotation of tibia, and pronated foot for the changes in lower extremity alignment in genu varum deformity. However, they disregarded the subsequent changes of genu valgum deformity [10].
Regarding the changes in genu valgum, Neumann (2010) noted internal rotation of tibia and pronation of foot as the concomitant changes. However, they overlooked the changes in lower extremity in the subjects with genu varum deformity [11]. According to the literature, there is no consensus among researchers about the changes in lower extremity alignment in the subjects with such deformities. Also, investigations failed to thoroughly examine the subsequent changes of these deformities. Therefore, the present study aimed to investigate the changes in lower extremity alignment in the subjects with genu varum and genu valgum deformities.
We also compared the samples with the healthy population as well as with each other, in order to determine the subsequent changes of these deformities. As a result, lower extremity alignment was investigated by foot arch index, tibia vara, the rotation of tibia, knee hyperextension, Q angle, the internal and external rotation of hip, and anteversion of hip in the study groups.
2. Materials and Methods
The statistical sample of the study comprised 120 students aged 18-26 years from Tehran University. The subjects were assigned into 3 groups based on inclusion criteria and by convenience sampling method (40 to genu varum, 40 to genu valgum, and 40 to healthy subject groups). The anthropometric characteristics of the subjects are presented in Table 1. Exclusion criteria included histories of surgery, fracture or dislocation in lower extremity, pain in any part of the body on the test day, severe muscular soreness in lower extremity on the test day, evident anomaly in the hip and spinal column of the subjects, such as increased kyphosis, increased lordosis and scoliosis, and apparent difference in the length of leg, greater than 2 cm in each subject [12, 13].
Each subject signed the consent form prior to study participation. Furthermore, this study was approved by the Ethics Committee of Tehran University. For evaluating and assigning the subjects to genu varum and genu valgum groups, they were requested to stand barefoot against the wall in anatomical position, with heels, hips and upper backs contacting the wall. Then, they were requested to bring their legs close to each other. The subject was assigned to genu varum group if the distance between internal condyles of knee was more than 3 cm and subject was assigned to genu valgum group if the distance between the internal malleoli of ankle was more than 3 cm. The subject was assigned to the healthy group, if the distance between malleoli and internal condyles was less than 3 cm [14, 15].
Lower extremity alignment was measured for the anteversion of hip, internal rotation of hip, external rotation of hip, Q angle, knee hyperextension, tibial torsion, tibia vara, and foot arch index. All measurements were done by goniometer and each variable was measured three times and an average of three measurements was recorded. All measurements related to the variables were performed by a single examiner to eliminate inter-rater bias. Prior to the study, a pilot study was conducted on 10 healthy subjects in order to determine the intra-rater reliability of the test.
Assessment tools
Anteversion of hip
Craig’s Test was used to measure the anteversion of hip. The subjects were requested to lie prone and hold the knee at 90º flexion. Then, the examiner touched the posterior part of greater trochanter and passively rotated the subject’s hip until the greater trochanter was parallel with the examination table (at this moment, the femur neck was parallel with surface of table). The angle between the vertical line and shaft of tibia was recorded as the extent of anteversion of hip for each subject [8, 16] (Figure 1).
Internal and external rotation of hip
These parameters were measured while the subject was sitting on the table, with his knee and hip at 90º flexion. The subject was then instructed to perform internal and external rotation up to the end of the range of motion. In this position, the movable goniometer arm was placed on tibia and its fixed arm on the ground perpendicularly. The formed angle was recorded as the internal and external rotation of hip [8].
Q angle
To measure this angle, the line connecting ASIS (anterior superior iliac spine) to the center of patella and also the line connecting anterior tibial tuberosity to the center of patella were drawn, and goniometer center was placed in the center of patella, goniometer arms were placed along with the drawn lines, and the formed angle was recorded as the Q angle for each subject [8, 17, 18].
Knee hyperextension
To measure it, the subject was requested to keep a normal standing position. Then the center of goniometer was placed on femoral epicondyle and its arms were placed parallel to greater trochanter of hip and the central line of lateral section of tibia. The formed angle was recorded as knee hyperextension [8, 19].
Tibial torsion
Tight-foot method was used to measure tibial torsion in this study. The subject was lying prone on the table, the knee joint was placed at 90º flexion, and the center of the heel was marked in plantar surface of the foot, from which a line was drawn to the middle of the foot, then a line dividing the hip into 2 equal halves was drawn. The angle between the 2 lines was recorded as tibial torsion angle [8, 20, 21] (Figure 2).
Tibia vara
To measure tibia vara, the subject was requested to stand on one single leg, keep the toes of opposite foot in contact with the floor in order to keep balance, and look at a point in the front. Then, the examiner stood behind the subject, detected the line dividing the posterior part of the leg into 2 equal halves, and drew a line from upper two-third of the leg to the top of the ankle. The angle formed between this line and the floor was recorded as the extent of tibia vara [22] (Figure 3).
Plantar arch index
Staheli Method was used to measure the plantar arch in the subjects. First, a sufficient amount of talcum powder was sprayed on a plate prepared in advance. The subject was asked to start walking normally a few meters away from the plate, put his foot on it and pass. Then, the narrowest point of the forefoot and the widest point of the heel of each foot were determined from the footprint on the plate. Next, the Staheli index was calculated by dividing the narrowest point of the barefoot by the widest point of the heel [23].
Statistical analysis
The mean and standard deviation were used to describe the data. The obtained data were analyzed by SPSS. One-way Analysis of Variance (ANOVA) was also used. After determining significance, Tukey test was used to find differences between the groups. Significance level was set at P≤0.05.
3. Results
Anthropometric index values are presented in Table 1. According to the results of present study presented in Tables 2 and 3, the internal rotation of hip, Q angle, anteversion of hip, knee hyperextension and plantar arch index were significantly higher in the subjects with genu valgum deformity, as compared to the subjects with genu varum deformity. Moreover, Q angle value, the anteversion of hip and knee hyperextension were significantly higher in genu valgum group than the controls (P≤0.05).
These parameters were measured while the subject was sitting on the table, with his knee and hip at 90º flexion. The subject was then instructed to perform internal and external rotation up to the end of the range of motion. In this position, the movable goniometer arm was placed on tibia and its fixed arm on the ground perpendicularly. The formed angle was recorded as the internal and external rotation of hip [8].
Q angle
To measure this angle, the line connecting ASIS (anterior superior iliac spine) to the center of patella and also the line connecting anterior tibial tuberosity to the center of patella were drawn, and goniometer center was placed in the center of patella, goniometer arms were placed along with the drawn lines, and the formed angle was recorded as the Q angle for each subject [8, 17, 18].
Knee hyperextension
To measure it, the subject was requested to keep a normal standing position. Then the center of goniometer was placed on femoral epicondyle and its arms were placed parallel to greater trochanter of hip and the central line of lateral section of tibia. The formed angle was recorded as knee hyperextension [8, 19].
Tibial torsion
Tight-foot method was used to measure tibial torsion in this study. The subject was lying prone on the table, the knee joint was placed at 90º flexion, and the center of the heel was marked in plantar surface of the foot, from which a line was drawn to the middle of the foot, then a line dividing the hip into 2 equal halves was drawn. The angle between the 2 lines was recorded as tibial torsion angle [8, 20, 21] (Figure 2).
Tibia vara
To measure tibia vara, the subject was requested to stand on one single leg, keep the toes of opposite foot in contact with the floor in order to keep balance, and look at a point in the front. Then, the examiner stood behind the subject, detected the line dividing the posterior part of the leg into 2 equal halves, and drew a line from upper two-third of the leg to the top of the ankle. The angle formed between this line and the floor was recorded as the extent of tibia vara [22] (Figure 3).
Plantar arch index
Staheli Method was used to measure the plantar arch in the subjects. First, a sufficient amount of talcum powder was sprayed on a plate prepared in advance. The subject was asked to start walking normally a few meters away from the plate, put his foot on it and pass. Then, the narrowest point of the forefoot and the widest point of the heel of each foot were determined from the footprint on the plate. Next, the Staheli index was calculated by dividing the narrowest point of the barefoot by the widest point of the heel [23].
Statistical analysis
The mean and standard deviation were used to describe the data. The obtained data were analyzed by SPSS. One-way Analysis of Variance (ANOVA) was also used. After determining significance, Tukey test was used to find differences between the groups. Significance level was set at P≤0.05.
3. Results
Anthropometric index values are presented in Table 1. According to the results of present study presented in Tables 2 and 3, the internal rotation of hip, Q angle, anteversion of hip, knee hyperextension and plantar arch index were significantly higher in the subjects with genu valgum deformity, as compared to the subjects with genu varum deformity. Moreover, Q angle value, the anteversion of hip and knee hyperextension were significantly higher in genu valgum group than the controls (P≤0.05).
The results also indicated that tibia vara value was significantly higher in the subjects with genu varum deformity than those with genu valgum deformity and the control group (P≤0.05). However, no significant differences were found between the tibial torsion and external rotation of hip in the study groups (P≥0.05). Prior to the study, a pilot study was conducted on 10 healthy subjects in order to determine the intra-rater reliability of the test. The results indicated high intra-rater reliability for all variables (ICC≤0.84).
4. Discussion
Results of the study indicated that the internal rotation of hip, Q angle, anteversion of hip, hip knee hyperextension and plantar arch index were significantly higher in the subjects with genu valgum deformity, compared to the subjects with genu varum deformity. The results also indicated that tibia vara value was significantly higher in the subjects with genu varum deformity than those with genu valgum deformity. However, no significant differences were found between the tibial torsion and external rotation of hip in the study groups.
Anteversion of hip
The present study indicated that the mean anteversion score of hip was higher in the subjects with genu valgum deformity than the subjects with genu varum deformity and control group (P≤0.05). However, there was no significant difference between the genu varum group and the controls (P≥0.05).
Anteversion of hip is the angle formed between the head and neck of femur with condylar axis of the hip. If this angle increases, femur loses its stability in the acetabulum and inclines toward the outer side of acetabulum. In order to recover this position and restore femur into acetabulum and increase stability, a person with increased anteversion gives a compensatory internal rotation to femur [24, 25]. It may disrupt the natural alignment of the knees and make the distal end of femur and subsequently the whole knee joint come closer to the midline of the body, forcing the knees to valgus position and causing genu valgum deformity-over time. Results of the present study are consistent with the findings of Magee (2013), who reported increased anteversion in the subjects with genu valgum deformity [25]. No study was found examining this factor in the subjects with these deformities.
Internal and external rotation
The results indicated that internal rotation was significantly higher in genu valgum group than the genu varum group (P≤0.05). However, there was no significant difference between the values of this variable in other groups (P≥0.05).
Lawrence et al. (2008) reported that the strength of external rotator muscles is associated with internal rotation of hip and these muscles control the internal rotation of hip by applying eccentric force and reduce it [26]. In consistent with our findings, other studies have also reported the direct relationship between reduced strength of these muscles and increased internal rotation and adduction of hip [27, 28]. Studies suggested that the increased internal rotation of hip in the people with genu valgum deformity is due to the weakness of external rotator muscles, and decreased strength of these muscles in such people reduces their control on the internal rotation of hip, leading to increased amount of this factor in this group.
Movements like the internal and external rotation of hip, which occur in opposite directions, are interdependent, and an increase in the range of motion of each will subsequently decrease the range of motion of the other one. According to the present study, the subjects with genu valgum deformity had more internal rotation of hip than the genu varum deformity group. Thus, such increase in the internal rotation of hip was expected to decrease external rotation of hip in this group. Although external rotation was higher in the subjects with genu varum deformity than those with genu valgum deformity, the difference was not statistically significant.
Q angle and plantar arch index
Results of the present study indicated that Q angle was significantly higher in the subjects with genu valgum deformity than those with genu varum deformity and the control group (P≤0.05). The obtained results also indicated that the mean score of plantar arch index was significantly higher in the subjects with genu valgum deformity than those with genu varum deformity (P≤0.05). Based on the theory of kinetic chain, the changes in one segment or part of body may cause changes in other parts of the body and affect their status. According to this theory, reduced plantar arch results in the internal rotation of tibia, making the knees undergo a valgus position and the hips rotate internally. For this reason and because of decreased plantar arch in the subjects with genu valgum deformity, their knees undergo valgus position and displace internally, leading to increased Q angle in them [29, 30].
Neumann et al. (2010), Magee (2008), Schamberger et al. (2012), and Riegger (1996) have noted flatfoot and increased Q angle in people with genu valgum deformity [11, 25, 31, 32].
Knee hyperextension
Results of the study indicated that knee hyperextension was significantly higher in the subjects with genu valgum deformity than those with genu varum deformity and the controls (P≤0.05). This suggests that knee joint has more extension in this group. This study indicated that the internal rotation of hip was found in the subjects with genu valgum deformity. This could likely make gluteal muscles undergo a stretched position in this group, which leads to the weakness of these muscles, resulting in further extension in knees of such subjects, compared to other groups [9, 19].
Tibial torsion
The obtained results indicated no significant differences between tibial torsion in the subjects with genu varum deformity and those with genu valgum and control group (P≥0.05). No study was found consistent with the present research, indicating a lack of significant difference in tibial torsion in the subjects with genu valgum deformity and those with genu varum deformity. However, some textbooks, described the compensatory internal or external rotation of tibia in the subjects with genu valgum and genu varum deformities [9-11, 31, 32]. However, the findings of the present study are inconsistent with the ideas of these authors.
Most researchers have suggested that in genu valgum and genu varum deformities, tibia will have compensatory torsion in the opposite direction of hip rotation [9, 25, 31]. The researcher, therefore, is expected to observe a compensatory external torsion in the subjects with genu valgum deformity due to increased internal rotation of hip. However, this was not the case and no difference was found between tibial torsion in the subjects with genu valgum deformity and those with genu varum deformity and control group.
The researchers have no compelling reason why there was no tibial compensatory process in the people with genu valgum deformity. Therefore, future studies should be conducted to clarify the issue. Finally, tibial torsion should be assessed and measured individually, in order to detect possible changes in tibial torsion in people with such deformities. Therefore, the mechanism of the changes occurred in the individual’s tibia, if any, could be revealed and the risks of probable damages threatening them could be identified.
Tibia vara
Based on this study, the mean score of tibia vara is significantly higher in the subjects with genu varum deformity than those with genu valgum deformity and control group (P≤0.05). Although the mean score of tibia vara was lower in the subjects with genu valgum deformity than the control group, no significant difference was found between these two groups (P≥0.05).
Tibia vara is the angle between the axis perpendicular to the plane and distal one-third of tibia, indicating curvature or arcuate shape of tibia [22]. One of the main causes of tibia vara in lower extremity is unbalanced mechanical stress exerted on the internal and external parts of tibia [33, 34]. When genu varum deformity occurs, legs get away from each other, subsequently making the proximal end of tibia distant from the midline of the body. In this condition, pressure on tibia is not distributed equally at its length and its inner part experiences more pressure than its outer parts [35].
The pressure on tibia and far distance of proximal one-third of tibia from the midline of the body may increase the amount of curvature or increase tibia vara in the people with genu varum deformity. It should be noted that increased tibia vara may occur during childhood due to some nutritional problems and some diseases like Blount’s disease [34, 36]. In this case, increased curvature of tibia may make the knees of the child distant from each other and expose the child to a risk of genu varum deformity. Finally, it can be argued that increased tibia vara is a characteristic change observed with genu varum deformity, whether genu varum deformity increases tibia vara or vice versa.
Based on the study results, the changes occurring in lower extremity alignment in the subjects with genu valgum deformity include increased anteversion, increased hip internal rotation ( compared to the subjects with genu varum), increased Q angle, increased knee hyperextension, and more flatfoot (compared to the subjects with genu varum). In addition, the changes occurring in lower extremity alignment of the people with genu varum deformity include decreased internal rotation of hip (compared to the subjects with genu valgum), increased tibia vara, and high arch (compared to the subjects with genu valgum). The main limitation of the present study is the lack of related articles. Therefore, the required information was gained by related books of Orthopedic and kinesiology.
The present research is among the few studies examining the changes of lower extremity alignment in genu valgum and genu varum deformities. Thus, the obtained data can be used as a reference in prescription of exercise in this population.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles were considered in this article. The participants were informed about the purpose of the research and its implementation stages; they were also assured about the confidentiality of their information; Moreover, They were allowed to leave the study whenever they wish, and if desired, the results of the research would be available to them.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors contributions
Conceptualization, Methodology, and Investigation: All authors; Writing-Original Draft: Esmaeil Mozafaripour; Writing-Review & Editing: Reza Rajabi and Hooman Minoonejad; Funding Acquisition and Resources: All authors; Supervision: Reza Rajabi and Hooman Minoonejad.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
Authors appreciate Tehran University authorities for their cooperation in conducting this study.
References
- Hertel J, Dorfman JH, Braham RA. Lower extremity malalignments and anterior cruciate ligament injury history. Journal of Sports Science & Medicine. 2004; 3(4):220-5. [PMID] [PMCID]
- Powers CM, Chen PY, Reischl SF, Perry J. Comparison of foot pronation and lower extremity rotation in persons with and without patellofemoral pain. Foot & Ankle International. 2002; 23(7):634-40. [DOI:10.1177/107110070202300709] [PMID]
- Shultz SJ, Carcia CR, Gansneder BM, Perrin DH. The independent and interactive effects of navicular drop and quadriceps angle on neuromuscular responses to a weight-bearing perturbation. Journal of Athletic Training. 2006; 41(3):251-9. [PMID] [PMCID]
- Meyer EG, Haut RC. Anterior cruciate ligament injury induced by internal tibial torsion or tibiofemoral compression. Journal of Biomechanics. 2008; 41(16):3377-83. [DOI:10.1016/j.jbiomech.2008.09.023] [PMID]
- Kaneko M, Sakuraba K. Association between femoral anteversion and lower extremity posture upon single-leg landing: Implications for anterior cruciate ligament injury. Journal of Physical Therapy Science. 2013; 25(10):1213-7. [DOI:10.1589/jpts.25.1213] [PMID] [PMCID]
- Bonci CM. Assessment and evaluation of predisposing factors to anterior cruciate ligament injury. Journal of Athletic Training. 1999; 34(2):155-64. [PMID] [PMCID]
- Nyland J, Kuzemchek S, Parks M, Caborn DN. Femoral anteversion influences vastus medialis and gluteus medius EMG amplitude: Composite hip abductor EMG amplitude ratios during isometric combined hip abduction-external rotation. Journal of Electromyography and Kinesiology. 2004; 14(2):255-61. [DOI:10.1016/S1050-6411(03)00078-6]
- Amraee D, Alizadeh MH, Razi M, Yazdi HR, Minoonejad H. Risk factors associated with noncontact injuries of the anterior cruciate ligament in male athletes. Minerva Ortopedica e Traumatologica. 2013; 64(4):435-44.
- Sahrmann S. Movement system impairment syndromes of the extremities, cervical and thoracic spines. Amsterdam: Elsevier Health Sciences; 2011.
- Levangie PK, Norkin CC. Joint structure and function: A comprehensive analysis. Philadelphia, Pennsylvania: FA Davis; 2011. [PMID]
- Neumann DA. Kinesiology of the musculoskeletal system-e-book: Foundations for rehabilitation. Amsterdam: Elsevier Health Sciences; 2013.
- Papaioannou T, Stokes I, Kenwright J. Scoliosis associated with limb-length inequality. Journal of Bone and Joint Surgery. 1982; 64(1):59-62. [DOI:10.2106/00004623-198264010-00009] [PMID]
- Steen H, Terjesen T, Bjerkreim I. [Anisomelia: Clinical consequences and treatment (Danish)]. Journal for the Norwegian Medical Association: Journal for Practical Medicine, New Series. 1997; 117(11):1595-600.
- Samaei A, Bakhtiary AH, Elham F, Rezasoltani A. Effects of genu varum deformity on postural stability. International Journal of Sports Medicine. 2012; 33(06):469-73. [DOI:10.1055/s-0031-1301331] [PMID]
- Palastanga N, Field D, Soames R. Anatomy and human movement: Structure and function. Amsterdam: Elsevier Health Sciences; 2006.
- Piva SR, Fitzgerald K, Irrgang JJ, Jones S, Hando BR, Browder DA, et al. Reliability of measures of impairments associated with patellofemoral pain syndrome. BMC Musculoskeletal Disorders. 2006; 7(1):33. [DOI:10.1186/1471-2474-7-33] [PMID] [PMCID]
- Emami MJ, Ghahramani MH, Abdinejad F, Namazi H. Q-angle: An invaluable parameter for evaluation of anterior knee pain. Archives of Iranian Medicine. 2007; 10(1):24-6. [PMID]
- Greene CC, Edwards TB, Wade MR, Carson EW. Reliability of the quadriceps angle measurement. The American Journal of Knee Surgery. 2001; 14(2):97-103. [PMID]
- Loudon JK. Measurement of knee-joint-position sense in women with genu recurvatum. Journal of Sport Rehabilitation. 2000; 9(1):15-25. [DOI:10.1123/jsr.9.1.15]
- Kwon OY, Tuttle LJ, Commean PK, Mueller MJ. Reliability and validity of measures of hammer toe deformity angle and tibial torsion. The Foot. 2009; 19(3):149-55. [DOI:10.1016/j.foot.2009.03.004] [PMID] [PMCID]
- Lee SH, Chung CY, Park MS, Choi IH, Cho TJ. Tibial torsion in cerebral palsy: Validity and reliability of measurement. Clinical Orthopaedics and Related Research. 2009; 467(8):2098-104. [DOI:10.1007/s11999-009-0705-1] [PMID] [PMCID]
- Lohmann KN, Rayhel HE, Schneiderwind WP, Danoff JV. Static measurement of tibia vara: Reliability and effect of lower extremity position. Physical Therapy. 1987; 67(2):196-9. [DOI:10.1093/ptj/67.2.196] [PMID]
- Staheli LT, Chew DE, Corbett MA. The longitudinal arch: A survey of eight hundred and eighty-two feet in normal children and adults. The Journal of Bone and Joint Surgery; American Volume. 1987; 69(3):426-8. [PMID]
- Tönnis D, Heinecke A. Acetabular and femoral anteversion: Relationship with osteoarthritis of the hip. The Journal of Bone and Joint Surgery. 1999; 81(12):1747-70. [DOI:10.2106/00004623-199912000-00014] [PMID]
- Magee DJ. Orthopedic physical assessment. Amsterdam: Elsevier Health Sciences; 2008.
- Lawrence III RK, Kernozek TW, Miller EJ, Torry MR, Reuteman P. Influences of hip external rotation strength on knee mechanics during single-leg drop landings in females. Clinical Biomechanics. 2008; 23(6):806-13. [DOI:10.1016/j.clinbiomech.2008.02.009] [PMID]
- Nguyen AD, Shultz SJ, Schmitz RJ, Luecht RM, Perrin DH. A preliminary multifactorial approach describing the relationships among lower extremity alignment, hip muscle activation, and lower extremity joint excursion. Journal of Athletic Training. 2011; 46(3):246-56. [DOI:10.4085/1062-6050-46.3.246] [PMID] [PMCID]
- Bell DR, Oates DC, Clark MA, Padua DA. Two-and 3-dimensional knee valgus are reduced after an exercise intervention in young adults with demonstrable valgus during squatting. Journal of Athletic Training. 2013; 48(4):442-9. [DOI:10.4085/1062-6050-48.3.16] [PMID] [PMCID]
- Frank C, Page P, Lardner R. Assessment and treatment of muscle imbalance: The Janda approach. Champaign, Illinois: Human kinetics; 2009.
- Bell DR, Padua DA, Clark MA. Muscle strength and flexibility characteristics of people displaying excessive medial knee displacement. Archives of Physical Medicine and Rehabilitation. 2008; 89(7):1323-8. [DOI:10.1016/j.apmr.2007.11.048] [PMID]
- Shamberger W. The malalignment syndrome: Implications for medicine and sport. Amsterdam: Elsevier Health Sciences; 2012.
- Riegger-Krugh C, Keysor JJ. Skeletal malalignments of the lower quarter: Correlated and compensatory motions and postures. Journal of Orthopaedic & Sports Physical Therapy. 1996; 23(2):164-70. [DOI:10.2519/jospt.1996.23.2.164] [PMID]
- Thompson GH, Carter JR. Late-onset tibia vara (Blount's disease); Current concepts. Clinical Orthopaedics and Related Research. 1990; 255:24-35. [PMID]
- Beskin JL, Burke SW, Johnston CE, Roberts JM. Clinical basis for a mechanical etiology in adolescent Blount's disease. Orthopedics. 1986; 9(3):365-70. [PMID]
- Henderson RC, Greene WB. Etiology of late-onset tibia vara: Is varus alignment a prerequisite. Journal of Pediatric Orthopedics. 1994; 14(2):143-6. [DOI:10.1097/01241398-199403000-00002] [PMID]
- Lubani MM, Al-Shab TS, Al-Saleh QA, Sharda DC, Quattawi SA, Ahmed SA, et al. Vitamin-D-deficiency rickets in Kuwait: the prevalence of a preventable disease. Annals of Tropical Paediatrics. 1989; 9(3):134-9. [DOI:10.1080/02724936.1989.11748616] [PMID]
Type of Study: Applicable |
Subject:
General
Received: 2018/06/1 | Accepted: 2018/10/13 | Published: 2019/02/19
Received: 2018/06/1 | Accepted: 2018/10/13 | Published: 2019/02/19
References
1. Hertel J, Dorfman JH, Braham RA. Lower extremity malalignments and anterior cruciate ligament injury history. Journal of Sports Science & Medicine. 2004; 3(4):220-5. [PMID] [PMCID] [PMID] [PMCID]
2. Powers CM, Chen PY, Reischl SF, Perry J. Comparison of foot pronation and lower extremity rotation in persons with and without patellofemoral pain. Foot & Ankle International. 2002; 23(7):634-40. [DOI:10.1177/107110070202300709] [PMID] [DOI:10.1177/107110070202300709]
3. Shultz SJ, Carcia CR, Gansneder BM, Perrin DH. The independent and interactive effects of navicular drop and quadriceps angle on neuromuscular responses to a weight-bearing perturbation. Journal of Athletic Training. 2006; 41(3):251-9. [PMID] [PMCID] [PMID] [PMCID]
4. Meyer EG, Haut RC. Anterior cruciate ligament injury induced by internal tibial torsion or tibiofemoral compression. Journal of Biomechanics. 2008; 41(16):3377-83. [DOI:10.1016/j.jbiomech.2008.09.023] [PMID] [DOI:10.1016/j.jbiomech.2008.09.023]
5. Kaneko M, Sakuraba K. Association between femoral anteversion and lower extremity posture upon single-leg landing: Implications for anterior cruciate ligament injury. Journal of Physical Therapy Science. 2013; 25(10):1213-7. [DOI:10.1589/jpts.25.1213] [PMID] [PMCID] [DOI:10.1589/jpts.25.1213]
6. Bonci CM. Assessment and evaluation of predisposing factors to anterior cruciate ligament injury. Journal of Athletic Training. 1999; 34(2):155-64. [PMID] [PMCID] [PMID] [PMCID]
7. Nyland J, Kuzemchek S, Parks M, Caborn DN. Femoral anteversion influences vastus medialis and gluteus medius EMG amplitude: Composite hip abductor EMG amplitude ratios during isometric combined hip abduction-external rotation. Journal of Electromyography and Kinesiology. 2004; 14(2):255-61. [DOI:10.1016/S1050-6411(03)00078-6] [DOI:10.1016/S1050-6411(03)00078-6]
8. Amraee D, Alizadeh MH, Razi M, Yazdi HR, Minoonejad H. Risk factors associated with noncontact injuries of the anterior cruciate ligament in male athletes. Minerva Ortopedica e Traumatologica. 2013; 64(4):435-44.
9. Sahrmann S. Movement system impairment syndromes of the extremities, cervical and thoracic spines. Amsterdam: Elsevier Health Sciences; 2011.
10. Levangie PK, Norkin CC. Joint structure and function: A comprehensive analysis. Philadelphia, Pennsylvania: FA Davis; 2011. [PMID] [PMID]
11. Neumann DA. Kinesiology of the musculoskeletal system-e-book: Foundations for rehabilitation. Amsterdam: Elsevier Health Sciences; 2013.
12. Papaioannou T, Stokes I, Kenwright J. Scoliosis associated with limb-length inequality. Journal of Bone and Joint Surgery. 1982; 64(1):59-62. [DOI:10.2106/00004623-198264010-00009] [PMID] [DOI:10.2106/00004623-198264010-00009]
13. Steen H, Terjesen T, Bjerkreim I. [Anisomelia: Clinical consequences and treatment (Danish)]. Journal for the Norwegian Medical Association: Journal for Practical Medicine, New Series. 1997; 117(11):1595-600.
14. Samaei A, Bakhtiary AH, Elham F, Rezasoltani A. Effects of genu varum deformity on postural stability. International Journal of Sports Medicine. 2012; 33(06):469-73. [DOI:10.1055/s-0031-1301331] [PMID] [DOI:10.1055/s-0031-1301331]
15. Palastanga N, Field D, Soames R. Anatomy and human movement: Structure and function. Amsterdam: Elsevier Health Sciences; 2006.
16. Piva SR, Fitzgerald K, Irrgang JJ, Jones S, Hando BR, Browder DA, et al. Reliability of measures of impairments associated with patellofemoral pain syndrome. BMC Musculoskeletal Disorders. 2006; 7(1):33. [DOI:10.1186/1471-2474-7-33] [PMID] [PMCID] [DOI:10.1186/1471-2474-7-33]
17. Emami MJ, Ghahramani MH, Abdinejad F, Namazi H. Q-angle: An invaluable parameter for evaluation of anterior knee pain. Archives of Iranian Medicine. 2007; 10(1):24-6. [PMID] [PMID]
18. Greene CC, Edwards TB, Wade MR, Carson EW. Reliability of the quadriceps angle measurement. The American Journal of Knee Surgery. 2001; 14(2):97-103. [PMID] [PMID]
19. Loudon JK. Measurement of knee-joint-position sense in women with genu recurvatum. Journal of Sport Rehabilitation. 2000; 9(1):15-25. [DOI:10.1123/jsr.9.1.15] [DOI:10.1123/jsr.9.1.15]
20. Kwon OY, Tuttle LJ, Commean PK, Mueller MJ. Reliability and validity of measures of hammer toe deformity angle and tibial torsion. The Foot. 2009; 19(3):149-55. [DOI:10.1016/j.foot.2009.03.004] [PMID] [PMCID] [DOI:10.1016/j.foot.2009.03.004]
21. Lee SH, Chung CY, Park MS, Choi IH, Cho TJ. Tibial torsion in cerebral palsy: Validity and reliability of measurement. Clinical Orthopaedics and Related Research. 2009; 467(8):2098-104. [DOI:10.1007/s11999-009-0705-1] [PMID] [PMCID] [DOI:10.1007/s11999-009-0705-1]
22. Lohmann KN, Rayhel HE, Schneiderwind WP, Danoff JV. Static measurement of tibia vara: Reliability and effect of lower extremity position. Physical Therapy. 1987; 67(2):196-9. [DOI:10.1093/ptj/67.2.196] [PMID] [DOI:10.1093/ptj/67.2.196]
23. Staheli LT, Chew DE, Corbett MA. The longitudinal arch: A survey of eight hundred and eighty-two feet in normal children and adults. The Journal of Bone and Joint Surgery; American Volume. 1987; 69(3):426-8. [PMID] [DOI:10.2106/00004623-198769030-00014] [PMID]
24. Tönnis D, Heinecke A. Acetabular and femoral anteversion: Relationship with osteoarthritis of the hip. The Journal of Bone and Joint Surgery. 1999; 81(12):1747-70. [DOI:10.2106/00004623-199912000-00014] [PMID] [DOI:10.2106/00004623-199912000-00014]
25. Magee DJ. Orthopedic physical assessment. Amsterdam: Elsevier Health Sciences; 2008.
26. Lawrence III RK, Kernozek TW, Miller EJ, Torry MR, Reuteman P. Influences of hip external rotation strength on knee mechanics during single-leg drop landings in females. Clinical Biomechanics. 2008; 23(6):806-13. [DOI:10.1016/j.clinbiomech.2008.02.009] [PMID] [DOI:10.1016/j.clinbiomech.2008.02.009]
27. Nguyen AD, Shultz SJ, Schmitz RJ, Luecht RM, Perrin DH. A preliminary multifactorial approach describing the relationships among lower extremity alignment, hip muscle activation, and lower extremity joint excursion. Journal of Athletic Training. 2011; 46(3):246-56. [DOI:10.4085/1062-6050-46.3.246] [PMID] [PMCID] [DOI:10.4085/1062-6050-46.3.246]
28. Bell DR, Oates DC, Clark MA, Padua DA. Two-and 3-dimensional knee valgus are reduced after an exercise intervention in young adults with demonstrable valgus during squatting. Journal of Athletic Training. 2013; 48(4):442-9. [DOI:10.4085/1062-6050-48.3.16] [PMID] [PMCID] [DOI:10.4085/1062-6050-48.3.16]
29. Frank C, Page P, Lardner R. Assessment and treatment of muscle imbalance: The Janda approach. Champaign, Illinois: Human kinetics; 2009.
30. Bell DR, Padua DA, Clark MA. Muscle strength and flexibility characteristics of people displaying excessive medial knee displacement. Archives of Physical Medicine and Rehabilitation. 2008; 89(7):1323-8. [DOI:10.1016/j.apmr.2007.11.048] [PMID] [DOI:10.1016/j.apmr.2007.11.048]
31. Shamberger W. The malalignment syndrome: Implications for medicine and sport. Amsterdam: Elsevier Health Sciences; 2012.
32. Riegger-Krugh C, Keysor JJ. Skeletal malalignments of the lower quarter: Correlated and compensatory motions and postures. Journal of Orthopaedic & Sports Physical Therapy. 1996; 23(2):164-70. [DOI:10.2519/jospt.1996.23.2.164] [PMID] [DOI:10.2519/jospt.1996.23.2.164]
33. Thompson GH, Carter JR. Late-onset tibia vara (Blount's disease); Current concepts. Clinical Orthopaedics and Related Research. 1990; 255:24-35. [PMID] [PMID]
34. Beskin JL, Burke SW, Johnston CE, Roberts JM. Clinical basis for a mechanical etiology in adolescent Blount's disease. Orthopedics. 1986; 9(3):365-70. [PMID] [PMID]
35. Henderson RC, Greene WB. Etiology of late-onset tibia vara: Is varus alignment a prerequisite. Journal of Pediatric Orthopedics. 1994; 14(2):143-6. [DOI:10.1097/01241398-199403000-00002] [PMID] [DOI:10.1097/01241398-199403000-00002]
36. Lubani MM, Al-Shab TS, Al-Saleh QA, Sharda DC, Quattawi SA, Ahmed SA, et al. Vitamin-D-deficiency rickets in Kuwait: the prevalence of a preventable disease. Annals of Tropical Paediatrics. 1989; 9(3):134-9. [DOI:10.1080/02724936.1989.11748616] [PMID] [DOI:10.1080/02724936.1989.11748616]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |