Tue, May 7, 2024
Volume 10, Issue 4 (Autumn 2020)
PTJ 2020, 10(4): 195-204 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Asgari Ashtiani A, Askari A. Effects of Modified Pilates Exercises on Pain, Disability, and Lumbopelvic Motor Control in Patients With Chronic Low Back Pain. PTJ 2020; 10 (4) :195-204
URL: http://ptj.uswr.ac.ir/article-1-470-en.html
URL: http://ptj.uswr.ac.ir/article-1-470-en.html
1- Health Promotion Research Center, Zahedan University of Medical Sciences, Zahedan, Iran.
2- Clinic of Physiotherapy, Social Welfare Hospital, Zahedan, Iran.
2- Clinic of Physiotherapy, Social Welfare Hospital, Zahedan, Iran.
Full-Text [PDF 605 kb]
(1107 Downloads)
| Abstract (HTML) (2466 Views)
Full-Text: (1460 Views)
1. Introduction
ow Back Pain (LBP) is a musculoskeletal problem and among the main causes of disease in high-, middle-, and low-income countries [1]. Nearly 80%-85% of individuals are affected by LBP throughout life. Besides, given its high prevalence, LBP is a major public health and socioeconomic problem in Iran [2]. Based on the widely-used classification concerning the duration of the symptoms, LBP can be acute, sub-acute, and chronic [3]. Specific LBP occurs in approximately 2% of all patients with LBP. Non-specific LBP has inflammatorily or mechanically become chronic. Chronic LBP (CLBP) refers to the evidence of LBP restricting activity and reducing mobility and muscle tolerance [2].
Following reduced quality of life, the individual becomes more irritable and vulnerable, leading to feelings of weakness and fatigue [4]. M.M. Panjabi stated that non-natural movement control is an outcome of inadequate stability in the spinal part; it can be a reason for micro-trauma and LBP [4] Pelvic-lumbar movement, occurring during an active and voluntary movement of the body is of importance. This is because individuals perform a large number of primary to the middle range movements in daily living activities [5]. If the lumbar-pelvic area moves along the primary range, lumbar-pelvic frequency increases throughout the day; accordingly, this increased frequency might result in enhanced tissue stress in the lumbar-pelvic area [5].
Non-pharmaceutical interventions, which include various physical factors, such as chiropractic [6], exercise [7], and electrotherapy [8], create the basis of CLBP [2]. Aatit Paungmail et al. (2016) evaluated the effects of lumbar-pelvic stability exercises, compared to placebo treatment and control on the tissue bloodstream and the control of lumbar-pelvic area movement in patients with CLBP. They concluded that lumbar-pelvic stability tests, compared to placebo and control groups, were more effective in improving tissue bloodstream in the lumbar-pelvic area and controlling the movement of the lumbar-pelvic area [9].
Studies indicated that LBP should be treated with an understanding of training and an emphasis on how to correctly perform the movement [4]. Despite extensive data on LBP, no treatment has been found to present a continuous effect on relieving symptoms associated with back pain [1]. Movement control in the lumbar-pelvic area can improve stability and be considered as an essential component of LBP treatment [10]. Moreover, a wide variety of LBP categories has resulted in various clinical treatments [11]. This requires classification systems, which have been stated in the last two decades [12]. One of these classification systems prescribed for diagnosis and treatment is the impaired motor patterns classification system [13]. Accordingly, the classification of patients should be performed in homogeneous sets per their symptoms for better treatment of LBP [11]. These repetitive movements result in stress in soft tissue, the accumulation of tissue stress, pathology in the low back, and CLBP [14].
Without the stability of the spinal part (pelvic stability is part of the spinal stability), the lumbar area would have further movements, compared to the hip joints. This stress caused by repetitive movements prerequisites impairment in controlling lumbar-pelvic movement. Therefore, patients with CLBP encounter difficulty in controlling the lumbar-pelvic movement.
Spinal muscular atrophy and dysfunction may mitigate spinal force control and affect lumbopelvic stability [13]. According to Bergmark, spinal muscles are classified into two groups of deep/local and superficial/global muscles [15]. Reduced strength and endurance of superficial muscles in the posterior lumbar region critically impact LBP; thus, the endurance level of trunk extensor muscles is predictive of the first back pain attack [13]. The deep global muscles have a crucial role not only in alleviating stress and decreasing spinopelvic shear force but also in static and dynamic stability [16]. Amongst deep muscles, the lumbar multifidus and transversus abdominis are accounted as the most essential muscles strengthening the spinal stability [11]. The main risk factors for CLBP include reduced motor control and the weakness of such deep muscles, as lumbar multifidus and transverse abdominis [11, 16].
There exist numerous therapeutic exercises for improving spinal weakness, endurance, and motor control [10, 11, 12, 13]. As a rehabilitation intervention, Pilates exercise therapy involves improving the overall physical condition of the body, aiming at raising body awareness and perfecting body posture [17, 18, 19]. The modified Pilates method is a comprehensive approach to body-mind condition; it is simultaneously associated with such workouts as, trunk stability exercises, meditation, breathing technique, and whole-body function [18, 19]. These training exercises emphasized 5 essential principles; breathing technique, spinal alignment and posture, chest and scapular stability, neck movement, and Transverse Abdominis (TVA) muscle activity [17, 18, 20].
During Pilates exercises, pelvic tilt is modified by the activation of pelvic floor muscles. Besides, lumbopelvic stability is increased by the topical activation and co-contraction of trunk core muscles, especially transverse abdominus and multifidus in the spinal cord [21, 22]. Such training also features low intensity, long-term, and repetitive exercises; accordingly, they contribute to the improvement of strength, endurance, and neuromuscular control of the trunk muscles [23].
In a systematic study, Wells et al. investigated the effect of short-term Pilates exercises on pain relief and functional improvement in patients with non-specific CLBP [21]. Klobec et al. explored 50 elderlies undergoing 12 weeks of 1-to-2 hours of Pilates-based exercises. They found a significant improvement in the trainees’ muscular flexibility and endurance at the end of week 12; however, there was no significant improvement in their body balance and posture [24].
In general, no standard treatment and rehabilitation method is presented for LBP; thus, therapists act based on their personal experiences or sometimes trial and error in their therapeutic procedures. These heterogeneous results are indicative of the inadequacy of data in this area of research accentuating the necessity of further studies. The specific attributes of the Pilates method can help with the achievement of improved posture and motor control in patients with non-specific CLBP during exercise therapy. Therefore, Pilates can be a proposed therapeutic approach for rehabilitating patients with non-specific CLBP [18, 20]. Consequently, the present study intended to compare the effects of modified Pilates exercises and general exercises on lumbopelvic motor control, the muscular endurance of lumbar and abdominal, back pain, and functional disability in patients with non-specific CLBP.
2. Materials and Methods
The present randomized clinical trial was conducted by Zahedan University of Medical Sciences (Code: IR.ZAUMS.REC.1396.85) and Iranian Registry of Clinical Trials (IRCT) registration number (IRCT2018090940975N1). This research was conducted in 2018 at the Razmjoo Moghaddam Clinic of Zahedan University of Medical Sciences. In total, 30 patients with CLBP were randomly assigned to two groups of modified Pilates exercises and control (n=15/group). The modified Pilates exercises were performed for 6 weeks, and 3 times per week; in the control group, it was conducted for 6 consecutive weeks and 3 times per week. The study participants were selected by convenience sampling method. The sample size was determined based on a preliminary study. Initially, 10 patients were selected and randomly assigned to two study groups.
The main stage of the research was conducted on them. Based on the Mean±SD scores obtained from these study groups, the sample size required for the main study was estimated with a confidence level of 95% and a power test of 80%.
The inclusion criteria of the study were entailed any chronic LBP between the 12th rib and the rump region; irritation and stiffness in lumbar spine region with/without referral to the lower limbs (without root cause); a 3-month or prolonged course of the disease; an age range of 18-50 years [4, 25]; as well as no history of vertebral fracture, pregnancy, tumor, infection, previous spinal surgery, serious spinal deformities, cardiovascular disorders, vestibular system disorders, Central Nervous System (CNS) disorders, visual impairment, neurological symptoms with sensory defects and motor paralysis included, and neurologic and rheumatic diseases [4, 10, 25]. The exclusion criteria of the study involved the potential risk of exercises for patients; unaccomplished exercise therapy; the exacerbation of symptoms; receiving further therapies along with exercise therapy, and patients’ absence from more than three consecutive training sessions [26]. Clinical tests were performed and demographic characteristics were recorded.
A tape measure with an accuracy of centimeter was used to measure the height of the study subjects, a digital scale was applied to measure body weight (to calculate body mass index), and a pressure biofeedback unit was used to measure lumbopelvic motor control. Lumbar-pelvic movement control patterns were assessed during Bent Knee Fall Out (BKFO) and Knee Lift Abdominal Tests (KLAT) tests, using a compressive biofeedback unit. In the KLAT test, the patient was placed in the crook lying position. The patient was requested to lift one leg from the table and raise the leg up to 90º of leg flexion with knee flexion while he has simultaneously maintained the lumbar spinal cords fixed. The pressure in the compressive biofeedback was adjusted to 40 mm Hg. In the BKFO test, the patient was requested to be placed in partial crook lying in the supine position. Then, the patient slowly lowered the bent leg up to approximately 45º of abduction/side rotation, while his bent leg has been placed beside the smoothed foot; then it returned to the starting position. Concurrently, abdominal muscles were lowered to provide activated stabilization, while they were in the form of leg eccentric up to abduction/side rotation. The method used in the KLAT test was also implemented to score the BKFO test [22].
The VAS consists of a 10-cm line with labels at the end, as follows: “0” and “10” represent no and severe pain, respectively [26]. Disability was measured with the Oswestry Low Back Disability (OSWESTRY) questionnaire [27].
Muscle endurance was assessed by the Biering-Sorenson Test. The starting position is the patient adopting a half prone lying on a plinth with the superior edge of the iliac crest at the edge of the plinth and the arms crossed over the chest. The lower limbs are strategically stabilized with straps. The patient is requested to maintain the upper body in a horizontal position and the timer is started. The test ends if the patient can maintain the mentioned position for 4 minutes (240 seconds) or can no longer maintain the set position before 4 minutes elapses. The stop time is also recorded [20].
For measuring the level of endurance of the abdominal muscles, the person is in a position where the trunk is at an angle of 60º to the ground. The knees are in a hook position and the test legs are fixed by someone else. The support surface is pushed back. The person is requested to hold this posture and maintain the isometric to the best of their ability. The duration of maintaining the status (in seconds) will be recorded as an individual’s score [9].
Both study groups received electrotherapy and exercise therapy as the main parts of treatment intervention. Electrotherapy followed the same procedure for both treatment groups before starting the exercise therapy, as follows:
• Applying Conventional Transcutaneous Electrical Nerve Stimulation (TENS) -at 80 Hz frequency and 120 ms diversion- for 20 minutes.
• Applying UltraSound (US) -at 1 MHz frequency and 1.5 w/cm intensity- on paraspinal muscles of the lumbar region for 5 minutes.
• Using a Hot Pack on the lumbar region for 20 minutes.
The exercise therapy, however, followed a different procedure for both treatment groups; one group received Pilates exercises while the other performed general exercises (Tables 1 and 2).
.jpg)
.jpg)
The collected data were analyzed by SPSS. The normality of data distribution was examined by the Shapiro–Wilk test. Equality of variances was established using Levene’s test. Paired Samples t-test and Independent Samples t-test were used respectively for intra-group and inter-group comparison. The probability value (α) was considered as ˂%5 for statistical comparisons (P<0.05).
In case of abnormally in the distributed data, the Wilcoxon Signed-Rank test was used to compare the observed results before and after the intervention per treatment group (intragroup); the Mann-Whitney U test was used to compare the observed results before and after the intervention between the study groups (intergroup).
3. Results
The mean values of the age range, weight, height, and body mass index in the group of modified Pilates exercises and control are presented in Table 3.
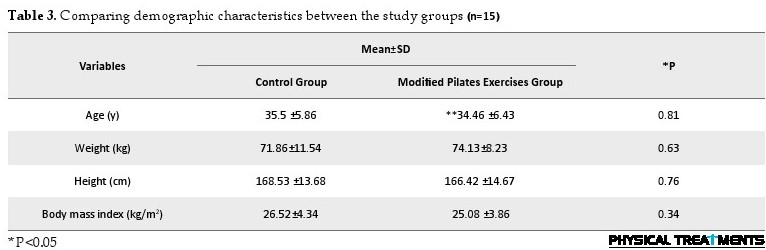
The present research results reflected the normal distribution of the data (Table 3). The mean and standard deviation values of data related to lumbopelvic motor control, pain, disability, as well as lumbar and trunk muscle endurance were compared at pretest and posttest stages in the study groups. Moreover, the P-value and the results of post-treatment data are listed in Table 4.
.jpg)
The results of intragroup comparison indicated a significant difference between the mean values of pain severity, functional disability, lumbopelvic motor control, and the muscular endurance of lumbar and abdominal in the Pilates exercise and general-exercise groups before and after the intervention based on the Wilcoxon Signed-Rank test (P=0.001) (Table 4).
To ensure the accuracy of the randomization process, the pre-intervention data were compared in both groups. The relevant results demonstrated no significant difference between the study groups in terms of the intended variables. In other words, the mean values of pain severity, functional disability, lumbopelvic motor control, and the muscular endurance of lumbar and abdominal were normalized in the patients of both treatment groups. The results of intergroup (Pilates exercise vs. general exercise) comparison presented no significant difference between the values of lumbopelvic motor control, trunk muscular endurance, and functional disability at posttest, based on the Mann-Whitney test (P˂0.05) (Table 4).
4. Discussion
According to the present research findings, there was a significant improvement in the trunk muscular endurance, pain severity, and functional disability in each group of patients in the course of intragroup post-intervention. In other words, both treatment groups witnessed positive outcomes in the intended variables. However, the results of intergroup comparisons indicated no significant difference between the values of lumbopelvic motor control, trunk muscular endurance, and functional disability of patients in both study groups. In general, the present study findings represented the positive effects of modified Pilates exercises on the treatment of patients with non-specific CLBP. The collected results concerning the effect of modified Pilates exercises on improving the control of lumbar-pelvic movements were in line with those of Hodges Paul W. et al. [21], Panjabi Manohar M. et al. [27], Ota M. [28], and Paungmali Aatit et al. [20].
Paungmali Aatit et al. reported that lumbar-pelvic stability tests and treatment in the control and placebo groups revealed significant improvement in controlling the lumbar-pelvic area movement [21]. Their results respecting improvement in the mean value of controlling lumbar-pelvic were consistent with those of the current research. Previous studies have reported that improvement in lumbar-pelvic area movement control was created by inter-segmental stiffness; preventing shear force that causes injury in the lumbar area. As a result, it relieves the pain in patients with CLBP [25]. However, Paungmali Aatit et al. argued that increased tissue bloodstream can be a reason for pain relief and the control of lumbar-pelvic area movement in patients with CLBP. Two important theories, including a vicious cycle and the new pain adaptation, may support such clinical reasons following pelvic-lumbar stability exercises. In vicious cycle theory, the proposed clinical reason is an ischemic spasm in the lumbar-pelvic muscles following vascular adaptation [22]. This ischemic spasm might result in increased pain in the tissues of the lumbar-pelvic area.
The pain might prevent further movement in the lumbar-pelvic area and cause spasm-pain-spasm. On the other hand, pain adaptation theory suggests that pain reduces the contractibility of the lumbar-pelvic area muscles, leading to their inadequacy. This issue might lead to the poor performance of the lumbar-pelvic area and poor movement control of the lumbar-pelvic area [21]. Thus, improving the tissue bloodstream in the muscles of the lumbar-pelvic area might improve back pain and lumbar-pelvic area movement control. However, none of these mechanical and vascular changes were observed in the explored control and placebo groups [22]. Thus, the goal of rehabilitation is to increase the blood circulation and movements in the lumbar-pelvic area; thus, it could clean the harmful inflammatory substances and facilitate muscular activity [9].
Therefore, lumbar-pelvic stability exercises lead to improved tissue bloodstream, which might reduce harmful inflammatory substances; accordingly, this process helps to improve the movement pattern in patients with CLBP. The results of these studies were also in line with those of our research. In our research, the treatment provided to the control group led to the increased bloodstream and the removal of waste substances; as a result, it reduced spasm and pain. Subsequently, it led to improved control of lumbar-pelvic area movements. Modified Pilates exercises group, correct movement pattern training, and movement modification lead to reduced stress, inflammation, and pain. In addition, modified Pilates exercises lead to coordination in the movement of the lumbar-pelvic area and prevent micro-trauma; thus, they improve the control of lumbar-pelvic movement [24].
In other words, modified Pilates exercised presented no positive effect on lumbopelvic motor control. Richardson and Hodges introduced TVA muscle as the core component in spinal stability and the first active muscle in routine activities [11]. This muscle plays an important role in lumbopelvic motor control. The role and activity of TVA muscle are assessed by measuring lumbopelvic motor control. Phrompaet stated that the 8-week Pilates exercises significantly improved lumbopelvic motor control and spinal muscle flexibility [18]. Pilates exercises focus on trunk muscles and breathing control that ultimately facilitate the activity of muscles involved in lumbopelvic stability. Furthermore, the CNS plays a crucial role in lumbopelvic stability; it activates such stabilizers as transverse abdominal muscles against internal and external forces.
The CNS control over trunk stability is improved by challenging trunk control through external and internal forces (the movement of body organs or use of exercise springs) in Pilates exercises. Gladwell et al. found that the 6-week Pilates exercises resulted in increased muscular flexibility, proprioception, enhanced general health, and pain relief in patients with LBP. The proposed proprioception in Gladwell’s study highlights the significant changes in spinal motor control [29]. The intended exercises used in the present study emphasized biopsychological and core elements that can significantly affect lumbopelvic motor control; this aim is achieved by particularly strengthening and controlling paraspinal, gluteal, and abdominal muscles [30].
Based on the present study findings, neither modified Pilates nor general exercises presented any significant effects on LBP. The insignificance of results may be because the study participants did not experience many defects in lumbopelvic motor control. Therefore, the proposed exercises could not lead to any apparent changes. Reduced trunk muscle strength affects the spinal ability to react to sudden and unexpected forces. Furthermore, motor control is disrupted following the tiredness of these muscles after their exposure to recurrent forces; it becomes a risk factor for the onset or incidence of back pain [3, 6, 25].
Moreover, the Pilates exercise group experienced more significant changes than the general exercise group. In Kliziene’s study, the maximum isometric power of patients’ trunk muscles increased after 16 weeks and remained for almost 2 months [24]. Moreover, trunk flexor muscle endurance was significantly dependent on the trunk extensor muscle endurance. Kliziene believed that regular exercises can increase the strength of trunk muscles. Besides, the intensity of muscular contraction is lower in modified Pilates exercises, like stability exercises, the repetition of which rises trunk muscle endurance [23, 28]. Therefore, the increased level of trunk muscle endurance in the Pilates group can be attributed to this feature. The present study treated the subjects with an average of 40 reps of each exercise per session for 18 workout sessions. Mostagi observed no significant difference between the level of trunk muscle endurance in Pilates and general groups, i.e., consistent with the present study data [25]. Moreover, there was no intragroup difference in the present study [18].
The variations in the sample size, type of exercises, number of repetitions, pain severity, and fear may contribute to the differences in the results of the Sorensen test. The mean age of female participants was 34.43 in the present study, while it was 36.1 for both genders in Mostagi’s study. Sex ratio was also effective in Sorensen test results. Physiological and pathophysiological differences, as well as the extent of pain and fear in patients, are likely to affect the test results. The type and repetition of exercises in Mostagi’s study were not similar to the present study. The former included Mat and Apparatus Pilates exercises, while the latter focused on the core exercises and trunk stability.
A limitation of the present study was the small sample size; however, it was still one of the largest populations available in the literature about Pilates in MS. Our study subjects were only females and their disability status were mild to moderate; therefore, we can only generalize our results to females that are not affected severely. Accordingly, the effects of our presented program could be different in males or a more severely affected population.
5. Conclusion
In general, the present study data were indicative of the positive effects of modified Pilates exercises on increasing lumbopelvic motor control, increasing trunk muscles endurance, pain relief, and functional disability improvement. Consequently, modified Pilates is recommended as a therapeutic program for the treatment of patients with non-specific LBP.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by Ethics Commitee of Zahedan Univrsity of Medical Sciences (Code: IR.ZAUMS.REC.1396.85).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally in preparing all parts of this research.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to special thanks to the patients who participated in the study . In addition we are grateful of zahedan university of medical science for approve this research.
References
ow Back Pain (LBP) is a musculoskeletal problem and among the main causes of disease in high-, middle-, and low-income countries [1]. Nearly 80%-85% of individuals are affected by LBP throughout life. Besides, given its high prevalence, LBP is a major public health and socioeconomic problem in Iran [2]. Based on the widely-used classification concerning the duration of the symptoms, LBP can be acute, sub-acute, and chronic [3]. Specific LBP occurs in approximately 2% of all patients with LBP. Non-specific LBP has inflammatorily or mechanically become chronic. Chronic LBP (CLBP) refers to the evidence of LBP restricting activity and reducing mobility and muscle tolerance [2].
Following reduced quality of life, the individual becomes more irritable and vulnerable, leading to feelings of weakness and fatigue [4]. M.M. Panjabi stated that non-natural movement control is an outcome of inadequate stability in the spinal part; it can be a reason for micro-trauma and LBP [4] Pelvic-lumbar movement, occurring during an active and voluntary movement of the body is of importance. This is because individuals perform a large number of primary to the middle range movements in daily living activities [5]. If the lumbar-pelvic area moves along the primary range, lumbar-pelvic frequency increases throughout the day; accordingly, this increased frequency might result in enhanced tissue stress in the lumbar-pelvic area [5].
Non-pharmaceutical interventions, which include various physical factors, such as chiropractic [6], exercise [7], and electrotherapy [8], create the basis of CLBP [2]. Aatit Paungmail et al. (2016) evaluated the effects of lumbar-pelvic stability exercises, compared to placebo treatment and control on the tissue bloodstream and the control of lumbar-pelvic area movement in patients with CLBP. They concluded that lumbar-pelvic stability tests, compared to placebo and control groups, were more effective in improving tissue bloodstream in the lumbar-pelvic area and controlling the movement of the lumbar-pelvic area [9].
Studies indicated that LBP should be treated with an understanding of training and an emphasis on how to correctly perform the movement [4]. Despite extensive data on LBP, no treatment has been found to present a continuous effect on relieving symptoms associated with back pain [1]. Movement control in the lumbar-pelvic area can improve stability and be considered as an essential component of LBP treatment [10]. Moreover, a wide variety of LBP categories has resulted in various clinical treatments [11]. This requires classification systems, which have been stated in the last two decades [12]. One of these classification systems prescribed for diagnosis and treatment is the impaired motor patterns classification system [13]. Accordingly, the classification of patients should be performed in homogeneous sets per their symptoms for better treatment of LBP [11]. These repetitive movements result in stress in soft tissue, the accumulation of tissue stress, pathology in the low back, and CLBP [14].
Without the stability of the spinal part (pelvic stability is part of the spinal stability), the lumbar area would have further movements, compared to the hip joints. This stress caused by repetitive movements prerequisites impairment in controlling lumbar-pelvic movement. Therefore, patients with CLBP encounter difficulty in controlling the lumbar-pelvic movement.
Spinal muscular atrophy and dysfunction may mitigate spinal force control and affect lumbopelvic stability [13]. According to Bergmark, spinal muscles are classified into two groups of deep/local and superficial/global muscles [15]. Reduced strength and endurance of superficial muscles in the posterior lumbar region critically impact LBP; thus, the endurance level of trunk extensor muscles is predictive of the first back pain attack [13]. The deep global muscles have a crucial role not only in alleviating stress and decreasing spinopelvic shear force but also in static and dynamic stability [16]. Amongst deep muscles, the lumbar multifidus and transversus abdominis are accounted as the most essential muscles strengthening the spinal stability [11]. The main risk factors for CLBP include reduced motor control and the weakness of such deep muscles, as lumbar multifidus and transverse abdominis [11, 16].
There exist numerous therapeutic exercises for improving spinal weakness, endurance, and motor control [10, 11, 12, 13]. As a rehabilitation intervention, Pilates exercise therapy involves improving the overall physical condition of the body, aiming at raising body awareness and perfecting body posture [17, 18, 19]. The modified Pilates method is a comprehensive approach to body-mind condition; it is simultaneously associated with such workouts as, trunk stability exercises, meditation, breathing technique, and whole-body function [18, 19]. These training exercises emphasized 5 essential principles; breathing technique, spinal alignment and posture, chest and scapular stability, neck movement, and Transverse Abdominis (TVA) muscle activity [17, 18, 20].
During Pilates exercises, pelvic tilt is modified by the activation of pelvic floor muscles. Besides, lumbopelvic stability is increased by the topical activation and co-contraction of trunk core muscles, especially transverse abdominus and multifidus in the spinal cord [21, 22]. Such training also features low intensity, long-term, and repetitive exercises; accordingly, they contribute to the improvement of strength, endurance, and neuromuscular control of the trunk muscles [23].
In a systematic study, Wells et al. investigated the effect of short-term Pilates exercises on pain relief and functional improvement in patients with non-specific CLBP [21]. Klobec et al. explored 50 elderlies undergoing 12 weeks of 1-to-2 hours of Pilates-based exercises. They found a significant improvement in the trainees’ muscular flexibility and endurance at the end of week 12; however, there was no significant improvement in their body balance and posture [24].
In general, no standard treatment and rehabilitation method is presented for LBP; thus, therapists act based on their personal experiences or sometimes trial and error in their therapeutic procedures. These heterogeneous results are indicative of the inadequacy of data in this area of research accentuating the necessity of further studies. The specific attributes of the Pilates method can help with the achievement of improved posture and motor control in patients with non-specific CLBP during exercise therapy. Therefore, Pilates can be a proposed therapeutic approach for rehabilitating patients with non-specific CLBP [18, 20]. Consequently, the present study intended to compare the effects of modified Pilates exercises and general exercises on lumbopelvic motor control, the muscular endurance of lumbar and abdominal, back pain, and functional disability in patients with non-specific CLBP.
2. Materials and Methods
The present randomized clinical trial was conducted by Zahedan University of Medical Sciences (Code: IR.ZAUMS.REC.1396.85) and Iranian Registry of Clinical Trials (IRCT) registration number (IRCT2018090940975N1). This research was conducted in 2018 at the Razmjoo Moghaddam Clinic of Zahedan University of Medical Sciences. In total, 30 patients with CLBP were randomly assigned to two groups of modified Pilates exercises and control (n=15/group). The modified Pilates exercises were performed for 6 weeks, and 3 times per week; in the control group, it was conducted for 6 consecutive weeks and 3 times per week. The study participants were selected by convenience sampling method. The sample size was determined based on a preliminary study. Initially, 10 patients were selected and randomly assigned to two study groups.
The main stage of the research was conducted on them. Based on the Mean±SD scores obtained from these study groups, the sample size required for the main study was estimated with a confidence level of 95% and a power test of 80%.
The inclusion criteria of the study were entailed any chronic LBP between the 12th rib and the rump region; irritation and stiffness in lumbar spine region with/without referral to the lower limbs (without root cause); a 3-month or prolonged course of the disease; an age range of 18-50 years [4, 25]; as well as no history of vertebral fracture, pregnancy, tumor, infection, previous spinal surgery, serious spinal deformities, cardiovascular disorders, vestibular system disorders, Central Nervous System (CNS) disorders, visual impairment, neurological symptoms with sensory defects and motor paralysis included, and neurologic and rheumatic diseases [4, 10, 25]. The exclusion criteria of the study involved the potential risk of exercises for patients; unaccomplished exercise therapy; the exacerbation of symptoms; receiving further therapies along with exercise therapy, and patients’ absence from more than three consecutive training sessions [26]. Clinical tests were performed and demographic characteristics were recorded.
A tape measure with an accuracy of centimeter was used to measure the height of the study subjects, a digital scale was applied to measure body weight (to calculate body mass index), and a pressure biofeedback unit was used to measure lumbopelvic motor control. Lumbar-pelvic movement control patterns were assessed during Bent Knee Fall Out (BKFO) and Knee Lift Abdominal Tests (KLAT) tests, using a compressive biofeedback unit. In the KLAT test, the patient was placed in the crook lying position. The patient was requested to lift one leg from the table and raise the leg up to 90º of leg flexion with knee flexion while he has simultaneously maintained the lumbar spinal cords fixed. The pressure in the compressive biofeedback was adjusted to 40 mm Hg. In the BKFO test, the patient was requested to be placed in partial crook lying in the supine position. Then, the patient slowly lowered the bent leg up to approximately 45º of abduction/side rotation, while his bent leg has been placed beside the smoothed foot; then it returned to the starting position. Concurrently, abdominal muscles were lowered to provide activated stabilization, while they were in the form of leg eccentric up to abduction/side rotation. The method used in the KLAT test was also implemented to score the BKFO test [22].
The VAS consists of a 10-cm line with labels at the end, as follows: “0” and “10” represent no and severe pain, respectively [26]. Disability was measured with the Oswestry Low Back Disability (OSWESTRY) questionnaire [27].
Muscle endurance was assessed by the Biering-Sorenson Test. The starting position is the patient adopting a half prone lying on a plinth with the superior edge of the iliac crest at the edge of the plinth and the arms crossed over the chest. The lower limbs are strategically stabilized with straps. The patient is requested to maintain the upper body in a horizontal position and the timer is started. The test ends if the patient can maintain the mentioned position for 4 minutes (240 seconds) or can no longer maintain the set position before 4 minutes elapses. The stop time is also recorded [20].
For measuring the level of endurance of the abdominal muscles, the person is in a position where the trunk is at an angle of 60º to the ground. The knees are in a hook position and the test legs are fixed by someone else. The support surface is pushed back. The person is requested to hold this posture and maintain the isometric to the best of their ability. The duration of maintaining the status (in seconds) will be recorded as an individual’s score [9].
Both study groups received electrotherapy and exercise therapy as the main parts of treatment intervention. Electrotherapy followed the same procedure for both treatment groups before starting the exercise therapy, as follows:
• Applying Conventional Transcutaneous Electrical Nerve Stimulation (TENS) -at 80 Hz frequency and 120 ms diversion- for 20 minutes.
• Applying UltraSound (US) -at 1 MHz frequency and 1.5 w/cm intensity- on paraspinal muscles of the lumbar region for 5 minutes.
• Using a Hot Pack on the lumbar region for 20 minutes.
The exercise therapy, however, followed a different procedure for both treatment groups; one group received Pilates exercises while the other performed general exercises (Tables 1 and 2).
.jpg)
.jpg)
The collected data were analyzed by SPSS. The normality of data distribution was examined by the Shapiro–Wilk test. Equality of variances was established using Levene’s test. Paired Samples t-test and Independent Samples t-test were used respectively for intra-group and inter-group comparison. The probability value (α) was considered as ˂%5 for statistical comparisons (P<0.05).
In case of abnormally in the distributed data, the Wilcoxon Signed-Rank test was used to compare the observed results before and after the intervention per treatment group (intragroup); the Mann-Whitney U test was used to compare the observed results before and after the intervention between the study groups (intergroup).
3. Results
The mean values of the age range, weight, height, and body mass index in the group of modified Pilates exercises and control are presented in Table 3.
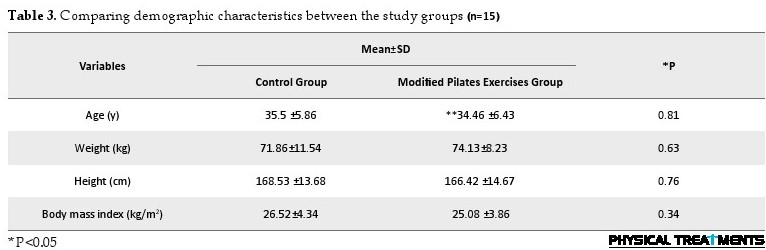
The present research results reflected the normal distribution of the data (Table 3). The mean and standard deviation values of data related to lumbopelvic motor control, pain, disability, as well as lumbar and trunk muscle endurance were compared at pretest and posttest stages in the study groups. Moreover, the P-value and the results of post-treatment data are listed in Table 4.
.jpg)
The results of intragroup comparison indicated a significant difference between the mean values of pain severity, functional disability, lumbopelvic motor control, and the muscular endurance of lumbar and abdominal in the Pilates exercise and general-exercise groups before and after the intervention based on the Wilcoxon Signed-Rank test (P=0.001) (Table 4).
To ensure the accuracy of the randomization process, the pre-intervention data were compared in both groups. The relevant results demonstrated no significant difference between the study groups in terms of the intended variables. In other words, the mean values of pain severity, functional disability, lumbopelvic motor control, and the muscular endurance of lumbar and abdominal were normalized in the patients of both treatment groups. The results of intergroup (Pilates exercise vs. general exercise) comparison presented no significant difference between the values of lumbopelvic motor control, trunk muscular endurance, and functional disability at posttest, based on the Mann-Whitney test (P˂0.05) (Table 4).
4. Discussion
According to the present research findings, there was a significant improvement in the trunk muscular endurance, pain severity, and functional disability in each group of patients in the course of intragroup post-intervention. In other words, both treatment groups witnessed positive outcomes in the intended variables. However, the results of intergroup comparisons indicated no significant difference between the values of lumbopelvic motor control, trunk muscular endurance, and functional disability of patients in both study groups. In general, the present study findings represented the positive effects of modified Pilates exercises on the treatment of patients with non-specific CLBP. The collected results concerning the effect of modified Pilates exercises on improving the control of lumbar-pelvic movements were in line with those of Hodges Paul W. et al. [21], Panjabi Manohar M. et al. [27], Ota M. [28], and Paungmali Aatit et al. [20].
Paungmali Aatit et al. reported that lumbar-pelvic stability tests and treatment in the control and placebo groups revealed significant improvement in controlling the lumbar-pelvic area movement [21]. Their results respecting improvement in the mean value of controlling lumbar-pelvic were consistent with those of the current research. Previous studies have reported that improvement in lumbar-pelvic area movement control was created by inter-segmental stiffness; preventing shear force that causes injury in the lumbar area. As a result, it relieves the pain in patients with CLBP [25]. However, Paungmali Aatit et al. argued that increased tissue bloodstream can be a reason for pain relief and the control of lumbar-pelvic area movement in patients with CLBP. Two important theories, including a vicious cycle and the new pain adaptation, may support such clinical reasons following pelvic-lumbar stability exercises. In vicious cycle theory, the proposed clinical reason is an ischemic spasm in the lumbar-pelvic muscles following vascular adaptation [22]. This ischemic spasm might result in increased pain in the tissues of the lumbar-pelvic area.
The pain might prevent further movement in the lumbar-pelvic area and cause spasm-pain-spasm. On the other hand, pain adaptation theory suggests that pain reduces the contractibility of the lumbar-pelvic area muscles, leading to their inadequacy. This issue might lead to the poor performance of the lumbar-pelvic area and poor movement control of the lumbar-pelvic area [21]. Thus, improving the tissue bloodstream in the muscles of the lumbar-pelvic area might improve back pain and lumbar-pelvic area movement control. However, none of these mechanical and vascular changes were observed in the explored control and placebo groups [22]. Thus, the goal of rehabilitation is to increase the blood circulation and movements in the lumbar-pelvic area; thus, it could clean the harmful inflammatory substances and facilitate muscular activity [9].
Therefore, lumbar-pelvic stability exercises lead to improved tissue bloodstream, which might reduce harmful inflammatory substances; accordingly, this process helps to improve the movement pattern in patients with CLBP. The results of these studies were also in line with those of our research. In our research, the treatment provided to the control group led to the increased bloodstream and the removal of waste substances; as a result, it reduced spasm and pain. Subsequently, it led to improved control of lumbar-pelvic area movements. Modified Pilates exercises group, correct movement pattern training, and movement modification lead to reduced stress, inflammation, and pain. In addition, modified Pilates exercises lead to coordination in the movement of the lumbar-pelvic area and prevent micro-trauma; thus, they improve the control of lumbar-pelvic movement [24].
In other words, modified Pilates exercised presented no positive effect on lumbopelvic motor control. Richardson and Hodges introduced TVA muscle as the core component in spinal stability and the first active muscle in routine activities [11]. This muscle plays an important role in lumbopelvic motor control. The role and activity of TVA muscle are assessed by measuring lumbopelvic motor control. Phrompaet stated that the 8-week Pilates exercises significantly improved lumbopelvic motor control and spinal muscle flexibility [18]. Pilates exercises focus on trunk muscles and breathing control that ultimately facilitate the activity of muscles involved in lumbopelvic stability. Furthermore, the CNS plays a crucial role in lumbopelvic stability; it activates such stabilizers as transverse abdominal muscles against internal and external forces.
The CNS control over trunk stability is improved by challenging trunk control through external and internal forces (the movement of body organs or use of exercise springs) in Pilates exercises. Gladwell et al. found that the 6-week Pilates exercises resulted in increased muscular flexibility, proprioception, enhanced general health, and pain relief in patients with LBP. The proposed proprioception in Gladwell’s study highlights the significant changes in spinal motor control [29]. The intended exercises used in the present study emphasized biopsychological and core elements that can significantly affect lumbopelvic motor control; this aim is achieved by particularly strengthening and controlling paraspinal, gluteal, and abdominal muscles [30].
Based on the present study findings, neither modified Pilates nor general exercises presented any significant effects on LBP. The insignificance of results may be because the study participants did not experience many defects in lumbopelvic motor control. Therefore, the proposed exercises could not lead to any apparent changes. Reduced trunk muscle strength affects the spinal ability to react to sudden and unexpected forces. Furthermore, motor control is disrupted following the tiredness of these muscles after their exposure to recurrent forces; it becomes a risk factor for the onset or incidence of back pain [3, 6, 25].
Moreover, the Pilates exercise group experienced more significant changes than the general exercise group. In Kliziene’s study, the maximum isometric power of patients’ trunk muscles increased after 16 weeks and remained for almost 2 months [24]. Moreover, trunk flexor muscle endurance was significantly dependent on the trunk extensor muscle endurance. Kliziene believed that regular exercises can increase the strength of trunk muscles. Besides, the intensity of muscular contraction is lower in modified Pilates exercises, like stability exercises, the repetition of which rises trunk muscle endurance [23, 28]. Therefore, the increased level of trunk muscle endurance in the Pilates group can be attributed to this feature. The present study treated the subjects with an average of 40 reps of each exercise per session for 18 workout sessions. Mostagi observed no significant difference between the level of trunk muscle endurance in Pilates and general groups, i.e., consistent with the present study data [25]. Moreover, there was no intragroup difference in the present study [18].
The variations in the sample size, type of exercises, number of repetitions, pain severity, and fear may contribute to the differences in the results of the Sorensen test. The mean age of female participants was 34.43 in the present study, while it was 36.1 for both genders in Mostagi’s study. Sex ratio was also effective in Sorensen test results. Physiological and pathophysiological differences, as well as the extent of pain and fear in patients, are likely to affect the test results. The type and repetition of exercises in Mostagi’s study were not similar to the present study. The former included Mat and Apparatus Pilates exercises, while the latter focused on the core exercises and trunk stability.
A limitation of the present study was the small sample size; however, it was still one of the largest populations available in the literature about Pilates in MS. Our study subjects were only females and their disability status were mild to moderate; therefore, we can only generalize our results to females that are not affected severely. Accordingly, the effects of our presented program could be different in males or a more severely affected population.
5. Conclusion
In general, the present study data were indicative of the positive effects of modified Pilates exercises on increasing lumbopelvic motor control, increasing trunk muscles endurance, pain relief, and functional disability improvement. Consequently, modified Pilates is recommended as a therapeutic program for the treatment of patients with non-specific LBP.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by Ethics Commitee of Zahedan Univrsity of Medical Sciences (Code: IR.ZAUMS.REC.1396.85).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally in preparing all parts of this research.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to special thanks to the patients who participated in the study . In addition we are grateful of zahedan university of medical science for approve this research.
References
- Scholtes SA, Norton BJ, Lang CE, Van Dillen LR. The effect of within-session instruction on lumbopelvic motion during a lower limb movement in people with and people without low back pain. Manual Therapy. 2010; 15(5):496-501. [DOI:10.1016/j.math.2010.05.003] [PMID] [PMCID]
- Ebadi S, Ansari NN, Naghdi S, Jalaei S, Sadat M, Bagheri H, et al. The effect of continuous ultrasound on chronic non-specific low back pain: A single blind placebo-controlled randomized trial. BMC Musculoskeletal Disorders. 2012; 13(1):192. [DOI:10.1186/1471-2474-13-192] [PMID] [PMCID]
- Castro-Sánchez AM, Lara-Palomo IC ,Matarán-Peñarrocha GA, Fernández-Sánchez M, Sánchez-Labraca N, Arroyo-Morales M. Kinesio Taping reduces disability and pain slightly in chronic non-specific low back pain: A randomised trial. Journal of Physiotherapy. 2012; 58(2):89-95. [DOI:10.1016/S1836-9553(12)70088-7]
- Garbenyte T, Poskaitis V, Zaveckas V, Siupsinskas L, Gudas R. Effect of general versus specialized exercises on movement control of lombopelvic region in subjects with chronic low back pain. Education, Physical Training, Sport. 2013; 3(90):21-30. [DOI:10.33607/bjshs.v3i90.165]
- Scholtes SA, Gombatto SP, Van Dillen LR. Differences in lumbopelvic motion between people with and people without low back pain during two lower limb movement tests. Clinical Biomechanics. 2009; 24(1):7-12. [DOI:10.1016/j.clinbiomech.2008.09.008] [PMID] [PMCID]
- McGill SM. The biomechanics of low back injury: Implications on current practice in industry and the clinic. Journal of Biomechanics. 1997; 30(5):465-75. [DOI:10.1016/S0021-9290(96)00172-8]
- Bala K, Gakhar M, Jagga V. Effect of endurance training of trunk extensor muscles on pain and endurance in patients with sub acute nonspecific low backache. Journal of Exercise Science and Physiotherapy. 2012; 8(2):82-6. http://www.efha.in/wp-content/uploads/2015/01/FULL-TEXT-UAIC-97301682020.pdf
- De Lorenzo CE. Pilates: What is it? Should it be used in rehabilitation? Sports Health. 2011; 3(4):352-61. [DOI:10.1177/1941738111410285] [PMID] [PMCID]
- Muscolino JE, Cipriani S. Pilates and the “powerhouse”-I. Journal of Bodywork and Movement Therapies. 2004; 8(1):15-24. [DOI:10.1016/S1360-8592(03)00057-3]
- Kloubec J. Pilates: How does it work and who needs it? Muscles, Ligaments and Tendons Journal. 2011; 1(2):61-6. [PMCID]
- Wells C, Kolt GS, Marshall P, Hill B, Bialocerkowski A. The effectiveness of Pilates exercise in people with chronic low back pain: A systematic review. PloS One. 2014; 9(7):e100402. [DOI:10.1371/journal.pone.0100402] [PMID] [PMCID]
- Cho KH, Beom JW, Lee TS, Lim JH, Lee TH, Yuk JH. Trunk muscles strength as a risk factor for nonspecific low back pain: A pilot study. Annals of Rehabilitation Medicine. 2014; 38(2):234-40 [DOI:10.5535/arm.2014.38.2.234] [PMID] [PMCID]
- Chok B, Lee R, Latimer J, Tan SB. Endurance training of the trunk extensor muscles in people with subacute low back pain. Physical Therapy. 1999; 79(11):1032-42. [DOI:10.1093/ptj/79.11.1032] [PMID]
- Van Dillen LR, Sahrmann SA, Wagner JM. Classification, intervention, and outcomes for a person with lumbar rotation with flexion syndrome. Physical Therapy. 2005; 85(4):336-51. [DOI:10.1093/ptj/85.4.336] [PMID]
- Bergmark A. Stability of the lumbar spine: A study in mechanical engineering. Acta Orthopaedica Scandinavica. 1989; 60(suppl 230):1-54. [DOI:10.3109/17453678909154177] [PMID]
- Panjabi M, Abumi K, Duranceau J, Oxland T. Spinal stability and intersegmental muscle forces: A biomechanical model. Spine. 1989; 14(2):194-200. [DOI:10.1097/00007632-198902000-00008] [PMID]
- Hodges P, Richardson C, Jull G. Evaluation of the relationship between laboratory and clinical tests of transversus abdominis function. Physiotherapy Research International. 1996; 1(1):30-40. [DOI:10.1002/pri.45] [PMID]
- Gladwell V, Head S, Haggar M, Beneke R. Does a program of Pilates improve chronic non-specific low back pain? Journal of Sport Rehabilitation. 2006; 15(4):338-50. [DOI:10.1123/jsr.15.4.338]
- Latimer J, Maher CG, Refshauge K, Colaco I. The reliability and validity of the Biering-Sorensen test in asymptomatic subjects and subjects reporting current or previous nonspecific low back pain. Spine. 1999; 24(20):2085-9. [DOI:10.1097/00007632-199910150-00004] [PMID]
- Paungmali A, Henry LJ, Sitilertpisan P, Pirunsan U, Uthaikhup S. Improvements in tissue blood flow and lumbopelvic stability after lumbopelvic core stabilization training in patients with chronic non-specific low back pain. Journal of Physical Therapy Science. 2016; 28(2):40-635. [DOI:10.1589/jpts.28.635] [PMID] [PMCID]
- Hodges PW. Pain and motor control: From the laboratory to rehabilitation. Journal of Electromyography and Kinesiology. 2011; 21(2):220-8. [DOI:10.1016/j.jelekin.2011.01.002] [PMID]
- Wright A. Recent concepts in the neurophysiology of pain .Manual Therapy. 1999; 4(4):196-202. [DOI:10.1054/math.1999.0207] [PMID]
- Kliziene I, Sipaviciene S, Vilkiene J, Astrauskiene A, Cibulskas G, Klizas S, et al. Effects of a 16-week Pilates exercises training program for isometric trunk extension and flexion strength. Journal of Bodywork and Movement Therapies. 2017; 21(1):124-32 [DOI:10.1016/j.jbmt.2016.06.005] [PMID]
- Mostagi FQRC, Dias JM, Pereira LM, Obara K, Mazuquin BF, Silva MF, et al. Pilates versus general exercise effectiveness on pain and functionality in non-specific chronic low back pain subjects. Journal of Bodywork and Movement Therapies. 2015; 19(4):636-45 [DOI:10.1016/j.jbmt.2014.11.009] [PMID]
- Ferreira-Valente M.A, Pais-Ribeiro JL, Jensen MP. Validity of four pain intensity rating scales. Pain. 2011; 152(10):2399-404. [DOI:10.1016/j.pain.2011.07.005] [PMID]
- Fairbank JC, Pynsent PB. The Oswestry disability index. Spine. 2000; 25(22):2940-52. [DOI:10.1097/00007632-200011150-00017] [PMID]
- Panjabi MM. The stabilizing system of the spine. Part I. Function, dysfunction, adaptation, and enhancement. Journal of Spinal Disorders. 1992; 5(4):383-9. [DOI:10.1097/00002517-199212000-00001] [PMID]
- Ota M, Kaneoka K, Hangai M, Koizumi K, Muramatsu T. Effectiveness of lumbar stabilization exercises for reducing chronic low back pain and improving quality-of-life. Journal of Physical Therapy Science. 2011; 23(4):679-81. [DOI:10.1589/jpts.23.679]
- Phrompaet S, Paungmali A, Pirunsan U, Sitilertpisan P. Effects of pilates training on lumbo-pelvic stability and flexibilty. Asian Journal of Sports Medicine. 2011; 2(1):16-22. [DOI:10.5812/asjsm.34822] [PMID] [PMCID]
- Patti A, Bianco A, Paoli A, Messina G, Montalto MA, Bellafiore M, et al. Pain perception and stabilometric parameters in people with chronic low back pain after a pilates exercise program: A randomized controlled trial. Medicine. 2016; 95(2):e2414. [DOI:10.1097/MD.0000000000002414] [PMID] [PMCID]
Type of Study: Research |
Subject:
Special
Received: 2020/07/6 | Accepted: 2020/08/26 | Published: 2020/10/1
Received: 2020/07/6 | Accepted: 2020/08/26 | Published: 2020/10/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |