Fri, Dec 19, 2025
Volume 14, Issue 1 (Winter 2024)
PTJ 2024, 14(1): 65-72 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Asgarpoor A, Yalfani A. The Effect of Cognitive Functional Therapy on Psychological Variables in Women With Non-specific Chronic Back Pain: A Randomized Control Trial. PTJ 2024; 14 (1) :65-72
URL: http://ptj.uswr.ac.ir/article-1-595-en.html
URL: http://ptj.uswr.ac.ir/article-1-595-en.html
1- Department of Pathology and Sport Biomechanics, Faculty of Sport Sciences, Bu-Ali Sina University, Hamedan, Iran.
Full-Text [PDF 510 kb]
(1245 Downloads)
| Abstract (HTML) (4552 Views)
Full-Text: (1025 Views)
Introduction
Chronic low back pain (CLBP) is one of the vital medical conditions worldwide in terms of reduced quality of life, disability, and increased social and economic costs [1]. The prevalence rate of CLBP has been reported by 84%, twice more common in women than in men [2]. The healthcare cost of LBP is estimated to be £14 billion in the United Kingdom and $14.5 billion in the United States [3]. LBP is grouped into non-specific and mechanical types [4]. Chronic non-specific back pain (CNSLBP) accounts for 90%-95% of the cases, affecting 20% of the world’s population [5].
According to conducted research, the prevalence of CNSLBP continues to rise [6] because most existing interventions were developed based on a biomedical model focusing on the structure or pathology, and do not target an individualized treatment approach for each case of chronic low back pain [7] while LBP is commonly believed to be partly caused by biomechanical reasons. Compelling evidence suggests that LBP is associated with a complex interplay of cognitive [8], physical [9], psychological [10], neurophysiological [10], lifestyle factors [11], and social factors [12].
Recently, there has been an increased focus among researchers on the neurological and cognitive aspects of LBP. Studies have uncovered the significant role played by psychological factors, such as Kinesiophobia and the perceived intensity of pain, in exacerbating LBP [13]. According to the fear-avoidance model, painful experiences instill fear of movement or reinjury in individuals, often resulting in avoidance behavior and prolonged immobility, along with feelings of depression and increased disability [14]. Over time, a protective adaptation to pain occurs through motor learning, wherein new motor programs in the motor cortex replace natural movements. As a result, this pain response leads to an intensified experience of pain, increased fear of movement, and heightened focus and attention on painful movements [15]. Consequently, identifying the psychological factors contributing to the persistence of chronic pain in patients with CNSLBP can be a valuable complement to therapeutic interventions in the fields of sports rehabilitation, physiotherapy, and physical medicine [13]. As a result, treatment approaches for CNSLBP have undergone a significant shift away from purely biomedical models and towards biopsychosocial models.
An alternative approach gaining increasing attention in the management of CLBP is cognitive functional therapy (CFT) [16]. CFT consists of multidimensional and personalized exercises that not only emphasize motor control but also consider psychological factors as integral components of the exercises [17]. CFT aims to change the patient’s beliefs, and the ability to cope with fear, teach pain mechanisms, and increase control of their body’s flexibility. Individuals are trained to reduce the overactivity of the trunk muscles and make behavioral changes related to pain in provocative postures and movements [18]. Clinical trials using CFT have shown promising results [16-18]. For example, in a randomized controlled clinical trial (RCT) conducted by Vibe Fersum et al. involving individuals with chronic low back pain, CFT demonstrated superior outcomes in terms of pain reduction and disability compared to manual therapy [19]. Additionally, another study revealed that CFT led to a reduction in pain intensity and disability during 3, 6, and 12-month follow-ups in people with chronic back pain [18].
Despite these promising initial findings, the body of research on interventions targeting psychological factors in individuals with chronic musculoskeletal pain remains limited [18, 20], and many questions remain, including the mechanisms of the effectiveness of these exercises in pain reduction and the design of therapeutic protocols. Therefore, it is necessary to conduct high-quality clinical trials to assess the effectiveness of CFT interventions commonly employed in clinical practice. Therefore, RCT was conducted to determine whether CFT is effective for CLBP. We hypothesized that CFT would lead to reduced pain, disability, and fear of movement.
Materials and Methods
Study design
This double-blind RCT (evaluators/patients) was planned with a pre- post-test design [21]. The statistical population included 40 women with CNSLBP who were recruited from orthopedic or sports medicine clinics in Hamedan Province, Iran. In this clinical trial, patients were randomly assigned into two experimental (n=20) and control groups (n=20). The experimental group followed CFT for 8 weeks and the control group received no intervention [22].
Sample size
We used G*Power software, to determine the sample size. According to the previous study, the power was 0.8, the α was 0.5, and the effect size was 0.8. The software output reported 40 subjects for this clinical trial.
Recruitment and participants
The statistical population of this clinical trial was women with CNSLBP. Patients were recruited from orthopedic and sports medicine clinics of Hamedan Province. An orthopedic surgeon evaluates patients before recruitment. Thirty women with CNSLBP were recruited for clinical trials based on the diagnosis of the spine orthopedic physician. The inclusion criteria included visual analog scale ≥3, Oswestry disability index ≥25, and Kinesiophobia >18, no history of spine surgery, and age range between 30-60 years. The exclusion criteria included pain in other segments of the body, lower and upper limb deformity, history of spine surgery, use of painkillers in the past 6 months, physical therapy in the past year, participation in sports, sciatica pain, spondylolysis, neuromuscular disorders, neurological, respiratory, muscle spasm, and vertebral fracture.
Randomization and blinding
Random allocation software, version 1.0 was used for randomization. Random codes were generated in blocks 4 and 6. We used sequentially numbered sealed envelopes to conceal allocation. A researcher who was not involved in data collection opened the sealed envelopes with consecutive numbers and delivered them to the patients. As a result, patients were randomly assigned to experimental (n=20) and control (n=20) groups. Patients were not aware of group allocation. In addition, to maintain blinding, patients were instructed not to disclose information about the group allocation to the evaluators.
Intervention
Experimental intervention: Cognitive-functional therapy (CFT)
This protocol has three main components that were chosen based on the study of O’Keefe et al. [18]. The first CFT session was approximately 60 minutes, and the 8-week individual follow-up was approximately based on individual characteristics from 30 to 45 minutes and for 18 sessions. The intervention was performed by another physiotherapist trained in CFT treatment. In this protocol, a physical therapist with more than 5 years of experience conducted an interview and physical examination of the patients to determine their unique training programs, considering modifiable cognitive, biopsychosocial, functional, and lifestyle behavior factors.
The three components include the following:
1. The cognitive component focuses on identifying what makes pain worse during the examination. This includes a discussion of the multidimensional nature of persistent pain and individual beliefs, and how emotions and behaviors (movement and lifestyle) can reinforce the vicious cycle of pain and disability.
2. Specific exercises are designed to improve movements and posture. To perform these exercises, we ensure that the patient feels safe by being exposed to activities that are painful, feared, or avoided. This component is called exposure with ‘control’.
3. Integrating functional exercises with activities of daily living such as bending and sitting. This phase varies between individuals but should integrate new behaviors with the goal of gradual exposure to activities in daily life, reducing fear as necessary. This component is called lifestyle change.
All participants underwent a comprehensive interview and physical examination by their therapist to identify any relevant multidimensional factors considered to be key drivers of their pain and disability [18]. Treatment with CFT will be individualized. The therapist listens to the person’s story of pain and designs the therapy based on their needs. The first session involves discussing the pain and starting the treatment. The therapist asks questions and examines the person’s body to understand what may be causing the pain [18, 23, 24].
Physical examination includes examination of pain responses, analysis of functional behavior through observation, ability to change behaviors, and ability to control pain related to functional goals. The subjects’ activity levels, such as their ability to relax the trunk muscles and normalize the posture and provocative movement behavior, will also be evaluated [18, 19, 24]. Where an ineffective behavior is observed, an alternative movement strategy is implemented. This component of the treatment is called exposure with control [16]. Safe exercises with low frequency are gradually developed and turned into functional exercises with more and more complex frequency. For example, if a participant is initially unable to relax her body muscles at first, diaphragmatic breathing exercises in relaxed positions, such as lying down, sitting, and standing were recommended. If the participant could perform this stage, she would enter the next stage, where more challenging tasks were performed from the point of view of mind, relaxation, and control.
During the treatment, the therapist might ask the person to do certain exercises at home, either by watching videos or reading instructions. With practice, the person learns new ways to move and do things without causing pain.
As the therapy progresses, the person learns how to use these new techniques in their daily life. They gradually do activities they used to avoid due to fear of pain. The goal is to make them stronger and less afraid of pain.
Outcome measures
Pain
Pain was assessed with a 10 cm visual analog scale. The patient was asked to indicate the pain intensity during daily activities [25].
Disability
Oswestry disability index was used to disability evaluate (intraclass correlation coefficient [ICC]=0.84) [26]. Disability is classified in four subcategories including, a score of less than 25 as the lowest level of disability, 25-50 as moderate disability, 50-75 as severe disability, and 75-100 as acute disability [27].
Tampa scale for kinesiophobia (TSK) questionnaire
In this study, the fear of movement was assessed using the Tampa scale for kinesiophobia (TSK) questionnaire in the pre-test and post-test. The questionnaire consists of 11 statements, and participants are asked to complete each statement based on their actual results. The purpose of this questionnaire is to evaluate the fear of movement from different dimensions, such as fear of injury and avoidance of activity. The scoring spectrum is based on a four-option Likert scale, where “completely disagree” scores 1 and “completely agree” scores 4. The validity of this questionnaire has been confirmed in a study by Rahmati et al. To calculate its reliability, Cronbach’s α coefficient was used, and a Cronbach’s α of 0.82 was obtained for this questionnaire [28].
Statistical analysis
We used SPSS software, version 26 for statistical analysis. Shapiro-Wilk test was used to ensure the normal distribution of data. The equality of error variances was checked using Levene’s test. Two-way repeated measures analysis of variance (ANOVA) was used to analyze the effect of the intervention on bio-psychosocial indices (pain, disability, and Kinesiophobia variables). Partial eta squared effect size was assessed for two-way ANOVA (group×time interaction). A significance level of P<0.05 was considered. A covariance test was used for between-group comparison.
Results
Table 1 presents the demographic characteristics of the groups. The results of the Shapiro-Wilk test showed no statistically significant difference between the groups for demographic characteristics.
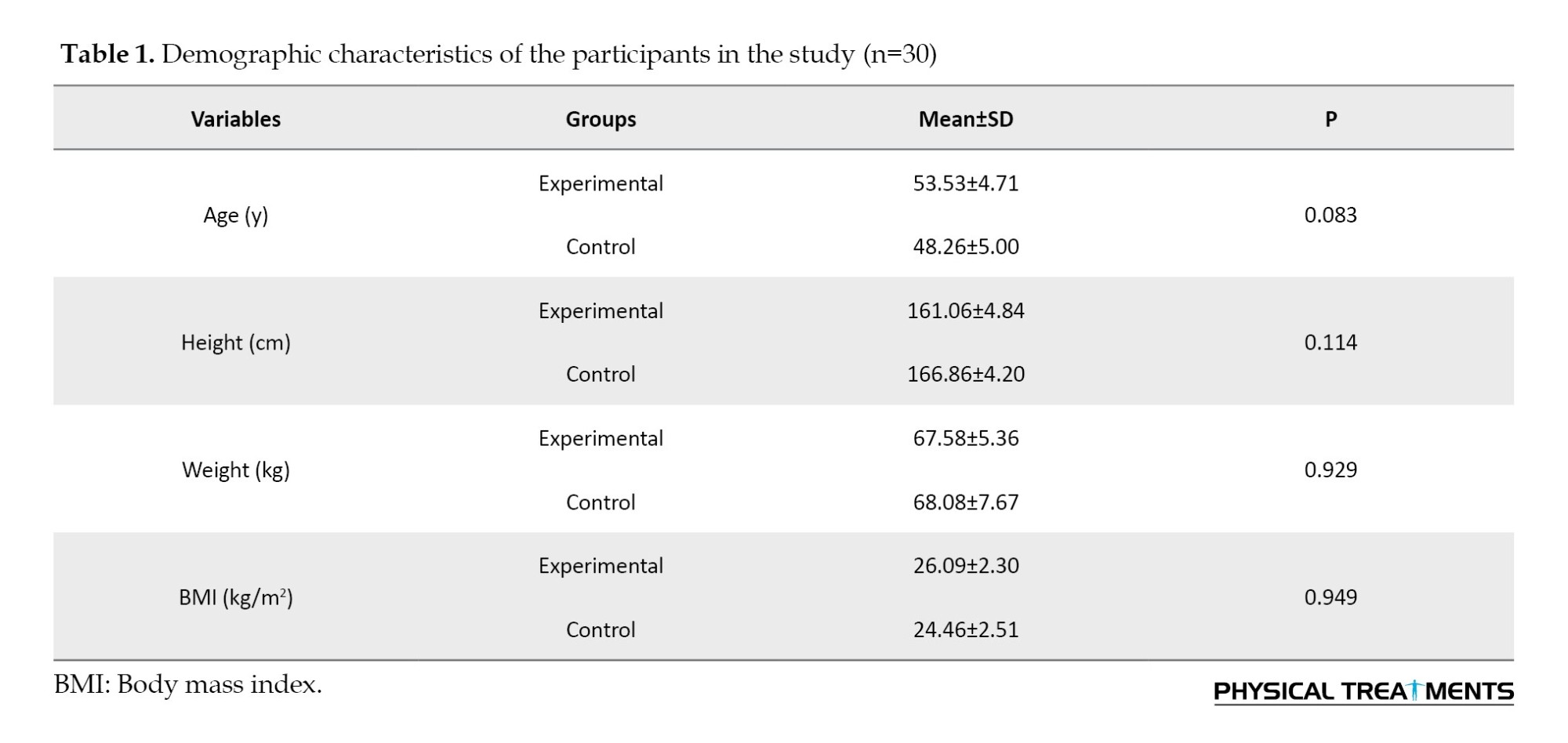
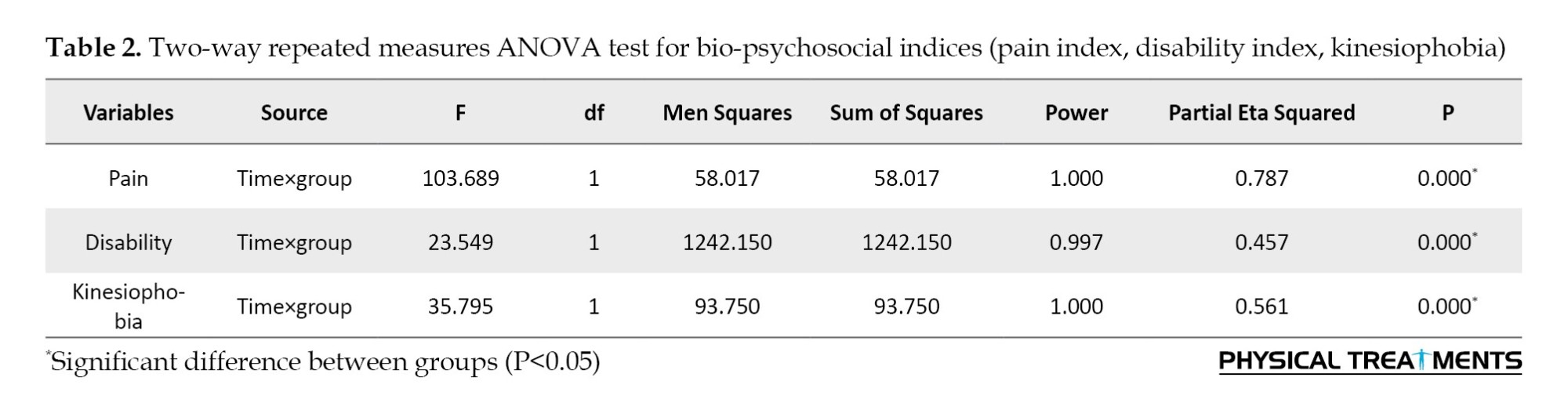
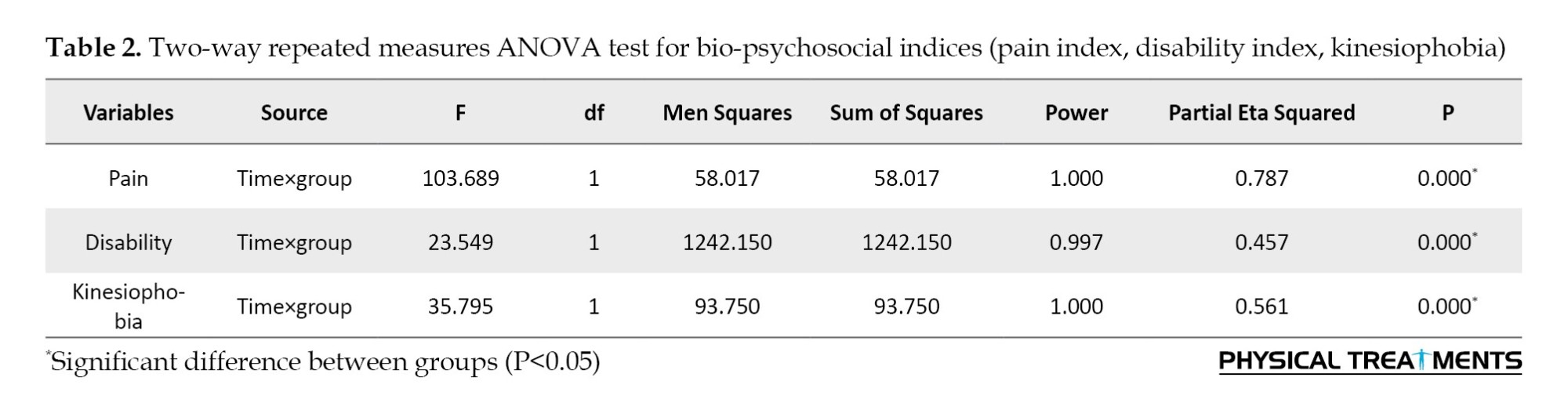
Table 2 presents the results of the two-way repeated measures ANOVA test. Two-way repeated measures ANOVA results showed that CFT intervention had a significant difference with high effect size in reducing pain (P=0.000, ƞ2=0.787), disability (P=0.000, ƞ2=0.457), and Kinesiophobia (P=0.000, ƞ2=0.561).
In Table 3, descriptive statistics showed that the experimental group had a 52% decrease in pain, 41% decrease in disability, and 12% decrease in Kinesiophobia.

Discussion
This clinical trial was conducted to evaluate the effectiveness of CFT intervention on pain, disability, and Kinesiophobia in patients with CNSLBP. The results of the research showed that CFT intervention has a significant effect in reducing pain, disability, and Kinesiophobia. Considering the close relationship between the variables of pain intensity, disability, and Kinesiophobia index and the overlap of these variables, an attempt was made to interpret the mechanism of CFT on these variables together.
O’Sullivan’s pain provocation classification system for LBP distinguishes between central and peripheral pain provocation. Central pain provocation is linked to psychological factors, such as fear of movement and depression, affecting around 30% of the LBP population. On the other hand, peripheral pain provocation stems from mechanical causes, movement impairments, and motor control issues, affecting approximately 30% of individuals with LBP [29]. Therefore, not only does the degree of injury have a role in shaping the level of functional limitation, and disability caused by chronic musculoskeletal pain, but people’s cognitions, beliefs, and thoughts also have a major impact on the disability caused by pain, therefore, functional cognitive exercises are effective on cognitive factors, and in this way, it can cause a decrease in kensiophobia and, as a result, a decrease in pain and disability in a person [30].
CFT has been used as a new method to improve the cognitive factors of people suffering from chronic low back pain, and the results have shown that these exercises have a positive and meaningful effect on cognitive factors [23]. One of the key factors in functional cognitive exercises is matching the characteristics of each person with the exercise that is specifically given to him. In CFT, the functional behavioral approach is targeted, such as a person’s awareness of her body, relaxation of contracted muscles, normalization of the wrong movement pattern, and reconstruction of a person’s mental image of her body [31].
The results of this study are consistent with those of Caneiro et al. [23], O’Keefe et al. [18], and Vibe Fersum et al. [19], all of which investigated the impact of CFT on individuals with CLBP.
In a case report by Caneiro et al., they examined changes related to kinesiophobia and disability through the implementation of functional cognitive exercises. The results demonstrated positive alterations in both kinesiophobia and disability variables. Remarkably, individuals undergoing these exercises exhibited a shift in their attitude toward pain perception and pain control within a span of six to 18 months [23]. These outcomes suggest that CFT can potentially facilitate the performance of painful and physically challenging activities, reduce central nervous system sensitivity, enhance self-confidence, and ultimately lead to a reduction in kinesiophobia, accompanied by decreased pain and disability.
Additionally, O’Keeffe et al. conducted research comparing the effects of cognitive-functional exercises and combined exercises on individuals with non-specific chronic back pain. The results showed a reduction of pain and improvement of functional disability in people with LBP [18]. Therefore, functional cognitive exercises lead to the improvement of pain and disability by changing a person’s attitude towards pain, pain control, and a person’s efficiency in daily activities [32].
In a RCT conducted by Vibe Fersum et al. involving individuals with chronic low back pain, it was observed that CFT yielded superior results in alleviating pain and reducing disability when compared to manual therapy [19]. CFT plays a crucial role in helping patients mitigate autonomic processes, such as an excessive focus on pain (e.g. kinesiophobia) and avoidance behaviors. By fostering more adaptive and healthier responses, CFT transforms the way patients engage with painful stimuli or pain-related sensations, promoting proactive responses to pain and minimizing unnecessary mental turmoil. The reduction of these processes among patients contributes to a diminished fear of movement, increased physical performance, and an overall enhancement in disability management [33].
The goal of this approach is to reconceptualize pain from a psycho-social perspective, while eliminating unhelpful beliefs, and adopting a healthy lifestyle [18].
Conclusion
By reducing fear of movement, CFT reduces pain and disability and strengthens positive beliefs. Therefore, it is suggested to use functional cognitive exercises as a complementary method in improving people with non-specific chronic back pain.
In this study, we had two limitations. First, our sample was only women. Second, no conditions were observed to evaluate long-term results. Therefore, it is recommended that researchers evaluate CFT interventions in both genders of patients with non-specific chronic low back pain and assess the long-term effects.
Ethical Considerations
Compliance with ethical guidelines
This study has been approved by the Ethics Committee of Bu-Ali Sina University (Code: IR.BASU.REC.1401.026) and the Clinical Trials System of Iran IRCT (Code: IRCT20230430058033N1). Patients provided their informed consent before any collection and the Helsinki declaration of 2008 was followed.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank all patients for participating in this clinical trial.
References
Chronic low back pain (CLBP) is one of the vital medical conditions worldwide in terms of reduced quality of life, disability, and increased social and economic costs [1]. The prevalence rate of CLBP has been reported by 84%, twice more common in women than in men [2]. The healthcare cost of LBP is estimated to be £14 billion in the United Kingdom and $14.5 billion in the United States [3]. LBP is grouped into non-specific and mechanical types [4]. Chronic non-specific back pain (CNSLBP) accounts for 90%-95% of the cases, affecting 20% of the world’s population [5].
According to conducted research, the prevalence of CNSLBP continues to rise [6] because most existing interventions were developed based on a biomedical model focusing on the structure or pathology, and do not target an individualized treatment approach for each case of chronic low back pain [7] while LBP is commonly believed to be partly caused by biomechanical reasons. Compelling evidence suggests that LBP is associated with a complex interplay of cognitive [8], physical [9], psychological [10], neurophysiological [10], lifestyle factors [11], and social factors [12].
Recently, there has been an increased focus among researchers on the neurological and cognitive aspects of LBP. Studies have uncovered the significant role played by psychological factors, such as Kinesiophobia and the perceived intensity of pain, in exacerbating LBP [13]. According to the fear-avoidance model, painful experiences instill fear of movement or reinjury in individuals, often resulting in avoidance behavior and prolonged immobility, along with feelings of depression and increased disability [14]. Over time, a protective adaptation to pain occurs through motor learning, wherein new motor programs in the motor cortex replace natural movements. As a result, this pain response leads to an intensified experience of pain, increased fear of movement, and heightened focus and attention on painful movements [15]. Consequently, identifying the psychological factors contributing to the persistence of chronic pain in patients with CNSLBP can be a valuable complement to therapeutic interventions in the fields of sports rehabilitation, physiotherapy, and physical medicine [13]. As a result, treatment approaches for CNSLBP have undergone a significant shift away from purely biomedical models and towards biopsychosocial models.
An alternative approach gaining increasing attention in the management of CLBP is cognitive functional therapy (CFT) [16]. CFT consists of multidimensional and personalized exercises that not only emphasize motor control but also consider psychological factors as integral components of the exercises [17]. CFT aims to change the patient’s beliefs, and the ability to cope with fear, teach pain mechanisms, and increase control of their body’s flexibility. Individuals are trained to reduce the overactivity of the trunk muscles and make behavioral changes related to pain in provocative postures and movements [18]. Clinical trials using CFT have shown promising results [16-18]. For example, in a randomized controlled clinical trial (RCT) conducted by Vibe Fersum et al. involving individuals with chronic low back pain, CFT demonstrated superior outcomes in terms of pain reduction and disability compared to manual therapy [19]. Additionally, another study revealed that CFT led to a reduction in pain intensity and disability during 3, 6, and 12-month follow-ups in people with chronic back pain [18].
Despite these promising initial findings, the body of research on interventions targeting psychological factors in individuals with chronic musculoskeletal pain remains limited [18, 20], and many questions remain, including the mechanisms of the effectiveness of these exercises in pain reduction and the design of therapeutic protocols. Therefore, it is necessary to conduct high-quality clinical trials to assess the effectiveness of CFT interventions commonly employed in clinical practice. Therefore, RCT was conducted to determine whether CFT is effective for CLBP. We hypothesized that CFT would lead to reduced pain, disability, and fear of movement.
Materials and Methods
Study design
This double-blind RCT (evaluators/patients) was planned with a pre- post-test design [21]. The statistical population included 40 women with CNSLBP who were recruited from orthopedic or sports medicine clinics in Hamedan Province, Iran. In this clinical trial, patients were randomly assigned into two experimental (n=20) and control groups (n=20). The experimental group followed CFT for 8 weeks and the control group received no intervention [22].
Sample size
We used G*Power software, to determine the sample size. According to the previous study, the power was 0.8, the α was 0.5, and the effect size was 0.8. The software output reported 40 subjects for this clinical trial.
Recruitment and participants
The statistical population of this clinical trial was women with CNSLBP. Patients were recruited from orthopedic and sports medicine clinics of Hamedan Province. An orthopedic surgeon evaluates patients before recruitment. Thirty women with CNSLBP were recruited for clinical trials based on the diagnosis of the spine orthopedic physician. The inclusion criteria included visual analog scale ≥3, Oswestry disability index ≥25, and Kinesiophobia >18, no history of spine surgery, and age range between 30-60 years. The exclusion criteria included pain in other segments of the body, lower and upper limb deformity, history of spine surgery, use of painkillers in the past 6 months, physical therapy in the past year, participation in sports, sciatica pain, spondylolysis, neuromuscular disorders, neurological, respiratory, muscle spasm, and vertebral fracture.
Randomization and blinding
Random allocation software, version 1.0 was used for randomization. Random codes were generated in blocks 4 and 6. We used sequentially numbered sealed envelopes to conceal allocation. A researcher who was not involved in data collection opened the sealed envelopes with consecutive numbers and delivered them to the patients. As a result, patients were randomly assigned to experimental (n=20) and control (n=20) groups. Patients were not aware of group allocation. In addition, to maintain blinding, patients were instructed not to disclose information about the group allocation to the evaluators.
Intervention
Experimental intervention: Cognitive-functional therapy (CFT)
This protocol has three main components that were chosen based on the study of O’Keefe et al. [18]. The first CFT session was approximately 60 minutes, and the 8-week individual follow-up was approximately based on individual characteristics from 30 to 45 minutes and for 18 sessions. The intervention was performed by another physiotherapist trained in CFT treatment. In this protocol, a physical therapist with more than 5 years of experience conducted an interview and physical examination of the patients to determine their unique training programs, considering modifiable cognitive, biopsychosocial, functional, and lifestyle behavior factors.
The three components include the following:
1. The cognitive component focuses on identifying what makes pain worse during the examination. This includes a discussion of the multidimensional nature of persistent pain and individual beliefs, and how emotions and behaviors (movement and lifestyle) can reinforce the vicious cycle of pain and disability.
2. Specific exercises are designed to improve movements and posture. To perform these exercises, we ensure that the patient feels safe by being exposed to activities that are painful, feared, or avoided. This component is called exposure with ‘control’.
3. Integrating functional exercises with activities of daily living such as bending and sitting. This phase varies between individuals but should integrate new behaviors with the goal of gradual exposure to activities in daily life, reducing fear as necessary. This component is called lifestyle change.
All participants underwent a comprehensive interview and physical examination by their therapist to identify any relevant multidimensional factors considered to be key drivers of their pain and disability [18]. Treatment with CFT will be individualized. The therapist listens to the person’s story of pain and designs the therapy based on their needs. The first session involves discussing the pain and starting the treatment. The therapist asks questions and examines the person’s body to understand what may be causing the pain [18, 23, 24].
Physical examination includes examination of pain responses, analysis of functional behavior through observation, ability to change behaviors, and ability to control pain related to functional goals. The subjects’ activity levels, such as their ability to relax the trunk muscles and normalize the posture and provocative movement behavior, will also be evaluated [18, 19, 24]. Where an ineffective behavior is observed, an alternative movement strategy is implemented. This component of the treatment is called exposure with control [16]. Safe exercises with low frequency are gradually developed and turned into functional exercises with more and more complex frequency. For example, if a participant is initially unable to relax her body muscles at first, diaphragmatic breathing exercises in relaxed positions, such as lying down, sitting, and standing were recommended. If the participant could perform this stage, she would enter the next stage, where more challenging tasks were performed from the point of view of mind, relaxation, and control.
During the treatment, the therapist might ask the person to do certain exercises at home, either by watching videos or reading instructions. With practice, the person learns new ways to move and do things without causing pain.
As the therapy progresses, the person learns how to use these new techniques in their daily life. They gradually do activities they used to avoid due to fear of pain. The goal is to make them stronger and less afraid of pain.
Outcome measures
Pain
Pain was assessed with a 10 cm visual analog scale. The patient was asked to indicate the pain intensity during daily activities [25].
Disability
Oswestry disability index was used to disability evaluate (intraclass correlation coefficient [ICC]=0.84) [26]. Disability is classified in four subcategories including, a score of less than 25 as the lowest level of disability, 25-50 as moderate disability, 50-75 as severe disability, and 75-100 as acute disability [27].
Tampa scale for kinesiophobia (TSK) questionnaire
In this study, the fear of movement was assessed using the Tampa scale for kinesiophobia (TSK) questionnaire in the pre-test and post-test. The questionnaire consists of 11 statements, and participants are asked to complete each statement based on their actual results. The purpose of this questionnaire is to evaluate the fear of movement from different dimensions, such as fear of injury and avoidance of activity. The scoring spectrum is based on a four-option Likert scale, where “completely disagree” scores 1 and “completely agree” scores 4. The validity of this questionnaire has been confirmed in a study by Rahmati et al. To calculate its reliability, Cronbach’s α coefficient was used, and a Cronbach’s α of 0.82 was obtained for this questionnaire [28].
Statistical analysis
We used SPSS software, version 26 for statistical analysis. Shapiro-Wilk test was used to ensure the normal distribution of data. The equality of error variances was checked using Levene’s test. Two-way repeated measures analysis of variance (ANOVA) was used to analyze the effect of the intervention on bio-psychosocial indices (pain, disability, and Kinesiophobia variables). Partial eta squared effect size was assessed for two-way ANOVA (group×time interaction). A significance level of P<0.05 was considered. A covariance test was used for between-group comparison.
Results
Table 1 presents the demographic characteristics of the groups. The results of the Shapiro-Wilk test showed no statistically significant difference between the groups for demographic characteristics.
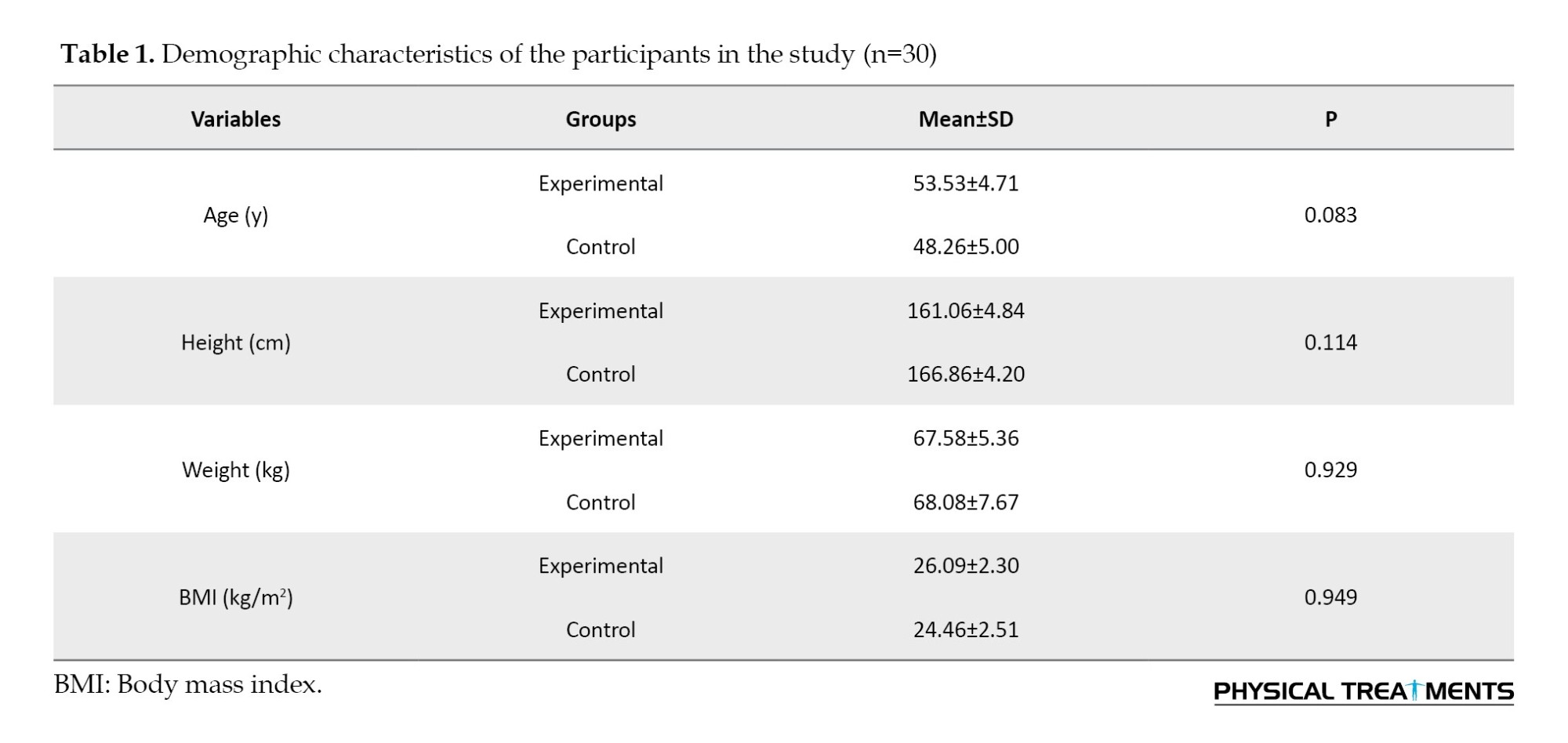
Table 2 presents the results of the two-way repeated measures ANOVA test. Two-way repeated measures ANOVA results showed that CFT intervention had a significant difference with high effect size in reducing pain (P=0.000, ƞ2=0.787), disability (P=0.000, ƞ2=0.457), and Kinesiophobia (P=0.000, ƞ2=0.561).
In Table 3, descriptive statistics showed that the experimental group had a 52% decrease in pain, 41% decrease in disability, and 12% decrease in Kinesiophobia.

Discussion
This clinical trial was conducted to evaluate the effectiveness of CFT intervention on pain, disability, and Kinesiophobia in patients with CNSLBP. The results of the research showed that CFT intervention has a significant effect in reducing pain, disability, and Kinesiophobia. Considering the close relationship between the variables of pain intensity, disability, and Kinesiophobia index and the overlap of these variables, an attempt was made to interpret the mechanism of CFT on these variables together.
O’Sullivan’s pain provocation classification system for LBP distinguishes between central and peripheral pain provocation. Central pain provocation is linked to psychological factors, such as fear of movement and depression, affecting around 30% of the LBP population. On the other hand, peripheral pain provocation stems from mechanical causes, movement impairments, and motor control issues, affecting approximately 30% of individuals with LBP [29]. Therefore, not only does the degree of injury have a role in shaping the level of functional limitation, and disability caused by chronic musculoskeletal pain, but people’s cognitions, beliefs, and thoughts also have a major impact on the disability caused by pain, therefore, functional cognitive exercises are effective on cognitive factors, and in this way, it can cause a decrease in kensiophobia and, as a result, a decrease in pain and disability in a person [30].
CFT has been used as a new method to improve the cognitive factors of people suffering from chronic low back pain, and the results have shown that these exercises have a positive and meaningful effect on cognitive factors [23]. One of the key factors in functional cognitive exercises is matching the characteristics of each person with the exercise that is specifically given to him. In CFT, the functional behavioral approach is targeted, such as a person’s awareness of her body, relaxation of contracted muscles, normalization of the wrong movement pattern, and reconstruction of a person’s mental image of her body [31].
The results of this study are consistent with those of Caneiro et al. [23], O’Keefe et al. [18], and Vibe Fersum et al. [19], all of which investigated the impact of CFT on individuals with CLBP.
In a case report by Caneiro et al., they examined changes related to kinesiophobia and disability through the implementation of functional cognitive exercises. The results demonstrated positive alterations in both kinesiophobia and disability variables. Remarkably, individuals undergoing these exercises exhibited a shift in their attitude toward pain perception and pain control within a span of six to 18 months [23]. These outcomes suggest that CFT can potentially facilitate the performance of painful and physically challenging activities, reduce central nervous system sensitivity, enhance self-confidence, and ultimately lead to a reduction in kinesiophobia, accompanied by decreased pain and disability.
Additionally, O’Keeffe et al. conducted research comparing the effects of cognitive-functional exercises and combined exercises on individuals with non-specific chronic back pain. The results showed a reduction of pain and improvement of functional disability in people with LBP [18]. Therefore, functional cognitive exercises lead to the improvement of pain and disability by changing a person’s attitude towards pain, pain control, and a person’s efficiency in daily activities [32].
In a RCT conducted by Vibe Fersum et al. involving individuals with chronic low back pain, it was observed that CFT yielded superior results in alleviating pain and reducing disability when compared to manual therapy [19]. CFT plays a crucial role in helping patients mitigate autonomic processes, such as an excessive focus on pain (e.g. kinesiophobia) and avoidance behaviors. By fostering more adaptive and healthier responses, CFT transforms the way patients engage with painful stimuli or pain-related sensations, promoting proactive responses to pain and minimizing unnecessary mental turmoil. The reduction of these processes among patients contributes to a diminished fear of movement, increased physical performance, and an overall enhancement in disability management [33].
The goal of this approach is to reconceptualize pain from a psycho-social perspective, while eliminating unhelpful beliefs, and adopting a healthy lifestyle [18].
Conclusion
By reducing fear of movement, CFT reduces pain and disability and strengthens positive beliefs. Therefore, it is suggested to use functional cognitive exercises as a complementary method in improving people with non-specific chronic back pain.
In this study, we had two limitations. First, our sample was only women. Second, no conditions were observed to evaluate long-term results. Therefore, it is recommended that researchers evaluate CFT interventions in both genders of patients with non-specific chronic low back pain and assess the long-term effects.
Ethical Considerations
Compliance with ethical guidelines
This study has been approved by the Ethics Committee of Bu-Ali Sina University (Code: IR.BASU.REC.1401.026) and the Clinical Trials System of Iran IRCT (Code: IRCT20230430058033N1). Patients provided their informed consent before any collection and the Helsinki declaration of 2008 was followed.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank all patients for participating in this clinical trial.
References
- Ahmadnezhad L, Yalfani A. [The relationship between pain and functional disability with local and global selected trunk muscles activity and comparison the activity of these muscles between men and women with non-specific chronic low back pain (Persian). J Anesth Pain. 2019; 10(2): 1-11. [Link]
- Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, et al. A systematic review of the global prevalence of low back pain. Arthritis and Rheumatism. 2012; 64(6):2028-37. [DOI:10.1002/art.34347] [PMID]
- Farahpour N, Jafarnezhadgero A, Allard P, Majlesi M. Muscle activity and kinetics of lower limbs during walking in pronated feet individuals with and without low back pain. Journal of Electromyography and Kinesiology. 2018; 39:35-41. [DOI:10.1016/j.jelekin.2018.01.006] [PMID]
- Abd Rahman NA, Li S, Schmid S, Shaharudin S. Biomechanical factors associated with non-specific low back pain in adults: A systematic review. Physical Therapy in Sport. 2023; 59:60-72. [DOI:10.1016/j.ptsp.2022.11.011] [PMID]
- Verbrugghe J, Agten A, Stevens S, Vandenabeele F, Roussel N, Verbunt J, et al. High intensity training improves symptoms of central sensitization at six-month follow-up in persons with chronic nonspecific low back pain: Secondary analysis of a randomized controlled trial. Brazilian Journal of Physical Therapy. 2023; 27(2):100496. [DOI:10.1016/j.bjpt.2023.100496] [PMID]
- Patricio P, Roy JS, Macedo L, Roy M, Léonard G, Hodges P, et al. Repetitive transcranial magnetic stimulation alone and in combination with motor control exercise for the treatment of individuals with chronic non- specific- low back pain (ExTraStim trial): Study protocol for a randomized controlled trial. BMJ Open. 2021; 11(3):e045504 [DOI:10.1136/bmjopen-2020-045504] [PMID]
- O’Sullivan P. It’s time for change with the management of non-speci¦c chronic low back pain. British Journal of Sports Medicine. 2012; 46(4):224-7. [DOI:10.1136/bjsm.2010.081638] [PMID]
- Campbell P, Bishop A, Dunn KM, Main CJ, Thomas E, Foster NE. Conceptual overlap of psychological constructs in low back pain. Pain. 2013; 154(9):1783-91. [DOI:10.1016/j.pain.2013.05.035] [PMID]
- Dankaerts W, O'Sullivan P, Burnett A, Straker L, Davey P, Gupta R. Discriminating healthy controls and two clinical subgroups of nonspecific chronic low back pain patients using trunk muscle activation and lumbosacral kinematics of postures and movements: A statistical classification model. Spine (Phila Pa 1976). 2009; 34(15):1610-8. [DOI:10.1097/BRS.0b013e3181aa6175] [PMID]
- Lee H, Hübscher M, Moseley GL, Kamper SJ, Traeger AC, Mansell G, et al. How does pain lead to disability? A systematic review and meta-analysis of mediation studies in people with back and neck pain. Pain. 2015; 156(6):988-97. [DOI:10.1097/j.pain.0000000000000146] [PMID]
- Briggs AM, Jordan JE, O’Sullivan PB, Buchbinder R, Burnett AF, Osborne RH, et al. Individuals with chronic low back pain have greater di¨culty in engaging in positive lifestyle behaviours than those without back pain: An assessment of health literacy. BMC Musculoskeletal Disorders. 2011; 12:161. [DOI:10.1186/1471-2474-12-161] [PMID]
- Steenstra IA, Verbeek JH, Heymans MW, Bongers PM. Prognostic factors for duration of sick leave in patients sick listed with acute low back pain: A systematic review of the literature. Occupational and Environmental Medicine. 2005; 62(12):851-60. [DOI:10.1136/oem.2004.015842] [PMID]
- Lima M, Ferreira AS, Reis FJJ, Paes V, Meziat-Filho N. Chronic low back pain and back muscle activity during functional tasks. Journal of Gait & Posture. 2018; 61:250-6. [DOI:10.1016/j.gaitpost.2018.01.021] [PMID]
- Rusu AC, Kreddig N, Hallner D, Hülsebusch J, Hasenbring MI. Fear of movement/(Re)injury in low back pain: Confirmatory validation of a German version of the Tampa Scale for Kinesiophobia. BMC Musculoskeletal Disorders. 2014; 15:280. [DOI:10.1186/1471-2474-15-280] [PMID]
- Ahmadi M, Yalfani A, Gandomi F, Rashid K. [The effect of twelve week neurofeedback training on perceptual pain, intensity, fear of pain, pelvic drop, and dynamic knee valgus index in men with patellofemoral pain syndrome: A randomized double blind clinical trial (Persian)]. Sadra Medical Journal. 2020; 8(2):151-64. [Link]
- O'Sullivan PB, Caneiro JP, O'Keeffe M, Smith A, Dankaerts W, Fersum K, et al. Cognitive functional therapy: An integrated behavioral approach for the targeted management of disabling low back pain. Physical Therapy. 98(5):408–23.[DOI:10.1093/ptj/pzy022] [PMID]
- Caneiro JP, Smith A, Rabey M, Moseley GL, O'Sullivan P. Process of change in pain-related fear: clinical insights from a single case report of persistent back pain managed with cognitive functional therapy.The Journal of Orthopaedic and Sports Physical Therapy. 2017; 47(9):637-51. [DOI:10.2519/jospt.2017.7371] [PMID]
- O'Keeffe M, Purtill H, Kennedy N, O'Sullivan P, Dankaerts W, Tighe A, et al. Individualised cognitive functional therapy compared with a combined exercise and pain education class for patients with non-specific chronic low back pain: A multicentre randomised controlled trial. BMJ Open. 2015; 5(6):e007156. [DOI:10.1136/bmjopen-2014-007156] [PMID]
- Vibe Fersum K, O'Sullivan P, Skouen JS, Smith A, Kvåle A. Efficacy of classification-based cognitive functional therapy in patients with non-specific chronic low back pain: A randomized controlled trial. European Journal of Pain. 2013; 17(6):916-28. [DOI:10.1002/j.1532-2149.2012.00252.x] [PMID]
- Abbasi S, Hadian Rasanani MR, Ghotbi N, Olyaei GR, Bozorgmehr A, Rasouli O. Short-term effect of kinesiology taping on pain, functional disability and lumbar proprioception in individuals with nonspecific chronic low back pain: A double-blinded, randomized trial. Chiropractic & Manual Therapies. 2020; 28(1):63. [DOI:10.1186/s12998-020-00349-y] [PMID]
- Yalfani A, Ahmadi M, Asgarpoor A, Hajia Amadi A. Effect of foot orthoses on dynamic balance in taekwondo athletes with flexible flatfoot: A randomized controlled trial. Foot (Edinburgh, Scotland). 2023; 56:102042. [PMID]
- Yalfani A, Abedi M, Raeisi Z. Effects of an 8-week virtual reality training program on pain, fall risk, and quality of life in elderly women with chronic low back pain: Double-blind randomized clinical trial. Games for Health Journal. 2022; 11(2):85-92. [DOI:10.1089/g4h.2021.0175] [PMID]
- Cañeiro JP, Ng L, Burnett A, Campbell A, O'Sullivan PB. Cognitive functional therapy for the management of low back pain in an adolescent male rower: A case report. Journal of Orthopaedic & Sports Physical Therapy. 2013; 43(8):542-54. [DOI:10.2519/jospt.2013.4699] [PMID]
- Meziat Filho N. Changing beliefs for changing movement and pain: Classification-based cognitive functional therapy (CB-CFT) for chronic non-specific low back pain. Manual Therapy. 2016; 21:303-6. [DOI:10.1016/j.math.2015.04.013] [PMID]
- Mostagi FQ, Dias JM, Pereira LM, Obara K, Mazuquin BF, Silva MF, et al. Pilates versus general exercise effectiveness on pain and functionality in non-specific chronic low back pain subjects. Journal of Bodywork and Movement Therapies. 2015; 19(4):636-45. [DOI:10.1016/j.jbmt.2014.11.009] [PMID]
- Inani SB, Selkar SP. Effect of sport stabilization exercise versus conventional exercise on pain and functional status in patients with non-specific low back pain: A randomized clinical trial. Journal of Back and Musculoskeletal Rehabilitation. 2013; 26(1):37-43. [DOI:10.3233/BMR-2012-0348] [PMID]
- Yalfani A, Raeisi Z, Koumasian Z. Effects of eight-week water versus mat pilates on female patients with chronic nonspecific low back pain: Double-blind randomized clinical trial. Journal of Bodywork and Movement Therapies. 2020; 24(4):70-75. [PMID]
- Rahmati N, Moghadam MA, Shairi MR, Paknejad M, Rahmati Z, Ghassami M, et al. [Psychometric properties of the Tampa Scale for Kinesiophobia amongst Iranian patients with chronic persistent pain (Persian)]. Payesh. 2014; 13(2):197-210. [Link]
- O'Sullivan P. Diagnosis and classification of chronic low back pain disorders: Maladaptive movement and motor control impairments as underlying mechanism. Manual Therapy. 2005; 10(4):242-55. [DOI:10.1016/j.math.2005.07.001] [PMID]
- Wand BM, O’Connell NE. Chronic non-specific low back pain-sub-groups or a single mechanism? BMC Musculoskeletal Disorders. 2008; 9:11. [DOI:10.1186/1471-2474-9-11] [PMID]
- Lewis S, Holmes P, Woby S, Hindle J, Fowler N. The relationships between measures of stature recovery, muscle activity and psychological factors in patients with chronic low back pain. Manual Therapy. 2012; 17(1):27-33. [DOI:10.1016/j.math.2011.08.001] [PMID]
- O’Sullivan P, Dankaerts W, O’Sullivan K, Fersum K. Multidimensional approach for the targeted management of low back pain. Grieve’s Modern Musculoskeletal Physiotherapy.Edinburgh: Elsevier; 2015. [Link]
- Hayes AM, Feldman G. Clarifying the construct of mindfulness in the context of emotion regulation and the process of change in therapy. Clinical Psychology: Science and Practice. 2004; 11(3):255-62. [DOI:10.1093/clipsy.bph080]
Type of Study: Research |
Subject:
General
Received: 2023/08/13 | Accepted: 2023/11/3 | Published: 2024/01/1
Received: 2023/08/13 | Accepted: 2023/11/3 | Published: 2024/01/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






