Wed, Jun 26, 2024
Volume 14, Issue 2 (Spring 2024)
PTJ 2024, 14(2): 137-146 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Afsari Z, Rahimi N M, Azimkhani A. Investigating the Effects of Dynamic Neuromuscular Stabilization Exercises on Chest Mobility, Upright Sitting Height, and Quality of Life in Obese Women. PTJ 2024; 14 (2) :137-146
URL: http://ptj.uswr.ac.ir/article-1-602-en.html
URL: http://ptj.uswr.ac.ir/article-1-602-en.html
1- Department of Sports Sciences, Faculty of Literature and Humanities, Imam Reza International University, Mashhad, Iran.
Full-Text [PDF 607 kb]
(58 Downloads)
| Abstract (HTML) (734 Views)
Full-Text: (30 Views)
Introduction
Obesity is a significant global health problem in the 20th and 21st centuries and can have negative effects on skeletal muscle function and joint mobility in obese individuals [1–4]. Skeletal muscles in obese individuals have to work harder to move the increased body mass, which can potentially lead to a positive training effect [5]. However, obesity can also result in a decrease in muscle mass and lower muscle quality, which can impair the ability of skeletal muscles to maintain locomotor performance and reduce mobility in obese individuals [6, 7]. Additionally, obesity can impact respiratory function, leading to reduced chest mobility [8]. On the other hand, prolonged periods of sitting and a sedentary lifestyle can disrupt muscle chains, decrease chest mobility of the chest, and limit joint range of motion in joints [9–11]. Consequently, sedentary behavior may influence the physiological curvature of the spine, pelvic tilting, and alignment of joint movement axes [12]. For example, overweight individuals have a higher risk (15% to 79%) of fall-related injuries requiring medical treatment compared to those with a healthy weight [13]. Furthermore, various injuries, such as sprains, strains, and dislocations are more common among individuals with a low physical fitness level [14].
The importance of considering strategies desired to prevent spinal malalignment and respiratory function disorders cannot be overstated. Therefore, it is crucial to identify factors and measures that can improve the efficiency of the diaphragm. Numerous studies have shown a correlation between the activity of the diaphragm and intercostal muscles and respiratory and postural function [15–17]. Many experts argue that maintaining proper posture is essential for regular respiratory function [18].
It is possible to train in a way that aligns the ribs and spinal column optimally. Correct breathing patterns can also help with breathing and maintaining stability in the spine [15]. To achieve success in any corrective or rehabilitation program that focuses on the movement system, it is important to consider retraining and correcting faulty respiratory patterns. Accordingly, to effectively perform breathing exercises, it is necessary to train in the corrective program under different conditions [9, 16, 17, 19]. The dynamic neuromuscular stabilization (DNS) method, which is based on developmental kinesiology models, can achieve these goals [20, 21]. One of the primary objectives of the DNS approach is to improve precise muscle coordination by placing the subjects in various developmental positions while achieving a functionally central position for the supported joints and all segments. Additionally, the DNS approach emphasizes the importance of combining spinal stabilization and breathing patterns during daily activities [22–24].
Obese individuals need to participate in rehabilitation programs that target the respiratory muscles to address the changes in posture, muscle strength, and breathing patterns [4]. The main goal of engaging in breathing exercises is to improve respiration and synchronize the different muscle groups involved [16, 17, 19]. Therefore, this study assesses the effectiveness of DNS exercises in improving chest mobility, upright sitting height, and quality of life (QoL) in obese women. We hypothesize that DNS exercises would lead to improvements in these areas. Additionally, we believe that performing DNS exercises dynamically and functionally is an effective approach for enhancing these variables.
Materials and Methods
This study employed a pre-test-post-test design and was conducted on a sample of 60 women classified as obese. We calculated the sample size based on power analysis for the repeated-measures analysis of variance test using the G*Power software, version 3.1.9.2, setting the power at 0.80, the moderate effect size at 0.50, and the significance level at 0.05 (2-tailed). This study used a group allocation ratio of 1:1. Meanwhile, it determined that 60 patients (30 in each group) would be necessary based on these calculations.
The inclusion criteria consisted of being female, aged between 30 and 60 years with body mass index values of 25 kg/m2 and higher. Individuals with mental, neuromuscular, musculoskeletal, chronic systemic disorders, and vestibular problems that may hinder exercise participation, subjects who had undergone surgery in the last six months, those who were pregnant or planning to become pregnant, individuals who were actively COVID-19 positive, and persons who had previously contracted COVID-19 were excluded from the study [25].
Chest mobility
The assessment of chest mobility was conducted with the subject in an upright position. A tape measure with a length of 200 cm was used at two distinct locations along the rib cage. These locations included the anterior axillary line, which was used to measure the mobility of the upper chest region (referred to as upper chest mobility; axillary line); and the point where the xiphoid process is located, which was used to assess the mobility of the lower chest region [26].
Furthermore, to minimize changes in soft tissue shape, the tape had to be held snugly. The outcome was the difference between the measured data at maximum inspiration, and maximum expiration, held for at least two seconds to record the data, with an average of three tests recorded. This is considered a reliable method (intraclass correlation [ICC]=0.81-0.91), widely used by clinicians for assessment [27].
Upright sitting height measurement
For the sitting height measurement, the participants were instructed to sit comfortably on a chair with the hip, knee, and ankle joints flexed at 90°. Sitting height was then measured by calculating the distance between the most superior midline of the head and the ischial tuberosity, using a stadiometer with a 200 cm measuring range [28].
QoL
The QoL was assessed using the short-form survey-26 questionnaire [29]. This questionnaire consists of 26 questions, which are divided into five domains. Physical health subscale which includes questions 3, 4, 10, 15, 16, 17, and 18 in the questionnaire. The score for this subscale can range from 7 to 35, with a difference of 28 between these two scores. Mental health subscale which includes questions 5, 6, 7, 11, 19, and 26 in the questionnaire. The score for this subscale can range from 6 to 30, with a difference of 24 between these two scores. Social relationship subscale which includes questions 20, 21, and 22 in the questionnaire. The score for this subscale can range from 3 to 15, with a difference of 12 between these two scores. Environmental health subscale which includes questions 8, 9, 12, 13, 14, 23, 24, and 25 in the questionnaire. The score for this subscale can range from 8 to 40, with a difference of 32 between these two scores. General public health and QoL subscale which includes questions 1 and 2 in the questionnaire. The score for this subscale can range from 2 to 10, with a difference of 8 between these two scores. Each subscale score ranges from 0 to 100. A score of 100 indicates the best and most positive QoL in that particular area, while a score of 0 indicates the worst QoL. To calculate the total score for an individual, the scores of the five subscales are added together and then divided by 5. The resulting score is then multiplied by 100 to obtain the final score for the person’s QoL.
Study interventions
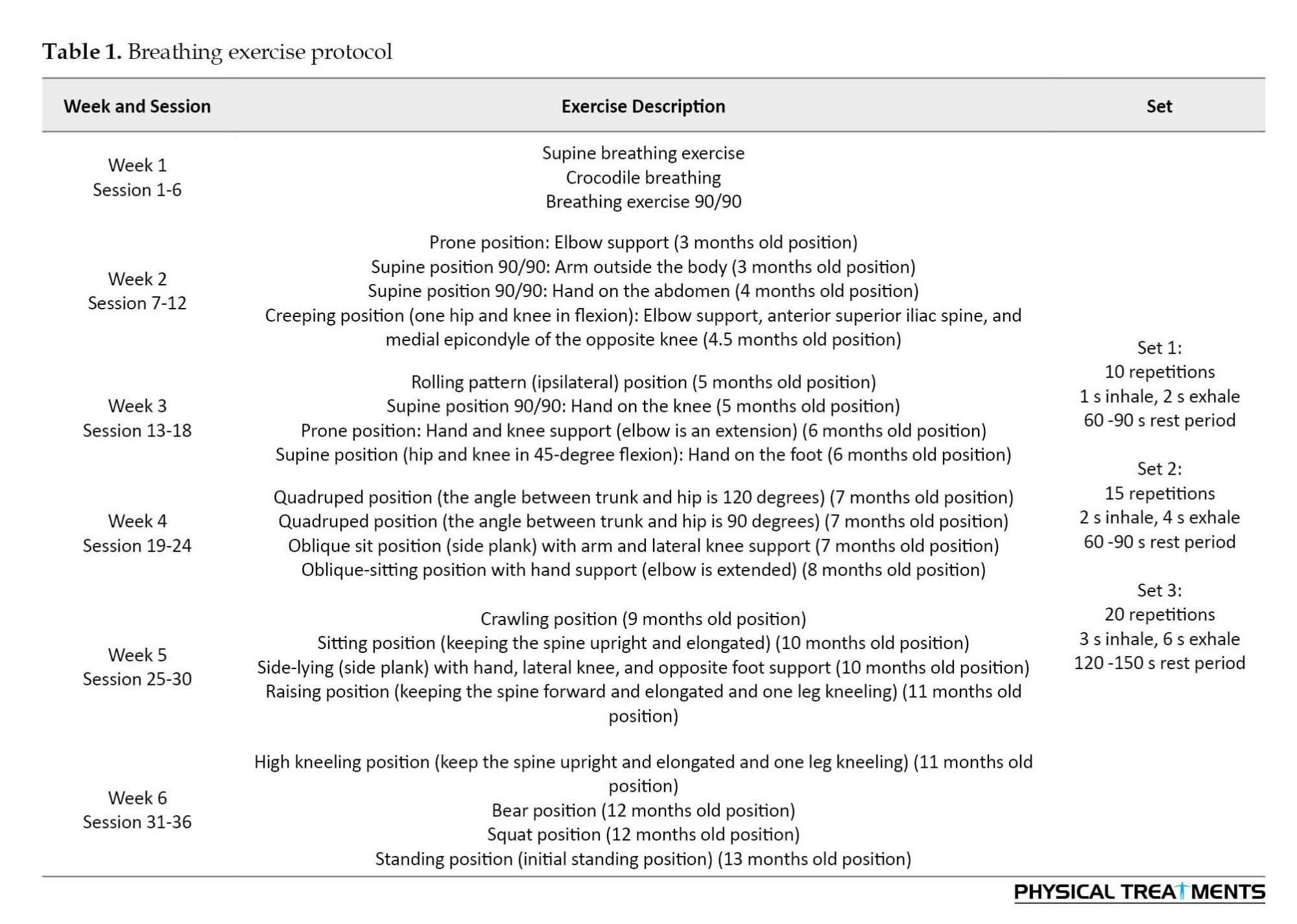
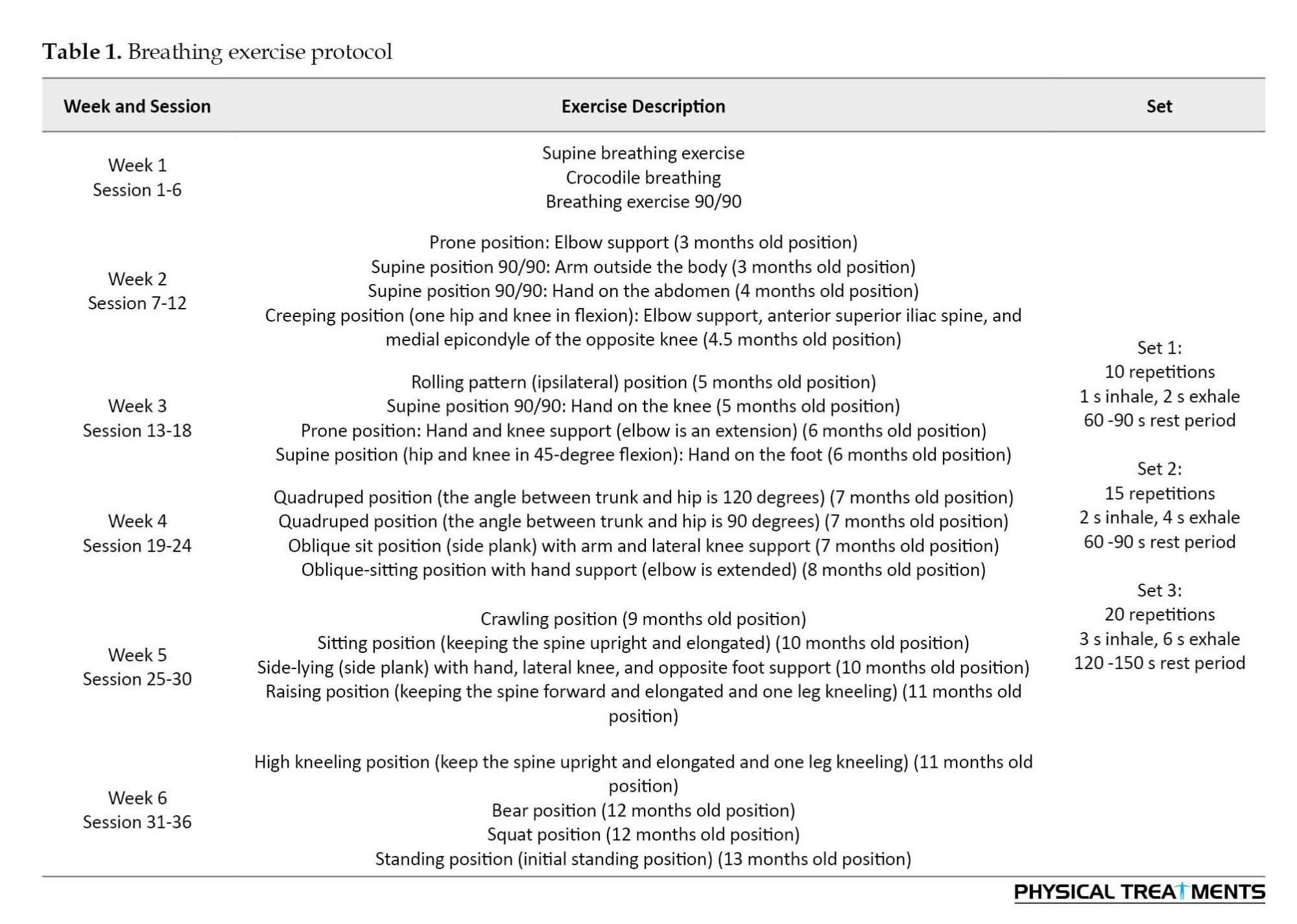
The subjects completed six sessions (45–60 min) per week (3 sessions of supervised exercise and 3 sessions of home-based exercise) of diaphragmatic breathing exercises in DNS patterns for 6 weeks. At first, verbal cues, manual guidance, and visual feedback were provided during the intervention so that participants learned how to adjust the pelvis, spine, ribcage, scapula alignment, and abdominal wall shape in various positions [23, 30, 31]. Moreover, to encourage the subjects to participate in exercise sessions regularly, they were educated on how incorrect movements, poor posture, and prolonged posture may affect neuromusculoskeletal health. In the first week, all subjects privately performed the breathing exercise program (3 patterns). From the second to the sixth week, subjects performed diaphragmatic breathing exercises using the developmental stabilization patterns of a healthy infant (Table 1).
Inhalation and exhalation were done through the nose and mouth, respectively [20, 21, 30, 32–34]. Home exercises were taught, and the ability to perform them correctly was supervised in each session. A physical therapist initially explained the therapy method verbally and used visual aids, such as photographs, in each group initially explained the therapy method verbally and used visual aids, (such as photographs), in each group session. Additionally, the therapist verbally and manually guided and corrected the participants to achieve optimal adjustment of the pelvis, spine, ribcage, and scapulae while properly stabilizing the core in different positions during supervised exercise sessions. Supervised exercises were performed on Saturday, Monday, and Wednesday and home-based exercises were performed on Sunday, Tuesday, and Thursday. The home-based exercise program was similar to the supervised exercise program in terms of the number of exercises and repetitions. Before each home exercise session, the participants attended a supervised practice session in which day were instructed on the proper technique and mechanics of each exercise. The participants were also given an illustrated exercise booklet to improve accuracy and compliance. Compliance was reported daily via telephone by the participants.
The intensity of the exercises was determined based on developmental positions to activate the stereotypical stabilization and breathing patterns seen in natural postural-locomotion patterns as defined by developmental kinesiology. This goal was achieved by placing the subjects in the developmental positions of an infant between three months and 13 months of age, as done in this study [20, 21, 30, 32, 33]. The protocol was implemented under the supervision of a trainer. The subjects performed the exercises, and the trainer monitored and updated their performance as needed. Additionally, the subjects agreed not to engage in other practices or physical activities without consent.
Statistical analysis
The statistical package for the social sciences (SPSS software, version 23, Inc., Chicago, Illinois) was used for the analysis at a significance level (α) of P<0.05 for all analyses. The Kolmogorov-Smirnov test was utilized to investigate the normality distribution. Repeated measures analysis of variance was utilized to analyze all data.
Results
According to the findings of the study (Tables 2 and 3), significant improvements were observed after 6 weeks in the mean of parameters, including chest wall mobility (upper chest mobility and lower chest mobility), sitting height, and QoL (physical, mental, environmental, and overall).


No significant improvement was found in the social subscale.
Discussion
This study assessed the effects of DNS exercises on chest mobility, upright sitting height, and QoL in obese women. The findings of this non-invasive investigation suggest that six weeks of DNS exercises can result in significant improvements in chest mobility, upright sitting height, and QoL for obese women. Our key findings are as follows: The DNS group exhibited improvements (when comparing pre- and post-training data) in upper chest mobility (76.2%), lower chest mobility (31.0%), upright sitting height (1.9%), QoL domains of physical health (12.3%), mental health (9.8%), social functioning (3.4%), environmental factors (1.3%), and overall QoL score (7.1%).
This investigation assessed thoracic mobility at two distinct levels: the upper and lower levels. After analyzing the experimental findings, it was found that there was a significant improvement in chest mobility at both of these levels. This discovery is in line with the results reported by Bezzoli et al. (2016), Mongkol (2016), Kim et al. (2015), and Mohammad Rahimi et al. (2020) [35, 36, 17]. In the study conducted by Bezzoli et al., the patients were instructed on activating the lumbar-pelvic cylinder muscles individually, while also practicing diaphragmatic breathing and maintaining a neutral lumbar posture in various positions. This resulted in a significant improvement in chest mobility [35]. Similarly, in our respiratory exercises, we emphasize deep diaphragmatic breathing and maintaining a neutral lumbar posture in different positions, using 20 developmental kinesiology patterns. This intervention effectively improves breathing patterns and thoracic mobility. Mongkol also found that yoga breathing exercises, characterized by forceful respiration, contribute to muscle flexibility and expansion of the chest wall. In their study, repetitive deep breathing exercises alleviated rib cage rigidity and improved thoracic kyphosis alignment [36]. In individuals with weakened diaphragm or deep spinal stabilizers, compensatory breathing patterns often lead to lifting of the lower rib cage during inhalation. However, our functional approach of activating torso stabilizing muscles before rib cage movement can enhance chest mobility and stability [9]. Overall, our findings suggest that a functional approach to harmonizing and enhancing proper breathing patterns can have favorable outcomes in improving torso stability and chest mobility [17].
Furthermore, when the thoracic spinal curvature is straightened, it leads to adaptive changes in the lumbopelvic region and improves posture [9, 17]. As a result, we focused our intervention on the extensor trunk muscles. In a study by Obayashi et al. (2012), they also found similar results, demonstrating the significant and remarkable impact that breathing muscle exercises can have on spinal alignment [39]. Moreover, the results of the current study are consistent with the findings of the study by Mohammad Rahimi et al. (2020); thoracic hyper-kyphosis and trunk extensor endurance were significantly enhanced by DNS breathing exercises [17]. Decreased extensor trunk muscle function is one of the effective factors of changing thoracic spine curvature [39] and a decrease in the upright sitting height. It seems that breathing exercises with an emphasis on the integrated spinal stabilizing system (ISSS) [32, 40], precise muscle timing and coordination to have movement efficiency and breathing technique [23, 24, 30, 32] lead to a significant improvement in extensor trunk muscle endurance and upright sitting height.
Numerous studies have shown that thoracic stabilization significantly influences the acquisition and maintenance of proper upright posture [41]. This effect is further supported by the interconnected structural and functional reactions that affect the thoracic spine [9]. Any dysfunction or misalignment in a joint or segment can have local and global impacts on the alignment and functioning of adjacent regions [9].
As for QoL, there was a statistically significant improvement in the obese women. This is in agreement with Wu et al. (2014) and Bezzoli et al. (2016), linking abdominal obesity to the physical health, mental, social, environmental, and total domain of the short form survey-26 [42, 35]. Our preliminary data show a statistically significant improvement in the physical health, mental, environmental, and overall domains but not the social ones. A possible reason for that could be that the breathing exercises used in the intervention group program facilitate body awareness and improved body schema and possibly decrease the fear of injuries and falling and anxiety, positively influencing the mental health components of the short form survey-26.
In addition, DNS exercises, which focus on functional movements, have been used to help increase the adherence rates of overweight or obese individuals to daily activity programs. It is important to recognize that breathing exercise programs play a significant role in improving the health and QoL for those who are overweight and or obese.
The incorporation of breathing exercises in this investigation has had a significant impact on enhancing remedial exercise methodologies. Additionally, a notable advantage of this study is that it included a total of 36 sessions (18 sessions of supervised exercise and 18 sessions of home-based exercise), which provided educational content and guidance for participants to correct their breathing patterns during daily activities. Although the subject matter remains a topic of debate, the attempt to explore existing literature on the effects of respiratory exercise on chest wall mobility, upright sitting height measurement, and overall QoL has produced insufficient findings.
Conclusion
Our study offers preliminary evidence of the relationship between breathing and posture. The main objective of breathing exercises is to educate participants on how to incorporate proper breathing patterns and alignment into their daily activities. Our study demonstrates that implementing breathing exercises can lead to significant improvements in muscle strength and posture. Considering the potential benefits, it is recommended that clinicians prioritize breathing exercises based on ideal developmental patterns, particularly for obese women seeking to enhance their muscular and postural conditions.
Study limitations
One limitation of this study was that it was impossible to provide measurements using valid medical devices like spirometers, radiography, or spinal mouse devices. However, the study had sufficient statistical power to identify differences. It is recommended to conduct further randomized controlled trials to gain a better understanding of the effects of such interventions over a longer period and in different age groups.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the Immam Reza International University (Code: IR.IMAMREZA.REC.1401.014).
Funding
The paper was extracted from the master's thesis of Zainab Afsari, approved by Department of Sport Sciences, Faculty of Literature and Humanities, Imam Reza International University.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors wish to express their particular thankfulness to Imam Reza International University. In addition, the authors thank the participants in the study.
References
Obesity is a significant global health problem in the 20th and 21st centuries and can have negative effects on skeletal muscle function and joint mobility in obese individuals [1–4]. Skeletal muscles in obese individuals have to work harder to move the increased body mass, which can potentially lead to a positive training effect [5]. However, obesity can also result in a decrease in muscle mass and lower muscle quality, which can impair the ability of skeletal muscles to maintain locomotor performance and reduce mobility in obese individuals [6, 7]. Additionally, obesity can impact respiratory function, leading to reduced chest mobility [8]. On the other hand, prolonged periods of sitting and a sedentary lifestyle can disrupt muscle chains, decrease chest mobility of the chest, and limit joint range of motion in joints [9–11]. Consequently, sedentary behavior may influence the physiological curvature of the spine, pelvic tilting, and alignment of joint movement axes [12]. For example, overweight individuals have a higher risk (15% to 79%) of fall-related injuries requiring medical treatment compared to those with a healthy weight [13]. Furthermore, various injuries, such as sprains, strains, and dislocations are more common among individuals with a low physical fitness level [14].
The importance of considering strategies desired to prevent spinal malalignment and respiratory function disorders cannot be overstated. Therefore, it is crucial to identify factors and measures that can improve the efficiency of the diaphragm. Numerous studies have shown a correlation between the activity of the diaphragm and intercostal muscles and respiratory and postural function [15–17]. Many experts argue that maintaining proper posture is essential for regular respiratory function [18].
It is possible to train in a way that aligns the ribs and spinal column optimally. Correct breathing patterns can also help with breathing and maintaining stability in the spine [15]. To achieve success in any corrective or rehabilitation program that focuses on the movement system, it is important to consider retraining and correcting faulty respiratory patterns. Accordingly, to effectively perform breathing exercises, it is necessary to train in the corrective program under different conditions [9, 16, 17, 19]. The dynamic neuromuscular stabilization (DNS) method, which is based on developmental kinesiology models, can achieve these goals [20, 21]. One of the primary objectives of the DNS approach is to improve precise muscle coordination by placing the subjects in various developmental positions while achieving a functionally central position for the supported joints and all segments. Additionally, the DNS approach emphasizes the importance of combining spinal stabilization and breathing patterns during daily activities [22–24].
Obese individuals need to participate in rehabilitation programs that target the respiratory muscles to address the changes in posture, muscle strength, and breathing patterns [4]. The main goal of engaging in breathing exercises is to improve respiration and synchronize the different muscle groups involved [16, 17, 19]. Therefore, this study assesses the effectiveness of DNS exercises in improving chest mobility, upright sitting height, and quality of life (QoL) in obese women. We hypothesize that DNS exercises would lead to improvements in these areas. Additionally, we believe that performing DNS exercises dynamically and functionally is an effective approach for enhancing these variables.
Materials and Methods
This study employed a pre-test-post-test design and was conducted on a sample of 60 women classified as obese. We calculated the sample size based on power analysis for the repeated-measures analysis of variance test using the G*Power software, version 3.1.9.2, setting the power at 0.80, the moderate effect size at 0.50, and the significance level at 0.05 (2-tailed). This study used a group allocation ratio of 1:1. Meanwhile, it determined that 60 patients (30 in each group) would be necessary based on these calculations.
The inclusion criteria consisted of being female, aged between 30 and 60 years with body mass index values of 25 kg/m2 and higher. Individuals with mental, neuromuscular, musculoskeletal, chronic systemic disorders, and vestibular problems that may hinder exercise participation, subjects who had undergone surgery in the last six months, those who were pregnant or planning to become pregnant, individuals who were actively COVID-19 positive, and persons who had previously contracted COVID-19 were excluded from the study [25].
Chest mobility
The assessment of chest mobility was conducted with the subject in an upright position. A tape measure with a length of 200 cm was used at two distinct locations along the rib cage. These locations included the anterior axillary line, which was used to measure the mobility of the upper chest region (referred to as upper chest mobility; axillary line); and the point where the xiphoid process is located, which was used to assess the mobility of the lower chest region [26].
Furthermore, to minimize changes in soft tissue shape, the tape had to be held snugly. The outcome was the difference between the measured data at maximum inspiration, and maximum expiration, held for at least two seconds to record the data, with an average of three tests recorded. This is considered a reliable method (intraclass correlation [ICC]=0.81-0.91), widely used by clinicians for assessment [27].
Upright sitting height measurement
For the sitting height measurement, the participants were instructed to sit comfortably on a chair with the hip, knee, and ankle joints flexed at 90°. Sitting height was then measured by calculating the distance between the most superior midline of the head and the ischial tuberosity, using a stadiometer with a 200 cm measuring range [28].
QoL
The QoL was assessed using the short-form survey-26 questionnaire [29]. This questionnaire consists of 26 questions, which are divided into five domains. Physical health subscale which includes questions 3, 4, 10, 15, 16, 17, and 18 in the questionnaire. The score for this subscale can range from 7 to 35, with a difference of 28 between these two scores. Mental health subscale which includes questions 5, 6, 7, 11, 19, and 26 in the questionnaire. The score for this subscale can range from 6 to 30, with a difference of 24 between these two scores. Social relationship subscale which includes questions 20, 21, and 22 in the questionnaire. The score for this subscale can range from 3 to 15, with a difference of 12 between these two scores. Environmental health subscale which includes questions 8, 9, 12, 13, 14, 23, 24, and 25 in the questionnaire. The score for this subscale can range from 8 to 40, with a difference of 32 between these two scores. General public health and QoL subscale which includes questions 1 and 2 in the questionnaire. The score for this subscale can range from 2 to 10, with a difference of 8 between these two scores. Each subscale score ranges from 0 to 100. A score of 100 indicates the best and most positive QoL in that particular area, while a score of 0 indicates the worst QoL. To calculate the total score for an individual, the scores of the five subscales are added together and then divided by 5. The resulting score is then multiplied by 100 to obtain the final score for the person’s QoL.
Study interventions
The subjects completed six sessions (45–60 min) per week (3 sessions of supervised exercise and 3 sessions of home-based exercise) of diaphragmatic breathing exercises in DNS patterns for 6 weeks. At first, verbal cues, manual guidance, and visual feedback were provided during the intervention so that participants learned how to adjust the pelvis, spine, ribcage, scapula alignment, and abdominal wall shape in various positions [23, 30, 31]. Moreover, to encourage the subjects to participate in exercise sessions regularly, they were educated on how incorrect movements, poor posture, and prolonged posture may affect neuromusculoskeletal health. In the first week, all subjects privately performed the breathing exercise program (3 patterns). From the second to the sixth week, subjects performed diaphragmatic breathing exercises using the developmental stabilization patterns of a healthy infant (Table 1).
Inhalation and exhalation were done through the nose and mouth, respectively [20, 21, 30, 32–34]. Home exercises were taught, and the ability to perform them correctly was supervised in each session. A physical therapist initially explained the therapy method verbally and used visual aids, such as photographs, in each group initially explained the therapy method verbally and used visual aids, (such as photographs), in each group session. Additionally, the therapist verbally and manually guided and corrected the participants to achieve optimal adjustment of the pelvis, spine, ribcage, and scapulae while properly stabilizing the core in different positions during supervised exercise sessions. Supervised exercises were performed on Saturday, Monday, and Wednesday and home-based exercises were performed on Sunday, Tuesday, and Thursday. The home-based exercise program was similar to the supervised exercise program in terms of the number of exercises and repetitions. Before each home exercise session, the participants attended a supervised practice session in which day were instructed on the proper technique and mechanics of each exercise. The participants were also given an illustrated exercise booklet to improve accuracy and compliance. Compliance was reported daily via telephone by the participants.
The intensity of the exercises was determined based on developmental positions to activate the stereotypical stabilization and breathing patterns seen in natural postural-locomotion patterns as defined by developmental kinesiology. This goal was achieved by placing the subjects in the developmental positions of an infant between three months and 13 months of age, as done in this study [20, 21, 30, 32, 33]. The protocol was implemented under the supervision of a trainer. The subjects performed the exercises, and the trainer monitored and updated their performance as needed. Additionally, the subjects agreed not to engage in other practices or physical activities without consent.
Statistical analysis
The statistical package for the social sciences (SPSS software, version 23, Inc., Chicago, Illinois) was used for the analysis at a significance level (α) of P<0.05 for all analyses. The Kolmogorov-Smirnov test was utilized to investigate the normality distribution. Repeated measures analysis of variance was utilized to analyze all data.
Results
According to the findings of the study (Tables 2 and 3), significant improvements were observed after 6 weeks in the mean of parameters, including chest wall mobility (upper chest mobility and lower chest mobility), sitting height, and QoL (physical, mental, environmental, and overall).


No significant improvement was found in the social subscale.
Discussion
This study assessed the effects of DNS exercises on chest mobility, upright sitting height, and QoL in obese women. The findings of this non-invasive investigation suggest that six weeks of DNS exercises can result in significant improvements in chest mobility, upright sitting height, and QoL for obese women. Our key findings are as follows: The DNS group exhibited improvements (when comparing pre- and post-training data) in upper chest mobility (76.2%), lower chest mobility (31.0%), upright sitting height (1.9%), QoL domains of physical health (12.3%), mental health (9.8%), social functioning (3.4%), environmental factors (1.3%), and overall QoL score (7.1%).
This investigation assessed thoracic mobility at two distinct levels: the upper and lower levels. After analyzing the experimental findings, it was found that there was a significant improvement in chest mobility at both of these levels. This discovery is in line with the results reported by Bezzoli et al. (2016), Mongkol (2016), Kim et al. (2015), and Mohammad Rahimi et al. (2020) [35, 36, 17]. In the study conducted by Bezzoli et al., the patients were instructed on activating the lumbar-pelvic cylinder muscles individually, while also practicing diaphragmatic breathing and maintaining a neutral lumbar posture in various positions. This resulted in a significant improvement in chest mobility [35]. Similarly, in our respiratory exercises, we emphasize deep diaphragmatic breathing and maintaining a neutral lumbar posture in different positions, using 20 developmental kinesiology patterns. This intervention effectively improves breathing patterns and thoracic mobility. Mongkol also found that yoga breathing exercises, characterized by forceful respiration, contribute to muscle flexibility and expansion of the chest wall. In their study, repetitive deep breathing exercises alleviated rib cage rigidity and improved thoracic kyphosis alignment [36]. In individuals with weakened diaphragm or deep spinal stabilizers, compensatory breathing patterns often lead to lifting of the lower rib cage during inhalation. However, our functional approach of activating torso stabilizing muscles before rib cage movement can enhance chest mobility and stability [9]. Overall, our findings suggest that a functional approach to harmonizing and enhancing proper breathing patterns can have favorable outcomes in improving torso stability and chest mobility [17].
Furthermore, when the thoracic spinal curvature is straightened, it leads to adaptive changes in the lumbopelvic region and improves posture [9, 17]. As a result, we focused our intervention on the extensor trunk muscles. In a study by Obayashi et al. (2012), they also found similar results, demonstrating the significant and remarkable impact that breathing muscle exercises can have on spinal alignment [39]. Moreover, the results of the current study are consistent with the findings of the study by Mohammad Rahimi et al. (2020); thoracic hyper-kyphosis and trunk extensor endurance were significantly enhanced by DNS breathing exercises [17]. Decreased extensor trunk muscle function is one of the effective factors of changing thoracic spine curvature [39] and a decrease in the upright sitting height. It seems that breathing exercises with an emphasis on the integrated spinal stabilizing system (ISSS) [32, 40], precise muscle timing and coordination to have movement efficiency and breathing technique [23, 24, 30, 32] lead to a significant improvement in extensor trunk muscle endurance and upright sitting height.
Numerous studies have shown that thoracic stabilization significantly influences the acquisition and maintenance of proper upright posture [41]. This effect is further supported by the interconnected structural and functional reactions that affect the thoracic spine [9]. Any dysfunction or misalignment in a joint or segment can have local and global impacts on the alignment and functioning of adjacent regions [9].
As for QoL, there was a statistically significant improvement in the obese women. This is in agreement with Wu et al. (2014) and Bezzoli et al. (2016), linking abdominal obesity to the physical health, mental, social, environmental, and total domain of the short form survey-26 [42, 35]. Our preliminary data show a statistically significant improvement in the physical health, mental, environmental, and overall domains but not the social ones. A possible reason for that could be that the breathing exercises used in the intervention group program facilitate body awareness and improved body schema and possibly decrease the fear of injuries and falling and anxiety, positively influencing the mental health components of the short form survey-26.
In addition, DNS exercises, which focus on functional movements, have been used to help increase the adherence rates of overweight or obese individuals to daily activity programs. It is important to recognize that breathing exercise programs play a significant role in improving the health and QoL for those who are overweight and or obese.
The incorporation of breathing exercises in this investigation has had a significant impact on enhancing remedial exercise methodologies. Additionally, a notable advantage of this study is that it included a total of 36 sessions (18 sessions of supervised exercise and 18 sessions of home-based exercise), which provided educational content and guidance for participants to correct their breathing patterns during daily activities. Although the subject matter remains a topic of debate, the attempt to explore existing literature on the effects of respiratory exercise on chest wall mobility, upright sitting height measurement, and overall QoL has produced insufficient findings.
Conclusion
Our study offers preliminary evidence of the relationship between breathing and posture. The main objective of breathing exercises is to educate participants on how to incorporate proper breathing patterns and alignment into their daily activities. Our study demonstrates that implementing breathing exercises can lead to significant improvements in muscle strength and posture. Considering the potential benefits, it is recommended that clinicians prioritize breathing exercises based on ideal developmental patterns, particularly for obese women seeking to enhance their muscular and postural conditions.
Study limitations
One limitation of this study was that it was impossible to provide measurements using valid medical devices like spirometers, radiography, or spinal mouse devices. However, the study had sufficient statistical power to identify differences. It is recommended to conduct further randomized controlled trials to gain a better understanding of the effects of such interventions over a longer period and in different age groups.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the Immam Reza International University (Code: IR.IMAMREZA.REC.1401.014).
Funding
The paper was extracted from the master's thesis of Zainab Afsari, approved by Department of Sport Sciences, Faculty of Literature and Humanities, Imam Reza International University.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors wish to express their particular thankfulness to Imam Reza International University. In addition, the authors thank the participants in the study.
References
- Rahimi GRM, Yousefabadi HA, Niyazi A, Rahimi NM, Alikhajeh Y. Effects of lifestyle intervention on inflammatory markers and waist circumference in overweight/obese adults with metabolic syndrome: A systematic review and meta-analysis of randomized controlled trials. Biological Research for Nursing. 2022; 24(1):94-105. [DOI:10.1177/10998004211044754] [PMID]
- Gao K, Su Z, Meng J, Yao Y, Li L, Su Y, et al. Effect of exercise training on some anti-inflammatory adipokines, high sensitivity C-reactive protein, and clinical outcomes in Sedentary adults with metabolic syndrome. Biological Research for Nursing. 2024; 26(1):125-38.[DOI:10.1177/10998004231195541] [PMID]
- Busutil R, Espallardo O, Torres A, Martínez-Galdeano L, Zozaya N, Hidalgo-Vega Á. The impact of obesity on health-related quality of life in Spain. Health and Quality of Life Outcomes. 2017; 15(1):197. [DOI:10.1186/s12955-017-0773-y] [PMID]
- Teasdale N, Simoneau M, Corbeil P, Handrigan G, Tremblay A, Hue O. Obesity alters balance and movement control. Current Obesity Reports. 2013; 2:235-40. [DOI:10.1007/s13679-013-0057-8]
- Tallis J, James RS, Seebacher F. The effects of obesity on skeletal muscle contractile function. The Journal of Experimental Biology. 2018; 221(Pt 13):jeb163840. [DOI:10.1242/jeb.163840] [PMID]
- Garcia-Vicencio S, Coudeyre E, Kluka V, Cardenoux C, Jegu AG, Fourot AV, et al. The bigger, the stronger? Insights from muscle architecture and nervous characteristics in obese adolescent girls. International Journal of Obesity (2005). 2016; 40(2):245-51. [DOI:10.1038/ijo.2015.158] [PMID]
- Tallis J, Hill C, James RS, Cox VM, Seebacher F. The effect of obesity on the contractile performance of isolated mouse soleus, EDL, and diaphragm muscles. Journal of Applied Physiology (Bethesda, Md.: 1985). 2017; 122(1):170-81. [DOI:10.1152/japplphysiol.00836.2016] [PMID]
- Salome CM, King GG, Berend N. Physiology of obesity and effects on lung function. Journal of Applied Physiology. 2010; 108(1):206-11. [DOI:10.1152/japplphysiol.00694.2009] [PMID]
- Page P, Frank C, Lardner R. Assessment and treatment of muscle imbalance: The Janda approach. Champaign: Human Kinetics; 2010. [DOI:10.5040/9781718211445]
- Czakwari A, Czernicki K, Durmala J. Faulty posture and style of life in young adults. In: Dangerfield PH, editor. Research into spinal deformities 6. Amsterdam: IOS Press; 2008. [Link]
- Huynh QL, Blizzard CL, Sharman JE, Magnussen CG, Dwyer T, Venn AJ. The cross-sectional association of sitting time with carotid artery stiffness in young adults. BMJ Open. 2014; 4(3):e004384. [DOI:10.1136/bmjopen-2013-004384] [PMID]
- Kim D, Cho M, Park Y, Yang Y. Effect of an exercise program for posture correction on musculoskeletal pain. Journal of Physical Therapy Science. 2015; 27(6):1791-4. [DOI:10.1589/jpts.27.1791] [PMID]
- Finkelstein EA, Chen H, Prabhu M, Trogdon JG, Corso PS. The relationship between obesity and injuries among US adults. American Journal of Health Promotion: AJHP. 2007; 21(5):460-8. [PMID]
- Matter KC, Sinclair SA, Hostetler SG, Xiang H. A comparison of the characteristics of injuries between obese and non-obese inpatients. Obesity. 2007; 15(10):2384-90. [DOI:10.1038/oby.2007.283] [PMID]
- De Troyer A, Wilson TA. Mechanism of the increased rib cage expansion produced by the diaphragm with abdominal support. Journal of Applied Physiology. 2015; 118(8):989-95. [DOI:10.1152/japplphysiol.00016.2015] [PMID]
- Ghavipanje V, Rahimi NM, Akhlaghi F. Six weeks effects of Dynamic Neuromuscular Stabilization (DNS) training in obese postpartum women with low back pain: A randomized controlled trial. Biological Research for Nursing. 2022; 24(1):106-14. [DOI:10.1177/10998004211044828] [PMID]
- Mohammad Rahimi N, Mahdavinejad R, Attarzadeh Hosseini SR, Negahban H. Efficacy of dynamic neuromuscular stabilization breathing exercises on chest mobility, trunk muscles, and thoracic kyphosis: A randomized controlled 6-week trial. Iranian Rehabilitation Journal. 2020; 18(3):329-36. [DOI:10.32598/irj.18.3.969.1]
- Pawlicka-Lisowska A, Motylewski S, Lisowski J, Michalak K, Poziomska-Piatkowska E. [Faulty posture and selected respiratory indicators (Polish)]. Polski Merkuriusz Lekarski: Organ Polskiego Towarzystwa Lekarskiego, 35(206):67–71. [PMID]
- Mohammad Rahimi N, Mahdavinezhad R, Attarzadeh Hosseini SR, Negahban H. Effect of dynamic neuromuscular stabilization breathing exercises on some spirometry indices of sedentary students with poor posture. Physical Treatments - Specific Physical Therapy Journal. 2019; 9(3):169-76. [DOI:10.32598/ptj.9.3.169]
- Kobesova A, Kolar P. Developmental kinesiology: Three levels of motor control in the assessment and treatment of the motor system. Journal of Bodywork and Movement Therapies. 2014; 18(1):23-33. [DOI:10.1016/j.jbmt.2013.04.002] [PMID]
- Davidek P, Andel R, Kobesova A. Influence of dynamic neuromuscular stabilization approach on maximum kayak paddling force. Journal of Human Kinetics. 2018; 61:15-27. [DOI:10.1515/hukin-2017-0127] [PMID]
- Yong MS, Lee HY, Lee YS. Effects of diaphragm breathing exercise and feedback breathing exercise on pulmonary function in healthy adults. Journal of Physical Therapy Science. 2017; 29(1):85-7. [DOI:10.1589/jpts.29.85] [PMID]
- Kolar P, Neuwirth J, Sanda J, Suchanek V, Svata Z, Volejnik J, et al. Analysis of diaphragm movement during tidal breathing and during its activation while breath holding using MRI synchronized with spirometry. Physiological Research. 2009; 58(3):383-92. [DOI:10.33549/physiolres.931376] [PMID]
- Kolar P, Sulc J, Kyncl M, Sanda J, Neuwirth J, Bokarius AV, et al. Stabilizing function of the diaphragm: Dynamic MRI and synchronized spirometric assessment. Journal of Applied Physiology. 2010; 109(4):1064-71. [DOI:10.1152/japplphysiol.01216.2009] [PMID]
- Ozturk B, Duruturk N. Effect of telerehabilitation applied during COVID-19 isolation period on physical fitness and quality of life in overweight and obese individuals. International Journal of Obesity. 2022; 46(1):95-9. [DOI:10.1038/s41366-021-00965-5] [PMID]
- Kim CB, Yang JM, Choi JD. The effects of chest expansion resistance exercise on chest expansion and maximal respiratory pressure in elderly with inspiratory muscle weakness. Journal of Physical Therapy Science. 2015; 27(4):1121-4. [DOI:10.1589/jpts.27.1121] [PMID]
- Bockenhauer SE, Chen H, Julliard KN, Weedon J. Measuring thoracic excursion: Reliability of the cloth tape measure technique. The Journal of the American Osteopathic Association. 2007; 107(5):191-6. [PMID]
- Shin J, Yoon H, Park J, Kim H, You JSH. Comparative immediate effects of isometric chin-tuck and dynamic neuromuscular stabilization on neck flexor muscle thickness and upright sitting height posture. Physical Therapy Korea. 2019; 26(4):1-9. [DOI: 10.12674/ptk.2019.26.4.001]
- Hesamzadeh A, Maddah SB, Mohammadi F, Fallahi Khoshknab M, Rahgozar M. [Comparison of elderlys” quality of life” living at homes and in private or public nursing homes (Persian)]. Salmand: Iranian Journal of Ageing. 2010; 4(4). [Link]
- Kolar P, Kobesova A. Postural-locomotion function in the diagnosis and treatment of movement disorders. Clinical Chiropractic. 2010; 1(13):58-68. [DOI:10.1016/j.clch.2010.02.063]
- Lim YL, Lepsikova M, Singh DKA. Effects of dynamic neuromuscular stabilization on lumbar flexion kinematics and posture among adults with chronic non-specific low back pain: A study protocol. In: Yacob N, Mohd Noor N, Mohd Yunus N, Lob Yussof R, Zakaria S, editors. Regional Conference on Science, Technology and Social Sciences (RCSTSS 2016). Singapore: Springer; 2018. [DOI:10.1007/978-981-13-0074-5_69]
- Frank C, Kobesova A, Kolar P. Dynamic neuromuscular stabilization & sports rehabilitation. International Journal of Sports Physical Therapy. 2013; 8(1):62-73. [PMID]
- Kobesova A, Dzvonik J, Kolar P, Sardina A, Andel R. Effects of shoulder girdle dynamic stabilization exercise on hand muscle strength. Isokinetics and Exercise Science. 2015; 23(1):21-32. [DOI:10.3233/IES-140560]
- Jang H-J, Hughes LC, Oh D-W, Kim S-Y. Effects of corrective exercise for thoracic hyperkyphosis on posture, balance, and well-being in older women: a double-blind, group-matched design. Journal of Geriatric Physical Therapy. 2019; 42(3):E17-27. [DOI: 10.1519/JPT.0000000000000146] [PMID]
- Bezzoli E, Andreotti D, Pianta L, Mascheroni M, Piccinno L, Puricelli L, et al. Motor control exercises of the lumbar-pelvic region improve respiratory function in obese men. A pilot study. Disability Rehabiliation. 2016; 1-7. [DOI: 10.1080/09638288.2016.1244292] [PMID]
- Mongkol S. The effects of yoga training on chest wall expansion and respiratory muscle strength in female subjects. Journal of Associated Medical Sciences. 2016; 49(3):363-9. [DOI: 10.14456/jams.2016.32]
- Mirtz TA. Acute respiratory distress syndrome: Clinical recognition and preventive management in chiropractic acute care practice. Journal of Manipulative and Physiological Therapeutics. 2001; 24(7):467-73. [DOI:10.1067/mmt.2001.117086]
- Fishman RS, Systrom DM. Preoperative cardiopulmonary exercise testing: Determining the limit to exercise and predicting outcome after thoracotomy. Journal of Cardiothoracic and Vascular Anesthesia. 1991; 5(6):614-26. [DOI:10.1016/1053-0770(91)90019-P] [PMID]
- Obayashi H, Urabe Y, Yamanaka Y, Okuma R. Effects of respiratory-muscle exercise on spinal curvature. Journal of Sport Rehabilitation. 2012; 21(1):63-8. [DOI:10.1123/jsr.21.1.63] [PMID]
- Hodges PW, Gandevia SC. Changes in intra-abdominal pressure during postural and respiratory activation of the human diaphragm. Journal of Applied Physiology. 2000; 89(3):967-76. [DOI:10.1152/jappl.2000.89.3.967] [PMID]
- Patroncini M. Impaired trunk muscle function in sub-acute neck pain: Etiologic in the subsequent development of low back pain? Manuelletherapie. 2005; 9(4):187-8. [DOI:10.1055/s-2005-858780]
- Wu S, Wang R, Jiang A, Ding Y, Wu M, Ma X, et al. Abdominal obesity and its association with health-related quality of life in adults: A population-based study in five Chinese cities. Health and Quality of Life Outcomes. 2014; 12:100. [DOI:10.1186/1477-7525-12-100] [PMID]
- Frilander H, Solovieva S, Mutanen P, Pihlajamäki H, Heliövaara M, Viikari-Juntura E. Role of overweight and obesity in low back disorders among men: A longitudinal study with a life course approach. BMJ Open. 2015; 5(8):e007805. [DOI:10.1136/bmjopen-2015-007805] [PMID]
- Nilsen TI, Holtermann A, Mork PJ. Physical exercise, body mass index, and risk of chronic pain in the low back and neck/shoulders: Longitudinal data from the Nord-Trøndelag health study. American Journal of Epidemiology. 2011; 174(3):267-73. [DOI:10.1093/aje/kwr087] [PMID]
Type of Study: Research |
Subject:
General
Received: 2023/10/3 | Accepted: 2024/03/9 | Published: 2024/04/1
Received: 2023/10/3 | Accepted: 2024/03/9 | Published: 2024/04/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






