Wed, Apr 17, 2024
Volume 8, Issue 1 (Spring 2018)
PTJ 2018, 8(1): 45-54 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Minoonejad H, Bazrafshan H, Akoochakian M, Aslani M. Effect of Attention Instructions of Balance Training in Athletes With Ankle Instability. PTJ 2018; 8 (1) :45-54
URL: http://ptj.uswr.ac.ir/article-1-310-en.html
URL: http://ptj.uswr.ac.ir/article-1-310-en.html
1- Department of Sports Medicine and Health, Faculty of Physical Education and Sport Sciences, University of Tehran, Tehran, Iran.
2- Department of Physical Education and Sports Sciences, Kish International Campus, University of Tehran, Kish, Iran.
2- Department of Physical Education and Sports Sciences, Kish International Campus, University of Tehran, Kish, Iran.
Full-Text [PDF 665 kb]
(2123 Downloads)
| Abstract (HTML) (4552 Views)
3. Results
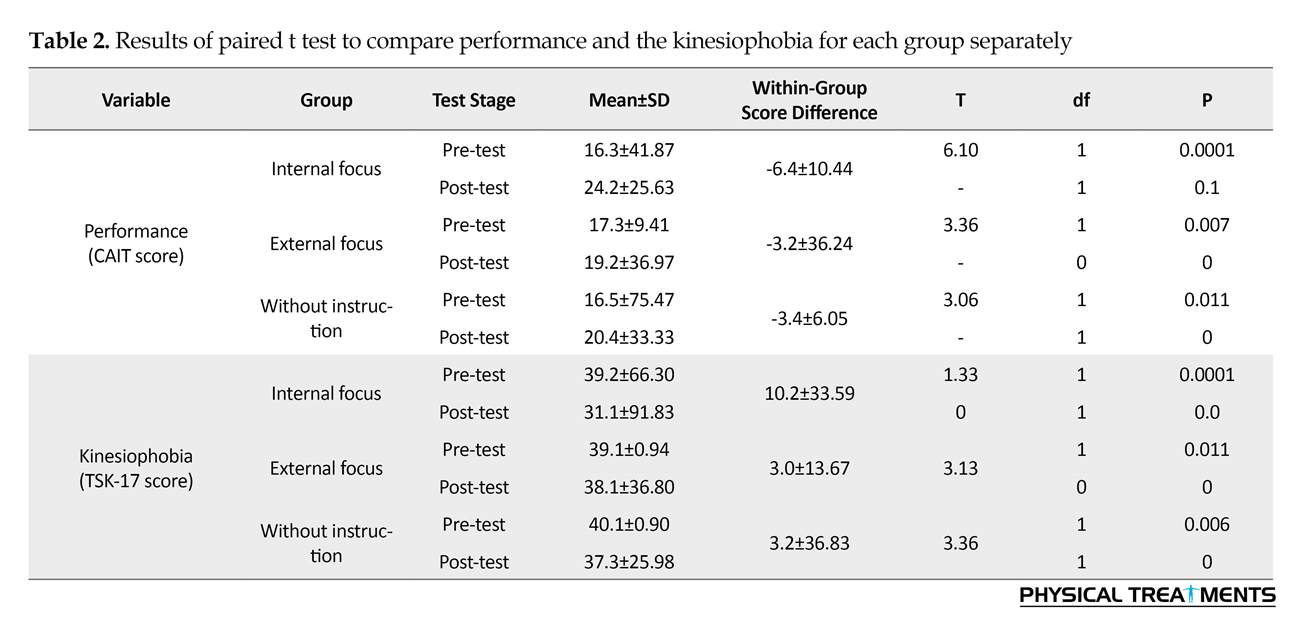
The paired t test and ANCOVA were used for within-group comparison (pre-test and post-test scores of each group) and for between-group comparison, respectively. Significance level in all tests was considered as P≤0.05 (Table 2).
Paired t test results revealed that in both questionnaires of performance and kinesiophobia there was a significant difference between pre-test and post-test in all 3 groups of “internal focus,” “external focus,” and “without instruction,” after 4 weeks of exercise. In detail, the CAIT scores in the post-test were significantly higher and TSK-17 scores were significantly lower than the pre-test (P≥0.05). This reflects performance improvement and reduced kinesiophobia in all 3 training groups.
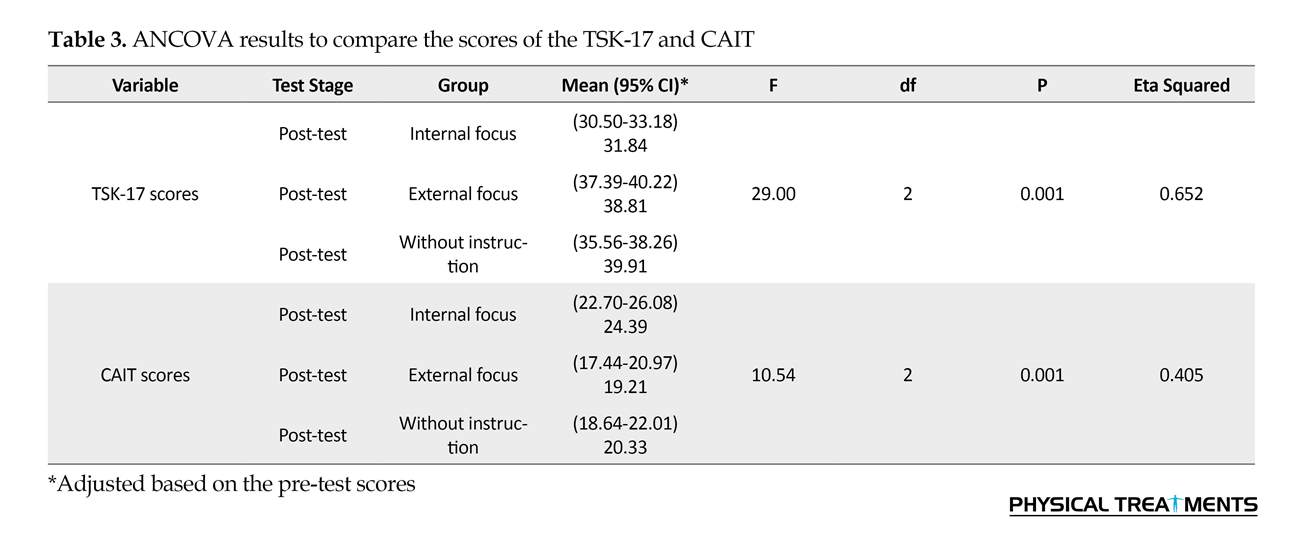
ANCOVA was used to compare the difference among the scores of the questionnaires in the 3 groups. The test results are reported in Table 2 and Figure 2. ANCOVA results demonstrated a significant difference between the 3 groups in the scores of CAIT and TSK-17 in post-test after controlling the effect of pre-test (covariate) (P≥0.05). Therefore, Bonferroni post hoc test was used to assess the differences between the groups. The results of this test are presented in Table 3 and 4.
The results of Bonferroni post hoc test suggested a significant difference in the scores of the CAIT between “internal focus” and “external focus” training groups. In particular, the scores of CAIT in post-test were significantly higher in the “internal focus” group than the “external focus” group, after 4 weeks of balance exercises (P≥0.05). In addition the scores of the CAIT in post-test in the “internal focus” group were significantly higher than the “external focus” group, after 4 weeks of balance exercises (P≥0.05).
There were no significant differences in the scores of CAIT between the “external focus” group and no-concentration group (P<0.05). The Bonferroni Test results suggested a significant difference in the scores of TSK-17 between the “internal focus” and the “external focus” training groups (P≥0.05). Thus, the scores of TSK-17 in post-test in the focus group of “internal focus” was significantly less than that of “external focus” group (P<0.05). In addition, there was no significant difference between the “internal focus” and “without instruction” groups (P>0.05).
4. Discussion
This research investigated the effect of attentional focus during rehabilitation on improving QoL in athletes with FAI. Comparison was conducted using a measure of performance through the CAIT and TSK-17, respectively, before and after 4 weeks of exercise with wobble board. The results of pre-test and post-test revealed that after 4 weeks of exercise with wobble board, all 3 exercise groups had significant progress in performance improvement and reduced kinesiophobia by receiving the “internal focus” instructions, instructions for “external focus”, and “without paying attention to the instructions” (CAIT scores in post-test were significantly higher and the TSK-17 scores in the post-test were significantly lower than those of the pre-test).
The ankle sprain is accompanied by the elongation of ligaments in this area, and sensory mechanical receptors within the ligament will become defective. Functional impairment in the ankle sensory receptors causes a defect in the depth of area and prevents the accurate understanding of central nervous system from ankle joint position in the space. Samadi investigated the effect of a 6-week nervous-muscle exercise with wobble board under supervision on the index of understanding the stability in male athletes with functional ankle instability through performance evaluation questionnaires. He reported that these exercises can improve performance and understanding the stability in these people [3]. The results of this study also suggested that 4 weeks of training with wobble board with the exact same protocol used in Samadi study would result in the improvement of performance and reduced kinesiophobia in athletes with functional ankle instability. This result is consistent with the findings of Samadi.
Between-group comparisons in the post-test results revealed that after 4 weeks of exercise with wobble board, internal focus group had a significant progress in performance and reduced kinesiophobia in the post-test, compared with the other 2 groups (post-test CAIT scores in the “internal focus” group were significantly higher and post-test TSK-17 scores were significantly lower than that of the other 2 groups). There was no significant difference between the 2 groups of “external focus” and “without receiving instructions” in post-test.
Defective sense of depth described by the sensorimotor function through the inability to accurately determine the motion of the joint and the joint position sense, is accompanied by reduced body awareness. Beker et al. argued that body awareness depends on perception capacity and the differentiation of information obtained from sensory interpreters including the depth receptors in the muscles and joints which is often linked to the person’s body and his/her perception of it [35]. According to Gylnesten, body awareness is the mental and phenomenological aspect of the proprioception and visceral sensation, received consciously and emerges by mental processes such as attention, interpretation, and evaluation [29]. According to Dragsand et al. body awareness will lead to faster improvement of patients with mental and musculoskeletal disorders [30].
Connors (2012) mentioned that long-term use of internal instructions during balance exercises would improve body awareness. He conducted a qualitative study on the mechanism of the Feldenkrais exercise, which was found effective in performance improvement in recent studies. He aimed to analyze content and the principles governing these balance training sessions. He mentioned that internal focus instructions (attention to body and components of motion during execution) and repetition and exercise variation have been used in these categories. This widespread attention to internal guidelines is related to body awareness exercises [36]. In many domestic studies, “internal focus” was used in performing different training methods (e.g. Tai chi, Pilates, Yoga, etc.) for patients with musculoskeletal disorders. Their results have suggested that using this type of focus attention has improved the QoL in this population [29].
International studies, which are indirectly consistent with this research, reported the favorable effects of exercises that emphasize body awareness on improvement of the joint position sense. For instance, Fung et al. reported that performing 3 months of Tai chi exercises was effective on the improvement of joint position sense [19]. Also, according to Kerr et al. (2008), Tai chi increases long-term learning process by improving tactile intelligence through the mechanisms of physical plasticity without tactile stimulation and direct contact [18]. Joint position sense is among the conscious assumptions of proprioception.
Similarly, Panics (2008) emphasized on the role of body awareness on the sensation of a joint position and investigated the effect of 4 months of exercise with wobble board on improving the knee joint sensation in healthy athletes. Deep sense information is transferred to higher brain centers through informed perceptions as well as the stimulation and repetition of motor activity. While expressing the 3 stages of motion control, including spinal feedback, cognitive planning, and brain stem activity in deep rehabilitation programs, Panics mentioned the main purpose of the knee joint proficiency training in Handball players to improve awareness and knee and ankle control in functional activities [37].
The effectiveness of using internal guidelines in the present study seem consistent with the above-mentioned studies. In these studies, attention to the body has been highlighted during exercise in the long run. Their results suggested improved body awareness. In line with the current study, Panics used the wobble board exercises for athletes and reported the significant improvement of knee joint position sense before and after the training period by measuring the knee joint position sense, compared with the control group. It is possible to consider improvement of the knee joint position sense as the reason to improve body awareness in the study by Panics.
The present study also could have probably improved awareness through improving the sense of position of knee and ankle joints through 4 weeks of exercise with the wobble board in the “internal focus” group. The defect in deep sense and body awareness decreased the QoL in patients with functional ankle instability. Thus, improving body awareness through internal attention during exercises has probably improved the QoL in this group over time.
Performing exercises with wobble board in all 3 groups of “internal focus”, “external focus”, and “without attention instructions” have improved the QoL. However, interventions to “internal focus” have more improved the QoL compared to the “external focus” and “without attention instruction”. It is suggested that coaches use this type of intervention during rehabilitation process (especially at the beginning of the rehabilitation phase). Data are insufficient in this area and further studies are required to investigate the effectiveness of internal and external focus in exercises.
Ethical Considerations
Compliance with ethical guidelines
All ethical notes were considered in this article. The participants were informed about the purpose of the research. They were assured about the confidentiality of their information. They were allowed to leave the study whenever they wish.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors contributions
Conceptualization, Methodology, Investigation: Hooman Minoonejad, Hengameh Bazrafshan, and Mahdiyeh Akoochakian; Writing Original Draft, Review & Editing: Hooman Minoonejad, and Mehdi Aslani; Supervision: Hooman Minoonejad.
Conflict of interest
The authors declared no conflict of interest.
References
Full-Text: (2011 Views)
1. Introduction
unctional Ankle Instability (FAI) is a complication occurring after repeated sprains in many people, especially athletes [1-3]. Freeman first described this complication as the chronic occurrence of an external ankle sprain, along with a feeling of energy depletion and sometimes pain and swelling [4]. Lateral Ankle Sprain (LAS) is the most frequent musculoskeletal damage in athletes in most sports [5, 6]. LAS leads to taking longest time off from exercise and imposes high costs [4, 7, 8]. The incidence rate of this damage in athletes is about 80%. Of whom, 40 to 75% suffer from FAI. This complication which is accompanied by defects of proprioception, muscular activity and function, and neuromuscular transmission and balance, limits individuals’ daily activity performance and sport performances over time and as a result, affects their Quality of Life (QoL) [9, 10].
By incorporating the biopsychosocial dimensions of individuals’ health, Health-Related Quality of Life (HRQoL) is a multifaceted approach to healthcare. It is considered as a determinant factor in monitoring the treatment and well-being [11]. The instability of the ankle is accompanied by the loss of QoL. Some researchers believe that functional instability is a mental dissent in the absence of any mechanical disorders [12]. Results of self-report studies on patients with this condition using questionnaires also documented decline in the quality of both daily and sport activities as well as their intellectual beliefs.
Studies are available on the QoL of athletes with ankle instability using psychometric measurement scales in addition to the functional evaluation measures. The use of these tools in order to assess the imbalance in QoL in athletes with ankle instability is a great help to sports therapists. As a result, the ideas and intellectual values and patients’ awareness of their health status can be understood and investigated through a self-report questionnaire [10].
This possibility can be achieved in the rehabilitation of musculoskeletal disorders among patients with FAI, by comparing pain, function, and patient satisfaction before and after conducting an intervention [13]. The assessment tools of ankle performance include Ankle Instability Instrument (AII), Ankle Joint Functional Assessment Tool (AJFAT), Cumberland Ankle Instability Tool (CAIT), Foot and Ankle Ability Measure (FAAM), Foot and Ankle Disability Index (FADI), and Foot and Ankle Outcome Score (FAOS). Of all, only CAIT and AII, which are devoted exclusively to sprains, can be used to compare HRQoL in patients with this condition [14].
By recognizing the least reasonable clinical changes, these questionnaires can examine the instability in different situations in addition to predicting the performance status due to instability [15]. Haji Maghsoudi has reported and verified CAIT as a tool with excellent test-retest reliability and acceptable internal consistency to evaluate athletes with FAI [15]. However, CAIT is a region-specific tool and disregards psychological factors affecting the report of injury by the injured. Exclusive dimension-specific tools have been used in a limited number of studies. For example, Tampa Scale of Kinesiophobia (TSK-17) has been employed as a measure for kinesiophobia and recurrent damage in patients with chronic injury including ankle instability [16, 17].
Conservative treatments are the main accepted tools in the management of recurrent injury prevention in rehabilitation of ankle instability [18]. Reportedly, using the wobble board has been more effective in the prevention of rebound sprained ankle. In addition, its functional instability is better than other therapeutic exercise methods, due to improving the proprioception, neuromuscular transmission, muscle performance, and finally the balance [19]. According to studies, the attentional demands of patients with ankle instability in some functional activities including walking and controlling the posture are different from the normal population [6]. Recently, body awareness exercises with an intellectual-physical approach have been widely considered in the rehabilitation of non-specific musculoskeletal disorders [20].
Improving the QoL relates with the improvement of body awareness. Body awareness should receive information from the surroundings by sensory receptors including visual, atrial, and somatosensory receptors and transmit them to the central nervous system [21]. Proprioception receptors, including joint position sense of recognition and kinesthesia are the most important components effective in gaining body awareness [22, 23]. After ankle sprain and subsequently, instability in the joint due to torn external ligaments of ankle, the proprioception of this area will be disturbed [24].
As a result, patients with ankle instability have weak body awareness [24]. Thus, it seems necessary to include body awareness exercises in training programs. Athletes are constantly exposed to forces which disturb their balance and postural control and athletes with FAI have less postural control [25]. Thus, using balancing exercises to eliminate neuromuscular defects caused by a sprain seems appropriate to improve the posture control of this group, and using the wobble board is recommended for this purpose [26-31]. Proprioception, neuromuscular transmission, and muscle activity performance can be improved through wobble board exercises [29].
Using special instructions during workout for the mind-body coordination, can improve body awareness in the long run. Qualitative studies have reported the positive effects of exercises such as Pilates, Yoga and Tai chi, which emphasize on body awareness and improving QoL [17, 29, 31]. The main axis of all these methods in athlete sports activities is attentional focus to gain awareness [32]. Attention could be defined as the information processing capacity of an individual. It can be oriented with the instructions and feedback provided to the individual. The attention source can be internal (focusing on body movements) or external (focusing on the effects of movement on the environment or its consequences) [32].
According to the studies on QoL, performance improvement and the kinesiophobia can be considered as criteria for measuring QoL. Thus, CAIT and TSK-17 have been introduced as appropriate tools to measure these criteria [27]. Due to cognitive changes following the instability of the ankle, attentional demands of these people during exercise therapy should be taken into account in addition to their skeletal muscle rehabilitation needs. Therefore, this study aimed to investigate the effect of attentional focus on improving the QoL during 4-week rehearsal training with wobble board with respect to criteria such as performance improvement and kinesiophobia in athletes with functional ankle instability.
2. Materials and Methods
This was a quasi-experimental study. The statistical population included male and female athlete students with 20-25 years of age playing basketball, volleyball, and futsal, afflicted with the FAI caused by external ankle sprain. This study was conducted in 2016 at the laboratory of the Faculty of Physical Education of the University of Tehran. Purposive sampling method was used to select the samples. Functional instability was detected through the AJFAT which contained 12 questions. Those with scores more than 26 met the research inclusion criteria [5].
76 people were identified by initial assessment and by examining inclusion and exclusion criteria, 46 people were eligible to participate in the study. Inclusion criteria included a history of ankle sprain and feeling energy-depletion in the ankle at least once in the last 6 months [33, 34], having FAI in the dominant leg, having at least 3 years of athletic experience at the level of academic teams with the continuation of 3 sessions per week, lacking experience in exercise with wobble board, not having mechanical instability (diagnosed by Anterior Drawer Diagnostic Test and Talar Tilt Test), lacking history of surgery or severe damage to the lower extremity, like ligament or knee meniscus injury in the past year, and lacking visible musculoskeletal abnormalities in the lower extremity such as genu varum, genu valgum, and pronation [5].
unctional Ankle Instability (FAI) is a complication occurring after repeated sprains in many people, especially athletes [1-3]. Freeman first described this complication as the chronic occurrence of an external ankle sprain, along with a feeling of energy depletion and sometimes pain and swelling [4]. Lateral Ankle Sprain (LAS) is the most frequent musculoskeletal damage in athletes in most sports [5, 6]. LAS leads to taking longest time off from exercise and imposes high costs [4, 7, 8]. The incidence rate of this damage in athletes is about 80%. Of whom, 40 to 75% suffer from FAI. This complication which is accompanied by defects of proprioception, muscular activity and function, and neuromuscular transmission and balance, limits individuals’ daily activity performance and sport performances over time and as a result, affects their Quality of Life (QoL) [9, 10].
By incorporating the biopsychosocial dimensions of individuals’ health, Health-Related Quality of Life (HRQoL) is a multifaceted approach to healthcare. It is considered as a determinant factor in monitoring the treatment and well-being [11]. The instability of the ankle is accompanied by the loss of QoL. Some researchers believe that functional instability is a mental dissent in the absence of any mechanical disorders [12]. Results of self-report studies on patients with this condition using questionnaires also documented decline in the quality of both daily and sport activities as well as their intellectual beliefs.
Studies are available on the QoL of athletes with ankle instability using psychometric measurement scales in addition to the functional evaluation measures. The use of these tools in order to assess the imbalance in QoL in athletes with ankle instability is a great help to sports therapists. As a result, the ideas and intellectual values and patients’ awareness of their health status can be understood and investigated through a self-report questionnaire [10].
This possibility can be achieved in the rehabilitation of musculoskeletal disorders among patients with FAI, by comparing pain, function, and patient satisfaction before and after conducting an intervention [13]. The assessment tools of ankle performance include Ankle Instability Instrument (AII), Ankle Joint Functional Assessment Tool (AJFAT), Cumberland Ankle Instability Tool (CAIT), Foot and Ankle Ability Measure (FAAM), Foot and Ankle Disability Index (FADI), and Foot and Ankle Outcome Score (FAOS). Of all, only CAIT and AII, which are devoted exclusively to sprains, can be used to compare HRQoL in patients with this condition [14].
By recognizing the least reasonable clinical changes, these questionnaires can examine the instability in different situations in addition to predicting the performance status due to instability [15]. Haji Maghsoudi has reported and verified CAIT as a tool with excellent test-retest reliability and acceptable internal consistency to evaluate athletes with FAI [15]. However, CAIT is a region-specific tool and disregards psychological factors affecting the report of injury by the injured. Exclusive dimension-specific tools have been used in a limited number of studies. For example, Tampa Scale of Kinesiophobia (TSK-17) has been employed as a measure for kinesiophobia and recurrent damage in patients with chronic injury including ankle instability [16, 17].
Conservative treatments are the main accepted tools in the management of recurrent injury prevention in rehabilitation of ankle instability [18]. Reportedly, using the wobble board has been more effective in the prevention of rebound sprained ankle. In addition, its functional instability is better than other therapeutic exercise methods, due to improving the proprioception, neuromuscular transmission, muscle performance, and finally the balance [19]. According to studies, the attentional demands of patients with ankle instability in some functional activities including walking and controlling the posture are different from the normal population [6]. Recently, body awareness exercises with an intellectual-physical approach have been widely considered in the rehabilitation of non-specific musculoskeletal disorders [20].
Improving the QoL relates with the improvement of body awareness. Body awareness should receive information from the surroundings by sensory receptors including visual, atrial, and somatosensory receptors and transmit them to the central nervous system [21]. Proprioception receptors, including joint position sense of recognition and kinesthesia are the most important components effective in gaining body awareness [22, 23]. After ankle sprain and subsequently, instability in the joint due to torn external ligaments of ankle, the proprioception of this area will be disturbed [24].
As a result, patients with ankle instability have weak body awareness [24]. Thus, it seems necessary to include body awareness exercises in training programs. Athletes are constantly exposed to forces which disturb their balance and postural control and athletes with FAI have less postural control [25]. Thus, using balancing exercises to eliminate neuromuscular defects caused by a sprain seems appropriate to improve the posture control of this group, and using the wobble board is recommended for this purpose [26-31]. Proprioception, neuromuscular transmission, and muscle activity performance can be improved through wobble board exercises [29].
Using special instructions during workout for the mind-body coordination, can improve body awareness in the long run. Qualitative studies have reported the positive effects of exercises such as Pilates, Yoga and Tai chi, which emphasize on body awareness and improving QoL [17, 29, 31]. The main axis of all these methods in athlete sports activities is attentional focus to gain awareness [32]. Attention could be defined as the information processing capacity of an individual. It can be oriented with the instructions and feedback provided to the individual. The attention source can be internal (focusing on body movements) or external (focusing on the effects of movement on the environment or its consequences) [32].
According to the studies on QoL, performance improvement and the kinesiophobia can be considered as criteria for measuring QoL. Thus, CAIT and TSK-17 have been introduced as appropriate tools to measure these criteria [27]. Due to cognitive changes following the instability of the ankle, attentional demands of these people during exercise therapy should be taken into account in addition to their skeletal muscle rehabilitation needs. Therefore, this study aimed to investigate the effect of attentional focus on improving the QoL during 4-week rehearsal training with wobble board with respect to criteria such as performance improvement and kinesiophobia in athletes with functional ankle instability.
2. Materials and Methods
This was a quasi-experimental study. The statistical population included male and female athlete students with 20-25 years of age playing basketball, volleyball, and futsal, afflicted with the FAI caused by external ankle sprain. This study was conducted in 2016 at the laboratory of the Faculty of Physical Education of the University of Tehran. Purposive sampling method was used to select the samples. Functional instability was detected through the AJFAT which contained 12 questions. Those with scores more than 26 met the research inclusion criteria [5].
76 people were identified by initial assessment and by examining inclusion and exclusion criteria, 46 people were eligible to participate in the study. Inclusion criteria included a history of ankle sprain and feeling energy-depletion in the ankle at least once in the last 6 months [33, 34], having FAI in the dominant leg, having at least 3 years of athletic experience at the level of academic teams with the continuation of 3 sessions per week, lacking experience in exercise with wobble board, not having mechanical instability (diagnosed by Anterior Drawer Diagnostic Test and Talar Tilt Test), lacking history of surgery or severe damage to the lower extremity, like ligament or knee meniscus injury in the past year, and lacking visible musculoskeletal abnormalities in the lower extremity such as genu varum, genu valgum, and pronation [5].
Initially, the study plan was briefly explained to the subjects. All study participant provided an informed consent form. Eventually, 37 athletes (16 girls and 21 boys) enrolled into the study and were randomly assigned into 3 training groups of “internal focus” (5 female and 7 male athletes), “external focus”, and the control group (5 female and 7 male athletes).
Demographic information of the first experimental group were as follows: Mean±SD age of 22.41±2.10 years, Mean±SD height of 173.58±6.59 cm, Mean±SD weight of 68.75±9.29 kg, and Mean±SD BMI of 22.78±2.56 kg/m2. Demographic information for the second experimental group were as follows: Mean±SD age of 21.1±1.72 years, Mean±SD height of 174.72±11.9 cm, Mean±SD weight of 67.18±11.42 kg, and Mean±SD BMI of 21.1±1.61 kg/m2. Finally, these information for the control group were Mean±SD age of 21.33±0.98 years, Mean±SD height of 174.25±8.8 cm, Mean±SD weight of 70.08±12.19 kg, and Mean±SD BMI mean score of 22.92±3.24 kg/m2. Then, CAIT and TSK-17 were completed by the athletes [10, 14-17]. All 3 study groups started their first training session, a day after the initial measurements.
The exercise duration was different in each group due to different instructions for each training group. The control group performed their exercises without any intervention. Subjects of all groups were requested to keep their balance as much as possible when performing balance exercises in all training sessions. An example of the instructions of “internal focus” used for the relevant group is to pay attention to the angle of lower extremity of the joints and the muscles and ligaments around their ankle. Regarding the guidelines of “external focus”, used for the other group, this can be mentioned that subjects should focus on the marker on the ground. Feedbacks were provided to the subjects in each session, for 4 weeks. Balance exercise protocol with wobble board was the same for all groups, during the 4 weeks of exercise [33].
Each subject participated in 3 sessions of exercise every other day on a weekly basis. Subjects should have attended all 12 sessions and were not allowed to be absent for 2 consecutive training sessions, otherwise, they were excluded from the research process. The training protocol was the same for the groups and included neuromuscular exercises, standing on both legs or with the injured leg on the wobble board with open or closed eyes and moving the board in different directions. The exercises instructions are presented in Table 1 and Figure 1. Every exercise included 30-s sets with a 10 s rest between sets and 30 s intervals between 2 different exercises.
Every training session took approximately 13-20 minutes. The same training protocol simultaneously started in all 3 groups, continued for up to 4 consecutive weeks (3 sessions per week), and ended concurrently after 12 training sessions in the 3 groups. One day after completing the exercises, the CAIT and TSK-17 were again completed by the subjects to compare the results with the pre-test.
SPSS was used for data analysis. Kolmogorov-Smirnov Test was also used to evaluate the normality of the data and Paired t-test and Analysis of Covariance (ANCOVA) were applied for within-group comparisons (pre-test and post-test scores of each group) and for between-group comparisons, respectively. Significance level was set at P<0.05.
Demographic information of the first experimental group were as follows: Mean±SD age of 22.41±2.10 years, Mean±SD height of 173.58±6.59 cm, Mean±SD weight of 68.75±9.29 kg, and Mean±SD BMI of 22.78±2.56 kg/m2. Demographic information for the second experimental group were as follows: Mean±SD age of 21.1±1.72 years, Mean±SD height of 174.72±11.9 cm, Mean±SD weight of 67.18±11.42 kg, and Mean±SD BMI of 21.1±1.61 kg/m2. Finally, these information for the control group were Mean±SD age of 21.33±0.98 years, Mean±SD height of 174.25±8.8 cm, Mean±SD weight of 70.08±12.19 kg, and Mean±SD BMI mean score of 22.92±3.24 kg/m2. Then, CAIT and TSK-17 were completed by the athletes [10, 14-17]. All 3 study groups started their first training session, a day after the initial measurements.
The exercise duration was different in each group due to different instructions for each training group. The control group performed their exercises without any intervention. Subjects of all groups were requested to keep their balance as much as possible when performing balance exercises in all training sessions. An example of the instructions of “internal focus” used for the relevant group is to pay attention to the angle of lower extremity of the joints and the muscles and ligaments around their ankle. Regarding the guidelines of “external focus”, used for the other group, this can be mentioned that subjects should focus on the marker on the ground. Feedbacks were provided to the subjects in each session, for 4 weeks. Balance exercise protocol with wobble board was the same for all groups, during the 4 weeks of exercise [33].
Each subject participated in 3 sessions of exercise every other day on a weekly basis. Subjects should have attended all 12 sessions and were not allowed to be absent for 2 consecutive training sessions, otherwise, they were excluded from the research process. The training protocol was the same for the groups and included neuromuscular exercises, standing on both legs or with the injured leg on the wobble board with open or closed eyes and moving the board in different directions. The exercises instructions are presented in Table 1 and Figure 1. Every exercise included 30-s sets with a 10 s rest between sets and 30 s intervals between 2 different exercises.
Every training session took approximately 13-20 minutes. The same training protocol simultaneously started in all 3 groups, continued for up to 4 consecutive weeks (3 sessions per week), and ended concurrently after 12 training sessions in the 3 groups. One day after completing the exercises, the CAIT and TSK-17 were again completed by the subjects to compare the results with the pre-test.
SPSS was used for data analysis. Kolmogorov-Smirnov Test was also used to evaluate the normality of the data and Paired t-test and Analysis of Covariance (ANCOVA) were applied for within-group comparisons (pre-test and post-test scores of each group) and for between-group comparisons, respectively. Significance level was set at P<0.05.
3. Results
The paired t test and ANCOVA were used for within-group comparison (pre-test and post-test scores of each group) and for between-group comparison, respectively. Significance level in all tests was considered as P≤0.05 (Table 2).
Paired t test results revealed that in both questionnaires of performance and kinesiophobia there was a significant difference between pre-test and post-test in all 3 groups of “internal focus,” “external focus,” and “without instruction,” after 4 weeks of exercise. In detail, the CAIT scores in the post-test were significantly higher and TSK-17 scores were significantly lower than the pre-test (P≥0.05). This reflects performance improvement and reduced kinesiophobia in all 3 training groups.
ANCOVA was used to compare the difference among the scores of the questionnaires in the 3 groups. The test results are reported in Table 2 and Figure 2. ANCOVA results demonstrated a significant difference between the 3 groups in the scores of CAIT and TSK-17 in post-test after controlling the effect of pre-test (covariate) (P≥0.05). Therefore, Bonferroni post hoc test was used to assess the differences between the groups. The results of this test are presented in Table 3 and 4.
The results of Bonferroni post hoc test suggested a significant difference in the scores of the CAIT between “internal focus” and “external focus” training groups. In particular, the scores of CAIT in post-test were significantly higher in the “internal focus” group than the “external focus” group, after 4 weeks of balance exercises (P≥0.05). In addition the scores of the CAIT in post-test in the “internal focus” group were significantly higher than the “external focus” group, after 4 weeks of balance exercises (P≥0.05).
There were no significant differences in the scores of CAIT between the “external focus” group and no-concentration group (P<0.05). The Bonferroni Test results suggested a significant difference in the scores of TSK-17 between the “internal focus” and the “external focus” training groups (P≥0.05). Thus, the scores of TSK-17 in post-test in the focus group of “internal focus” was significantly less than that of “external focus” group (P<0.05). In addition, there was no significant difference between the “internal focus” and “without instruction” groups (P>0.05).
4. Discussion
This research investigated the effect of attentional focus during rehabilitation on improving QoL in athletes with FAI. Comparison was conducted using a measure of performance through the CAIT and TSK-17, respectively, before and after 4 weeks of exercise with wobble board. The results of pre-test and post-test revealed that after 4 weeks of exercise with wobble board, all 3 exercise groups had significant progress in performance improvement and reduced kinesiophobia by receiving the “internal focus” instructions, instructions for “external focus”, and “without paying attention to the instructions” (CAIT scores in post-test were significantly higher and the TSK-17 scores in the post-test were significantly lower than those of the pre-test).
The ankle sprain is accompanied by the elongation of ligaments in this area, and sensory mechanical receptors within the ligament will become defective. Functional impairment in the ankle sensory receptors causes a defect in the depth of area and prevents the accurate understanding of central nervous system from ankle joint position in the space. Samadi investigated the effect of a 6-week nervous-muscle exercise with wobble board under supervision on the index of understanding the stability in male athletes with functional ankle instability through performance evaluation questionnaires. He reported that these exercises can improve performance and understanding the stability in these people [3]. The results of this study also suggested that 4 weeks of training with wobble board with the exact same protocol used in Samadi study would result in the improvement of performance and reduced kinesiophobia in athletes with functional ankle instability. This result is consistent with the findings of Samadi.
Between-group comparisons in the post-test results revealed that after 4 weeks of exercise with wobble board, internal focus group had a significant progress in performance and reduced kinesiophobia in the post-test, compared with the other 2 groups (post-test CAIT scores in the “internal focus” group were significantly higher and post-test TSK-17 scores were significantly lower than that of the other 2 groups). There was no significant difference between the 2 groups of “external focus” and “without receiving instructions” in post-test.
Defective sense of depth described by the sensorimotor function through the inability to accurately determine the motion of the joint and the joint position sense, is accompanied by reduced body awareness. Beker et al. argued that body awareness depends on perception capacity and the differentiation of information obtained from sensory interpreters including the depth receptors in the muscles and joints which is often linked to the person’s body and his/her perception of it [35]. According to Gylnesten, body awareness is the mental and phenomenological aspect of the proprioception and visceral sensation, received consciously and emerges by mental processes such as attention, interpretation, and evaluation [29]. According to Dragsand et al. body awareness will lead to faster improvement of patients with mental and musculoskeletal disorders [30].
Connors (2012) mentioned that long-term use of internal instructions during balance exercises would improve body awareness. He conducted a qualitative study on the mechanism of the Feldenkrais exercise, which was found effective in performance improvement in recent studies. He aimed to analyze content and the principles governing these balance training sessions. He mentioned that internal focus instructions (attention to body and components of motion during execution) and repetition and exercise variation have been used in these categories. This widespread attention to internal guidelines is related to body awareness exercises [36]. In many domestic studies, “internal focus” was used in performing different training methods (e.g. Tai chi, Pilates, Yoga, etc.) for patients with musculoskeletal disorders. Their results have suggested that using this type of focus attention has improved the QoL in this population [29].
International studies, which are indirectly consistent with this research, reported the favorable effects of exercises that emphasize body awareness on improvement of the joint position sense. For instance, Fung et al. reported that performing 3 months of Tai chi exercises was effective on the improvement of joint position sense [19]. Also, according to Kerr et al. (2008), Tai chi increases long-term learning process by improving tactile intelligence through the mechanisms of physical plasticity without tactile stimulation and direct contact [18]. Joint position sense is among the conscious assumptions of proprioception.
Similarly, Panics (2008) emphasized on the role of body awareness on the sensation of a joint position and investigated the effect of 4 months of exercise with wobble board on improving the knee joint sensation in healthy athletes. Deep sense information is transferred to higher brain centers through informed perceptions as well as the stimulation and repetition of motor activity. While expressing the 3 stages of motion control, including spinal feedback, cognitive planning, and brain stem activity in deep rehabilitation programs, Panics mentioned the main purpose of the knee joint proficiency training in Handball players to improve awareness and knee and ankle control in functional activities [37].
The effectiveness of using internal guidelines in the present study seem consistent with the above-mentioned studies. In these studies, attention to the body has been highlighted during exercise in the long run. Their results suggested improved body awareness. In line with the current study, Panics used the wobble board exercises for athletes and reported the significant improvement of knee joint position sense before and after the training period by measuring the knee joint position sense, compared with the control group. It is possible to consider improvement of the knee joint position sense as the reason to improve body awareness in the study by Panics.
The present study also could have probably improved awareness through improving the sense of position of knee and ankle joints through 4 weeks of exercise with the wobble board in the “internal focus” group. The defect in deep sense and body awareness decreased the QoL in patients with functional ankle instability. Thus, improving body awareness through internal attention during exercises has probably improved the QoL in this group over time.
Performing exercises with wobble board in all 3 groups of “internal focus”, “external focus”, and “without attention instructions” have improved the QoL. However, interventions to “internal focus” have more improved the QoL compared to the “external focus” and “without attention instruction”. It is suggested that coaches use this type of intervention during rehabilitation process (especially at the beginning of the rehabilitation phase). Data are insufficient in this area and further studies are required to investigate the effectiveness of internal and external focus in exercises.
Ethical Considerations
Compliance with ethical guidelines
All ethical notes were considered in this article. The participants were informed about the purpose of the research. They were assured about the confidentiality of their information. They were allowed to leave the study whenever they wish.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors contributions
Conceptualization, Methodology, Investigation: Hooman Minoonejad, Hengameh Bazrafshan, and Mahdiyeh Akoochakian; Writing Original Draft, Review & Editing: Hooman Minoonejad, and Mehdi Aslani; Supervision: Hooman Minoonejad.
Conflict of interest
The authors declared no conflict of interest.
References
- de Noronha M, Refshauge KM, Herbert RD, Kilbreath SL. Do voluntary strength, proprioception, range of motion, or postural sway predict occurrence of lateral ankle sprain. British Journal of Sports Medicine. 2006; 40(10):824-28. [DOI:10.1136/bjsm.2006.029645] [PMID] [PMCID]
- Wikstrom EA, Fournier KA, McKeon PO. Postural control differs between those with and without chronic ankle instability. Gait & Posture. 2010; 32(1):82-6. [DOI:10.1016/j.gaitpost.2010.03.015] [PMID]
- Witchalls J, Blanch P, Waddington G, Adams R. Intrinsic functional deficits associated with increased risk of ankle injuries: A systematic review with meta-analysis. British Journal of Sports Medicine. 2012; 46(7):515-23. [DOI:10.1136/bjsports-2011-090137] [PMID]
- Freeman MA, Dean MR, Hanham IW. The etiology and prevention of f unctional instability of the foot. The Journal of Bone and Joint Surgery British. 1965; 47(4):678-85. [DOI:10.1302/0301-620X.47B4.678] [PMID]
- Rotem-Lehrer N, Laufer Y. Effect of focus of attention on transfer of a postural control task following an ankle sprain. Journal of Orthopaedic & Sports Physical Therapy. 2007; 37(9):564-9.
- Rahnama L, Salavati M, Akhbari B, Mazaheri M. Attentional demands and postural control in athletes with and without functional ankle instability. Journal of Orthopedic & Sports Physical Therapy. 2010; 40(3):180-7. [DOI:10.2519/jospt.2010.3188].
- Beynnon BD, Murphy DF, Alosa DM. Predictive factors for lateral ankle sprains: A literature review. Journal of Athletic Training. 2002; 37(4):376-80. [PMID] [PMCID]
- Kobayashi T, Gamada K. Lateral ankle sprain and chronic ankle instability: A critical review. Foot & Ankle Specialist. 2014; 7(4):298-326. [DOI:10.1177/1938640014539813] [PMID]
- De Noronha M, Refshauge KM, Crosbie J, Kilbreath SL. Relationship between functional ankle instability and postural control. Journal of Orthopaedic & Sports Physical Therapy. 2008; 38(12):782-9.
- Houston MN, Van Lunen BL, Hoch MC. Health-related quality of life in individuals with chronic ankle instability. Journal of Athletic Training. 2014; 49(6):758-63. [DOI:10.4085/1062-6050-49.3.54] [PMID] [PMCID]
- Parsons JT, Snyder AR. Health-related quality of life as a primary clinical outcome in sport rehabilitation. Journal of Sport Rehabilitation. 2011; 20(1):17-36. [DOI:10.1123/jsr.20.1.17] [PMID]
- Madras D, Barr JB. Rehabilitation for functional ankle instability. Journal of Sport Rehabilitation. 2003; 12(2):133-42. [DOI:10.1123/jsr.12.2.133]
- Brownstein B, Bronner S. Functional movement in orthopaedic and sports physical therapy: Evaluation, treatment, and outcomes. London: Churchill Livingstone; 1997.
- Donahue M, Simon J, Docherty CL. Critical review of self-reported functional ankle instability measures. Foot & Ankle International. 2011; 32(12):1140-6. [DOI:10.3113/FAI.2011.1140] [PMID]
- Haji Maghsoudi M, Naseri N, Nouri Zadeh S, Jalali S. [Evidence of reliability for persian version of the Cumberland Ankle Instability Tool (CAIT) in Iranian athletes with lateral ankle sprain (Persian)]. Archives of Rehabilitation. 2016; 16(4):304-11.
- Rahmati N, Asghari MMA, Shaeiri MR, Paknejad M, Rahmati Z, Ghassami M, et al. [Psychometric properties of the tampa scale for kinesiophobia amongst iranian patients with chronic persistent pain (Persian)]. Payesh. 2014; 13(2):197-210.
- Houston MN, Hoch JM, Hoch MC. Patient-reported outcome measures in individuals with chronic ankle instability: A systematic review. Journal of Athletic Training. 2015; 50(10):1019-33. [DOI:10.4085/1062-6050-50.9.01] [PMID] [PMCID]
- Hale SA, Hertel J, Olmsted-Kramer LC. The effect of a 4-week comprehensive rehabilitation program on postural control and lower extremity function in individuals with chronic ankle instability. Journal of Orthopaedic & Sports Physical Therapy. 2007; 37(6):303-11. [DOI:10.2519/jospt.2007.2322]
- van der Wees PJ, Lenssen AF, Hendriks EJ, Stomp DJ, Dekker J, de Bie RA. Effectiveness of exercise therapy and manual mobilisation in acute ankle sprain and functional instability: A systematic review. Australian Journal of Physiotherapy. 2006; 52(1):27-37. [DOI:10.1016/S0004-9514(06)70059-9]
- Malmgren-Olsson EB, Armelius BA, Armelius K. A comparative outcome study of body awareness therapy, Feldenkrais, and conventional physiotherapy for patients with nonspecific musculoskeletal disorders: Changes in psychological symptoms, pain, and self-image. Physiotherapy Theory and Practice. 2001; 17(2):77-95. [DOI:10.1080/095939801750334167]
- Hansson EE, Beckman A, Håkansson A. Effect of vision, proprioception, and the position of the vestibular organ on postural sway. Acta Oto-Laryngologica. 2010; 130(12):1358-63. [DOI:10.3109/00016489.2010.498024] [PMID]
- Kynsburg A, Pánics G, Halasi T. Long-term neuromuscular training and ankle joint position sense. Acta Physiologica Hungarica. 2010; 97(2):183-91. [DOI:10.1556/APhysiol.97.2010.2.4] [PMID]
- Moradi K, Minoonejad H, Rajabi R. [The immediate effect of core stability exercises on postural sway in athletes with functional ankle instability (Persian)]. Scientific Journal of Rehabilitation Medicine. 2015; 4(3):103-12.
- Robbins S, Waked E, Rappel R. Ankle taping improves proprioception before and after exercise in young men. British Journal of Sports Medicine. 1995; 29(4):242-7. [DOI:10.1136/bjsm.29.4.242] [PMID] [PMCID]
- Freeman M. Instability of the foot affer injuries to the lateral ligament of the ankle. Journal of Bone & Joint Surgery British. 1965; 47(4):669-77. [DOI:10.1302/0301-620X.47B4.669] [PMID]
- Women KK, Sonepat H. Effect of wobble board balance training program on static balance, dynamic balance & triple hop distance in male collegiate basketball athlete. International Journal of Physiotherapy and Research. 2014; 2(4):657-2.
- Wester JU, Jespersen SM, Nielsen KD, Neumann L. Wobble board training after partial sprains of the lateral ligaments of the ankle: A prospective randomized study. Journal of Orthopaedic & Sports Physical Therapy. 1996; 23(5):332-6. [DOI:10.2519/jospt.1996.23.5.332] [PMID]
- Clark VM, Burden AM. A 4-week wobble board exercise program improved muscle onset latency and perceived stability in individuals with a functionally unstable ankle. Physical Therapy in Sport. 2005; 6(4):181-7. [DOI:10.1016/j.ptsp.2005.08.003]
- Samadi H, Rajabi R, Karimizade Ardakani M. [The effect of six weeks of neuromuscular training on joint position sense and lower extremity function in male athletes with functional ankle instability (Persian)]. Journal of Sport Medicine. 2017; 9(1):15-33. [DOI:10.22059/JSMED.2017.62869]
- Balogun J, Adesinasi C, Marzouk D. The effects of a wobble board exercise training program on static balance performance and strength of lower extremity muscles. Physiotherapy Canada. 1992; 44(4):23-30.
- Linens SW, Ross SE, Arnold BL. Wobble board rehabilitation for improving balance in ankles with chronic instability. Clinical Journal of Sport Medicine. 2016; 26(1):76-82. [DOI:10.1097/JSM.0000000000000191] [PMID]
- Pashaabadi A, Farokhi A, Jamshidi A, Shahbazi M. Effect of attentional focus on postural sways and muscular activity in semi skilled gymnasts. Journal of Modern Rehabilitation. 2014; 8(1):28-34.
- Matsusaka N, Yokoyama S, Tsurusaki T, Inokuchi S, Okita M. Effect of ankle disk training combined with tactile stimulation to the leg and foot on functional instability of the ankle. The American Journal of Sports Medicine. 2001; 29(1):25-30. [DOI:10.1177/03635465010290010901] [PMID]
- Kaminski TW, Hartsell HD. Factors contributing to chronic ankle instability: A strength perspective. Journal of Athletic Training. 2002; 37(4):394-405. [PMID] [PMCID]
- Ali Zamani S, Ghasemi GA, Karimi A, Salehi H. [Pilates exercise effect on pain and general health of female patients with chronic low back pain (Persian)]. Journal of Research in Rehabilitation Sciences. 2011; 7(1):117-25.
- Connors KA, Galea MP, Said CM, Remedios LJ. Feldenkrais Method balance classes are based on principles of motor learning and postural control retraining: A qualitative research study. Physiotherapy. 2010; 96(4):324-36. [DOI:10.1016/j.physio.2010.01.004] [PMID]
- Panics G, Tallay A, Pavlik A, Berkes I. Effect of proprioception training on knee joint position sense in female team handball players. British Journal of Sports Medicine. 2008; 42(6):472-6. [DOI:10.1136/bjsm.2008.046516] [PMID]
Type of Study: Applicable |
Subject:
General
Received: 2017/04/13 | Accepted: 2018/10/13 | Published: 2019/02/19
Received: 2017/04/13 | Accepted: 2018/10/13 | Published: 2019/02/19
References
1. de Noronha M, Refshauge KM, Herbert RD, Kilbreath SL. Do voluntary strength, proprioception, range of motion, or postural sway predict occurrence of lateral ankle sprain. British Journal of Sports Medicine. 2006; 40(10):824-28. [DOI:10.1136/bjsm.2006.029645] [PMID] [PMCID] [DOI:10.1136/bjsm.2006.029645]
2. Wikstrom EA, Fournier KA, McKeon PO. Postural control differs between those with and without chronic ankle instability. Gait & Posture. 2010; 32(1):82-6. [DOI:10.1016/j.gaitpost.2010.03.015] [PMID] [DOI:10.1016/j.gaitpost.2010.03.015]
3. Witchalls J, Blanch P, Waddington G, Adams R. Intrinsic functional deficits associated with increased risk of ankle injuries: A systematic review with meta-analysis. British Journal of Sports Medicine. 2012; 46(7):515-23. [DOI:10.1136/bjsports-2011-090137] [PMID] [DOI:10.1136/bjsports-2011-090137]
4. Freeman MA, Dean MR, Hanham IW. The etiology and prevention of f unctional instability of the foot. The Journal of Bone and Joint Surgery British. 1965; 47(4):678-85. [DOI:10.1302/0301-620X.47B4.678] [PMID] [DOI:10.1302/0301-620X.47B4.678]
5. Rotem-Lehrer N, Laufer Y. Effect of focus of attention on transfer of a postural control task following an ankle sprain. Journal of Orthopaedic & Sports Physical Therapy. 2007; 37(9):564-9. [DOI:10.2519/jospt.2007.2519] [PMID]
6. Rahnama L, Salavati M, Akhbari B, Mazaheri M. Attentional demands and postural control in athletes with and without functional ankle instability. Journal of Orthopedic & Sports Physical Therapy. 2010; 40(3):180-7. [DOI:10.2519/jospt.2010.3188]. [DOI:10.2519/jospt.2010.3188]
7. Beynnon BD, Murphy DF, Alosa DM. Predictive factors for lateral ankle sprains: A literature review. Journal of Athletic Training. 2002; 37(4):376-80. [PMID] [PMCID] [PMID] [PMCID]
8. Kobayashi T, Gamada K. Lateral ankle sprain and chronic ankle instability: A critical review. Foot & Ankle Specialist. 2014; 7(4):298-326. [DOI:10.1177/1938640014539813] [PMID] [DOI:10.1177/1938640014539813]
9. De Noronha M, Refshauge KM, Crosbie J, Kilbreath SL. Relationship between functional ankle instability and postural control. Journal of Orthopaedic & Sports Physical Therapy. 2008; 38(12):782-9. [DOI:10.2519/jospt.2008.2766] [PMID]
10. Houston MN, Van Lunen BL, Hoch MC. Health-related quality of life in individuals with chronic ankle instability. Journal of Athletic Training. 2014; 49(6):758-63. [DOI:10.4085/1062-6050-49.3.54] [PMID] [PMCID] [DOI:10.4085/1062-6050-49.3.54]
11. Parsons JT, Snyder AR. Health-related quality of life as a primary clinical outcome in sport rehabilitation. Journal of Sport Rehabilitation. 2011; 20(1):17-36. [DOI:10.1123/jsr.20.1.17] [PMID] [DOI:10.1123/jsr.20.1.17]
12. Madras D, Barr JB. Rehabilitation for functional ankle instability. Journal of Sport Rehabilitation. 2003; 12(2):133-42. [DOI:10.1123/jsr.12.2.133] [DOI:10.1123/jsr.12.2.133]
13. Brownstein B, Bronner S. Functional movement in orthopaedic and sports physical therapy: Evaluation, treatment, and outcomes. London: Churchill Livingstone; 1997.
14. Donahue M, Simon J, Docherty CL. Critical review of self-reported functional ankle instability measures. Foot & Ankle International. 2011; 32(12):1140-6. [DOI:10.3113/FAI.2011.1140] [PMID] [DOI:10.3113/FAI.2011.1140]
15. Haji Maghsoudi M, Naseri N, Nouri Zadeh S, Jalali S. [Evidence of reliability for persian version of the Cumberland Ankle Instability Tool (CAIT) in Iranian athletes with lateral ankle sprain (Persian)]. Archives of Rehabilitation. 2016; 16(4):304-11.
16. Rahmati N, Asghari MMA, Shaeiri MR, Paknejad M, Rahmati Z, Ghassami M, et al. [Psychometric properties of the tampa scale for kinesiophobia amongst iranian patients with chronic persistent pain (Persian)]. Payesh. 2014; 13(2):197-210.
17. Houston MN, Hoch JM, Hoch MC. Patient-reported outcome measures in individuals with chronic ankle instability: A systematic review. Journal of Athletic Training. 2015; 50(10):1019-33. [DOI:10.4085/1062-6050-50.9.01] [PMID] [PMCID] [DOI:10.4085/1062-6050-50.9.01]
18. Hale SA, Hertel J, Olmsted-Kramer LC. The effect of a 4-week comprehensive rehabilitation program on postural control and lower extremity function in individuals with chronic ankle instability. Journal of Orthopaedic & Sports Physical Therapy. 2007; 37(6):303-11. [DOI:10.2519/jospt.2007.2322] [DOI:10.2519/jospt.2007.2322]
19. van der Wees PJ, Lenssen AF, Hendriks EJ, Stomp DJ, Dekker J, de Bie RA. Effectiveness of exercise therapy and manual mobilisation in acute ankle sprain and functional instability: A systematic review. Australian Journal of Physiotherapy. 2006; 52(1):27-37. [DOI:10.1016/S0004-9514(06)70059-9] [DOI:10.1016/S0004-9514(06)70059-9]
20. Malmgren-Olsson EB, Armelius BA, Armelius K. A comparative outcome study of body awareness therapy, Feldenkrais, and conventional physiotherapy for patients with nonspecific musculoskeletal disorders: Changes in psychological symptoms, pain, and self-image. Physiotherapy Theory and Practice. 2001; 17(2):77-95. [DOI:10.1080/095939801750334167] [DOI:10.1080/095939801750334167]
21. Hansson EE, Beckman A, Håkansson A. Effect of vision, proprioception, and the position of the vestibular organ on postural sway. Acta Oto-Laryngologica. 2010; 130(12):1358-63. [DOI:10.3109/00016489.2010.498024] [PMID] [DOI:10.3109/00016489.2010.498024]
22. Kynsburg A, Pánics G, Halasi T. Long-term neuromuscular training and ankle joint position sense. Acta Physiologica Hungarica. 2010; 97(2):183-91. [DOI:10.1556/APhysiol.97.2010.2.4] [PMID] [DOI:10.1556/APhysiol.97.2010.2.4]
23. Moradi K, Minoonejad H, Rajabi R. [The immediate effect of core stability exercises on postural sway in athletes with functional ankle instability (Persian)]. Scientific Journal of Rehabilitation Medicine. 2015; 4(3):103-12.
24. Robbins S, Waked E, Rappel R. Ankle taping improves proprioception before and after exercise in young men. British Journal of Sports Medicine. 1995; 29(4):242-7. [DOI:10.1136/bjsm.29.4.242] [PMID] [PMCID] [DOI:10.1136/bjsm.29.4.242]
25. Freeman M. Instability of the foot affer injuries to the lateral ligament of the ankle. Journal of Bone & Joint Surgery British. 1965; 47(4):669-77. [DOI:10.1302/0301-620X.47B4.669] [PMID] [DOI:10.1302/0301-620X.47B4.669]
26. Women KK, Sonepat H. Effect of wobble board balance training program on static balance, dynamic balance & triple hop distance in male collegiate basketball athlete. International Journal of Physiotherapy and Research. 2014; 2(4):657-2.
27. Wester JU, Jespersen SM, Nielsen KD, Neumann L. Wobble board training after partial sprains of the lateral ligaments of the ankle: A prospective randomized study. Journal of Orthopaedic & Sports Physical Therapy. 1996; 23(5):332-6. [DOI:10.2519/jospt.1996.23.5.332] [PMID] [DOI:10.2519/jospt.1996.23.5.332]
28. Clark VM, Burden AM. A 4-week wobble board exercise program improved muscle onset latency and perceived stability in individuals with a functionally unstable ankle. Physical Therapy in Sport. 2005; 6(4):181-7. [DOI:10.1016/j.ptsp.2005.08.003] [DOI:10.1016/j.ptsp.2005.08.003]
29. Samadi H, Rajabi R, Karimizade Ardakani M. [The effect of six weeks of neuromuscular training on joint position sense and lower extremity function in male athletes with functional ankle instability (Persian)]. Journal of Sport Medicine. 2017; 9(1):15-33. [DOI:10.22059/JSMED.2017.62869]
30. Balogun J, Adesinasi C, Marzouk D. The effects of a wobble board exercise training program on static balance performance and strength of lower extremity muscles. Physiotherapy Canada. 1992; 44(4):23-30.
31. Linens SW, Ross SE, Arnold BL. Wobble board rehabilitation for improving balance in ankles with chronic instability. Clinical Journal of Sport Medicine. 2016; 26(1):76-82. [DOI:10.1097/JSM.0000000000000191] [PMID] [DOI:10.1097/JSM.0000000000000191]
32. Pashaabadi A, Farokhi A, Jamshidi A, Shahbazi M. Effect of attentional focus on postural sways and muscular activity in semi skilled gymnasts. Journal of Modern Rehabilitation. 2014; 8(1):28-34.
33. Matsusaka N, Yokoyama S, Tsurusaki T, Inokuchi S, Okita M. Effect of ankle disk training combined with tactile stimulation to the leg and foot on functional instability of the ankle. The American Journal of Sports Medicine. 2001; 29(1):25-30. [DOI:10.1177/03635465010290010901] [PMID] [DOI:10.1177/03635465010290010901]
34. Kaminski TW, Hartsell HD. Factors contributing to chronic ankle instability: A strength perspective. Journal of Athletic Training. 2002; 37(4):394-405. [PMID] [PMCID] [PMID] [PMCID]
35. Ali Zamani S, Ghasemi GA, Karimi A, Salehi H. [Pilates exercise effect on pain and general health of female patients with chronic low back pain (Persian)]. Journal of Research in Rehabilitation Sciences. 2011; 7(1):117-25.
36. Connors KA, Galea MP, Said CM, Remedios LJ. Feldenkrais Method balance classes are based on principles of motor learning and postural control retraining: A qualitative research study. Physiotherapy. 2010; 96(4):324-36. [DOI:10.1016/j.physio.2010.01.004] [PMID] [DOI:10.1016/j.physio.2010.01.004]
37. Panics G, Tallay A, Pavlik A, Berkes I. Effect of proprioception training on knee joint position sense in female team handball players. British Journal of Sports Medicine. 2008; 42(6):472-6. [DOI:10.1136/bjsm.2008.046516] [PMID] [DOI:10.1136/bjsm.2008.046516]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |