Sun, May 5, 2024
Volume 13, Issue 1 (Winter 2023)
PTJ 2023, 13(1): 11-22 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Jafari Naeimi A, Ghafari R, Hoseinzadeh M. Investigating the Relationship of Functional Tests With Pain Intensity in Active Women and Men With Non-specific Chronic Low Back Pain. PTJ 2023; 13 (1) :11-22
URL: http://ptj.uswr.ac.ir/article-1-539-en.html
URL: http://ptj.uswr.ac.ir/article-1-539-en.html
1- Department of Physical Education and Sport Sciences, Faculty of Physical Education and Sport Science, Shomal University, Amol, Iran.
2- Department of Sports Injuries and Corrective Exercises, Sport Sciences Research Institute, Tehran, Iran.
2- Department of Sports Injuries and Corrective Exercises, Sport Sciences Research Institute, Tehran, Iran.
Keywords: Chronic non-specific low back pain, Motor function, Functional movement screen, +9, Y balance
Full-Text [PDF 2451 kb]
(256 Downloads)
| Abstract (HTML) (766 Views)
Full-Text: (342 Views)
Introduction
Low back pain is the most common musculoskeletal complication in humans with a prevalence of up to 80% throughout life [1]. In many cases, low back pain may improve without specific medical treatments; however, the recurrence rate of this complication is high [2]. Low back pain is the most common reason for motor restriction in individuals under the age of 45 years and its treatment process requires spending a great amount of money [3, 4, 5]. Low back pain is also one of the most prevalent medical issues in gymnastics, football, volleyball, and tennis athletes. It has been reported that 20% of sports-related injuries involve the spine [6, 7].
Standing and accompanying activities, such as walking, climbing the stairs, and so on are an integral part of daily activities, which require the maintenance and control of the body balance. One of the factors maintaining body balance is controlling the oscillating movements of the trunk around the ankle joint, which is provided by the proper activity of the trunk muscles [8]. The results of various studies examining balance control and postural reactions in individuals with low back pain have revealed that postural stability indices are different in individuals with low back pain compared to healthy people and balance control changes in these individuals [9]. On the other hand, some studies have reported a significant relationship between the change in the control of postural stability and the delayed reaction of the surface muscles of the trunk after a sudden disturbance of the trunk in individuals with low back pain [10].
Cook et al. has recently introduced the functional movement screen (FMS) test as a tool to quantify the quality of functional movement patterns [11]. This set of tests consists of 7 functional and fundamental movements, the implementation of which requires balance, stability, mobility, and movement control [11]. Given its non-invasiveness, inexpensiveness, and ease of scoring and implementation, this test is a suitable tool for the qualitative assessment of functional movement patterns by identifying limitations, asymmetry, and pain during functional movements [11]. Although this test is not diagnostic, it is used solely as a screening tool and a starting point for musculoskeletal evaluations [12]. The relevant literature has reported the appropriate and acceptable reliability and validity of this test in quantifying the quality of functional movement patterns [13].
Armstrong et al. (2020) dealt with the relationship between the scores of the FMS and Y balance tests with the Beighton hypermobility test in women dancers and concluded that some FMS tests, such as deep squats, shoulder flexibility, and straight leg raising require upper joint mobility [14].
Soltandoost et al. (2020) investigated the relationship between FMS and pain, endurance, and dynamic balance of the core stability muscles in military personnel with and without non-specific chronic low back pain. The results showed that pain is negatively associated with FMS scores, and the FMS test is positively significant about dynamic balance and endurance of core stability muscles; therefore, they concluded that FMS is an effective tool for identifying functional defects in military personnel suffering from non-specific chronic low back pain [15].
Since the FMS tests could not specifically assess the spine, especially the lumbopelvic hip area, the researchers introduced the +9 tests. In the +9 test, researchers have tried to add new tests and remove redundant and unnecessary ones, introducing a series of more appropriate tests to evaluate athletes’ performance [16]. The +9 tests consist of 6 FMS tests along with 3 other tests that are designed to challenge and test the dynamic performance of trunk flexors and spine rotators. Thus, the number of these tests has reached +9 tests which aims to increase the performance of this series of tests [17, 18]. Given the novelty of the +9 functional test, there is a lack of research in this area. Most of the studies have investigated the validity and reliability of this test [16, 19].
According to the studies conducted on low back pain in recent years, no study has so far investigated the relationship between functional tests and non-specific chronic low back pain. Therefore, this study aims to investigate the relationship between functional test results and pain intensity in active women and men with non-specific chronic low back pain.
Materials and Methods
The present study is cross-sectional and correlational. This study used the purposive sampling method to select the participants based on the inclusion and exclusion criteria. The participants included men and women who referred to the Alef-Gym Fitness Club in Babol city, Iran. Among the above statistical population, according to the inclusion and exclusion criteria, 80 men and women with non-specific chronic low back pain, diagnosed by a specialist, were purposefully selected to participate in the study. To determine the sample size, we employed the G*Power software, version 3.1.9.4. The power of the test and the starting point of the effect size were determined at 0.80 and 1.02, respectively. The effect size in previous studies [20, 21, 22] is between 0.89 and 0.65, and the starting point of the effect size was determined to have a significant sample size of 1.02; thus, the sample size was calculated at 80 subjects. The inclusion criteria were being in the age range of 20 to 35 years, having recreational sports activity twice a week during the last year, voluntary and informed consent of the subjects to participate in the study, reporting pain in the lower back between the lower back and chest (as the pain in the visual analogue scale index is above 2) at least during the last 6 months or more and confirmed by a specialist [23], a history of surgery in the last 6 months in the lower limbs, and the absence of COVID-19 disease. Moreover, the exclusion criteria were having pain above 7 on the visual analogue scale (VAS) index.
The subjects had a history of sports activities in different disciplines only for fun and twice a week during the past year, and none of them had exercised professionally.
To measure the research variables, the participants were asked to attend according to the specified schedule at the Alef-Gym Fitness Club in Babol city, Iran. After the presence of the subjects, the basic information form was first completed by each participant. Then, the anthropometric measurements of each person were done. FMS, +9, and Y balance tests were used to evaluate the subjects’ performance.
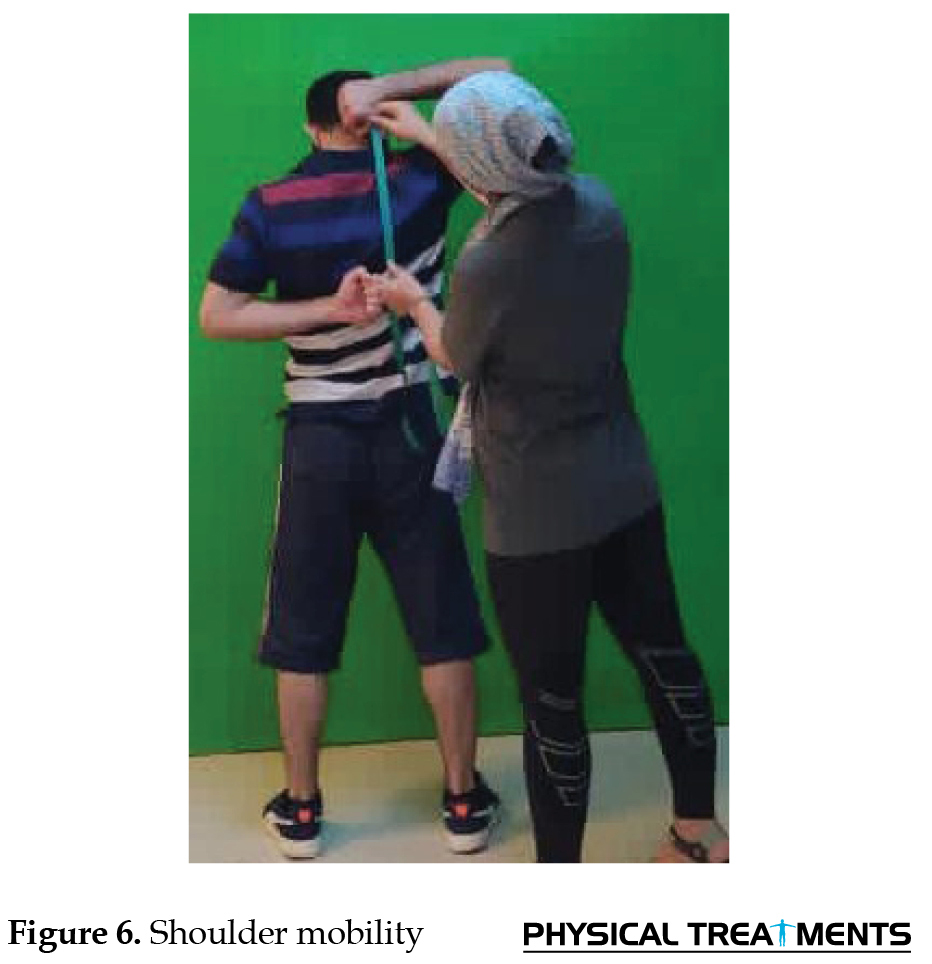
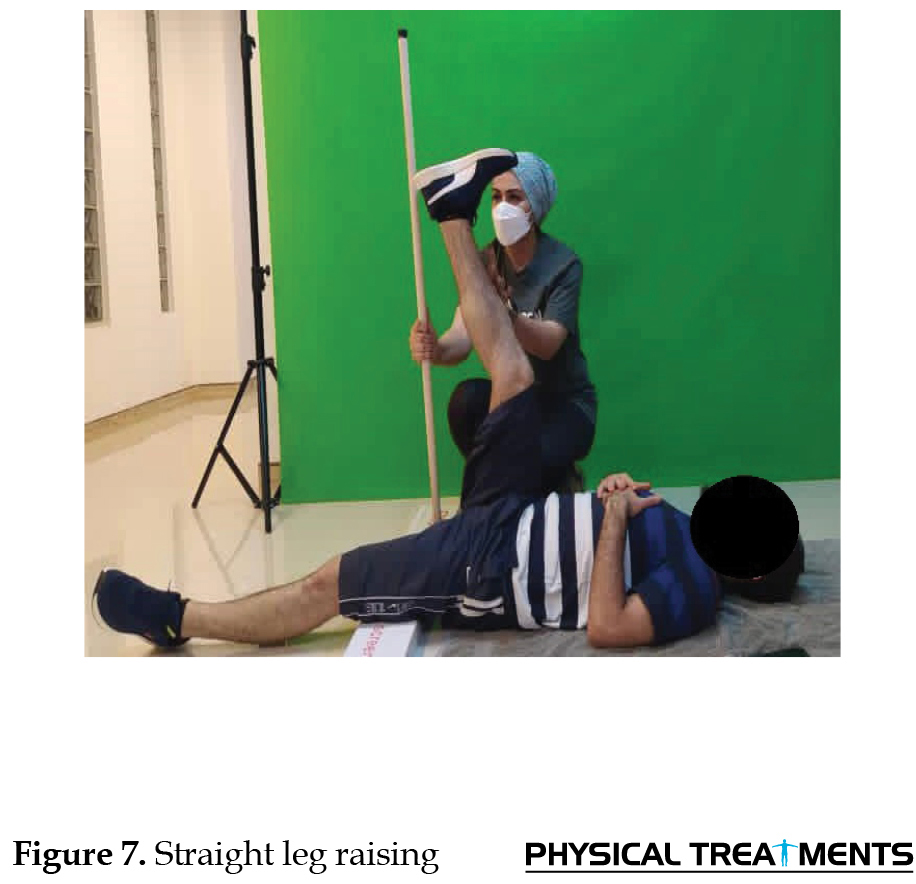
The FMS tests included 7 movement tests that can diagnose limitations and changes in normal movement patterns. These tests were considered for the interaction between the mobility of the movement chain and the stability necessary to implement functional and necessary movement patterns. In the FMS test, if the tests were performed correctly and without compensatory movements, a score of 3 was given, if a movement was performed with compensatory movements, a score of 2 was awarded, and if the person could not carry out a movement without compensatory movements, a score of 1 was awarded, and if the subjects felt pain while performing the movement or performing the detection test, they would not receive points. These tests included deep squats, hurdle steps, inline lunges, shoulder mobility, active leg raising, rotary stability, and push up [24]. Tests of FMS and +9 are presented in Figures 1-10. +9 test
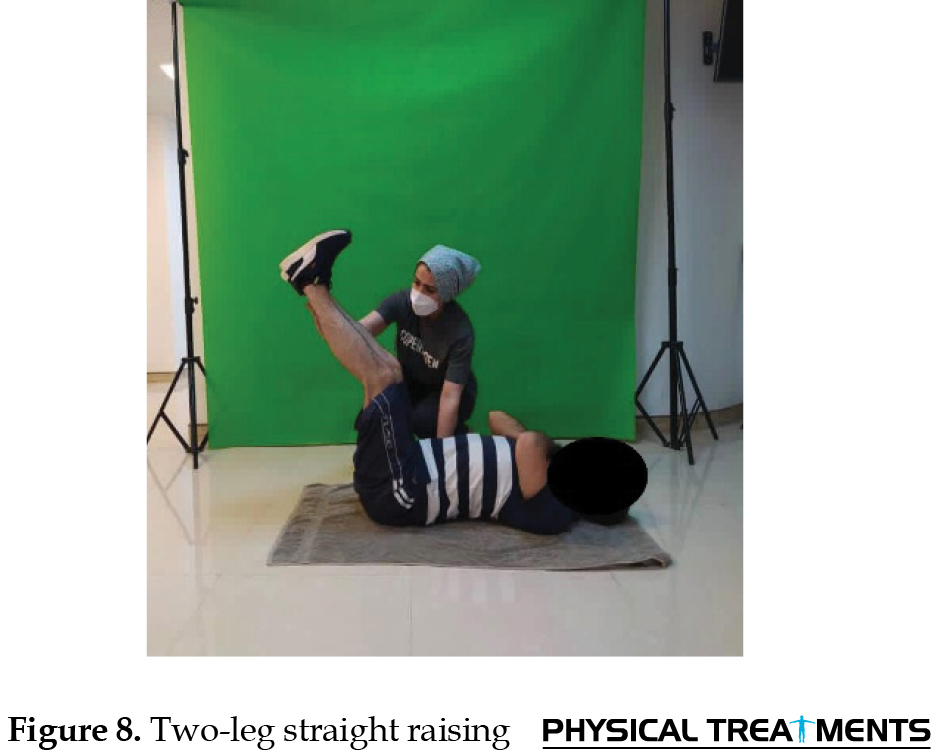
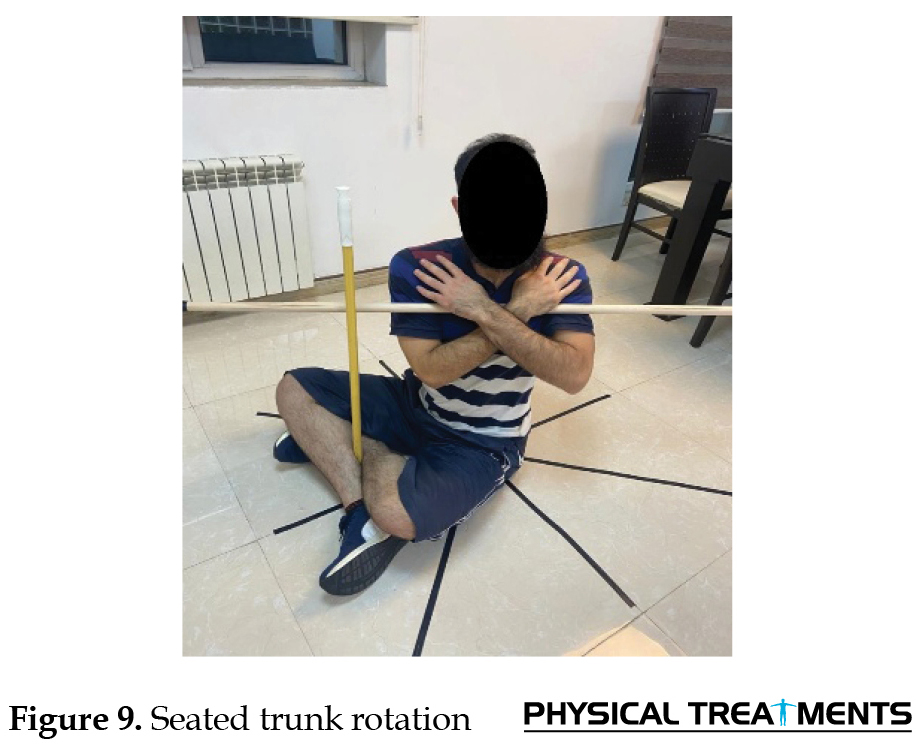
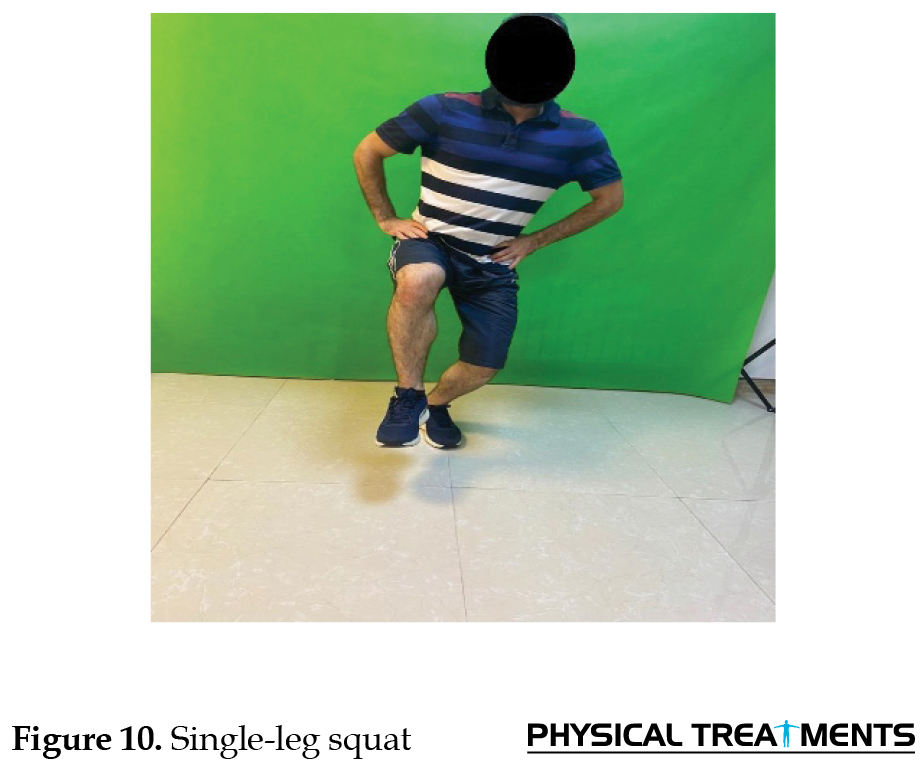
Among the +9 tests, six tests are the same as FMS tests, which include deep squat, hurdle step, inline lunge, shoulder mobility, active leg raising, rotary stability, and push up, and 3 tests of seated trunk rotation, single-leg squat test, and two-leg straight raising test (Figure 8-10) have been added to the FMS tests.
Y balance test
Performing this test requires strength, flexibility, neuromuscular control, core stability, balance, and a sense of depth; thus, it is an appropriate test for pre-season and medical evaluations [25].
The intra-rater and inter-rater reliability coefficients for different aspects were 0.85 to 0.91 and 0.99 to 1.00, respectively. Moreover, the intra-rater and inter-rater reliability coefficients for the composite score (total test score) were mentioned by Pliski to be 0.91 and 0.99, respectively [26].
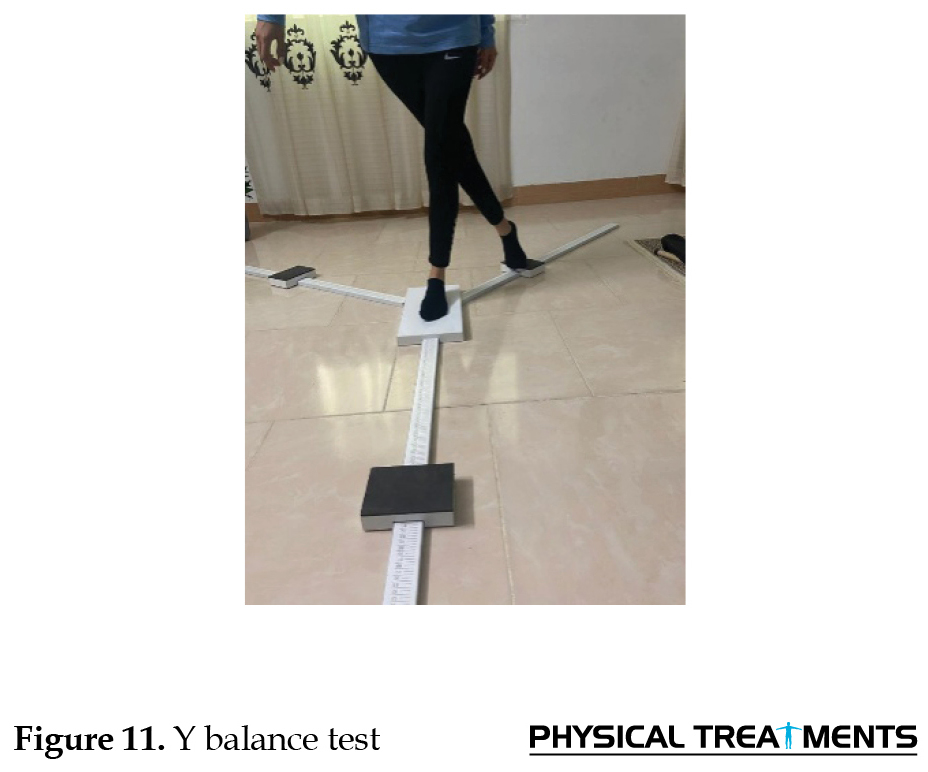
This test is performed in 3 directions: Anterior, posterior-internal, and posterior-external; however, in this study, only the total score obtained from the mean of the 3 directions was calculated. In this test, the subject stands on one leg in the center of Y and tries to reach the other leg while maintaining balance on the supporting leg. The subject touches the farthest possible point with his toe in each of the designated directions without error. The reach distance is defined as the distance from the point of touch to the center, which is measured in centimeters. To minimize the learning effects, each subject practices this test 6 times with a 15-s rest interval in each of the three directions. After a 5-min rest, the subject performed the main test in the main directions. In case of any error, if the leg that was in the center moves or the person’s balance is disturbed, the subject was asked to repeat the test. Considering that this test has a significant relationship with the length of the leg, to perform this test and normalize the data, before starting the measurement process, using a tape measure, we measure the actual length of the leg from the upper anterior cruciate ligament to the inner ankle in an arched position. This was measured while the subject was lying on the ground [27]. In this study, the mean reach was assessed in 3 directions and the total balance score was calculated (Figure 11). Finally, to measure the intensity of pain, the visual pain intensity scale was applied [28]. This scale is regarded to be both the most reliable and easiest method to subjectively measure the intensity of pain. In this method, a 10 cm ruler was placed in front of the subject. Then, it was explained to the participant that as the number increases, the intensity of the pain escalates; accordingly, the number zero indicates “no pain” while the number 10 indicates the greatest intensity of pain in this area. Based on the explanations presented and the intensity of the pain in the lower back, the subject chooses the desired number and the researcher recorded this number [28]
Finally, the Spearman correlation coefficient tests were used at a significance level of P<0.05 to investigate the relationship between the visual analogue scale pain index and the aforementioned functional tests because of the non-normality of the data. The data were analyzed using the SPSS software, version 21.
Results
The participants’ demographic characteristics are given in Table 1.
.jpg)
The Mean±SD of the variables are given in Table 2.
.jpg)
The Kolmogorov-Smirnov test was applied to check the normality of the data. The results indicated that the data related to the research variables had no normal distribution. Thus, the assumption of using parametric tests was not met, and the non-parametric Spearman correlation test was used to check the relationship between the variables. According to Table 3, a significant relationship exists between the results of all FMS and +9 functional tests with the intensity of low back pain except the shoulder mobility test (P=0.40, r=0.09).
.jpg)
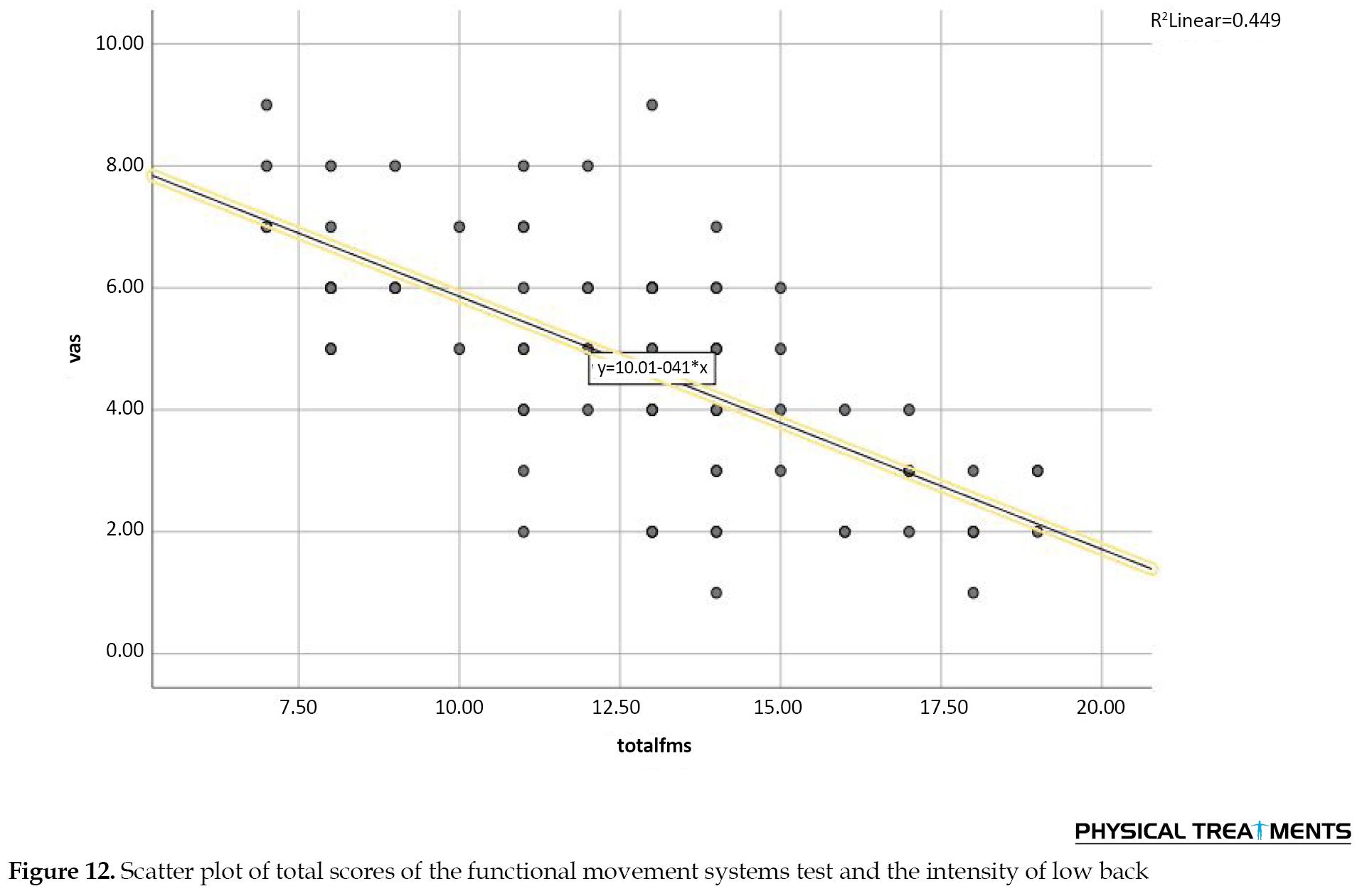
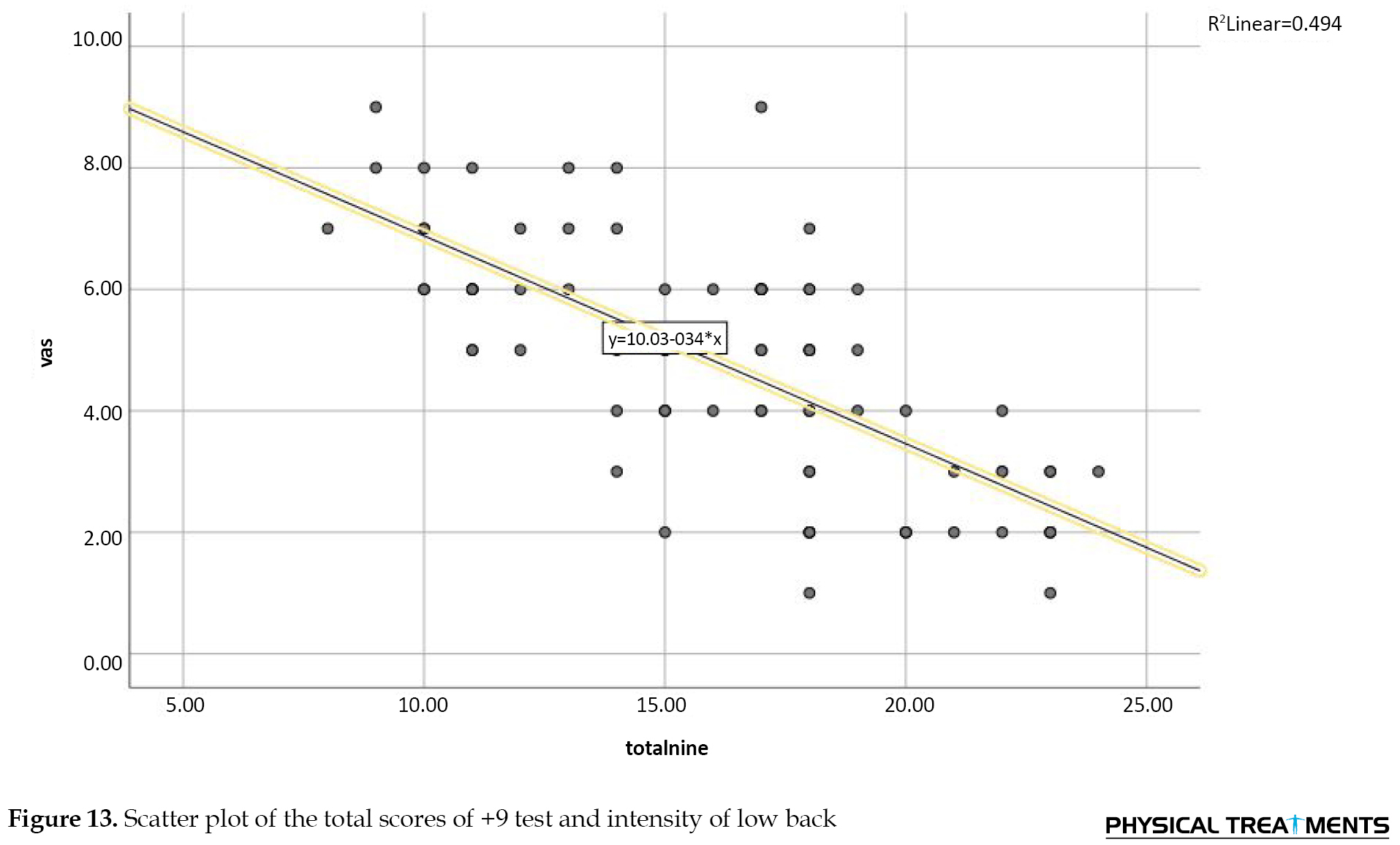
Furthermore, a significantly negative relationship was detected between the results of the total scores of the tests of FMS and +9 and Y balance with the intensity of low back pain (P=0.001, r=-0.66; P=0.001, r=-0.71; P=0.001, r=-0.71, respectively).
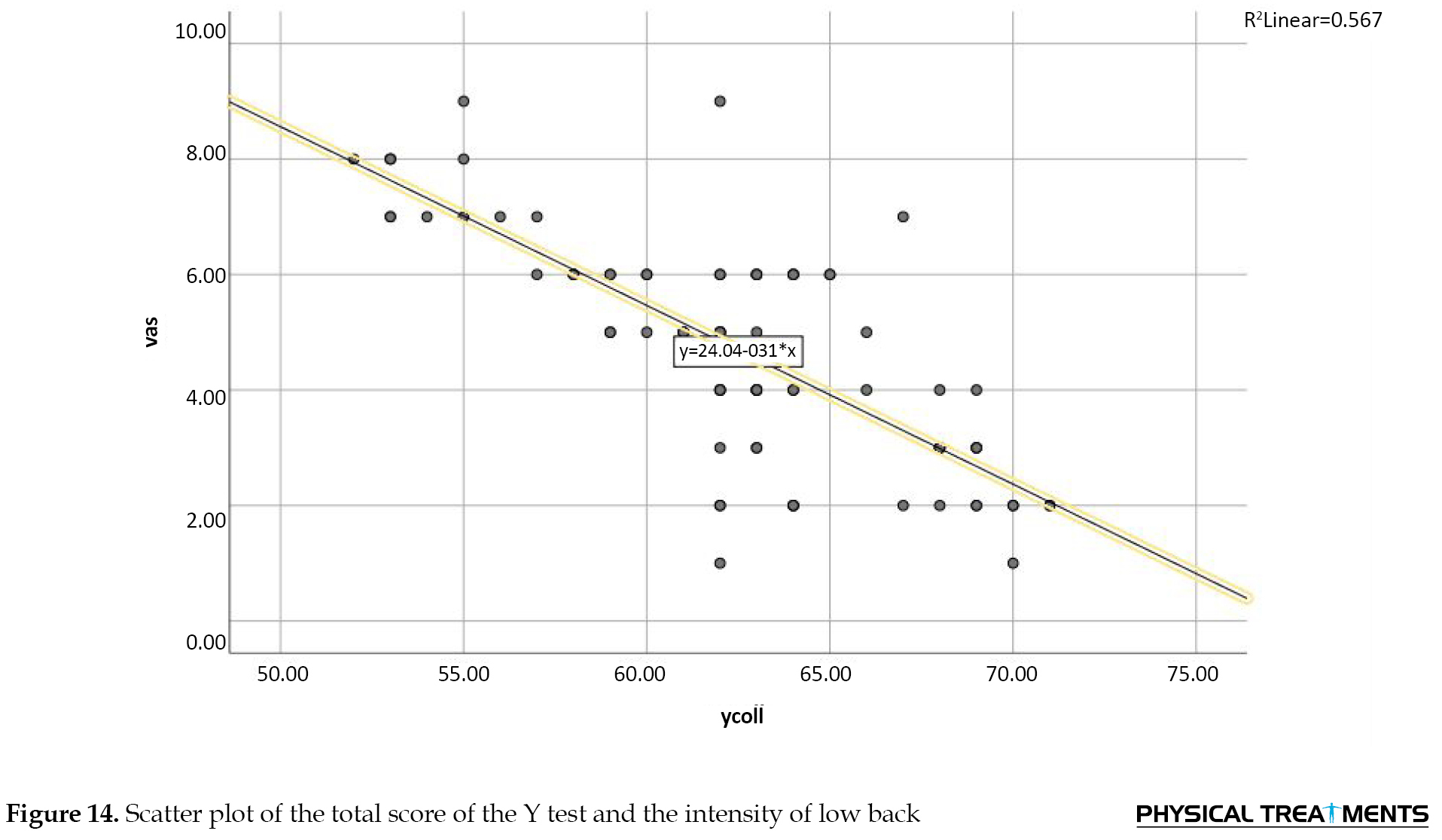
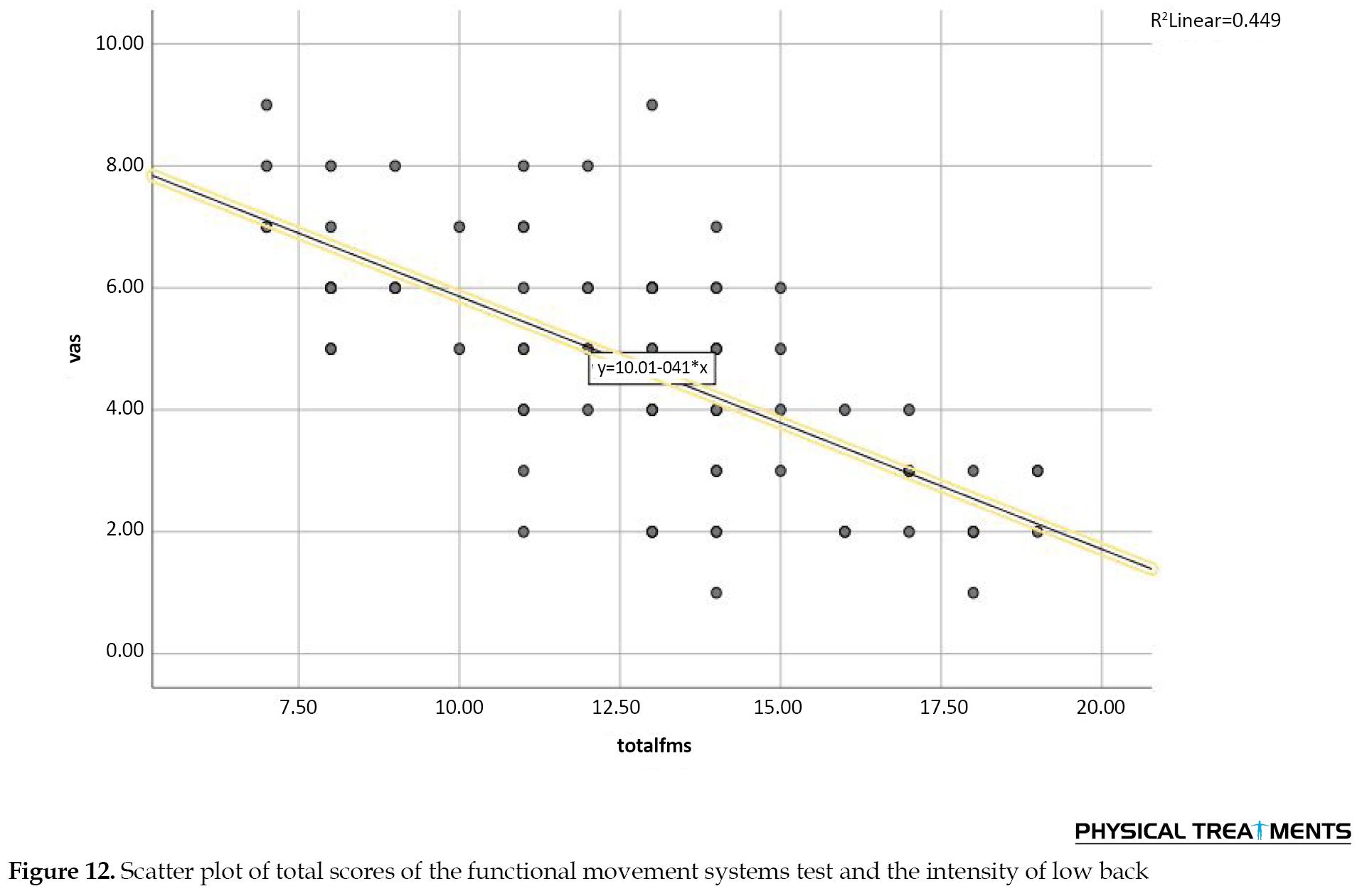
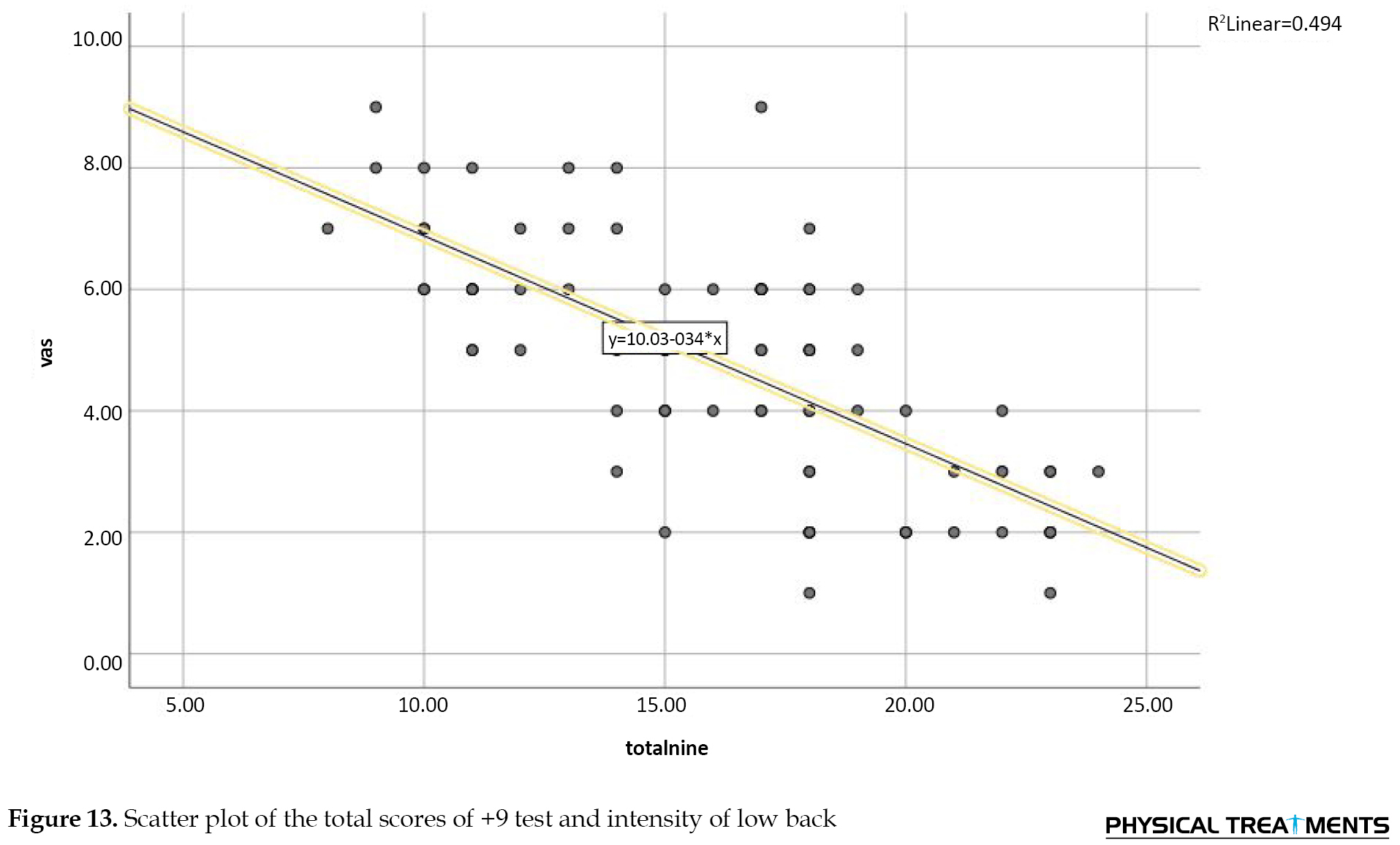
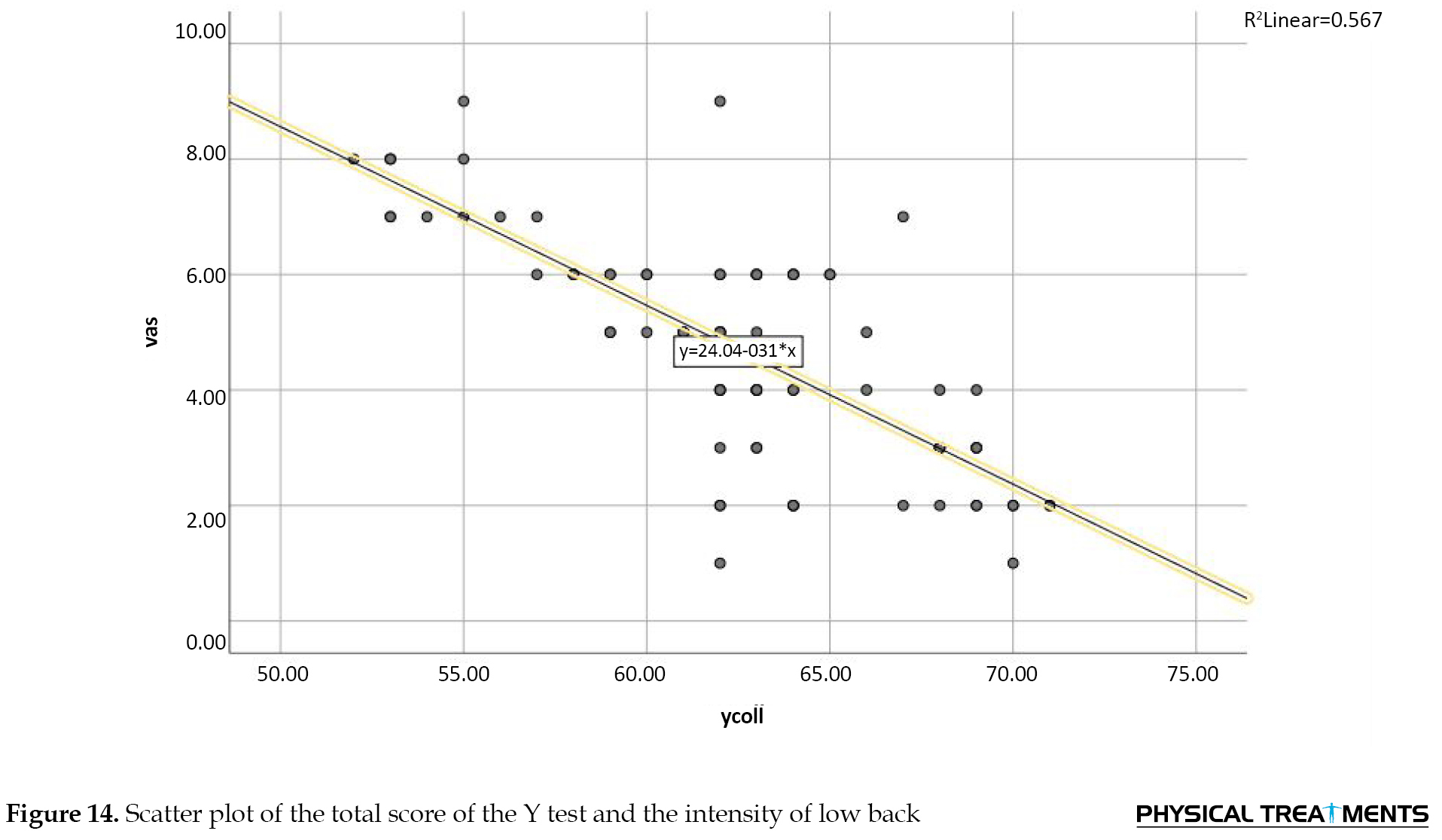
Figures 12, 13, and 14 show the amount of dispersion between the total score of the FMS, +9, and Y balance tests with the intensity of low back pain. As seen, there is a negative linear relationship between the two variables, i.e. the increase in the total score of the FMS, +9, and Y balance tests has been associated with a decrease in the intensity of low back pain.
Discussion
The findings of this study showed a significant relationship in all FMS and +9 tests except for the shoulder mobility test (P=0.40) with the intensity of low back in men and women. In addition, a significant relationship existed between the total scores of the FMS, +9, and Y balance tests along with the intensity of low back of women and men.
The findings of this study are in line with results of Sedaghati et al. (2016) [29], Saki et al. (2018) [30], Michel et al. (2019) [31], Ko et al. (2016) [22], Ehsani et al. (2017) [32], Berenshteyn et al. (2019) [20], Emami et al. (2018) [33], and Kramer et al. (2020) [34].
Based on the study’s findings, the FMS and +9 tests can screen and measure the individuals’ basic movement capacity, based on which it is possible to identify the areas that have defects in terms of mobility and stability [35]. The shoulder mobility test includes the unilateral and reciprocal performance of the range of motion of the shoulder joint, involving internal rotation of the shoulder, adduction in one shoulder, external rotation of the shoulder, and abduction in the other shoulder. This test requires normal mobility of the scapula and extending of the spine. The push-up test is the stability of the trunk and spine in the front and back in activities of the closed kinetic chain of the upper limbs. This test assesses the stability of the trunk in the sagittal plane, while the symmetry in the movements of the upper limbs during performing this movement is considered. In this test, the function is very important because if the trunk does not have enough stability in sports activities, the kinetic energy will be wasted and will lead to weak functional movements and eventually cause minor damages and injuries [36].
In the deep squat test, coordination and mobility between organs and muscles, core stability, and total body mechanics in neuromuscular control, and mobility and stability of the shoulder, scapula, and thoracic spine area are required [11]. A person’s poor performance in deep squats can be caused by 3 factors as follows: 1) limitation in the mobility of the upper limb and weakness in the glenohumeral; 2) limitation in the mobility of the lower limb; and 3) limitation in the motor control of the core stability area [11]. In the lunge test, limitations in the thoracic spine area and reduced mobility of the thighs, knees, and ankles, as well as defects in the function of the core stability area can be among the reasons for a decrease in FMS scores. In the push-up test, the strength of the upper limbs and the core stability are of great importance [11].
In the rotary stability test, neuromuscular coordination and energy transfer in the whole body (from the upper to the lower limb and vice versa) and checking the trunk stability in several planes are important. Additionally, weakness in trunk stability, difficulty in shoulder and hip stability, and difficulty in the mobility of the knee, thigh, and trunk are among the reasons for weakness in this test [11]. In rotating the trunk and raising the leg straightly, the range of motion of the lumbar spine and inter-muscular coordination, and the strength of the core stability muscles are respectively among the important score factors in these tests.
According to the above explanations, in many FMS and +9 tests, the performance of the core stability muscles is of great importance; however, in people with low back pain, the muscles of the core stability area are delayed in activation. This delay in the activation of muscles will probably lead to defects in the quality of motor patterns and a decrease in the scores of the FMS and +9 tests; therefore, a significantly negative correlation between the scores of the functional tests of +9 and FMS with the low back pain level of individuals is conceivable, and only in the shoulder mobility and single-leg squat tests, the core stability muscles are not directly involved in the movement.
Core stability plays an important role in preventing injuries [37]. Maintaining positional alignment and dynamic postural balance during functional activities is one of the tasks of the core body area, which helps prevent wrong patterns [38] Asymmetry in position and movement does not allow the core area to be stable [38]. Limitations in the strength and stability of the deep muscles of the core stability area lead to incorrect exercise techniques and make the person prone to injury [39]. An optimal core area maintains the normal length-tension relationship of the agonist and antagonist muscles, resulting in optimal kinematics of the joints in the waist-hip and thigh complex in the movements of the functional chain of motor and creating maximum stability for the movements of the lower limbs [38]. The core stability area as an interface with the adequate transfer of force generated in the lower limb to the upper limb via the trunk assists to perform a function better [40]. The results revealed that stability muscles before lower limb movers and in all motor plates increase the stiffness of the spine in creating a stable support. These findings are consistent with the closed kinetic chain theory. Studies have shown that a decrease in strength in the muscles of the core area causes an increase in body fluctuations, and as a result, it may cause a disturbance in body balance. As mentioned, the weakness or lack of sufficient coordination in the muscle structure of the core body area can lead to a decrease in the effectiveness of correct motor patterns, the occurrence of compensatory motor patterns, and ultimately dysfunction. Accordingly, it can be concluded that the weakness of core stabilizing muscles can have a negative effect on motor patterns. Therefore, the study’s findings can be confirmed according to the mentioned cases, and individuals’ weakness of the core stability muscles with non-specific chronic low back pain has led to the occurrence of incorrect and compensatory motor patterns in the FMS and +9 functional tests.
Furthermore, according to the researchers’ studies, the existence of low back pain puts the patient in a vicious cycle as patients with chronic low back pain because of long-term pain (more than 3 months). With limitations in motor function even in daily activities, they face problems and the physical activity of this population is seriously limited. The core stability muscles are the first muscles to suffer dysfunction when low back pain occurs, and since these muscles guide the joint in different motor patterns and motor function caused by these different patterns, their damage causes damage to the joint’s function and finally functional disabilities occur in movements [41].
Considering the significant relationship between the Y balance test and the amount of low back pain, studies have reported that the core body section is the basis of the kinetic chain and the endurance of the muscles in this area is important for motor function and providing stability and dynamic balance of the body. In 2011, Ruh and his colleagues in a review study investigated balance and postural control based on the range of pressure centers in people with low back pain and healthy people. The results showed that in most of the articles (14.16, 88%), the mean speed of displacement of the pressure center in people with low back pain was significantly higher than in healthy people. In addition, in people with low back pain, an increase in fluctuation in the anterior-posterior plate was also seen [38].
The difference in the frontal plate can be due to the important role of the hip abductor muscles in maintaining balance while standing on one leg and in dynamic functions, such as walking. The gluteus medius muscle plays the role of thigh abductor and hip stabilizer in the frontal plate and is especially important when standing, especially standing on one leg. On the other hand, the hip joint and trunk are mostly responsible for controlling and maintaining balance in the frontal plate, so the hip joint and the gluteus medius muscle play an important role in maintaining balance when forcing pressure on this plate [42]. In addition, according to Tak, the weakness of the gluteus medius muscle is common in individuals with specific chronic low back pain [43], and the existence of these cases can confirm a significant relationship between the Y balance test scores and the amount of pain in individuals with non-specific chronic low back pain.
Study limitations
The limitations of the present study include the spread of COVID-19 and the small number of participants. Therefore, it is suggested that after the end of the COVID-19 outbreak, researchers should conduct the present study with a larger number of subjects so that the results can be generalized more strongly. It is also recommended to investigate the prediction of low back pain by the functional tests of the present study in future research.
Conclusion
According to the study’s findings, there is a significantly negative relationship between the functional tests of +9, FMS, and Y balance with the intensity of low back pain in active women and men. Therefore, by improving the quality of motor patterns and performing balance exercises, it is possible to reduce the amount of pain in people with non-specific chronic low back pain.
Ethical Considerations
Compliance with ethical guidelines
The present study was registered at Iranian Registry of Clinical Trials (Code: IR.SSRC.REC.1401.026).
Funding
This study was extracted from the MA thesis of Atefeh Jafari Naeimi approved by Department of Physical Education and Sport Sciences, Shomal University.
Authors' contributions
Conceptualization and data collection: Atefeh Jafari Naeimi; Study design: All authors; Results interpretation: Mehdi Hosseinzadeh.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We are grateful to all the people who helped us in this project.
References
Low back pain is the most common musculoskeletal complication in humans with a prevalence of up to 80% throughout life [1]. In many cases, low back pain may improve without specific medical treatments; however, the recurrence rate of this complication is high [2]. Low back pain is the most common reason for motor restriction in individuals under the age of 45 years and its treatment process requires spending a great amount of money [3, 4, 5]. Low back pain is also one of the most prevalent medical issues in gymnastics, football, volleyball, and tennis athletes. It has been reported that 20% of sports-related injuries involve the spine [6, 7].
Standing and accompanying activities, such as walking, climbing the stairs, and so on are an integral part of daily activities, which require the maintenance and control of the body balance. One of the factors maintaining body balance is controlling the oscillating movements of the trunk around the ankle joint, which is provided by the proper activity of the trunk muscles [8]. The results of various studies examining balance control and postural reactions in individuals with low back pain have revealed that postural stability indices are different in individuals with low back pain compared to healthy people and balance control changes in these individuals [9]. On the other hand, some studies have reported a significant relationship between the change in the control of postural stability and the delayed reaction of the surface muscles of the trunk after a sudden disturbance of the trunk in individuals with low back pain [10].
Cook et al. has recently introduced the functional movement screen (FMS) test as a tool to quantify the quality of functional movement patterns [11]. This set of tests consists of 7 functional and fundamental movements, the implementation of which requires balance, stability, mobility, and movement control [11]. Given its non-invasiveness, inexpensiveness, and ease of scoring and implementation, this test is a suitable tool for the qualitative assessment of functional movement patterns by identifying limitations, asymmetry, and pain during functional movements [11]. Although this test is not diagnostic, it is used solely as a screening tool and a starting point for musculoskeletal evaluations [12]. The relevant literature has reported the appropriate and acceptable reliability and validity of this test in quantifying the quality of functional movement patterns [13].
Armstrong et al. (2020) dealt with the relationship between the scores of the FMS and Y balance tests with the Beighton hypermobility test in women dancers and concluded that some FMS tests, such as deep squats, shoulder flexibility, and straight leg raising require upper joint mobility [14].
Soltandoost et al. (2020) investigated the relationship between FMS and pain, endurance, and dynamic balance of the core stability muscles in military personnel with and without non-specific chronic low back pain. The results showed that pain is negatively associated with FMS scores, and the FMS test is positively significant about dynamic balance and endurance of core stability muscles; therefore, they concluded that FMS is an effective tool for identifying functional defects in military personnel suffering from non-specific chronic low back pain [15].
Since the FMS tests could not specifically assess the spine, especially the lumbopelvic hip area, the researchers introduced the +9 tests. In the +9 test, researchers have tried to add new tests and remove redundant and unnecessary ones, introducing a series of more appropriate tests to evaluate athletes’ performance [16]. The +9 tests consist of 6 FMS tests along with 3 other tests that are designed to challenge and test the dynamic performance of trunk flexors and spine rotators. Thus, the number of these tests has reached +9 tests which aims to increase the performance of this series of tests [17, 18]. Given the novelty of the +9 functional test, there is a lack of research in this area. Most of the studies have investigated the validity and reliability of this test [16, 19].
According to the studies conducted on low back pain in recent years, no study has so far investigated the relationship between functional tests and non-specific chronic low back pain. Therefore, this study aims to investigate the relationship between functional test results and pain intensity in active women and men with non-specific chronic low back pain.
Materials and Methods
The present study is cross-sectional and correlational. This study used the purposive sampling method to select the participants based on the inclusion and exclusion criteria. The participants included men and women who referred to the Alef-Gym Fitness Club in Babol city, Iran. Among the above statistical population, according to the inclusion and exclusion criteria, 80 men and women with non-specific chronic low back pain, diagnosed by a specialist, were purposefully selected to participate in the study. To determine the sample size, we employed the G*Power software, version 3.1.9.4. The power of the test and the starting point of the effect size were determined at 0.80 and 1.02, respectively. The effect size in previous studies [20, 21, 22] is between 0.89 and 0.65, and the starting point of the effect size was determined to have a significant sample size of 1.02; thus, the sample size was calculated at 80 subjects. The inclusion criteria were being in the age range of 20 to 35 years, having recreational sports activity twice a week during the last year, voluntary and informed consent of the subjects to participate in the study, reporting pain in the lower back between the lower back and chest (as the pain in the visual analogue scale index is above 2) at least during the last 6 months or more and confirmed by a specialist [23], a history of surgery in the last 6 months in the lower limbs, and the absence of COVID-19 disease. Moreover, the exclusion criteria were having pain above 7 on the visual analogue scale (VAS) index.
The subjects had a history of sports activities in different disciplines only for fun and twice a week during the past year, and none of them had exercised professionally.
To measure the research variables, the participants were asked to attend according to the specified schedule at the Alef-Gym Fitness Club in Babol city, Iran. After the presence of the subjects, the basic information form was first completed by each participant. Then, the anthropometric measurements of each person were done. FMS, +9, and Y balance tests were used to evaluate the subjects’ performance.
The FMS tests included 7 movement tests that can diagnose limitations and changes in normal movement patterns. These tests were considered for the interaction between the mobility of the movement chain and the stability necessary to implement functional and necessary movement patterns. In the FMS test, if the tests were performed correctly and without compensatory movements, a score of 3 was given, if a movement was performed with compensatory movements, a score of 2 was awarded, and if the person could not carry out a movement without compensatory movements, a score of 1 was awarded, and if the subjects felt pain while performing the movement or performing the detection test, they would not receive points. These tests included deep squats, hurdle steps, inline lunges, shoulder mobility, active leg raising, rotary stability, and push up [24]. Tests of FMS and +9 are presented in Figures 1-10. +9 test
Among the +9 tests, six tests are the same as FMS tests, which include deep squat, hurdle step, inline lunge, shoulder mobility, active leg raising, rotary stability, and push up, and 3 tests of seated trunk rotation, single-leg squat test, and two-leg straight raising test (Figure 8-10) have been added to the FMS tests.
Y balance test
Performing this test requires strength, flexibility, neuromuscular control, core stability, balance, and a sense of depth; thus, it is an appropriate test for pre-season and medical evaluations [25].
The intra-rater and inter-rater reliability coefficients for different aspects were 0.85 to 0.91 and 0.99 to 1.00, respectively. Moreover, the intra-rater and inter-rater reliability coefficients for the composite score (total test score) were mentioned by Pliski to be 0.91 and 0.99, respectively [26].
This test is performed in 3 directions: Anterior, posterior-internal, and posterior-external; however, in this study, only the total score obtained from the mean of the 3 directions was calculated. In this test, the subject stands on one leg in the center of Y and tries to reach the other leg while maintaining balance on the supporting leg. The subject touches the farthest possible point with his toe in each of the designated directions without error. The reach distance is defined as the distance from the point of touch to the center, which is measured in centimeters. To minimize the learning effects, each subject practices this test 6 times with a 15-s rest interval in each of the three directions. After a 5-min rest, the subject performed the main test in the main directions. In case of any error, if the leg that was in the center moves or the person’s balance is disturbed, the subject was asked to repeat the test. Considering that this test has a significant relationship with the length of the leg, to perform this test and normalize the data, before starting the measurement process, using a tape measure, we measure the actual length of the leg from the upper anterior cruciate ligament to the inner ankle in an arched position. This was measured while the subject was lying on the ground [27]. In this study, the mean reach was assessed in 3 directions and the total balance score was calculated (Figure 11). Finally, to measure the intensity of pain, the visual pain intensity scale was applied [28]. This scale is regarded to be both the most reliable and easiest method to subjectively measure the intensity of pain. In this method, a 10 cm ruler was placed in front of the subject. Then, it was explained to the participant that as the number increases, the intensity of the pain escalates; accordingly, the number zero indicates “no pain” while the number 10 indicates the greatest intensity of pain in this area. Based on the explanations presented and the intensity of the pain in the lower back, the subject chooses the desired number and the researcher recorded this number [28]
Finally, the Spearman correlation coefficient tests were used at a significance level of P<0.05 to investigate the relationship between the visual analogue scale pain index and the aforementioned functional tests because of the non-normality of the data. The data were analyzed using the SPSS software, version 21.
Results
The participants’ demographic characteristics are given in Table 1.
.jpg)
The Mean±SD of the variables are given in Table 2.
.jpg)
The Kolmogorov-Smirnov test was applied to check the normality of the data. The results indicated that the data related to the research variables had no normal distribution. Thus, the assumption of using parametric tests was not met, and the non-parametric Spearman correlation test was used to check the relationship between the variables. According to Table 3, a significant relationship exists between the results of all FMS and +9 functional tests with the intensity of low back pain except the shoulder mobility test (P=0.40, r=0.09).
.jpg)
Furthermore, a significantly negative relationship was detected between the results of the total scores of the tests of FMS and +9 and Y balance with the intensity of low back pain (P=0.001, r=-0.66; P=0.001, r=-0.71; P=0.001, r=-0.71, respectively).
Figures 12, 13, and 14 show the amount of dispersion between the total score of the FMS, +9, and Y balance tests with the intensity of low back pain. As seen, there is a negative linear relationship between the two variables, i.e. the increase in the total score of the FMS, +9, and Y balance tests has been associated with a decrease in the intensity of low back pain.
Discussion
The findings of this study showed a significant relationship in all FMS and +9 tests except for the shoulder mobility test (P=0.40) with the intensity of low back in men and women. In addition, a significant relationship existed between the total scores of the FMS, +9, and Y balance tests along with the intensity of low back of women and men.
The findings of this study are in line with results of Sedaghati et al. (2016) [29], Saki et al. (2018) [30], Michel et al. (2019) [31], Ko et al. (2016) [22], Ehsani et al. (2017) [32], Berenshteyn et al. (2019) [20], Emami et al. (2018) [33], and Kramer et al. (2020) [34].
Based on the study’s findings, the FMS and +9 tests can screen and measure the individuals’ basic movement capacity, based on which it is possible to identify the areas that have defects in terms of mobility and stability [35]. The shoulder mobility test includes the unilateral and reciprocal performance of the range of motion of the shoulder joint, involving internal rotation of the shoulder, adduction in one shoulder, external rotation of the shoulder, and abduction in the other shoulder. This test requires normal mobility of the scapula and extending of the spine. The push-up test is the stability of the trunk and spine in the front and back in activities of the closed kinetic chain of the upper limbs. This test assesses the stability of the trunk in the sagittal plane, while the symmetry in the movements of the upper limbs during performing this movement is considered. In this test, the function is very important because if the trunk does not have enough stability in sports activities, the kinetic energy will be wasted and will lead to weak functional movements and eventually cause minor damages and injuries [36].
In the deep squat test, coordination and mobility between organs and muscles, core stability, and total body mechanics in neuromuscular control, and mobility and stability of the shoulder, scapula, and thoracic spine area are required [11]. A person’s poor performance in deep squats can be caused by 3 factors as follows: 1) limitation in the mobility of the upper limb and weakness in the glenohumeral; 2) limitation in the mobility of the lower limb; and 3) limitation in the motor control of the core stability area [11]. In the lunge test, limitations in the thoracic spine area and reduced mobility of the thighs, knees, and ankles, as well as defects in the function of the core stability area can be among the reasons for a decrease in FMS scores. In the push-up test, the strength of the upper limbs and the core stability are of great importance [11].
In the rotary stability test, neuromuscular coordination and energy transfer in the whole body (from the upper to the lower limb and vice versa) and checking the trunk stability in several planes are important. Additionally, weakness in trunk stability, difficulty in shoulder and hip stability, and difficulty in the mobility of the knee, thigh, and trunk are among the reasons for weakness in this test [11]. In rotating the trunk and raising the leg straightly, the range of motion of the lumbar spine and inter-muscular coordination, and the strength of the core stability muscles are respectively among the important score factors in these tests.
According to the above explanations, in many FMS and +9 tests, the performance of the core stability muscles is of great importance; however, in people with low back pain, the muscles of the core stability area are delayed in activation. This delay in the activation of muscles will probably lead to defects in the quality of motor patterns and a decrease in the scores of the FMS and +9 tests; therefore, a significantly negative correlation between the scores of the functional tests of +9 and FMS with the low back pain level of individuals is conceivable, and only in the shoulder mobility and single-leg squat tests, the core stability muscles are not directly involved in the movement.
Core stability plays an important role in preventing injuries [37]. Maintaining positional alignment and dynamic postural balance during functional activities is one of the tasks of the core body area, which helps prevent wrong patterns [38] Asymmetry in position and movement does not allow the core area to be stable [38]. Limitations in the strength and stability of the deep muscles of the core stability area lead to incorrect exercise techniques and make the person prone to injury [39]. An optimal core area maintains the normal length-tension relationship of the agonist and antagonist muscles, resulting in optimal kinematics of the joints in the waist-hip and thigh complex in the movements of the functional chain of motor and creating maximum stability for the movements of the lower limbs [38]. The core stability area as an interface with the adequate transfer of force generated in the lower limb to the upper limb via the trunk assists to perform a function better [40]. The results revealed that stability muscles before lower limb movers and in all motor plates increase the stiffness of the spine in creating a stable support. These findings are consistent with the closed kinetic chain theory. Studies have shown that a decrease in strength in the muscles of the core area causes an increase in body fluctuations, and as a result, it may cause a disturbance in body balance. As mentioned, the weakness or lack of sufficient coordination in the muscle structure of the core body area can lead to a decrease in the effectiveness of correct motor patterns, the occurrence of compensatory motor patterns, and ultimately dysfunction. Accordingly, it can be concluded that the weakness of core stabilizing muscles can have a negative effect on motor patterns. Therefore, the study’s findings can be confirmed according to the mentioned cases, and individuals’ weakness of the core stability muscles with non-specific chronic low back pain has led to the occurrence of incorrect and compensatory motor patterns in the FMS and +9 functional tests.
Furthermore, according to the researchers’ studies, the existence of low back pain puts the patient in a vicious cycle as patients with chronic low back pain because of long-term pain (more than 3 months). With limitations in motor function even in daily activities, they face problems and the physical activity of this population is seriously limited. The core stability muscles are the first muscles to suffer dysfunction when low back pain occurs, and since these muscles guide the joint in different motor patterns and motor function caused by these different patterns, their damage causes damage to the joint’s function and finally functional disabilities occur in movements [41].
Considering the significant relationship between the Y balance test and the amount of low back pain, studies have reported that the core body section is the basis of the kinetic chain and the endurance of the muscles in this area is important for motor function and providing stability and dynamic balance of the body. In 2011, Ruh and his colleagues in a review study investigated balance and postural control based on the range of pressure centers in people with low back pain and healthy people. The results showed that in most of the articles (14.16, 88%), the mean speed of displacement of the pressure center in people with low back pain was significantly higher than in healthy people. In addition, in people with low back pain, an increase in fluctuation in the anterior-posterior plate was also seen [38].
The difference in the frontal plate can be due to the important role of the hip abductor muscles in maintaining balance while standing on one leg and in dynamic functions, such as walking. The gluteus medius muscle plays the role of thigh abductor and hip stabilizer in the frontal plate and is especially important when standing, especially standing on one leg. On the other hand, the hip joint and trunk are mostly responsible for controlling and maintaining balance in the frontal plate, so the hip joint and the gluteus medius muscle play an important role in maintaining balance when forcing pressure on this plate [42]. In addition, according to Tak, the weakness of the gluteus medius muscle is common in individuals with specific chronic low back pain [43], and the existence of these cases can confirm a significant relationship between the Y balance test scores and the amount of pain in individuals with non-specific chronic low back pain.
Study limitations
The limitations of the present study include the spread of COVID-19 and the small number of participants. Therefore, it is suggested that after the end of the COVID-19 outbreak, researchers should conduct the present study with a larger number of subjects so that the results can be generalized more strongly. It is also recommended to investigate the prediction of low back pain by the functional tests of the present study in future research.
Conclusion
According to the study’s findings, there is a significantly negative relationship between the functional tests of +9, FMS, and Y balance with the intensity of low back pain in active women and men. Therefore, by improving the quality of motor patterns and performing balance exercises, it is possible to reduce the amount of pain in people with non-specific chronic low back pain.
Ethical Considerations
Compliance with ethical guidelines
The present study was registered at Iranian Registry of Clinical Trials (Code: IR.SSRC.REC.1401.026).
Funding
This study was extracted from the MA thesis of Atefeh Jafari Naeimi approved by Department of Physical Education and Sport Sciences, Shomal University.
Authors' contributions
Conceptualization and data collection: Atefeh Jafari Naeimi; Study design: All authors; Results interpretation: Mehdi Hosseinzadeh.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We are grateful to all the people who helped us in this project.
References
- Walker BF. The prevalence of low back pain: A systematic review of the literature from 1966 to 1998. Journal of Spinal Disorders. 2000; 13(3):205-17. [DOI:10.1097/00002517-200006000-00003] [PMID]
- Balagué F, Mannion AF, Pellisé F, Cedraschi C. Non-specific low back pain. The Lancet. 2012; 379(9814):482-91. [DOI:10.1016/S0140-6736(11)60610-7] [PMID]
- Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS, et al. The rising prevalence of chronic low back pain. Archives of Internal Medicine. 2009; 169(3):251-8. [DOI:10.1001/archinternmed.2008.543] [PMID] [PMCID]
- Hoy DG, Protani M, De R, Buchbinder R. The epidemiology of low back pain. Best Practice & Research Clinical Rheumatology. 2010; 24(6):783-92. [DOI:10.1016/j.berh.2010.10.002] [PMID]
- Majid K, Truumees E. Epidemiology and natural history of low back pain. Seminars in Spine Surgery. 2008; 87-8. [Link]
- Andrews JR, Harrelson GL, Wilk KE. Physical rehabilitation of the injured athlete. Philadelphia: Elsevier Health Sciences; 2012. [Link]
- Caine DJ, Maffulli N. Epidemiology of pediatric sports injuries: Individual sports. Basel: Karger Publishers; 2005. [DOI:10.1159/isbn.978-3-318-01179-1]
- Mazaheri M, Coenen P, Parnianpour M, Kiers H, van Dieën JH. Low back pain and postural sway during quiet standing with and without sensory manipulation: A systematic review. Gait & Posture. 2013; 37(1):12-22. [DOI:10.1016/j.gaitpost.2012.06.013] [PMID]
- Li R, Wang N, Yan X, Wei K. Comparison of postural control between healthy subjects and individuals with nonspecific low back pain during exposure to visual stimulus. Chinese Medical Journal. 2014; 127(7):1229-34. [Link]
- Radebold A, Cholewicki J, Polzhofer GK, Greene HS. Impaired postural control of the lumbar spine is associated with delayed muscle response times in patients with chronic idiopathic low back pain. Spine. 2001; 26(7):724-30. [DOI:10.1097/00007632-200104010-00004] [PMID]
- Cook G, Burton L, Hoogenboom B. Pre-participation screening: The use of fundamental movements as an assessment of function-part 1. North American Journal of Sports Physical Therapy. 2006; 1(2):62-72. [PMID]
- Cook G, Burton L, Hoogenboom BJ, Voight M. Functional movement screening: The use of fundamental movements as an assessment of function-part 2. International Journal of Sports Physical Therapy. 2014; 9(4):549-63. [PMID]
- Kraus K, Schütz E, Taylor WR, Doyscher R. Efficacy of the functional movement screen: A review. The Journal of Strength & Conditioning Research. 2014; 28(12):3571-84. [DOI:10.1519/JSC.0000000000000556] [PMID]
- Armstrong R. The relationship between the functional movement screen, star excursion balance test and the Beighton score in dancers. The Physician and Sportsmedicine. 2020; 48(1):53-62. [DOI:10.1080/00913847.2019.1624658] [PMID]
- Soltandoost Nari SM, Shamsoddini A. Relationships between functional movement screen and pain, dynamic balance, and trunk muscle endurance in military personnel with non-specific chronic low back pain. Physical Treatments - Specific Physical Therapy. 2020; 10(4):221-30. [DOI:10.32598/ptj.10.4.457.1]
- Frohm A, Heijne A, Kowalski J, Svensson P, Myklebust G. A nine-test screening battery for athletes: A reliability study. Scandinavian Journal of Medicine & Science in Sports. 2012; 22(3):306-15. [DOI:10.1111/j.1600-0838.2010.01267.x]
- Bakken A, Targett S, Bere T, Eirale C, Farooq A, Tol JL, et al. The functional movement test 9+ is a poor screening test for lower extremity injuries in professional male football players: A 2-year prospective cohort study. British Journal of Sports Medicine. 2018; 52(16):1047-53. [DOI:10.1136/bjsports-2016-097307] [PMID]
- Leandersson J, Heijne A, Flodström F, Frohm A, von Rosen P. Can movement tests predict injury in elite orienteerers? An 1-year prospective cohort study. Physiotherapy Theory and Practice. 2020; 36(8):956-64. [DOI:10.1080/09593985.2018.1513106] [PMID]
- Rafnsson ET, Frohm A, Myklebust G, Bahr R, Valdimarsson Ö, Árnason Á. Nine test screening battery-intra-rater reliability and screening on icelandic male handball players. British Journal of Sports Medicine. 2014; 48(7):674. [DOI:10.1136/bjsports-2014-093494.307]
- Berenshteyn Y, Gibson K, Hackett GC, Trem AB, Wilhelm M. Is standing balance altered in individuals with chronic low back pain? A systematic review. Disability and Rehabilitation. 2019; 41(13):1514-23. [DOI:10.1080/09638288.2018.1433240] [PMID]
- da Silva RA, Vieira ER, Fernandes KBP, Andraus RA, Oliveira MR, Sturion LA, et al. People with chronic low back pain have poorer balance than controls in challenging tasks. Disability and Rehabilitation. 2018; 40(11):1294-300. [DOI:10.1080/09638288.2017.1294627] [PMID]
- Ko MJ, Noh KH, Kang MH, Oh JS. Differences in performance on the functional movement screen between chronic low back pain patients and healthy control subjects. Journal of Physical Therapy Science. 2016; 28(7):2094-6. [DOI:10.1589/jpts.28.2094] [PMID] [PMCID]
- Fong SS, Tam YT, Macfarlane DJ, Ng SS, Bae YH, Chan EW, et al. Core muscle activity during TRX suspension exercises with and without kinesiology taping in adults with chronic low back pain: Implications for rehabilitation. Evidence-Based Complementary and Alternative Medicine. 2015; 2015:910168. [DOI:10.1155/2015/910168] [PMID] [PMCID]
- Budnar Jr RG, Birdwell R, Moody C, Hill DW, Duplanty AA, Jackson AW, et al. Functional movement screentm scores in collegiate track and field athletes in relation to injury risk and performance. International Journal of Exercise Science. 2013; 2(5):68. [Link]
- Gribble PA, Hertel J, Plisky P. Using the Star Excursion Balance Test to assess dynamic postural-control deficits and outcomes in lower extremity injury: A literature and systematic review. Journal of Athletic Training. 2012; 47(3):339-57. [DOI:10.4085/1062-6050-47.3.08] [PMID] [PMCID]
- Plisky PJ, Gorman PP, Butler RJ, Kiesel KB, Underwood FB, Elkins B. The reliability of an instrumented device for measuring components of the star excursion balance test. North American Journal of Sports Physical Therapy. 2009; 4(2):92-9. [PMID]
- Moradi k, Mioonejad h, Rajabi R. The immediate effect of core stability exercises on postural sway in athletes with functional ankle instability. Journal Of Rehabilitation Medicine. 2015; 4(3):101-10. [Link]
- Fan XY, Yan BX, Ding JY, Gao Q, XU RN, Liu B, et al. Effects of breathing exercise on nonspecific low back pain. Chinese Journal of Rehabilitation Theory and Practice. 2018; 24(1):93-6. [Link]
- Sedaghati P. [Relationship the dynamic balance and core stability muscles endurance with the results of functional movement screening among the girl basketball players (Persian)]. Journal of Exercise Science and Medicine. 2018; 9(2):169-84. [Link]
- Saki F, Sedaghati P. [Investigation of the relationship between functional movement screen composite scores and core stability muscles endurance in taekwondoists (Persian)]. Journal of Paramedical Sciences & Rehabilitation. 2018; 7(4):62-72. [Link]
- Mitchell UH, Johnson AW, Adamson B. Relationship between functional movement screen scores, core strength, posture, and body mass index in school children in Moldova. The Journal of Strength & Conditioning Research. 2015; 29(5):1172-9. [DOI:10.1519/JSC.0000000000000722] [PMID]
- Ehsani F, Hajihasani A, Hedayati R. [Relationship between abdominal muscle activity and postural control during standing tasks in females with chronic nonspecific low back pain (Persian)]. Journal of Mazandaran University of Medical Sciences. 2017; 27(148):68-78. [Link]
- Emami F, Yoosefinejad AK, Razeghi M. Correlations between core muscle geometry, pain intensity, functional disability and postural balance in patients with nonspecific mechanical low back pain. Medical Engineering & Physics. 2018; 60:39-46. [DOI:10.1016/j.medengphy.2018.07.006] [PMID]
- Kramer TA, Sacko RS, Pfeifer CE, Gatens DR, Goins JM, Stodden DF. The association between the functional movement screen(tm), y-balance test, and physical performance tests in male and female high school athletes. International Journal of Sports Physical Therapy. 2019; 14(6):911-9. [DOI:10.26603/ijspt20190911] [PMID] [PMCID]
- Kibler W, Chandler TJ, Uhl T, Maddux RE. A musculoskeletal approach to the preparticipation physical examination: Preventing injury and improving performance. The American Journal of Sports Medicine. 1989; 17(4):525-31. [DOI:10.1177/036354658901700413] [PMID]
- Knapik JJ, Cosio-Lima LM, Reynolds KL, Shumway RS. Efficacy of functional movement screening for predicting injuries in coast guard cadets. The Journal of Strength & Conditioning Research. 2015; 29(5):1157-62. [DOI:10.1519/JSC.0000000000000704] [PMID]
- Zazulak BT, Hewett TE, Reeves NP, Goldberg B, Cholewicki J. Deficits in neuromuscular control of the trunk predict knee injury risk: A prospective biomechanical-epidemiologic study. The American Journal of Sports Medicine. 2007; 35(7):1123-30. [DOI:10.1177/0363546507301585] [PMID]
- Sato K, Mokha M. Does core strength training influence running kinetics, lower-extremity stability, and 5000-M performance in runners? The Journal of Strength & Conditioning Research. 2009; 23(1):133-40. [DOI:10.1519/JSC.0b013e31818eb0c5] [PMID]
- Lederman E. The myth of core stability. Journal of Bodywork and Movement Therapies. 2010; 14(1):84-98. [DOI:10.1016/j.jbmt.2009.08.001] [PMID]
- Linderman JK, Board R, Astorino T, Baker JS, Boone T, Birnbaum L, et al. the relationship between core strength and performance in division i female soccer players. Journal of Exercise Physiology Online. 2009; 12(2):21-8. [Link]
- Letafatkar A, Nazarzadeh M, Hadadnezhad M, Farivar N. The efficacy of a HUBER exercise system mediated sensorimotor training protocol on proprioceptive system, lumbar movement control and quality of life in patients with chronic non-specific low back pain. Journal of Back and Musculoskeletal Rehabilitation. 2017; 30(4):767-78. [DOI:10.3233/BMR-150404] [PMID]
- Cooper NA, Scavo KM, Strickland KJ, Tipayamongkol N, Nicholson JD, Bewyer DC, et al. Prevalence of gluteus medius weakness in people with chronic low back pain compared to healthy controls. European Spine Journal. 2016; 25(4):1258-65. [DOI:10.1007/s00586-015-4027-6] [PMID]
- Tak SJ, Lee GC, Lee YW, Choi WJ. The effects of active release technique on the gluteus medius for pain relief in persons with chronic low back pain. Physical Therapy Rehabilitation Science. 2013; 2(1):27-30. [Link]
Type of Study: Applicable |
Subject:
Special
Received: 2022/08/19 | Accepted: 2023/04/18 | Published: 2023/01/13
Received: 2022/08/19 | Accepted: 2023/04/18 | Published: 2023/01/13
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






.jpg)
.jpg)
.jpg)
.jpg)
.jpg)