BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://ptj.uswr.ac.ir/article-1-269-en.html
2- Department of Technical Orthopedic, Faculty of Rehabilitation Sciences, Isfahan University of Medical Sciences, Isfahan, Iran.
1. Introduction
Stroke is claimed to be the third main cause of death and disabilities in the world [1, 2]. Hemiparesis is the main symptom of the stroke [1, 2] that finally affects the patients’ abilities in standing and walking [3-5]. These patients suffer from impairment in static and dynamic balance [6] and have a high records of falling [3-5]. Stability in standing and walking is controlled by musculoskeletal, somatosensory, and vestibular systems [7-10]. Based on the results of various studies, stroke subjects are unable to control their standing balance and are at risk of falling [6, 11, 12].
Therefore, various therapeutic interventions, such as physical therapy, Kinesio tape, and assistive technology have been recommended to improve their balance during standing and walking [13, 14]. Kinesio Taping (KT) technique was introduced by Kase in 1973 as a therapeutic tape and taping technique to support the joints and muscles without restricting their range of motion [15]. KT is based on three important concepts; space, movement, and cooling. The major functions of KT based on Kase theory include supporting muscles, removing body fluids congestion, activating endogenous analgesic system, and correcting joint problems [15].
This method is currently used to improve the standing stability of the subjects with various musculoskeletal and neurological disorders. In this regard, two theories discuss the effects of KT administration on stability. Based on the first theory, KT affects the structural stiffness of the joints and acts as a mechanism of postural control [16]. According to the second theory, KT constantly stretches the entire skin of the leg, which rises proprioception and accordingly sensory inputs to central nerve system [15, 17]. The sensory inputs can be used by central nervous system to improve standing and postural control (feed forward active control mechanism) [18].
In 2011, Cortesi investigated the effect of gastrocnemius muscles KT on standing stability of the subjects with Multiple Sclerosis (MS) disorders [18]. The results of the research showed that gastrocnemius KT decreased centre of pressure (CoP) sways during quiet standing [19]. It is also effective for achieving the maximal response of motor units through increase in coordination [20].
The effects of KT with Botox injection on spasticity of tibialis posterior muscle was also reported in the literature. Based on these studies, the level of spasticity decreases significantly [21].
Due to high risk of falling in the subjects with stroke, it is important to use various treatments to increase their standing stability. This study aimed to investigate the effects of gastrocnemius muscles KT on the stability of stroke subjects during quiet standing. This study is mainly based on the hypothesis that KT improves standing stability of stroke subjects.
2. Materials and Methods
This was a clinical trial study, in which a total of 22 stroke subjects (11 with disability in the right side of the body and 11 in the left side of the body) in chronic phase were recruited. The main inclusion criteria were as follows: having stroke accident for the first time [22], within 6 months after injury [23], the stroke caused by medial carotid artery, Ability to stand for at least 1 minute without any assistive devise [24, 25], ability to walk for at least 10 meters [21, 26, 27], and having Modified Modified Ashworth Scale (MMAS) less than 4 and equal or more 1 [26].
Ethics Committee of Isfahan University of Medical Sciences approved the study. A consent form was signed by each participant before data collection. The subjects were divided into patients with right-sided stroke and left-sided stroke.
Study procedure
The subjects’ stability was evaluated during static and dynamic conditions. The static stability was assessed during quiet standing on a force plate [28, 29]. Dynamic stability was evaluated by time up and go test (TUG) [18].
A Kistler force plate (50×60cm) was used to evaluate the stability during quiet standing. The subjects were asked to stand on the force plate for 1 minute in a comfortable position. They gazed at a point 2 m from the force plate. The force plate data were collected with a frequency of 100 Hz. Then, the obtained data were filtered with Butterworth low pass filter with a cut off frequency of 10 Hz. The first and last 15 seconds of the data were deleted to remove the effects of sudden standing on the force plate and muscles fatigue. The tests were repeated to collect 5 successful trials. It should be mentioned that high degree of repeatability of the stability parameters can be achieved if the mean values of 5 trials be used for final analysis [24, 25].
Time up and go test
It is the time a person takes to rise from a chair, walk 3 meters, turn around, walk back to the chair and sit down [30-32]. A chronometer was used to record the time of the test. Some variables such as centre of pressure (CoP) excursions in both mediolateral (ML) and anteroposterior (AP) directions (CoPEAP, CoPEML); path length of centre of pressure in both planes of AP (PLAP) and ML (PLML), velocity of CoP in both planes of AP (VAP) and ML (VML) were used based on the following equations. X and Y are the CoP in anteroposterior and mediolateral directions, respectively.
Cop eap(mm)=Xmax-Xmin
COP EML(mm)=Ymax-Ymin
The spasticity of lower extremity musculatures was evaluated by use of Modified Modified Ashworth Scale, which is considered a valid clinical measurement to grade spasticity [15]. This includes mobilization of each joint to reach a clinician-based assessment with ordinal outcome. The obtained score ranges from 0=no increase in tone to 4=limb rigid in flexion or extension
In the next step, KT with inhibitive technique was attached to gastrocnemius muscles based on the technique recommended by interventional KT association [33]. The KT used in this study was manufactured by ARES Company (5×5 dimensions). The same procedure was used to collect the data, immediately after using KT, and then one hour later.
Statistical analysis
The mean values of the aforementioned parameters were calculated for each subject. The normal distribution of the parameters was evaluated by Shapiro-Wilk test. Because of normal distribution of the parameters, the effects of taping were evaluated by performing repeated measure of analysis of variance with Minitab software (v. 17) [34].
3. Results
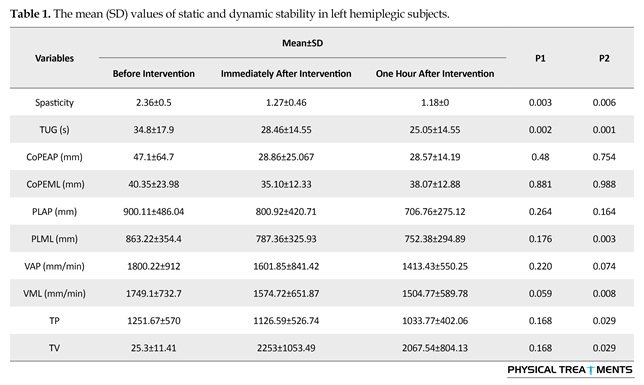
The results of stability analysis of stroke subjects with hemiplegia in left and right sides are shown in Tables 1 and 2, respectively. The mean values of TUG test of stroke subjects with symptoms in right side were 18.26±5.05, 15.54±3.83, and 14.05±4.59 seconds for first (before taping), second (immediately after taping), and third (one hour after taping) conditions, respectively (the difference between group conditions was significant (P<0.05). The mean value of CoP in anteroposterior direction in this group of subjects was 34.82±26.49 mm compared to 31.1±18.23 mm when KT was used (P=0.296). Although the mean value of the most stability parameters in both ML and AP directions decreased one hour after KT usage, the differences were not significant (P>0.05).
The mean value of spasticity of lower extremity musculatures test of stroke subjects with symptoms in left side were 2.36, 1.27 and 1.18 for first (before taping), second (immediately after taping) and third (one hour after taping) conditions, respectively. The difference between group conditions was significant (P<0.05). The mean value of spasticity of lower extremity musculatures test of stroke subjects with symptoms in the right side were 2.45 , 1.54, and 1.18 for first (before taping), second (immediately after taping), and third (one hour after taping) conditions, respectively. The difference between group conditions was significant (P<0.05). However, the differences between right-sided and left-sided stroke patients were not significant (P>0.05).
The stroke subjects with hemiplegic symptom in the left side of the body show significant improvement in dynamic stability (based on TUG test) following the use of KT and one hour later (P<0.05). Although the excursion of CoP in AP and ML directions decreased following use of KT, the difference was not significant. The effect of KT on standing stability one hour after use was significantly more than that in group without taping or immediately after KT usage.
4. Discussion
The performance of the subjects with stroke differs significantly from that of normal subjects. Various treatments have been used to restore the subjects’ abilities during standing and walking. KT is one of the methods used in this regard [35, 36]. There is not enough evidence on the effect of gastrocnemius taping on stability performance of the stroke subjects. Therefore, this study aimed to evaluate the effects of KT on dynamic and static performance of stroke subjects.
The result of this study showed that the dynamic stability of two groups of subjects improved significantly,
TUG: Time Up and Go; CoPEAP: Center of Pressure Excursion in Anteroposterior direction; CoPEML: Center of Pressure Excursion in Mediolateral direction; PLAP: Path Length of center of pressure in Anteroposterior direction; PLML: Path Length of center of pressure in Mediolateral direction; VAP: Velocity of center of pressure in Anteroposterior direction; VML: Velocity of center of pressure in Mediolateral direction; TP: Total Path length of center of pressure; TV: Total path length of center of pressure Velocity
especially one hour after using KT. However, it seems that dynamic stability of stroke subjects with impairment in the left side is less than that with impairment in the right side, which may be due to the time of involvement (the mean value of time of involvement was 32.18 and 12.45 months for the left side and right side, respectively). Administration of KT decreased the CoP sway in the subjects with left side involved and the difference was significant. However, the stability of stroke subjects with disability in the right side of the body did not significantly improve one hour after KT. The main reason for dynamic stability could be the effects of KT on ankle joint plantar flexor spasticity. Following the use of KT, the spasticity of gastrocnemius decreased which led to increase in ankle joint dorsiflexion motion. Based on the results of previous studies, dynamic stability based on TUG test depends on spasticity of ankle plantar flexor and range of dorsiflexion motion [21, 37-39]. Therefore, the dynamic stability of both subjects improved due to decrease in spasticity of plantar flexor muscles.
Another interesting study result was related to static stability of the subjects with left-sided hemiplegia who were improved more than that of the subjects with disability in the right side. The main reason may be due to more instability of the left hemiplegic subjects compared to right hemiplegic subjects. As they were more unstable, the effect of taping on this group of the subjects may be more than that of right hemiplegic subjects. It was also showed that in previous studies, left hemiplegic subjects showed greater sway area and lateral displacement compared to right hemiplegic subjects.
This study has some limitations too. The main limitation relates to different follow up time after injury which were different between left and right hemiplegic subjects. However, only the effect immediately after using KT and then one hour after were evaluated. Therefore, it is recommended that the effects of KT be evaluated after some period of use.
Acknowledgements
The study was approved by the Clinical Research Council of Isfahan University of Medical Sciences. We thank our colleagues from Isfahan University of Medical Sciences and the Vice-Chancellery for Research for financial supporting this research.
Conflict of Interest
The author declared no Conflicts of interest.
Reference
[1]World Health Organization. WHO handbook for reporting results of cancer treatment. Geneva: World Health Organization; 1979.
[2]Warlow C, Van Gijn J, Dennis M, Wardlaw J, Bamford J, Hankey G, et al. Is it a vascular event and where is the lesion: Identifying and interpreting the symptoms and signs of cerebrovascular disease. In: Warlow C, Van Gijn J, Dennis M, Wardlaw J, Bamford J, Hankey G, et al., editors. Stroke: Practical Management; 2008. doi: /10.1002/9780470696361.ch3
[3]Geurts ACH, de Haart M, van Nes IJW, Duysens J. A review of standing balance recovery from stroke. Gait & Posture. 2005; 22(3):267–81. doi: 10.1016/j.gaitpost.2004.10.002
[4]Kenneth N. K. Fong, Chetwyn C. H. C. Relationship of motor and cognitive abilities to functional performance in stroke rehabilitation. Brain Injury. 2001; 15(5):443–53. doi: 10.1080/02699050118772
[5]Keenan MA, Perry J, Jordan C. Factors affecting balance and ambulation following stroke. Clinical Orthopaedics and Related Research. 1984; 182:165-71. doi: 10.1097/00003086-198401000-00021
[6]Carr J, Shepherd RB. Neurological rehabilitation: optimizing motor performance. Auckland: Butterworth-Heinemann; 1998.
[7]Fitzpatrick R, Rogers DK, McCloskey DI. Stable human standing with lower-limb muscle afferents providing the only sensory input. The Journal of Physiology. 1994; 480(2):395–403. doi: 10.1113/jphysiol.1994.sp020369
[8]Marigold DS, Eng JJ, Tokuno CD, Donnelly CA. Contribution of muscle strength and integration of afferent input to postural instability in persons with stroke. Neurorehabilitation and Neural Repair. 2004; 18(4):222–9. doi: 10.1177/1545968304271171
[9]Smania N, Picelli A, Gandolfi M, Fiaschi A, Tinazzi M. Rehabilitation of sensorimotor integration deficits in balance impairment of patients with stroke hemiparesis: A before/after pilot study. Neurological Sciences. 2008; 29(5):313–9. doi: 10.1007/s10072-008-0988-0
[10]Lukács M. Electrophysiological signs of changes in motor units after ischaemic stroke. Clinical Neurophysiology. 2005; 116(7):1566–70. doi: 10.1016/j.clinph.2005.04.005
[11]Dean CM, Richards CL, Malouin F. Task-related circuit training improves performance of locomotor tasks in chronic stroke: A randomized, controlled pilot trial. Archives of Physical Medicine and Rehabilitation. 2000; 81(4):409–17. doi: 10.1053/mr.2000.3839
[12]Shepherd RB. Exercise and training to optimize functional motor performance in stroke: Driving neural reorganization. Neural Plasticity. 2001; 8(1-2):121–9. doi: 10.1155/np.2001.121
[13]Karadag-Saygi E, Cubukcu-Aydoseli K, Kablan N, Ofluoglu D. The role of kinesiotaping combined with botulinum toxin to reduce plantar flexors spasticity after stroke. Topics in Stroke Rehabilitation. 2010; 17(4):318–22. doi: 10.1310/tsr1704-318
[14]Lazarus C. The use of kinesio tape for the treatment of foot drop in a patient with sub-acute stroke: A case report [PhD dissertation]. Florida: Florida Gulf Coast University; 2013.
[15]Kase K, Tatsuyuki H, Tomoko O. Kinesio taping perfect manual. Mississippi: Kinesio Taping Association; 1996.
[16]Haselkorn JK, Loomis S. Multiple sclerosis and spasticity. Physical Medicine and Rehabilitation Clinics of North America. 2005; 16(2):467–81. doi: 10.1016/j.pmr.2005.01.006
[17]Kase K, Wallis J, Kase T. Clinical therapeutic applications of the kinesio taping method. Mississippi: Kinesio Taping Association; 2003.
[18]Cortesi M, Cattaneo D, Jonsdottir J. Effect of kinesio taping on standing balance in subjects with multiple sclerosis: A pilot study m {1}. NeuroRehabilitation. 2011; 28(4):365-72. doi: 10.3233/NRE-2011-0665.
[19]Klein DA, Stone WJ, Phillips WT, Gangi J, Hartman S. PNF training and physical function in assisted-living older adults. Journal of Aging and Physical Activity. 2002; 10(4):476–88. doi: 10.1123/japa.10.4.476
[20]Bae SS. An introduction to physical therapy. 5th ed. Seoul: Daihaks Publishing; 2003.
[21]Reiter F, Danni M, Lagalla G, Ceravolo G, Provinciali L. Low-dose botulinum toxin with ankle taping for the treatment of spastic equinovarus foot after stroke. Archives of Physical Medicine and Rehabilitation. 1998; 79(5):532–5. doi: 10.1016/s0003-9993(98)90068-5
[22]Kadabi N. Effectiveness of 4 weeks task specific training in improving postural control & balance in subacute & chronic stroke patients: A randomized controllled trial [PhD dissertation]. Belgaum: KLE University; 2011.
[23]Penta M, Tesio L, Arnould C, Zancan A, Thonnard JL. The ABILHAND questionnaire as a measure of manual ability in chronic stroke patients: Rasch-Based validation and relationship to upper limb impairment. Stroke. 2001; 32(7):1627–34. doi: 10.1161/01.str.32.7.1627
[24]Lafond D, Corriveau H, Hébert R, Prince F. Intrasession reliability of center of pressure measures of postural steadiness in healthy elderly people. Archives of Physical Medicine and Rehabilitation. 2004; 85(6):896–901. doi: 10.1016/j.apmr.2003.08.089
[25]Santos BR, Delisle A, Larivière C, Plamondon A, Imbeau D. Reliability of centre of pressure summary measures of postural steadiness in healthy young adults. Gait & Posture. 2008; 27(3):408–15. doi: 10.1016/j.gaitpost.2007.05.008
[26]Karadag-Saygi E, Cubukcu-Aydoseli K, Kablan N, Ofluoglu D. The role of kinesiotaping combined with botulinum toxin to reduce plantar flexors spasticity after stroke. Topics in Stroke Rehabilitation. 2010; 17(4):318–22. doi: 10.1310/tsr1704-318
[27]Kaur J, Kumar A. Effect of task-specific training on gait parameters in hemiparetic stroke patients. Indian Journal of Physical Medicine and Rehabilitation. 2009; 20(1):23-6.
[28]Chiari L, Cappello A, Lenzi D, Della Croce U. An improved technique for the extraction of stochastic parameters from stabilograms. Gait & Posture. 2000; 12(3):225–34. doi: 10.1016/s0966-6362(00)00086-2
[29]Prieto TE, Myklebust JB, Hoffmann RG, Lovett EG, Myklebust BM. Measures of postural steadiness: Differences between healthy young and elderly adults. IEEE Transactions on Biomedical Engineering. 1996; 43(9):956–66. doi: 10.1109/10.532130
[30]Lundin-Olsson L, Nyberg L, Gustafson Y. Attention, frailty, and falls: The effect of a manual task on basic mobility. Journal of the American Geriatrics Society. 1998; 46(6):758–61. doi: 10.1111/j.1532-5415.1998.tb03813.x
[31]Podsiadlo D, Richardson S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. Journal of the American Geriatrics Society. 1991; 39(2):142–8. doi: 10.1111/j.1532-5415.1991.tb01616.x
[32]Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go test. Physical therapy. 2000; 80(9):896-903. PMID: 10960937
[33]Kase K, Wallis J, Kase T. Clinical therapeutic applications of the kinesio taping method. Alberquerque: Universal Printing & Publishing Inc.; 2003.
[34]Fitzpatrick JJ, Wallace M. Encyclopedia of nursing research. New York: Springer; 2006.
[35]Baek YH, Seo JC, Lee JD. The effect of taping on the activity of daily living lf poststroke-hemiplegic: A clinical study. Journal of Korean Acupuncture and Moxibustion Society. 2001; 18:175-85.
[36]Kim KS, Seo HM, Lee HD. Effect of taping method on ADL, range of motion, hand function & quality of life in post-stroke patients for 5 weeks. The Korean Journal of Rehabilitation Nursing. 2002; 5(1):7-17.
[37]Ryerson SD. The foot in hemiplegia. Physical Therapy of the Foot and Ankle. New York: Churchill-Livingstone; 1988.
[38]Booth BJ, Doyle M, Montgomery J. Serial casting for the management of spasticity in the head-injured adult. Physical Therapy. 1983; 63(12):1960–6. doi: 10.1093/ptj/63.12.1960
[39]Ng SSM, Shepherd RB. Weakness in patients with stroke: Implications for strength training in neurorehabilitation. Physical Therapy Reviews. Informa UK Limited; 2000; 5(4):227–38. doi: 10.1179/108331900786166650
Received: 2016/06/11 | Accepted: 2016/09/2 | Published: 2016/10/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |