Wed, Apr 24, 2024
Volume 7, Issue 3 (Autumn 2017)
PTJ 2017, 7(3): 185-192 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Alizadeh M H, Shahab A, Minonetzhad H, Rajabi R. Studying the Predictive Power of Common FIFA Pre-Season Medical Assessments and Functional Tests With the Rate and Severity of Injuries to Elite Football Players. PTJ 2017; 7 (3) :185-192
URL: http://ptj.uswr.ac.ir/article-1-348-en.html
URL: http://ptj.uswr.ac.ir/article-1-348-en.html
1- Department of Sport Mediciane and Health, Faculty of Physical Education and Sport Scienses, University of Tehran, Tehran, Iran.
2- Department of Sport Mediciane and Health, Faculty of Physical Education and Sport Scienses, Alborz Campus, University of Tehran, Tehran, Iran.
2- Department of Sport Mediciane and Health, Faculty of Physical Education and Sport Scienses, Alborz Campus, University of Tehran, Tehran, Iran.
Full-Text [PDF 646 kb]
(1744 Downloads)
| Abstract (HTML) (5000 Views)
Full-Text: (1780 Views)
1. Introduction
Football is one of the most viewed sports in the world. Recent statistics from Fédération Internationale de Football Association (FIFA) show that the number of people who are currently playing Football has reached 270 million [1]. Football is characterized by intense physical contact as well as short, fast and non-continuous movements, such as acceleration, deceleration, jumps and sudden changes of direction [2, 3].
The incidence of injury among male football players has been estimated as 10 to 35 injuries per 1000 hours of matches. That is, every elite male football player incurs approximately one performance-limiting injury per year [4]. Zarei et al. reported high injury rate among football players in Iranian Pro League (66.8 injuries per 1000 match hours) [5]. Half of these injuries were mild injuries resulting in less than one week of absence and the other half were severe injuries which caused more than 4 weeks of absence from football fields [6]. Jung et al. calculated the annual cost of football injuries in Switzerland as €95 million in 2003 plus a loss of more than 500000 working days [7]. In another study, the estimated direct and indirect costs (medical costs and work absenteeism) of injuries in the Netherlands were €1.3 billion a year [8].
Professional sport teams use general medical assessments and functional tests before the start of season to identify athletes who are susceptible to injuries. Akturk et al. in a study on Dutch active and retired professional football players using medical examinations on cardiovascular, musculoskeletal and neurological systems, recommended improvement and adding to the current medical examinations, especially with regard to the prevention of potential long-term health problems [9]. According to Fuller et al. players with cardiovascular, neurological and musculoskeletal risk factors are more likely to be injured and affected by intense exercise [10]. Hughes et al. in a systematic review, concluded that medical screening tests of professional football players are defective in predicting and preventing injuries [11].
Functional tests such as lower limb Y-Balance Test (YBT), Functional Movement Screen (FMS), and Single-Leg Hop (SLH) have been assessed regarding their ability to predict injury in various sports and different subjects [12-22]. In most studies, lower limb injuries have been reported as the most affected part of body in professional footballers [23]. Balance disturbance is one of the risk factors for increasing the chance of lower limb injury. Gonell et al. suggested that Y-BT can be incorporated into physical examinations to identify football players who are susceptible to injury [21]. Smith et al. also found an association between higher than 4 cm asymmetry in anterior reach for both limbs with increased risk of injury, but they did not find any correlation between the total score of this test with increased risk of injury [15].
About FMS pre-season test, reports indicate that a score of lower than 14 is associated with serious injuries causing time loss and missing training and the next match [12]. Marques et al. [24] reported that young and elite football players (14-20 years) had poor performance in deep squat and trunk stability tests also the asymmetry between right and left body side was high. Duke et al. [25] used FMS test to predict risk of time-loss injury in experienced male rugby ::::union:::: athletes and suggested that FMS could be a proper predictor for time-loss due to injuries. On the other hand, Moran in a systemic review reported that FMS had no association with injury prediction [26].
About SLH test, there are also different results regarding the predictive power of this test. For example, Brumitt et al. reported that female collegiate athletes with a greater than 10% side‐to‐side asymmetry between SLH distances had a 4‐fold increase in ankle injury, but SLH could not predict injuries in the back or lower limb of female student athletes [16]. In literature, no research was found on predicting injury in athletes by Carioca and Co-Contraction Tests. However, based on the study of Brumitt et al. slower performance in Lower Extremity Functional Test (LEFT), which consisted of Carioca Test, made female athletes 6 times more likely to sustain a thigh or knee injury [16]. Lephart et al. in a study on injured athletes who were ready to return to sport activities, showed that these athletes could perform co-contraction and Carioca Tests significantly at shorter time than athletes who were not ready yet.
In light of these results, the mentioned tests are capable of identifying athletes who are prone to injury; however because of conflicting findings, coaches and club medical staff are suspicious about using each test or a combination of them in identifying athletes at risk of injury. Regarding the popularity of football and the high severity and incidence of its injuries as well as the high cost of treatment for football-induced injuries, and their impact on the reduction of players’ performance and the sports clubs’ financial loss, it is necessary to perform a complete evaluation and fully examine the musculoskeletal system (from medical and functional perspective) for predicting the likelihood of injury. In this respect, this study aimed to investigate the common medical and functional tests for their ability to predict the rate and severity of injuries to elite football players in the first mid-season play of 2017-2018.
2. Materials and Methods
The present study is a correlational study, and based on the type of data collection method, it is a prospective and longitudinal study [27]. Study population consists of Iranian elite football players in professional sport clubs. Of them, 97 players were selected from three professional clubs. They were 17-35 years old and had been invited to the national football team. Five of them were excluded from the study because their injuries were not recorded by the club medical staff during the mid-season.
Anthropometric characteristics of subjects were as follows: Mean (SD) weight=77.15(7.72) kg; Mean (SD) height=181(6.23) cm, Mean (SD) age=25.14(14.6) years; and Mean (SD) BMI=22.1(98.66) kg/m2. The physician of each team recorded the injuries sustained throughout the season in the FIFA standard injury report form [28]. These forms were collected weekly by the researcher. The recorded injuries should be sustained in training or during the match, and be in such a state that need medical help (medical staff need to take an action for their treatment) [29, 30].
Functional Movement Screen test
The Functional Movement Screen tests (Figure 1) consist of seven movement tests which are able to detect limits and changes in normal movement patterns. This test was designed to provide interaction between movement chain and the necessary sustainability to implement functional movement patterns. In this test, the seven movement were scored from 1-3 points; if they done properly and without compensation, the subject earns 3 points; if done with some compensatory movements, the given score is 2; and if the subjects could not complete the movements, the given score is 1. The seven movement patterns are: deep squat, hurdle step, in-line lunge, active straight-leg raise, trunk stability push-up, rotary stability, and shoulder mobility [31].
Carioca test
The Carioca Test (Figure 2) requires crossover steps at a total distance of 80 feet (24.38 m). The subjects began moving from left to right, then reversed direction following the first 40-foot (12.19 m) length, thus performing the test moving a total of 80 feet (24.38 m) in the minimum amount of time possible [32]. This test may cause dynamic pivot shift phenomenon in those with Anterior Cruciate Ligament (ACL) injury. Lephart et al. reported high reliability (r=0.92 to 0.96) for this test [32].
Co-contraction test
The Co-Contraction test (Figure 3) was performed by securing the athlete with a heavy 48 inch (121 cm) length of rubber band (Thera band) which was anchored to a metal loop secured on a wall 60 inch (152 cm) above the floor. The band is stretched twice its recoil length and then the subject stands facing the wall with the toes of his/her feet on the semicircle. Then he is asked to complete five wall-to-wall lengths of the 180° semicircle with a radius of 96 inch (243 cm) from the metal loop in the minimum amount of time possible. Each semicircle is considered as one length. The test is repeated three times and then the average time is calculated [32].
This test reproduces the rotational forces at the knee that may cause tibial translation. Proper and timely contraction of the anterior and posterior muscles of the thigh can prevent this tibia subluxation and cause knee stability [33]. Lephart et al. reported high reliability (r=0.92 to 0.96) for this test [32].
Football is one of the most viewed sports in the world. Recent statistics from Fédération Internationale de Football Association (FIFA) show that the number of people who are currently playing Football has reached 270 million [1]. Football is characterized by intense physical contact as well as short, fast and non-continuous movements, such as acceleration, deceleration, jumps and sudden changes of direction [2, 3].
The incidence of injury among male football players has been estimated as 10 to 35 injuries per 1000 hours of matches. That is, every elite male football player incurs approximately one performance-limiting injury per year [4]. Zarei et al. reported high injury rate among football players in Iranian Pro League (66.8 injuries per 1000 match hours) [5]. Half of these injuries were mild injuries resulting in less than one week of absence and the other half were severe injuries which caused more than 4 weeks of absence from football fields [6]. Jung et al. calculated the annual cost of football injuries in Switzerland as €95 million in 2003 plus a loss of more than 500000 working days [7]. In another study, the estimated direct and indirect costs (medical costs and work absenteeism) of injuries in the Netherlands were €1.3 billion a year [8].
Professional sport teams use general medical assessments and functional tests before the start of season to identify athletes who are susceptible to injuries. Akturk et al. in a study on Dutch active and retired professional football players using medical examinations on cardiovascular, musculoskeletal and neurological systems, recommended improvement and adding to the current medical examinations, especially with regard to the prevention of potential long-term health problems [9]. According to Fuller et al. players with cardiovascular, neurological and musculoskeletal risk factors are more likely to be injured and affected by intense exercise [10]. Hughes et al. in a systematic review, concluded that medical screening tests of professional football players are defective in predicting and preventing injuries [11].
Functional tests such as lower limb Y-Balance Test (YBT), Functional Movement Screen (FMS), and Single-Leg Hop (SLH) have been assessed regarding their ability to predict injury in various sports and different subjects [12-22]. In most studies, lower limb injuries have been reported as the most affected part of body in professional footballers [23]. Balance disturbance is one of the risk factors for increasing the chance of lower limb injury. Gonell et al. suggested that Y-BT can be incorporated into physical examinations to identify football players who are susceptible to injury [21]. Smith et al. also found an association between higher than 4 cm asymmetry in anterior reach for both limbs with increased risk of injury, but they did not find any correlation between the total score of this test with increased risk of injury [15].
About FMS pre-season test, reports indicate that a score of lower than 14 is associated with serious injuries causing time loss and missing training and the next match [12]. Marques et al. [24] reported that young and elite football players (14-20 years) had poor performance in deep squat and trunk stability tests also the asymmetry between right and left body side was high. Duke et al. [25] used FMS test to predict risk of time-loss injury in experienced male rugby ::::union:::: athletes and suggested that FMS could be a proper predictor for time-loss due to injuries. On the other hand, Moran in a systemic review reported that FMS had no association with injury prediction [26].
About SLH test, there are also different results regarding the predictive power of this test. For example, Brumitt et al. reported that female collegiate athletes with a greater than 10% side‐to‐side asymmetry between SLH distances had a 4‐fold increase in ankle injury, but SLH could not predict injuries in the back or lower limb of female student athletes [16]. In literature, no research was found on predicting injury in athletes by Carioca and Co-Contraction Tests. However, based on the study of Brumitt et al. slower performance in Lower Extremity Functional Test (LEFT), which consisted of Carioca Test, made female athletes 6 times more likely to sustain a thigh or knee injury [16]. Lephart et al. in a study on injured athletes who were ready to return to sport activities, showed that these athletes could perform co-contraction and Carioca Tests significantly at shorter time than athletes who were not ready yet.
In light of these results, the mentioned tests are capable of identifying athletes who are prone to injury; however because of conflicting findings, coaches and club medical staff are suspicious about using each test or a combination of them in identifying athletes at risk of injury. Regarding the popularity of football and the high severity and incidence of its injuries as well as the high cost of treatment for football-induced injuries, and their impact on the reduction of players’ performance and the sports clubs’ financial loss, it is necessary to perform a complete evaluation and fully examine the musculoskeletal system (from medical and functional perspective) for predicting the likelihood of injury. In this respect, this study aimed to investigate the common medical and functional tests for their ability to predict the rate and severity of injuries to elite football players in the first mid-season play of 2017-2018.
2. Materials and Methods
The present study is a correlational study, and based on the type of data collection method, it is a prospective and longitudinal study [27]. Study population consists of Iranian elite football players in professional sport clubs. Of them, 97 players were selected from three professional clubs. They were 17-35 years old and had been invited to the national football team. Five of them were excluded from the study because their injuries were not recorded by the club medical staff during the mid-season.
Anthropometric characteristics of subjects were as follows: Mean (SD) weight=77.15(7.72) kg; Mean (SD) height=181(6.23) cm, Mean (SD) age=25.14(14.6) years; and Mean (SD) BMI=22.1(98.66) kg/m2. The physician of each team recorded the injuries sustained throughout the season in the FIFA standard injury report form [28]. These forms were collected weekly by the researcher. The recorded injuries should be sustained in training or during the match, and be in such a state that need medical help (medical staff need to take an action for their treatment) [29, 30].
Functional Movement Screen test
The Functional Movement Screen tests (Figure 1) consist of seven movement tests which are able to detect limits and changes in normal movement patterns. This test was designed to provide interaction between movement chain and the necessary sustainability to implement functional movement patterns. In this test, the seven movement were scored from 1-3 points; if they done properly and without compensation, the subject earns 3 points; if done with some compensatory movements, the given score is 2; and if the subjects could not complete the movements, the given score is 1. The seven movement patterns are: deep squat, hurdle step, in-line lunge, active straight-leg raise, trunk stability push-up, rotary stability, and shoulder mobility [31].
Carioca test
The Carioca Test (Figure 2) requires crossover steps at a total distance of 80 feet (24.38 m). The subjects began moving from left to right, then reversed direction following the first 40-foot (12.19 m) length, thus performing the test moving a total of 80 feet (24.38 m) in the minimum amount of time possible [32]. This test may cause dynamic pivot shift phenomenon in those with Anterior Cruciate Ligament (ACL) injury. Lephart et al. reported high reliability (r=0.92 to 0.96) for this test [32].
Co-contraction test
The Co-Contraction test (Figure 3) was performed by securing the athlete with a heavy 48 inch (121 cm) length of rubber band (Thera band) which was anchored to a metal loop secured on a wall 60 inch (152 cm) above the floor. The band is stretched twice its recoil length and then the subject stands facing the wall with the toes of his/her feet on the semicircle. Then he is asked to complete five wall-to-wall lengths of the 180° semicircle with a radius of 96 inch (243 cm) from the metal loop in the minimum amount of time possible. Each semicircle is considered as one length. The test is repeated three times and then the average time is calculated [32].
This test reproduces the rotational forces at the knee that may cause tibial translation. Proper and timely contraction of the anterior and posterior muscles of the thigh can prevent this tibia subluxation and cause knee stability [33]. Lephart et al. reported high reliability (r=0.92 to 0.96) for this test [32].
Single-Leg Hop Test
The Single-Leg Hop Test (Figure 4) is used to evaluate the function, especially in people who are under rehabilitation after ACL reconstruction and evaluates the rehabilitation process. This a proper test for predicting the power of athletes’ lower limbs [34]. According to Reid et al. [35], the validity and reliability of this test are 0.82 and 0.93, respectively and it is suitable for patients undergoing rehabilitation following ACL reconstruction, and thus a proper test for preseason screening.
The Y-Balance Test
The Y-Balance Test is done in three directions of anterior, posteromedial and posterolateral. The subject stands on a single leg in the center of Y and tries to reach the opposite limb while maintaining the balance. He/she touches the furthest possible point by toe in any of directions without error (Figure 5). The distance from the contact point to the center is the distance to be reached which is recorded in cm. Since this test has a significant association with leg length, in order to perform this test and normalize the data, before starting to record, the actual length of the leg was measured by a tape meter from
The Single-Leg Hop Test (Figure 4) is used to evaluate the function, especially in people who are under rehabilitation after ACL reconstruction and evaluates the rehabilitation process. This a proper test for predicting the power of athletes’ lower limbs [34]. According to Reid et al. [35], the validity and reliability of this test are 0.82 and 0.93, respectively and it is suitable for patients undergoing rehabilitation following ACL reconstruction, and thus a proper test for preseason screening.
The Y-Balance Test
The Y-Balance Test is done in three directions of anterior, posteromedial and posterolateral. The subject stands on a single leg in the center of Y and tries to reach the opposite limb while maintaining the balance. He/she touches the furthest possible point by toe in any of directions without error (Figure 5). The distance from the contact point to the center is the distance to be reached which is recorded in cm. Since this test has a significant association with leg length, in order to perform this test and normalize the data, before starting to record, the actual length of the leg was measured by a tape meter from
anterior superior iliac spine to the medial malleolus in the supine position [36].
Medical tests
Some of the common preseason medical tests in Iran that have been approved by FIFA are as follow: 1. History taking; 2. Orthopedic examinations of three parts: knee/ankle, upper limb, pelvis/spine; 3. Cardiovascular examination by the specialist and angiography fellowship; 4. ECG recording, Echocardiography (according to FIFA protocol); 5. Complete blood and urine tests; 6. VO2 max test, examining maximum aerobic power by respiratory gas analysis; 7. Squeeze test (examining the risk of injuries in quadriceps, hamstring and groin). They were executed by the trained physicians who had experiences of preseason medical examinations for 4 years at Noorafshar Hospital in Tehran.
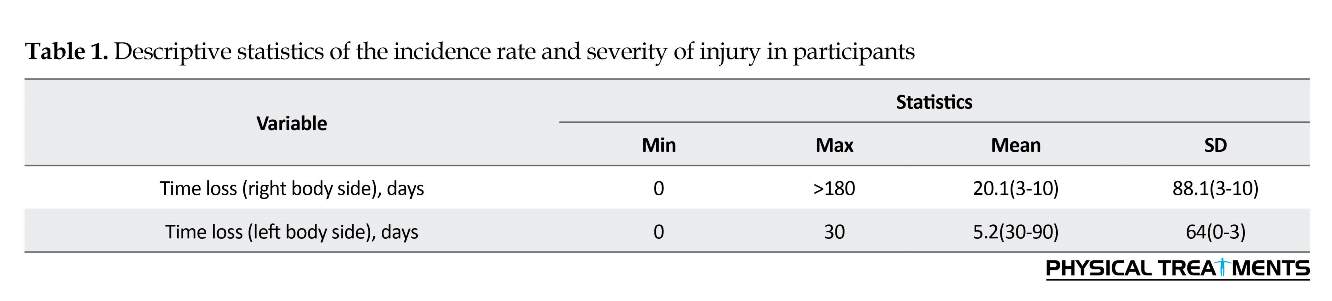
In the present study, the injury incidence rate is quantitative, but the severity of the injury is qualitative and nominal in 6 categories: 0=no injury, 1=3-10 days of absence from the match, 2=10-30 days of absence, 3=30-90 days of absence, 4=90-180 days of absence, and 5=more than 180 days of absence. The Kolmogorov-Smirnov (K-S) test was used to check the data normality. The results showed that the data distribution was not normal. Hence, to investigate the relationship between the predictability scores of five functional tests as well as medical test, we employed the univariate regression analysis (ENTER method). Statistical analyses were performed in SPSS V. 22. The significance level was set at 0.05.
3. Results
The Kolmogorov-Smirnov test results showed that the variables were not normally distributed. Hence we used non-parametric test to evaluate the predictive power of variables. The descriptive statistics of the incidence rate
Medical tests
Some of the common preseason medical tests in Iran that have been approved by FIFA are as follow: 1. History taking; 2. Orthopedic examinations of three parts: knee/ankle, upper limb, pelvis/spine; 3. Cardiovascular examination by the specialist and angiography fellowship; 4. ECG recording, Echocardiography (according to FIFA protocol); 5. Complete blood and urine tests; 6. VO2 max test, examining maximum aerobic power by respiratory gas analysis; 7. Squeeze test (examining the risk of injuries in quadriceps, hamstring and groin). They were executed by the trained physicians who had experiences of preseason medical examinations for 4 years at Noorafshar Hospital in Tehran.
In the present study, the injury incidence rate is quantitative, but the severity of the injury is qualitative and nominal in 6 categories: 0=no injury, 1=3-10 days of absence from the match, 2=10-30 days of absence, 3=30-90 days of absence, 4=90-180 days of absence, and 5=more than 180 days of absence. The Kolmogorov-Smirnov (K-S) test was used to check the data normality. The results showed that the data distribution was not normal. Hence, to investigate the relationship between the predictability scores of five functional tests as well as medical test, we employed the univariate regression analysis (ENTER method). Statistical analyses were performed in SPSS V. 22. The significance level was set at 0.05.
3. Results
The Kolmogorov-Smirnov test results showed that the variables were not normally distributed. Hence we used non-parametric test to evaluate the predictive power of variables. The descriptive statistics of the incidence rate
and severity of injuries to participants are shown in Table 1. Univariate regression analysis was used to predict the time-loss injuries and injury rate by predictor variables.
Results of univariate regression analysis showed that, among predictor variables, only SLH test with right leg could predict the severity of injury (P=0.035) (Table 2). Also, according to the results shown in Table 3, only Carolina test (combination of Carioca and Co-Contraction Tests) could predict the injury incidence rate in football players (P=0.010).
4. Discussion
The purpose of this study was to study the pre-season functional tests to predict the rate and severity of injuries to elite football players. The results showed that only SLH test with right leg could predict the severity of injury. Also, the Carolina test was able to predict the injury rate.
These results are consistent with the findings of some studies [15, 26, 37] and contrary to the other study results [12-14, 25]. The studies of Keisel et al. [12] and Butler et al. [14] were retrospective and maybe all of the injuries have not been recorded. Also, their sample size was small. They reported that their findings could not be used to establish cause and effect relationships. Another reason may be related to Y-BT test which measures the flexibility, strength, and coordination of the lower extremity muscles, but based on the study of Bakken et al. the strength of muscles around knee is a weak screening tool to predict lower extremity muscle injuries in professional soccer players [38]. However, the hamstring/quadriceps and thigh adduction/thigh abduction muscle ratios can predict injuries in hamstring, quadriceps, and thigh adductor muscles [39].
According to Butler et al. used Y-BT test to predict lower extremity injury in amateur college football players [40]. Since the level of competition is also a risk factor for injury and amateur players are more likely to sustain an injury with more time-loss than professionals, acquiring a low score in this test and considering high injury rates in soccer could be a reason for predicting injury in this research. Also, since the authors of both studies had contributions to the sale profits of Y Balance Test Kit™. So it can affect their results, too. Contrary to the previous findings, although the Y-BT test may still be appropriate in the rehabilitation programs and identifying a defect in dynamic postural control following injury, our findings did not support this test as a screening tool for predicting injury risk in elite football players.
The results of Duke et al. who used FMS test to predict risk of time-loss injury in rugby athletes, are not in agreement with our findings [25]. Also, Chalmers et
Results of univariate regression analysis showed that, among predictor variables, only SLH test with right leg could predict the severity of injury (P=0.035) (Table 2). Also, according to the results shown in Table 3, only Carolina test (combination of Carioca and Co-Contraction Tests) could predict the injury incidence rate in football players (P=0.010).
4. Discussion
The purpose of this study was to study the pre-season functional tests to predict the rate and severity of injuries to elite football players. The results showed that only SLH test with right leg could predict the severity of injury. Also, the Carolina test was able to predict the injury rate.
These results are consistent with the findings of some studies [15, 26, 37] and contrary to the other study results [12-14, 25]. The studies of Keisel et al. [12] and Butler et al. [14] were retrospective and maybe all of the injuries have not been recorded. Also, their sample size was small. They reported that their findings could not be used to establish cause and effect relationships. Another reason may be related to Y-BT test which measures the flexibility, strength, and coordination of the lower extremity muscles, but based on the study of Bakken et al. the strength of muscles around knee is a weak screening tool to predict lower extremity muscle injuries in professional soccer players [38]. However, the hamstring/quadriceps and thigh adduction/thigh abduction muscle ratios can predict injuries in hamstring, quadriceps, and thigh adductor muscles [39].
According to Butler et al. used Y-BT test to predict lower extremity injury in amateur college football players [40]. Since the level of competition is also a risk factor for injury and amateur players are more likely to sustain an injury with more time-loss than professionals, acquiring a low score in this test and considering high injury rates in soccer could be a reason for predicting injury in this research. Also, since the authors of both studies had contributions to the sale profits of Y Balance Test Kit™. So it can affect their results, too. Contrary to the previous findings, although the Y-BT test may still be appropriate in the rehabilitation programs and identifying a defect in dynamic postural control following injury, our findings did not support this test as a screening tool for predicting injury risk in elite football players.
The results of Duke et al. who used FMS test to predict risk of time-loss injury in rugby athletes, are not in agreement with our findings [25]. Also, Chalmers et
al. found out that football players with asymmetrical movements during pre-season FMS testing were more likely to sustain an injury during the regular season [37], but no association was observed between FMS threshold score of ≤14 with injury in elite football players. Although researchers have reported strong reliability for screening tests of functional movements, there are many contradictions about the validity of FMS test [41, 42]. The use of FMS test to predict the rate and severity of injuries from one sport to another and differences in sample size, statistical tests, and injury definitions, have provided conflicting results. Therefore, more research has to be done on a variety of sports to confirm the predicative ability of the FMS.
In the current study, SLH test (with right leg) was able to predict the intensity of injury. Since the average injury severity in the right body side was 3-10 days of absence, this test was able to predict mild injuries such as first degree ankle sprains. This is against the results of Brumitt et al. [43]. They reported that the pre-season standing long jump and SLH tests in college basketball players cannot predict non-contact time loss lower quadrant (such as ACL and ankle sprains) injuries; however, they can help sports medicine professionals evaluate athletic readiness prior to discharging an athlete back to sport after injury [43]. Their measurement was compared to the height of subjects and the distance hopped. This was not done in our study.
Also, they only reported non-contact injuries and the time loss in non-contact injuries was more than 10 days. In our study, both contact and non-contact injuries were examined, and it seems that only low-severity contact injuries have been predicted. One of the limitations of Brumitt et al. study was the absence of homogeneity of the sports where athletes of 10 different sports (tennis, football, wrestling, etc.) were selected. Thus, the rate and severity of injuries in these sports are different and not comparable.
Of different functional tests, only Carolina test could predict the injury rate. Since the incidence of lower extremity injuries in football is high, and it is one of the sports full of movements at all directions, most injuries to the lower extremity in this sport occur at several levels. Maybe because of the nature of Carioca and Co-Contraction Tests and the kinematics of the lower extremity, this simulated test is a mechanism for the most of lower limb injuries in football.
In 2014 FIFA World Cup, 63.4% of injuries were contact injuries [44], while there is no contact in any of the functional tests, and there is no test that can measure the performance of the athlete in contact with another player (e.g. the opponent). Also, about 60% of injuries in football occur at the last minutes of a match or training during muscle tiredness which increase the risk of moderate to severe injuries. But athletes do not perform functional tests in fatigue conditions, but in the best physical and mental state. These factors may be considered as limitations for the functional tests in this research and other studies to predict the rate and severity of injuries.
Hewett in his study concluded that it is difficult to predict the initial injury by the current tests and it is impossible to predict the player who is the first to be injured from an anatomical region [25]. However, it can predict secondary injuries (previous injuries), especially in ACL and ankle sprain of lateral ligaments [45]. He considered the kinetics and kinematics of the lower extremity (ground reaction force and knee valgus) as the best way to predict ACL injury in athletes.
This study showed that SLH test can predict the severity of injury, and the Carolina test was able to predict the injury incidence rate. However, the screening tools of functional activities have a very limited application in identifying the severity and rate of injuries to elite football players. Because of the nature of injuries and various risk factors like previous injury, the researchers must use the tests that covers many risk factors of injury and best simulates the conditions of injury in training or match.
Ethical Considerations
Compliance with ethical guidelines
University of Tehran, Ethics Committee on Research has approved the present research.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors declared no conflict of interest.
References
In the current study, SLH test (with right leg) was able to predict the intensity of injury. Since the average injury severity in the right body side was 3-10 days of absence, this test was able to predict mild injuries such as first degree ankle sprains. This is against the results of Brumitt et al. [43]. They reported that the pre-season standing long jump and SLH tests in college basketball players cannot predict non-contact time loss lower quadrant (such as ACL and ankle sprains) injuries; however, they can help sports medicine professionals evaluate athletic readiness prior to discharging an athlete back to sport after injury [43]. Their measurement was compared to the height of subjects and the distance hopped. This was not done in our study.
Also, they only reported non-contact injuries and the time loss in non-contact injuries was more than 10 days. In our study, both contact and non-contact injuries were examined, and it seems that only low-severity contact injuries have been predicted. One of the limitations of Brumitt et al. study was the absence of homogeneity of the sports where athletes of 10 different sports (tennis, football, wrestling, etc.) were selected. Thus, the rate and severity of injuries in these sports are different and not comparable.
Of different functional tests, only Carolina test could predict the injury rate. Since the incidence of lower extremity injuries in football is high, and it is one of the sports full of movements at all directions, most injuries to the lower extremity in this sport occur at several levels. Maybe because of the nature of Carioca and Co-Contraction Tests and the kinematics of the lower extremity, this simulated test is a mechanism for the most of lower limb injuries in football.
In 2014 FIFA World Cup, 63.4% of injuries were contact injuries [44], while there is no contact in any of the functional tests, and there is no test that can measure the performance of the athlete in contact with another player (e.g. the opponent). Also, about 60% of injuries in football occur at the last minutes of a match or training during muscle tiredness which increase the risk of moderate to severe injuries. But athletes do not perform functional tests in fatigue conditions, but in the best physical and mental state. These factors may be considered as limitations for the functional tests in this research and other studies to predict the rate and severity of injuries.
Hewett in his study concluded that it is difficult to predict the initial injury by the current tests and it is impossible to predict the player who is the first to be injured from an anatomical region [25]. However, it can predict secondary injuries (previous injuries), especially in ACL and ankle sprain of lateral ligaments [45]. He considered the kinetics and kinematics of the lower extremity (ground reaction force and knee valgus) as the best way to predict ACL injury in athletes.
This study showed that SLH test can predict the severity of injury, and the Carolina test was able to predict the injury incidence rate. However, the screening tools of functional activities have a very limited application in identifying the severity and rate of injuries to elite football players. Because of the nature of injuries and various risk factors like previous injury, the researchers must use the tests that covers many risk factors of injury and best simulates the conditions of injury in training or match.
Ethical Considerations
Compliance with ethical guidelines
University of Tehran, Ethics Committee on Research has approved the present research.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors declared no conflict of interest.
References
- FIFA Communication Division, Information Services. FIFA big Count 2006: 270 million people active in football. Zürich: Fédération Internationale de Football Association; 2007.
- Cohen M, Abdalla RJ, Ejnisman B, Amaro JT. [Orthopedic injuries in football (Portuguese)]. Brazilian Journal of Orthopedics. 1997; 32(12):940-4.
- Fuller CW, Ekstrand J, Junge A, Andersen TE, Bahr R, Dvorak J, et al. Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. Scandinavian Journal of Medicine & Science in Sports. 2006; 16(2):83-92. [DOI:10.1111/j.1600-0838.2006.00528.x] [PMID]
- Junge A, Dvorak J. Soccer injuries. Sports Medicine. 2004; 34(13):929-38. [DOI:10.2165/00007256-200434130-00004] [PMID]
- Zarei M, Rahnama N, Rajabi R. The effect of soccer players’ positional role in Iran super league on sport injury rates. World Journal of Sport Sciences. 2009; 2(1):60-4.
- Paus V, Torrengo F, Del Compare P. Incidence of injuries in juvenil soccer players. Revista de la Asociación Argentina de Traumatología del Deporte. 2003; 10(1):28-34.
- Junge A, Lamprecht M, Stamm H, Hasler H, Bizzini M, Tschopp M, et al. Countrywide campaign to prevent soccer injuries in Swiss amateur players. The American Journal of Sports Medicine. 2011; 39(1):57-63. [DOI:10.1177/0363546510377424] [PMID]
- Barengo NC, Meneses-Echávez JF, Ramírez-Vélez R, Cohen DD, Tovar G, Bautista JEC. The impact of the FIFA 11+ training program on injury prevention in football players: A systematic review. International Journal of Environmental Research and Public Health. 2014; 11(11):11986-12000. [DOI:10.3390/ijerph111111986] [PMID] [PMCID]
- Akturk A, Gouttebarge V, Frings-Dresen MH, Inklaar, H. Medical examinations in Dutch professional football (soccer): A qualitative study. International Journal of Sports Medicine. 2014; 15(4):343-51.
- Fuller CW, Ojelade EO, Taylor A. Preparticipation medical evaluation in professional sport in the UK: Theory or practice. British Journal of Sports Medicine. 2007; 41(12):890-6. [DOI:10.1136/bjsm.2007.038935]
- Hughes T, Sergeant JC, Parkes MJ, Callaghan MJ. Prognostic factors for specific lower extremity and spinal musculoskeletal injuries identified through medical screening and training load monitoring in professional football (soccer): A systematic review. BMJ Open Sport & Exercise Medicine. 2017; 3(1):e000263. [DOI:10.1136/bmjsem-2017-000263]
- Kiesel K, Plisky PJ, Voight ML. Can serious injury in professional football be predicted by a preseason functional movement screen. North American Journal of Sports Physical Therapy. 2007; 2(3):147-58. [PMID]
- Plisky PJ, Rauh MJ, Kaminski TW, Underwood FB. Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. Journal of Orthopaedic & Sports Physical Therapy. 2006; 36(12):911-9. [DOI:10.2519/jospt.2006.2244] [PMID]
- Butler RJ, Lehr ME, Fink ML, Kiesel KB, Plisky PJ. Dynamic balance performance and noncontact lower extremity injury in college football players: An initial study. Sports Health. 2013; 5(5):417-22. [DOI:10.1177/1941738113498703] [PMID] [PMCID]
- Smith CA, Chimera NJ, Warren M. Association of y balance test reach asymmetry and injury in division I athletes. Medicine and Science in Sports and Exercise. 2015; 47(1):136-41. [DOI:10.1249/MSS.0000000000000380] [PMID]
- Brumitt J, Heiderscheit BC, Manske RC, Niemuth PE, Rauh MJ. Lower extremity functional tests and risk of injury in division iii collegiate athletes. International Journal of Sports Physical Therapy. 2013; 8(3):216-27. [PMID] [PMCID]
- Manske R, Reiman M. Functional performance testing for power and return to sports. Sports Health. 2013; 5(3):244-50. [DOI:10.1177/1941738113479925] [PMID] [PMCID]
- Azzam MG, Throckmorton TW, Smith RA, Graham D, Scholler J, Azar FM. The functional movement screen as a predictor of injury in professional basketball players. Current Orthopaedic Practice. 2015; 26(6):619-23. [DOI:10.1097/BCO.0000000000000296]
- Brumitt J, Engilis A, Eubanks A, Mattocks A, Peet J, Bush N. Risk factors associated with noncontact time-loss lower-quadrant injury in male collegiate soccer players. Science and Medicine in Football. 2017; 1(2):96-101. [DOI:10.1080/24733938.2017.1282164]
- Dossa K, Cashman G, Howitt S, West B, Murray N. Can injury in major junior hockey players be predicted by a pre-season functional movement screen: A prospective cohort study. The Journal of the Canadian Chiropractic Association. 2014; 58(4):421-7. [PMID] [PMCID]
- Gonell AC, Romero JAP, Soler LM. Relationship between the Y balance test scores and soft tissue injury incidence in a soccer team. International Journal of Sports Physical Therapy. 2015; 10(7):955-66. [PMID] [PMCID]
- Kiesel KB, Butler RJ, Plisky PJ. Prediction of injury by limited and asymmetrical fundamental movement patterns in american football players. Journal of Sport Rehabilitation. 2014; 23(2):88-94. [DOI:10.1123/JSR.2012-0130] [PMID]
- Morgan BE, Oberlander MA. An examination of injuries in major league soccer: The inaugural season. The American Journal of Sports Medicine. 2001; 29(4):426-30. [DOI:10.1177/03635465010290040701] [PMID]
- Marques VB, Medeiros TM, de Souza Stigger F, Nakamura FY, Baroni BM. The Functional Movement Screen (FMS™) in elite young soccer players between 14 and 20 years: Composite score, individual-test scores and asymmetries. International Journal of Sports Physical Therapy. 2017; 12(6):977-85. [DOI:10.26603/ijspt20170977] [PMID] [PMCID]
- Duke SR, Martin SE, Gaul CA. Preseason functional movement screen predicts risk of time-loss injury in experienced male rugby :::::union::::: Athletes. The Journal of Strength & Conditioning Research. 2017; 31(10):2740-7. [DOI:10.1519/JSC.0000000000001838] [PMID]
- Moran RW, Schneiders AG, Mason J, Sullivan SJ. Do Functional Movement Screen (FMS) composite scores predict subsequent injury? A systematic review with meta-analysis. British Journal of Sports Medicine. 2017; 51(23):1661–9. [DOI:10.1136/bjsports-2016-096938]
- Euser AM, Zoccali C, Jager KJ, Dekker FW. Cohort studies: Prospective versus retrospective. Nephron Clinical Practice. 2009; 113(3):c214-c7. [DOI:10.1159/000235241] [PMID]
- Fünten Kad, Faude O, Lensch J, Meyer T. Injury characteristics in the German professional male soccer leagues after a shortened winter break. Journal of Athletic Training. 2014; 49(6):786-93. [DOI:10.4085/1062-6050-49.3.51] [PMID] [PMCID]
- Keller CS, Noyes FR, Buncher CR. The medical aspects of soccer injury epidemiology. The American Journal of Sports Medicine. 1988; 16(1_suppl):S-105-S-12. [DOI:10.1177/03635465880160s121]
- Ekstrand J. Epidemiology of football injuries. Science & Sports. 2008; 23(2):73-7. [DOI:10.1016/j.scispo.2007.10.012]
- Budnar Jr RG, Birdwell R, Moody C, Hill DW, Duplanty AA, Jackson AW, et al. Functional movement screentm scores in collegiate track and field athletes in relation to injury risk and performance. International Journal of Exercise Science: Conference Proceedings. 2013; 2(5);68. [PMCID]
- Lephart SM, Perrin DH, Fu FH, Minger K. Functional performance tests for the anterior cruciate ligament insufficient athlete. Journal of Athletic Training. 1991; 26(1):44-50.
- Kong DH, Yang SJ, Ha JK, Jang SH, Seo JG, Kim JG. Validation of functional performance tests after anterior cruciate ligament reconstruction. Knee Surgery & Related Research. 2012; 24(1):40-5. [DOI:10.5792/ksrr.2012.24.1.40] [PMID] [PMCID]
- Hamilton RT, Shultz SJ, Schmitz RJ, Perrin DH. Triple-hop distance as a valid predictor of lower limb strength and power. Journal of Athletic Training. 2008; 43(2):144-51. [DOI:10.4085/1062-6050-43.2.144] [PMID] [PMCID]
- Reid A, Birmingham TB, Stratford PW, Alcock GK, Giffin JR. Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Physical Therapy. 2007; 87(3):337-49. [DOI:10.2522/ptj.20060143] [PMID]
- Moradi K, Mioonejad H, Rajabi R. [The immediate effect of core stability exercises on postural sway in athletes with functional ankle instability (Persian)]. Scientific Journal of Rehabilitation Medicine. 2015; 4(3):101-10.
- Chalmers S, Fuller JT, Debenedictis TA, Townsley S, Lynagh M, Gleeson C, et al. Asymmetry during preseason Functional Movement Screen testing is associated with injury during a junior Australian football season. Journal of Science and Medicine in Sport. 2017; 20(7):653-7. [DOI:10.1016/j.jsams.2016.12.076] [PMID]
- Bakken A, Targett S, Bere T, Eirale C, Farooq A, Mosler AB, et al. Muscle strength is a poor screening test for predicting lower extremity injuries in professional male soccer players: A 2-year prospective cohort study. The American Journal of Sports Medicine. 2018; 46(6): 1481-91. [DOI:10.1177/0363546518756028]
- Dallinga JM, Benjaminse A, Lemmink KA. Which screening tools can predict injury to the lower extremities in team sports? Sports Medicine. 2012; 42(9):791-815. [DOI:10.1007/BF03262295] [PMID]
- van Beijsterveldt AM, Steffen K, Stubbe JH, Frederiks JE, van de Port IG, Backx FJ. Soccer injuries and recovery in Dutch male amateur soccer players: Results of a prospective cohort study. Clinical Journal of Sport Medicine. 2014; 24(4):337-42. [DOI:10.1097/JSM.0000000000000028] [PMID]
- Bonazza NA, Smuin D, Onks CA, Silvis ML, Dhawan A. Reliability, validity, and injury predictive value of the functional movement screen: A systematic review and meta-analysis. The American Journal of Sports Medicine. 2017; 45(3):725-32. [DOI:10.1177/0363546516641937] [PMID]
- Dorrel BS, Long T, Shaffer S, Myer GD. Evaluation of the functional movement screen as an injury prediction tool among active adult populations: A systematic review and meta-analysis. Sports Health. 2015; 7(6):532-7. [DOI:10.1177/1941738115607445] [PMID] [PMCID]
- Brumitt J, Engilis A, Isaak D, Briggs A, Mattocks A. Preseason jump and hop measures in male collegiate basketball players: An epidemiologic report. International Journal of Sports Physical Therapy. 2016; 11(6):954-61. [PMID] [PMCID]
- Junge A, Dvořák J. Football injuries during the 2014 FIFA World Cup. British Journal of Sports Medicine. 2015; 49(9):599-602. [DOI:10.1136/bjsports-2014-094469] [PMID] [PMCID]
- Hewett TE. Prediction of future injury in sport: Primary and secondary anterior cruciate ligament injury risk and return to sport as a model. Journal of Orthopaedic & Sports Physical Therapy. 2017; 47(4):228-31. [DOI:10.2519/jospt.2017.0603] [PMID]
Type of Study: Research |
Subject:
Special
Received: 2017/03/17 | Accepted: 2017/08/20 | Published: 2017/10/1
Received: 2017/03/17 | Accepted: 2017/08/20 | Published: 2017/10/1
References
1. FIFA Communication Division, Information Services. FIFA big Count 2006: 270 million people active in football. Zürich: Fédération Internationale de Football Association; 2007.
2. Cohen M, Abdalla RJ, Ejnisman B, Amaro JT. [Orthopedic injuries in football (Portuguese)]. Brazilian Journal of Orthopedics. 1997; 32(12):940-4.
3. Fuller CW, Ekstrand J, Junge A, Andersen TE, Bahr R, Dvorak J, et al. Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. Scandinavian Journal of Medicine & Science in Sports. 2006; 16(2):83-92. [DOI:10.1111/j.1600-0838.2006.00528.x] [PMID] [DOI:10.1111/j.1600-0838.2006.00528.x]
4. Junge A, Dvorak J. Soccer injuries. Sports Medicine. 2004; 34(13):929-38. [DOI:10.2165/00007256-200434130-00004] [PMID] [DOI:10.2165/00007256-200434130-00004]
5. Zarei M, Rahnama N, Rajabi R. The effect of soccer players' positional role in Iran super league on sport injury rates. World Journal of Sport Sciences. 2009; 2(1):60-4.
6. Paus V, Torrengo F, Del Compare P. Incidence of injuries in juvenil soccer players. Revista de la Asociación Argentina de Traumatología del Deporte. 2003; 10(1):28-34.
7. Junge A, Lamprecht M, Stamm H, Hasler H, Bizzini M, Tschopp M, et al. Countrywide campaign to prevent soccer injuries in Swiss amateur players. The American Journal of Sports Medicine. 2011; 39(1):57-63. [DOI:10.1177/0363546510377424] [PMID] [DOI:10.1177/0363546510377424]
8. Barengo NC, Meneses-Echávez JF, Ramírez-Vélez R, Cohen DD, Tovar G, Bautista JEC. The impact of the FIFA 11+ training program on injury prevention in football players: A systematic review. International Journal of Environmental Research and Public Health. 2014; 11(11):11986-12000. [DOI:10.3390/ijerph111111986] [PMID] [PMCID] [DOI:10.3390/ijerph111111986]
9. Akturk A, Gouttebarge V, Frings-Dresen MH, Inklaar, H. Medical examinations in Dutch professional football (soccer): A qualitative study. International Journal of Sports Medicine. 2014; 15(4):343-51.
10. Fuller CW, Ojelade EO, Taylor A. Preparticipation medical evaluation in professional sport in the UK: Theory or practice. British Journal of Sports Medicine. 2007; 41(12):890-6. [DOI:10.1136/bjsm.2007.038935] [DOI:10.1136/bjsm.2007.038935]
11. Hughes T, Sergeant JC, Parkes MJ, Callaghan MJ. Prognostic factors for specific lower extremity and spinal musculoskeletal injuries identified through medical screening and training load monitoring in professional football (soccer): A systematic review. BMJ Open Sport & Exercise Medicine. 2017; 3(1):e000263. [DOI:10.1136/bmjsem-2017-000263] [DOI:10.1136/bmjsem-2017-000263]
12. Kiesel K, Plisky PJ, Voight ML. Can serious injury in professional football be predicted by a preseason functional movement screen. North American Journal of Sports Physical Therapy. 2007; 2(3):147-58. [PMID] [PMID] [PMCID]
13. Plisky PJ, Rauh MJ, Kaminski TW, Underwood FB. Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. Journal of Orthopaedic & Sports Physical Therapy. 2006; 36(12):911-9. [DOI:10.2519/jospt.2006.2244] [PMID] [DOI:10.2519/jospt.2006.2244]
14. Butler RJ, Lehr ME, Fink ML, Kiesel KB, Plisky PJ. Dynamic balance performance and noncontact lower extremity injury in college football players: An initial study. Sports Health. 2013; 5(5):417-22. [DOI:10.1177/1941738113498703] [PMID] [PMCID] [DOI:10.1177/1941738113498703]
15. Smith CA, Chimera NJ, Warren M. Association of y balance test reach asymmetry and injury in division I athletes. Medicine and Science in Sports and Exercise. 2015; 47(1):136-41. [DOI:10.1249/MSS.0000000000000380] [PMID] [DOI:10.1249/MSS.0000000000000380]
16. Brumitt J, Heiderscheit BC, Manske RC, Niemuth PE, Rauh MJ. Lower extremity functional tests and risk of injury in division iii collegiate athletes. International Journal of Sports Physical Therapy. 2013; 8(3):216-27. [PMID] [PMCID] [PMID] [PMCID]
17. Manske R, Reiman M. Functional performance testing for power and return to sports. Sports Health. 2013; 5(3):244-50. [DOI:10.1177/1941738113479925] [PMID] [PMCID] [DOI:10.1177/1941738113479925]
18. Azzam MG, Throckmorton TW, Smith RA, Graham D, Scholler J, Azar FM. The functional movement screen as a predictor of injury in professional basketball players. Current Orthopaedic Practice. 2015; 26(6):619-23. [DOI:10.1097/BCO.0000000000000296] [DOI:10.1097/BCO.0000000000000296]
19. Brumitt J, Engilis A, Eubanks A, Mattocks A, Peet J, Bush N. Risk factors associated with noncontact time-loss lower-quadrant injury in male collegiate soccer players. Science and Medicine in Football. 2017; 1(2):96-101. [DOI:10.1080/24733938.2017.1282164] [DOI:10.1080/24733938.2017.1282164]
20. Dossa K, Cashman G, Howitt S, West B, Murray N. Can injury in major junior hockey players be predicted by a pre-season functional movement screen: A prospective cohort study. The Journal of the Canadian Chiropractic Association. 2014; 58(4):421-7. [PMID] [PMCID] [PMID] [PMCID]
21. Gonell AC, Romero JAP, Soler LM. Relationship between the Y balance test scores and soft tissue injury incidence in a soccer team. International Journal of Sports Physical Therapy. 2015; 10(7):955-66. [PMID] [PMCID] [PMID] [PMCID]
22. Kiesel KB, Butler RJ, Plisky PJ. Prediction of injury by limited and asymmetrical fundamental movement patterns in american football players. Journal of Sport Rehabilitation. 2014; 23(2):88-94. [DOI:10.1123/JSR.2012-0130] [PMID] [DOI:10.1123/JSR.2012-0130]
23. Morgan BE, Oberlander MA. An examination of injuries in major league soccer: The inaugural season. The American Journal of Sports Medicine. 2001; 29(4):426-30. [DOI:10.1177/03635465010290040701] [PMID] [DOI:10.1177/03635465010290040701]
24. Marques VB, Medeiros TM, de Souza Stigger F, Nakamura FY, Baroni BM. The Functional Movement Screen (FMS™) in elite young soccer players between 14 and 20 years: Composite score, individual-test scores and asymmetries. International Journal of Sports Physical Therapy. 2017; 12(6):977-85. [DOI:10.26603/ijspt20170977] [PMID] [PMCID] [DOI:10.26603/ijspt20170977]
25. Duke SR, Martin SE, Gaul CA. Preseason functional movement screen predicts risk of time-loss injury in experienced male rugby ::::union:::: Athletes. The Journal of Strength & Conditioning Research. 2017; 31(10):2740-7. [DOI:10.1519/JSC.0000000000001838] [PMID] [DOI:10.1519/JSC.0000000000001838]
26. Moran RW, Schneiders AG, Mason J, Sullivan SJ. Do Functional Movement Screen (FMS) composite scores predict subsequent injury? A systematic review with meta-analysis. British Journal of Sports Medicine. 2017; 51(23):1661–9. [DOI:10.1136/bjsports-2016-096938] [DOI:10.1136/bjsports-2016-096938]
27. Euser AM, Zoccali C, Jager KJ, Dekker FW. Cohort studies: Prospective versus retrospective. Nephron Clinical Practice. 2009; 113(3):c214-c7. [DOI:10.1159/000235241] [PMID] [DOI:10.1159/000235241]
28. Fünten Kad, Faude O, Lensch J, Meyer T. Injury characteristics in the German professional male soccer leagues after a shortened winter break. Journal of Athletic Training. 2014; 49(6):786-93. [DOI:10.4085/1062-6050-49.3.51] [PMID] [PMCID] [DOI:10.4085/1062-6050-49.3.51]
29. Keller CS, Noyes FR, Buncher CR. The medical aspects of soccer injury epidemiology. The American Journal of Sports Medicine. 1988; 16(1_suppl):S-105-S-12. [DOI:10.1177/03635465880160s121] [DOI:10.1177/03635465880160S121]
30. Ekstrand J. Epidemiology of football injuries. Science & Sports. 2008; 23(2):73-7. [DOI:10.1016/j.scispo.2007.10.012] [DOI:10.1016/j.scispo.2007.10.012]
31. Budnar Jr RG, Birdwell R, Moody C, Hill DW, Duplanty AA, Jackson AW, et al. Functional movement screentm scores in collegiate track and field athletes in relation to injury risk and performance. International Journal of Exercise Science: Conference Proceedings. 2013; 2(5);68. [PMCID]
32. Lephart SM, Perrin DH, Fu FH, Minger K. Functional performance tests for the anterior cruciate ligament insufficient athlete. Journal of Athletic Training. 1991; 26(1):44-50.
33. Kong DH, Yang SJ, Ha JK, Jang SH, Seo JG, Kim JG. Validation of functional performance tests after anterior cruciate ligament reconstruction. Knee Surgery & Related Research. 2012; 24(1):40-5. [DOI:10.5792/ksrr.2012.24.1.40] [PMID] [PMCID] [DOI:10.5792/ksrr.2012.24.1.40]
34. Hamilton RT, Shultz SJ, Schmitz RJ, Perrin DH. Triple-hop distance as a valid predictor of lower limb strength and power. Journal of Athletic Training. 2008; 43(2):144-51. [DOI:10.4085/1062-6050-43.2.144] [PMID] [PMCID] [DOI:10.4085/1062-6050-43.2.144]
35. Reid A, Birmingham TB, Stratford PW, Alcock GK, Giffin JR. Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Physical Therapy. 2007; 87(3):337-49. [DOI:10.2522/ptj.20060143] [PMID] [DOI:10.2522/ptj.20060143]
36. Moradi K, Mioonejad H, Rajabi R. [The immediate effect of core stability exercises on postural sway in athletes with functional ankle instability (Persian)]. Scientific Journal of Rehabilitation Medicine. 2015; 4(3):101-10.
37. Chalmers S, Fuller JT, Debenedictis TA, Townsley S, Lynagh M, Gleeson C, et al. Asymmetry during preseason Functional Movement Screen testing is associated with injury during a junior Australian football season. Journal of Science and Medicine in Sport. 2017; 20(7):653-7. [DOI:10.1016/j.jsams.2016.12.076] [PMID] [DOI:10.1016/j.jsams.2016.12.076]
38. Bakken A, Targett S, Bere T, Eirale C, Farooq A, Mosler AB, et al. Muscle strength is a poor screening test for predicting lower extremity injuries in professional male soccer players: A 2-year prospective cohort study. The American Journal of Sports Medicine. 2018; 46(6): 1481-91. [DOI:10.1177/0363546518756028] [DOI:10.1177/0363546518756028]
39. Dallinga JM, Benjaminse A, Lemmink KA. Which screening tools can predict injury to the lower extremities in team sports? Sports Medicine. 2012; 42(9):791-815. [DOI:10.1007/BF03262295] [PMID] [DOI:10.1007/BF03262295]
40. van Beijsterveldt AM, Steffen K, Stubbe JH, Frederiks JE, van de Port IG, Backx FJ. Soccer injuries and recovery in Dutch male amateur soccer players: Results of a prospective cohort study. Clinical Journal of Sport Medicine. 2014; 24(4):337-42. [DOI:10.1097/JSM.0000000000000028] [PMID] [DOI:10.1097/JSM.0000000000000028]
41. Bonazza NA, Smuin D, Onks CA, Silvis ML, Dhawan A. Reliability, validity, and injury predictive value of the functional movement screen: A systematic review and meta-analysis. The American Journal of Sports Medicine. 2017; 45(3):725-32. [DOI:10.1177/0363546516641937] [PMID] [DOI:10.1177/0363546516641937]
42. Dorrel BS, Long T, Shaffer S, Myer GD. Evaluation of the functional movement screen as an injury prediction tool among active adult populations: A systematic review and meta-analysis. Sports Health. 2015; 7(6):532-7. [DOI:10.1177/1941738115607445] [PMID] [PMCID] [DOI:10.1177/1941738115607445]
43. Brumitt J, Engilis A, Isaak D, Briggs A, Mattocks A. Preseason jump and hop measures in male collegiate basketball players: An epidemiologic report. International Journal of Sports Physical Therapy. 2016; 11(6):954-61. [PMID] [PMCID] [PMID] [PMCID]
44. Junge A, Dvořák J. Football injuries during the 2014 FIFA World Cup. British Journal of Sports Medicine. 2015; 49(9):599-602. [DOI:10.1136/bjsports-2014-094469] [PMID] [PMCID] [DOI:10.1136/bjsports-2014-094469]
45. Hewett TE. Prediction of future injury in sport: Primary and secondary anterior cruciate ligament injury risk and return to sport as a model. Journal of Orthopaedic & Sports Physical Therapy. 2017; 47(4):228-31. [DOI:10.2519/jospt.2017.0603] [PMID] [DOI:10.2519/jospt.2017.0603]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






.jpg)

.jpg)