Fri, Apr 19, 2024
Volume 9, Issue 2 (Spring 2019)
PTJ 2019, 9(2): 107-116 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sahebozamani M, Salari A, Daneshjoo A, Karimi Afshar F. Assessment of Balance Recovery Strategies During Manipulation of Somatosensory, Vision, and Vestibular Systems in Deaf Persons. PTJ 2019; 9 (2) :107-116
URL: http://ptj.uswr.ac.ir/article-1-391-en.html
URL: http://ptj.uswr.ac.ir/article-1-391-en.html
1- Department Sports pathology and corrective movements, Faculty of Physical Education, Shahid Bahonar University of Kerman, Kerman, Iran.
2- Department of Sport Medicine, Faculty of Medical Sciences, Kerman University of Medical Sciences, Kerman, Iran.
2- Department of Sport Medicine, Faculty of Medical Sciences, Kerman University of Medical Sciences, Kerman, Iran.
Full-Text [PDF 577 kb]
(1356 Downloads)
| Abstract (HTML) (2695 Views)
To this end, five spherical reflective markers with 51 mm in diameter were mounted on the right side of the body. As the subject’s movement is needed to be recognized by the cameras, five sphere-shaped reflective markers were installed on anterior superior iliac spine projection, great trochanter in the thigh bone, external epicondyle in thigh, external ankle, and the fifth metatarsal. As a result, a two-dimensional model was defined with four sections, including leg, shin, thigh, and pelvis, for calculating the sways of ankle joint and hip joint while imposing perturbations in the sagittal plane (Figure 2).
The ankle joint was assumed as an angle between foot and shin, but the hip joint was considered as an angle between thigh and pelvis. In the following of the test, every subject stood on the treadmill with bare feet, their hand being crossed on the chest, and the right side of the body being directed to the cameras. The positioning was left at the subjects’ discretion, depending on the leg place to find their normal and comfortable position.
The subjects were asked to stand on the treadmill, once in front of the treadmill monitor, and once back to treadmill monitor, to do movements under the planned movement directions and the imposed anterior-posterior perturbations while maintaining their straight posture despite the imposed abrupt velocity. It is worth mentioning that the monitor screen was covered with medical tape to control further visual confounders.
Next, the treadmill was abruptly started to run without any warning to the subject, and the perturbations were imposed in the anterior or posterior directions to the posture of the subject. The subjects were requested to resist the imposed perturbation without stepping, and when their feet were moved, the movement would be required to repeat. The speed of the treadmill was set at 1.1 m/s according to the pilot project (performing the test by the subjects before the initial testing) for all subjects that made a 40 cm movement in the treadmill. The cameras installed at distance of 2 m from treadmill recorded the sways of the hip and ankle joints for 5 s after imposing perturbation; the recorded information was, then, analyzed, using Cortex software. Every subject did each movement in triple time, and the mean of these repeated movements was evaluated to calculate parameters and study variables. Thirty seconds was considered for the rest between each repetition.
In the last stage, the recorded information in the software was extracted as a file in Excel format, and it was studied further for calculating the kinematic changes in the range of motion of ankle and hip. The subjects were secured with a supporting belt hanged from the roof to the middle of treadmill. The above-mentioned perturbations (anterior-posterior perturbations) are studied in different positions.
The above perturbations (anterior and posterior perturbation) were performed in 4 different sensory states, each representing a test as follows:
State 1. reference state or applying perturbations without sensory interference; state 2. applying perturbations simultaneously with interfering vestibular and vision system; state 3. applying perturbations simultaneously with interfering vision and proprioception; state 4. applying perturbations simultaneously with interfering the vestibular system and proprioception
It is worth noting that in state 1, no manipulation of vestibular, vision systems, and proprioception was conducted. In state 2, the vestibular system (head hyperextension motions) and the vision system (closing eyes using a blindfold) were disrupted, and only sensory data were received without the disorder. In state 3, the somatosensory system data (putting foam under the subject’s feet) and vision were disrupted, and the dominant system for restoring the balance was the vestibular system. Finally, in state 4, the somatosensory and vestibular data systems were disrupted, and vision system data was used to restore balance.
The descriptive statistics were used to present the characteristics of the subjects, as well as the research variables. The Independent t-test was used to compare the scores of the subjects in the two groups. All statistical tests had a 95% confidence interval, and the alpha was smaller than or equal to 0.05, using SPSS V. 24.
3. Results
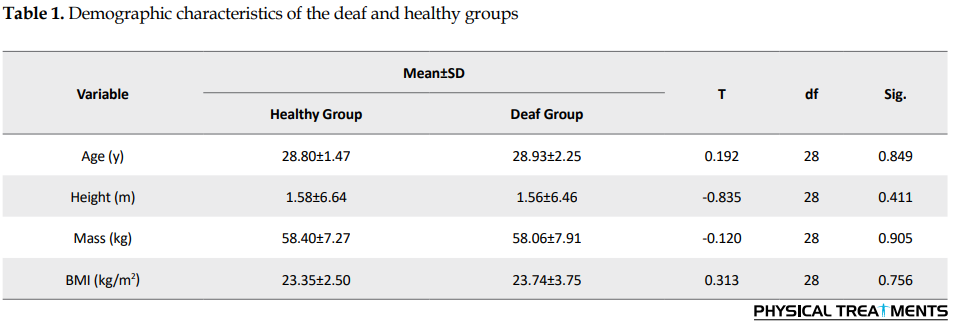
Table 1 presents the characteristics related to age, height, weight, and body mass index (BMI) of subjects. The results show no significant difference between age, height, weight, and BMI of the groups, and the groups were homogeneous in these variables.
The following tables present information related to the swings of the ankle and hip joints in different states in the group after the anterior-posterior and posterior-anterior perturbations. To assess the superiority of each ankle or hip strategy in subjects, the ratio of was used, i.e. the higher the ratio, the more support on hip strategy, and smaller values suggest more use of ankle strategy to restore balance.
Based on the analysis of the results, the mean of hip and ankle swings in different states except for the first one was significantly higher in the deaf group compared to the healthy group both in the anterior-posterior perturbations and the posterior-anterior perturbations (P<0.05). However, there was no significant difference between the ratios of hip-to-ankle swings (the dominant strategy for balance recovery) in all states except for the third state (P>0.05).
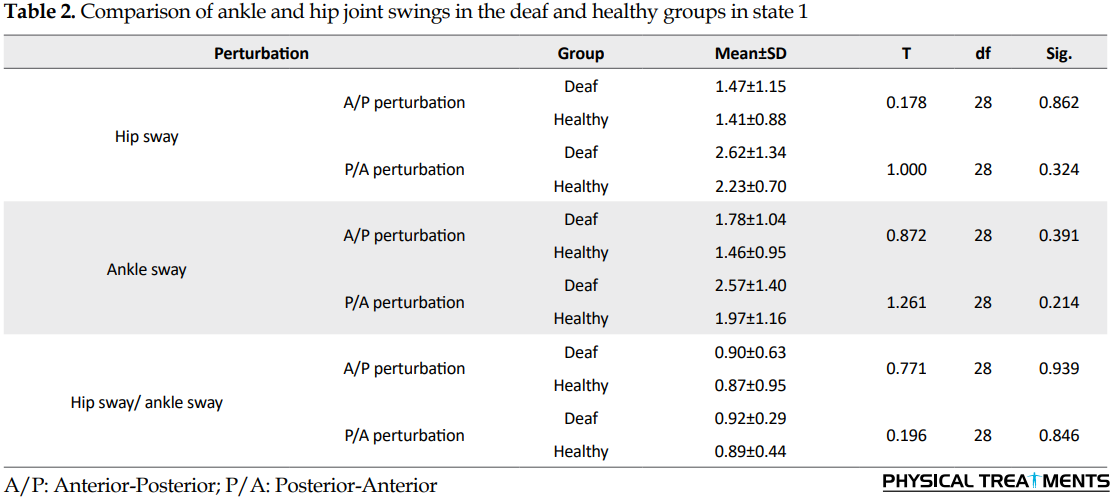
In state 1, there was no significant difference between the hip and ankle swings in the two groups; however, the number of swings in the joints was higher in response to anterior-posterior and posterior-anterior perturbations in the deaf persons than in the healthy subjects (Table 2).
The results also indicated no significant difference between the hip-to-ankle swing ratios and for balance recovery in both groups. Also, in the anterior-posterior perturbation and posterior-anterior perturbations, ankle strategy was the dominant strategy (based on statistical results if the ratio is less than 1, the dominant strategy is the ankle strategy). In this state, the swings of the joints were lower than those of the other states. In state 2, despite differences in joint swings of the hip and ankle between two groups, there was no significant difference between the hip/ankle ratio in the two groups, and the dominant strategy for the balance recovery in both groups was the ankle strategy (Table 3).
In the state 3, there was a significant difference between the hip and ankle joint swings in the subjects, as well as the hip/ankle ratio to the two groups, and the results indicated that the support of the individuals on the hip swings increased for restoring the balance. In this state, the hip/ankle ratio swings were higher than the other three states (Table 4). In the state 4, despite the difference in hip and ankle swings between the two groups, there was no significant difference in the hip/ankle ratio to the two groups, and the dominant strategy for the balance recovery in both groups was the ankle strategy (Table 5).
4. Discussion
Maintaining and restoring body balance depends on the accurate and precise information sent to the central nervous system by the visual, somatosensory, and vestibular systems. These systems inform the central nervous system of the state and movements of various organs in the body. After processing this information, they send the required motion command to the involved muscles.
Previous research has shown that sensory information related to the posture is multiple, and visual, somatosensory, and vestibular systems comprise the most important ones. In certain circumstances, the role of one of them may be more prominent. For instance, in the darkness, the role of other senses other than vision becomes more important. In other words, these systems overlap, meaning that if the information of one of the systems is incomplete, the central nervous system issues the necessary command, using the information of the other two systems.
In the present study, the data of two other sensory systems were disrupted to obtain the efficiency of each system in balancing the recovery. For example, by closing the eyes and hypertension of the head, the central nervous system will have its support to restore balance by the information obtained from sensory receptors [7, 14].
The results of this study indicated that in the first state (reference state), where there was no manipulation in the vestibular, vision, and proprioception systems, the rate of hip/ankle joints swing in response to anterior-posterior and posterior-anterior perturbations was more common in the deaf group than the healthy people, but there was no significant difference between the two groups.
In state 2, with disrupted vestibular and vision systems and proper somatosensory data, there was a substantial difference between the two groups in the rates of hip/ankle joints swings. In state 3, with the impaired somatosensory and vision system data and where the dominant system for retrieving the balance was the vestibular system, there was a significant difference between the two groups in the rate of hip and ankle joint swings and the individuals’ support to hip swings increased for restoring balance.
Eventually, in state 4, when the somatosensory and vestibular systems were disrupted, and visual data were used to restore balance, there was a significant difference between the two groups in the number of joint swings. The degree of swing in the first state existing in all 3 sensory systems is lower than the other states. In the third state, with disrupted vision and proprioception and the vestibular system as the dominant system to restore balance, the swings were more than other states. In general, in all states, the amount of hip/ankle swings of the deaf group was higher than the healthy subjects.
These results were consistent with the reports of Malek Abadi Zadeh, Kegel et al. Melo et al. Rine et al. Jafari et al. and Rajendran [14-20]. The above studies reported that damage to the vestibular system had a negative effect on postural control in people with hearing impairment, and postural swings in these individuals are more than healthy people and suffer from a poorer balance, reducing the chances of successful recovery in these individuals. Based on the previous study, it plays an essential role in maintaining and restoring the balance of sensory systems, including the vestibular portion of the inner ear, visual sense, and proprioception. Because of the dependence of the balance system on sensory inputs, if one of the sensory inputs reduces or stops, the swings of the body increases and, as a result, the muscle activity increases to maintain the balance [21, 22].
In general, according to the results obtained from the research, increasing the hip and ankle swings in the deaf group to restore the balance created in the above-mentioned states increases the center of gravity within the base of support and reduces the ability to control the posture of individuals against the disturbances imposed on the body.
The results of the present study also indicated that in all states, except for the third state, where the vestibular system was the dominant system for balance recovery, there was no significant difference between the two groups in hip and ankle ratios. Generally, the mean swing ratio in the healthy group was less than the deaf group. Also, the mean swings of the joints studied were lower in the first state and higher in the third state compared to the other states. Also, the strategy used to restore balance in all states in both groups was the ankle strategy, except for the third state, where the subjects in both healthy and the deaf groups had greater support on hip swings to restore balance. These subjects should use one of the visual, sensory, and vestibular systems to restore balance. According to a research report on the balance of the deaf persons, they can perform equilibrium activities without any problem in spite of a malfunction in the vestibular data in the absence of impairment in the visual and sensory system data [13, 23-25].
In the present study, the subjects indicated higher swings in the absence of interference in the systems and lower swings and showed more swings when the vestibular system was dominant. By investigating the vestibular and motor skills in children with hearing impairment, Horak et al. found that children with hearing impairment had a defect in the vestibular system and had a problem when the vestibular system data were the only sensory source available. In deaf people, compensatory mechanisms have grown in response to vestibular defects. It is likely that in the event of visual or somatosensory impairment, i.e. damage to compensatory mechanisms, there will be signs of a disorder in balance performance.
Based on the results of this study, when the vision system was the dominant system for balance recovery, the rate of swing and the ratio of the hip to ankle swings in healthy people were lower compared to the situation, where the somatosensory system was dominant. However, in deaf people, when the somatosensory system was the dominant system for balance recovery, the rate of swings and the ratio of hip to ankle decreased compared to the situation, where the vision system was dominant, probably emphasizing the role of the somatosensory system in restoring the balance of the deaf group. Preserving the body posture depends on interacting with the visual, vestibular, and somatosensory systems [23]. In a study on balance, Assaiante et al. found that in healthy people, the vision system plays a key role before the age of seven.
At age seven, the role of the vision system is negligible, but after the age nine, the role of vision becomes more essential again [25]. Moreover, Bardy and Laurent stated that when tasks for non-athletic subjects gradually become more complicated, the role of vision is emphasized in their postural control [26]. This point is significant in the balance and vision topics, with approximately 20% of the neural fibers of the eyes associated with the vestibular system, and vision problems are sometimes owing to vestibular disorders [27].
The sudden spins of the head occur because of the semicircular duct signals causing the same amount of eye rotation but in the opposite direction of the head rotation. This is because of the reflexes are directed to the oculomotor nuclei through the vestibular nuclei and the median longitudinal nucleus [1]. Consequently, we observe that vestibular system is vital to gaze stabilization (gazing ability). Hence, damage to the vestibular system causes impairment in balance and gazing performance [28].
Since congenital deaf people are weak and defective in the vestibular system and, as stated, the vestibular system data are vital for gaze stabilization, the visual system efficiency of them is lower than that of the healthy people and this factor may reduce the efficiency of the visual system compared to the somatosensory system in the deaf group [1]. In this regard, the results of Khanna’s research shows that in normal conditions, the individual relies more on his somatosensory system to correct body swings rather than the visual inputs [29]. In addition, Szymczyk expresses that the proprioception and skin receptors are sufficient in the deaf group to the extent that they can compensate for any interference in receiving other data from the sensory systems controlling the balance [13].
In general, the results of the present study indicated that in the absence of manipulation of vestibular, vision, and proprioception systems, the swing rates of the hip and ankle joints were lower, and both the deaf and healthy groups used ankle strategy to restore balance. Moreover, by creating disorder in sending sensory impulses from feedback resources to the central nervous system to restore the balance, more improper correction commands were created resulting in higher hip and ankle swings [30].
By and large, the deaf people, in the face of sensory disturbances and immediate perturbations, are more likely to rely on body somatosensory systems to restore balance as a superior equilibrium system. In this regard, the roles of the visual and the vestibular systems are in the next priorities, while healthy people rely primarily on vision system information to regain balance as the supreme balance system. In other words, they rely on the visual system and, then, on the vestibular system.
The results of this study can be used to design deaf rehabilitation programs. The results indicate that muscular neural training that improves the somatosensory system may have more effect on improving the balance of deaf persons. Therefore, such exercises are suggested to be considered more in sports programs and rehabilitation of deaf people to prevent them from falling by providing the necessary measures to improve the balance power and control the body posture to restore balance.
Ethical Considerations
Compliance with ethical guidelines
The Ethics Committee of Kerman University of Medical Sciences approved the study (IR.KMU.REC.1395.351). Iranian Registry of Clinical Trials: IRCT2017022132705N1.
Funding
The present paper was extracted from PhD. thesis of the second author, Department of Sport Injuries and Corrective movements, Faculty of Physical Education, Shahid Bahonar University of Kerman, Kerman, Iran.
Authors' contributions
Conceptualization, methodology, and investigation: All authors; Writing-original draft: Asma Salari; Writing-review & editing: Mansour Sahebozamani, Abdolhamid Daneshjoo and Fatemeh Karimi Afshar; Funding acquisition and resources: All authors; Supervision: Asma Salari.
Conflict of interests
The authors declared no conflict of interest
References
Full-Text: (948 Views)
1. Introduction
One of the most critical factors in communicating with others is hearing, and any disruption in this system isolates the deaf and hearing-impaired people from the community and, consequently, prevent them from development in personality and other aspects of their growth [1]. Over 120 million people suffer from hearing impairments worldwide [2]. The most hearing-impairment incidents were reported in Asian children at 2.6 per 1000 births and 0.7 per 1000 births for non-Asian children [3]. In Iran, out of every 1000 births, five or six children suffer from hearing impairment [4].
Hearing-impairment problems are often addressed only in terms of communication. The communication problem is the primary defect of hearing impairment [3]. though other physical problems may also be associated In this regard, by damaging the sensory integrity and motor growth, balance impairment is one of the defects that often occurs in hearing-impaired people. These disorders may affect learning other motor skills, visual development, perceptual-motor development, and sensory integrity [5, 6].
Posture balance or stability is the ability of the body to maintain the center of gravity within the base of support or the ability to maintain a position for a movement or in response to the application of an external perturbation. As one of the controversial concepts of the sensory-motor system, equilibrium investigates the mutual and complex relationship among sensory data and motor responses required for maintaining or modifying postures and plays an essential role in preventing people from falling while walking or standing [1, 7].
Numerous biomechanical, sensory, and motor factors work to maintain physical stability and balance, among which the vestibular system, the position, and vision senses should be considered more. Information obtained from these systems is involved in forming a reference framework, and their combination leads to a standard that measures sequential changes in posture. In other words, it creates the general schema of the body and enables the nervous system to be permanently aware of the state of the body in space and the state of the body parts towards each other.
Clinically, upright (direct) postural stability requires the coordination of afferents of each of the visual, vestibular, and somatosensory systems that act simultaneously and in synchronization, all necessary for postural corrective responses. Disorder in each of these systems is usually compensated by the two remaining systems. One of the systems often generates false or inadequate information, and in this situation, it is crucial that the remaining senses provide correct and sufficient information to maintain balance.
For example, in the case of somatosensory controversy (in moving cases or softness of the support), the balance with closed eyes is significantly reduced compared with open eyes. Somatosensory inputs provide information about the orientation of different parts of the body relative to each other and also to the base of support. The visual sense measures the eyes and the head orientation towards the peripheral objects and plays a vital role in maintaining balance. At a constant level, closing eyes cause a slight postural fluctuation in a healthy person; however, if the somatosensory input is disrupted because of ligament damage or other factors, closing eyes will significantly increase the postural fluctuation [8].
If the above coordination is well shaped, the body will be able to help maintain a center of gravity within the base of support by continuing a proper strategy for postural control and maintaining balance in different situations.
The previous research determined that each strategy used to retrieve the balance has a definite pattern of synergistic muscle activity. These motion patterns pertain to compensatory mechanisms that are used both in forward and backward motions as predictive behaviors for maintaining and retrieving equilibrium. These mechanisms include fixed support such as ankle and hip, in which the relocation of the center of pressure is controlled without a change in the base of support, and change in support strategies such as stepping and gripping, where the center of pressure is controlled by changing the base of support. These strategies help prevent the center of gravity from leaving the base of support, as well as preventing people from falling so that they can retrieve the postural stability [9, 10].
Based on the previous studies, because of the defect in the vestibular system, absolute and profound congenital deaf people are weaker in maintaining balance and postural control than healthy people so that it can reduce the chance of successful recovery in these individuals [11, 12]. Moreover, research on the postural stability of people with vestibular disorder shows that when both visual and somatosensory data are properly sent, they will have normal postural deviation. Conversely, when visual and somatosensory data were inadequate, it was difficult for them to maintain their posture [13]. But, there is still ambiguity about the effectiveness and priority of the data of each of the sensory systems involved in postural control to select a strategy for obtaining balance.
In other words, to what extent are the deaf people dependent on different sources of afferents to recover balance to compensate for the lost sensory inputs? Besides, it has not yet been determined that what kind of balance recovery strategy is used when manipulating sensory systems involved in balance in the face of perturbation?
Therefore, the present study aims at investigating the contribution of sensory, visual, and vestibular systems in balancing strategies. We try to provide evidence and suggestions for designing rehabilitation and training interventions, focusing on reducing the risk of falling in deaf people.
2. Materials and Methods
This research was a quasi-experimental study, in which the subjects were selected among 110 healthy and deaf women after initial evaluations. The authors selected 15 subjects from both groups by purposeful sampling method according to the inclusion and exclusion criteria. The most important criteria were the rate of hearing impairment (absolute or profound and congenital) with deafness greater than 90 dB (demographic information and medical records of the deaf persons were collected from their medical records), non-history of pathology, and apparent postural anomalies considered in the selection of samples. Because of their inability to speak and listen, a deaf interpreter accompanied at all stages of working with deaf people along with a researcher in the lab.
One of the most critical factors in communicating with others is hearing, and any disruption in this system isolates the deaf and hearing-impaired people from the community and, consequently, prevent them from development in personality and other aspects of their growth [1]. Over 120 million people suffer from hearing impairments worldwide [2]. The most hearing-impairment incidents were reported in Asian children at 2.6 per 1000 births and 0.7 per 1000 births for non-Asian children [3]. In Iran, out of every 1000 births, five or six children suffer from hearing impairment [4].
Hearing-impairment problems are often addressed only in terms of communication. The communication problem is the primary defect of hearing impairment [3]. though other physical problems may also be associated In this regard, by damaging the sensory integrity and motor growth, balance impairment is one of the defects that often occurs in hearing-impaired people. These disorders may affect learning other motor skills, visual development, perceptual-motor development, and sensory integrity [5, 6].
Posture balance or stability is the ability of the body to maintain the center of gravity within the base of support or the ability to maintain a position for a movement or in response to the application of an external perturbation. As one of the controversial concepts of the sensory-motor system, equilibrium investigates the mutual and complex relationship among sensory data and motor responses required for maintaining or modifying postures and plays an essential role in preventing people from falling while walking or standing [1, 7].
Numerous biomechanical, sensory, and motor factors work to maintain physical stability and balance, among which the vestibular system, the position, and vision senses should be considered more. Information obtained from these systems is involved in forming a reference framework, and their combination leads to a standard that measures sequential changes in posture. In other words, it creates the general schema of the body and enables the nervous system to be permanently aware of the state of the body in space and the state of the body parts towards each other.
Clinically, upright (direct) postural stability requires the coordination of afferents of each of the visual, vestibular, and somatosensory systems that act simultaneously and in synchronization, all necessary for postural corrective responses. Disorder in each of these systems is usually compensated by the two remaining systems. One of the systems often generates false or inadequate information, and in this situation, it is crucial that the remaining senses provide correct and sufficient information to maintain balance.
For example, in the case of somatosensory controversy (in moving cases or softness of the support), the balance with closed eyes is significantly reduced compared with open eyes. Somatosensory inputs provide information about the orientation of different parts of the body relative to each other and also to the base of support. The visual sense measures the eyes and the head orientation towards the peripheral objects and plays a vital role in maintaining balance. At a constant level, closing eyes cause a slight postural fluctuation in a healthy person; however, if the somatosensory input is disrupted because of ligament damage or other factors, closing eyes will significantly increase the postural fluctuation [8].
If the above coordination is well shaped, the body will be able to help maintain a center of gravity within the base of support by continuing a proper strategy for postural control and maintaining balance in different situations.
The previous research determined that each strategy used to retrieve the balance has a definite pattern of synergistic muscle activity. These motion patterns pertain to compensatory mechanisms that are used both in forward and backward motions as predictive behaviors for maintaining and retrieving equilibrium. These mechanisms include fixed support such as ankle and hip, in which the relocation of the center of pressure is controlled without a change in the base of support, and change in support strategies such as stepping and gripping, where the center of pressure is controlled by changing the base of support. These strategies help prevent the center of gravity from leaving the base of support, as well as preventing people from falling so that they can retrieve the postural stability [9, 10].
Based on the previous studies, because of the defect in the vestibular system, absolute and profound congenital deaf people are weaker in maintaining balance and postural control than healthy people so that it can reduce the chance of successful recovery in these individuals [11, 12]. Moreover, research on the postural stability of people with vestibular disorder shows that when both visual and somatosensory data are properly sent, they will have normal postural deviation. Conversely, when visual and somatosensory data were inadequate, it was difficult for them to maintain their posture [13]. But, there is still ambiguity about the effectiveness and priority of the data of each of the sensory systems involved in postural control to select a strategy for obtaining balance.
In other words, to what extent are the deaf people dependent on different sources of afferents to recover balance to compensate for the lost sensory inputs? Besides, it has not yet been determined that what kind of balance recovery strategy is used when manipulating sensory systems involved in balance in the face of perturbation?
Therefore, the present study aims at investigating the contribution of sensory, visual, and vestibular systems in balancing strategies. We try to provide evidence and suggestions for designing rehabilitation and training interventions, focusing on reducing the risk of falling in deaf people.
2. Materials and Methods
This research was a quasi-experimental study, in which the subjects were selected among 110 healthy and deaf women after initial evaluations. The authors selected 15 subjects from both groups by purposeful sampling method according to the inclusion and exclusion criteria. The most important criteria were the rate of hearing impairment (absolute or profound and congenital) with deafness greater than 90 dB (demographic information and medical records of the deaf persons were collected from their medical records), non-history of pathology, and apparent postural anomalies considered in the selection of samples. Because of their inability to speak and listen, a deaf interpreter accompanied at all stages of working with deaf people along with a researcher in the lab.
At the beginning of the study, a summary of the research design was explained to all subjects. After obtaining consent from the volunteers, these subjects were examined for medical history and general health (general health questionnaire) to check the lack of neurological disease, dizziness, surgery, and previous damage, especially in the lower extremities. Balance recovery strategies in this study were investigated as a two-dimensional kinematic through a motion analysis system with six high-speed cameras (ICC ≥0.79) (Figure 1).
To this end, five spherical reflective markers with 51 mm in diameter were mounted on the right side of the body. As the subject’s movement is needed to be recognized by the cameras, five sphere-shaped reflective markers were installed on anterior superior iliac spine projection, great trochanter in the thigh bone, external epicondyle in thigh, external ankle, and the fifth metatarsal. As a result, a two-dimensional model was defined with four sections, including leg, shin, thigh, and pelvis, for calculating the sways of ankle joint and hip joint while imposing perturbations in the sagittal plane (Figure 2).
The ankle joint was assumed as an angle between foot and shin, but the hip joint was considered as an angle between thigh and pelvis. In the following of the test, every subject stood on the treadmill with bare feet, their hand being crossed on the chest, and the right side of the body being directed to the cameras. The positioning was left at the subjects’ discretion, depending on the leg place to find their normal and comfortable position.
The subjects were asked to stand on the treadmill, once in front of the treadmill monitor, and once back to treadmill monitor, to do movements under the planned movement directions and the imposed anterior-posterior perturbations while maintaining their straight posture despite the imposed abrupt velocity. It is worth mentioning that the monitor screen was covered with medical tape to control further visual confounders.
Next, the treadmill was abruptly started to run without any warning to the subject, and the perturbations were imposed in the anterior or posterior directions to the posture of the subject. The subjects were requested to resist the imposed perturbation without stepping, and when their feet were moved, the movement would be required to repeat. The speed of the treadmill was set at 1.1 m/s according to the pilot project (performing the test by the subjects before the initial testing) for all subjects that made a 40 cm movement in the treadmill. The cameras installed at distance of 2 m from treadmill recorded the sways of the hip and ankle joints for 5 s after imposing perturbation; the recorded information was, then, analyzed, using Cortex software. Every subject did each movement in triple time, and the mean of these repeated movements was evaluated to calculate parameters and study variables. Thirty seconds was considered for the rest between each repetition.
In the last stage, the recorded information in the software was extracted as a file in Excel format, and it was studied further for calculating the kinematic changes in the range of motion of ankle and hip. The subjects were secured with a supporting belt hanged from the roof to the middle of treadmill. The above-mentioned perturbations (anterior-posterior perturbations) are studied in different positions.
The above perturbations (anterior and posterior perturbation) were performed in 4 different sensory states, each representing a test as follows:
State 1. reference state or applying perturbations without sensory interference; state 2. applying perturbations simultaneously with interfering vestibular and vision system; state 3. applying perturbations simultaneously with interfering vision and proprioception; state 4. applying perturbations simultaneously with interfering the vestibular system and proprioception
It is worth noting that in state 1, no manipulation of vestibular, vision systems, and proprioception was conducted. In state 2, the vestibular system (head hyperextension motions) and the vision system (closing eyes using a blindfold) were disrupted, and only sensory data were received without the disorder. In state 3, the somatosensory system data (putting foam under the subject’s feet) and vision were disrupted, and the dominant system for restoring the balance was the vestibular system. Finally, in state 4, the somatosensory and vestibular data systems were disrupted, and vision system data was used to restore balance.
The descriptive statistics were used to present the characteristics of the subjects, as well as the research variables. The Independent t-test was used to compare the scores of the subjects in the two groups. All statistical tests had a 95% confidence interval, and the alpha was smaller than or equal to 0.05, using SPSS V. 24.
3. Results
Table 1 presents the characteristics related to age, height, weight, and body mass index (BMI) of subjects. The results show no significant difference between age, height, weight, and BMI of the groups, and the groups were homogeneous in these variables.
The following tables present information related to the swings of the ankle and hip joints in different states in the group after the anterior-posterior and posterior-anterior perturbations. To assess the superiority of each ankle or hip strategy in subjects, the ratio of was used, i.e. the higher the ratio, the more support on hip strategy, and smaller values suggest more use of ankle strategy to restore balance.
Based on the analysis of the results, the mean of hip and ankle swings in different states except for the first one was significantly higher in the deaf group compared to the healthy group both in the anterior-posterior perturbations and the posterior-anterior perturbations (P<0.05). However, there was no significant difference between the ratios of hip-to-ankle swings (the dominant strategy for balance recovery) in all states except for the third state (P>0.05).
In state 1, there was no significant difference between the hip and ankle swings in the two groups; however, the number of swings in the joints was higher in response to anterior-posterior and posterior-anterior perturbations in the deaf persons than in the healthy subjects (Table 2).
The results also indicated no significant difference between the hip-to-ankle swing ratios and for balance recovery in both groups. Also, in the anterior-posterior perturbation and posterior-anterior perturbations, ankle strategy was the dominant strategy (based on statistical results if the ratio is less than 1, the dominant strategy is the ankle strategy). In this state, the swings of the joints were lower than those of the other states. In state 2, despite differences in joint swings of the hip and ankle between two groups, there was no significant difference between the hip/ankle ratio in the two groups, and the dominant strategy for the balance recovery in both groups was the ankle strategy (Table 3).
In the state 3, there was a significant difference between the hip and ankle joint swings in the subjects, as well as the hip/ankle ratio to the two groups, and the results indicated that the support of the individuals on the hip swings increased for restoring the balance. In this state, the hip/ankle ratio swings were higher than the other three states (Table 4). In the state 4, despite the difference in hip and ankle swings between the two groups, there was no significant difference in the hip/ankle ratio to the two groups, and the dominant strategy for the balance recovery in both groups was the ankle strategy (Table 5).
4. Discussion
Maintaining and restoring body balance depends on the accurate and precise information sent to the central nervous system by the visual, somatosensory, and vestibular systems. These systems inform the central nervous system of the state and movements of various organs in the body. After processing this information, they send the required motion command to the involved muscles.
Previous research has shown that sensory information related to the posture is multiple, and visual, somatosensory, and vestibular systems comprise the most important ones. In certain circumstances, the role of one of them may be more prominent. For instance, in the darkness, the role of other senses other than vision becomes more important. In other words, these systems overlap, meaning that if the information of one of the systems is incomplete, the central nervous system issues the necessary command, using the information of the other two systems.
In the present study, the data of two other sensory systems were disrupted to obtain the efficiency of each system in balancing the recovery. For example, by closing the eyes and hypertension of the head, the central nervous system will have its support to restore balance by the information obtained from sensory receptors [7, 14].
The results of this study indicated that in the first state (reference state), where there was no manipulation in the vestibular, vision, and proprioception systems, the rate of hip/ankle joints swing in response to anterior-posterior and posterior-anterior perturbations was more common in the deaf group than the healthy people, but there was no significant difference between the two groups.
In state 2, with disrupted vestibular and vision systems and proper somatosensory data, there was a substantial difference between the two groups in the rates of hip/ankle joints swings. In state 3, with the impaired somatosensory and vision system data and where the dominant system for retrieving the balance was the vestibular system, there was a significant difference between the two groups in the rate of hip and ankle joint swings and the individuals’ support to hip swings increased for restoring balance.
Eventually, in state 4, when the somatosensory and vestibular systems were disrupted, and visual data were used to restore balance, there was a significant difference between the two groups in the number of joint swings. The degree of swing in the first state existing in all 3 sensory systems is lower than the other states. In the third state, with disrupted vision and proprioception and the vestibular system as the dominant system to restore balance, the swings were more than other states. In general, in all states, the amount of hip/ankle swings of the deaf group was higher than the healthy subjects.
These results were consistent with the reports of Malek Abadi Zadeh, Kegel et al. Melo et al. Rine et al. Jafari et al. and Rajendran [14-20]. The above studies reported that damage to the vestibular system had a negative effect on postural control in people with hearing impairment, and postural swings in these individuals are more than healthy people and suffer from a poorer balance, reducing the chances of successful recovery in these individuals. Based on the previous study, it plays an essential role in maintaining and restoring the balance of sensory systems, including the vestibular portion of the inner ear, visual sense, and proprioception. Because of the dependence of the balance system on sensory inputs, if one of the sensory inputs reduces or stops, the swings of the body increases and, as a result, the muscle activity increases to maintain the balance [21, 22].
In general, according to the results obtained from the research, increasing the hip and ankle swings in the deaf group to restore the balance created in the above-mentioned states increases the center of gravity within the base of support and reduces the ability to control the posture of individuals against the disturbances imposed on the body.
The results of the present study also indicated that in all states, except for the third state, where the vestibular system was the dominant system for balance recovery, there was no significant difference between the two groups in hip and ankle ratios. Generally, the mean swing ratio in the healthy group was less than the deaf group. Also, the mean swings of the joints studied were lower in the first state and higher in the third state compared to the other states. Also, the strategy used to restore balance in all states in both groups was the ankle strategy, except for the third state, where the subjects in both healthy and the deaf groups had greater support on hip swings to restore balance. These subjects should use one of the visual, sensory, and vestibular systems to restore balance. According to a research report on the balance of the deaf persons, they can perform equilibrium activities without any problem in spite of a malfunction in the vestibular data in the absence of impairment in the visual and sensory system data [13, 23-25].
In the present study, the subjects indicated higher swings in the absence of interference in the systems and lower swings and showed more swings when the vestibular system was dominant. By investigating the vestibular and motor skills in children with hearing impairment, Horak et al. found that children with hearing impairment had a defect in the vestibular system and had a problem when the vestibular system data were the only sensory source available. In deaf people, compensatory mechanisms have grown in response to vestibular defects. It is likely that in the event of visual or somatosensory impairment, i.e. damage to compensatory mechanisms, there will be signs of a disorder in balance performance.
Based on the results of this study, when the vision system was the dominant system for balance recovery, the rate of swing and the ratio of the hip to ankle swings in healthy people were lower compared to the situation, where the somatosensory system was dominant. However, in deaf people, when the somatosensory system was the dominant system for balance recovery, the rate of swings and the ratio of hip to ankle decreased compared to the situation, where the vision system was dominant, probably emphasizing the role of the somatosensory system in restoring the balance of the deaf group. Preserving the body posture depends on interacting with the visual, vestibular, and somatosensory systems [23]. In a study on balance, Assaiante et al. found that in healthy people, the vision system plays a key role before the age of seven.
At age seven, the role of the vision system is negligible, but after the age nine, the role of vision becomes more essential again [25]. Moreover, Bardy and Laurent stated that when tasks for non-athletic subjects gradually become more complicated, the role of vision is emphasized in their postural control [26]. This point is significant in the balance and vision topics, with approximately 20% of the neural fibers of the eyes associated with the vestibular system, and vision problems are sometimes owing to vestibular disorders [27].
The sudden spins of the head occur because of the semicircular duct signals causing the same amount of eye rotation but in the opposite direction of the head rotation. This is because of the reflexes are directed to the oculomotor nuclei through the vestibular nuclei and the median longitudinal nucleus [1]. Consequently, we observe that vestibular system is vital to gaze stabilization (gazing ability). Hence, damage to the vestibular system causes impairment in balance and gazing performance [28].
Since congenital deaf people are weak and defective in the vestibular system and, as stated, the vestibular system data are vital for gaze stabilization, the visual system efficiency of them is lower than that of the healthy people and this factor may reduce the efficiency of the visual system compared to the somatosensory system in the deaf group [1]. In this regard, the results of Khanna’s research shows that in normal conditions, the individual relies more on his somatosensory system to correct body swings rather than the visual inputs [29]. In addition, Szymczyk expresses that the proprioception and skin receptors are sufficient in the deaf group to the extent that they can compensate for any interference in receiving other data from the sensory systems controlling the balance [13].
In general, the results of the present study indicated that in the absence of manipulation of vestibular, vision, and proprioception systems, the swing rates of the hip and ankle joints were lower, and both the deaf and healthy groups used ankle strategy to restore balance. Moreover, by creating disorder in sending sensory impulses from feedback resources to the central nervous system to restore the balance, more improper correction commands were created resulting in higher hip and ankle swings [30].
By and large, the deaf people, in the face of sensory disturbances and immediate perturbations, are more likely to rely on body somatosensory systems to restore balance as a superior equilibrium system. In this regard, the roles of the visual and the vestibular systems are in the next priorities, while healthy people rely primarily on vision system information to regain balance as the supreme balance system. In other words, they rely on the visual system and, then, on the vestibular system.
The results of this study can be used to design deaf rehabilitation programs. The results indicate that muscular neural training that improves the somatosensory system may have more effect on improving the balance of deaf persons. Therefore, such exercises are suggested to be considered more in sports programs and rehabilitation of deaf people to prevent them from falling by providing the necessary measures to improve the balance power and control the body posture to restore balance.
Ethical Considerations
Compliance with ethical guidelines
The Ethics Committee of Kerman University of Medical Sciences approved the study (IR.KMU.REC.1395.351). Iranian Registry of Clinical Trials: IRCT2017022132705N1.
Funding
The present paper was extracted from PhD. thesis of the second author, Department of Sport Injuries and Corrective movements, Faculty of Physical Education, Shahid Bahonar University of Kerman, Kerman, Iran.
Authors' contributions
Conceptualization, methodology, and investigation: All authors; Writing-original draft: Asma Salari; Writing-review & editing: Mansour Sahebozamani, Abdolhamid Daneshjoo and Fatemeh Karimi Afshar; Funding acquisition and resources: All authors; Supervision: Asma Salari.
Conflict of interests
The authors declared no conflict of interest
References
- Seyedi M, Seidi F, Rahimi A, Minoonejad H. [An Investigation of the efficiency of sensory systems involved in postural control in deaf athletes and non-athletes (Persian)]. Sport Medicine (Harakat). 2015; 7(1):111-27.
- Firouzbakht M, Eftekhar Ardebili H, Majlesi F, Rahimi A, Ansari Dezfooli M, Esmailzadeh M. [Prevalence of neonatal hearing impairment in province capitals (Persian)]. Journal of School of Public Health and Institute of Public Health Research. 2008; 5(4):1-9.
- Farzaneh Hessari A, Daneshmandi H, Mahdavi S. [The effect of 8 weeks core stabilization training program on balance in deaf students (Persian)]. Sport Medicine (Harakat). 2012; (7):67-83.
- Khodashenas E, Moradi H, Asadi Ghaleni M, Heydari E, Shams A, Enayati A, et al. [The effect of selective training program on the static and dynamic balance of deaf children (Persian)]. medical journal of mashhad university of medical sciences. 2017; 60(1):383-91.
- Najafi fard A, Hemayat Talab R, Sheikh M. The effect of eight-week period of rebound therapy exercises on the balance of male students with hearing disabilities. International Journal of Sport Studies. 2015; 5(11):1206-11.
- Valizade A, Rezazade F, Aali Sh, Mustafazadeh A. [Comparison of static balance among blind, deaf and normal children in different conditions (Persian)]. Archives of Rehabilitation. 2014; 14(4):106-12.
- Wojtkowski M. [Balance disorders in hearing impaired children (Polish)]. Otolaryngologia polska. 2000; 54(2):215-6. [PMID]
- Maki BE, McIlroy WE. The role of limb movements in maintaining upright stance: the “change-in-support” strategy. Physical therapy. 1997; 77(5):488-507. [DOI:10.1093/ptj/77.5.488] [PMID]
- Beyranvand R, Sahebazzamani M, Daneshjoo AH. [The effect of hyperkyphosis on balance recovery strategy of young and old people in response to sudden perturbations (Persian)]. Daneshvar Medicine. 2017; 24(130):37-47.
- the Vestibular Disorders Association, Watson MA, Owen Black F. The human balance system: A complex coordination of central and peripheral systems [Internet]. 2008 [Updated 2019 September 30]. available from: http://vestibular.org/sites/default/files/page_files/Human%20Balance%20System_0.pdf
- Mohammadtaghi B, Hejazi Dinan p. [Effects of manipulating visual, auditory and proprioceptive sensory in formations on the balance in healthy subjects and lower limb amputees (Persian)]. Journal of Shahrekord Uuniversity of Medical Sciences. 2016; 18(5):115-27.
- An MH, Yi CH, Jeon HS, Park SY. Age-related changes of single-limb standing balance in children with and without deafness. International journal of pediatric otorhinolaryngology. 2009; 73(11):1539-44. [DOI:10.1016/j.ijporl.2009.07.020] [PMID]
- Szymczyk D, Drużbicki M, Dudek J, Szczepanik M, Snela S. Balance and postural stability in football players with hearing impairment. Young Sport Science of Ukraine. 2012; 16(3):258-63.
- Rajendran V, Roy FG, Jeevanantham D. Postural control, motor skills, and health-related quality of life in children with hearing impairment: a systematic review. European Archives of Oto-Rhino-Laryngology. 2012; 269(4):1063-71. [DOI:10.1007/s00405-011-1815-4] [PMID]
- Jafari Z, Malayeri S, Rezazadeh N, Haji Heydari F. [Static and dynamic balance in congenital severe to profound hearing-impaired children (Persian)]. Audiology. 2011; 20(2):102-12.
- de Souza Melo R, dos Santos Marinho SE, Araújo Freire ME, Arruda Souza R, Melo Damasceno HA, Falcão Raposo MC. Static and dynamic balance of children and adolescents with sensorineural hearing loss. Einstein (São Paulo). 2017; 15(3):262-8. [DOI:10.1590/s1679-45082017ao3976] [PMID] [PMCID]
- Braswell J, Rine RM. Preliminary evidence of improved gaze stability following exercise in two children with vestibular hypofunction. International journal of pediatric otorhinolaryngology. 2006; 70(11):1967-73. [DOI:10.1016/j.ijporl.2006.06.010] [PMID]
- De Kegel A, Dhooge I, Peersman W, Rijckaert J, Baetens T, Cambier D, et al. Construct validity of the assessment of balance in children who are developing typically and in children with hearing impairments. Physical therapy. 2010; 90(12):1783-94. [DOI:10.2522/ptj.20100080] [PMID]
- Knudtson A, Todd T, Jung T, Furtado O, Wagatsuma M, Kim Y. Comparison of balance between young adults with and without hearing impairment. Medicine & Science in Sports & Exercise. 2016; 48(5S):401. [DOI:10.1249/01.mss.0000486210.78238.f0]
- Malekabadizadeh Z, Barati AH, Khorashadizadeh M. The effect of hearing impairment and intellectual disability on children’s static and dynamic balance. Auditory and Vestibular Research. 2016; 25(2):82-8.
- Bolger D, Ting LH, Sawers A. Individuals with transtibial limb loss use interlimb force asymmetries to maintain multi-directional reactive balance control. Clinical Biomechanics. 2014; 29(9):1039-47. [DOI:10.1016/j.clinbiomech.2014.08.007] [PMID] [PMCID]
- Barnett CT, Vanicek N, Polman R. Postural responses during volitional and perturbed dynamic balance tasks in new lower limb amputees: a longitudinal study. Gait & posture. 2013; 37(3):319-25. [DOI:10.1016/j.gaitpost.2012.07.023] [PMID]
- Suarez H, Angeli S, Suarez A, Rosales B, Carrera X, Alonso R. Balance sensory organization in children with profound hearing loss and cochlear implants. International journal of pediatric otorhinolaryngology. 2007; 71(4):629-37. [DOI:10.1016/j.ijporl.2006.12.014] [PMID]
- Horak FB, Shumway-Cook A, Crowe TK, Owen Black F. Vestibular function and motor proficiency of children with impaired hearing, or with learning disability and motor impairments. Developmental Medicine & Child Neurology. 1988; 30(1):64-79. [DOI:10.1111/j.1469-8749.1988.tb04727.x] [PMID]
- Assaiante C, Amblard B. An ontogenetic model for the sensorimotor organization of balance control in humans. Human Movement Science. 1995; 14(1):13-43. [DOI:10.1016/0167-9457(94)00048-J]
- Bardy BG, Laurent M. How is body orientation controlled during somersaulting? Journal of Experimental Psychology: Human Perception and Performance. 1998; 24(3):963-77. [DOI:10.1037//0096-1523.24.3.963] [PMID]
- Shokrollahzadeh F, Mirzajani A. [The role of vision on the body balance (Persian)]. Journal of Modern Rehabilitation. 2015; 9(2):1-7.
- Rine RM. Growing evidence for balance and vestibular problems in children. Audiological medicine. 2009; 7(3):138-42. [DOI:10.1080/16513860903181447]
- Khanna P, Kapoor G, Zutshi K. Balance deficits and recovery timeline after different fatigue protocols. Indian Journal of Physiotherapy and Occupational Therapy-An International Journal. 2008; 2(3):42-54.
- Kiyani P, Farahpoor N. [Evaluation of performance of the vestibular proprioception and vision systems on postural control of old men (Persian)]. Iranian Journal of Ageing. 2015; 10(3):44-53.
Type of Study: Research |
Subject:
Special
Received: 2019/05/7 | Accepted: 2019/07/6 | Published: 2019/11/12
Received: 2019/05/7 | Accepted: 2019/07/6 | Published: 2019/11/12
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |