Sun, Aug 25, 2024
Volume 14, Issue 3 (Summer 2024)
PTJ 2024, 14(3): 227-240 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Shahbandi B, Kalantariyan M. The Effect of Functional Training on 9+ Functional Test Scores in Active Men. PTJ 2024; 14 (3) :227-240
URL: http://ptj.uswr.ac.ir/article-1-600-en.html
URL: http://ptj.uswr.ac.ir/article-1-600-en.html
1- Department of Sports Pathology and Corrective Exercise, Faculty of Physical Education and Sports Sciences, South Tehran Branch, Islamic Azad University, Tehran, Iran.
2- Department of Sports Pathology and Corrective Exercise, School of Sports Sciences, Shahid Rajaee Teacher Training University, Tehran, Iran.
2- Department of Sports Pathology and Corrective Exercise, School of Sports Sciences, Shahid Rajaee Teacher Training University, Tehran, Iran.
Full-Text [PDF 1063 kb]
(73 Downloads)
| Abstract (HTML) (510 Views)
Full-Text: (36 Views)
Introduction
Adequate posture serves as a vital indicator reflecting the efficacy of the motor system and the overall musculoskeletal well-being [1]. Deviations from the norm in musculoskeletal structures, induced by irregularities and incorrect movement patterns, engender atypical stressors in these structures [2]. While initial stages may not elicit any overt complaints from individuals regarding the presence of anomalies within their movement patterns [3], the absence of due diligence in addressing such issues can culminate in a myriad of adverse consequences. These repercussions encompass but are not limited to pain, disability, diminished quality of life, joint surface deterioration, psychological afflictions [4-6], and augmented economic burdens [1, 7]. Muscle imbalances serve as the impetus for the repetitive enactment of erroneous movement patterns, a cyclic occurrence that ultimately begets faulty motor programming and movement acquisition. Over time, these manifestations precipitate shifts in joint forces and alterations in joint proprioception. These, in turn, mark the initiation of micro trauma and eventually give rise to degenerative alterations, characterized as macrotrauma, ultimately compromising postural control [8].
Undoubtedly, exercise stands as the paramount determinant of individuals’ health, and the burgeoning empirical evidence underscores the growing significance of physical activity in this regard [9, 10]. Integral to the realm of sports participation is the specter of sports-related injuries, a concern that extends its impact to mortality rates, decreased athletic efficiency, and shortened sporting careers. Consequently, researchers and medical practitioners in sports medicine are tirelessly seeking efficacious solutions to ascertain the risk factors associated with these injuries, with the ultimate aim of reducing their incidence [11]. One avenue towards identifying athletes susceptible to injuries and delineating pertinent risk factors involves the practice of pre-participation assessments in sports [12]. In light of the escalating incidence of sports-related injuries, contemporary sports medicine has embraced pre-competition screenings and evaluations, a measure intended not only to proactively avert injuries but also to enhance athletes’ performance and mitigate the manifestation of functional impairments. It is crucial to underscore that the foremost objective of pre-participation assessments is the amelioration of athletes’ health and safety during training and competition, with the ultimate goal of promoting their well-being, rather than excluding them from participation in sports [11, 12].
An integral component of pre-participation assessments involves the scrutiny of movement patterns and the discernment of potential risk factors during the execution of functional movements [12, 13]. Furthermore, these evaluations gauge the extent of asymmetry and limitations present in various regions of an individual’s physique [13-15].
One of the most prevalent approaches to assess movement patterns and conduct performance tests to identify individuals at risk of injury involves the utilization of the functional movement screening (FMS) test [13, 16-24]. The FMS is specifically crafted to assess diverse movement capabilities, making it applicable not only to high-level athletes but also to recreational participants [16, 17]. This tool serves to detect limitations and deviations from typical movement patterns. These assessments are meticulously designed to scrutinize the intricate interplay between the mobility within the movement chain and the requisite stability essential for executing functional and vital movement patterns. Research endeavors exploring the relationship between FMS scores and injury incidence have recognized FMS scores as a predictive factor for injury occurrence [25].
In this regard, high-performance profile (HPP), which is a developed screening system to evaluate movement patterns, was designed by the United States Tennis Association (USTA) and evaluates the performance of tennis players [10]. The purpose of HPP is to reveal weaknesses and deficiencies related to strength and flexibility, as well as to identify areas of the body that athletes need to focus more on training. Since the FMS tests do not have the necessary focus for specific assessment of the condition of the spine, especially the lumbopelvic region, in this test, an attempt has been made to correct it by adding new tests and removing unnecessary and repetitive ones and introducing a series of more appropriate tests to evaluate people’s performance. In the last 10 years, a set of different parts of the Cook and HPP tests have been used by specialists in the evaluation test and screening of the functional movements of the forum [10]. A total of seven tests have been extracted from two different sources and two more tests have been added to the total of tests to challenge and test the dynamic performance of trunk flexors and spine rotators, and the number of these tests has reached nine. The purpose of this work is to increase the functionality of this series of tests [11, 12].
Simultaneously, given the burgeoning popularity of bodybuilding across various age demographics within society, it stands as a highly attractive pursuit. With an increasing number of individuals engaging in bodybuilding for the sake of improved health, it becomes imperative to assess performance test-derived risk factors within this domain, thus enhancing our capacity to safeguard individual well-being.
Corrective exercises serve as a viable means to ameliorate and rectify identified movement impairments. These exercises have been designed with the specific aim of remediating defects within movement patterns, enhancing movement equilibrium, and restoring postural stability. Notably, research studies have demonstrated that a targeted approach, involving the identification of movement impairments and the subsequent implementation of appropriate exercises to ameliorate and reduce these anomalies, can contribute to reduced damage incurred [26, 27]. In contrast to conventional resistance training programs, corrective exercises place paramount emphasis on the refinement of movement pattern quality [28].
Conducting pre-season and pre-competition screenings constitutes an effective strategy for procuring essential data to inform the development of tailored components within sports programs. Beyond accommodating the unique demands of each sport, these screenings offer the opportunity to preemptively mitigate hazardous elements through the incorporation of corrective training methodologies, either as standalone interventions or integrated into the existing training protocol. Such proactive measures enable athletes to engage in their respective sports with heightened confidence [17, 29]. Given the paramount significance of movement patterns and their intricate relationship with sports-related injuries, the present research endeavors to identify improper movement patterns exhibited by athletes specializing in resistance training. Furthermore, this study was conducted to introduce corrective and training modalities to ameliorate and reduce the associated risk factors. Also, considering that many studies have been conducted regarding FMS, but according to studies in the field of 9+ test, it is very limited, therefore research is conducted that focuses on functional exercises on functional test scores.
Materials and Methods
The current research design was a randomized field trial. The statistical population for this research encompassed individuals engaged in recreational “resistance training”, who were selected from among the resistance training athletes of district five of Tehran Province, Iran. Employing G*Power software, version 3.1.9.7, a sample size of 38 participants was determined, with an effect size of 0.8, an α level of 0.05, and a power of 80%. These participants were subsequently divided into two groups, consisting of 15 individuals in the control group and 15 individuals in the training group, as per the specified assumptions, even accounting for potential sample attrition.
The inclusion criteria included male gender, age falling within the 18 to 30-year range, engagement in a minimum of three weekly bodybuilding sessions involving the utilization of machines and weights, the absence of discernible abnormalities in the upper and lower extremities, the absence of musculoskeletal injuries in any bodily organs and functional movement score below 14. The exclusion criteria included subjects expressing dissatisfaction and a reluctance to continue with the research procedures, failure to participate in two consecutive sessions or three alternating sessions of exercises, the onset of pain or discomfort during exercise protocols, or the utilization of alternative treatment methods, such as physiotherapy.
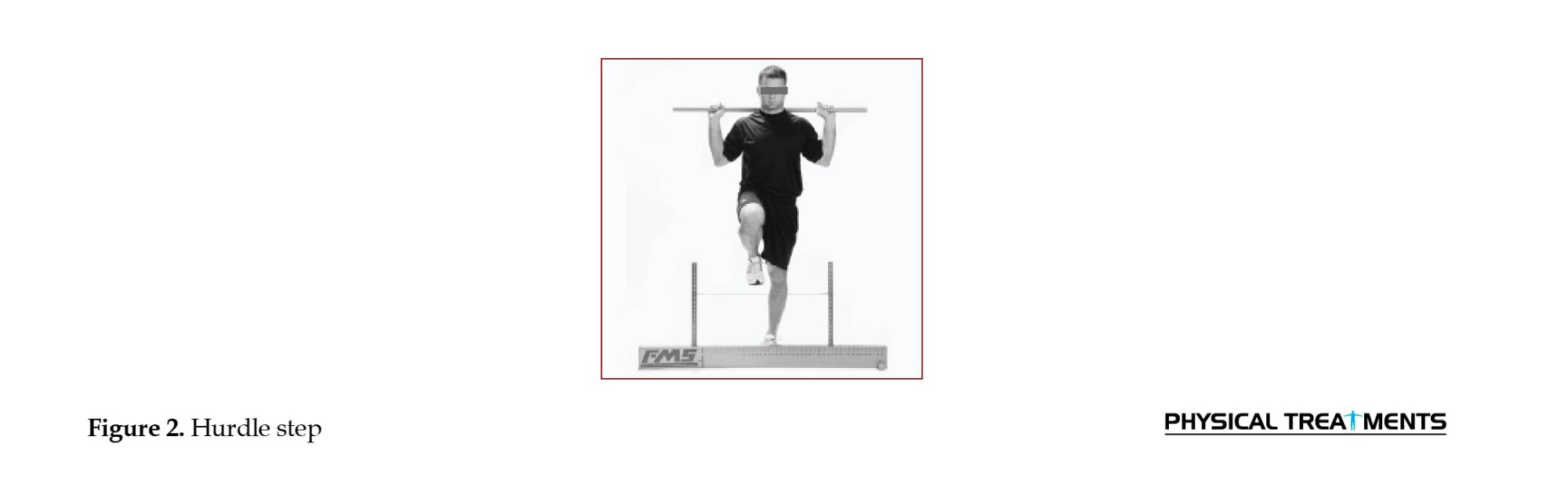
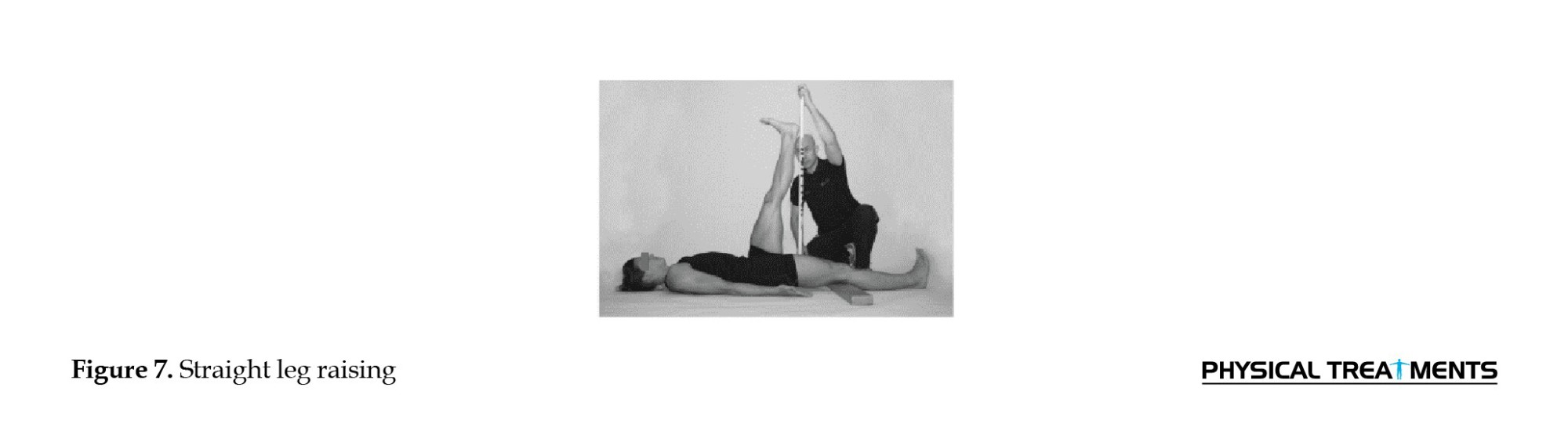
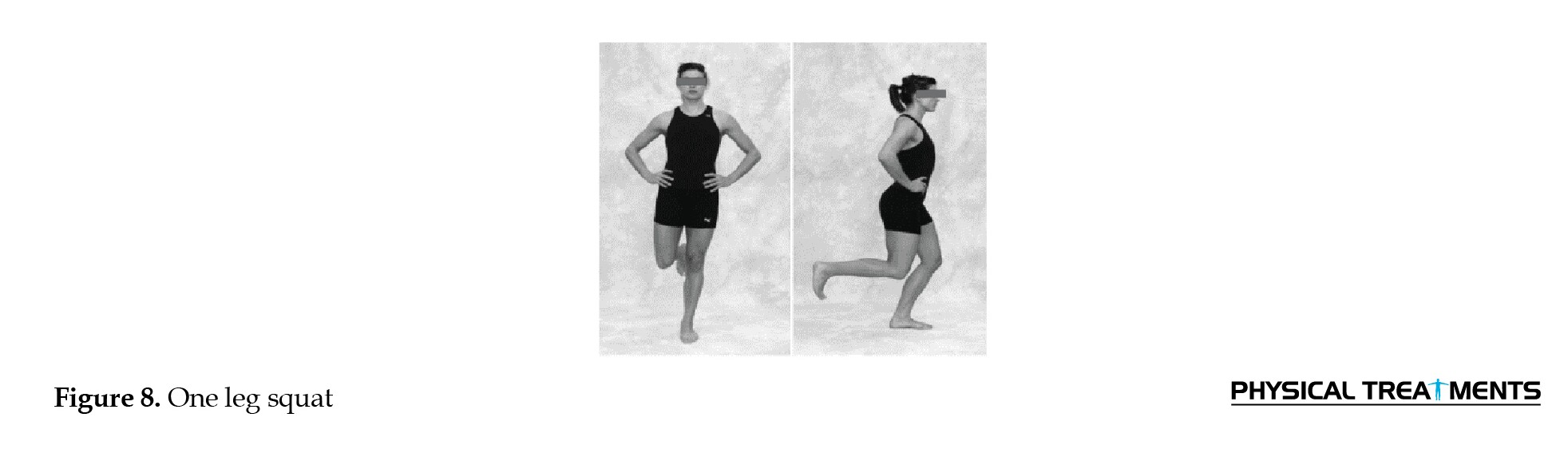
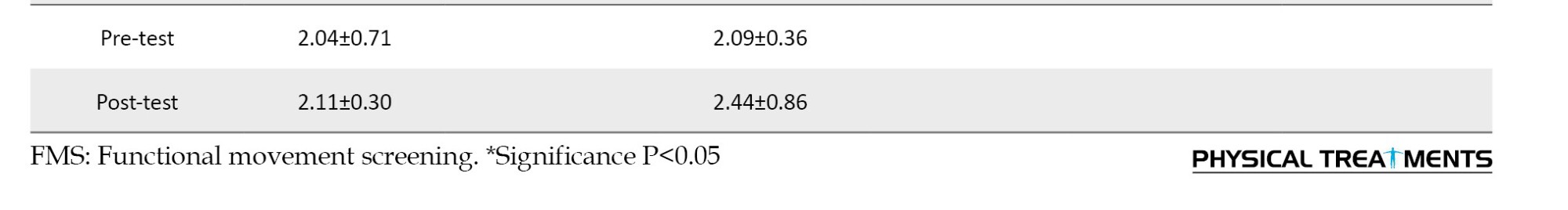
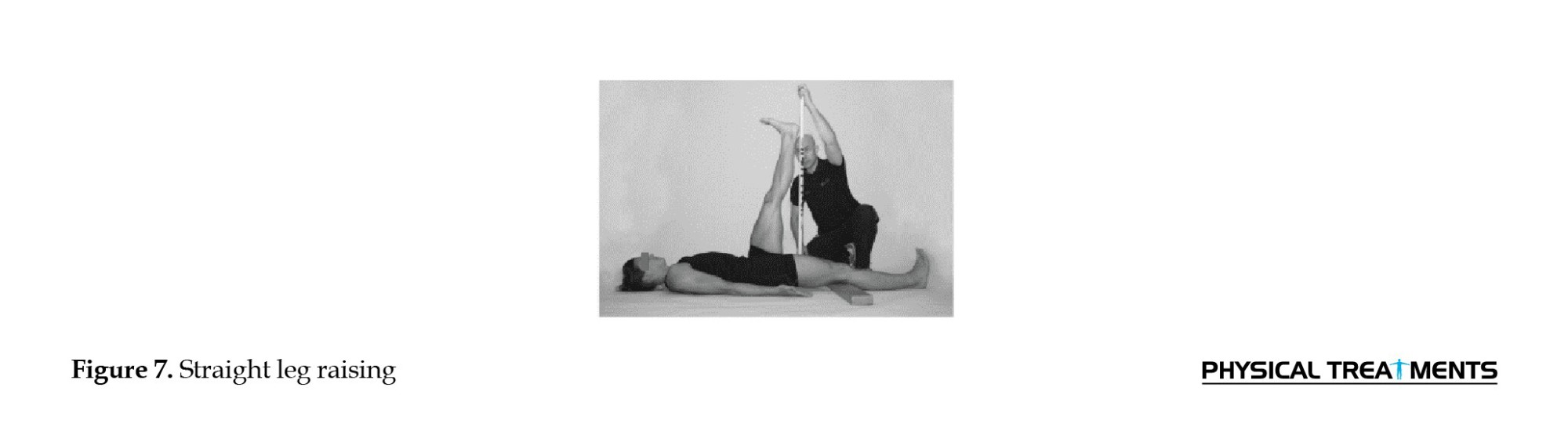
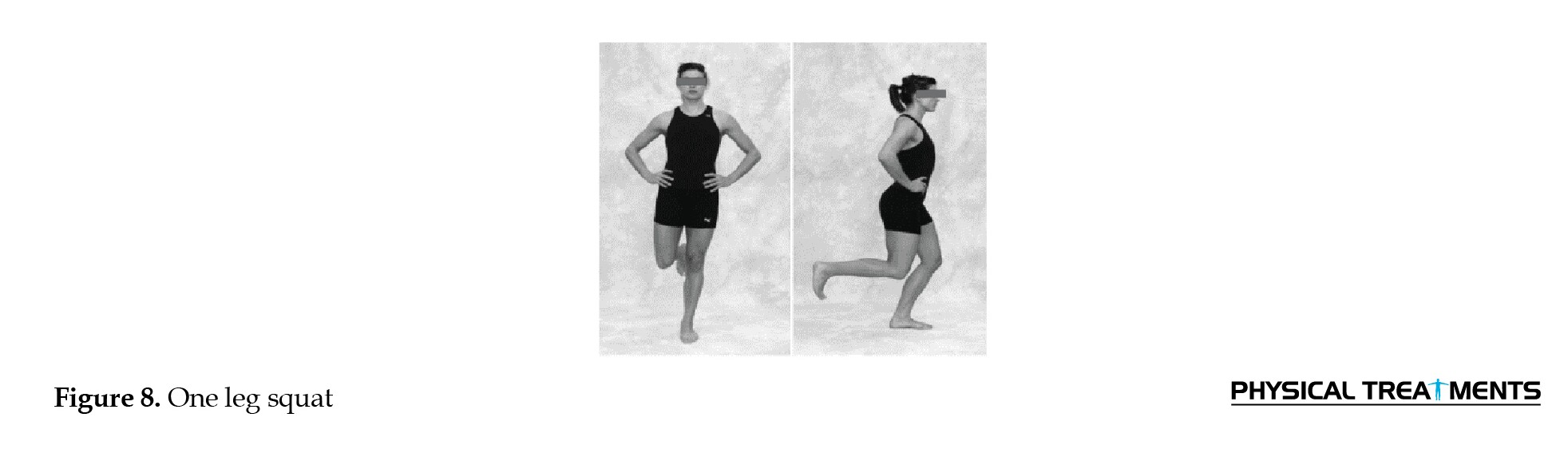
The athletes’ movement patterns were evaluated using the 9+ test. The 9+ assessment includes 10 distinct movement tests specifically designed to detect any limitations or deviations from typical movement patterns. These tests are meticulously crafted to assess the intricate interplay between the mobility of the movement chain and the requisite stability essential to execute functional and fundamental movement patterns. In the context of the 9+ test, a score of 3 is assigned when the tests are executed correctly without any compensatory movements. A score of 2 is awarded if the movement is performed with compensatory movements, while a score of 1 is allotted when an individual is unable to execute the movement without resorting to compensatory actions. The series of tests include assessments for the deep squat, hurdle step, lunge, shoulder mobility, straight leg raising, push-up, one leg squat, seated trunk rotation, straight leg raises test, and rotational stability [30, 31] (Figures 1-10).







The participants were stratified into two distinct groups, an experimental group and a control group. All participants, belonging to both groups, convened at the Jahan-Ara Sports Club at predetermined intervals and completed assessments about the functional screening test, following a 5-minute warm-up period. Subsequently, individuals with a 9+ score below 14 were identified and assigned to either the experimental or control group. Those allocated to the experimental group engaged in an eight-week protocol of functional exercises, involving three sessions per week, each spanning 40 minutes.
The primary objective of each corrective exercise is to systematically enhance the capacity to execute various movement patterns while simultaneously refining form and control. Corrective exercises are strategically structured to target discrete elements of the exercises, breaking them down into more granular components of movement patterns. In the initial six weeks, the exercises are meticulously tailored to address specific functional movement patterns (Table 1).

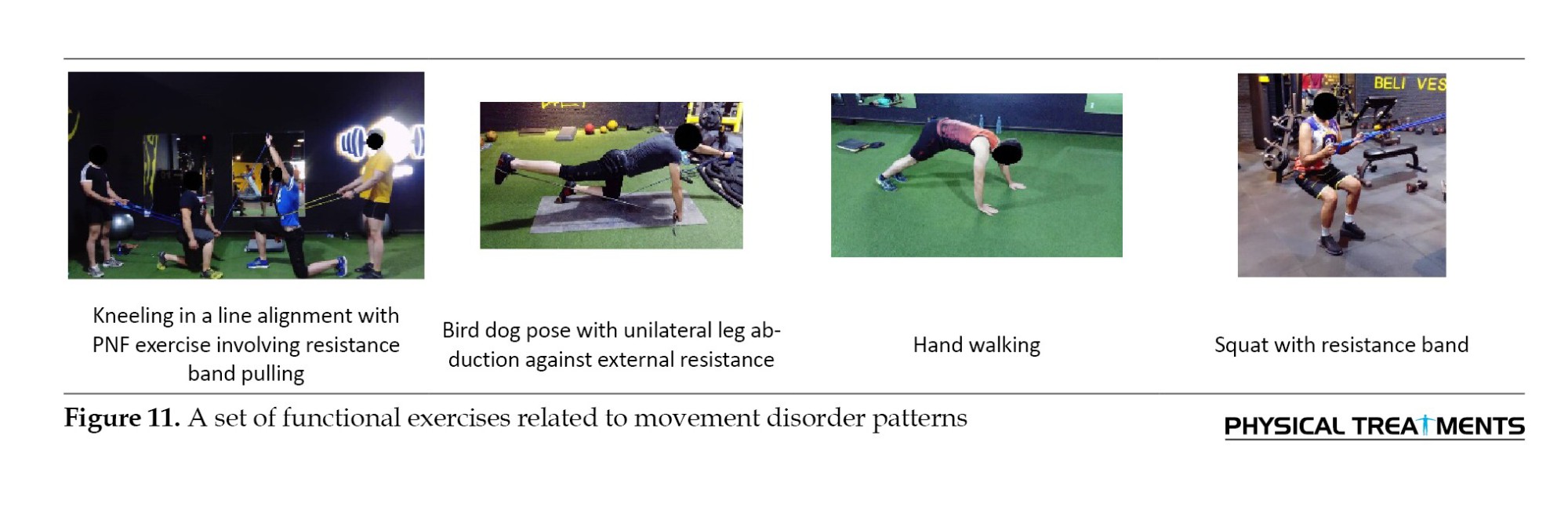
These exercises primarily aim to enhance either stability or mobility. Conversely, during weeks 7 and 8, a set of exercises is introduced that simultaneously challenges both mobility and stability (Table 2), incorporating integral components of movement patterns. The overarching aim throughout this progression is to continually refine and optimize these patterns [27].

The training programs comprised three sessions lasting 45 minutes each for eight weeks. It is noteworthy that the exercise protocol’s volume and intensity were meticulously tailored by the frequency, intensity, time, and type (FITT) principles.
Upon the conclusion of the 8-week corrective exercise intervention, each participant underwent a re-evaluation using the functional movement pattern. Subsequently, the participants were assessed through a comparative analysis of the initial and post-intervention evaluations to ascertain the changes in scores.
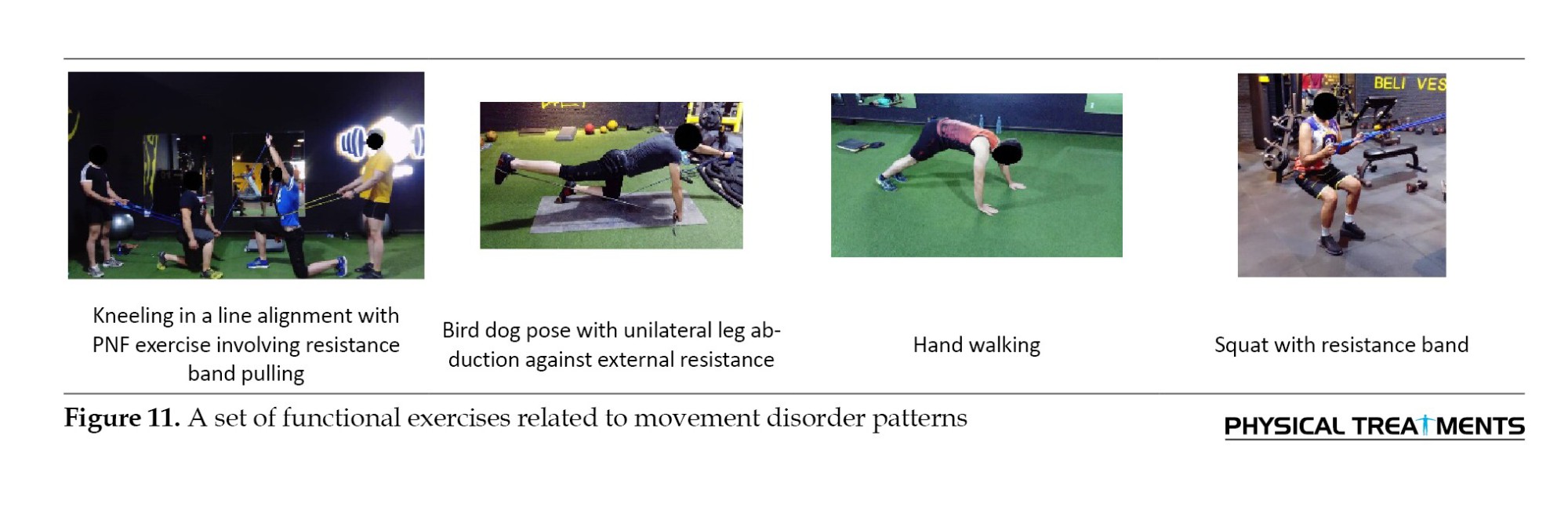
Figure 11 shows a selection of functional exercises associated with movement impairment patterns.
Subsequently, following the compilation of research data, the normality of the data was assessed using the Shapiro-Wilk test. Intragroup comparisons were conducted utilizing the paired t-test, while intergroup comparisons were performed employing the analysis of covariance (ANCOVA) test, all at a significance level of 95%, utilizing SPSS software, version 22.
Results
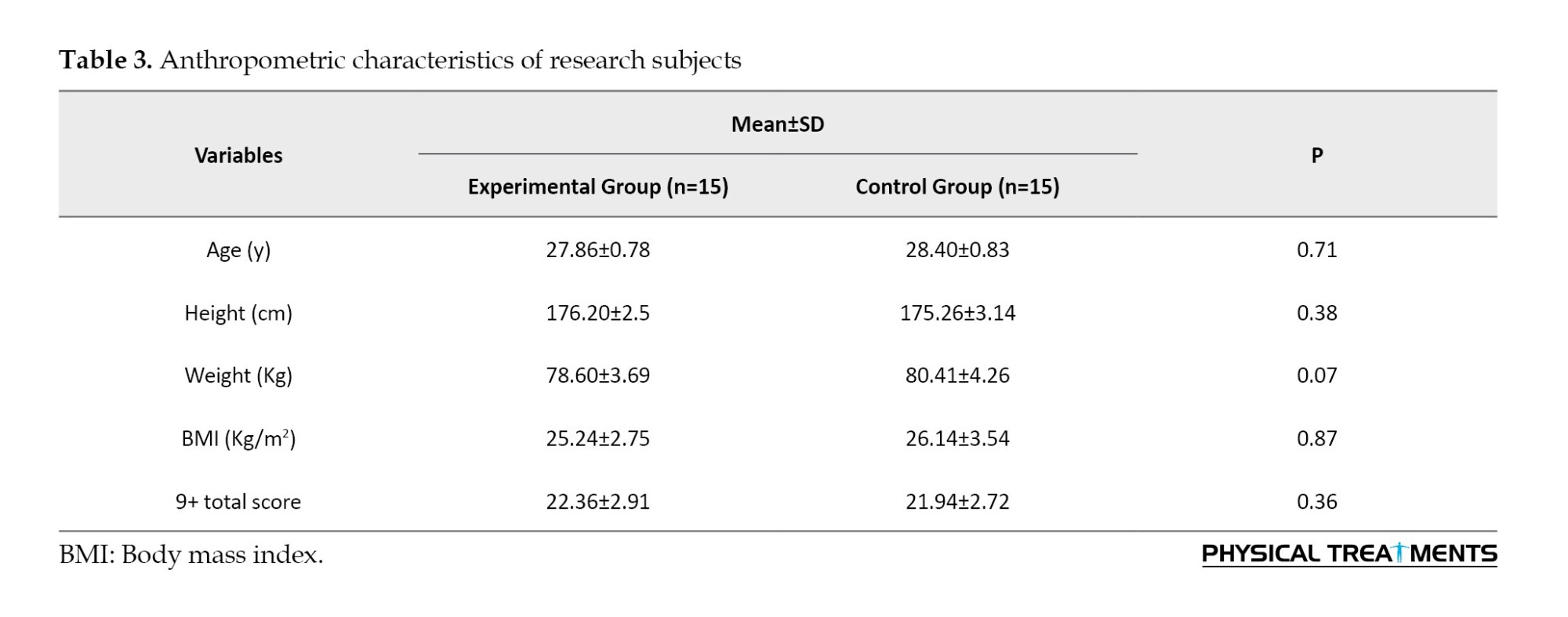
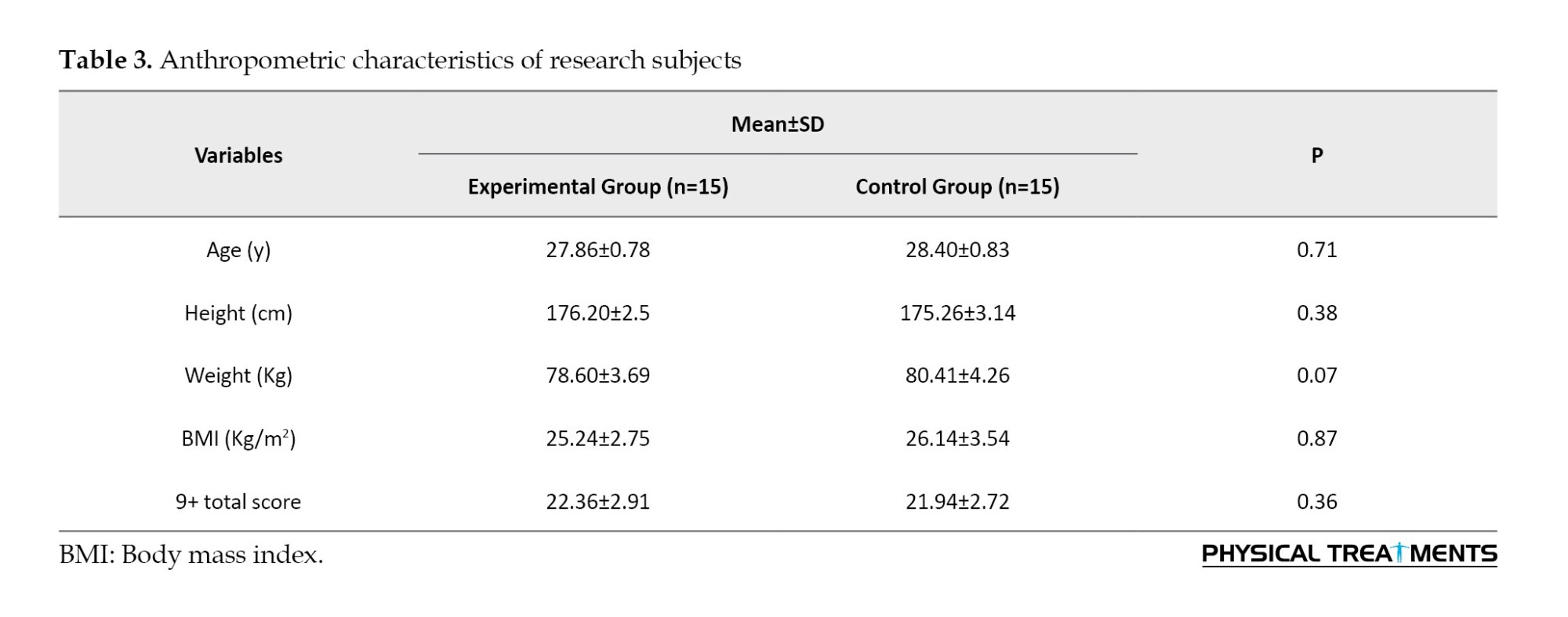
Table 3 presents the anthropometric characteristics of the research subjects, categorized by age, height, weight, and body mass index (BMI).
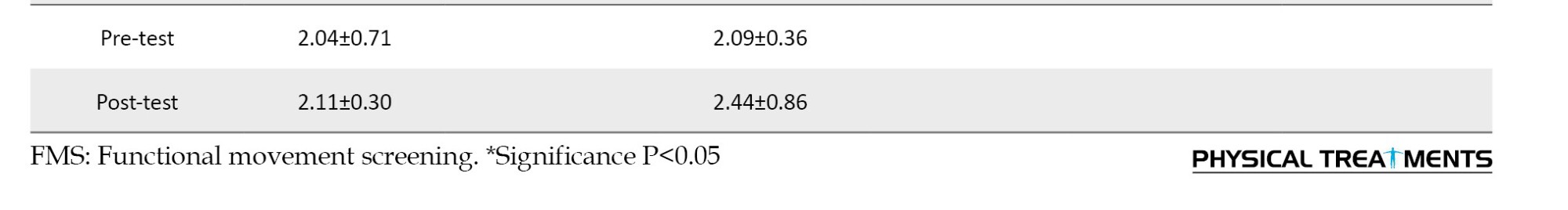
The analysis employed in this study involved the use of a paired t-test to evaluate intragroup differences and covariance analysis to assess intergroup differences, as outlined in Table 4. The findings from the paired t-test revealed a significant discrepancy between the pre-test and post-test scores (P<0.05) in all 9+ tests, except the shoulder mobility test (P=0.85), specifically within the experimental group. Furthermore, the results derived from the ANCOVA test demonstrated a substantial differentiation between the experimental and control groups across all 9+ tests, except the shoulder mobility test (P=0.22) (P<0.05). Remarkably, the experimental group exhibited superior scores in all 9+ test variables, excluding the shoulder mobility test, compared to the control group following an 8-week corrective exercise protocol.

Discussion
The results of the paired t-test analysis in this study demonstrated a notable divergence. Specifically, in all 9+ tests, except for the shoulder mobility assessment, a significant disparity between the pre-test and post-test scores was exclusively observed in the experimental group (P<0.05). Additionally, the outcomes derived from the ANCOVA test unveiled a substantial distinction between the two groups, namely the experimental and control groups, across all 9+ tests, except for the shoulder mobility evaluation (P<0.05). In summary, across all variables assessed in the 9+ test, the experimental group exhibited superior scores compared to the control group after 8 weeks of corrective exercises.
The results of this current study are consistent with the research outcomes reported by Chen et al. [32], Boucher et al. [27], Jafari et al. [33], Woods et al. [34], Soltandoost et al. [35], Siamaki et al. [36], and Butcher et al. [27].
Given the scarcity of research about the implementation of corrective exercises in the bodybuilding community, this section endeavors to utilize the most relevant studies available on this subject.
Boucher et al. in their study investigated the impact of a four-week corrective exercise protocol on FMS test scores among high school girls. Their results indicated a significant increase in the FMS test score in the post-test (17.29) compared to the pre-test (14.43) [27]. The resemblance in training protocols between Boucher’s research and the present study contributes to the alignment of the two investigations.
Jafari et al. [33] similarly explored the impact of corrective exercises on FMS test scores among firefighters. Their results indicated that the FMS test score for the experimental group increased significantly, rising from a mean of 10 in the pre-test to 17 in the post-test. The resemblance between the two studies can be attributed to similarities in their training protocols and the inclusion of exercises involving movements, such as single-leg balance, single-leg deadlift, mountaineer, and squat, among others.
Leaderman’s definition of functional movements encompasses a distinct repertoire of movements tailored to each individual. Within this collection of movements, there are those essential for daily activities like eating, cleaning, and walking, categorized as general skills. Additionally, another subset of movements known as special skills exists, encompassing both unique and potentially shared activities, such as sports and occupational tasks (Figures 2, 3, 4, 5 and 6). What may constitute a functional set for one individual can entail playing tennis, while for another, it may involve practicing yoga poses. When an individual acquires a new movement or skill, it becomes an addition to their repertoire of movements. Movements falling outside an individual’s typical range are deemed as extra-functional. In Leatherman’s work on neuromuscular rehabilitation, rehabilitation is characterized as a process aimed at enhancing an individual’s movement capacity by leveraging their existing set of movements. According to this definition, when rehabilitating and enhancing the capabilities of someone who plays tennis, the set of functional tennis movements should be employed. Conversely, movement patterns utilized in therapy and rehabilitation that do not belong to the individual’s functional set (i.e. are extra-functional) are likely to yield diminished effects. For instance, a rehabilitation program centered around a set of soccer movements would be less effective and less pertinent for an injured tennis player [37].
In the context of neuromuscular rehabilitation, Leatherman outlines a set of codes governing the rehabilitation program and the requisite neuromuscular adaptations to attain the intended outcome [37]. These codes encompass elements, such as cognition, being active, feedback, repetition, and similarity in practical application.
Hence, for effective recovery and rehabilitation, an individual must possess cognitive awareness of their actions (cognitive) and the objectives of the recovery process, engaging actively in its pursuit (being active). The correction of movements necessitates internal sensory feedback or guidance (feedback), and the task should be repetitively practiced at various intervals (repetition). Moreover, rehabilitation exercises should closely resemble the goal of rehabilitation and the intended task (similarity). By incorporating these adaptation codes into the training protocol, motor control rehabilitation and enhancement become readily achievable [37]. According to the principle of similarity, most exercises chosen to rectify existing deficiencies mirror the targeted tasks. Therefore, as per Lederman’s assertions, the likelihood of improving these deficits and increasing performance test scores appears promising.
The shoulder mobility test assesses the unilateral and reciprocal range of motion in the shoulder joint, encompassing internal rotation and adduction in one shoulder and external rotation and abduction in the other. Successful performance in this evaluation necessitates the proper mobility of the scapula and extension of the spine. Inadequate performance on this test may be attributed to various factors, including an imbalance in the range of motion between external and internal rotation within a shoulder joint. Specifically, the shortening of the pectoralis minor and latissimus dorsi muscles can lead to postural alterations, such as forward head posture and rounded shoulders in athletes. Given the emphasis placed by bodybuilders on increasing chest and back muscle volume, the shortening of these muscles can result in a reduction in the range of motion for internal and external shoulder rotation. Consequently, engaging in exercises involving lying on one’s side while extending the arm and rotating the trunk, lying on the side with shoulder movements, and lying on the side while elevating the arm and rotating the trunk likely contributed to the amelioration of this diminished range of motion. As a result, the shoulder mobility test scores likely improved in the post-test.
The stability push-up test assesses the ability of the trunk and spine to maintain stability in both anterior and posterior planes during closed motor chain activities involving the upper limbs. This evaluation specifically focuses on the trunk’s stability in the sagittal plane. Symmetry in upper limb movements, particularly during activities like push-ups, is a key consideration in this test. The significance of this assessment lies in the fact that adequate trunk stability is essential in sports activities to optimize movement efficiency. Inadequate stability can result in the wastage of energy during physical exertion, ultimately leading to diminished functional movements and an increased risk of microtrauma and injury. The improvement in scores observed in the post-test for this evaluation can likely be attributed to the inclusion of specific exercises in the training protocol. These exercises, such as kneeling exercises in a linear fashion coupled with proprioceptive neuromuscular facilitation (PNF) techniques, and resistance band exercises designed to challenge the central stability region, along with the push-up hand walkout and return to a standing position, likely contributed to enhancing performance in the stability push-up test.
The deep squat test necessitates high coordination and mobility involving multiple anatomical structures, including organs, muscles, and the central stability system. It also places a demand on overall body mechanics and neurovascular control. Moreover, it evaluates the mobility and stability of the shoulder, scapula, and thoracic region of the spine [38, 39]. Poor performance in the deep squat test can typically be attributed to three primary factors:
1. Constraints in upper limb mobility and glenohumeral joint weakness.
2. Limitations in lower limb mobility.
3. Impairments in motor control in the central stability region [39].
In the huddle step test, the mobility of the front foot and the stability of the back foot carry significant weight. Insufficient mobility in the stepping foot and inadequate stability in the stance foot can lead to reduced scores in this particular evaluation [39]. When it comes to the lunge test, diminished 9+ scores are often associated with restrictions in the thoracic spine area and decreased mobility in the hip, knee, and ankle joints.
Engaging in a protocol of specific exercises, such as lying on one’s side while simultaneously turning away and raising the arms and shoulders, along with trunk rotation, has the potential to enhance upper limb mobility. Likewise, performing thigh-bending exercises during the single-leg deadlift movement while pulling the hands forward, executing the “climbing the mountain” maneuver, and adopting the “flying dog” position while raising the opposite arm and leg in synchrony, as well as doing the same “flying dog” pose with the additional element of extending the opposite arm and leg against elastic resistance, likely contributes to improved motor control within the central stability region. This multifaceted approach may result in increased scores in the deep squat test during the post-test assessment. Furthermore, incorporating exercises, such as half-knee lunges while simultaneously raising the opposite hand, engaging in a line-kneeling stance while throwing a ball toward a partner, and assuming a kneeling position while performing PNF exercises by pulling against resistance from a rubber band are practices that may address identified weaknesses. The amelioration of these identified deficiencies represents a plausible rationale for the observed improvements in Lange test scores following the exercise intervention.
The push-up test underscores the significance of trunk stability, upper limb strength, and central region stability [39]. Engaging in exercises, such as the flying dog pose while extending the opposite arm and leg against the resistance provided by a rubber band, executing kneeling exercises in a row while throwing a ball towards a partner, practicing kneeling in a row with PNF exercises, and pulling a resistance rubber band against resistance all contribute to the potential rectification of these shortcomings and the subsequent elevation of scores in the post-test.
Conversely, the rotary stability test emphasizes neuromuscular coordination and energy transference throughout the body, both from upper to lower limbs and vice versa. It also assesses trunk stability across multiple planes. Weaknesses in overall body stability, challenges with scapula and hip stability, as well as limitations in knee, thigh, and trunk mobility, are recognized as factors contributing to lower scores in this particular test [39]. It is plausible that engaging in the aforementioned exercises has served to address these deficiencies, resulting in improved scores in the post-test.
Conclusion
Based on the research results, an 8-week program focusing on “functional impairment” in athletes engaged in “resistance training” and exhibiting movement impairments can result in significant enhancements in their movement patterns. Consequently, it is recommended that coaches consider implementing these exercises to ameliorate the movement patterns of “resistance training” athletes.
Limitation
One of the limitations of the current research is the small number of research subjects.
Suggestions
It is suggested to investigate the effect of functional exercises in the current research on female athletes and with a larger number of subjects.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research has not received any grant from any organization.
Authors' contributions
Conceptualization and data collection: Behnam Shahbandi; Study design: All authors; Data interpretation: Mohammad Kalantariyan.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors extend their gratitude to all the coaches, officials, and athletes who contributed to the successful execution of this research project.
References
Adequate posture serves as a vital indicator reflecting the efficacy of the motor system and the overall musculoskeletal well-being [1]. Deviations from the norm in musculoskeletal structures, induced by irregularities and incorrect movement patterns, engender atypical stressors in these structures [2]. While initial stages may not elicit any overt complaints from individuals regarding the presence of anomalies within their movement patterns [3], the absence of due diligence in addressing such issues can culminate in a myriad of adverse consequences. These repercussions encompass but are not limited to pain, disability, diminished quality of life, joint surface deterioration, psychological afflictions [4-6], and augmented economic burdens [1, 7]. Muscle imbalances serve as the impetus for the repetitive enactment of erroneous movement patterns, a cyclic occurrence that ultimately begets faulty motor programming and movement acquisition. Over time, these manifestations precipitate shifts in joint forces and alterations in joint proprioception. These, in turn, mark the initiation of micro trauma and eventually give rise to degenerative alterations, characterized as macrotrauma, ultimately compromising postural control [8].
Undoubtedly, exercise stands as the paramount determinant of individuals’ health, and the burgeoning empirical evidence underscores the growing significance of physical activity in this regard [9, 10]. Integral to the realm of sports participation is the specter of sports-related injuries, a concern that extends its impact to mortality rates, decreased athletic efficiency, and shortened sporting careers. Consequently, researchers and medical practitioners in sports medicine are tirelessly seeking efficacious solutions to ascertain the risk factors associated with these injuries, with the ultimate aim of reducing their incidence [11]. One avenue towards identifying athletes susceptible to injuries and delineating pertinent risk factors involves the practice of pre-participation assessments in sports [12]. In light of the escalating incidence of sports-related injuries, contemporary sports medicine has embraced pre-competition screenings and evaluations, a measure intended not only to proactively avert injuries but also to enhance athletes’ performance and mitigate the manifestation of functional impairments. It is crucial to underscore that the foremost objective of pre-participation assessments is the amelioration of athletes’ health and safety during training and competition, with the ultimate goal of promoting their well-being, rather than excluding them from participation in sports [11, 12].
An integral component of pre-participation assessments involves the scrutiny of movement patterns and the discernment of potential risk factors during the execution of functional movements [12, 13]. Furthermore, these evaluations gauge the extent of asymmetry and limitations present in various regions of an individual’s physique [13-15].
One of the most prevalent approaches to assess movement patterns and conduct performance tests to identify individuals at risk of injury involves the utilization of the functional movement screening (FMS) test [13, 16-24]. The FMS is specifically crafted to assess diverse movement capabilities, making it applicable not only to high-level athletes but also to recreational participants [16, 17]. This tool serves to detect limitations and deviations from typical movement patterns. These assessments are meticulously designed to scrutinize the intricate interplay between the mobility within the movement chain and the requisite stability essential for executing functional and vital movement patterns. Research endeavors exploring the relationship between FMS scores and injury incidence have recognized FMS scores as a predictive factor for injury occurrence [25].
In this regard, high-performance profile (HPP), which is a developed screening system to evaluate movement patterns, was designed by the United States Tennis Association (USTA) and evaluates the performance of tennis players [10]. The purpose of HPP is to reveal weaknesses and deficiencies related to strength and flexibility, as well as to identify areas of the body that athletes need to focus more on training. Since the FMS tests do not have the necessary focus for specific assessment of the condition of the spine, especially the lumbopelvic region, in this test, an attempt has been made to correct it by adding new tests and removing unnecessary and repetitive ones and introducing a series of more appropriate tests to evaluate people’s performance. In the last 10 years, a set of different parts of the Cook and HPP tests have been used by specialists in the evaluation test and screening of the functional movements of the forum [10]. A total of seven tests have been extracted from two different sources and two more tests have been added to the total of tests to challenge and test the dynamic performance of trunk flexors and spine rotators, and the number of these tests has reached nine. The purpose of this work is to increase the functionality of this series of tests [11, 12].
Simultaneously, given the burgeoning popularity of bodybuilding across various age demographics within society, it stands as a highly attractive pursuit. With an increasing number of individuals engaging in bodybuilding for the sake of improved health, it becomes imperative to assess performance test-derived risk factors within this domain, thus enhancing our capacity to safeguard individual well-being.
Corrective exercises serve as a viable means to ameliorate and rectify identified movement impairments. These exercises have been designed with the specific aim of remediating defects within movement patterns, enhancing movement equilibrium, and restoring postural stability. Notably, research studies have demonstrated that a targeted approach, involving the identification of movement impairments and the subsequent implementation of appropriate exercises to ameliorate and reduce these anomalies, can contribute to reduced damage incurred [26, 27]. In contrast to conventional resistance training programs, corrective exercises place paramount emphasis on the refinement of movement pattern quality [28].
Conducting pre-season and pre-competition screenings constitutes an effective strategy for procuring essential data to inform the development of tailored components within sports programs. Beyond accommodating the unique demands of each sport, these screenings offer the opportunity to preemptively mitigate hazardous elements through the incorporation of corrective training methodologies, either as standalone interventions or integrated into the existing training protocol. Such proactive measures enable athletes to engage in their respective sports with heightened confidence [17, 29]. Given the paramount significance of movement patterns and their intricate relationship with sports-related injuries, the present research endeavors to identify improper movement patterns exhibited by athletes specializing in resistance training. Furthermore, this study was conducted to introduce corrective and training modalities to ameliorate and reduce the associated risk factors. Also, considering that many studies have been conducted regarding FMS, but according to studies in the field of 9+ test, it is very limited, therefore research is conducted that focuses on functional exercises on functional test scores.
Materials and Methods
The current research design was a randomized field trial. The statistical population for this research encompassed individuals engaged in recreational “resistance training”, who were selected from among the resistance training athletes of district five of Tehran Province, Iran. Employing G*Power software, version 3.1.9.7, a sample size of 38 participants was determined, with an effect size of 0.8, an α level of 0.05, and a power of 80%. These participants were subsequently divided into two groups, consisting of 15 individuals in the control group and 15 individuals in the training group, as per the specified assumptions, even accounting for potential sample attrition.
The inclusion criteria included male gender, age falling within the 18 to 30-year range, engagement in a minimum of three weekly bodybuilding sessions involving the utilization of machines and weights, the absence of discernible abnormalities in the upper and lower extremities, the absence of musculoskeletal injuries in any bodily organs and functional movement score below 14. The exclusion criteria included subjects expressing dissatisfaction and a reluctance to continue with the research procedures, failure to participate in two consecutive sessions or three alternating sessions of exercises, the onset of pain or discomfort during exercise protocols, or the utilization of alternative treatment methods, such as physiotherapy.
The athletes’ movement patterns were evaluated using the 9+ test. The 9+ assessment includes 10 distinct movement tests specifically designed to detect any limitations or deviations from typical movement patterns. These tests are meticulously crafted to assess the intricate interplay between the mobility of the movement chain and the requisite stability essential to execute functional and fundamental movement patterns. In the context of the 9+ test, a score of 3 is assigned when the tests are executed correctly without any compensatory movements. A score of 2 is awarded if the movement is performed with compensatory movements, while a score of 1 is allotted when an individual is unable to execute the movement without resorting to compensatory actions. The series of tests include assessments for the deep squat, hurdle step, lunge, shoulder mobility, straight leg raising, push-up, one leg squat, seated trunk rotation, straight leg raises test, and rotational stability [30, 31] (Figures 1-10).







The participants were stratified into two distinct groups, an experimental group and a control group. All participants, belonging to both groups, convened at the Jahan-Ara Sports Club at predetermined intervals and completed assessments about the functional screening test, following a 5-minute warm-up period. Subsequently, individuals with a 9+ score below 14 were identified and assigned to either the experimental or control group. Those allocated to the experimental group engaged in an eight-week protocol of functional exercises, involving three sessions per week, each spanning 40 minutes.
The primary objective of each corrective exercise is to systematically enhance the capacity to execute various movement patterns while simultaneously refining form and control. Corrective exercises are strategically structured to target discrete elements of the exercises, breaking them down into more granular components of movement patterns. In the initial six weeks, the exercises are meticulously tailored to address specific functional movement patterns (Table 1).

These exercises primarily aim to enhance either stability or mobility. Conversely, during weeks 7 and 8, a set of exercises is introduced that simultaneously challenges both mobility and stability (Table 2), incorporating integral components of movement patterns. The overarching aim throughout this progression is to continually refine and optimize these patterns [27].

The training programs comprised three sessions lasting 45 minutes each for eight weeks. It is noteworthy that the exercise protocol’s volume and intensity were meticulously tailored by the frequency, intensity, time, and type (FITT) principles.
Upon the conclusion of the 8-week corrective exercise intervention, each participant underwent a re-evaluation using the functional movement pattern. Subsequently, the participants were assessed through a comparative analysis of the initial and post-intervention evaluations to ascertain the changes in scores.
Figure 11 shows a selection of functional exercises associated with movement impairment patterns.
Subsequently, following the compilation of research data, the normality of the data was assessed using the Shapiro-Wilk test. Intragroup comparisons were conducted utilizing the paired t-test, while intergroup comparisons were performed employing the analysis of covariance (ANCOVA) test, all at a significance level of 95%, utilizing SPSS software, version 22.
Results
Table 3 presents the anthropometric characteristics of the research subjects, categorized by age, height, weight, and body mass index (BMI).
The analysis employed in this study involved the use of a paired t-test to evaluate intragroup differences and covariance analysis to assess intergroup differences, as outlined in Table 4. The findings from the paired t-test revealed a significant discrepancy between the pre-test and post-test scores (P<0.05) in all 9+ tests, except the shoulder mobility test (P=0.85), specifically within the experimental group. Furthermore, the results derived from the ANCOVA test demonstrated a substantial differentiation between the experimental and control groups across all 9+ tests, except the shoulder mobility test (P=0.22) (P<0.05). Remarkably, the experimental group exhibited superior scores in all 9+ test variables, excluding the shoulder mobility test, compared to the control group following an 8-week corrective exercise protocol.

Discussion
The results of the paired t-test analysis in this study demonstrated a notable divergence. Specifically, in all 9+ tests, except for the shoulder mobility assessment, a significant disparity between the pre-test and post-test scores was exclusively observed in the experimental group (P<0.05). Additionally, the outcomes derived from the ANCOVA test unveiled a substantial distinction between the two groups, namely the experimental and control groups, across all 9+ tests, except for the shoulder mobility evaluation (P<0.05). In summary, across all variables assessed in the 9+ test, the experimental group exhibited superior scores compared to the control group after 8 weeks of corrective exercises.
The results of this current study are consistent with the research outcomes reported by Chen et al. [32], Boucher et al. [27], Jafari et al. [33], Woods et al. [34], Soltandoost et al. [35], Siamaki et al. [36], and Butcher et al. [27].
Given the scarcity of research about the implementation of corrective exercises in the bodybuilding community, this section endeavors to utilize the most relevant studies available on this subject.
Boucher et al. in their study investigated the impact of a four-week corrective exercise protocol on FMS test scores among high school girls. Their results indicated a significant increase in the FMS test score in the post-test (17.29) compared to the pre-test (14.43) [27]. The resemblance in training protocols between Boucher’s research and the present study contributes to the alignment of the two investigations.
Jafari et al. [33] similarly explored the impact of corrective exercises on FMS test scores among firefighters. Their results indicated that the FMS test score for the experimental group increased significantly, rising from a mean of 10 in the pre-test to 17 in the post-test. The resemblance between the two studies can be attributed to similarities in their training protocols and the inclusion of exercises involving movements, such as single-leg balance, single-leg deadlift, mountaineer, and squat, among others.
Leaderman’s definition of functional movements encompasses a distinct repertoire of movements tailored to each individual. Within this collection of movements, there are those essential for daily activities like eating, cleaning, and walking, categorized as general skills. Additionally, another subset of movements known as special skills exists, encompassing both unique and potentially shared activities, such as sports and occupational tasks (Figures 2, 3, 4, 5 and 6). What may constitute a functional set for one individual can entail playing tennis, while for another, it may involve practicing yoga poses. When an individual acquires a new movement or skill, it becomes an addition to their repertoire of movements. Movements falling outside an individual’s typical range are deemed as extra-functional. In Leatherman’s work on neuromuscular rehabilitation, rehabilitation is characterized as a process aimed at enhancing an individual’s movement capacity by leveraging their existing set of movements. According to this definition, when rehabilitating and enhancing the capabilities of someone who plays tennis, the set of functional tennis movements should be employed. Conversely, movement patterns utilized in therapy and rehabilitation that do not belong to the individual’s functional set (i.e. are extra-functional) are likely to yield diminished effects. For instance, a rehabilitation program centered around a set of soccer movements would be less effective and less pertinent for an injured tennis player [37].
In the context of neuromuscular rehabilitation, Leatherman outlines a set of codes governing the rehabilitation program and the requisite neuromuscular adaptations to attain the intended outcome [37]. These codes encompass elements, such as cognition, being active, feedback, repetition, and similarity in practical application.
Hence, for effective recovery and rehabilitation, an individual must possess cognitive awareness of their actions (cognitive) and the objectives of the recovery process, engaging actively in its pursuit (being active). The correction of movements necessitates internal sensory feedback or guidance (feedback), and the task should be repetitively practiced at various intervals (repetition). Moreover, rehabilitation exercises should closely resemble the goal of rehabilitation and the intended task (similarity). By incorporating these adaptation codes into the training protocol, motor control rehabilitation and enhancement become readily achievable [37]. According to the principle of similarity, most exercises chosen to rectify existing deficiencies mirror the targeted tasks. Therefore, as per Lederman’s assertions, the likelihood of improving these deficits and increasing performance test scores appears promising.
The shoulder mobility test assesses the unilateral and reciprocal range of motion in the shoulder joint, encompassing internal rotation and adduction in one shoulder and external rotation and abduction in the other. Successful performance in this evaluation necessitates the proper mobility of the scapula and extension of the spine. Inadequate performance on this test may be attributed to various factors, including an imbalance in the range of motion between external and internal rotation within a shoulder joint. Specifically, the shortening of the pectoralis minor and latissimus dorsi muscles can lead to postural alterations, such as forward head posture and rounded shoulders in athletes. Given the emphasis placed by bodybuilders on increasing chest and back muscle volume, the shortening of these muscles can result in a reduction in the range of motion for internal and external shoulder rotation. Consequently, engaging in exercises involving lying on one’s side while extending the arm and rotating the trunk, lying on the side with shoulder movements, and lying on the side while elevating the arm and rotating the trunk likely contributed to the amelioration of this diminished range of motion. As a result, the shoulder mobility test scores likely improved in the post-test.
The stability push-up test assesses the ability of the trunk and spine to maintain stability in both anterior and posterior planes during closed motor chain activities involving the upper limbs. This evaluation specifically focuses on the trunk’s stability in the sagittal plane. Symmetry in upper limb movements, particularly during activities like push-ups, is a key consideration in this test. The significance of this assessment lies in the fact that adequate trunk stability is essential in sports activities to optimize movement efficiency. Inadequate stability can result in the wastage of energy during physical exertion, ultimately leading to diminished functional movements and an increased risk of microtrauma and injury. The improvement in scores observed in the post-test for this evaluation can likely be attributed to the inclusion of specific exercises in the training protocol. These exercises, such as kneeling exercises in a linear fashion coupled with proprioceptive neuromuscular facilitation (PNF) techniques, and resistance band exercises designed to challenge the central stability region, along with the push-up hand walkout and return to a standing position, likely contributed to enhancing performance in the stability push-up test.
The deep squat test necessitates high coordination and mobility involving multiple anatomical structures, including organs, muscles, and the central stability system. It also places a demand on overall body mechanics and neurovascular control. Moreover, it evaluates the mobility and stability of the shoulder, scapula, and thoracic region of the spine [38, 39]. Poor performance in the deep squat test can typically be attributed to three primary factors:
1. Constraints in upper limb mobility and glenohumeral joint weakness.
2. Limitations in lower limb mobility.
3. Impairments in motor control in the central stability region [39].
In the huddle step test, the mobility of the front foot and the stability of the back foot carry significant weight. Insufficient mobility in the stepping foot and inadequate stability in the stance foot can lead to reduced scores in this particular evaluation [39]. When it comes to the lunge test, diminished 9+ scores are often associated with restrictions in the thoracic spine area and decreased mobility in the hip, knee, and ankle joints.
Engaging in a protocol of specific exercises, such as lying on one’s side while simultaneously turning away and raising the arms and shoulders, along with trunk rotation, has the potential to enhance upper limb mobility. Likewise, performing thigh-bending exercises during the single-leg deadlift movement while pulling the hands forward, executing the “climbing the mountain” maneuver, and adopting the “flying dog” position while raising the opposite arm and leg in synchrony, as well as doing the same “flying dog” pose with the additional element of extending the opposite arm and leg against elastic resistance, likely contributes to improved motor control within the central stability region. This multifaceted approach may result in increased scores in the deep squat test during the post-test assessment. Furthermore, incorporating exercises, such as half-knee lunges while simultaneously raising the opposite hand, engaging in a line-kneeling stance while throwing a ball toward a partner, and assuming a kneeling position while performing PNF exercises by pulling against resistance from a rubber band are practices that may address identified weaknesses. The amelioration of these identified deficiencies represents a plausible rationale for the observed improvements in Lange test scores following the exercise intervention.
The push-up test underscores the significance of trunk stability, upper limb strength, and central region stability [39]. Engaging in exercises, such as the flying dog pose while extending the opposite arm and leg against the resistance provided by a rubber band, executing kneeling exercises in a row while throwing a ball towards a partner, practicing kneeling in a row with PNF exercises, and pulling a resistance rubber band against resistance all contribute to the potential rectification of these shortcomings and the subsequent elevation of scores in the post-test.
Conversely, the rotary stability test emphasizes neuromuscular coordination and energy transference throughout the body, both from upper to lower limbs and vice versa. It also assesses trunk stability across multiple planes. Weaknesses in overall body stability, challenges with scapula and hip stability, as well as limitations in knee, thigh, and trunk mobility, are recognized as factors contributing to lower scores in this particular test [39]. It is plausible that engaging in the aforementioned exercises has served to address these deficiencies, resulting in improved scores in the post-test.
Conclusion
Based on the research results, an 8-week program focusing on “functional impairment” in athletes engaged in “resistance training” and exhibiting movement impairments can result in significant enhancements in their movement patterns. Consequently, it is recommended that coaches consider implementing these exercises to ameliorate the movement patterns of “resistance training” athletes.
Limitation
One of the limitations of the current research is the small number of research subjects.
Suggestions
It is suggested to investigate the effect of functional exercises in the current research on female athletes and with a larger number of subjects.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research has not received any grant from any organization.
Authors' contributions
Conceptualization and data collection: Behnam Shahbandi; Study design: All authors; Data interpretation: Mohammad Kalantariyan.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors extend their gratitude to all the coaches, officials, and athletes who contributed to the successful execution of this research project.
References
- McEvoy MP, Grimmer K. Reliability of upright posture measurements in primary school children. BMC Musculoskeletal Disorders. 2005; 6:35. [DOI:10.1186/1471-2474-6-35] [PMID] [PMCID]
- Claeys K, Brumagne S, Deklerck J, Vanderhaeghen J, Dankaerts W. Sagittal evaluation of usual standing and sitting spinal posture. Journal of Bodywork and Movement Therapies. 2016; 20(2):326-33. [DOI:10.1016/j.jbmt.2015.10.002] [PMID]
- Kratenová J, Zejglicová K, Malý M, Filipová V. Prevalence and risk factors of poor posture in school children in the Czech Republic. The Journal of School Health. 2007; 77(3):131-7. [DOI:10.1111/j.1746-1561.2007.00182.x] [PMID]
- Mitchell UH, Johnson AW, Vehrs PR, Feland JB, Hilton SC. Performance on the functional movement screen in older active adults. Journal of Sport and Health Science. 2016; 5(1):119-25. [DOI:10.1016/j.jshs.2015.04.006] [PMID] [PMCID]
- Guimond S, Massrieh W. Intricate correlation between body posture, personality trait and incidence of body pain: A cross-referential study report. Plos One. 2012; 7(5):e37450. [DOI:10.1371/journal.pone.0037450] [PMID] [PMCID]
- Sedrez JA, da Rosa MI, Noll M, Medeiros Fda S, Candotti CT. [Risk factors associated with structural postural changes in the spinal column of children and adolescents (Portuguese)]. Revista Paulista de Pediatria. 2015; 33(1):72-81. [DOI:10.1016/S2359-3482(15)30033-6] [PMID] [PMCID]
- Çelenay ŞT, Kaya DÖ, Özüdoğru A. Spinal postural training: Comparison of the postural and mobility effects of electrotherapy, exercise, biofeedback trainer in addition to postural education in university students. Journal of Back and Musculoskeletal Rehabilitation. 2015; 28(1):135-44. [DOI:10.3233/BMR-140501] [PMID]
- Page P, Frank C, Lardner R. Assessment and treatment of muscle imbalance: The Janda approach. Champaign: Human Kinetics; 2010. [Link]
- Engebretsen L, Soligard T, Steffen K, Alonso JM, Aubry M, Budgett R, et al. Sports injuries and illnesses during the London Summer Olympic Games 2012. British Journal of Sports Medicine. 2013; 47(7):407-14. [DOI:10.1136/bjsports-2013-092380] [PMID]
- Jahani Golbar S, Gharakhanlou R, Barmaki S, Khazani A, Khorshidi-Hosseini M. A comparison of age average of iranian medal winners in olympic and Asian games to their counterparts from selected countries. Annals of Applied Sport Science. 2015; 3(4):69-75. [DOI:10.18869/acadpub.aassjournal.3.4.69]
- van Mechelen W, Hlobil H, Kemper HC. Incidence, severity, aetiology and prevention of sports injuries. A review of concepts. Sports Medicine. 1992; 14(2):82-99. [DOI:10.2165/00007256-199214020-00002] [PMID]
- Sanders B, Blackburn TA, Boucher B. Preparticipation screening - the sports physical therapy perspective. International Journal of Sports Physical Therapy. 2013; 8(2):180-93. [PMID] [PMCID]
- Padua DA, DiStefano LJ, Beutler AI, de la Motte SJ, DiStefano MJ, Marshall SW. The landing error scoring system as a screening tool for an anterior cruciate ligament injury-prevention program in elite-youth soccer athletes. Journal of Athletic Training. 2015; 50(6):589-95. [DOI:10.4085/1062-6050-50.1.10] [PMID] [PMCID]
- Garrison M, Westrick R, Johnson MR, Benenson J. Association between the functional movement screen and injury development in college athletes. International Journal of Sports Physical Therapy. 2015; 10(1):21-8. [PMID] [PMCID]
- Bardenett SM, Micca JJ, DeNoyelles JT, Miller SD, Jenk DT, Brooks GS. Functional movement screen normative values and validity in high school athletes: Can the fms™ be used as a predictor of injury? International Journal of Sports Physical Therapy. 2015; 10(3):303-8. [PMID] [PMCID]
- Cook G, Burton L, Hoogenboom BJ, Voight M. Functional movement screening: the use of fundamental movements as an assessment of function - part 1. International Journal of Sports Physical Therapy. 2014; 9(3):396-409. [PMID] [PMCID]
- Cook G, Burton L, Hoogenboom BJ, Voight M. Functional movement screening: the use of fundamental movements as an assessment of function-part 2. International Journal of Sports Physical Therapy. 2014; 9(4):549-63. [PMID] [PMCID]
- Smith HC, Johnson RJ, Shultz SJ, Tourville T, Holterman LA, Slauterbeck J, et al. A prospective evaluation of the Landing Error Scoring System (LESS) as a screening tool for anterior cruciate ligament injury risk. The American Journal of Sports Medicine. 2012; 40(3):521-6. [DOI:10.1177/0363546511429776] [PMID] [PMCID]
- Plisky PJ, Rauh MJ, Kaminski TW, Underwood FB. Star excursion balance test as a predictor of lower extremity injury in high school basketball players. The Journal of Orthopaedic and Sports Physical Therapy. 2006; 36(12):911-9. [DOI:10.2519/jospt.2006.2244] [PMID]
- McGuine TA, Greene JJ, Best T, Leverson G. Balance as a predictor of ankle injuries in high school basketball players. Clinical Journal of Sport Medicine. 2000; 10(4):239-44. [DOI:10.1097/00042752-200010000-00003] [PMID]
- Larsen JB, Farup J, Lind M, Dalgas U. Muscle strength and functional performance is markedly impaired at the recommended time point for sport return after anterior cruciate ligament reconstruction in recreational athletes. Human Movement Science. 2015; 39:73-87. [DOI:10.1016/j.humov.2014.10.008] [PMID]
- Linens SW, Ross SE, Arnold BL, Gayle R, Pidcoe P. Postural-stability tests that identify individuals with chronic ankle instability. Journal of Athletic Training. 2014; 49(1):15-23. [DOI:10.4085/1062-6050-48.6.09] [PMID] [PMCID]
- Failla M, Zarzycki R, Logerstedt D, Wellsandt E, Axe MJ, Snyder-Mackler L. Hop test symmetry scores early after Rehab predict successful 2 year outcomes of ACLR.Orthopaedic Journal of Sports Medicine. 2017; 5(7 suppl6):2325967117S00325. [DOI:10.1177/2325967117S00325] [PMCID]
- Hoog P, Warren M, Smith CA, Chimera NJ. Functional hop tests and tuck jump assessment scores between female division i collegiate athletes participating in high versus low acl injury prone sports: A cross sectional analysis. Int J Sports Phys Ther. 2016; 11(6):945-53. [PMID] [PMCID]
- Dossa K, Cashman G, Howitt S, West B, Murray N. Can injury in major junior hockey players be predicted by a pre-season functional movement screen - A prospective cohort study. The Journal of the Canadian Chiropractic Association. 2014; 58(4):421-7. [PMID] [PMCID]
- Campa F, Spiga F, Toselli S. The Effect of a 20-Week Corrective Exercise Program on Functional Movement Patterns in Youth Elite Male Soccer Players. Journal of Sport Rehabilitation. 2019; 28(7):746-51. [DOI:10.1123/jsr.2018-0039] [PMID]
- Boucher B, Rich A, Gobert D, Gardner B, Metzner P, King C, et al. The Effectiveness of a functional movement assessment and 4-week exercise training program for female high school athletes. Journal of Strength and Conditioning Research. 2021; 35(1):102-10. [DOI:10.1519/JSC.0000000000002549] [PMID]
- Liao T, Li L, Wang YT. Effects of functional strength training program on movement quality and fitness performance among girls aged 12-13 years. Journal of Strength and Conditioning Research. 2019; 33(6):1534-41. [DOI:10.1519/JSC.0000000000002190] [PMID]
- Cowen VS. Functional fitness improvements after a worksite-based yoga initiative. Journal of Bodywork and Movement Therapies. 2010; 14(1):50-4. [DOI:10.1016/j.jbmt.2009.02.006] [PMID]
- Kiesel K, Plisky PJ, Voight ML. Can serious injury in professional football be predicted by a preseason functional movement screen? North American Journal of Sports Physical Therapy. 2007; 2(3):147-58. [PMID] [PMCID]
- Budnar Jr RG, Birdwell R, Moody C, Hill DW, Duplanty AA, Jackson AW, et al. Functional Movement Screentm Scores in Collegiate Track and Field Athletes in Relation to Injury Risk and Performance. International Journal of Exercise Science. 2013; 2(5):68. [Link]
- Chen J, Zhang C, Chen S, Zhao Y. Effects of functional correction training on injury risk of athletes: A systematic review and meta-analysis. PeerJ. 2021; 9:e11089. [DOI:10.7717/peerj.11089] [PMID] [PMCID]
- Jafari M, Zolaktaf V, Ghasemi G. Functional movement screen composite scores in firefighters: Effects of corrective exercise training. Journal of Sport Rehabilitation. 2020; 29(1):102-6. [PMID]
- Woods CT, McKeown I, Keogh J, Robertson S. The association between fundamental athletic movements and physical fitness in elite junior Australian footballers. Journal of Sports Sciences. 2018; 36(4):445-50. [DOI:10.1080/02640414.2017.1313996] [PMID]
- Soltandoost SM, Alizadeh MH, Shamsoddini A. Effects of functional movement training program on functional movement screening scores and selected physical fitness factors in active injury-prone military men. Journal of Military Medicine, 2020. 22(4):174-82. [Link]
- Siamaki R, Minoonejad H, Alizadeh MH, Soori R. [Are fundamental functional patterns affected by functional training in youth male soccer players (Persian)]? Journal of Research in Rehabilitation Sciences. 2017; 13(1):7-13. [DOI:10.22122/JRRS.V13I1.2838]
- Lederman E. Neuromuscular rehabilitation: Summary. In: Lederman E, editor. Neuromuscular rehabilitation in manual and physical therapy. Amsterdam: Elsevier Health Sciences; 2010. [DOI:10.1016/B978-0-443-06969-7.00014-0]
- Knapik JJ, Cosio-Lima LM, Reynolds KL, Shumway RS. Efficacy of functional movement screening for predicting injuries in coast guard cadets. Journal of Strength and Conditioning Research. 2015; 29(5):1157-62. [DOI:10.1519/JSC.0000000000000704] [PMID]
- Cook G, Burton L, Hoogenboom B. Pre-participation screening: The use of fundamental movements as an assessment of function - part 1. North American Journal of Sports Physical Therapy. 2006; 1(2):62-72. [PMID] [PMCID]
Type of Study: Applicable |
Subject:
Special
Received: 2023/09/20 | Accepted: 2024/05/5 | Published: 2024/07/1
Received: 2023/09/20 | Accepted: 2024/05/5 | Published: 2024/07/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






